Abstract
As science and technology have advanced, surgical techniques have become increasingly sophisticated. A revolution was triggered by the appearance of new electrical and optical instruments, shifting the field of surgery in the direction of “minimally invasive” and “noninvasive” procedures. Natural orifice specimen extraction surgery has emerged as a rising star in the field of minimally invasive surgery. It has increased rapidly, and it has become a hot topic in recent years. Natural orifice specimen extraction surgery has shown advantages in alleviating postoperative pain, improving bowel movements, providing a cosmetic effect, and improving psychological state without adversely affecting cancer outcomes. Different approaches have been classified and summarized for natural orifice specimen extraction surgery based on the procedure for specimen extraction and the location of the tumor, and natural orifice specimen extraction surgery can be used in resection all parts of the colorectum. The international natural orifice specimen extraction surgery consensus and monograph have also been published to improve the standardization of the application of this technique. Additional steps need to be taken to standardize natural orifice specimen extraction surgery, such as conducting large-scale randomized controlled trials, establishing a training system, and developing specific tools. Still, the natural orifice specimen extraction surgery procedure continues to follow the development of minimally invasive surgery and may be one of the future treatment options.
METHOD
Studies including clinical trial, meta-analysis, review, and consensus describing natural orifice specimen extraction were identified using Medline, Pubmed, and Embase. Two researchers independently screened titles and abstracts to select articles for full-text reading. The search strategy included the terms in combination: natural orifice specimen extraction AND colorectal cancer. The last search was run on June 1, 2022.
THE HISTORY AND DEVELOPMENT OF MINIMALLY INVASIVE COLORECTAL SURGERY
Open surgery was the predominant treatment method for colorectal cancer 100 years ago. Dr William Ernest Miles discovered the route of colorectal lymph node metastasis from his clinical practice and autopsy. In addition to developing abdominoperineal resection, he also laid the foundation for radical rectal resection. Several colorectal surgical procedures were developed afterward, including total mesorectal excision (TME) and complete mesocolic excision (CME). These achievements improved the prognosis of patients significantly. The term great incision was used to describe a highly skilled surgeon. There were, however, a number of complications following open surgery because of the enormous trauma involved, and postoperative recovery was difficult. Many other organs are also affected, negatively effecting on the patient's quality of life. A long incision may also result in unsatisfactory cosmetic outcomes, which may have an adverse psychological impact. In light of these adverse outcomes, surgeons began exploring minimally invasive techniques through radical resection and attempting to minimize surgical trauma. Surgery has moved from open procedures to minimally invasive surgery (MIS) to improve methodology and science.
The introduction of laparoscopic surgery was a landmark event in the history of surgery. Initially, it was used in simple procedures such as cholecystectomy and ovariectomy. Jacobs performed the first laparoscopic colonic resection in 1991, and this technique has quickly gained popularity treating colorectal cancer [1]. Following a decade of exploration, practice, and simplification, laparoscopic colectomy was superior to open surgery in terms of mortality, postoperative recovery, hospital stay, and cosmetic outcome, without the risk of compromising long-term cancer outcome [[2], [3], [4], [5]].
The invention of robotics was also a significant technological development for surgery. This procedure overcomes some of the limitations of laparoscopic surgery in treating colorectal cancer. With the introduction of three-dimensional vision, surgeons gained a distinct perception of the surgical field with the addition of depth perception. This technology has resolved the issues related to physiological tremors of surgeons and enabled them to perform surgery more dexterously with articulated instruments.
THE BOTTLENECK IN MINIMALLY INVASIVE COLORECTAL SURGERY
In MIS, the ultimate goal is to achieve the same therapeutic effects of standard surgical procedures but with the least amount of trauma to the patient. Unfortunately, neither laparoscopic nor robotic surgery avoids abdominal incisions. As a result of the incision used for the specimen removal, an increased risk of hernia, wound infection, postoperative pain, and psychological distress can be anticipated [[6], [7], [8], [9]]. Innovative techniques are necessary to treat colorectal cancer without an incision.
A SCARLESS TECHNIQUE—NATURAL ORIFICE SPECIMEN EXTRACTION SURGERY
Because of the success of intracorporeal anastomosis and changing methods of specimen extraction, surgery without abdominal incision has become feasible. As a rising star in MIS, natural orifice specimen extraction surgery (NOSES) has recently gained widespread attention. NOSES is defined as follows: surgical specimen resection is performed intra-abdominally, and then the specimen is extracted through an incision in a hollow organ communicating with the outside of the body, such as the anus, vagina, or mouth [10]. A major feature of NOSES in colorectal surgery is the reconstruction of the digestive tract intracorporeally as well as the removal of specimens through a natural orifice, eliminating the need to perform a mini-laparotomy.
-
1.
Oncological and bacteriological safety
Safety is usually the primary concern when it comes to a novel surgical procedure. Some literature has criticized the procedure of intracorporeal anastomosis and specimen extraction as possibly increasing the risk of intra-abdominal infection and tumor cell growth. Based on the international consensus on NOSES for colorectal cancer, it is recommended that an auxiliary tool be used, such as a wound protector or sterile specimen bag, to prevent direct contact between the specimen and the natural orifice to ensure an aseptic and tumor-free procedure [10]. Studies have been conducted on NOSES in recent years that have demonstrated that it is a safe technique in certain circumstances. A meta-analysis comparing short-term outcomes between NOSES and conventional laparoscopy in colorectal cancer found that NOSES had a lower incidence of postoperative complications than conventional laparoscopy [11]. According to another meta-analysis with 16 studies on long-term outcomes, NOSES achieved a similar oncological effect as conventional laparoscopy [12].
-
2.
Potential benefits
Compared with conventional laparoscopy, NOSES offers numerous advantages in minimizing postoperative complications without compromising oncological outcomes. Numerous studies have demonstrated that NOSES improves postoperative pain control. According to the single-blinded randomized clinical trial of Wolthuis et al, patients undergoing NOSES were less likely to require postoperative analgesia and experienced lower pain scores [15]. Furthermore, NOSES can significantly accelerate the recovery of bowel function and contribute to a shorter hospital stay [13,15,16]. Perhaps this is due to a decline in direct bowel manipulations and mesenteric traction levels. An accelerated bowel recovery contributes to a reduction in the length of hospital stay.
Furthermore, incision-related complications are virtually eliminated, and patients will be able to achieve a more pleasing cosmetic outcome without abdominal scarring. There is also the issue of psychological stress that cannot be ignored. NOSES was shown to be beneficial in terms of postoperative emotions in a large-scale survey conducted in China [17]. At present, people tend to concentrate on spiritual matters. The scar-free operation will ease the patients' anxiety and reduce their resistance to surgery. People may accept surgical treatment more readily when in a positive mood.
-
3.
Establishment of the theoretical system
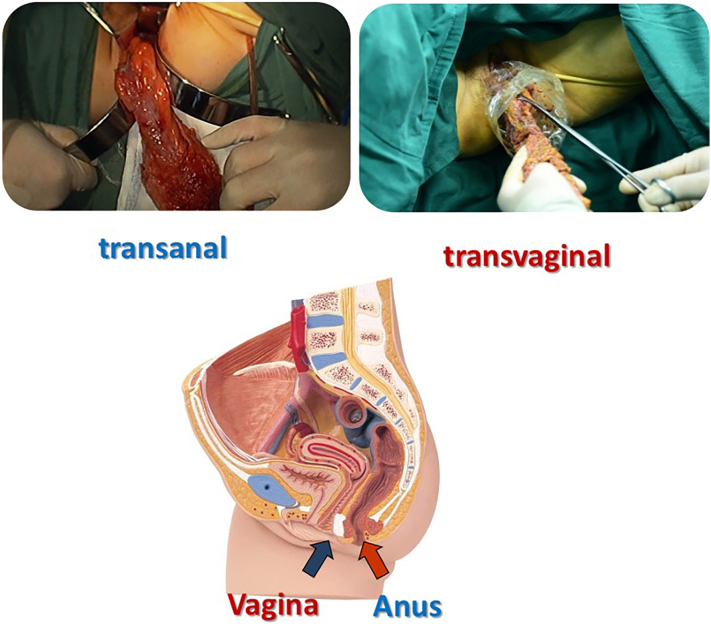
It has taken about 30 years for surgeons worldwide to gradually accept and begin to use this technique after Stewert et al first reported it in 1991 [18] (Fig 1). It has been well established that NOSES is a theoretical system in colorectal surgery [10,19]. As a function of the method of specimen collection in colorectal surgery, NOSES is categorized as either transanal extraction or transvaginal extraction (Fig 2). In terms of specimen extraction methods, NOSES can be classified into the following 3 types: (1) the transanal specimen eversion and extracorporeal resection technique (eversion–resection) (Fig 3), (2) the transluminal specimen extraction and extracorporeal resection technique (extraction–resection) (Fig 4), and (3) the intra-abdominal specimen resection and transluminal extraction technique (resection–extraction) (Fig 5). An additional classification was proposed that considers tumor location and the method of specimen extraction. There are 10 approaches in total: 5 for rectal resection and 5 for colectomy. Since these approaches have been developed and are being utilized clinically, NOSES is not restricted to a specific region and can be used in all segments of the colorectum.
-
4.
Present status
Fig 1.
Development history of NOSES.
Fig 2.
The specimen can be extracted through the anus or vagina in NOSES.
Fig 3.
When the tumor is located in the lower rectum, the proximal rectal resection is first performed, and the specimen is everted extracorporeally. The distal rectal resection is then performed under direct vision.
Fig 4.
When the tumor is located in the middle rectum, the distal end of the tumor is transected, and the specimen is extracted extracorporeally. The proximal rectal resection is then performed under direct vision.
Fig 5.
When the tumor is located in the upper rectum or colon, the specimen is resected intracorporeally and extracted through the natural orifice.
Many centers and surgeons have adopted this technique in recent years. A new alliance of NOSES members was set up in August 2018 in Beijing, China, to expand the influence of NOSES. This alliance is composed of more than 60 international members from 16 countries. All alliance members drafted the international NOSES consensus document. This guideline was published in February 2019 to standardize the implementation of NOSES in colorectal surgery [10]. Additionally, a multicenter NOSES data platform has been established in China. Seventy-nine centers with more than 5000 cases were included, and the data have been published recently [20,21].
FUTURE EXPECTATIONS FOR NOSES
NOSES is a category of MIS that has developed rapidly over the past several years. However, there is still much to be accomplished. The first objective would be to conduct evidence-based research. In spite of the large number of studies on NOSES, most were retrospective, and confounders and bias may have limited their conclusions. An RCT at a large scale is critical to establish the safety and benefits of NOSES further. We are about halfway through enrollment in a multicenter prospective randomized clinical trial (ChiCTR2000036314) of NOSES led by our center. In addition, a training system must be implemented. NOSES requires more technical expertise and a steeper learning curve than conventional laparoscopic surgery, particularly for aseptic, tumor-free procedures. It has been suggested that an effective surgical training system may speed up learning and improve safety during the early stages [22]. To standardize the application of NOSES, an international consensus has been recently published in the journal Gastroenterology Report, and the monograph of Natural Orifice Specimen Extraction Surgery-Colorectal Cancer has been released by Springer Publishing and People's Medical Publishing House (English Edition). This monograph focuses on NOSES main principles and technical aspects and has been translated into 6 languages. In addition, NOSES workshops, training courses, and live surgical demonstrations have been conducted. To help more surgeons worldwide gain a comprehensive grasp of the basics of this technique, some other forms of training, such as online education, still need to be explored. Finally, some NOSES-specific instruments are expected to be developed to facilitate easier operation.
Although no minimally invasive technique is perfect and impeccably designed at present, NOSES is in line with the recent trend of minimally invasive technology. Critically analyzing, rigorously refining, and further developing this minimally invasive technique with a scientific approach are crucial for the benefit of doctors and patients. In our opinion, the existing NOSES problems will be solved in the near future, and this technique will play an essential role in the development of minimally invasive colorectal surgery in the future.
Disclosures
Author Contribution
Conception and design: XSW, ZL, MGZ; (II) administrative support: XSW and ZL; (III) manuscript written: MGZ, ZL; (VII) manuscript revision: ZL, XSW.
Funding Source
This work is supported by the National Key R&D Program of China (2017YFC0908200), CAMS Initiative for Innovative Medicine (CAMS-I2M-001), Beijing Science and Technology Program (D17110002617004), and Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2021-RC310-009).
Ethics Approval
This study does not involve human participants.
Conflict of interest
No authors have conflicts of interest or financial ties to disclose.
Contributor Information
Mingguang Zhang, Email: zmgslimshady@163.com.
Zheng Liu, Email: Zheng.liu@cicams.ac.cn.
Xishan Wang, Email: wxshan_cams@163.com.
References
- 1.Jacobs M., Verdeja J.C., Goldstein H.S. Minimally invasive colon resection (laparoscopic colectomy) Surg Laparosc Endosc. 1991;1(3):144–150. [PubMed] [Google Scholar]
- 2.Lacy A.M., García-Valdecasas J.C., Delgado S., Castells A., Taurá P., Piqué J.M., et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359(9325):2224–2229. doi: 10.1016/S0140-6736(02)09290-5. [DOI] [PubMed] [Google Scholar]
- 3.Colon Cancer Laparoscopic or Open Resection Study Group, Buunen M., Veldkamp R., WCJ Hop, Kuhry E., Jeekel J., et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10(1):44–52. doi: 10.1016/S1470-2045(08)70310-3. [DOI] [PubMed] [Google Scholar]
- 4.Liang J.-T., Huang K.-C., Lai H.-S., Lee P.-H., Jeng Y.-M. Oncologic results of laparoscopic versus conventional open surgery for stage II or III leftsided colon cancers: a randomized controlled trial. Ann Surg Oncol. 2007;14(1):109–117. doi: 10.1245/s10434-006-9135-4. [DOI] [PubMed] [Google Scholar]
- 5.Fleshman J., Sargent D.J., Green E., Anvari M., Stryker S.J., Beart R.W., et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246(4):655–662. doi: 10.1097/SLA.0b013e318155a762. discussion662–4. [DOI] [PubMed] [Google Scholar]
- 6.Hackert T., Uhl W., Buchler M.W. Specimen retrieval in laparoscopic colon surgery. Dig Surg. 2002;19(6):502–506. doi: 10.1159/000067605. [DOI] [PubMed] [Google Scholar]
- 7.Kaminski J.P., Pai A., Ailabouni L., et al. Role of epidural and patientcontrolled analgesia in site-specific laparoscopic colorectal surgery. JSLS. 2014;18(4) doi: 10.4293/JSLS.2014.00207. e2014.00207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ihedioha U., Mackay G., Leung E., Molloy R.G., O’Dwyer P.J. Laparoscopic colorectal resection does not reduce incisional hernia rates when compared with open colorectal resection. Surg Endosc. 2008;22(3):689–692. doi: 10.1007/s00464-007-9462-y. [DOI] [PubMed] [Google Scholar]
- 9.Winslow E.R., Fleshman J.W., Birnbaum E.H., Brunt L.M. Wound complications of laparoscopic vs open colectomy. Surg Endosc. 2002;16(10):1420–1425. doi: 10.1007/s00464-002-8837-3. [DOI] [PubMed] [Google Scholar]
- 10.Guan X., Liu Z., Longo A., et al. International Alliance of NOSES. International consensus on natural orifice specimen extraction surgery (NOSES) for colorectal cancer. Gastroenterol Rep (Oxf) 2019;7(1):24–31. doi: 10.1093/gastro/goy055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou Z., Chen L., Liu J., Ji F., Shang Y., Yang X., et al. Laparoscopic natural orifice specimen extraction surgery versus conventional surgery in colorectal cancer: a meta-analysis of randomized controlled trials. Gastroenterol Res Pract. 2022;2022 doi: 10.1155/2022/6661651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang S., Tang J., Sun W., Yao H., Li Z. The natural orifice specimen extraction surgery compared with conventional laparoscopy for colorectal cancer: a meta-analysis of efficacy and long-term oncological outcomes. Int J Surg. 2022;97 doi: 10.1016/j.ijsu.2021.106196. [Epub 2021 Dec 16] [DOI] [PubMed] [Google Scholar]
- 13.Saurabh B., Chang S.C., Ke T.W., et al. Natural orifice specimen extraction with single stapling colorectal anastomosis for laparoscopic anterior resection: feasibility, outcomes, and technical considerations. Dis Colon Rectum. 2017;60(1):43–50. doi: 10.1097/DCR.0000000000000739. [DOI] [PubMed] [Google Scholar]
- 15.Zhang M, Hu X, Guan X, Zheng W, Liu Z, Jiang Z, et al. Surgical outcomes and sexual function after laparoscopic colon cancer surgery with transvaginal versus conventional specimen extraction: A retrospective propensity score matched cohort study. Int J Surg. 2022 Aug;104:106787. doi: 10.1016/j.ijsu.2022.106787. [DOI] [PubMed] [Google Scholar]
- 16.Xingmao Z., Haitao Z., Jianwei L., Huirong H., Junjie H., Zhixiang Z. Totally laparoscopic resection with natural orifice specimen extraction (NOSE) has more advantages comparing with laparoscopic-assisted resection for selected patients with sigmoid colon or rectal cancer. Int J Colorectal Dis. 2014;29(9):1119–1124. doi: 10.1007/s00384-014-1950-7. [DOI] [PubMed] [Google Scholar]
- 17.Guan X., Jiao S., Huang H.Y., et al. An investigation report on the current situation of natural orifice specimen extraction surgery in China [J/CD] Chin J Colorec Dis (Electronic Edition) 2021;10(2):122–131. [Google Scholar]
- 18.Stewert E.A., Liau A.S., Friedman A.J. Operative laparoscopy followed by colpotomy for resecting a colonic leiomyosarcoma: a case report. J Reprod Med. 1991;36(12):883–884. [PubMed] [Google Scholar]
- 19.Xishan W. Natural orifice specimen extraction surgery-colorectal cancer. In: Xishan W, Zheng L, Guiyu W (ed) Overview of NOSES, Volume 3, 2nd edn. Springer, Berlin, pp 5–10.
- 20.Guan X., Wang G.Y., Zhou Z.Q., et al. Retrospective study of 718 colorectal neoplasms treated by natural orifice specimen extraction surgery in 79 hospitals[J/CD] Chin J Colorec Dis (Electronic Edition) 2017;6(6):469–477. [Google Scholar]
- 21.Guan Xu, Xiyue Hu, Jiang Zheng, Wei Ye, Sun Donghui, Miao Wu, et al. Short-term and oncological outcomes of natural orifice specimen extraction surgery (NOSES) for colorectal cancer in China: a national database study of 5055 patients. Science Bulletin. 2022;67(13):1331–1334. doi: 10.1016/j.scib.2022.05.014. [DOI] [PubMed] [Google Scholar]
- 22.Chen G., Liu Z., Han P., Li J.W., Cui B.B. The learning curve for the laparoscopic approach for colorectal cancer: a single institution’s experience. J Laparoendosc Adv Surg Tech A. 2013;23(1):17–21. doi: 10.1089/lap.2011.0540. [DOI] [PubMed] [Google Scholar]