Abstract
Equality, equity, and parity in the workplace are necessary to optimize patient care across all aspects of medicine. Gender-based inequities remain an obstacle to quality of care, including within the now majority women subspecialty of gynecologic oncology. The results of the 2020 SGO State of the Society Survey prompted this evidence-based review. Evidence related to relevant aspects of the clinical care model by which women with malignancies are cared for is summarized. Recommendations are made that include ways to create work environments where all members of a gynecologic oncology clinical care team, regardless of gender, can thrive. These recommendations aim to improve equality and equity within the specialty and, in doing so, elevate the care that our patients receive.
Background
All gynecologic oncology healthcare team members, regardless of gender, should have equal opportunities to be hired, supported, and advance in their careers. The professional tenet of physicians is, first, do no harm. This is interpreted to focus on patient care, but harm comes in many forms, including the environment in which the healthcare team learns, trains, grows, practices, and under which patients receive care. Gender impacts each of these elements of the clinical care delivery setting. Documented gender-based professional inequities persist within the majority-women field of obstetrics and gynecology (OBGYN), and its subspecialty gynecologic oncology (GO) [1–5]. A review of the evidence, focusing on understanding how to remedy these inequities, will benefit us all by improving the work environment for future generations. Gender bias and its resultant effects, including harassment, discrimination, microaggressions, and attrition are pervasive and long-standing within medicine. Women and men did not matriculate into medical schools at equal rates until 2003, despite the passage of Title IX in 1972 removing quotas on the numbers of women entering medical schools [6]. Since the 1990s, OBGYN has been one of the preferred specialties for women medical students entering residency training. Women now constitute 83% of OBGYN residents and 64% of full-time OBGYN faculty [7]. An increasing number of women entering GO has ensued. The Society of Gynecologic Oncology (SGO) 2020 State of the Society Survey (SGO SOSS, see footnote1) reported 54% of gynecologic oncologists self-identified as female, the first time women made up the majority of the membership [1]. Notably, all advanced practice provider respondents also identified as women.
This document summarizes the current state of gender equity in GO and provides solutions for eliminating existing disparities (Table 1). This content primarily applies to people who self-identify as women but can be extended to people of all genders. There is a paucity of data related to non-binary individuals. The terms “woman” and “women” are used throughout the manuscript to reflect gender for brevity and clarity but are not meant to exclude non-binary persons.
Table 1:
Recommendations
| 1. All members of the health care team, including gynecologic oncology teams, must have equal opportunities to be hired, supported, and advance in their careers. |
| 2. Institutions should develop systems for reporting sexual misconduct, apply zero tolerance policies to harassment and enforce existing laws prohibiting discrimination. |
| 3. Inclusion of team members from any gender, race, ethnicity and any intersections must be intentional, unbiased and merit-based to foster productive environments where all persons can thrive. |
| 4. Bidirectional teaching metrics should be concrete and objective; feedback should be presented in a constructive and supportive manner regardless of age, gender, race or ethnicity. |
| 5. Creation of clinical and surgical workplaces with equitable physical, emotional, and material support, as well as fairly-distributed referrals and clinical opportunities to gynecologic oncologists of all genders, will improve the profession and benefit patient care. |
| 6. Transparent and gender-neutral mechanisms and metrics for mentorship, advancement to leadership, and inclusion in professional activities should be developed and promoted to yield objective merit-based opportunities and promotion. |
| 7. Empowering wellness strategies across the discipline and attention to work-life integration, including respect for individual choices regarding pregnancy and parenting, will ultimately result in improved long-term productivity and retention for GOs of any gender. |
| 8: Equitable support and transparency in metrics will provide equity in compensation on an individual level; structural inequities must be addressed to correct inequities in compensation for the specialty. |
RECOMMENDATION 1:
All members of the health care team, including gynecologic oncology teams, must have equal opportunities to be hired, supported, and advance in their careers.
Bias, Discrimination, and Harassment
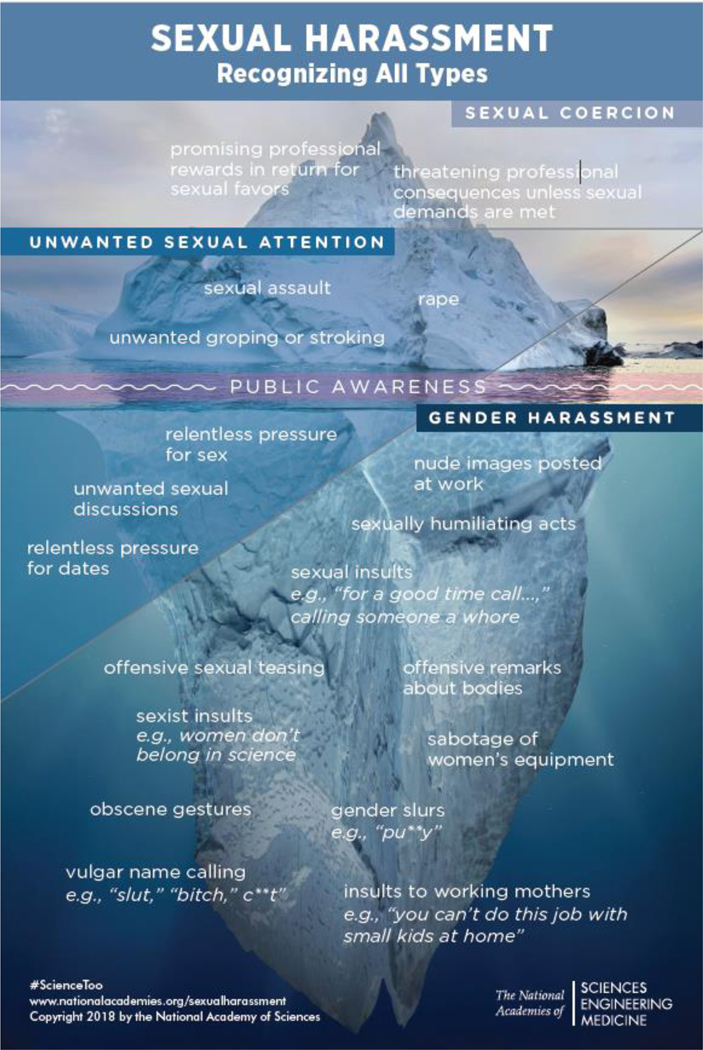
Gender bias, discrimination, and harassment persist despite significant advances and the inclusion of women in medicine [2, 6, 8–10]. A 2018 report of the National Academies of Sciences, Engineering, and Medicine (NASEM), entitled “Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine” explored the influence of sexual harassment on the career advancement of women in the scientific, technical and medical workforce and provided descriptive terminology for gender equity (Table 2)[8]. Central to the NASEM report is that the minority of sexual harassment is easily observed. Most is subtle and hidden from view (Figure 1). In the report, the frequency of gender harassment among women during medical school was 45%, significantly higher than for women pursuing graduate education in science or engineering [8]. A recent survey of GOs, reported that 71% of women experience sexual harassment. Few who experienced discrimination and harassment (14.5%) reported their experience. Women were more likely than men to report that the experience impacted their career advancement or compensation [3].
Table 2:
Definitions Relevant to Gender Equity[8]
| Term | Definition |
|---|---|
| Sex | A biological classification based on an individual’s chromosomes, gonads, sex hormones, external reproductive organs, and internal genitalia. |
| Gender | Socially constructed and enacted roles and behaviors that occur in a historical and cultural context and vary across societies and over time. Individuals act in many ways that fulfill or challenge the gender expectations of their society |
| Gender Bias | Deeply ingrained societal differential responses toward women and men as a result of long-term habitual behavior. Bias can be explicit defined as conscious, or implicit defined as outside of conscious awareness or control. |
| Discrimination | Making unjustified distinctions between human beings based on the groups, classes, or other categories to which they are perceived to belong |
| Sexual Harassment | A type of sex/gender discrimination that encompasses gender harassment, unwanted sexual attention, and sexual coercion |
| • Gender harassment | Verbal and nonverbal behaviors that convey hostility, objectification, exclusion, or second-class status about members of one gender |
| • Unwanted sexual attention | Unwelcome sexual advances, which can include assault |
| • Sexual coercion | A type of sexual harassment in which favorable professional or educational treatment is conditioned on sexual activity (such as through the use of bribes or threats) |
|
Microaggression/
Incivility |
Brief and commonplace daily verbal, behavioral, or environmental indignities, whether intentional or unintentional, that communicate hostile, derogatory, or negative messages |
Figure 1:
Most sexual harassment is subtle and hidden from view[8]
Harassment related to gender systematically creates an environment that diminishes respect for and power of women in the workplace, contributing to the attrition of women from medicine. In addition, it negatively impacts bystanders, team members, learners, institutions, and, importantly, the delivery of health care[8, 10, 11]. Harassment is more likely tolerated in environments where bias and discrimination are permitted[8].
Implicit biases have hindered the inclusion of women as equal participants in medical culture[8]. Negative stereotypes include lack of commitment due to work absence, desire for part-time status, and disinterest in leadership positions [8, 12]. Microaggressions can augment the recipient physician’s experience of discrimination while reinforcing incorrect prevailing perceptions [8, 13]. The effects of bias and discrimination extend to bystanders, who may be similarly negatively impacted by bearing witness to these events, eroding institutional and organizational trust and potentially diminishing workplace function [14–16]. “Upstanding” – speaking or acting in support of an individual or cause, on behalf of a person being attacked or bullied – has been proposed as a method to combat the negative effects of microaggressions in the workplace that can be easily implemented by members of any healthcare team [16].
RECOMMENDATION 2.
Institutions should develop systems for reporting sexual misconduct, apply zero-tolerance policies to harassment and enforce existing laws prohibiting discrimination.
Diversity, Inclusion and Intersectionality
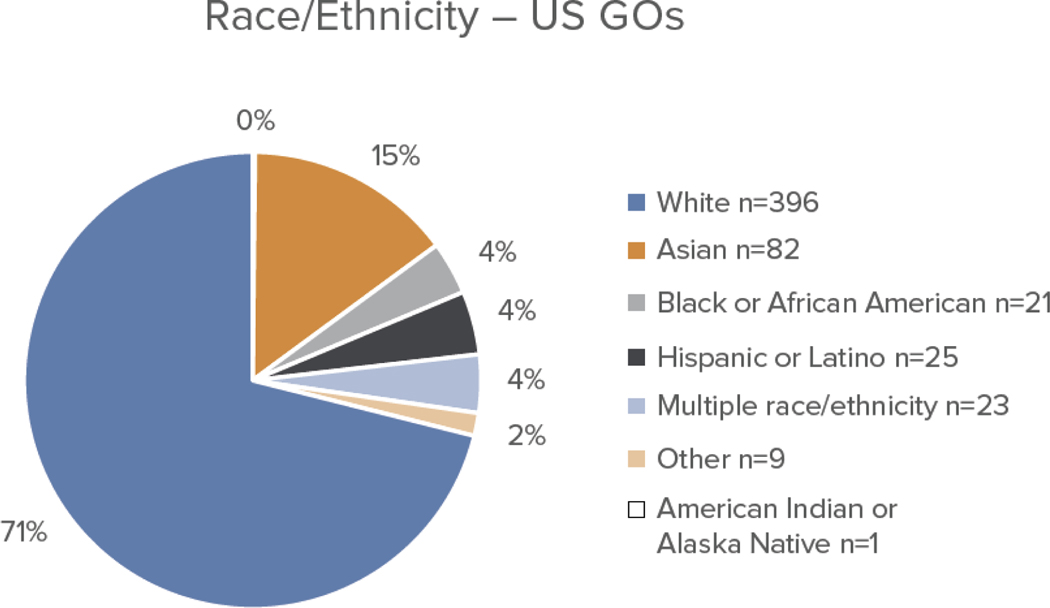
Women physicians from racial and ethnic groups, historically underrepresented in medicine (URM), are the least represented among U. S. academic faculty across all subspecialities, including GO [17]. The SGO membership has become more diverse over time, with 30% of GOs self-identifying as being from racial or ethnic groups historically underrepresented in medicine in the 2020 SOSS (Figure 2), compared to 13% in 2005. Diversity is critical to the success of any organization, with multiple studies revealing that more diverse leadership leads to increased productivity, creativity and improved outcomes [18, 19]. Diversity in this sense applies not only to gender but to race, ethnicity, sexual preference, ability and more. Intersectional identities multiply an individual’s risks of experiencing harassment, discrimination and bias. Women with multiple under-represented identities, such as being a sexual-minority or of color, experience harassment in the workplace more frequently than White women leading to greater negative results on evaluation of job performance, satisfaction, and retention [8, 15].
Figure 2:
Race/ethnicity reported by gynecologic oncologists in the SGO 2020 State of the Society survey[1](see footnote)
RECOMMENDATION 3:
Inclusion of team members from any gender, but also race, ethnicity and any intersections must be intentional, unbiased and merit-based to foster productive environments where all persons can thrive.
Education, Training and the Learning Environment
Fostering safe and equitable learning experiences for all trainees will ensure that the next generation of GOs is prepared with the skills and competence to provide excellent care to persons with gynecologic cancers. Women trainees in OBGYN programs report lower rates of discrimination than those in male-majority surgical environments, however a majority women physician workforce has been insufficient to eliminate workplace sexism [20–23]. A cross-sectional survey of over 7000 general surgery residents revealed that 65.1% of women compared to 10% of men reported gender-based discrimination. Notably, discrimination was perceived as initiated by patients, family members, nurses, hospital staff, and attending surgeons, all interactions relevant to trainees in OBGYN and GO [22]. Similar rates of gender-based discrimination were found in studies of residents from multiple surgical disciplines that included OBGYN trainees [20, 23]. Women surgical trainees who report frequent and severe microaggressions are more likely to experience burnout or leave medicine [22, 24].
Progressive autonomy and objective feedback are critical to medical and surgical training; however, gendered differences in the delivery of both are common. Within the OBGYN clerkship, medical students who are men receive more opportunities to perform procedural tasks [25]. Women surgical residents receive less autonomy from faculty than do male residents, even when controlling for potential confounders such as level of training, intrinsic procedural difficulty, patient-related case complexity, faculty gender, and training program environment [26, 27]. Trainees who are men receive more positive, consistent, and concrete advice related to skills and performance while women receive conflicting and often even contradictory messaging around performance, as well as more frequent commentary related to personality and attitude[28–30]. Furthermore, protective hesitation, the practice of not providing clear and consistent feedback to women due to worry about the recipients’ response, leaves women less likely to get constructive or actionable feedback[31].
Gender bias in the learning environment is bidirectional. Medical students are more likely to evaluate women attending physicians negatively regardless of the medical student gender, particularly if the attending physicians are surgeons [32–34]. A stereotypical “warm” teaching style improves perceptions of likeability for women in academics but backfires by lowering assessments of competence, while a “cold”, or “stiff” demeanor is perceived as more competent [34].
RECOMMENDATION 4.
Bidirectional teaching metrics should be concrete and objective; feedback should be presented in a constructive and supportive manner regardless of age, gender, race or ethnicity.
The Clinical Environment and Support
Common perceptions of gender roles related to medicine are held as frequently by health professionals as they are amongst members of the general population [12]. Men are more likely to be associated with procedural or technical specialties and a career in a surgical field; whereas, women are considered more suited for communal specialties such as family medicine [12, 35]. Patients, staff and colleagues have biases that often require time and energy for women surgeons to correct and influence their professional communication [36]. This expenditure is multiplied for GOs, due to the volume and heterogeneity of required interactions across varied clinical realms: the clinic, infusion suite, operating room, and ICU. The accumulation of microaggressions related to gender can leave individual members of the patient care team primed for disappointment, discomfort, and/or stress which is ultimately an obstacle to optimal patient care [36, 37].
Expectations that differ for surgeons who are women influence interactions with patients. Extra time is often required to develop credibility with patients and families to overcome misconceptions surrounding women’s role in healthcare as nurses or medical support staff, rather than as surgeon, expert or senior physician [38]. Patients often assume women physicians will spend more time in their explanations and display more empathy than men [39]. Referral patterns reflect these gendered expectations, as referrals for more emotional or “needy” patients are more often sent to women. These consults are often time-consuming, and less likely result in revenue generating procedures or surgery [40]. After a surgical complication, women surgeons face greater and more generalized backlash, experiencing a sharper drop in reputation and in referrals; whereas similar mishaps for men are infrequently widely shared or addressed [40].
Gender influences operating room teamwork and efficiency. Gender congruency across the surgical team has been correlated, paradoxically, with higher levels of discord. Operating room staff remain predominantly women, leaving women gynecologic surgeons at higher risk for conflict and lack of cooperation in the surgical environment [41, 42]. These interpersonal interactions have downstream effects on patient care. The “decision to incision” time for emergent trauma surgery was significantly longer for women surgeons paired with women operating room staff, compared to other surgeon/staff combinations [43].
The 2020 SGO SOSS identified gender-associated differences in clinical activities which are summarized in Table 3. GOs who are women reported spending equal times in clinical activities as men but are more likely than men to prescribe chemotherapy, a time-consuming and less lucrative aspect of gynecologic oncology practice. Additionally, whereas women GOs report overall fewer surgical cases per year, with case volume reports certainly subject to recall, selection, confirmation and other biases, there is an apparent additional imbalance in ovarian, cervical and vulvar cancer cases relative to endometrial cancer cases. This uneven distribution of cases suggests that women GOs are performing fewer complex GO cases which may then contribute in a circular fashion to perceptions of their abilities across the profession. GOs who are men self-reported being supported by more total clinical staff and equivalent research staff although women report a larger percentage of their time devoted to research activities compared to men.
Table 3.
Practice characteristics by gender from the 2020 SGO State of the Specialty Survey [1]
| Male (n=312) | Female (n=367) | P-value | |
|---|---|---|---|
| Clinical Activities | |||
| - Chemo Prescribing | 73% | 82% | 0.004 |
| - 2+ hospitals | 37% | 39% | 0.639 |
| - Intraoperative consults | 75% | 77% | 0.363 |
| - Medical admissions | 75% | 77% | 0.568 |
| - OB coverage | 61% | 64% | 0.450 |
| - ED coverage | 67% | 74% | 0.075 |
| % FTE time | |||
| - Clinical | 63 | 63 | 1.000 |
| - Research | 19 | 26 | 0.005 |
| - Admin | 15 | 13 | 0.981 |
| - Teaching | 10 | 9 | 0.183 |
| Case Volumes/year | |||
| - Cervix | 20.8 | 13.4 | 0.005 |
| - Corpus | 74 | 65 | 0.075 |
| - Ovary | 34.6 | 26 | 0.008 |
| - Vagina/Vulva | 11.5 | 8 | 0.001 |
| - Benign Cases/month | 26.1 | 13.5 | 0.034 |
| FTE support | |||
| - Staff (Practice) | 8.6 | 5.8 | 0.038 |
| - Staff (Hospital) | 11.9 | 10.1 | 0.144 |
| - Total Staff | 19.3 | 14.8 | 0.010 |
Values are reported as % for clinical activities and FTE and median for case volumes and FTE support. Categorical values were evaluated with chi-squared tests; continuous variables with were compared using Mann-Whitney testing.
RECOMMENDATION 5:
Creation of clinical and surgical workplaces with equitable physical, emotional, and material support, as well as fairly-distributed referrals and clinical opportunities to gynecologic oncologists of all genders, will improve the profession and benefit patient care.
Advancement and Leadership
Women in GO face persistent barriers to promotion and advancement in academic rank [4, 7, 44]. Despite large numbers of women practicing within the specialty, the likelihood of advancement for women in OBGYN is similar to that of other specialties. Within OBGYN, the number of women department chairs lags behind expected rates when quantified by the gender composition of historical residency cohorts [44]. As a minority of OBGYN department chairs are GOs, the complex concerns unique to the care of women with gynecologic cancers may be far removed from the day-to-day affairs of most OBGYN chairs. [4, 45]. Further, the value of women in GO and the care of people with gynecologic cancers are compromised by cancer center leadership, which remains overwhelmingly male, and is rarely centered on gynecology [4, 45]. Gender and specialty leadership gaps likely disadvantage women GOs who require advocacy for clinical support, leverage for participation in basic, translational and clinical research, and assistance in mitigating the gender bias experienced within their clinical and research environments [4].
Advancement in academics is largely dependent on scholarly productivity and publications. Although male GO faculty had significantly higher h-indices at the assistant professor level, this difference disappeared as faculty advanced in rank suggesting that the potential for scholarly activities are similar regardless of gender [46]. Authorship among women GOs has been increasing over time, reflecting the increasing percentages of women in the field; however, senior authorship has lagged [47]. Women remain underrepresented in leadership across major medical journals, including those focused on women’s health [48, 49]. A lack of diversity in these influential positions limits opportunity for networking for women and URM, and may influence selection of reviewers and publication outcomes threatening intellectual diversity and widening academic achievement gaps [50]. A publication bias in the peer review process has been described, perhaps as a downstream effect of the relative paucity of women in editorial positions. Research conducted in women is less likely to be accepted for publication than the same research conducted in men, despite comparable scientific rigor and higher ratings of scientific impact[51].
Grant funding, including mentored career development awards, is, on average, less for women than men [52, 53]. The transition rates to R01 funding are lower for women who receive early career funding than that of men [53]. In addition, historically, the National Institutes of Health (NIH) has applied a disproportionately lower share of its resources to diseases that primarily affect women [54]. NIH funding to OBGYN departments is disproportionately low, representing less than 1% of NIH funding [55]. Gynecologic cancers rank in the bottom half of funding allocation from the National Cancer Institute when benchmarked to lethality indices [56].
Active mentorship and sponsorship have been part of every successful evidenced-based intervention to improve leadership attainment, yet identifying mentors remains more challenging for women at every level of development [57]. Women prefer gender-concordant mentorship, yet women remain underrepresented in leadership, meaning the reach of female advocacy may be limited compared to that provided by male mentors[58]. Women are more likely to report their work being used by their mentor to advance the mentor’s career rather than that of the mentee [59]. Faculty needs assessments may help develop programs focused on supporting women. Cross-institutional or cross-specialty mentorship programs should be considered and encouraged.
RECOMMENDATION 6:
Transparent and gender-neutral mechanisms and metrics for mentorship, advancement to leadership, and inclusion in professional activities should be developed and promoted to yield objective, merit-based opportunities and promotion.
Wellness and Work-Life Balance
The prevalence of burnout, characterized by high rates of emotional exhaustion, depersonalization, and low personal accomplishment, is high in medicine, and notably high among GOs [1, 60, 61]. Women GOs were more likely to self-report burnout in the 2020 SOSS, with preliminary analysis showing a concerning increase in burnout for women compared to men. Similarly, there also appears to be an increase in negative mental health indexes among women. These data will be further detailed in an upcoming publication from the SGO Wellness Committee and SOSS Task Force.
A consistent contributor to burnout for women in medicine and surgery is the disproportionate share of household management and childcare tasks typically assigned to women [62, 63]. Therefore, institutional “time banks” where activities that support the success of the team or institution (e.g. stepping up to fill a clinical shift at the last minute) can be ”traded” for work or home support services should be considered [64].
Pregnancy and parenting disproportionately impact women in medicine. Overall, , women GOs perceive the responsibility of parenting to diproportionately affect academic opportunities for women more than men, women GOs perceive parenting negatively affects academic opportunities more than men [65]. Institutional standards for allowed time off for pregnancy and parenting are often less than the 12 weeks recommended by ACOG[2, 65, 66]. Additionally, perceived pressures or financial considerations may lead to shortening of parental leave. Retaliation by colleagues following parental leave is commonly perceived by physician mothers[67]. Resident physicians are covered typically by coresidents who are infrequently compensated and frequently expected to be “repaid” in kind [66]. The use of 12-week parental leave may lead to required extensions in training and impact fellowship start dates and potentially delay board certification [2, 68]. Physicians working in incentive-based reimbursement systems often have the added issue of reduced productivity and consequent lower income in following years, in addition to limited or no support for requested length of parental leave[2, 9]. Limited opportunities for lactation create discrimination or inconvenience with one-third of breastfeeding physicians reporting discrimination due to pumping, and one-quarter reporting inappropriate comments regarding breastfeeding [67]. Physicians have lower rates of exclusive breastfeeding than recommended by the American Academy of Pediatrics, and many cannot meet their own breastfeeding goals[69].
Although professional women have historically carried a disproportionate share of domestic responsibilities compared to male peers, generational priorities around parenting may now outweigh those related to gender [63]. Today, medical students of both genders equally consider flexibility and work-life balance weighing into their choice of specialty [70]. Regardless of gender, gynecologic specialists who parent wish they had taken more parental time off and had additional support for parenting [65].
RECOMMENDATION 7:
Empowering wellness strategies across the discipline and attention to work-life integration, including respect for individual choices regarding pregnancy and parenting, will ultimately improve long-term productivity and retention for GOs of any gender.
Wage Gap
Persistently lower wages for women physicians are documented even when adjusted for other factors such as experience, age, specialty, faculty rank, NIH funding, and publications.[71]. The 2020 SGO SOSS results show a large persistent gender gap in earnings among GOs with men’s reported earnings 35% higher than those reported by women. Women were more likely to report receiving a straight salary (31 vs 20%), and men were more likely to report receiving productivity-based compensation, such as bonuses and incentives (79 vs 66%) [1]. These data were confirmed by an independent, self-selected, anonymous self-reported SGO survey [5].
The 2020 SSOS men self-reported generating 35% more total wRVUs compared to women. Yet, women are at a systematic disadvantage in relative value unit (RVU)-based productivity metrics due to the extra time they spend with patients, family, and staff due to expectations from colleagues, staff, and patients [72]. Additionally, the SOSS demonstrated differences in practice environments between male and female GOs (Table 3). Differences in clinical activities such as chemotherapy prescribing, for which only 11% of GOs were compensated in 2019, contribute to the observed wage gap. Differences influence practice efficiency in practice support [1]. Surgeons who are women are working harder for every earned wRVU [73].
The wRVU system is additionally biased according to sex of the patients receiving care. The Centers for Medicare & Medicaid Services set rates, and insurers subsequently reimburse procedures performed on female patients at a lower rate than similar procedures for male patients. Male-specific surgeries are reimbursed at an average rate of 28% higher than the comparable female-specific procedures [74]. These shortcomings of the current reimbursement system result in what is referred to as “double discrimination”, lower pay in a surgical specialty with the largest percentage of women surgeons, that serves primarily female patients[75].
Occupational segregation, defined as the distribution of workers across and within professions based upon demographic characteristics, drives much of the gender wage gap in the US[72, 76]. Gender clustering of women into specialties influences perceptions of the field, such that specialties with high proportions of female physicians or those that involve the care of women or children are perceived as lower in status and relatively lower salaries follow [35]. OBGYN is, in 2021, the lowest paid of the procedural specialties[77]. A relative decline in salary for OBGYNs compared to the average physician salary over the past four decades, can be compared directly to urology, which remains predominated by male physicians. Urologists have maintained their salaries over time whereas compensation for gynecologists has declined relative to average physician salaries [72]. These trends highlight the importance of gender equity for all GOs to maintain the professional stature of the specialty and ensure our negotiating power within healthcare organizations.
RECOMMENDATION 8:
Equitable support and transparency in metrics will provide equity in compensation on an individual level; address structural inequities to correct inequities in compensation for the specialty.
Conclusions and Call to Action
All gynecologic oncology healthcare team members should be supported within a work environment that allows them to thrive and provide the highest quality patient care. Environments conducive to workplace success include those free from discrimination, where equal resources, opportunities, and work-life integration are available to all[78]. The literature displays gaps in gender equity throughout multiple domains relevant to gynecologic oncology that must be addressed intentionally; the passive inclusion of women has been insufficient to create professional equity in this specialty dedicated to the care of women. Evidence-based interventions that have demonstrated efficacy in achieving the goal of gender equity include the Executive Leadership in Academic Medicine for Women Program (ELAM), a one-year program that includes coaching, networking and mentoring; and the Gender Bias Habit-Breaking Intervention, a 2.5 hour bias literacy workshop [2]. Incorporation of these or similar curricula into gynecologic oncology divisions and SGO programing is certainly advisable and possible.
The systemic nature of gender-based bias requires acknowledgement and action on the level of our healthcare organizations. Existing laws against discrimination and harassment, such as Title VII and Title IX, must be enforced [11]. Overt and subtle manifestations of inequity must be identified, reported and investigated utilizing unbiased systems. Involved parties need to be brought together to remedy historic inaction and embark upon constructive culture change[79]. Organizations can actively counteract bias through the incorporation of evidence-based anti-sexist hiring processes and trainings [79, 80]. Organizations can create transparent compensation models for physicians, which have been demonstrated to eliminate gender pay disparity[81]. Leadership term limits can inspire metric-based succession planning and diversity; diversity dashboards and leadership “report cards” can improve retention for women and URM [82].
While we await these needed organizational efforts, individual level efforts can begin to move the needle towards creating gender-equitable workplace cultures. When witnessing discrimination or bias, a bystander can speak up and speak out and become an upstander [16]. Mentorship and sponsorship are critical to the professional development and career advancement of people of all genders irrespective of race/ethnicity or sexual orientation. Every member of the healthcare team, regardless of rank, can participate in and foster these relationships. Bidirectional mentorship can provide junior faculty with needed career development support while the senior faculty learns new teaching or communication skills [58]. Given the high percentage of women currently practicing and providing care to women with gynecologic malignancies, passively awaiting equity is no longer an option. We should encourage and support “critical actors” who catalyze change in existing cultures within all health care settings where patients with gynecologic cancers receive care [83].
Gender Equity Manuscript Highlights.
All gynecologic oncology team members should have equal opportunities to advance in their careers.
Institutions should have systems to report sexual misconduct and apply zero-tolerance policies.
Gender-neutral mechanisms for mentorship, advancement and inclusion should be developed.
Work-life integration policies, including respect for parenting choices, will improve productivity and retention.
Footnotes
The 2020 State of the Society Survey (SOSS) was developed by the SOSS Task Force as a web-based voluntary survey administered from August 15 – September 30, 2019. Response rate was 48% (n=690). Data are self-reported and not verified, and should be interpreted as such. Some data in the survey are more robust, such as gender, answers to yes/no questions, and verified wellness indexes: some data are less so, such as estimated number of cervical cancer cases done per year, salary, wRVUs or smaller subdivisions of the larger group. The survey is not a peer-reviewed or open access publication. While some univariate analyses were able to be performed, multivariate analyses were not.
Declaration of Competing Interest
All authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.The Society of Gynecologic Oncology 2020 State of the Society Survey. 2020. [Google Scholar]
- 2.Heisler CA, et al. , Has a critical mass of women resulted in gender equity in gynecologic surgery? American Journal of Obstetrics and Gynecology, 2020. [DOI] [PubMed] [Google Scholar]
- 3.Stasenko M, et al. , Survey of sexual harassment and gender disparities among gynecologic oncologists. 2019, American Society of Clinical Oncology. [Google Scholar]
- 4.Temkin SM, et al. , Take me to your leader: Reporting structures and equity in academic gynecologic oncology. Gynecologic Oncology, 2020. [DOI] [PubMed] [Google Scholar]
- 5.Croft KM, et al. Compensation differences by gender in gynecologic oncology. in SGO 2020 Annual Meeting on Women’s Cancer. 2020. SGO. [Google Scholar]
- 6.Lautenberger D and Dandar V, The State of Women in Academic Medicine 2018–2019: Exploring Pathways to Equity. 2020. [Google Scholar]
- 7.AAMC. Table 13: U.S. Medical School Faculty by Sex, Rank, and Department, 2019. 2019 09/17/2020]; Available from: https://www.aamc.org/data-reports/faculty-institutions/interactive-data/2019-us-medical-school-faculty. [Google Scholar]
- 8.National Academies of Sciences, E. and Medicine, Sexual harassment of women: climate, culture, and consequences in academic sciences, engineering, and medicine. 2018: National Academies Press. [PubMed] [Google Scholar]
- 9.Stephens EH, et al. , The Current Status of Women in Surgery: How to Affect the Future. JAMA Surgery, 2020. 155(9): p. 876–885. [DOI] [PubMed] [Google Scholar]
- 10.von Gruenigen VE and Karlan BY, Sexual harassment in the work place: Its impact on gynecologic oncology and women’s health. Gynecol Oncol, 2018. 149(2): p. 227–229. [DOI] [PubMed] [Google Scholar]
- 11.Jagsi R, Sexual Harassment in Medicine — #MeToo. New England Journal of Medicine, 2017. 378(3): p. 209–211. [DOI] [PubMed] [Google Scholar]
- 12.Salles A, et al. , Estimating Implicit and Explicit Gender Bias Among Health Care Professionals and Surgeons. JAMA Netw Open, 2019. 2(7): p. e196545. [DOI] [PubMed] [Google Scholar]
- 13.Periyakoil VS, et al. , Common Types of Gender-Based Microaggressions in Medicine. Academic Medicine, 2019. [DOI] [PubMed] [Google Scholar]
- 14.Miner KN and Cortina LM, Observed Workplace Incivility toward Women, Perceptions of Interpersonal Injustice, and Observer Occupational Well-Being: Differential Effects for Gender of the Observer. Frontiers in Psychology, 2016. 7(482). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nunez-Smith M, et al. , Health care workplace discrimination and physician turnover. Journal of the National Medical Association, 2009. 101(12): p. 1274–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mello MM and Jagsi R, Standing Up against Gender Bias and Harassment-A Matter of Professional Ethics. The New England journal of medicine, 2020. 382(15): p. 1385. [DOI] [PubMed] [Google Scholar]
- 17.Silver JK, Should her name begin with “Doctor”? BMJ, 2020. 371: p. m4754. [DOI] [PubMed] [Google Scholar]
- 18.Gomez LE and Bernet P, Diversity improves performance and outcomes. Journal of the National Medical Association, 2019. 111(4): p. 383–392. [DOI] [PubMed] [Google Scholar]
- 19.Cordova RD, Beaudin CL, and Iwanabe KE, Addressing diversity and moving toward equity in hospital care. Frontiers of health services management, 2010. 26(3): p. 19–34. [PubMed] [Google Scholar]
- 20.Brown A, Bonneville G, and Glaze S, Nevertheless, They Persisted: How Women Experience Gender-Based Discrimination During Postgraduate Surgical Training. Journal of Surgical Education, 2021. 78(1): p. 17–34. [DOI] [PubMed] [Google Scholar]
- 21.Hansen M, et al. , Implicit gender bias among US resident physicians. BMC Medical Education, 2019. 19(1): p. 396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu Y-Y, et al. , Discrimination, abuse, harassment, and burnout in surgical residency training. New England Journal of Medicine, 2019. 381(18): p. 1741–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pendleton AA, et al. , A multi-institutional study of patient-derived gender-based discrimination experienced by resident physicians. The American Journal of Surgery, 2020. [DOI] [PubMed] [Google Scholar]
- 24.Barnes KL, et al. , Gender Bias Experiences of Female Surgical Trainees. Journal of Surgical Education, 2019. [DOI] [PubMed] [Google Scholar]
- 25.Chang JC, Odrobina MR, and McIntyre-Seltman K, The effect of student gender on the obstetrics and gynecology clerkship experience. Journal of Women’s Health, 2010. 19(1): p. 8792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoops H, et al. , Resident autonomy in the operating room: Does gender matter? The American Journal of Surgery, 2019. 217(2): p. 301–305. [DOI] [PubMed] [Google Scholar]
- 27.Meyerson SL, et al. , The effect of gender on operative autonomy in general surgery residents. Surgery, 2019. 166(5): p. 738–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gerull KM, et al. , Assessing gender bias in qualitative evaluations of surgical residents. The American Journal of Surgery, 2019. 217(2): p. 306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mueller AS, et al. , Gender Differences in Attending Physicians’ Feedback to Residents: A Qualitative Analysis. Journal of graduate medical education, 2017. 9(5): p. 577–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choo EK, Damned if you do, damned if you don’t: bias in evaluations of female resident physicians. Journal of graduate medical education, 2017. 9(5): p. 586–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Correll S and Simard C, Vague feedback is holding women back. Harvard Business Review, 2016. 94: p. 2–5. [Google Scholar]
- 32.Morgan HK, et al. , Student evaluation of faculty physicians: gender differences in teaching evaluations. Journal of Women’s Health, 2016. 25(5): p. 453–456. [DOI] [PubMed] [Google Scholar]
- 33.Arah OA, Heineman MJ, and Lombarts KM, Factors influencing residents’ evaluations of clinical faculty member teaching qualities and role model status. Medical education, 2012. 46(4): p. 381–389. [DOI] [PubMed] [Google Scholar]
- 34.Burnell N, Cojuharenco I, and Murad Z, Now you see it now you don’t: The effect of teaching style and seniority on gender bias in teaching evaluations. 2018. [Google Scholar]
- 35.Carnes M, et al. , Why is John More Likely to Become Department Chair Than Jennifer? Transactions of the American Clinical and Climatological Association, 2015. 126: p. 197–214. [PMC free article] [PubMed] [Google Scholar]
- 36.Greenberg CC, Association for Academic Surgery presidential address: sticky floors and glass ceilings. Journal of Surgical Research, 2017. 219: p. ix–xviii. [DOI] [PubMed] [Google Scholar]
- 37.Foote MB, et al. , Use of “doctor” badges for physician role identification during clinical training. JAMA internal medicine, 2019. 179(11): p. 1582–1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hutchison K, Four types of gender bias affecting women surgeons and their cumulative impact. Journal of Medical Ethics, 2020. 46(4): p. 236–241. [DOI] [PubMed] [Google Scholar]
- 39.Linzer M and Harwood E, Gendered Expectations: Do They Contribute to High Burnout Among Female Physicians? Journal of General Internal Medicine, 2018. 33(6): p. 963–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sarsons H, Interpreting Signals in the Labour Market: Evidence from Medical Referrals. 2017, Harvard University. [Google Scholar]
- 41.Jones LK, et al. , Ethological observations of social behavior in the operating room. Proceedings of the National Academy of Sciences, 2018. 115(29): p. 7575–7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dossett LA, et al. , Women Surgeons’ Experiences of Interprofessional Workplace Conflict. JAMA Network Open, 2020. 3(10): p. e2019843-e2019843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schachter AE, et al. , Women Support Women, Right? Gender Disparities in Decision-to-Incision Time in Emergency Surgery. Journal of the American College of Surgeons, 2020. 231(4): p. S113S114. [Google Scholar]
- 44.Hofler LG, et al. , Comparison of women in department leadership in obstetrics and gynecology with other specialties. Obstetrics and gynecology, 2016. 127(3): p. 442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hofler L, et al. , subspecialty and gender of obstetrics and gynecology faculty in departmentbased leadership roles. Obstetrics and gynecology, 2015. 125(2): p. 471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hill EK, et al. , Gender differences in scholarly productivity within academic gynecologic oncology departments. Obstetrics and gynecology, 2015. 126(6): p. 1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salinaro JR, et al. , Gender trends in gynecologic oncology authorship: Implications for the critical evaluation of gender distribution in academic rank and leadership positions. Gynecologic Oncology, 2018. 151(3): p. 542–546. [DOI] [PubMed] [Google Scholar]
- 48.Lewiss RE, et al. , Is Academic Medicine Making Mid-Career Women Physicians Invisible? Journal of Women’s Health, 2019. [DOI] [PubMed] [Google Scholar]
- 49.Jagsi R, et al. , The “Gender Gap” in Authorship of Academic Medical Literature — A 35-Year Perspective. New England Journal of Medicine, 2006. 355(3): p. 281–287. [DOI] [PubMed] [Google Scholar]
- 50.Nguyen V, et al. , Academic Surgical Oncologists’ Productivity Correlates with Gender, Grant Funding, and Institutional NCI Comprehensive Cancer Center Affiliation. Ann Surg Oncol, 2018. 25(7): p. 1852–1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murrar S, et al. , Research Conducted in Women Was Deemed More Impactful but Less Publishable than the Same Research Conducted in Men. Journal of Women’s Health, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oliveira DFM, et al. , Comparison of National Institutes of Health Grant Amounts to First-Time Male and Female Principal Investigators. JAMA, 2019. 321(9): p. 898–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lerchenmueller MJ and Sorenson O, The gender gap in early career transitions in the life sciences. Research Policy, 2018. 47(6): p. 1007–1017. [Google Scholar]
- 54.Mirin AA, Gender Disparity in the Funding of Diseases by the US National Institutes of Health. Journal of Women’s Health, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rice LW, et al. , Increasing NIH funding for academic departments of obstetrics and gynecology: a call to action. Am J Obstet Gynecol, 2020. 223(1): p. 79.e1–79.e8. [DOI] [PubMed] [Google Scholar]
- 56.Spencer RJ, et al. , Disparities in the allocation of research funding to gynecologic cancers by Funding to Lethality scores. Gynecologic Oncology, 2019. 152(1): p. 106–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Laver KE, et al. , A systematic review of interventions to support the careers of women in academic medicine and other disciplines. BMJ open, 2018. 8(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Burgess A, van Diggele C, and Mellis C, Mentorship in the health professions: a review. The clinical teacher, 2018. 15(3): p. 197–202. [DOI] [PubMed] [Google Scholar]
- 59.Sambunjak D, Straus SE, and Marušić A, Mentoring in academic medicine: a systematic review. Jama, 2006. 296(9): p. 1103–1115. [DOI] [PubMed] [Google Scholar]
- 60.Rath KS, et al. , Burnout and associated factors among members of the Society of Gynecologic Oncology. American journal of obstetrics and gynecology, 2015. 213(6): p. 824. e1–824. e9. [DOI] [PubMed] [Google Scholar]
- 61.Cass I, et al. , Stress and burnout among gynecologic oncologists: A Society of Gynecologic Oncology Evidence-based Review and Recommendations. Obstetrical & Gynecological Survey, 2016. 71(12): p. 715–717. [DOI] [PubMed] [Google Scholar]
- 62.Johnson HM, et al. , Associations Between Career Satisfaction, Personal Life Factors, and Work-Life Integration Practices Among US Surgeons by Gender. JAMA Surgery, 2020. 155(8): p. 742–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jolly S, et al. , Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Annals of internal medicine, 2014. 160(5): p. 344–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fassiotto M, et al. , An Integrated Career Coaching and Time-Banking System Promoting Flexibility, Wellness, and Success: A Pilot Program at Stanford University School of Medicine. Academic medicine: journal of the Association of American Medical Colleges, 2018. 93(6): p. 881–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hill EK, et al. , Gender and the balance of parenting and professional life among gynecology subspecialists. Journal of minimally invasive gynecology, 2019. 26(6): p. 1088–1094. [DOI] [PubMed] [Google Scholar]
- 66.Hariton E, et al. , Pregnancy and parental leave among obstetrics and gynecology residents: results of a nationwide survey of program directors. American Journal of Obstetrics and Gynecology, 2018. 219(2): p. 199.e1–199.e8. [DOI] [PubMed] [Google Scholar]
- 67.Juengst SB, et al. , Family Leave and Return-to-Work Experiences of Physician Mothers. JAMA network open, 2019. 2(10): p. e1913054-e1913054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lumpkin ST, et al. , Fellowship or family? A comparison of residency leave policies with the family and medical leave act. Journal of Surgical Research, 2019. 241: p. 302–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Melnitchouk N, Scully RE, and Davids JS, Barriers to breastfeeding for US physicians who are mothers. JAMA internal medicine, 2018. 178(8): p. 1130–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Smith V, Bethune C, and Hurley KF, Examining Medical Student Specialty Choice Through a Gender Lens: An Orientational Qualitative Study. Teaching and Learning in Medicine, 2018. 30(1): p. 33–44. [DOI] [PubMed] [Google Scholar]
- 71.Jena AB, Olenski AR, and Blumenthal DM, Sex Differences in Physician Salary in US Public Medical Schools. JAMA Intern Med, 2016. 176(9): p. 1294–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pelley E and Carnes M, When a specialty becomes “women’s work”: Trends in and implications of specialty gender segregation in medicine. Academic Medicine, 2020. 95(10): p. 1499–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Butkus R, et al. , Achieving gender equity in physician compensation and career advancement: a position paper of the American College of Physicians. Annals of internal medicine, 2018. 168(10): p. 721–723. [DOI] [PubMed] [Google Scholar]
- 74.Benoit MF, Ma JF, and Upperman BA, Comparison of 2015 Medicare relative value units for gender-specific procedures: Gynecologic and gynecologic-oncologic versus urologic CPT coding. Has time healed gender-worth? Gynecologic Oncology, 2017. 144(2): p. 336–342. [DOI] [PubMed] [Google Scholar]
- 75.Watson KL and King LP, Double Discrimination, the Pay Gap in Gynecologic Surgery, and Its Association With Quality of Care. Obstetrics & Gynecology, 2021. 137(4): p. 657–661. [DOI] [PubMed] [Google Scholar]
- 76.Hegewisch A and Hartmann H, Occupational segregation and the gender wage gap: A job half done. 2014. [Google Scholar]
- 77.Kane L Medscape Physician Compensation Report 2021: The Recovery Begins. 2021. [cited 2021 May 16]; Available from: https://www.medscape.com/slideshow/2021-compensation-overview-6013761#3.
- 78.Westring AF, et al. , A culture conducive to women’s academic success: Development of a measure. Academic medicine: journal of the Association of American Medical Colleges, 2012. 87(11): p. 1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Morgan AU, et al. , Eliminating Gender-Based Bias in Academic Medicine: More Than Naming the “Elephant in the Room”. Journal of General Internal Medicine, 2018. 33(6): p. 966–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bates C, et al. , Striving for Gender Equity in Academic Medicine Careers: A Call to Action. Academic medicine : journal of the Association of American Medical Colleges, 2016. 91(8): p. 1050–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hayes SN, Noseworthy JH, and Farrugia G. A structured compensation plan results in equitable physician compensation: a single-center analysis. in Mayo Clinic Proceedings. 2020. Elsevier. [DOI] [PubMed] [Google Scholar]
- 82.Beeler WH, Mangurian C, and Jagsi R, Unplugging the Pipeline — A Call for Term Limits in Academic Medicine. New England Journal of Medicine, 2019. 381(16): p. 1508–1511. [DOI] [PubMed] [Google Scholar]
- 83.Helitzer DL, et al. , Changing the culture of academic medicine: critical mass or critical actors? Journal of women’s health, 2017. 26(5): p. 540–548. [DOI] [PMC free article] [PubMed] [Google Scholar]