Abstract
Little is publicly known about coverage denials for medical services not meeting medical necessity criteria. We characterized the extent of these denials and their key features using Medicare Advantage claims for a large insurer from 2014–2019. In this setting, claims could be denied because of Traditional Medicare’s government coverage rules or additional Medicare Advantage private insurer rules. We observed $416M in denied spending, with 0.81 denials and $60 of denied spending per beneficiary annually. We found 1.40% of services were denied and 0.68% of total spending was denied, with rates rising over time. Traditional Medicare’s coverage rules accounted for 85% of denied services and 64% of denied spending; remaining denials were due to additional Medicare Advantage insurer rules. Denial rates varied greatly across service type and provider type, with the most denials for laboratory services and hospital outpatient providers. Traditional Medicare and Medicare Advantage insurer coverage policies each addressed different sources of medical spending; together, they contributed to denying a modest but nontrivial portion of payments.
Introduction
Coverage policy is an important tool for health insurers to influence health care use and spending. In principle, excluding targeted low-value services from coverage can reduce spending while discouraging unnecessary or harmful medical services.1,2 Targeting specific services thought to be low-value distinguishes coverage policies from broader benefit design tools like cost sharing or global budgets.
Several features of the US health care system may foster coverage limitations. Insurers face pressure to curb the large and rising share of the economy devoted to health care spending.3 Apparent widespread use of low-value services suggests many potential targets for restriction.4,5 In addition, electronic billing, now the norm,6 facilitates claims-based coverage adjudication and denials with high-volume automated claims processing.
Coverage limitations, however, face technical and political obstacles. Defining ineffective services can be challenging. Coverage denials are a source of frustration for physicians and patients. Although institutions like the Patient-Centered Outcomes Research Institute, the Institute for Clinical and Economic Review, and Choosing Wisely reflect growing interest in comparative effectiveness of medical services, it is not clear whether comparative effectiveness research has significantly informed coverage policies. Although the legal standard for Medicare coverage is that services be “reasonable and necessary”,7,8 Medicare still does not require clinical effectiveness evidence as part of its coverage determination process.7 According to a recent analysis of Medicare national coverage rules, only 18 new services were not covered from 2006–2010, and all new services were covered from 2011–2016.7
Basic descriptive facts about coverage denials remain unknown to physicians, researchers, and policymakers because of data limitations. Non-covered medical services are not readily identifiable in in the datasets traditionally used in health policy research such as adjudicated insurance claims or medical expenditure surveys. For example, while denied claims appear in standard Medicare claims datasets, there is no distinction between claims denied for medical necessity reasons and claims denied for administrative reasons like redundant claim submissions. As a result, little is publicly known about fundamental features of coverage denials such as frequency, amount of associated spending, types of services and providers facing denials, reasons for denial, and whether denials are increasing over time.
It is also largely unknown how coverage denials differ between private insurance and government-provided insurance. Medicare Advantage, the program that provides commercial health insurance to Medicare beneficiaries, provides a unique opportunity to examine this issue. In government-administered, fee-for-service Medicare, explicit coverage policies are made at both the national level by government officials and at the regional level by government contractors. However, the development of explicit coverage determinations only occurs following requests by the staff of CMS, its contractors, or external parties.7 As a result, many medical services have not been the subject of formal coverage determination policies and are implicitly covered because a billing code exists for the service.7 Private health insurers in Medicare Advantage must abide by all explicit Medicare coverage determinations including national coverage determinations (NCD) and local coverage determinations (LCDs). In the absence of an NCD, LCD, or other explicit Medicare coverage determination, however, Medicare Advantage insurers can apply additional coverage restrictions if they determine that a service fails to meet the “reasonable and necessary” standard.7
We characterized coverage denials in Aetna’s Medicare Advantage plans using data from all claims denied between 2014 and 2019. We examined the frequency of denials, amount of spending associated with them, service types and provider specialties facing denials, reasons for denial, and trends in denials over time. We also quantified and characterized the differences between denials resulting from Medicare coverage rules and from the private insurer’s additional coverage rules.
Study Data and Methods
Data Sources and Sample Population
We analyzed 2014–2019 medical claims for Medicare Advantage beneficiaries enrolled with Aetna. These proprietary data contained claims-based information on diagnoses and health care utilization as well as beneficiary age, sex, Medicaid dual eligibility, and Census tract sociodemographic characteristics (household income and race). All beneficiaries with at least one month of coverage in a group or individual Aetna Medicare Advantage medical plan were included in the analysis, yielding a sample of 2,884,583 beneficiaries with 6,987,217 beneficiary-year observations.
We studied institutional and professional claims for inpatient and outpatient medical services.7 Unlike standard sources of claims data, these claims provide detailed information about whether a claim was denied and why. Our analysis was restricted to claims whose coverage determination had been finalized. Finalized claims have been processed by the insurer so that duplicate claims for the same services have been eliminated. We did not study pharmacy claims covered under prescription drug plans because their coverage is not subject to Medicare NCD and LCD determinations; the analysis did include Part B-type drugs, which includes outpatient injectable and infused drugs administered by clinicians (e.g. chemotherapy).
Identification of Denied Services and Spending
The focus of our study was services denied for failing to meet a “reasonable and necessary” standard according to Medicare or Medicare Advantage insurer coverage criteria. These services were denied after they were performed, unlike denials during a prior authorization review. Claims processing codes allowed us to identify whether a service was denied on the basis of Medicare coverage rules (i.e. NCD, LCD or other governmental restrictions) or Aetna Medicare Advantage coverage rules. Aetna coverage rules and their justifications are described in Clinical Policy Bulletins (CPBs). As of this writing, Aetna has developed 975 CPBs, while Medicare has 348 NCDs and 1,234 LCDs.9,10 Coverage rules specify the clinical circumstances in which a service would or would not be covered as well as the service and diagnosis codes corresponding to those circumstances. Of note, CPBs are also used for coverage determination in Aetna’s non-Medicare insurance products. We excluded claim lines denied on the basis of administrative criteria such as a non-specific procedure code or coverage by an alternate insurance mechanism (e.g. such as a bundled payment for a separate claim or a fee-for-service Medicare hospice benefit). We also excluded denied claim lines with missing procedure codes (0.21% of denials) since procedure codes were necessary for imputing denied spending. After an initial review of denial classifications, we re-assigned all dental and per-visit home health denials initially assigned as Medicare Advantage denials to Traditional Medicare denials because Aetna advised us that Traditional Medicare rules were the reason for these denials.
For a small number of denials (less than 2% of denied services), it was necessary to impute whether the denial occurred because of Medicare rules or Medicare Advantage rules. For these services, claims processing codes did not specify which set of rules caused the denial. Instead, the codes indicated that medical review of the services had not been conducted by the insurer because the provider did not supply medical records. We attributed these denials to Medicare rules or to Medicare Advantage insurer rules probabilistically based on whether the procedure code was typically the subject of Medicare denials or Medicare Advantage insurer denials. For each procedure code, we calculated the proportion of denied claims in each category and imputed each claim’s category using those probabilities.
We calculated denied spending, the allowed charges that would have been paid had the service been covered, as follows. For each denied service, we imputed spending as the average allowed charges for paid claims sharing the same combination of procedure code, place of service, provider type, and geographic market. Geographic markets, ranging in size from large metropolitan areas to groups of less populous states, had been defined by the insurer for the purpose of business planning and performance tracking. For denials with no matching paid claims within this combination (5.1% of denied services), we used the average allowed charges sharing the combination of place of service, geographic market, and a service type category defined by similar procedure codes. For denials with no matching paid claims even within this combination, we used the average charge in a broader service type category (e.g. laboratory procedures instead of chemistry studies).
Analysis of Denied Services and Spending
To assess aggregate rates of service denials, we calculated the share of services and share of spending denied according to Medicare coverage rules and to Medicare Advantage insurer coverage rules, in aggregate and by year. Denominators for these share calculations included paid services and services denied due to coverage criteria. Confidence intervals were calculated via bootstrapping.
We summarized features of denied services according to characteristics of the denial, the service, and the provider. For services denied according to Medicare Advantage insurer coverage rules, we summarized the stated reasons for denial within six categories: cosmetic, experimental/investigational, not a treatment for disease, without proven efficacy, related to a primary denied service, and without supporting medical records provided. We analyzed types of denied services using broad and specific categories of procedure codes. Service categories were assigned using the insurer’s proprietary procedure code grouper, which categorizes procedure codes not only in the taxonomies of Current Procedural Terminology and Healthcare Common Procedure Coding System (92% of denied services in our sample), but also in other taxonomies for services such as anesthesia and rehabilitation. We summarized the distributions of denied spending and denied services across 17 broad categories of service types (e.g. laboratory procedures, radiology procedures) that were mutually exclusive and collectively exhaustive. We combined categories with small amounts of spending for brevity but included full results in the Online Appendix.11 We also tabulated shares of denied services and denied spending among the more specific service categories and individual procedure codes that were most represented among denials. For each service category, we calculated both the share of all denials within the category and the share of all services in that category (both paid and denied) that were denied. It was not feasible to briefly summarize the service category assignments for the several thousand procedure codes we analyzed. However, in the Appendix,11 we listed the broad and specific services category assignments for the procedure codes with the greatest amounts of denied spending, encompassing 90% of total denied spending.
Finally, we summarized the distribution of denied spending across provider type. Provider type was defined by the insurer and included professional clinical specialties (e.g. cardiology) and various categories for institutional claims (e.g. hospital emergency department or ambulatory surgical facility).
Study Oversight
The research protocol was deemed non-human subjects research by the relevant Institutional Review Board.
Limitations
Our study has several limitations. First, we studied retrospective coverage denials for medical services and not other dimensions of coverage restrictions such as prior authorization requirements or limits on prescription drug plan coverage. Low rates of denials after services are performed may reflect prior authorization policies, which confirm planned services meet medical necessity rules before they are performed; recent research verified that prior authorization policies are extensive.12 We did not include denials from Aetna’s concurrent review program, which evaluates whether hospitalizations meet coverage criteria prior to claim submission. We also excluded denied hospital claims with missing procedure codes, which totaled 0.2% of denied services. These exclusions may have led to a modest undercount of denied services.
Second, the scope and distribution of denials may differ for Medicare Advantage insurers other than Aetna. However, Aetna’s coverage policies appear to be fairly representative of coverage policies across Medicare Advantage plans; Aetna was recently shown to challenge physician claims at only modestly higher rates than other insurers, and it covers a similar proportion of specialty drugs as other commercial plans.13,14
Third, some of the denied claims we studied might have been paid if the providers had supplied accurate justifications for the services. If a provider error in documenting medical necessity led to the denial, then one might view the primary reason for the denial as an administrative criterion rather than clinical criterion. However, it was not possible to identify such cases in our data. Finally, although we categorized services denied by Aetna under Medicare coverage rules as Medicare denials, it is possible these claims may have been processed more leniently in fee-for-service Medicare. Even though NCD and LCD coverage policies are shared in fee-for-service Medicare and Medicare Advantage, the comprehensiveness of enforcement may differ.15
Results
Among Medicare Advantage beneficiaries in our sample, we detected 5,638,416 denials and $416M in denied spending due to Medicare or Medicare Advantage coverage criteria. This corresponded to 0.81 denials per beneficiary per year (95% CI 0.81–0.81) and $60 of denied spending per beneficiary per year (95% CI $59–60). Denied services accounted for 1.40% (95% CI 1.39–1.41) of total services (paid and denied services), and denied spending accounted for 0.68% (95% CI 0.67–0.70) of total spending (paid and denied spending). 31.7% of beneficiaries received one or more denied services per year (95% CI 31.7%–31.7%). (Data not shown.)
Appendix Exhibit A1 shows beneficiary characteristics overall and stratified by receipt of denied services.11
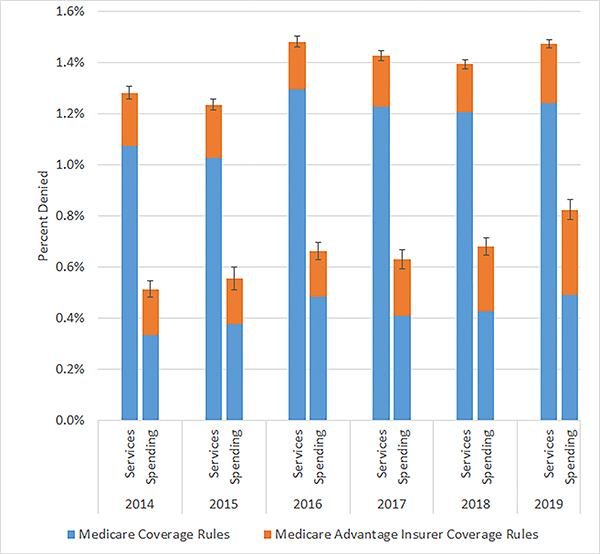
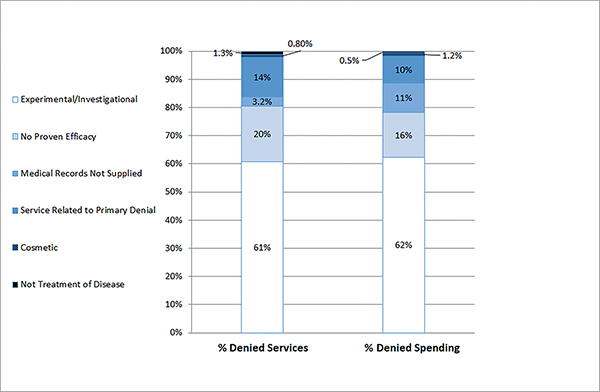
Exhibit 1 illustrates temporal trends in denial rates overall and by coverage criteria. On average, Medicare coverage rules accounted for 85% of denied services and 64% of denied spending, with Aetna Medicare Advantage coverage rules accounting for the remainder. From 2014 to 2019, denial rates increased from 1.3% of services to 1.5% and from 0.51% of spending to 0.83%, corresponding to relative increases of 15% and 60%, respectively. The proportion of denied spending attributable to Medicare rules decreased from 65% to 60%. Exhibit 2 shows the reasons services were denied under Aetna Medicare Advantage coverage rules. These services were most commonly classified as experimental or investigational (61% of denied services) or without proven efficacy (20% of denied services).
Exhibit 1 (Figure). Shares of Medicare Advantage spending denied under Traditional Medicare coverage rules and private insurer (Aetna Medicare Advantage) coverage rules, by year.
Source: Authors’ calculations, 2014–2019 Aetna Medicare Advantage claims.
Notes: Shares are presented as the percent of spending denied either due to Medicare coverage determinations or due to Aetna Medicare Advantage coverage rules. Share denominators include paid services and denials due to coverage criteria. Denials due to other (i.e. administrative) reasons and prescription claims are not included in share numerator or denominator values. Error bars represent 95% confidence intervals for total denials from both sets of coverage rules.
Exhibit 2 (Figure). Reasons for denial under Aetna Medicare Advantage coverage rules.
Source: Authors’ calculations, 2014–2019 Aetna Medicare Advantage claims.
Notes: Denial reasons, as assigned by the insurer, only apply to private insurer coverage rules and not traditional Medicare coverage determinations.
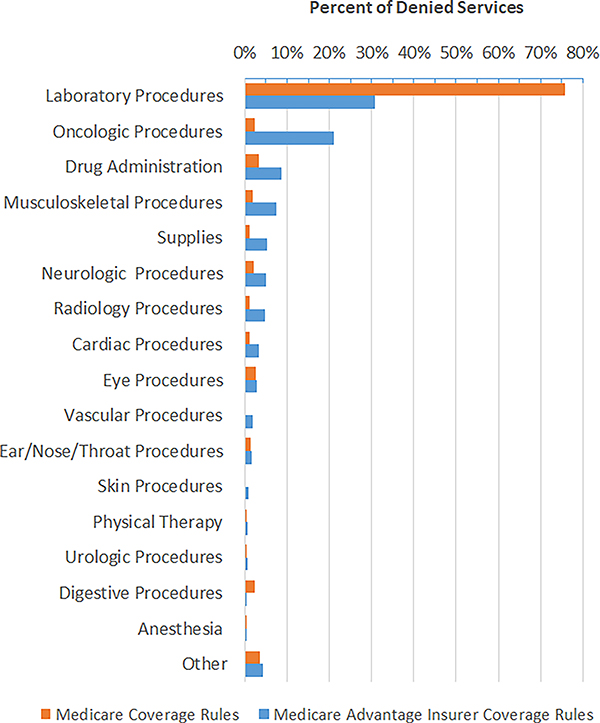
Exhibit 3 presents the distribution of denied services by broad service type. Most denied services were laboratory procedures, which were 76% of the services denied under Medicare rules and 31% of the services denied under Medicare Advantage rules. Nearly all denials under Medicare rules were laboratory services, whereas denials under Medicare Advantage insurer rules were less heavily concentrated in laboratory procedures. Appendix Exhibit A2 presents a corresponding distribution of denied services according to spending rather than service use.11 Laboratory services denials comprised 36% of spending denied under Medicare rules and 18% of spending under Medicare Advantage rules. Oncologic procedures and drug administration were the next greatest shares of spending denied under Medicare Advantage insurer rules (14% and 13%, respectively).
Exhibit 3 (Figure). Distribution of denials across broad service type.
Source: Authors’ calculations, 2014–2019 Aetna Medicare Advantage claims.
Notes: The share of denied services is presented for each service type, defined by broad service category The category “other” includes service categories with the least associated spending, collectively 4.2% of all denied spending. The denominator for each share is the total number of services denied within each category of coverage rules (traditional Medicare or Aetna Medicare Advantage).
Exhibit 4 presents the largest shares of denied spending and services by specific service type. Chemistry studies were the largest share of spending denied under Medicare (29%); chemotherapy was the largest share of spending denied under Medicare Advantage insurer rules (14%). However, as shown in Appendix Exhibit A6, only 0.9% of all chemotherapy spending (paid and denied) was denied under Medicare Advantage insurer rules, and only 7% of all chemistry study spending was denied under Medicare rules 11 See Appendix Exhibits A3─A6 for all rates of denied spending as shares of overall spending, and rates of denied services as share of overall services, by service category.11
Exhibit 4:
Largest denial shares by narrow service type
| Medicare Coverage Rules | Medicare Advantage Insurer Coverage Rules | ||||
|---|---|---|---|---|---|
| Specific Service Type | Denied Spending Share | Denied Services Share | Specific Service Type | Denied Spending Share | Denied Services Share |
|
| |||||
| Chemistry studies | 29.0% | 56.9% | Chemotherapy | 13.6% | 1.8% |
| Vascular procedures, other | 5.5% | 2.4% | Chemistry studies | 11.2% | 19.3% |
| Drug administration | 4.1% | 0.7% | Drug administration | 9.4% | 10.5% |
| Microbiology studies | 3.7% | 8.4% | Supplies | 6.9% | 5.4% |
| Self-injected drug administration | 3.1% | 0.1% | Microbiology studies | 6.3% | 11.1% |
| Vascular access procedures | 2.6% | 1.3% | Percutaneous coronary intervention | 3.3% | 0.2% |
| Rehabilitation or Physical Therapy | 2.3% | 2.2% | Miscellaneous administrative codes | 2.9% | 0.4% |
| Supplies | 2.3% | 1.1% | Knee arthroscopy | 2.7% | 2.2% |
| Chemotherapy | 2.1% | 0.1% | Neurologic procedures, other | 2.6% | 0.1% |
| Skin lesion biopsy/excision | 1.9% | 0.9% | Major vascular procedures | 2.5% | 10.1% |
| Neurologic procedures, other | 1.9% | 0.5% | Vascular access procedures | 2.3% | 3.5% |
| Anesthesia | 1.8% | 0.5% | Ultrasound | 2.1% | 0.5% |
| Echocardiography | 1.6% | 0.6% | Nasal/sinus endoscopy | 2.0% | 0.9% |
| Pacemaker or defibrillator procedure | 1.6% | 0.0% | Eye Procedures - Other | 2.0% | 1.1% |
| Peripheral nerve procedures | 1.5% | 0.0% | EEG | 2.0% | 0.1% |
|
| |||||
| Total | 65.1% | 75.6% | Total | 71.6% | 67.2% |
Source: Authors’ calculations, 2014–2019 Aetna Medicare Advantage claim
Notes: The shares of denied services and denied spending are presented for the 15 specific service categories accounting for the greatest shares of denied spending. The denominator for each share is the total number of services or total spending that was denied within each category of coverage rules (Medicare or Medicare Advantage).
Institutional providers accounted for the greatest shares of denied spending (Appendix Exhibit A7).11 Hospital outpatient departments accounted for 35% of denied spending, laboratories 20%, and emergency departments 5.3%. Family practice providers and cardiologists accounted for the next greatest shares of denied spending (3.0% and 2.5%, respectively).
Denied claims contained 5,058 unique procedure codes. The most frequent was for glycosylated hemoglobin (A1C) testing, which constituted 9% of services denied under Medicare rules. The procedure accounting for the greatest amount of denied spending was Vitamin D testing. See Appendix Exhibits A8 and A911 for other services accounting for the most frequent denials and greatest amounts of denied spending.
Discussion
Although health insurers may deny payment for medical services failing to meet medical necessity criteria, the frequency and circumstances of these denials has not been established. In this study of a large Medicare Advantage insurer, approximately 1 in 70 services was denied under medical necessity rules. Although denied spending was less than 1% of annual spending, this rate grew over time and aggregate denied spending totaled hundreds of millions of dollars. While prior studies have documented aggregate rates of claim denials,14,16 these studies did not distinguish between denials due medical necessity rules and denials due to common administrative issues like incomplete or redundant claims. Our findings provide initial evidence on the restrictiveness of government and private insurer medical necessity policies in Medicare, which led to payment denial for modest but nontrivial portions of medical services and medical spending.
Medicare Advantage coverage rules accounted for one third of denied spending, demonstrating how private insurer rules supplement government coverage restrictions in Medicare. Prior research comparing health care spending in Medicare Advantage and Traditional Medicare has suggested that Medicare Advantage lowers spending by reducing health care utilization;17–20 it is not clear, however, whether more restrictive coverage policies have been a mechanism behind these spending reductions. Though Medicare Advantage insurers have been shown to challenge physician claims more than Traditional Medicare, that analysis did not specifically examine challenges due to clinical coverage criteria.14
Although Medicare Advantage insurers can enforce the coverage criteria they produce, denials are subject to a regulated appeals process and inappropriate denials can result in penalties such as reductions in plan Star Rating.21,22 Notably, in-network providers are not permitted to charge patients money for the services denied under the private insurer coverage rules. Data from Affordable Care Act marketplace plans indicate that appeals of denied claims are rare.23
Our results also illustrate differences in the types of services subject to government coverage rules versus private insurer coverage rules in Medicare. We found that a large majority of services denied under Traditional Medicare coverage rules were laboratory services, and the plurality of denied spending was for chemistry tests such as Vitamin D or glycosylated hemoglobin levels, which tend to be common and low-priced. These laboratory claims tend to be denied because they lack appropriate diagnosis codes. Medicare has instituted extensive diagnostic coding requirements for laboratory services; the most recent Medicare manual on laboratory diagnostic coding is over 2,000 pages long.24 In contrast, Medicare Advantage insurer restrictions tended to affect rarer, higher-priced services including chemotherapy. Although less than one percent of chemotherapy spending was denied according to these coverage rules, such denials constituted a high proportion of denied spending because of the high price of these services. This finding aligns with prior research showing that private insurers have instituted more extensive coverage rules for high-priced infusion drugs than Medicare has.12
Our results may represent a lower bound on the savings achieved for services subject to coverage denials because estimates did not include services deterred by the coverage restrictions and therefore never performed, i.e., a sentinel effect. Deterring an inappropriate service would be preferable to denying it retrospectively for patients, providers, and insurers. There is limited and mixed evidence on the extent to which coverage policies deter medical services. One study found little evidence of deterrence of eight medical services shortly after they were subject to Medicare coverage restrictions,25 while another showed large reductions for a service targeted by coverage restrictions and antifraud enforcement.26 Some portion of savings achieved by denials, however, are eroded by the administrative costs of developing and enforcing coverage policies, and by the expense of any substitute services performed in place of the denied services.27
Coverage policy is a unique tool for addressing overuse of health care services. Unlike other broad incentives to reduce health care spending such as cost sharing or global budgets, coverage policies can provide more nuanced incentives based on evidence-based determinations of service necessity. By describing the scope and distribution of coverage denials in Medicare Advantage, our study provides a glimpse into how this managed care tool has been shaped and wielded. In this setting, government and private insurer coverage criteria have contributed to defining a small portion of medical care as unnecessary. How much larger this portion would be if deterred services could be quantified is unknown.
Supplementary Material
Contributor Information
Aaron L. Schwartz, University of Pennsylvania and Corporal Michael J. Crescenz Veterans Affairs Medical Center, Philadelphia, Pennsylvania.
Yujun Chen, CVS Health, New York, New York..
Chris L. Jagmin, CVS Health, Woonsocket, Rhode Island.
Dorothea J. Verbrugge, CVS Health, Woonsocket, Rhode Island.
Troyen A. Brennan, CVS Health, Woonsocket, Rhode Island.
Peter W. Groeneveld, University of Pennsylvania and Corporal Michael J. Crescenz Veterans Affairs Medical Center.
Joseph P. Newhouse, Harvard University and National Bureau of Economic Research, Cambridge, Massachusetts.
References
- 1.Garber AM. Evidence-based coverage policy. Health Aff. (Millwood) 2001;20(5):62–82. [DOI] [PubMed] [Google Scholar]
- 2.Mark Fendrick A, Smith DG, Chernew ME. Applying value-based insurance design to low-value health services. Health Aff. (Millwood) 2010;29(11):2017–21. [DOI] [PubMed] [Google Scholar]
- 3.National Health Expenditure Data | CMS [Internet]. 2020. [cited 2020 Jul 15]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData
- 4.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med. 2014;174(7):1067–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colla CH, Morden NE, Sequist TD, Schpero WL, Rosenthal MB. Choosing Wisely: prevalence and correlates of low-value health care services in the United States. J Gen Intern Med. 2015;30(2):221–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CAQH. 2020 CAQH Index - Closing the Gap: The Industry Continues to Improve, But Opportunities for Automation Remain. Washington DC:. 2021. Accessed Oct 12, 2021. Available from: https://www.caqh.org/sites/default/files/explorations/index/report/2020%20CAQH%20index%20report.pdf
- 7.Medicare Payment Advisory Commission. Medicare coverage policy and use of low-value care. In: Medicare and the Health Care Delivery System; [Internet]. 2018. p. 293–363. Available from: http://www.medpac.gov/docs/default-source/reports/jun18_ch10_medpacreport_sec.pdf?sfvrsn=0 [Google Scholar]
- 8.Neumann PJ, Chambers JD. Medicare’s Enduring Struggle to Define “Reasonable and Necessary” Care. N Engl J Med. 2012;367(19):1775–7. [DOI] [PubMed] [Google Scholar]
- 9.Aetna. Medical CPBs [Internet]. [cited 2021 Feb 9]. Available from: https://www.aetna.com/health-care-professionals/clinical-policy-bulletins/medical-clinical-policy-bulletins/numeric-order.html
- 10.Centers for Medicare and Medicaid Services. Medical Coverage Database [Internet]. [cited 2021 Feb 9]. Available from: https://www.cms.gov/medicare-coverage-database/indexes/national-and-local-indexes.aspx [Google Scholar]
- 11. To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 12.Schwartz AL, Brennan TA, Verbrugge DJ, Newhouse JP. Measuring the Scope of Prior Authorization Policies. JAMA Heal Forum [Internet]. 2021. May 28 [cited 2021 Jun 4];2(5):e210859. Available from: https://jamanetwork.com/journals/jama-health-forum/fullarticle/2780396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chambers JD, Chenoweth M, Thorat T, Neumann PJ. Private Payers Disagree With Medicare Over Medical Device Coverage About Half The Time. Health Aff [Internet]. 2015. Aug 2 [cited 2020 Jul 15];34(8):1376–82. Available from: http://www.healthaffairs.org/doi/10.1377/hlthaff.2015.0133 [DOI] [PubMed] [Google Scholar]
- 14.Gottlieb JD, Shapiro AH, Dunn A. The complexity of billing and paying for physician care. Health Aff (Millwood). 2018;37(4):619–26. [DOI] [PubMed] [Google Scholar]
- 15.Foote SB, Town RJ. Implementing evidence-based Medicine through Medicare coverage decisions. Health Aff [Internet]. 2007. Nov;26(6):1634–42. Available from: http://www.healthaffairs.org/doi/10.1377/hlthaff.26.6.1634 [DOI] [PubMed] [Google Scholar]
- 16.Kapur K, Gresenz CR, Studdert DM. Managing care: utilization review in action at two capitated medical groups. Health Aff (Millwood). Jan-Jun 2003;Suppl Web Exclusives:W3-275–82. [DOI] [PubMed] [Google Scholar]
- 17.Curto V, Einav L, Finkelstein A, Levin J, Bhattacharya J. Health care spending and utilization in public and private medicare. Am Econ J Appl Econ 2019;11(2):302–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Landon BE, Zaslavsky AM, Saunders RC, Pawlson LG, Newhouse JP, Ayanian JZ. Analysis Of Medicare Advantage HMOs compared with traditional Medicare shows lower use of many services during 2003–09. Health Aff [Internet]. 2012. Dec 2 [cited 2020 Oct 16];31(12):2609–17. Available from: http://www.healthaffairs.org/doi/10.1377/hlthaff.2012.0179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duggan M, Gruber J, Vabson B. The consequences of health care privatization: Evidence from medicare advantage exits. Am Econ J Econ Policy. 2018;10(1):153–86. [Google Scholar]
- 20.Geruso M, Layton T. Upcoding: Evidence from Medicare on squishy risk adjustment. J Polit Econ. 2020;128(3):984–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Code of Federal Regulations, Special rules for ambulance services, emergency and urgently needed services, and maintenance and post-stabilization care services. 42 CFR § 422.113 Available at https://www.ecfr.gov/current/title-42/chapter-IV/subchapter-B/part-422/subpart-C/section-422.113 (accessed 17 Oct. 2021).
- 22.Centers for Medicare & Medicaid Services. Medicare 2020 Part C & D Star Ratings Technical Notes [Internet]. 2019. Available from: https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/Downloads/Star-Ratings-Technical-Notes-Oct-10-2019.pdf
- 23.Pollitz K, McDermott D. Claims Denials and Appeals in ACA Marketplace Plans. Issue Brief, KFF, Washington DC: 2021. [cited 2021 Sep 15]. Available from: https://www.kff.org/private-insurance/issue-brief/claims-denials-and-appeals-in-aca-marketplace-plans/ [Google Scholar]
- 24.Centers for Medicare and Medicaid Services. Medicare National Coverage Determinations (NCD) Coding Policy Manual and Change Report (ICD-10-CM): Clinical Diagnostic Laboratory Services [Internet]. Baltimore, MD; 2021. Available from: https://www.cms.gov/Medicare/Coverage/CoverageGenInfo/LabNCDsICD10
- 25.Foote SB, Virnig BA, Town RJ, Hartman L. The impact of medicare coverage policies on health care utilization. Health Serv Res. 2008;43(4):1285–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Howard DH, McCarthy I. Deterrence effects of antifraud and abuse enforcement in health care. J Health Econ. 2021. Jan 1;75:102405. [DOI] [PubMed] [Google Scholar]
- 27.Parikh RB, Fishman E, Chi W, Zimmerman RP, Gupta A, Barron JJ, et al. Association of Utilization Management Policy with Uptake of Hypofractionated Radiotherapy among Patients with Early-Stage Breast Cancer. JAMA Oncol. 2020;6(6):839–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.