ABSTRACT
Polyether-ether-ketone (PEEK) is believed to be the next-generation biomedical material for orthopaedic implants that may replace metal materials because of its good biocompatibility, appropriate mechanical properties and radiolucency. Currently, some PEEK implants have been used successfully for many years. However, there is no customised PEEK orthopaedic implant made by additive manufacturing licensed for the market, although clinical trials have been increasingly reported. In this review article, design criteria, including geometric matching, functional restoration, strength safety, early fixation, long-term stability and manufacturing capability, are summarised, focusing on the clinical requirements. An integrated framework of design and manufacturing processes to create customised PEEK implants is presented, and several typical clinical applications such as cranioplasty patches, rib prostheses, mandibular prostheses, scapula prostheses and femoral prostheses are described. The main technical challenge faced by PEEK orthopaedic implants lies in the poor bonding with bone and soft tissue due to its biological inertness, which may be solved by adding bioactive fillers and manufacturing porous architecture. The lack of technical standards is also one of the major factors preventing additive-manufactured customised PEEK orthopaedic implants from clinical translation, and it is good to see that the abundance of standards in the field of additive-manufactured medical devices is helping them enter the clinical market.
Keywords: 3D printing, additive manufacturing, customised implant, polyether-ether-ketone
Introduction
Polyether-ether-ketone (PEEK) is a semi-crystalline thermoplastic polymer in the poly-aryl-ether-ketone family, which was first developed in 1978. The main chain of macromolecular is mainly composed of benzene rings, ketone group and ether group, with a larger number of benzene rings providing heat resistance and stability, and the ketone groups and ether group providing balance between rigidity and flexibility.1 Therefore, PEEK is characterised by high chemical resistance, good biocompatibility, bioinertness, high-temperature resistance and favourable mechanical properties.2 PEEK has the following advantages compared with biomedical metal materials such as 316L stainless steel, titanium alloy and tantalum. First, its mechanical properties, including density of 1.28-1.32 g/cm,3 flexural modulus of 3 GPa, and flexural strength of 110 MPa, are similar to those of human bone,3 thus avoiding the stress shielding caused by a mismatch in stiffness between implant and bone. Second, PEEK is radiolucent and nonmagnetic, thus it does not interfere with imaging examinations such as computed tomography (CT) and magnetic resonance imaging. Third, the abnormal feeling caused by the high thermal conductivity of metal material4 can be avoided by PEEK since its thermal conductivity of 0.29 W/m/K5 is closer to that of human cortical bone of 0.68 W/m/K6 than Ti6Al4V. Because of these advantages, PEEK is believed to be one of the next-generation biomaterials that may replace titanium alloy in the manufacture of orthopaedic implants.
To date, many PEEK orthopaedic implants have entered the market worldwide, among which the intervertebral fusion cage has been used successfully for many years.7-9 Major medical device manufacturers worldwide have related products on the market, such as SYNFIXTM Evolution Implant from Depuy Synthes, LYDESDALE PTCTM from Medtronic and AVSTM TL from Stryker. In recent years, some PEEK implants developed for use in artificial joints10, 11 and trauma treatments12 have also entered the market. In addition, PEEK has a long history of use in stomatology, with other applications including fixed partial dentures, abutments, dental implants and removable dentures.13-15
In summary, the excellent biocompatibility of PEEK and its advantages compared to metal materials give it immeasurable development prospects for application in the field of orthopaedic implants. Combined with additive manufacturing (AM) technology, which is also known as three-dimensional (3D) printing, customised PEEK implants can be rapidly obtained,16, 17 which helps solve rare and complex clinical cases as well as providing the implant with better adaptability. Further, the development of AM allows creation of a PEEK implant with gradient material components and gradient porous structure, thus fabricating an implant with better performance than traditional manufacturing processes. Although there are a few articles that reviewed the AM technology and medical application of PEEK, reviews that include the full process of AM PEEK customised orthopaedic implant from clinical requirements to the final application are rare. This article summarised the common clinical requirements, corresponding design criteria and manufacturing processes for AM PEEK customised implant, and illustrates the relationships among clinical requirements, design and manufacturing through several clinical applications which were all designed and manufactured by the author’s team. Furthermore, the future perspective for PEEK implants and the clinical industrialisation of AM PEEK implants are discussed.
Clinical Requirements
The development of AM of PEEK has given rise to the customised PEEK orthopaedic implant. Several clinical requirements need to be fulfilled or partially met by a customised orthopaedic implant.
Anatomical geometrical matching is one of the basic requirements for a customised implant, which is an obvious advantage of the customised implant compared to regular medical devices, and was also the initial trigger for the application of AM in the field of orthopaedic implants.18, 19 Medical images, represented by CT, are usually employed as the original data in the design of a customised implant, thus geometrical matching is available from the beginning of the design process.20
The key purpose of an implant is to replace the mechanical function of the defective bone. For example, the critical mechanical function of the skull is to protect the brain, thus damage to the cranial plates by accidental impact loading must be considered. Maxillofacial bone plays a role in maintaining the facial profile and composes the temporomandibular joint, so the anatomical shape and ability to bear the masticatory forces become implant.21, 22 Meanwhile, for joint replacement, restoring the arthrokinematics is the primary goal of the implant. Thus the design, AM and application of a customised implant should be developed around the core objective of mechanical function.
Because an orthopaedic implant serves the function of movement and supports the body for a long period, good mechanical performance, especially endurance properties, is vital. Fracture in vivo is a typical and severe pattern of mechanical failure of orthopaedic implants.23, 24 In artificial joint replacement, 1-3% of revision surgeries were led by the fracture of implants.25 The safety issues of an orthopaedic implant have to be prevented by all means due to the unpredictability of fracture and consequent collateral damage. Unfortunately, it is practically impossible to carry out destructive mechanical testing before clinical application due to the uniqueness of a customised implant. Therefore, it is necessary to ensure long-term safety from the perspectives of design, AM and clinical use of the customised implant to prevent the serious complication of mechanical failure.
Immediate fixation to surrounding bone are usually completed during surgery to ensure that there would be no dislocation or loosening. Bone cement,26 screws27 and strapping are commonly-used initial fixation approaches in orthopaedic surgery. Stable initial fixation would guarantee the mechanical relationship between implant and natural bone, allowing the implant to serve the function of bearing and transmitting the physiological load.
Stable long-term biological fixation between implant and bone through osseointegration is expected.28 Issues such as the osteoinductive activity of implant material,29 porous structure30, 31 for the formation of a biological bone-implant interface through bone ingrowth,32, 33 as well as the bony support to the implant which depends on remodelling of the surrounding bone, are the main concerns regarding the long-term stability of AM customised orthopaedic implants.
The above clinical requirements from different perspectives bring challenges to the material, design, and manufacturing processes of 3D-printed PEEK implants. In terms of material, due to the chemical inertness of PEEK, integrate with bone and soft tissues is challenging, which is unfavourable for the long-term biological interface with an implant. In the context of design, challenges arising from the clinical requirements from different aspects and their trade-off are increasingly recognised. Typically, for example, a porous structure is usually introduced to an orthopaedic implant to promote osseointegration and long-term biological fixation, although it undoubtedly weakens the mechanical properties of the implant.30 As for manufacturing, the high melting temperature, semi-crystalline structure34 and significant cooling shrinkage rate of PEEK materials35, 36 increases the complexity of the AM process and results in uncontrollable properties of 3D-printed parts, which poses challenges for the manufacture of large-size orthopaedic implants with high accuracy and good mechanical properties.
Design and Manufacturing of Polyether-ether-ketone Customised Implants
Design of customised implants
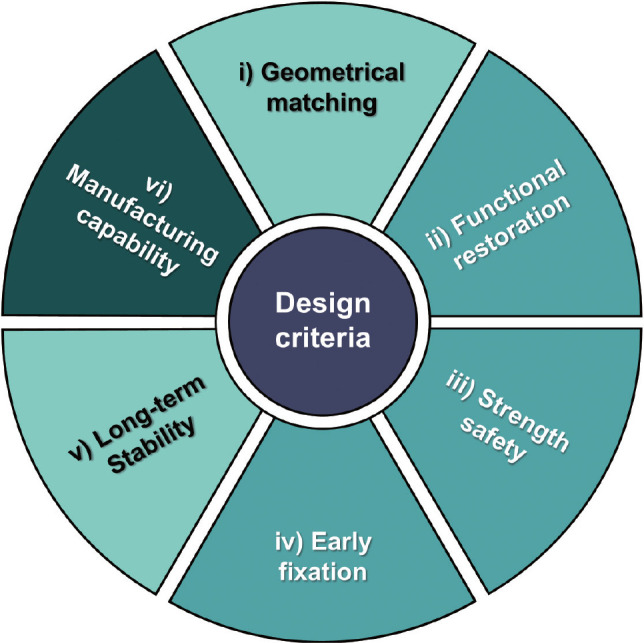
Design criteria
Design acts as a bridge for connecting the front-end clinics with the back-end AM, thus the clinical requirements and constraints of AM must be considered when designing a customised implant. The following design criteria should be met based on the different clinical requirements and manufacturing capabilities of 3D printing technology (Figure 1).
Geometrical matching. Anatomical shape matching is a primary criterion for any implant related to restoring a patient’s appearance, such as implants for maxillofacial repair, cranioplasty plates and mandibular reconstruction, for which aesthetic restoration is a significant evaluation index of clinical efficacy. However, it could be undesirable to replicate all the geometric features of the replaced bone or the contralateral bone in the design since it may lead to over-complicated and unnecessary geometry, which may induce unexpected stress concentrations and low manufacturing quality. In the design of a rib prosthesis described by Kang et al.,37 the central line of the ribs was lofted, creating simplified rib prostheses instead of reconstructing an exact 3D model from CT images, and it proved to be an effective and practical method.
Functional restoration. The core element in implant design is to restore the mechanical function of defective bone, however, different implants have different considerations. For instance, arthrokinematics must be reconstructed for an implant containing articular surfaces; thoracic expansion and contraction during breathing must be considered in a sternum prosthesis design; bearing and transferring loads are the primary function of a long bone. It can be seen that functional restoration is a complicated aspect of design criteria and is closely related to the scenarios of clinical application. Therefore, the designer should cooperate closely with the surgeon in the design process to understand the major function of the customised implant.
Strength safety. This is a criterion that should consistently be recognised in implant design. Many types of implants bear alternating loads in vivo, such as artificial joints or intervertebral fusion cages, thus endurance properties of the implant must be checked or measured. For example, strict standards have been established for the wear and fatigue testing of artificial hip and knee joints to evaluate their long-term safety.38 Some implants play the role of temporary load-bearing. Typically, fracture fixation plates are not expected to be loaded after fracture healing, so their safety under static loads becomes the focus.39 Some implants, such as skull and ribs, are not expected to carry much load but must protect the organs within from accidental impacts. Thus their strength could be comparable to the natural bone.37 In the finite element analysis (FEA) of an implant, the safety factor, defined as the ratio of the allowable stress of the material to the maximum stress of the implant,30 is employed to evaluate the strength safety quantitatively.
Early fixation. Specific structures for immediate fixation based on the fixation strategy in the clinic is indispensable in the design. Counterbore holes for screws, slots for wire banding and intramedullary nails are all specific structures for immediate fixation. Micro-motion at the interface between bone and implant is used as a quantitative indicator for early fixation. The promotional effect of micro-motion on fracture healing was first found by Cameron et al.,40 and Maniatopoulos et al.41 proposed a threshold of micro-motion, that is, micro-motion within an appropriate range promoted healing between implant and bone, while higher micro-motion resulted in poor early fixation thus disrupting the healing interface. Li et al.42 reviewed a previous study on the threshold of micro-motion, and summarised that micro-motion in the range of 50-100 μm would contribute to the interface healing and bone ingrowth of a porous implant.
Long-term stability. Accounting for the risk of failure of immediate fixation, the long-term stability derived from osseointegration43, 44 of bone and implant as well as the bony support from surrounding tissue is the deeper pursuit. In research into porous implants of titanium or its alloy, consensuses have formed on the optimal pore size and architecture.45, 46 However, these consensuses cannot be directly used in PEEK because of the vast difference in mechanical and chemical properties between PEEK and titanium. As for the bony support, appropriate mechanical stimulation to the surrounding bone is one of the keys to enhancing the growth and further maintaining the stable fixation of the implant. The stress or strain experienced by bone tissue in vivo is difficult to measure. However, it can be predicted by computational simulation based on Wolff’s law, and the material and structure of the implant can be optimised to obtain better long-term stability.
Manufacturing capability. Although AM technology possess high flexibility, the constraints of manufacturing capability should be taken into account as a prerequisite in the design process, which is embodied in several aspects. The first is whether an implant with large size or complex geometry can be printed accurately. Warpage is one of the difficulties faced in the 3D printing of PEEK caused by its significant shrinkage upon cooling, which cannot be eliminated as it would harm the manufacturing accuracy and lead to poor quality in the 3D printing of PEEK. Secondly, porous structures have been proven to be beneficial to osseointegration. The major AM techniques used for thermoplastic materials, selective laser sintering (SLS)47 and fused filament fabrication (FFF),43, 44 each have capabilities which are different due to the different principles. Usually, SLS can be used to create porous structures with complex architecture,48 such as diamond, rhombic dodecahedron, or body-centred cubic shapes, which are difficult for FFF. The third consideration is whether the time spent in AM can meet the surgery requirement. For some customised implants used for patients with bone tumours or severe trauma, the implantation surgery needs to be implemented as soon as possible, thus the timeliness should be checked before surgical planning of the customised implant.
Figure 1. Design criteria for three-dimensional printed customised implant.
Some requirements are necessary for the above design criteria, including mechanical safety, functional restoration, and early stability, while others can be compromised to achieve the necessary criteria. The manufacturing capability should be fully considered before and during the design processes.
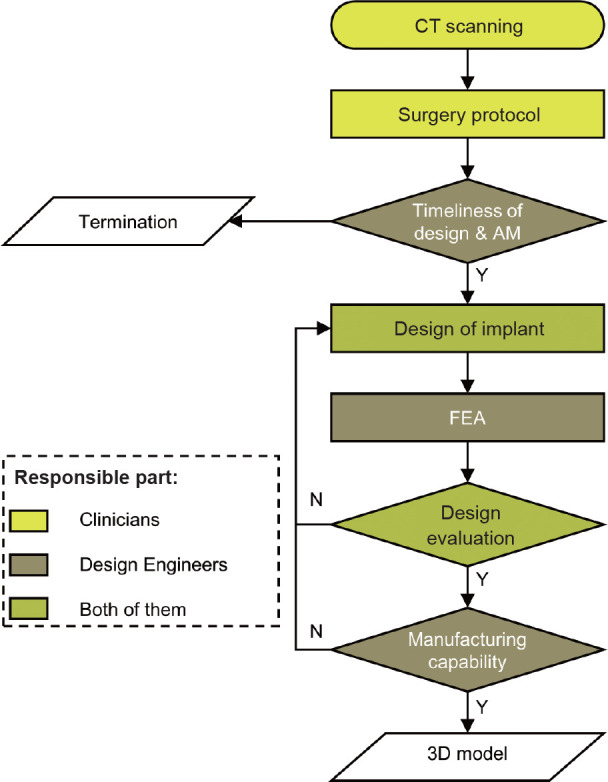
Design processes
A flowchart of the design process and the relationship between each step and the criteria of the customised implant is presented in Figure 2, in which the different colours of the flow blocks represent the suggestion of whether clinicians or engineers are responsible for that step. The customised design process usually began with CT images, and the surgical protocol would be decided based on these. The timeliness of designing and AM must be preliminarily checked to confirm that the implant can be provided before the surgery. Otherwise, treatment with a 3D-printed customised implant should be ruled out. The implant would be designed based on the CT images and surgical protocol, and geometrical matching and functional restoration would be considered in this step. FEA would be involved to evaluate the mechanical safety, early stability and long-term stability of the implant by numerical prediction of maximum stress, interface micro-motion and strain of periprosthetic bone. The manufacturing feasibility of the final designed implant would be rechecked before delivery to the manufacturer. In the above steps, CT scanning and surgical protocol are mainly performed by clinicians, while design engineers should conduct timeliness evaluation, FEA and assessment of manufacturing capability. Both clinicians and engineers would be responsible for the other steps, the design of the implant and design evaluation.
Figure 2. Flowchart of the design process. 3D: three-dimensional; CT: computed tomography; FEA: finite element analysis; N: no; Y: yes.
Additive manufacturing of polyether-ether-ketone implant
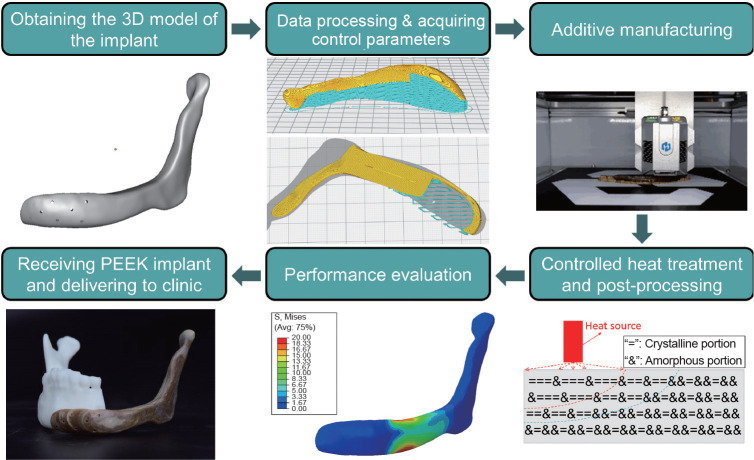
As presented in Figure 3, the manufacturing process of a PEEK implant includes the following key steps: i) obtaining a 3D model of the implant; ii) data processing and acquiring control parameters; iii) AM; iv) controlled heat treatment and post-processing; v) performance evaluation; and vi) receipt of the PEEK implant and delivery to the clinic.
Figure 3. The manufacturing process of a PEEK implant. 3D: three-dimensional; PEEK: polyether-ether-ketone.
Obtaining the three-dimensional model of an implant
The 3D model of the PEEK implant comes from its precision design process and needs to be carefully checked before manufacturing. The contour or facet data of the 3D model need to be complete, and the model’s accuracy should meet the requirements of the implant. Then the 3D model of the PEEK implant can be loaded into the data processing software.
Data processing and acquisition of control parameters
AM technology is usually a process of creating objects layer-by-layer,49 so the data processing usually includes the process of parameter setting, layer-cutting, and printing path planning in each layer. Finally, a complete control parameter packet is formed. The setting of process parameters is closely related to the performance of PEEK implants, thus issues related to the properties of final parts such as temperature and rheological properties, AM process characteristics, and the final performance requirements of implants, should be comprehensively considered. Anisotropy is one of the typical characteristics of the AM process, which is affected by the polymer chain orientation determined by layer-cutting and printing path planning. Therefore, the actual stress condition of a PEEK implant in the clinical application should be considered during data processing to ensure that the anisotropy will not affect the service life of the implant.
Additive manufacturing (three-dimensional printing)
At present, FFF,50, 51 which is also known as fused deposition modelling, and SLS are the most suitable AM methods for processing PEEK materials. Because of its better ability to control the crystallisation of PEEK and the better fracture elongation of printed samples,52 FFF has been routinely applied to manufacture PEEK implants for use in clinical trials.37, 53 Continuous PEEK filaments with specific diameters have been employed as the raw material for FFF. The filaments are continuously fed into a nozzle, heated to a semiliquid state, and then extruded onto the previous layer along the cross-section contour and filling trajectory. At the same time, the extruded material is solidified and adhered to the surrounding material to build the PEEK implant.
As a semi-crystalline polymer material, the crystal-zone proportion of PEEK is called crystallinity. The mechanical, physical, and chemical properties are vastly different between the crystal and amorphous zones. The crystallisation properties of PEEK materials are greatly affected by the thermal history of the materials.52, 54 Therefore, by controlling the thermal conditions of AM, which mainly includes printing temperature, ambient temperature and heat treatment conditions, the crystallinity of the PEEK formed can be precisely controlled, and the strength, modulus and other properties can be adjusted in large ranges.55-57 Yang et al.52 conducted a comprehensive study on the thermal conditions of AM PEEK, the tensile modulus, tensile strength and elongation at break was varied from 2.8 GPa to 4.2 GPa, from 50 MPa to 84 MPa, and from 20% to 135%, respectively.
Controlled heat treatment and post-processing
Because of the semi-crystalline nature of PEEK material, additive-manufactured PEEK implants can be heat treated to achieve a controlled recrystallisation process.58, 59 The changes of the overall or local recrystallisation and the mechanical properties can be controlled by altering the temperature and the time spent during heat treatment to obtain a bionic PEEK implant with partitioning mechanical properties. Other post-processing methods, such as sanding, polishing, cleaning, and disinfection, are usually performed to obtain the final PEEK implant.
Performance testing and evaluation
A method of evaluating the performance of additive-manufactured PEEK implants ought to be established based on its real clinical application conditions to ensure implant safety, which requires detailed discussion between doctors and AM engineers.
Receiving the PEEK implant and delivery to the clinic
Package, transport, store, and deliver the PEEK implant according to the medical device standards enacted by national supervisory departments.
Clinical Applications
Cranioplasty patch
The skull plays a vital role in protecting the brain and is also important in the aesthetic appearance of the head. Cerebral infections, head trauma, or resection of bone-invading intracranial tumours may cause large cranial bone defects (more than 3 cm in diameter), affecting the head aesthetics, quality of life and psychological well-being of patients.60-63 Therefore, reconstruction of large cranial bone defects with appropriate head aesthetics and physiological function has attracted extensive attention from scholars and clinicians.
Titanium mesh, PEEK, polymethylmethacrylate, acellular bone autografts, and hydroxyapatite implants are being utilised to treat bony defects of the skull.64, 65 Currently, titanium mesh is the primary choice. However, the inherent disadvantages of titanium mesh, such as its high thermal conductivity, deformation in vivo, and artefact generation in medical imaging examinations, cause many difficulties. PEEK has been used in cranioplasty since the early 2000s. It has become popular in neurosurgery due to its mechanical properties, since it is a tough, rigid, biocompatible material, providing good protection.66 Unlike titanium, it is radiolucent and does not produce artefacts in imaging examinations.67
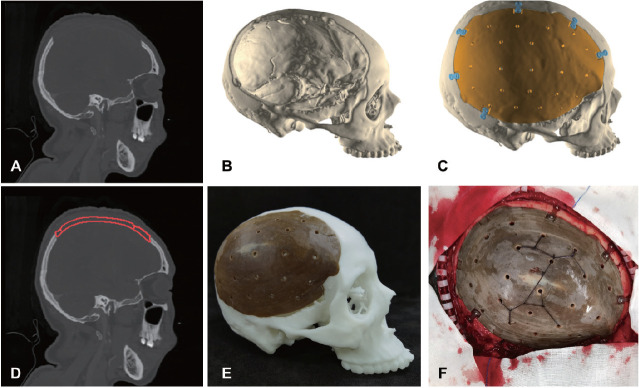
Because of the performance requirements of the skull, the reconstruction of large-area cranial bone defects needs to meet the aesthetics of head anatomical structures and the physiological function of the skull. The design, fabrication and clinical application workflows of a 3D-printed PEEK cranioplasty patch are shown in Figure 4. Based on thin-slice CT images of the head and the actual circumstances of the patient, a 3D model of the skull with the defect is constructed to create a complete design scheme under the clinician’s guidance. A PEEK implant is personalised-designed, and a customised PEEK cranioplasty patch is then fabricated by FFF. The post-treatment processing of the PEEK cranioplasty patch consists of grinding, polishing, and surface heat treatment. Finally, the 3D-printed PEEK cranioplasty patch can be applied in the clinic since it has been matched for size preoperatively, assuming it passes the quality inspection.
Figure 4. 3D-printed PEEK cranioplasty patch. (A) CT image. (B) 3D model of the defected skull. (C) 3D model of cranioplasty patch (yellow). (D) Cranioplasty patch (red) within CT image. (E) 3D-printed PEEK cranioplasty patch. (F) Intraoperative photograph. 3D: three-dimensional; CT: computed tomography; PEEK: polyether-ether-ketone.
Implant for paranasal augmentation
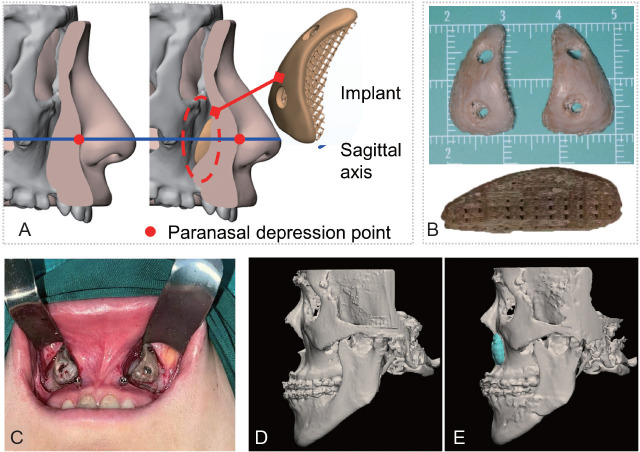
The midface is an essential area of the human facial profile, and a flattened or concave midface caused by paranasal tissue deficiency may lead to an aesthetically displeasing and odd-looking face.68 Midface concavity can be improved by paranasal augmentation with autologous tissue and implants. However, several salient issues have emerged in the clinical practice of paranasal augmentation. Firstly, as the golden standard of augmentation material, autologous bone is limited by supply and requires related skeletal surgery. Secondly, unsatisfactory post-operative results may be encountered due to imperfect implant design.69 Thirdly, bone resorption and implant migration may occur after surgery,70 influencing the long-term survival of the implant. To address the above issues, a new paranasal augmentation method has been developed using a 3D-printed porous PEEK/BaSiO4 implant.
To guide the design of the implant, three criteria-anatomical fit, mechanical matching and long-term stability-have been established, in which anatomical fit focuses on the shape design and the other two govern the mechanical performance of the implant. Implant design consists of four steps: pre-operative CT scan, facial model reconstruction, macro geometrical design and porous structure design (Figure 5). The shape of the implant requires thickness calculation, matching of the implant to the maxilla and prediction of soft-tissue changes. The implant is divided into solid and porous parts, allowing osseointegration with the periprosthetic bone. The pore shape is tetragonal, and the pore size is identified by mechanical analysis to ensure the safety and long-term stability of the implant. By adding bioactive ceramics fillers, for example BaSiO4, into the PEEK matrix, the osseointegration of the PEEK-based implant could be enhanced and thus promises long-term fixation with bone, rather than the mechanical fixation provided by the screws. The PEEK/BaSiO4 are more easily visualised on the X-ray than pure PEEK, facilitating the post-operative assessment of the long-term stability of the implant. Further optimisation of the pore shape will be considered to achieve better bone ingrowth.
Figure 5. Design and application of an implant for paranasal augmentation. (A) Pre-operative design of the implant. (B) A 3D-printed porous PEEK/BaSiO4 implant. (C) Intraoperative view of a paranasal implant fixed with screws. (D, E) Pre-operative (D) and 3-month post-operative (E) comparison through CT models. 3D: three-dimensional; CT: computed tomography; PEEK: polyether-ether-ketone.
Mandibular prosthesis
The mandible maintains the facial contour and is involved in chewing, swallowing, and speech. Malignant tumours, deformities, injury, and infection may result in a mandibular bone defect, further harming facial appearance and physiological function. Consequently, how to repair mandibular defects and restore function has attracted extensive attention. The gold standard for reconstructing mandibular defects is commonly represented by the free microvascular fibular. Nevertheless, the shortage of autologous bone sources greatly restricts its use to repair large-size defects, and bone harvesting will cause secondary trauma. Meanwhile, non-vascularised autogenous bone is prone to bone resorption owing to the mechanical factors and lack of nutrient supply, leading to further inflammation and infection. In addition, many biomaterials, including metals, inorganic materials, organic materials, and composites, have been used as a substitute for the mandibular defect. While each material has its unique advantages and weaknesses, there are still some problems in clinical application to be resolved.
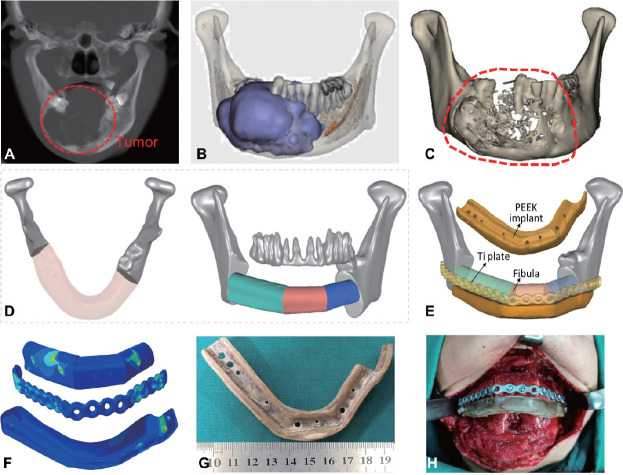
The repair of a mandibular defects needs to restore the physiological functions as well as considering the anatomical morphology and aesthetic effect. For this purpose, a new functional repair method has been developed for mandibular defects, combining a 3D-printed PEEK implant and a free vascularised fibula graft.71 Throughout the design process, three criteria were taken into account: safety, functionality and shape-matching.
The detailed design workflow for mandibular defect repair in one case, combining a fibula autograft with a 3D-printed PEEK implant, is shown in Figure 6. Based on the patient’s CT images, 3D models of tumour and bone were built, and clinical osteotomy was simulated by digital technologies under the clinician’s guidance to determine the defect area. Some key parameters were measured according to the shape and occlusion function requirement, and a vascularised fibula graft was segmented for assembly. A titanium plate and PEEK implant were custom-designed. To ensure safety and stability, biomechanical and mechanobiological properties of the mandibular reconstruction model were evaluated under various masticatory motions by the finite element (FE) method. Subsequently, the PEEK implant was printed by FFF. The clinical application was carried out after passing quality inspection. Follow-up observation revealed that the vascularised fibula was well integrated and did not produce inflammation. Finally, dental implants were fitted in the second stage which was completed with a satisfactory outcome.
Figure 6. 3D-printed PEEK implant for mandibular defect repair. (A) CT image. (B) 3D model with tumour (blue). (C) 3D model of the mandible. Dotted outline indicates the location of the tumour. (D) Pre-operative planning for fibula graft and (E) implantation. (F) FEA results of PEEK implant and Ti plate. (G) 3D printed PEEK mandibular prosthesis. (H) Intraoperative photograph. 3D: three-dimensional; CT: computed tomography; FEA: finite element analysis; PEEK: polyether-ether-ketone; Ti: titanium.
Although this combination of a 3D-printed PEEK implant with a free vascularised fibula graft has proven to be effective for the repair of mandibular defects, the osseointegration capability at the implant-bone interface needs to be further improved due to the bioinert nature of the PEEK material. Therefore, some strategies, such as surface modification, microstructure design, and PEEK/bio-ceramic composites, will be studied to facilitate osseointegration, further enhancing the implant’s long-term stability and service life.
Reconstruction of the chest wall
The thoracic cage is the skeletal framework of the thoracic wall, and it is formed by the 12 thoracic vertebrae, 12 pairs of ribs with associated costal cartilages, and the sternum. It supports the thorax, protecting internal organs from external forces and resisting the negative internal pressures generated by the elastic recoil of the lungs and respiration-induced movements. However, as a result of malignant tumours, congenital deformities, and thoracic injuries caused by road traffic accidents, the reconstruction of chest wall defects is often necessary in the clinic. Traditional means of repairing chest wall defects frequently involved bending a metal plate or embracing rib fracture plate. Meanwhile, with the unique advantages of 3D printing technology, some custom-designed metal implants have been applied. However, post-operative complications have revealed that respiratory limitation reaching up to 27% may be related to the choice of rigid repair.72 Due to the significant differences in elastic modulus or toughness between metal materials and host bone, the long-term stability of an implant may be affected in the actual bearing conditions of daily life. Therefore, improvements in the clinical performance of implants and a reduction of post-operative complications through the use of better-suited biomaterials and a subject-specific design are still required.
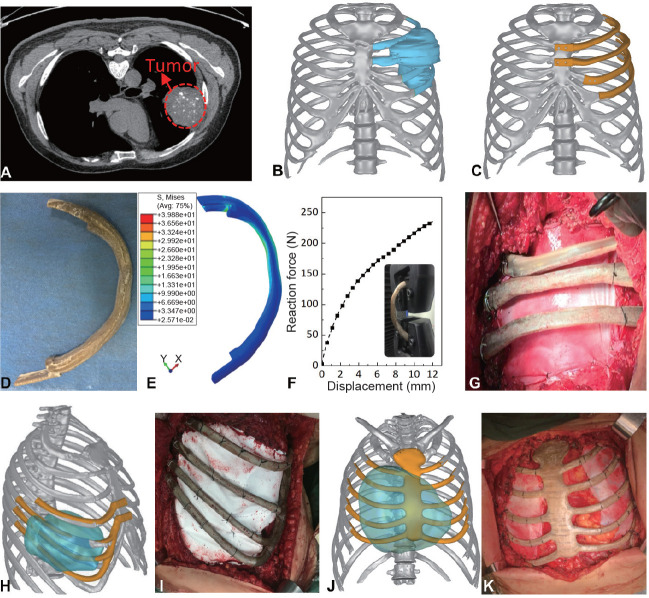
Chest wall reconstruction needs to restore the integrity of the thoracic contour and consider its safety in service and impact on respiratory function. Hence, a new design method has been proposed for a 3D-printed PEEK rib prosthesis based on the centroid trajectory of a natural rib diaphysis and variable section sweep. By this means, the shape and performance can be controlled, effectively reducing the adverse influence of the stepping effect in the printing process on prosthetic performance. The detailed framework of a 3D-printed PEEK rib implant for chest wall reconstruction is shown in Figure 7A-K. 3D models of the thoracic cage and the tumour were generated from CT images, and a simulated osteotomy was carried out under the condition of a 30 mm out-diffusion of the tumour boundary. Then, a personalised sternal rib implant was designed and evaluated by the FE method and experimental testing. Finally, the PEEK implant was applied in the clinic following overall testing qualification.
Figure 7. 3D-printed PEEK implant for chest wall reconstruction. (A) CT image. (B) 3D model with tumour (blue). (C) 3D model of the thoracic cavity and rib prosthesis (yellow). (D) 3D printed rib prosthesis. (E) FEA results. (F) Results of mechanical testing. (G) Intraoperative photograph. (H, I) Design (H) and implantation (I) of the costal arch prosthesis. (J, K) Design (J) and implantation (K) of the sternum prosthesis. The yellow indicates the implant, and the blue indicates the tumour. 3D: three-dimensional; CT: computed tomography; FEA: finite element analysis; PEEK: polyether-ether-ketone.
In addition, according to the shape of the chest wall defect after tumour resection, costal arch implants and sternal rib implants were further developed and are shown in Figure 7H-K.73 To date, more than one hundred clinical applications have been completed, and the follow-up results showed that the 3D PEEK implants have good safety and stability.53 However, due to the lack of natural rib cartilage, respiratory movement was still limited to a certain extent, but it was better than could be obtained with a metal implant. Consequently, a new bionic methodology for designing a costal cartilage prosthesis has been developed, using a wavy elastic structure.74 By changing the design parameters, the mechanical properties of the bionic elastic structure can be accurately adjusted to match that of costal cartilage. Therefore, the designed PEEK costal cartilage prostheses can replace the natural costal cartilage with better breathing function for patients undergoing chest wall reconstruction.
Scapula replacement
A bone tumour in the scapula is a rare entity. The most common lesion is chondrosarcoma, followed by Ewing’s sarcoma and osteosarcoma.75 A scapular tumour usually has no obvious early symptoms and an extensive invasion when found. Therefore, scapular reconstruction is often required after total scapular resection, and scapular prostheses are the primary means of scapula reconstruction to achieve a better shape and restore function.76
Based on the clinical requirements of scapular reconstruction, a suitable scapular prosthesis should have the following functions under the premise of safety. On the one hand, the prosthesis should help maintain the shoulder joint and restore the anatomical structure of the scapula. On the other hand, the prosthesis should combine firmly with the surrounding soft tissue and muscle to achieve stable reconstruction and restore the motor function of the shoulder joint.
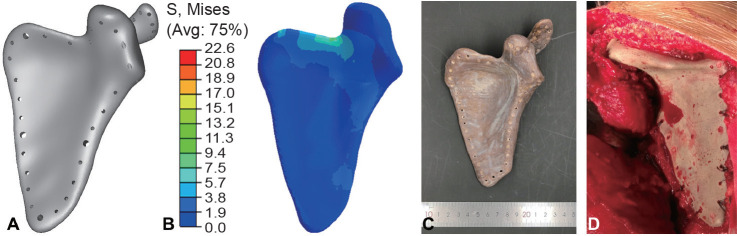
We designed a novel scapular prosthesis (Figure 8). CT images were imported into Mimics 16.0 (Materialise, Leuven, Belgium) to reconstruct a 3D model of the scapula. The prosthesis was designed based on a mirror image of the healthy scapula transferred onto the affected side to maintain the anatomical structure of the scapula. Uniform channels were designed around the prosthesis, making it convenient for surgeons to suture the major muscle ligaments of the shoulder joint and thus achieve a stable reconstruction effect. Furthermore, PEEK material was used to reduce the weight of the prosthesis. The safety of the prosthesis was evaluated using the FE method according to a previous study.77 The maximum von Mises stress of the PEEK scapular prosthesis was 22.6 MPa, lower than the yield strength of PEEK material,78 which indicated that the strength of the designed PEEK scapular prosthesis could sustain the loading requirement in vivo. Afterward, the PEEK prosthesis was fabricated by FFF technology using the 3D-printing system (Surgeon 200, Jugao-AM, Xi’an, China) with a layer thickness of 0.2 mm, a printing speed of 40 mm/s and a nozzle temperature of 420°C. Finally, the prosthesis was implanted into the patient.
Figure 8. 3D-printed PEEK scapula prosthesis. (A) Design. (B) Strength evaluation. (C) Photograph of scapula prosthesis. (D) Intraoperative photograph. 3D: three-dimensional; PEEK: polyether-ether-ketone.
The patient was followed up three months after surgery and the constant score of the reconstructed shoulder function was 68 points. The anatomical shape and motor function of the scapula were restored successfully.79 However, there were also some limitations of the prosthesis. The radiolucency and bioinert nature of the PEEK material affected post-operative observation and long-term stability of the prosthesis, respectively. Therefore, new technologies such as novel materials and surface modifications are supposed to be used to overcome the above shortcomings of the PEEK scapular prosthesis.
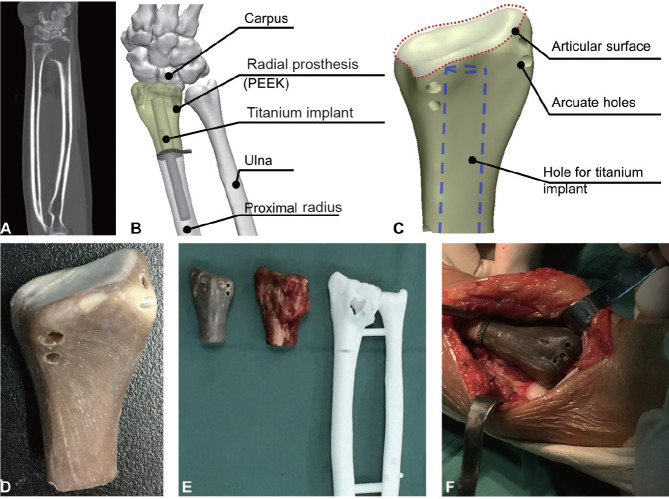
Radial prosthesis
The radius plays an essential role in movement of the arm and wrist motion. When a giant cell tumour occurred on the radius, the affected radial segment must be removed and reconstructed. AM PEEK radial prosthesis was a feasible way to reconstruct the removed segment. Based on awareness of these functions, a distal radial prosthesis was designed, as shown in Figure 9. The geometry of the prosthesis was reconstructed according to a 3D model reconstructed from CT data.
Figure 9. Clinical application of a 3D-printed PEEK radial prosthesis. (A) CT image. (B) Surgical plan of radial reconstruction. (C) Design of the radial prosthesis. (D) Photograph of the 3D-printed PEEK radial prosthesis. (E) Photographs of the prosthesis, tumour and medical model. (F) Intraoperative photograph. 3D: three-dimensional; CT: computed tomography; PEEK: polyether-ether-ketone.
The primary requirements of the radial prosthesis include stable fixation to the bone and soft tissue and movement of the wrist joint. The arcuate holes were positioned according to the attachment position of muscles of the forearm, allowing suturing to the muscle. The articular surface should have higher hardness and finish to form the wrist joint with the carpus. Due to the poor osseointegration of PEEK material, a 3D-printed implant made from Ti6Al4V was used in combination with the PEEK implant to obtain biological fixation with the proximal radius. The Ti6Al4V implant consisted of three parts, an intramedullary nail with a porous structure, which is expected to integrate with the bone, a distal part, which would be inserted into the PEEK prosthesis to build a mechanical fixation through an interference fit, and a small cylinder to prevent relative rotation between the proximal radius and the Ti6Al4V implant.
The PEEK radial prosthesis was manufactured by FFF (Surgeon 200, Jugao-AM). Higher hardness of the articular surface was obtained by local thermal treatment to improve the crystallinity of PEEK, then the prosthesis was polished.
Osteoarticular allograft arthroplasty, fibula autograft arthroplasty80, 81 and prosthesis replacement are the main techniques of wrist arthroplasty after resection of bone tumours of the distal radius, of which the former two are more frequent in the clinic.82 However, better anatomical matching would be obtained through the use of a 3D-printed customised radial prosthesis, which also avoids the complications related to the use of grafts.83 Lu et al.84 reported a series of clinical cases involving 3D-printed radial prostheses, which consisted of a metal part manufactured by electron beam melting technology and an ultrahigh-molecular-weight polyethylene liner. A retrieval study of a 3D-printed porous titanium implant of the radial prosthesis by Park et al.85 showed that tissue ingrowth was observed in the porous implant. In the clinical case reported in this section, a porous titanium nail was employed to promote bone ingrowth and further osseointegration. Some issues, such as promoting the osseointegration of PEEK through composites and porous design, as well as the combination of a porous structure with mechanical sutures to produce biological integration between soft tissue and PEEK implant, may be improved in further study.
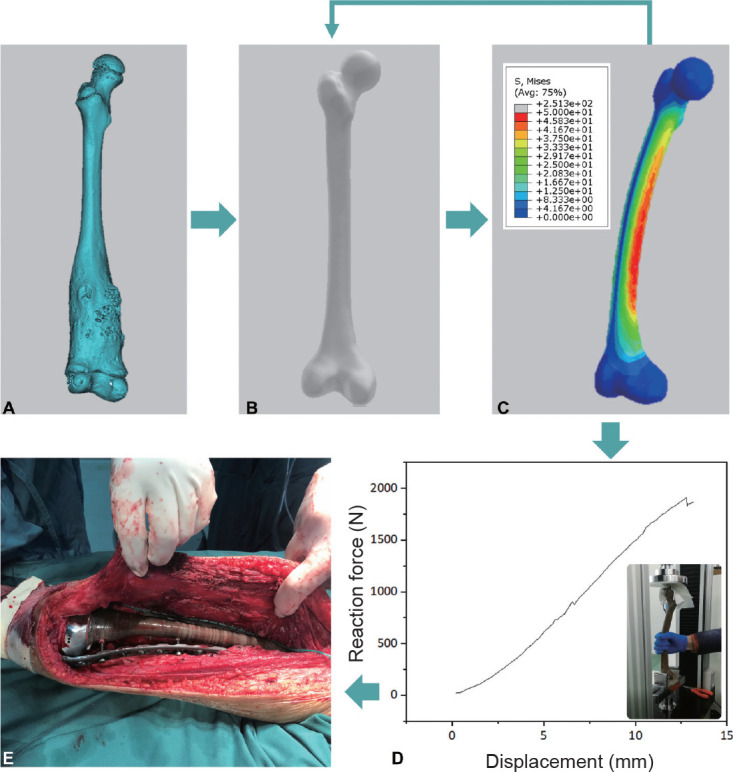
Replacement of femoral segment
The resection of a malignant femoral tumour causes an extensive defect in the human femur and affects its structure and function.86 Prosthetic replacement technology can preserve the essential functions of human lower limbs and significantly improve the life quality of patients with bone defects.87 3D printing technology has been used to create metal implants to repair human lower limb long bones,88, 89 but PEEK has rarely been reported for lower limb long bone repair due to its low strength compared to metals.
Reconstruction of a long bone segment of the lower limb must take into account the following design criteria. i) An appropriate load-bearing ability. The prosthesis must support the loading generated by everyday activities without undergoing fracture, plastic deformation or excessive elastic deformation. ii) A matching shape. A typical case is shown in Figure 10. The geometry of the PEEK femoral substitute was initially designed according to the femur of the healthy side. Since load-bearing is the predominant function of a femoral substitute, the safety of the designed PEEK femoral substitute was evaluated through FEA. Defining the safety factor as the ratio of the yield strength of PEEK to the maximum stress of the designed prosthesis enabled quantitative measurement of the safety performance of the femoral prosthesis. In order to prevent the prosthesis from breaking in the human body under normal activity, the allowable safety factor must be greater than 1. Otherwise, the designed prosthesis should be revised and be recalculated until the safety factor meets the requirements. A femoral implant was manufactured using the FFF method, and the bearing capacity of the implant was tested. It revealed that the 3D-printed PEEK femoral prosthesis could withstand a maximum vertical load of 1900 N, which satisfied the mechanical requirements. The PEEK femoral prosthesis was successfully implanted in the patient’s body and had a high degree of consistency with the surrounding tissue structure, which guaranteed the stability and safety of the femoral prosthesis in the human body.
Figure 10. 3D-printed PEEK femoral segmental prosthesis. (A) 3D model of the femur with tumour. (B) Femur of healthy side. (C) FEA results of the PEEK femoral prosthesis. (D) Force-displacement curve of the 3D-printed PEEK femoral prosthesis. (E) Intraoperative photograph. 3D: three-dimensional; FEA: finite element analysis; PEEK: polyether-ether-ketone.
Ethical approval
Ethical approval for the clinical applications were granted by Air Force Medical University, China (approval No. TDLL-2016196-450, approved on November 10, 2016), Stomatological Hospital, Southern Medical University, China (approval No. 201928, approved on December 28, 2019) and the Affiliated Hospital of Southwest Medical University (approval No. KY2021133, approved on May 28, 2021). The study complied with all requirements of the 1964 Declaration of Helsinki, as revised in 2013. All the patients or their legal guardians volunteered to participate the study and signed informed consent forms.
Discussion
Summary
In this review, clinical cases employing 3D-printed implants to repair several parts of the human body were designed and manufactured by our group in cooperation with different physicians. Different departments such as neurosurgery, orthopaedics, oral and maxillofacial surgery, and thoracic surgery were involved in the cases, reflecting the broad applicability of AM of PEEK and its composites in orthopaedic implants.
Some or all of the design criteria described in the section on design criteria were embodied, and similar design processes were followed in the clinical cases. For example, the femur plays a critical role in the mechanical function of load-bearing and movement of the human body, thus the long-term safety of a femoral prosthesis should be thoroughly checked to avoid implant fracture. Thus, in the case of the femoral prosthesis, the mechanical performance of the implant under the gait cycle was predicted by FEA. The mechanical properties of the implant were also tested to ensure the mechanical safety of the femoral prosthesis. As for the mandible, although it does not bear the weight of the human body, the physiological loading from the action of chewing could not be ignored. However, it is difficult to apply the loads from the maxillofacial muscles to the mandible prosthesis, so FEA was carried out to ensure the safety of the prosthesis. Repairing the deformity was the primary purpose of the implant for paranasal augmentation, thus the geometry of the design and the prediction of improvement of deformity were the major focuses. To reduce the risk of long-term dislocation caused by unstable long-term fixation with screws, osseointegration was further pursued to obtain biological fixation with the bone.
All the implants described in this paper were manufactured by FFF. Compared with manufacture by SLS, PEEK parts made by FFF possessed increased toughness.52, 90 Most of the implants in this paper such as the skull, ribs, or scapula, were not expected to bear large physiological loads in the human body, thus the higher toughness enabled them to survive accidental impact and protect internal organs. In contrast, higher ultimate strength was required for the load-bearing implant represented by the femoral prosthesis. The mechanics of PEEK parts could be adjusted through changes in crystallinity by controlling the temperature of the building chamber as described by Yang et al.,52 which is expected to be used to manufacture implants with different mechanical properties in different parts, for example, the wrist joint of the radial implant in this paper.
Challenges and developments
Although the many advantages of PEEK and it is widely used in the clinic, its biological inertness limits effective integration between host tissues (soft tissue, bone tissue) and PEEK prostheses, leading to long-term loosening and post-operative infection.91 To enhance the bonding strength between PEEK and surrounding tissue, many studies have been carried out on modification of PEEK by physical or chemical methods. The introduction of active groups onto the surface of PEEK through spray-coating, plasma treatment or chemical grafting has been used for PEEK surface functionalisation. A bioactive coating on the surface of PEEK significantly improves its biological activity.92, 93 However, owing to the poor bonding strength between the coating and the PEEK matrix, wear and delamination of the coating may result in post-operative inflammation and implant failure. PEEK surfaces treated by plasma usually exhibited better wettability and specific surface properties, which were conducive to osteoblast attachment and differentiation.94 However, the residual stresses caused by plasma spraying reduced the mechanical fatigue strength.95
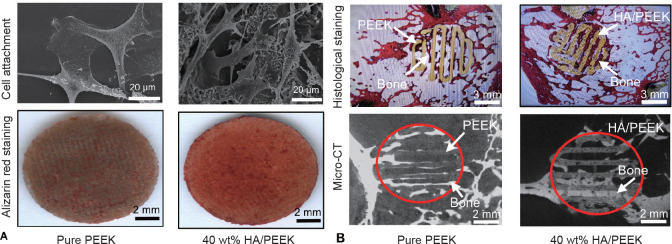
In addition, any chemical modification process is usually complicated, and it is challenging to achieve a uniform modification effect. Meanwhile, grafted surfaces result in new challenges for subsequent implant preservation and disinfection. Thus, chemically-modified PEEK materials still have a long way to go before they are ready for clinical applications. Engineering the usability of AM, PEEK-based composites by introducing bioactive materials such as hydroxyapatite, calcium phosphate and calcium silicate, is a feasible method to solve the problem of poor bonding between PEEK and natural tissues.78, 96 The promotional effects of bioactive fillers on the cell response and osseointegration has been widely reported,78, 97 as shown in Figure 11. The morphology of MC-3T3 cell and calcium nodules results were shown in Figure 11A. More pseudopodium and calcium nodules were found on the surface of HA/PEEK composites after cultured with 5 days, demonstrating that positive osteogenesis of the addition of HA particle. The pure PEEK and HA/PEEK composites scaffolds were implanted into femoral condyle of rabbit. The histological staining and Micro-CT results of bone ingrowth were shown as Figure 11B. More bone ingrowth volume was found in HA/PEEK scaffolds. In addition, reinforced fillers such as carbon fibre have also been employed to enhance the mechanical properties of PEEK.98, 99 Up to now, improving both mechanical properties and biological characterisation remain the focus of PEEK-based composites.
Figure 11. Biological evaluation of HA/PEEK composites. (A) In vitro cell experiment. (B) Bone-ingrowth in scaffolds of PEEK and 40 wt% HA/PEEK. The red circle indicates the outline of PEEK and HA/PEEK scaffolds in CT images. HA: hydroxyapatite; PEEK: polyether-ether-ketone.
Material modification alone may not be sufficient to achieve better bonding between PEEK and surrounding tissues. The mechanical lock between the PEEK implant and surrounding tissues led by porous structure is essential. Various technologies have been used to manufacture PEEK implants with porous structure, including the salt leaching method,100 sulfonation treatment101 and 3D printing.95 Both in vitro and in vivo studies have shown the vital role of porous structure in the osseointegration of PEEK-based implants. PEEK-based composite scaffolds and chemical modification could be combined with a porous structure to realise more complex biological functions.91, 102, 103
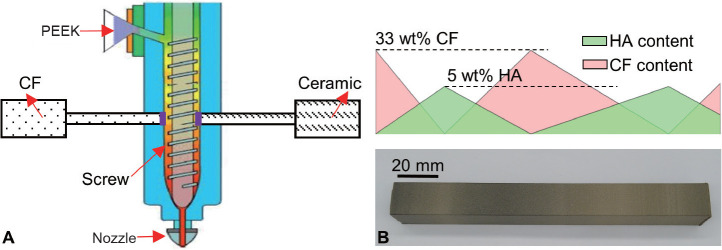
In order to achieve excellent mechanical properties and biocompatibility of PEEK implants, a multi-material heterogeneous prosthesis design and manufacture method is proposed. Firstly, screw extrusion printing equipment (Figure 12A) capable of online mixing of PEEK, bioceramics and carbon fibre has been developed, which precisely controlled material composition (Figure 12B). By this means, 3D-printed PEEK orthopaedic implants with graded material composition and porous structure can be manufactured, satisfying both mechanical and biological requirements.
Figure 12. (A) Schematic diagram of screw extrusion printing equipment and (B) heterogeneous specimen. CF: carbon fibre; HA: hydroxyapatite; PEEK: polyether-ether-ketone.
Clinical translation
The regulatory system consisting of regulation, technical standards and evaluation guidance is the prerequisite for the clinical translation of AM PEEK orthopaedic implants instead of clinical research under the supervision of ethics committees. Authorities from different countries have acted to face the challenge brought by AM medical devices. The first milestone in the regulation of AM medical devices was the workshop entitled “Additive Manufacturing of Medical Devices: An Interactive Discussion on the Technical Considerations of 3D Printing” held by the US Food and Drug Administration (FDA) in October 2014.104 The workshop indicated that the authorities had begun to establish a regulatory system for AM medical devices.104 Later, the FDA published the “Technical Considerations for Additive Manufactured Medical Devices-Guidance for Industry and Food and Drug Administration Staff” in December 2017. Since 2018, more than 10 technical reviews of guidance for the registration of AM medical devices have been released or drafted by the National Medical Products Administration (NMPA) of China. “Regulation for the Supervision and Management of Custom Medical Devices” was issued by NMPA in July 2019,105 in which the filing system was introduced. Under the filing system, the manufacturer and medical organisation shall file together for each AM custom implant clinical case. The filing system of NMPA is similar to the regulatory model for custom devices of the FDA, but the number of custom devices that a company can produce is not limited while a significant limitation from the FDA on the custom devices is that each company can only produce five devices per year.106
Although AM technology has been used in orthopaedic implants for nearly 20 years, few products have been approved to enter the market. Two general categories constrain the industrialisation of AM orthopaedic implants. On the one hand, the uncertainty caused by the customisation made it difficult to conduct any statistical analysis in the evaluation of the safety and efficacy of the implant, which brought challenges to the properties testing, risk assessment and evaluation of the clinical effect.107 On the other hand, the forming principle of AM brought some difficulties to the quality evaluation of the AM orthopaedic implant, such as the change of chemical and physical properties of raw materials because of the heating-cooling process during AM and the introduction of impurities.
Technical standards are one of the most vital accordances during the production and marketing of orthopaedic devices. The International Standardisation Organisation (ISO) and American Society of Testing Materials (ASTM) jointly established a technical committee TC 261 and ASTM F42 for AM technology.108 The National Standardisation Technical Committee of China TC 562 was created in 2016.109 These committees establish standards for the materials, software, equipment, and test methods in AM, in which medical devices are not included. However, improvements of the standards governing raw materials, manufacturing equipment, and testing methods related to AM also played an essential role in promoting the marketing of orthopaedic implants since they provided standardised approaches to investigating the effects of AM processes on the geometric, physical, chemical and mechanical properties of products. To date, more than 100 devices made by AM have been cleared by the FDA, and the NMPA has also approved 11 AM medical devices by April 2021105 in China, including intervertebral fusion cages with porous structure, acetabular cups and pelvic reconstruction prostheses.
However, to the best of our knowledge, no PEEK orthopaedic implant made by AM has been approved to enter the market to date. The lack of standards was a vital reason. At present, there are only a few standards applicable to PEEK orthopaedic implants worldwide, for example, ASTM F2026,3 ASTM F3333110 and ISO 15309,111 but no standards for AM of PEEK. Therefore, the AM PEEK implant encountered resistance during the performance evaluation and approval processes. Fortunately, the NMPA announced the “Technical Review Guidance for Registration of AM PEEK Orthopaedic Implant” in March 2022,112 which guided the development and production of AM PEEK orthopaedic implants.
Outlook
With deeper understanding of the bonding between PEEK-based composites with soft and bone tissue, PEEK-based composites would be the future of AM PEEK orthopaedic implant. Two major problems, including the poor bonding with natural tissue which was caused by the innerness, and endurance of using as load-bearing implant due to its the weak mechanical strength compared to the metal, facing by PEEK orthopaedic implant could be solved by adding bioactive fillers and enhance fillers, such as HA and carbon fibre, into the PEEK matrix. AM PEEK orthopaedic implants would be commercialised in the near future as the continuous improvement of regulatory and technical standards related to the AM medical devices.
Conclusion
The use of PEEK in orthopaedic implants is becoming increasingly widespread because of its excellent biocompatibility and appropriate mechanical properties. Clinical research on customised PEEK implants such as ribs, radius and cranioplasty patches has obtained encouraging progress which benefited from the development of AM, and strongly supported the clinical translation of customised PEEK implants. Although the weak bonding between PEEK implants and natural tissues still needs to be overcome, the strategies of using PEEK-based composites and porous structure are expected to solve the problem. In addition, there are some obstacles in terms of regulation and technical standards that need to be overcome before the clinical translation of AM customised PEEK implants.
Funding Statement
The work was supported by the National Key R&D Program of China (No. 2018YFE0207900), the National Natural Science Foundation of China (No. 51835010), the Key R&D Program of Guangdong Province, China (No. 2018B090906001), China Postdoctoral Science Foundation (No. 2020M683458), the Natural Science Basic Research Program of ShaanXi Province, China (No. 2022JQ-378), the Engineering and Physical Science Research Council (EPSRC) via DTP Case Programme (No. EP/T517793/1), the Fundamental Research Funds for the Central Universities (No. XZY012021007), the Laboratory Construction Project for Jihua Laboratory (No. X200031TM200), Open Project (No. BHJ17C019) and the Youth Innovation Team of Shaanxi Universities.
Footnotes
Acknowledgement: None.
Conflicts of interest statement: There are no conflicts of interest in this work.
References
- 1.Kurtz S. M. Chapter 1 - An overview of PEEK biomaterials. In: Kurtz S. M., editor. PEEK biomaterials handbook. Second Edition. William Andrew Publishing; 2019. pp. 3–9. [Google Scholar]
- 2.Panayotov I. V., Orti V., Cuisinier F., Yachouh J. Polyetheretherketone (PEEK) for medical applications. J Mater Sci Mater Med. 2016;27:118. doi: 10.1007/s10856-016-5731-4. [DOI] [PubMed] [Google Scholar]
- 3.American Society of Testing Materials. ASTM F2026-17: Standard Specification for Polyetheretherketon (PEEK) Polymers for Surgical Implant Applications [Google Scholar]
- 4.Zanotti B., Zingaretti N., Verlicchi A., Robiony M., Alfieri A., Parodi P. C. Cranioplasty: review of materials. J Craniofac Surg. 2016;27:2061–2072. doi: 10.1097/SCS.0000000000003025. [DOI] [PubMed] [Google Scholar]
- 5.Kim S. R., Kim D. H., Kim D. J., Kim M. H., Park J. M. Study on thermal conductivity of polyetheretherketone/thermally conductive filler composites. Solid State Phenomena. 2007;124-6:1079–1082. [Google Scholar]
- 6.Feldmann A., Wili P., Maquer G., Zysset P. The thermal conductivity of cortical and cancellous bone. Eur Cell Mater. 2018;35:25–33. doi: 10.22203/eCM.v035a03. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz S. M., Devine J. N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials. 2007;28:4845–4869. doi: 10.1016/j.biomaterials.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seaman S., Kerezoudis P., Bydon M., Torner J. C., Hitchon P. W. Titanium vs. polyetheretherketone (PEEK) interbody fusion: Meta-analysis and review of the literature. J Clin Neurosci. 2017;44:23–29. doi: 10.1016/j.jocn.2017.06.062. [DOI] [PubMed] [Google Scholar]
- 9.Rao P. J., Pelletier M. H., Walsh W. R., Mobbs R. J. Spine interbody implants: material selection and modification, functionalization and bioactivation of surfaces to improve osseointegration. Orthop Surg. 2014;6:81–89. doi: 10.1111/os.12098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cowie R. M., Briscoe A., Fisher J., Jennings L. M. PEEK-OPTIMA(TM) as an alternative to cobalt chrome in the femoral component of total knee replacement: A preliminary study. Proc Inst Mech Eng H. 2016;230:1008–1015. doi: 10.1177/0954411916667410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schierjott R. A., Giurea A., Neuhaus H. J., Schwiesau J., Pfaff A. M., Utzschneider S., Tozzi G., Grupp T. M. Analysis of carbon fiber reinforced PEEK hinge mechanism articulation components in a rotating hinge knee design: a comparison of in vitro and retrieval findings. Biomed Res Int. 2016;2016:7032830. doi: 10.1155/2016/7032830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guzzini M., Lanzetti R. M., Lupariello D., Morelli F., Princi G., Perugia D., Ferretti A. Comparison between carbon-peek plate and conventional stainless steal plate in ankle fractures. A prospective study of two years follow up. Injury. 2017;48:1249–1252. doi: 10.1016/j.injury.2017.03.035. [DOI] [PubMed] [Google Scholar]
- 13.Ma Z., Zhao X., Zhao J., Zhao Z., Wang Q., Zhang C. biologically modified polyether ether ketone as dental implant material. Front Bioeng Biotechnol. 2020;8:620537. doi: 10.3389/fbioe.2020.620537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wiesli M. G., Özcan M. High-performance polymers and their potential application as medical and oral implant materials: a review. Implant Dent. 2015;24:448–457. doi: 10.1097/ID.0000000000000285. [DOI] [PubMed] [Google Scholar]
- 15.Jiang X., Yao Y., Tang W., Han D., Zhang L., Zhao K., Wang S., Meng Y. Design of dental implants at materials level: An overview. J Biomed Mater Res A. 2020;108:1634–1661. doi: 10.1002/jbm.a.36931. [DOI] [PubMed] [Google Scholar]
- 16.Zhao F., Li D., Jin Z. Preliminary investigation of poly-ether-ether-ketone based on fused deposition modeling for medical applications. Materials (Basel) 2018;11:288. doi: 10.3390/ma11020288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haleem A., Javaid M. Polyether ether ketone (PEEK) and its 3D printed implants applications in medical field: an overview. Clin Epidemiol Glob Health. 2019;7:571–577. [Google Scholar]
- 18.He J., Li D., Lu B., Wang Z., Tao Z. Custom fabrication of composite tibial hemi-knee joint combining CAD/CAE/CAM techniques. Proc Inst Mech Eng H. 2006;220:823–830. doi: 10.1243/09544119JEIM207. [DOI] [PubMed] [Google Scholar]
- 19.Harrysson O. L., Hosni Y. A., Nayfeh J. F. Custom-designed orthopedic implants evaluated using finite element analysis of patient-specific computed tomography data: femoral-component case study. BMC Musculoskelet Disord. 2007;8:91. doi: 10.1186/1471-2474-8-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murr L. E. Additive manufacturing of biomedical devices: an overview. Mater Technol. 2018;33:57–70. [Google Scholar]
- 21.Moiduddin K. Implementation of computer-assisted design, analysis, and additive manufactured customized mandibular implants. J Med Biol Eng. 2018;38:744–756. [Google Scholar]
- 22.Ackland D. C., Robinson D., Redhead M., Lee P. V. S., Moskaljuk A., Dimitroulis G. A personalized 3D-printed prosthetic joint replacement for the human temporomandibular joint: From implant design to implantation. J Mech Behav Biomed Mater. 2017;69:404–411. doi: 10.1016/j.jmbbm.2017.01.048. [DOI] [PubMed] [Google Scholar]
- 23.Norman P., Iyengar S., Svensson I., Flivik G. Fatigue fracture in dual modular revision total hip arthroplasty stems: failure analysis and computed tomography diagnostics in two cases. J Arthroplasty. 2014;29:850–855. doi: 10.1016/j.arth.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 24.Giesinger K., Ebneter L., Day R. E., Stoffel K. K., Yates P. J., Kuster M. S. Can plate osteosynthesis of periprosthethic femoral fractures cause cement mantle failure around a stable hip stem? A biomechanical analysis. J Arthroplasty. 2014;29:1308–1312. doi: 10.1016/j.arth.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 25.Westerman A. P., Moor A. R., Stone M. H., Stewart T. D. Hip stem fatigue: The implications of increasing patient mass. Proc Inst Mech Eng H. 2018;232:520–530. doi: 10.1177/0954411918767200. [DOI] [PubMed] [Google Scholar]
- 26.de Oliveira B. J. S., Campanelli L. C., Oliveira D. P., de Bribean Guerra A. P., Bolfarini C. Surface characterization and fatigue performance of a chemical-etched Ti-6Al-4V femoral stem for cementless hip arthroplasty. Surf Coat Technol. 2017;309:1126–1134. [Google Scholar]
- 27.Dong E., Iqbal T., Fu J., Li D., Liu B., Guo Z., Cuadrado A., Zhen Z., Wang L., Fan H. Preclinical strength checking for artificial pelvic prosthesis under multi-activities - a case study. J Bionic Eng. 2019;16:1092–1102. [Google Scholar]
- 28.Mathai B., Dhara S., Gupta S. Orthotropic bone remodelling around uncemented femoral implant: a comparison with isotropic formulation. Biomech Model Mechanobiol. 2021;20:1115–1134. doi: 10.1007/s10237-021-01436-6. [DOI] [PubMed] [Google Scholar]
- 29.Majumdar T., Eisenstein N., Frith J. E., Cox S. C., Birbilis N. Additive manufacturing of titanium alloys for orthopedic applications: a materials science viewpoint. Adv Eng Mater. 2018;20:1800172. [Google Scholar]
- 30.Sun C., Wang L., Kang J., Li D., Jin Z. Biomechanical optimization of elastic modulus distribution in porous femoral stem for artificial hip joints. J Bionic Eng. 2018;15:693–702. [Google Scholar]
- 31.Wang X., Xu S., Zhou S., Xu W., Leary M., Choong P., Qian M., Brandt M., Xie Y. M. Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants: A review. . Biomaterials. 2016;83:127–141. doi: 10.1016/j.biomaterials.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 32.Hedayati R., Janbaz S., Sadighi M., Mohammadi-Aghdam M., Zadpoor A. A. How does tissue regeneration influence the mechanical behavior of additively manufactured porous biomaterials? J Mech Behav Biomed Mater. 2017;65:831–841. doi: 10.1016/j.jmbbm.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 33.Taniguchi N., Fujibayashi S., Takemoto M., Sasaki K., Otsuki B., Nakamura T., Matsushita T., Kokubo T., Matsuda S. Effect of pore size on bone ingrowth into porous titanium implants fabricated by additive manufacturing: an in vivo experiment. Mater Sci Eng C Mater Biol Appl. 2016;59:690–701. doi: 10.1016/j.msec.2015.10.069. [DOI] [PubMed] [Google Scholar]
- 34.Bessard E., De Almeida O., Bernhart G. Unified isothermal and non-isothermal modelling of neat PEEK crystallization. J Therm Anal Calorim. 2014;115:1669–1678. [Google Scholar]
- 35.Zanjanijam A. R., Major I., Lyons J. G., Lafont U., Devine D. M. Fused filament fabrication of PEEK: a review of process-structure-property relationships. Polymers. 2020;12:1665. doi: 10.3390/polym12081665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singh S., Prakash C., Ramakrishna S. 3D printing of polyether-ether-ketone for biomedical applications. Eur Polym J. 2019;114:234–248. [Google Scholar]
- 37.Kang J., Wang L., Yang C., Wang L., Yi C., He J., Li D. Custom design and biomechanical analysis of 3D-printed PEEK rib prostheses. Biomech Model Mechanobiol. 2018;17:1083–1092. doi: 10.1007/s10237-018-1015-x. [DOI] [PubMed] [Google Scholar]
- 38.Arabnejad S., Johnston B., Tanzer M., Pasini D. Fully porous 3D printed titanium femoral stem to reduce stress-shielding following total hip arthroplasty. J Orthop Res. 2017;35:1774–1783. doi: 10.1002/jor.23445. [DOI] [PubMed] [Google Scholar]
- 39.Ahirwar H., Gupta V. K., Nanda H. S. Finite element analysis of fixed bone plates over fractured femur model. Comput Methods Biomech Biomed Engin. 2021;24:1742–1751. doi: 10.1080/10255842.2021.1918123. [DOI] [PubMed] [Google Scholar]
- 40.Cameron H. U., Pilliar R. M., MacNab I. The effect of movement on the bonding of porous metal to bone. J Biomed Mater Res. 1973;7:301–311. doi: 10.1002/jbm.820070404. [DOI] [PubMed] [Google Scholar]
- 41.Maniatopoulos C., Pilliar R. M., Smith D. C. Threaded versus porous-surfaced designs for implant stabilization in bone-endodontic implant model. J Biomed Mater Res. 1986;20:1309–1333. doi: 10.1002/jbm.820200907. [DOI] [PubMed] [Google Scholar]
- 42.Li Z., Müller R., Ruffoni D. Bone remodeling and mechanobiology around implants: Insights from small animal imaging. J Orthop Res. 2018;36:584–593. doi: 10.1002/jor.23758. [DOI] [PubMed] [Google Scholar]
- 43.Cheong V. S., Fromme P., Mumith A., Coathup M. J., Blunn G. W. Novel adaptive finite element algorithms to predict bone ingrowth in additive manufactured porous implants. J Mech Behav Biomed Mater. 2018;87:230–239. doi: 10.1016/j.jmbbm.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 44.Adell R., Hansson B. O., Brånemark P. I., Breine U. Intra-osseous anchorage of dental prostheses. II. Review of clinical approaches. Scand J Plast Reconstr Surg. 1970;4:19–34. doi: 10.3109/02844317009038440. [DOI] [PubMed] [Google Scholar]
- 45.Wang S., Zhou X., Liu L., Shi Z., Hao Y. On the design and properties of porous femoral stems with adjustable stiffness gradient. Med Eng Phys. 2020;81:30–38. doi: 10.1016/j.medengphy.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 46.Li J., Cui X., Hooper G. J., Lim K. S., Woodfield T. B. F. Rational design, bio-functionalization and biological performance of hybrid additive manufactured titanium implants for orthopaedic applications: A review. J Mech Behav Biomed Mater. 2020;105:103671. doi: 10.1016/j.jmbbm.2020.103671. [DOI] [PubMed] [Google Scholar]
- 47.Yan M., Tian X., Peng G., Li D., Zhang X. High temperature rheological behavior and sintering kinetics of CF/PEEK composites during selective laser sintering. Compos Sci Technol. 2018;165:140–147. [Google Scholar]
- 48.Yan R., Xie C., Zhao Z., Li J. Optimization of selective laser sintering process parameters based on PA12 powders for bone tissue scaffolds. 3D Print Addit Manuf. 2021 doi: 10.1089/3dp.2021.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peng F., Zhao Z., Xia X., Cakmak M., Vogt B. D. Enhanced impact resistance of three-dimensional-printed parts with structured filaments. ACS Appl Mater Interfaces. 2018;10:16087–16094. doi: 10.1021/acsami.8b00866. [DOI] [PubMed] [Google Scholar]
- 50.Kumar P., Ahuja I. P. S., Singh R. Application of fusion deposition modelling for rapid investment casting - a review. Int J Mater Eng Innov. 2012;3:204–227. [Google Scholar]
- 51.Brenken B., Barocio E., Favaloro A., Kunc V., Pipes R. B. Fused filament fabrication of fiber-reinforced polymers: A review. Addit Manuf. 2018;21:1–16. [Google Scholar]
- 52.Yang C., Tian X., Li D., Cao Y., Zhao F., Shi C. Influence of thermal processing conditions in 3D printing on the crystallinity and mechanical properties of PEEK material. J Mater Process Technol. 2017;248:1–7. [Google Scholar]
- 53.Wang L., Huang L., Li X., Zhong D., Li D., Cao T., Yang S., Yan X., Zhao J., He J., Cao Y., Wang L. Three-dimensional printing PEEK implant: a novel choice for the reconstruction of chest wall defect. Ann Thorac Surg. 2019;107:921–928. doi: 10.1016/j.athoracsur.2018.09.044. [DOI] [PubMed] [Google Scholar]
- 54.Luo M., Tian X., Zhu W., Li D. Controllable interlayer shear strength and crystallinity of PEEK components by laser-assisted material extrusion. J Mater Res. 2018;33:1632–1641. [Google Scholar]
- 55.Deng X., Zeng Z., Peng B., Yan S., Ke W. Mechanical properties optimization of poly-ether-ether-ketone via fused deposition modeling. Materials (Basel) 2018;11:216. doi: 10.3390/ma11020216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Khunt C. P., Makhesana M. A., Mawandiya B. K., Patel K. M. Investigations on the influence of printing parameters during processing of biocompatible polymer in fused deposition modelling (FDM) Adv Mater Process Technol. 2021 doi: 10.1080/2374068X.2021.1927651. [DOI] [Google Scholar]
- 57.Wang P., Zou B., Xiao H., Ding S., Huang C. Effects of printing parameters of fused deposition modeling on mechanical properties, surface quality, and microstructure of PEEK. J Mater Process Technol. 2019;271:62–74. [Google Scholar]
- 58.Park S. J., Lee J. E., Park J., Lee N. K., Son Y., Park S. H. High-temperature 3D printing of polyetheretherketone products: Perspective on industrial manufacturing applications of super engineering plastics. Mater Des. 2021;211:110163. [Google Scholar]
- 59.Basgul C., Yu T., MacDonald D. W., Siskey R., Marcolongo M., Kurtz S. M. Does annealing improve the interlayer adhesion and structural integrity of FFF 3D printed PEEK lumbar spinal cages? J Mech Behav Biomed Mater. 2020;102:103455. doi: 10.1016/j.jmbbm.2019.103455. [DOI] [PubMed] [Google Scholar]
- 60.Alkhaibary A., Alharbi A., Alnefaie N., Oqalaa Almubarak A., Aloraidi A., Khairy S. Cranioplasty: a comprehensive review of the history, materials, surgical aspects, and complications. World Neurosurg. 2020;139:445–452. doi: 10.1016/j.wneu.2020.04.211. [DOI] [PubMed] [Google Scholar]
- 61.Aydin S., Kucukyuruk B., Abuzayed B., Aydin S., Sanus G. Z. Cranioplasty: review of materials and techniques. J Neurosci Rural Pract. 2011;2:162–167. doi: 10.4103/0976-3147.83584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bonda D. J., Manjila S., Selman W. R., Dean D. The recent revolution in the design and manufacture of cranial implants: modern advancements and future directions. Neurosurgery. 2015;77:814–824. doi: 10.1227/NEU.0000000000000899. discussion 824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sharma N., Aghlmandi S., Dalcanale F., Seiler D., Zeilhofer H. F., Honigmann P., Thieringer F. M. Quantitative assessment of point-of-care 3D-printed patient-specific polyetheretherketone (PEEK) cranial implants. Int J Mol Sci. 2021;22:8521. doi: 10.3390/ijms22168521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Feroze A. H., Walmsley G. G., Choudhri O., Lorenz H. P., Grant G. A., Edwards M. S. Evolution of cranioplasty techniques in neurosurgery: historical review, pediatric considerations, and current trends. J Neurosurg. 2015;123:1098–1107. doi: 10.3171/2014.11.JNS14622. [DOI] [PubMed] [Google Scholar]
- 65.Fiaschi P., Pavanello M., Imperato A., Dallolio V., Accogli A., Capra V., Consales A., Cama A., Piatelli G. Surgical results of cranioplasty with a polymethylmethacrylate customized cranial implant in pediatric patients: a single-center experience. J Neurosurg Pediatr. 2016;17:705–710. doi: 10.3171/2015.10.PEDS15489. [DOI] [PubMed] [Google Scholar]
- 66.Lethaus B., Safi Y., ter Laak-Poort M., Kloss-Brandstätter A., Banki F., Robbenmenke C., Steinseifer U., Kessler P. Cranioplasty with customized titanium and PEEK implants in a mechanical stress model. J Neurotrauma. 2012;29:1077–1083. doi: 10.1089/neu.2011.1794. [DOI] [PubMed] [Google Scholar]
- 67.Punchak M., Chung L. K., Lagman C., Bui T. T., Lazareff J., Rezzadeh K., Jarrahy R., Yang I. Outcomes following polyetheretherketone (PEEK) cranioplasty: systematic review and meta-analysis. J Clin Neurosci. 2017;41:30–35. doi: 10.1016/j.jocn.2017.03.028. [DOI] [PubMed] [Google Scholar]
- 68.Yen C. I., Chen R. F., Zelken J., Chang C. S., Yang S. Y., Chen H. C., Chang S. Y., Yang J. Y., Chuang S. S., Hsiao Y. C. The influence of paranasal augmentation on the measurement of the nose for the treatment of midfacial concavity. Aesthet Surg J. 2018;38:241–251. doi: 10.1093/asj/sjx166. [DOI] [PubMed] [Google Scholar]
- 69.de Moraes Ferreira A. C., Muãoz X. M., Okamoto R., Pellizer E. P., Garcia I. R., Jr Postoperative complications in craniomaxillofacial reconstruction with medpor. J Craniofac Surg. 2016;27:425–428. doi: 10.1097/SCS.0000000000002325. [DOI] [PubMed] [Google Scholar]
- 70.Kim J. H., Jung M. S., Lee B. H., Jeong H. S., Suh I. S., Ahn D. K. Silicone implant-based paranasal augmentation for mild midface concavity. Arch Craniofac Surg. 2016;17:20–24. doi: 10.7181/acfs.2016.17.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kang J., Zhang J., Zheng J., Wang L., Li D., Liu S. 3D-printed PEEK implant for mandibular defects repair - a new method. J Mech Behav Biomed Mater. 2021;116:104335. doi: 10.1016/j.jmbbm.2021.104335. [DOI] [PubMed] [Google Scholar]
- 72.Berthet J. P., Wihlm J. M., Canaud L., Joyeux F., Cosma C., Hireche K., Alric P., Marty-Ané C. H. The combination of polytetrafluoroethylene mesh and titanium rib implants: an innovative process for reconstructing large full thickness chest wall defects. Eur J Cardiothorac Surg. 2012;42:444–453. doi: 10.1093/ejcts/ezs028. [DOI] [PubMed] [Google Scholar]
- 73.Li D. C., Yang C. C., Kang J. F., Wang L., Huang L. J., Wang L., Cao Y., Shi C. Q., Lian Q. Precision design and control-performance manufacturing research of large-size individualized PEEK implants. Jixie Gongcheng Xuebao. 2018;54:121–125. [Google Scholar]
- 74.Zhang C., Wang L., Kang J., Fuentes O. M., Li D. Bionic design and verification of 3D printed PEEK costal cartilage prosthesis. J Mech Behav Biomed Mater. 2020;103:103561. doi: 10.1016/j.jmbbm.2019.103561. [DOI] [PubMed] [Google Scholar]
- 75.Capanna R., Totti F., Van der Geest I. C., Müller D. A. Scapular allograft reconstruction after total scapulectomy: surgical technique and functional results. J Shoulder Elbow Surg. 2015;24:e203–211. doi: 10.1016/j.jse.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 76.Wang B., Wu Q., Zhang Z., Liu J., Shao Z. Reconstruction with constrained scapular prosthesis after total scapulectomy for scapular malignant tumor. J Surg Oncol. 2018;118:177–183. doi: 10.1002/jso.25118. [DOI] [PubMed] [Google Scholar]
- 77.Lacroix D., Murphy L. A., Prendergast P. J. Three-dimensional finite element analysis of glenoid replacement prostheses: a comparison of keeled and pegged anchorage systems. J Biomech Eng. 2000;122:430–436. doi: 10.1115/1.1286318. [DOI] [PubMed] [Google Scholar]
- 78.Zheng J., Kang J., Sun C., Yang C., Wang L., Li D. Effects of printing path and material components on mechanical properties of 3D-printed polyether-ether-ketone/hydroxyapatite composites. J Mech Behav Biomed Mater. 2021;118:104475. doi: 10.1016/j.jmbbm.2021.104475. [DOI] [PubMed] [Google Scholar]
- 79.Liu D., Fu J., Fan H., Li D., Dong E., Xiao X., Wang L., Guo Z. Application of 3D-printed PEEK scapula prosthesis in the treatment of scapular benign fibrous histiocytoma: case report. J Bone Oncol. 2018;12:78–82. doi: 10.1016/j.jbo.2018.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Barik S., Jain A., Ahmad S., Singh V. Functional outcome in giant cell tumor of distal radius treated with excision and fibular arthroplasty: a case series. Eur J Orthop Surg Traumatol. 2020;30:1109–1117. doi: 10.1007/s00590-020-02679-2. [DOI] [PubMed] [Google Scholar]
- 81.Wiratnaya I. G. E., Budiartha I., Setiawan I., Sindhughosa D. A., Kawiyana I. K. S., Astawa P. Hernia mesh prevent dislocation after wide excision and reconstruction of giant cell tumor distal radius. World J Orthop. 2017;8:741–746. doi: 10.5312/wjo.v8.i9.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liu W., Wang B., Zhang S., Li Y., Hu B., Shao Z. Wrist reconstruction after en bloc resection of bone tumors of the distal radius. Orthop Surg. 2021;13:376–383. doi: 10.1111/os.12737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Saikia K. C., Borgohain M., Bhuyan S. K., Goswami S., Bora A., Ahmed F. Resection-reconstruction arthroplasty for giant cell tumor of distal radius. Indian J Orthop. 2010;44:327–332. doi: 10.4103/0019-5413.65134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lu M., Min L., Xiao C., Li Y., Luo Y., Zhou Y., Zhang W., Tu C. Uncemented three-dimensional-printed prosthetic replacement for giant cell tumor of distal radius: a new design of prosthesis and surgical techniques. Cancer Manag Res. 2018;10:265–277. doi: 10.2147/CMAR.S146434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Qassemyar Q., Assouly N., Madar Y., Temam S., Kolb F. Total nasal reconstruction with 3D custom made porous titanium prosthesis and free thoracodorsal artery perforator flap: A case report. Microsurgery. 2018;38:567–571. doi: 10.1002/micr.30302. [DOI] [PubMed] [Google Scholar]
- 86.Pang X., Wang L., Wang Z., Geng L. E. I., Li D., Jin Z., Liu C., Zhang C. Finite element analysis of total knee replacement with various misalignment angles in the sagittal plane. J Mech Med Biol. 2016;16:1650096. [Google Scholar]
- 87.Sevelda F., Schuh R., Hofstaetter J. G., Schinhan M., Windhager R., Funovics P. T. Total femur replacement after tumor resection: limb salvage usually achieved but complications and failures are common. Clin Orthop Relat Res. 2015;473:2079–2087. doi: 10.1007/s11999-015-4282-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ji Y., Wu Y., Li J. Use of three-dimensional-printed custom-made prosthesis to treat unicondylar femoral defect secondary to pathological fracture caused by giant cell tumor. J Int Med Res. 2021;49:3000605211025347. doi: 10.1177/03000605211025347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Park J. W., Kang H. G., Kim J. H., Kim H. S. 3D-printed connector for revision limb salvage surgery in long bones previously using customized implants. Metals. 2021;11:707. [Google Scholar]
- 90.Vaezi M., Yang S. Extrusion-based additive manufacturing of PEEK for biomedical applications. Virtual Phys Prototyp. 2015;10:123–135. [Google Scholar]
- 91.Zheng J., Zhao H., Dong E., Kang J., Liu C., Sun C., Li D., Wang L. Additively-manufactured PEEK/HA porous scaffolds with highly-controllable mechanical properties and excellent biocompatibility. Mater Sci Eng C Mater Biol Appl. 2021;128:112333. doi: 10.1016/j.msec.2021.112333. [DOI] [PubMed] [Google Scholar]
- 92.Guo C., Lu R., Wang X., Chen S. Antibacterial activity, bio-compatibility and osteogenic differentiation of graphene oxide coating on 3D-network poly-ether-ether-ketone for orthopaedic implants. J Mater Sci Mater Med. 2021;32:135. doi: 10.1007/s10856-021-06614-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lee J. H., Jang H. L., Lee K. M., Baek H. R., Jin K., Hong K. S., Noh J. H., Lee H. K. In vitro and in vivo evaluation of the bioactivity of hydroxyapatite-coated polyetheretherketone biocomposites created by cold spray technology. Acta Biomater. 2013;9:6177–6187. doi: 10.1016/j.actbio.2012.11.030. [DOI] [PubMed] [Google Scholar]
- 94.Gan K., Liu H., Jiang L., Liu X., Song X., Niu D., Chen T., Liu C. Bioactivity and antibacterial effect of nitrogen plasma immersion ion implantation on polyetheretherketone. Dent Mater. 2016;32:e263–e274. doi: 10.1016/j.dental.2016.08.215. [DOI] [PubMed] [Google Scholar]
- 95.Torstrick F. B., Lin A. S. P., Potter D., Safranski D. L., Sulchek T. A., Gall K., Guldberg R. E. Porous PEEK improves the bone-implant interface compared to plasma-sprayed titanium coating on PEEK. Biomaterials. 2018;185:106–116. doi: 10.1016/j.biomaterials.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 96.Zheng J., Dong E., Kang J., Sun C., Liu C., Wang L., Li D. Effects of raster angle and material components on mechanical properties of polyether-ether-ketone/calcium silicate scaffolds. Polymers. 2021;13:2547. doi: 10.3390/polym13152547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zheng J., Zhao H., Ouyang Z., Zhou X., Kang J., Yang C., Sun C., Xiong M., Fu M., Jin D., Wang L., Li D., Li Q. Additively-manufactured PEEK/HA porous scaffolds with excellent osteogenesis for bone tissue repairing. Compos B Eng. 2022;232:109508. [Google Scholar]
- 98.Deng Y., Zhou P., Liu X., Wang L., Xiong X., Tang Z., Wei J., Wei S. Preparation, characterization, cellular response and in vivo osseointegration of polyetheretherketone/nano-hydroxyapatite/carbon fiber ternary biocomposite. Colloids Surf B Biointerfaces. 2015;136:64–73. doi: 10.1016/j.colsurfb.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 99.Han X., Yang D., Yang C., Spintzyk S., Scheideler L., Li P., Li D., Geis-Gerstorfer J., Rupp F. Carbon fiber reinforced PEEK composites based on 3D-printing technology for orthopedic and dental applications. J Clin Med. 2019;8:240. doi: 10.3390/jcm8020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Evans N. T., Torstrick F. B., Lee C. S., Dupont K. M., Safranski D. L., Chang W. A., Macedo A. E., Lin A. S., Boothby J. M., Whittingslow D. C., Carson R. A., Guldberg R. E., Gall K. High-strength, surface-porous polyether-ether-ketone for load-bearing orthopedic implants. Acta Biomater. 2015;13:159–167. doi: 10.1016/j.actbio.2014.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Su Y., He J., Jiang N., Zhang H., Wang L., Liu X., Li D., Yin Z. Additively-manufactured poly-ether-ether-ketone (PEEK) lattice scaffolds with uniform microporous architectures for enhanced cellular response and soft tissue adhesion. Mater Des. 2020;191:108671. [Google Scholar]
- 102.Oladapo B. I., Zahedi S. A., Ismail S. O., Omigbodun F. T., Bowoto O. K., Olawumi M. A., Muhammad M. A. 3D printing of PEEK-cHAp scaffold for medical bone implant. Bio-des Manuf. 2021;4:44–59. [Google Scholar]
- 103.Nawaz A., Bano S., Yasir M., Wadood A., Ur Rehman M. A. Ag and Mn-doped mesoporous bioactive glass nanoparticles incorporated into the chitosan/gelatin coatings deposited on PEEK/bioactive glass layers for favorable osteogenic differentiation and antibacterial activity. Mater Adv. 2020;1:1273–1284. [Google Scholar]
- 104.Di Prima M., Coburn J., Hwang D., Kelly J., Khairuzzaman A., Ricles L. Additively manufactured medical products - the FDA perspective. 3D Print Med. 2016;2:1. doi: 10.1186/s41205-016-0005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jin Z., He C., Fu J., Han Q., He Y. Balancing the customization and standardization: exploration and layout surrounding the regulation of the growing field of 3D-printed medical devices in China. Biodes Manuf. 2022 doi: 10.1007/s42242-022-00187-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Min Y., Lan W., Liu B. Discussion on Administrative Innovation of Medical Device in China and U.S. Zhongguo Yi Liao Qi Xie Za Zhi. 2018;42:206–209. doi: 10.3969/j.issn.1671-7104.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 107.Morrison R. J., Kashlan K. N., Flanangan C. L., Wright J. K., Green G. E., Hollister S. J., Weatherwax K. J. Regulatory considerations in the design and manufacturing of implantable 3D-printed medical devices. Clin Transl Sci. 2015;8:594–600. doi: 10.1111/cts.12315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Monzón M. D., Ortega Z., Martínez A., Ortega F. Standardization in additive manufacturing: activities carried out by international organizations and projects. Int J Adv Manuf Technol. 2015;76:1111–1121. [Google Scholar]
- 109.Ding H. Y., Wu S. T., Yuan K., Shu C. P., Wang F., Chen C., Tang Y. B., Jiang Z. Y. Research progress of standards on additive manufacturing. Zhongguo Cailiao Jinzhan. 2020;39:955–961. [Google Scholar]
- 110.American National Standards Institute. ASTM F3333-20: Standard specification for chopped carbon fiber reinforced (CFR) polyetheretherketion (PEEK) polymers for surgical implant applications. 2020 [Google Scholar]
- 111.International Organization for Standardization. ISO 15309:2013: Implants for surgery — Differential scanning calorimetry of poly ether ether ketone (PEEK) polymers and compounds for use in implantable medical devices [Google Scholar]
- 112.Center for Medical Device Evaluation; National Medical Products Administration. The announcement of technical review guidance for registration of AM PEEK orthopaedic implant. [Accessed February 28 2022]. https://www.cmde.org.cn/CL0050/25174.html