Abstract
Intensive care unit (ICU) patients with end-organ failure will require specialised machines or extracorporeal therapies to support the failing organs that would otherwise lead to death. ICU patients with severe acute kidney injury may require renal replacement therapy (RRT) to remove fluid and wastes from the body, and patients with severe cardiorespiratory failure will require extracorporeal membrane oxygenation (ECMO) to maintain adequate oxygen delivery whilst the underlying pathology is evaluated and managed. The presence of ECMO and RRT machines can further augment the existing pharmacokinetic (PK) alterations during critical illness. Significant changes in the apparent volume of distribution (Vd) and drug clearance (CL) for many important drugs have been reported during ECMO and RRT. Conventional antimicrobial dosing regimens rarely consider the impact of these changes and consequently, are unlikely to achieve effective antimicrobial exposures in critically ill patients receiving ECMO and/or RRT. Therefore, an in-depth understanding on potential PK changes during ECMO and/or RRT is required to inform antimicrobial dosing strategies in patients receiving ECMO and/or RRT. In this narrative review, we aim to discuss the potential impact of ECMO and RRT on the PK of antimicrobials and antimicrobial dosing requirements whilst receiving these extracorporeal therapies. The potential benefits of therapeutic drug monitoring (TDM) and dosing software to facilitate antimicrobial therapy for critically ill patients receiving ECMO and/or RRT are also reviewed and highlighted.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00134-022-06847-2.
Keywords: Antimicrobial, Dosing software, Extracorporeal membrane oxygenation, Pharmacokinetics, Renal replacement therapy, Therapeutic drug monitoring
Take-home message
| Extra-corporeal membrane oxygenation (ECMO) and renal replacement therapy (RRT) machines can further exacerbate existing pharmacokinetic alterations observed during critical illness complicating drug dosing, particularly for antimicrobials. Effective pharmacotherapy during ECMO and/or RRT can be achieved with the support of therapeutic drug monitoring and dosing software. |
Introduction
Critically ill patients with life-threatening conditions often require specialised machines or extracorporeal therapies as part of care provided in the intensive care unit (ICU). Such patients may develop end-organ damage (due to acute and/or chronic disease) or in extreme cases, multiple organ dysfunction syndrome [1]. This syndrome can include cardiorespiratory and/or renal dysfunction, which necessitates extracorporeal therapies to support the failing organs that would otherwise lead to death. ICU patients with severe acute kidney injury may require renal replacement therapy (RRT) to remove fluid and wastes from the body, and patients with severe cardiorespiratory failure will require extracorporeal membrane oxygenation (ECMO) to maintain adequate oxygen delivery whilst the underlying pathology is evaluated and managed. As ECMO and RRT do not resolve the underlying cause of organ failure by themselves, effective pharmacotherapy is crucial to reverse the cause of critical illness for such patients [2]. For example, in patients with sepsis or septic shock, both of which are common in ECMO and RRT patients in the ICU, therapeutic outcomes will heavily rely on whether effective antimicrobial therapy is delivered to these patients. However, antimicrobial dosing is challenging in these patients as both extracorporeal devices are hypothesised to further exacerbate existing physiological derangements during critical illness [2]. Conventional drug dosing which rarely considers these extreme homeostatic changes has a higher likelihood to fail in this patient population [3–5]. Aggressive antimicrobial dosing regimens (e.g. beta-lactam antimicrobials) appear to now be more common in many ICUs to account for this phenomenon leading to increasing reports of excessive drug exposure and toxicity in this patient population over the last 10 years [6]. Therefore, an in-depth understanding on potential pathophysiological and pharmacokinetic (PK) changes during ECMO and/or RRT is required to inform drug dosing strategies in critically ill patients receiving these extracorporeal machines/devices. Indeed, use of dosing software, an increasingly used technology, may facilitate optimised antimicrobial therapy.
We aim to review the potential impact of ECMO and RRT on the PK of antimicrobials and how these extracorporeal devices influence drug dosing requirements in critically ill adult patients receiving each. Although ECMO and RRT can influence the PK of many important drugs (e.g. sedatives and analgesics), this review will mostly focus on the PK, and dosing requirements of antimicrobials as instructive data are currently available for this drug class. We also highlight potential solutions to dosing challenges during ECMO and/or RRT in the form of individualised and optimised dosing strategies, supported by therapeutic drug monitoring (TDM) and dosing software.
Pharmacokinetic and pharmacodynamic issues in critically ill patients
Pharmacokinetic issues
Optimal pharmacotherapy is challenging in critically ill patients as they manifest extreme physiological derangements that are not commonly encountered in general ward environments [7]. These dosing challenges have been reviewed in detail previously [8–11]. Critical illness is typically characterised by marked pathophysiological changes that can be driven by both the natural underlying disease process (e.g. sepsis) and the medical interventions provided (e.g. aggressive intravenous fluid and vasoactive infusions). These patients may also have pre-existing chronic co-morbidities which can reduce their physiological reserves even further. Additionally, the presence of extracorporeal therapies/machines (e.g. ECMO and/or RRT) can further exacerbate the existing pathophysiological changes during critical illness [2, 12, 13]. The interplay of these factors may significantly alter drug PK in critically ill patients and can be broadly considered in terms of altered apparent volume of distribution (Vd) and drug clearance (CL). Significant Vd and CL alterations leading to altered drug exposures have been reported for many important drugs during ECMO and RRT [13–15]. Conventional dosing regimens rarely consider the impact of the altered PK phenomenon and consequently, are unlikely to achieve effective drug exposures in a considerable proportion of critically ill patients receiving ECMO and/or RRT [3–5, 16]. Importantly, sub-optimal drug dosing in this patient population may lead to therapeutic failure and/or drug toxicity [8].
Pharmacokinetic/pharmacodynamic issues
Effective use of some drugs during ECMO and/or RRT can be more challenging than for some other drugs. For example, although sedatives and vasoactive agents can be titrated to the desired pharmacological response, there are no reliable or timely clinical markers to guide antimicrobial therapy. However, each antimicrobial/antimicrobial class exhibits different pharmacokinetic/pharmacodynamic (PK/PD) indices that are associated with increased effectiveness [17], and achieving these concentration exposures increases the likelihood of therapeutic of response. Clear relationships have been described for most antimicrobials linking plasma PK/PD exposures with clinical efficacy [8, 18] and for some drugs, toxicity [8, 18]. Therefore, antimicrobial dosing that can achieve and maintain plasma antimicrobial concentrations within this therapeutic exposure range increases the likelihood of therapeutic clinical efficacy whilst limiting the probability of toxicity in patients receiving ECMO and/or RRT. However, most studies defining these therapeutic exposures are based on studies of plasma concentrations, and do not always reflect concentrations at the site of infection (e.g. epithelial lining fluid in pneumonia) which may be highly variable. Therefore, although these ranges provide strong guidance, pharmacokinetic outliers may not be represented by a plasma derived therapeutic range meaning that clinical judgement still needs to be provided. Further research is needed in this area and the application of TDM and dosing software are meant only to supplement, and not to supersede, clinical judgement during decision making.
Minimum inhibitory concentration considerations
As minimum inhibitory concentration (MIC) is an integral component of antimicrobial PK/PD, failure to consider both PK and MIC differences may lead to sub-optimal antimicrobial dosing and therapeutic failure. This is especially important when TDM is performed in “high-risk” patient populations (e.g. critically ill ECMO and/or RRT patients), which are more likely to be infected by pathogens with reduced antimicrobial susceptibility (i.e. higher MICs) when compared with any other population (e.g. patients in the general wards) [19]. Additionally, TDM- and software-guided dosing adjustments need to consider MIC variation, specifically in the context of MIC determination method (broth microdilution versus Etest®), assay variation, species identification and wild-type distributions [20]. Importantly, an individual MIC measurement should not be regarded as a “true” value but only an estimate of pathogen susceptibility.
Renal replacement therapy
Variability in RRT modalities and techniques
RRT is typically provided as continuous renal replacement therapy (CRRT) or as standard intermittent haemodialysis (IHD). Alternatives, such as slow extended haemodialysis (SLED), prolonged intermittent renal replacement therapy (PIRRT) or peritoneal dialysis (PD), are used less often [21].
CRRT remains dominant in Europe and most countries around the world [22]. However, with lower dialysate and blood flow rates compared to IHD, PIRRT is now used in some centres, especially in the subacute phase of illness [23]. Advantages of PIRRT include increased patient mobility, more opportunities for physical and occupational therapy as compared with CRRT and greater haemodynamic stability than IHD. Thus, the dichotomy of CRRT versus IHD is to some extent artificial. Modern CRRT machines can deliver therapy that resembles IHD, and IHD treatments can be slowed to deliver therapy over 10–12 h as SLED or PIRRT. Therefore, CRRT and standard IHD represent extremes of a continuum with associated variable effects on drug removal and dosing requirements.
The two main mechanisms of solute and drug removal are diffusion and convection, whereas ultrafiltration is utilised for fluid removal. Diffusion is the movement of solutes across the membrane across a concentration gradient and is the main mechanism of removal for small molecules in dialysis. Convection is the movement of solutes across the membrane along with water as pressure is applied (known as “solvent drag”) and is the main mechanism of removal for small and middle molecules in hemofiltration. Conventional IHD, continuous veno-venous haemodialysis (CVVHD), and SLED primarily utilise diffusion, whereas continuous veno-venous haemofiltration (CVVH) primarily utilises convection. Finally, continuous veno-venous haemodiafiltration (CVVHDF) utilises both mechanisms [24].
All RRT modalities have specific advantages and disadvantages, and Supplementary Table 1 lists the major advantages and disadvantages of CRRT, IHD, PIRRT and PD when used in patients with AKI. In most cases, the choice of RRT is guided by the clinical condition of the patient and availability of devices, kits, and expertise. To date, there is no robust evidence that either modality is superior in terms of survival or renal recovery. However, individual patients may benefit more from one technique than other techniques at different phases of critical illness. Thus, the decision of which modality to use, both between individual patients and within the same patient over time, may vary during the course of a patient’s illness.
Effect of RRT settings on antimicrobial drug PK
RRT support may increase drug CL, affect drug dosing, and contribute to clinical failure and/or the development of resistance in the case of antimicrobials [25]. Clinicians must ensure that the appropriate drug is selected, and adequate dose is delivered whilst accounting for RRT CL and the altered PK in critical illness. As there are different modalities of RRT, there is not one single approach to optimising antimicrobial drug dosing.
Different factors affect antimicrobial PK in patients receiving RRT and these relationships are summarised in Table 1. They are the main determinants of antimicrobial dose adjustments. Factors related to RRT system properties are key. They first include the RRT modality factor. For example, CRRT provides constant drug CL whilst PIRRT and IHD present two distinct PK phases characterised by inter and intra-dialytic elimination that may require different dosing adjustments. Comparing equal effluent doses in CRRT, techniques combining convection and diffusion (CVVHDF) may provide higher drug CL for beta-lactam antimicrobials and linezolid [26, 27].
Table 1.
Relevant factors that can influence antimicrobial pharmacokinetics in patients receiving renal replacement therapy
| Patient-specific factors | |
| Critical illness | Vd ↑ |
| CL ↑ or ↓ based on renal function or RRT settings | |
| Residual renal function | CL ↑ compared to anuric patients |
| Hypoalbuminemia | Free drug concentrations ↑ |
| CL ↑ for highly protein bound drugs | |
| Vd ↑ | |
| Drug-specific factors | |
| Solubility | Hydrophilic drugs more likely to be affected by RRT-related CL |
| Lipophilic drugs potentially affected by membrane adsorption | |
| Molecular weight | CL ↑ for low molecular weight drugs |
| This may not be a major determinant of drug removal due to the use of high flux hemofilters with large pore size | |
| Protein binding | CL ↑ for low protein bound drugs |
| Electric charge | CL ↑ for anionic antibiotics (e.g. cefotaxime and ceftazidime) compared to cationic antibiotics (e.g. aminoglycosides) retained in plasma by negatively charged molecules like albumin (Gibbs–Donnan effect) |
| PK/PD target | RRT-related CL influences maintenance dose for time-dependent antibiotics (e.g. 100%fT>1–4 × MIC) |
| RRT-related CL influences dosing frequency for concentration-dependent antibiotics (Cmax/MIC) | |
| RRT-related CL influences maintenance dose and/or dosing frequency for time- and concentration-dependent antibiotics (AUC/MIC) | |
| RRT-specific factors | |
| RRT modality: Continuous versus Intermittent | Variable elimination rates depending on intra and inter-dialytic phases for IHD |
| Relatively constant drug CL depending on RRT intensity for CRRT | |
| RRT technique: Convective versus Diffusive | Higher CL of high molecular weight drugs with convection technique |
| Combining convection and diffusion (i.e. CVVHDF) often results in greater drug CL than by convection or diffusion alone at equal RRT doses | |
| Effluent flow rate | Higher CRRT effluent rates resulting in higher CL |
| Blood flow rate | CL ↑ with high blood flow rate |
| Negligible clinical impact for CRRT | |
| Dilution mode | CL ↓ in pre-dilution mode |
| Negligible clinical impact | |
| Membrane type/adsorption | Polyacrylonitrile membranes more likely to be associated with drug adsorption (e.g. amikacin, levofloxacin, echinocandins in particular) |
| Saturable effect | |
| Hemofilter life span | CL ↓ over time unless circuit components are replaced regularly |
| Down time | CL ↓ if prolonged circuit downtime |
AUC area under the concentration–time curve, CL clearance, Cmax maximal drug concentration during a dosing interval, CRRT continuous renal replacement therapy, CVVHDF continuous veno-venous hemodiafiltration, IHD intermittent hemodialysis, MIC minimum inhibitory concentration, RRT renal replacement therapy, PK/PD pharmacokinetic/pharmacodynamics, Vd volume of distribution
Another RRT system factor is the effluent flow rate factor. Drug removal is strongly influenced by dialysate and ultrafiltration flow rates [28]. Thus, higher RRT effluent flow rates lead to greater drug CL requiring higher antimicrobial doses to achieve the same plasma concentrations as with lower flow rates. Additionally, high ultrafiltration rates may result in greater removal of larger molecular weight drugs such as vancomycin.
Finally, residual renal function may significantly affect antimicrobial drug dosing. Patients with residual renal function have been shown to require increased dosing/dosing frequency of linezolid and meropenem when compared with anuric patients [29, 30].
Pharmacological considerations for antimicrobials are also important. Altered protein binding may be associated with drug CL changes because only the unbound fraction can be cleared across the hemofilter. During critical illness, albumin and α1-acid glycoprotein concentrations can be altered impacting the PK of acidic and basic drugs, respectively. Typically, high protein-bound antimicrobials (e.g. cefazolin, ceftriaxone, and teicoplanin) are not significantly affected by RRT. However, wide variations in protein binding occur in critically ill patients, especially in the case of hypoalbuminemia, which has been commonly reported and studied thus far [7]. This can increase RRT-related CL and affect antibiotic exposure. The extent to which a drug is removed by dialysis is strongly influenced by the physicochemical properties of the drug and the apparent Vd [13]. In general, lipophilic drugs, such as macrolides, quinolones, and echinocandins, which exhibit large apparent Vd are less affected by RRT compared to hydrophilic drugs, such as beta-lactam antimicrobials and aminoglycosides, because a low proportion of the drug is present in the bloodstream from where clearance occurs. However, for echinocandins, significant adsorption could occur with highly adsorptive membranes (e.g. AN69 surface-treated and poly-methyl-methacrylate filters) and deserve further investigations to determine optimal dosing in CRRT patients.
Drug dosing for critically ill patients receiving RRT remains challenging. Thus, a rational approach to antibiotic dosing during RRT in ICU patients consists of high loading doses to avoid low concentrations associated with increased apparent Vd, adjustments of first maintenance dose based on the effluent flow rate (Table 2), and subsequent adjustment as guided by TDM and Bayesian dosing software. Additionally, the site of infection and minimum inhibitory concentration (MIC) of causative pathogens should be considered whilst choosing the optimal antimicrobial dosing regimen for patients on RRT.
Table 2.
Example doses of antimicrobial drugs according to renal replacement therapy modality
| Free fraction (%) | CVVH | CVVHDF | CVVHD | PIRRT | ||||
|---|---|---|---|---|---|---|---|---|
| Ultrafiltration rate 20–25 mL/kg/h |
Ultrafiltration rate 35 mL/kg/h |
Effluent flow rate 20–25 mL/kg/h |
Effluent flow rate 35 mL/kg/h |
Dialysate flow rate 20–25 mL/kg/h |
Dialysate flow rate 35 mL/kg/h |
|||
| Beta-lactam antimicrobials | ||||||||
| Amoxicillin/Clavulanate | 80 | ND | ND | ND | ND | |||
| Cefazolin | 15–20 | 2 g q12h | ND | ND | ND | |||
| Cefepime | 80 | LD: 2 g | LD: 2 g | LD: 2 g | ND | 1.75 g q8h | 2 g q8h | LD: 2 g |
| MD:1.5 g q8h | MD: 1.75 g q 8 h | MD: 1.75 g q8h | MD: 1 g q6h | |||||
| Cefiderocol | 40 | 1.5 g q8–12 h | 1.5 g q8–12 ha | 1.5 g q8–12 ha | ND | |||
| Cefotaxime | 60–80 |
LD: 2 g MD: CI 4 g q24h |
ND | ND | ND | |||
| Ceftaroline | 80 | 0.6 g q12h | ND | ND | ND | |||
| Ceftazidime | 90 | ND |
LD: 2 g MD: CI 4 g/24 h |
ND | 2 g q12h | |||
| Ceftazidime/Avibactam | 90 | ND | 2.5 g q8h | ND | ND | |||
| Ceftolozane/Tazobactam | 80 | 1.5–3 g q8hb | ND | 1.5–3 g q8hb | 3 g q8h | 1.5–3 g q8hb | ND | |
| Ceftriaxone | 10 | 2 g q24h or 1 g q12h | 2 g q24h | 2 g q24h | 2 g q24h | |||
| Imipenem | 80 | ND | 0.5 g q8h | 1 g q8h | ND | 0.5 g q6h | ||
| Meropenem | 100 |
LD: 1 g MD:0.75 g q8h |
LD: 1 g MD:1 g q8h |
LD: 1 g MD: 1 g q12h |
LD: 1 g MD: 0.75 g q8h |
LD: 1 g MD: 1 g q8h |
1 g q12h | |
| Oxacillin | 10 | No adjustment | No adjustment | No adjustment | No adjustment | |||
| Piperacillin/Tazobactam | 70/80 |
LD: 4 g MD: CI 12 g q24h |
LD: 4 g MD: CI 12 g q24h |
LD: 4 g MD: CI 16 g q24h |
4 g q8h or 4 g q12h following 2 g replacement dose post PIRRT | |||
| Aztreonam | 45 | 1 g q8h | ND | 2 g q8h | ND | |||
| Aminoglycosides | ||||||||
| Amikacin | > 95 | 25 mg/kg ABW q48h | 25 mg/kg ABW | 25 mg/kg ABW | ND | |||
| Gentamicin | > 95 | 8 mg/kg ABW | 8 mg/kg ABW | 8 mg/kg ABW | 6–8 mg/kg ABW 1 h before PIRRT session | |||
| Tobramycin | 90–100 | 8 mg/kg ABW | 8 mg/kg ABW | 8 mg/kg ABW | 6–8 mg/kg ABW 1 h before PIRRT session | |||
| Glycopeptides | ||||||||
| Vancomycin | 50 | ND |
LD: 30 mg/kg MD: 10 mg/kg q24h |
ND | 20–25 mg/kg followed by TDM | |||
| Teicoplanin | 10–40 |
LD: 1200 mg MD: 600–1800 mg |
ND | ND | ND | |||
| Oxazolidinones | ||||||||
| Linezolid | 70 | No adjustment | No adjustment | No adjustment | No adjustment | |||
| Tedizolid | 10–30 | No adjustment | No adjustment | No adjustment | No adjustment | |||
| Fluoroquinolones | ||||||||
| Ciprofloxacin | 60–80 | 400 mg q8h | 400 mg q8h | 200 mg q8h | ND | |||
| Levofloxacin | 60–75 | 250 mg/24 h | 500 mg/24 h | ND | Consider alternative | 250 mg q24h | ||
| Other classes | ||||||||
| Tigecycline | 10–30 | No adjustment | No adjustment | No adjustment | No adjustment | |||
| Colistin | 60–75 | LD: 9 MUI |
LD: 6–9 MUI MD: 1.5–2 MUI q8h |
6 MUI q12h | 3 MUI q8h | |||
|
MD: 3 MUI q8h |
MD: 4.5 MUI q8h |
|||||||
| TMP-SMX | 5 mg/kg q12h | ND | 5 mg/kg q12h | 15 mg/kg/24 h in 4 divided doses | ||||
| Daptomycin | 20 | ND | 6–8 mg/kg q24h | 6–8 mg/kg q24h | 6 mg/kg q24h | |||
| Antifungal Drugs | ||||||||
| Fluconazole | 90 | ND |
LD: 800 mg MD: 400 mg q12h |
ND | 400 mg q12h | |||
| Voriconazole | 40 | 4 mg/kg q12h | 4 mg/kg q12h | 4 mg/kg q12h | ND | |||
| Preferable oral route | Preferable oral route | Preferable oral route | ||||||
| Isavuconazole | < 1 | No adjustment | No adjustment | No adjustment | No adjustment | |||
| Caspofungin | 3 | No adjustment | No adjustment | No adjustment | No adjustment | |||
| Micafungin | < 1 | No adjustment | No adjustment | No adjustment | No adjustment | |||
| Amphotericin B | 10 | No adjustment | No adjustment | No adjustment | No adjustment | |||
| Antiviral drugs | ||||||||
| Acyclovir | 70–90 | 5–7.5 mg/kg q24h | 5–7.5 mg/kg q24h | 5–7.5 mg/kg q24h | ND | |||
| Ganciclovir | 98 | ND | ND | 5 mg/kg q48h | ND | |||
| Oseltamivir | 97 | ND | 75 mg q12h | ND | ND | |||
ABW adjusted body weight; CVVH continuous veno-venous hemofiltration, CVVHDF continuous veno-venous hemodiafiltration, ND no data, LD loading dose, MD maintenance dose, PIRRT prolonged intermittent renal replacement therapy, TMP-SMX trimethoprim-sulfamethoxazole
As a general rule, the “loading dose” of a drug, is strictly dependent on Vd and does not require any adjustment in patients with renal failure, including those undergoing RRT for AKI. RRT intensity may influence maintenance doses as reported in Table 1 and suggestions were derived from the references listed in the Supplementary Materials and from the main guidelines for antimicrobial therapy during RRT
aExtrapolated from cefepime data
bConsider higher dosing regimens for deep seated infections or less susceptible isolates
Exposure and outcomes
A key question in antimicrobial drug dosing during RRT is whether a systematic approach leads to superior antimicrobial drug concentrations compared to clinical judgement. Such a systematic approach could be based on TDM, software-based PK calculations, or the administration via continuous infusion of those antimicrobial drugs for which bactericidal activity is dependent on the time above the minimal inhibitory concentration [4, 31–33]. The logic behind such methods is that the reality of critical illness and RRT is complex. Both, interventions and illness can change the apparent Vd. Similarly, events related to RRT (circuit clotting, progressive loss of functional membrane performance, cessation of therapy due to investigations, downtime due to circuit alarms) impact drug CL [8]. Thus, across ICUs worldwide, as demonstrated by the SMARRT study, there is extreme variability in antimicrobial drug dosing and concentrations leading to variable clinical outcomes [4]. Cumulatively, these data support a careful personalised approach to dosing accounting for the drug, patient's underlying organ function, type of RRT used and the duration of RRT.
Extracorporeal membrane oxygenation
ECMO is an advanced life support system which allows for prolonged cardiopulmonary support in patients with life-threatening respiratory or cardiac failure [34, 35]. ECMO does not provide treatment of the underlying illness, it is purely a supportive strategy that is implemented whilst underlying co-morbidities such as infection are treated.
Pharmacokinetic determinants during ECMO
In general, the ECMO circuit consists of a centrifugal blood pump, an oxygenator, heat exchanger and tubing. The ECMO circuit is primed with combination of crystalloid, albumin, and blood. Essentially, the addition of an ECMO circuit may further alter the PK in a critically ill patient in three ways: (1) sequestration of the drug by the ECMO circuit; (2) increasing the apparent Vd; and (3) altered drug CL due to alteration in renal and liver blood flow, and altered plasma protein binding [36, 37]. The combined impact of ECMO- and critical illness-related factors on drug PK are summarised in Table 3. Importantly, drug dosing that does not consider these PK changes can lead to either therapeutic failure or toxicity.
Table 3.
The interrelationship of lipophilicity, hydrophilicity and protein binding and the impact of critical illness, extracorporeal membrane oxygenation (ECMO) and renal replacement therapy (RRT) on drug pharmacokinetics
| Lipophilic | Hydrophilic | Protein bound (PB) | |
|---|---|---|---|
| General pharmacokinetics | High Vd & hepatic CL | Low Vd & renal CL | Low Vd & hepatic or renal CL |
| Critical illness | Vd unchanged | ↑ Vd | Vd & CL—as per lipophilicity or hydrophilicity and plasma protein |
| CL ↑or↓ based on hepatic function | CL ↑ or ↓based on renal function | ||
| ECMO | ↑ Vd | Low or slightly ↑ Vd | ↑ or low Vd for lipophilicity + PB drugs |
| CL ↑or↓ based on hepatic function | CL ↑ or ↓based on renal function | CL ↓or ↑ based on renal or hepatic function | |
| RRT | ↓CL as high Vd | ↓CL as low Vd | ↓ CL—if less free drug |
| Critical illness + ECMO + RRT | ↑↑Vd & ↓↓CL | ↑Vd & ↓ CL | ↑Vd & CL ↓↑ based on renal or hepatic function |
| ↓↓CL CRRT as ↑↑ Vd | ↓CL CRRT as ↑Vd | ||
| Hepatic dysfunction can ↓ CL | ↓ CL if renal function ↓ | ||
| Examples | Fluoroquinolones | Aminoglycosides beta-lactams | Ceftriaxone |
| Lincosamides | Colistin | ||
| Macrolides | Glycopeptides | Clindamycin | |
| Tigecycline | Linezolid |
ECMO extracorporeal membrane oxygenation, CL drug clearance, PB protein binding, CRRT continuous renal replacement therapy, RRT renal replacement therapy, Vd apparent volume of distribution
Drug sequestration
Some drugs are sequestered onto the ECMO circuit which has a very large surface area due to its oxygenator and tubing; the degree of loss is influenced by both the drug physicochemical properties and circuit factors [37–41]. This sequestration is likely a result of non-specific binding of the drug onto the circuit components, with the degree of sequestration influenced by the surface area and the drugs affinity to it. This effect may decrease over time as the binding sites become saturated, so dosing should be regularly reviewed to avoid drug accumulation and toxicity [42]. However, the concept of reversible binding and saturation is still not understood.
In vitro or ex vivo experiments can help evaluate the extent of drug sequestration by the ECMO circuitry and have demonstrated that lipophilic drugs and those highly protein bound are sequestered to a greater degree [40, 41]. An ex vivo study investigated the influence of plasma protein binding on sequestration in the ECMO circuit and concluded that for drugs with similar lipophilicity, the extent of protein binding may determine the degree of circuit loss and vice versa [41]. The same drug can be sequestered to a different extent depending on the oxygenator used, the type of tubing [39, 43], the pump [37], the age of the circuit [44], and the priming solution used [45].
Modern circuits have evolved to decrease the risks from ECMO and drug disposition. These developments include the use of hollow-fibre membrane oxygenators (replacing earlier silicone rubber membrane), centrifugal pumps (replacing roller-head) and integrating the heat exchanger. Although pre-coated polyvinyl chloride tubing are now widely used, it is not clear whether their use significantly decrease the absorption of drugs [43].
Extrapolating from some of the earlier ex vivo studies is challenging as they differ in circuit materials used compared with the improved ECMO technology in the modern era [46]. Hence, ongoing study of drug–ECMO circuit interactions for new machines and consumables remains important.
Increased apparent Vd
The physiological changes associated with critical illness, such as systemic inflammatory response syndrome (SIRS), fluid shifts, altered blood pH and organ dysfunction, are common in this patient group and result in increased apparent Vd of hydrophilic drugs. The addition of an ECMO circuit may further increase apparent Vd by drug sequestration and hemodilution from the priming solution. Drugs with a large apparent Vd (e.g. ciprofloxacin) would be less effected by haemodilution than those with low Vd (e.g. beta-lactam antimicrobials). The significance of haemodilution is more pronounced in neonates and infants, than in older children and adults as this represents a greater proportion of their circulating blood volume.
Altered drug CL
Drug CL in general is decreased in ECMO, likely due to of reduced renal and hepatic perfusion and hypoxia; in addition, the SIRS response seen in patients on ECMO decreases the expression and function of drug-metabolising enzymes [1, 47].
Pharmacokinetic changes during combined ECMO and RRT support
Almost 50% of patients on ECMO require RRT [48], the indications of which are multifactorial similar to other critically ill patients. RRT whilst on ECMO adds increasing complexity to the PK of drugs because the presence of two extracorporeal circuits can make the estimation of PK parameters more difficult [2]. The effects may cancel each other and are dependent on the physicochemical properties of the drug, in particular its lipophilicity and protein binding. The most common RRT used in combination with ECMO is CRRT, and the resultant PK changes are not a simple sum of both independent changes and requires further studies. The potential PK alterations of common antimicrobials during ECMO are summarised in Table 4.
Table 4.
Potential pharmacokinetic changes in adult critically patients on extracorporeal membrane oxygenation (ECMO) for commonly used antimicrobials
| Drug | Log P | Protein binding (%) | Volume of distribution | Expected ECMO sequestration effect | General dosing guidance |
|---|---|---|---|---|---|
| Antimicrobials | |||||
| Meropenem | − 0.69 | 2 | 0.25 L/kg |
Minimal circuit loss Vd: increased |
Dosing similar to critically ill not on ECMO TDM-guided dosing |
| Piperacillin/tazobactam | 0.67 | 30 | 0.243 L/kg |
Minimal circuit loss Vd: increased |
Dosing similar to critically ill not on ECMO TDM-guided dosing |
| Vancomycin | − 4.4 | 50 | 0.4–1 L/kg |
Minimal circuit loss Vd: increased |
Dosing similar to critically ill not on ECMO TDM-guided dosing |
| Aminoglycosides: gentamicin, tobramycin, amikacin | < 0 | < 30 | 0.2–0.3 L/kg |
Minimal circuit loss Vd: increased CL: decreased |
Insufficient data TDM-guided dosing |
| Antifungals | |||||
| Fluconazole | 0.56 | 12 | Approx. to total body water |
Minimal circuit loss Vd: increased |
Insufficient adult data May require increased LD |
| Voriconazole | 2.56 | 58 | 4.6 L/kg | Moderate to significant circuit loss |
Conflicting data Dosing similar to critically ill not on ECMO TDM-guided dosing |
| Caspofungin | − 2.8 | 97 | NA |
Moderate circuit loss Vd: increased |
Insufficient and conflicting data |
ECMO extracorporeal membrane oxygenation, CL drug clearance, LD loading dose, NA not available, Vd volume of distribution
Clinical studies and future directions
There are several clinical PK studies in patients with ECMO; the majority were performed in neonates and children showed significant changes in the PK of antimicrobials [49–52]. These results cannot be confidently extrapolated to adults due to significant body composition differences and the physiological processes that affect absorption, distribution, metabolism, and excretion are not fully developed and are thus different to those in adults.
The absence of real-time measurable PD endpoints for infection as well as the importance of optimised therapy has meant recent adult ECMO PK studies have focussed on this class of drugs (Table 4) [53–63]. A recent comprehensive review of clinical PK studies of antimicrobial dosing in ECMO concluded that most PK changes are more reflective of critical illness rather than the ECMO device [14].
An integrated approach combining the mechanistic ex vivo experiments together with clinical PK studies is necessary to provide evidence-based dosing guidance. Examples include the ECMO PK project, an incremental research approach to integrate ex vivo experiments, PK studies in ovine models and a clinical PK study (ASAP ECMO study) [36, 41, 56, 57, 59, 60, 64–68]. Others incorporate the sequestration impact from the ex vivo ECMO experiments with physiologically-based pharmacokinetics (PBPK) modelling [38, 49].
Practical dosing recommendations
Currently, there are a lack of robust guidelines for dosing of drugs in critically ill adult patients receiving ECMO. The physicochemical properties of drugs can be used to predict PK changes and determine loading dose adjustments and subsequent maintenance dosing in this patient group [36, 41, 66, 69] (Table 3). Drugs with high protein binding (e.g., > 70%) and highly lipophilic (e.g. Log P > 2) are likely to be sequestered on the circuit and may require an increase in their dose, or frequency of administration [15]. As the PK changes of increased apparent Vd and altered CL may both be seen concurrently in critical illness, the use of dosing strategies derived from critically ill adult patients not on ECMO is acceptable for empiric dosing of most other drugs [56, 57, 59, 60, 64].
Dosing software
Acute pathophysiological changes that occur during critical illness including when receiving life-saving RRT and ECMO machines are used, can lead to difficult-to-predict antimicrobial concentrations in plasma and other body compartments, including at the site of infection. Furthermore, lower pathogen susceptibility observed in the ICU means that there may be PK/PD considerations that also need to be taken into account when seeking to achieve adequate antimicrobial exposure in these patients [70].
In the light of these challenges, dose optimisation strategies may play a key role to improve PK/PD target attainment. TDM is one such strategy that has traditionally been used to minimise the risk of exposure-related toxicity, particularly in antimicrobials with a narrow therapeutic index, such as the aminoglycosides and glycopeptides. With growing evidence linking sub-therapeutic antimicrobial concentrations with treatment failure [16, 71, 72], the role of TDM has now expanded to ensure therapeutic effectiveness is maximised [73, 74].
When TDM is performed, biological samples (usually plasma) are transported to an analysis laboratory with a turnaround time of approximately 30-min to 48 h, depending on the drug and availability of assay. Given the importance of prompt effective antimicrobial therapy in sepsis management [75, 76], a reduction in this turnaround time so that corresponding antimicrobial dose adjustments could be initiated in a timely manner would potentially be of great benefit. Another limitation of current TDM practices revolves around the minimal set of antimicrobial assays currently available in most laboratories that service healthcare facilities. Given the above challenges, there is a real need to develop innovative technologies that overcome the current shortcomings of conventional TDM processes. In this vein, development of real-time TDM sensor monitoring appears to be a promising tool, with biosensor research attracting enormous interest within healthcare services [77]. Basic requirements for this technological innovation include: (1) transduction, including target identification in human matrices; (2) continuous sample collection e.g. through the use of interstitial fluid sampling techniques, such as microneedle biosensors; and (3) real-time signal processing of assay results [78].
Several biosensor techniques are presently being tested, such as aptamer-based electrochemical and electronic sensors. One of these technologies is derived from particle mobility, based on a so-called ‘competition assay’ [79]. The assay detects a binding event by a sudden decrease in particle mobility due to interactions between a particle and a sensor surface. Because these are mediated by weak biological interactions, they are reversible and can be monitored continuously. The transitions between these unbound and bound states are recorded over time for many hundreds of particles simultaneously by bright field optical microscopy, enabling the accurate determination of concentrations [79]. Key parameters to improve biosensor robustness include selectivity, sensitivity, reproducibility, reusability and long-term stability. There also needs to be a focus on validating the new technology against the golden standard of mass spectrometry. Attention to data confidentiality is an important consideration given the vast amount of data captured, processed, and managed during clinical use. Artificial intelligence (AI) may be able to facilitate data analysis and exposure prediction, so may play a significant future role in implementation of real-time biosensors [80].
The ability of computers to perform complex mathematical modelling and statistical analysis has allowed for published antimicrobial population PK models to be integrated with relevant patient-specific data, such as renal function, weight and TDM sample measurements (if using Bayesian forecasting). Termed model-informed precision dosing (MIPD), these types of software can generate a priori dosing recommendations required for initiation of empiric-based therapy. If using a Bayesian component, these software may also provide a posteriori PK parameter estimates that potentially improve future dosing recommendation accuracy. Additionally, some MIPD software have the ability to input pathogen MIC so that variations in pathogen susceptibility can be accounted for.
One issue of particular relevance to the ECMO and RRT population sub-groups of critically ill patients is the generalisability of existing PK models available in MIPD software. As many of these published models have been developed within specific patient populations, caution must be applied when extrapolating MIPD dosing recommendations to other critically ill sub-groups with external validation strongly suggested.
Use of MIPD software may result in dosing recommendations that are more likely to achieve PK/PD targets [81]; however, the clinical outcome benefits of these software applications are yet to be quantified in critically ill patients with sepsis. Future studies will firstly need to examine comparative predictive accuracy of dosing recommendations before second, the design of the most sensitive interventions from clinical advantages (if any) of MIPD can occur.
When a patient is connected to an extracorporeal circuit/machine, the implementation of real-time TDM biosensors informing MIPD software will have several advantages. Firstly, all circuits are dynamic processes, and real-time monitoring will make it possible to react to the dynamics of the systems as soon as possible. This is of paramount importance as interruptions and/or fluctuations in extracorporeal treatment modalities are very common during clinical care of patients. Secondly, the information collected via the sensor will allow for the MIPD tool to efficiently optimise antimicrobial dosing. For example, a severe acute kidney injury patient commencing RRT will have an increase in drug CL and the corresponding change in plasma drug concentrations can be detected and dosing can be adjusted more efficiently. Third, as TDM information is gathered at a faster pace with potentially more intensive sampling, there is a possibility for these data to inform and fine-tune population PK models used in MIPD software, making these applications “smarter” in dosing accuracy (Fig. 1). As we are still limited in our knowledge of the impact of extracorporeal circuits on drug exposure, there is scope for TDM biosensors to be used in the future research, especially when novel therapeutics are first administered to patients on extracorporeal treatments. Most importantly, clinical implementation of innovations such as MIPD relies heavily on improving clinician understanding of PK/PD concepts and principles. Without this underlying knowledge, clinicians may not fully appreciate the complexities of how changes in drug exposure are influenced by extracorporeal treatment modalities, such as ECMO or RRT, and will likely not be equipped to maximise the use of these technologies.
Fig. 1.
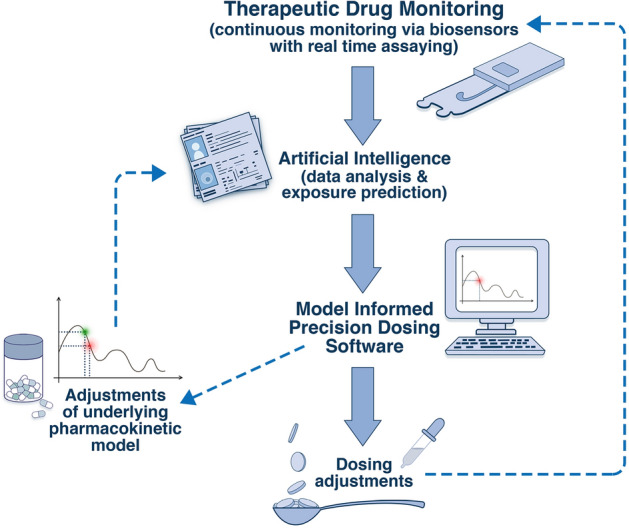
Future approach to therapeutic drug monitoring and use of dosing software in the ICU
In our opinion, ICU monitoring of antibiotic exposure has the capacity for significant progress in the near future. As a first step, MIPD software will need validated models that can help predict antibiotic exposure in critically ill patients on ECMO and RRT. However, as there are many variables that may influence drug exposure in these patients, and these variables change continuously, we know that MIPD alone is somewhat limited in its ability to improve attainment of target exposures. To this extent, although TDM remains the central tool to adapt antimicrobial dosing in most centres, TDM processes will need to become streamlined so that the time-lag between analysis and reporting is greatly reduced. Therefore, the ideal picture in 10–15 years would be that, in addition to MIPD software incorporated into the patient dossier, real-time TDM of antimicrobials in these patients can be achieved through a validated and in situ secured biosensor (either via micro-dialysis or the skin). Output data can be used and interpreted by a team composed of a clinical pharmacist/pharmacologist and intensive care specialist (with input from infectious diseases clinicians if required) to optimise antimicrobial doses accordingly. Alternatively, antimicrobial dosing could be automatically corrected by the system through use of smart antibiotic pumps that can adjust infusion rates. These infusor devices, however, would still need operator controlled and clinician overriding mechanisms in place at all times.
Conclusion
ECMO and RRT machines can further exacerbate existing PK alterations observed during critical illness potentially leading to therapeutic failure and/or drug toxicity. The combined use of ECMO and RRT is common in the ICU, and this further complicates drug dosing, particularly for antimicrobials. Poor antimicrobial exposure (either sub-therapeutic or supra-therapeutic exposures) is a recurrent theme that is associated with worse patient outcomes and is a worrying trend in critically ill patients, with or without the two extracorporeal devices. Optimised dosing strategies supported by other ‘machines’, and routine TDM (where possible) would be advantageous to prevent sub-therapeutic and toxic drug exposures in critically ill patients receiving ECMO and/or RRT.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
JAR receives funding from the Australian National Health and Medical Research Council for a Centre of Research Excellence (APP2007007) and an Investigator Grant (APP2009736), as well as an Advancing Queensland Clinical Fellowship. KS acknowledges research support from Metro North Hospital and Health Service. KW acknowledges support from the National Institutes of Health for his work in paediatric extracorporeal life support (5R01HD097775).
Author contributions
The idea and design of the paper were conceptualised by JAR. Literature review and data analysis were performed by all authors. The first draft of the paper was jointly written by all authors according to the assigned sections. All authors critically revised and commented on subsequent versions of the manuscript. All authors read and approved the final version of the paper.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Declarations
Conflicts of interest
All authors declare no conflict of interest in relation to this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hites M, Dell'Anna AM, Scolletta S, Taccone FS. The challenges of multiple organ dysfunction syndrome and extra-corporeal circuits for drug delivery in critically ill patients. Adv Drug Deliv Rev. 2014;77:12–21. doi: 10.1016/j.addr.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 2.Cheng V, Abdul-Aziz MH, Roberts JA. Applying antimicrobial pharmacokinetic principles for complex patients: critically ill adult patients receiving extracorporeal membrane oxygenation and renal replacement therapy. Curr Infect Dis Rep. 2021;23:13. doi: 10.1007/s11908-021-00757-y. [DOI] [Google Scholar]
- 3.Kuhn D, Metz C, Seiler F, Wehrfritz H, Roth S, Alqudrah M, Becker A, Bracht H, Wagenpfeil S, Hoffmann M, Bals R, Hubner U, Geisel J, Lepper PM, Becker SL. Antibiotic therapeutic drug monitoring in intensive care patients treated with different modalities of extracorporeal membrane oxygenation (ECMO) and renal replacement therapy: a prospective, observational single-center study. Crit Care. 2020;24:664. doi: 10.1186/s13054-020-03397-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberts JA, Joynt GM, Lee A, Choi G, Bellomo R, Kanji S, Mudaliar MY, Peake SL, Stephens D, Taccone FS, Ulldemolins M, Valkonen MM, Agbeve J, Baptista JP, Bekos V, Boidin C, Brinkmann A, Buizen L, Castro P, Cole CL, Creteur J, De Waele JJ, Deans R, Eastwood GM, Escobar L, Gomersall C, Gresham R, Jamal JA, Kluge S, Konig C, Koulouras VP, Lassig-Smith M, Laterre PF, Lei K, Leung P, Lefrant JY, Llaurado-Serra M, Martin-Loeches I, Mat Nor MB, Ostermann M, Parker SL, Rello J, Roberts DM, Roberts MS, Richards B, Rodriguez A, Roehr AC, Roger C, Seoane L, Sinnollareddy M, Sousa E, Soy D, Spring A, Starr T, Thomas J, Turnidge J, Wallis SC, Williams T, Wittebole X, Zikou XT, Paul SK, Lipman J, Collaborators SS, the ACTG The effect of renal replacement therapy and antibiotic dose on antibiotic concentrations in critically ill patients: data from the multinational sampling antibiotics in renal replacement therapy study. Clin Infect Dis. 2021;72:1369–1378. doi: 10.1093/cid/ciaa224. [DOI] [PubMed] [Google Scholar]
- 5.Bougle A, Dujardin O, Lepere V, Ait Hamou N, Vidal C, Lebreton G, Salem JE, El-Helali N, Petijean G, Amour J. PHARMECMO: therapeutic drug monitoring and adequacy of current dosing regimens of antibiotics in patients on Extracorporeal Life Support. Anaesth Crit Care Pain Med. 2019;38:493–497. doi: 10.1016/j.accpm.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Imani S, Buscher H, Marriott D, Gentili S, Sandaradura I. Too much of a good thing: a retrospective study of beta-lactam concentration-toxicity relationships. J Antimicrob Chemother. 2017;72:2891–2897. doi: 10.1093/jac/dkx209. [DOI] [PubMed] [Google Scholar]
- 7.Abdul-Aziz MH, Driver E, Lipman J, Roberts JA. New paradigm for rapid achievement of appropriate therapy in special populations: coupling antibiotic dose optimization rapid microbiological methods. Expert Opin Drug Metab Toxicol. 2018;14:693–708. doi: 10.1080/17425255.2018.1484452. [DOI] [PubMed] [Google Scholar]
- 8.Abdul-Aziz MH, Alffenaar JC, Bassetti M, Bracht H, Dimopoulos G, Marriott D, Neely MN, Paiva JA, Pea F, Sjovall F, Timsit JF, Udy AA, Wicha SG, Zeitlinger M, De Waele JJ, Roberts JA, Infection Section of European Society of Intensive Care M, Pharmacokinetic/pharmacodynamic, Critically Ill Patient Study Groups of European Society of Clinical M, Infectious D, Infectious Diseases Group of International Association of Therapeutic Drug M, Clinical T, Infections in the ICU, Sepsis Working Group of International Society of Antimicrobial C Antimicrobial therapeutic drug monitoring in critically ill adult patients: a Position Paper. Intensive Care Med. 2020;46:1127–1153. doi: 10.1007/s00134-020-06050-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tangden T, Ramos Martin V, Felton TW, Nielsen EI, Marchand S, Bruggemann RJ, Bulitta JB, Bassetti M, Theuretzbacher U, Tsuji BT, Wareham DW, Friberg LE, De Waele JJ, Tam VH, Roberts JA. The role of infection models and PK/PD modelling for optimising care of critically ill patients with severe infections. Intensive Care Med. 2017;43:1021–1032. doi: 10.1007/s00134-017-4780-6. [DOI] [PubMed] [Google Scholar]
- 10.Roberts JA, Taccone FS, Lipman J. Understanding PK/PD. Intensive Care Med. 2016;42:1797–1800. doi: 10.1007/s00134-015-4032-6. [DOI] [PubMed] [Google Scholar]
- 11.Udy AA, Roberts JA, Lipman J. Clinical implications of antibiotic pharmacokinetic principles in the critically ill. Intensive Care Med. 2013;39:2070–2082. doi: 10.1007/s00134-013-3088-4. [DOI] [PubMed] [Google Scholar]
- 12.Hahn J, Choi JH, Chang MJ. Pharmacokinetic changes of antibiotic, antiviral, antituberculosis and antifungal agents during extracorporeal membrane oxygenation in critically ill adult patients. J Clin Pharm Ther. 2017;42(6):661–671. doi: 10.1111/jcpt.12636. [DOI] [PubMed] [Google Scholar]
- 13.Jamal JA, Mueller BA, Choi GY, Lipman J, Roberts JA. How can we ensure effective antibiotic dosing in critically ill patients receiving different types of renal replacement therapy? Diagn Microbiol Infect Dis. 2015;82:92–103. doi: 10.1016/j.diagmicrobio.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 14.Abdul-Aziz MH, Roberts JA. Antibiotic dosing during extracorporeal membrane oxygenation: does the system matter? Curr Opin Anaesthesiol. 2020;33:71–82. doi: 10.1097/ACO.0000000000000810. [DOI] [PubMed] [Google Scholar]
- 15.Ha MA, Sieg AC. Evaluation of altered drug pharmacokinetics in critically ill adults receiving extracorporeal membrane oxygenation. Pharmacotherapy. 2017;37:221–235. doi: 10.1002/phar.1882. [DOI] [PubMed] [Google Scholar]
- 16.Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, Kaukonen KM, Koulenti D, Martin C, Montravers P, Rello J, Rhodes A, Starr T, Wallis SC, Lipman J, Study D DALI: defining antibiotic levels in intensive care unit patients: are current beta-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis. 2014;58:1072–1083. doi: 10.1093/cid/ciu027. [DOI] [PubMed] [Google Scholar]
- 17.Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26:1–10. doi: 10.1086/516284. [DOI] [PubMed] [Google Scholar]
- 18.Abdul-Aziz MH, Brady K, Cotta MO, Roberts JA. Therapeutic drug monitoring of antibiotics: defining the therapeutic range. Ther Drug Monit. 2022;44:19–31. doi: 10.1097/FTD.0000000000000940. [DOI] [PubMed] [Google Scholar]
- 19.Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, Kallen A, Limbago B, Fridkin S, National Healthcare Safety Network T, Participating NF Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009–2010. Infect Control Hosp Epidemiol. 2013;34:1–14. doi: 10.1086/668770. [DOI] [PubMed] [Google Scholar]
- 20.Mouton JW, Muller AE, Canton R, Giske CG, Kahlmeter G, Turnidge J. MIC-based dose adjustment: facts and fables. J Antimicrob Chemother. 2018;73:564–568. doi: 10.1093/jac/dkx427. [DOI] [PubMed] [Google Scholar]
- 21.Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, Edipidis K, Forni LG, Gomersall CD, Govil D, Honoré PM, Joannes-Boyau O, Joannidis M, Korhonen AM, Lavrentieva A, Mehta RL, Palevsky P, Roessler E, Ronco C, Uchino S, Vazquez JA, Vidal Andrade E, Webb S, Kellum JA. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41:1411–1423. doi: 10.1007/s00134-015-3934-7. [DOI] [PubMed] [Google Scholar]
- 22.Bagshaw SM, Wald R, Adhikari NKJ, Bellomo R, da Costa BR, Dreyfuss D, Du B, Gallagher MP, Gaudry S, Hoste EA, Lamontagne F, Joannidis M, Landoni G, Liu KD, McAuley DF, McGuinness SP, Neyra JA, Nichol AD, Ostermann M, Palevsky PM, Pettilä V, Quenot JP, Qiu H, Rochwerg B, Schneider AG, Smith OM, Thomé F, Thorpe KE, Vaara S, Weir M, Wang AY, Young P, Zarbock A. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240–251. doi: 10.1056/NEJMoa2000741. [DOI] [PubMed] [Google Scholar]
- 23.Zhang L, Yang J, Eastwood GM, Zhu G, Tanaka A, Bellomo R. Extended daily dialysis versus continuous renal replacement therapy for acute kidney injury: a meta-analysis. Am J Kidney Dis. 2015;66:322–330. doi: 10.1053/j.ajkd.2015.02.328. [DOI] [PubMed] [Google Scholar]
- 24.Neri M, Villa G, Garzotto F, Bagshaw S, Bellomo R, Cerda J, Ferrari F, Guggia S, Joannidis M, Kellum J, Kim JC, Mehta RL, Ricci Z, Trevisani A, Marafon S, Clark WR, Vincent JL, Ronco C. Nomenclature for renal replacement therapy in acute kidney injury: basic principles. Crit Care. 2016;20:318. doi: 10.1186/s13054-016-1489-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shields RK, Nguyen MH, Chen L, Press EG, Kreiswirth BN, Clancy CJ (2018) Pneumonia and renal replacement therapy are risk factors for ceftazidime-avibactam treatment failures and resistance among patients with carbapenem-resistant enterobacteriaceae infections. Antimicrob Agents Chemother 62(5):e02497–17 [DOI] [PMC free article] [PubMed]
- 26.Roger C, Muller L, Wallis SC, Louart B, Saissi G, Lipman J, Lefrant JY, Roberts JA. Population pharmacokinetics of linezolid in critically ill patients on renal replacement therapy: comparison of equal doses in continuous venovenous haemofiltration and continuous venovenous haemodiafiltration. J Antimicrob Chemother. 2016;71:464–470. doi: 10.1093/jac/dkv349. [DOI] [PubMed] [Google Scholar]
- 27.Roger C, Wallis SC, Muller L, Saissi G, Lipman J, Lefrant JY, Roberts JA. Influence of renal replacement modalities on amikacin population pharmacokinetics in critically ill patients on continuous renal replacement therapy. Antimicrob Agents Chemother. 2016;60:4901–4909. doi: 10.1128/AAC.00828-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jamal JA, Udy AA, Lipman J, Roberts JA. The impact of variation in renal replacement therapy settings on piperacillin, meropenem, and vancomycin drug clearance in the critically ill: an analysis of published literature and dosing regimens*. Crit Care Med. 2014;42:1640–1650. doi: 10.1097/CCM.0000000000000317. [DOI] [PubMed] [Google Scholar]
- 29.Barrasa H, Soraluce A, Isla A, Martín A, Maynar J, Canut A, Sánchez-Izquierdo JA, Rodríguez-Gascón A. Pharmacokinetics of linezolid in critically ill patients on continuous renal replacement therapy: Influence of residual renal function on PK/PD target attainment. J Crit Care. 2019;50:69–76. doi: 10.1016/j.jcrc.2018.11.016. [DOI] [PubMed] [Google Scholar]
- 30.Ulldemolins M, Soy D, Llaurado-Serra M, Vaquer S, Castro P, Rodríguez AH, Pontes C, Calvo G, Torres A, Martín-Loeches I. Meropenem population pharmacokinetics in critically ill patients with septic shock and continuous renal replacement therapy: influence of residual diuresis on dose requirements. Antimicrob Agents Chemother. 2015;59:5520–5528. doi: 10.1128/AAC.00712-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee BV, Fong G, Bolaris M, Neely M, Minejima E, Kang A, Lee G, Gong CL. Cost-benefit analysis comparing trough, two-level AUC and Bayesian AUC dosing for vancomycin. Clin Microbiol Infect. 2021;27:1346.e1341–1346.e1347. doi: 10.1016/j.cmi.2020.11.008. [DOI] [PubMed] [Google Scholar]
- 32.Wicha SG, Märtson AG, Nielsen EI, Koch BCP, Friberg LE, Alffenaar JW, Minichmayr IK. From therapeutic drug monitoring to model-informed precision dosing for antibiotics. Clin Pharmacol Ther. 2021;109:928–941. doi: 10.1002/cpt.2202. [DOI] [PubMed] [Google Scholar]
- 33.Roberts JA, Lipman J. Pharmacokinetic issues for antibiotics in the critically ill patient. Crit Care Med. 2009;37:840–851. doi: 10.1097/CCM.0b013e3181961bff. [DOI] [PubMed] [Google Scholar]
- 34.Bartlett RH, Gattinoni L. Current status of extracorporeal life support (ECMO) for cardiopulmonary failure. Minerva Anestesiol. 2010;76:534–540. [PubMed] [Google Scholar]
- 35.Bartlett RH. Extracorporeal life support: history and new directions. Asaio J. 2005;51:487–489. doi: 10.1097/01.mat.0000179141.08834.cb. [DOI] [PubMed] [Google Scholar]
- 36.Shekar K, Roberts JA, McDonald CI, Fisquet S, Barnett AG, Mullany DV, Ghassabian S, Wallis SC, Fung YL, Smith MT, Fraser JF. Sequestration of drugs in the circuit may lead to therapeutic failure during extracorporeal membrane oxygenation. Crit Care. 2012;16:R194. doi: 10.1186/cc11679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wildschut ED, Ahsman MJ, Allegaert K, Mathot RA, Tibboel D. Determinants of drug absorption in different ECMO circuits. Intensive Care Med. 2010;36:2109–2116. doi: 10.1007/s00134-010-2041-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raffaeli G, Pokorna P, Allegaert K, Mosca F, Cavallaro G, Wildschut ED, Tibboel D. Drug disposition and pharmacotherapy in neonatal ECMO: from fragmented data to integrated knowledge. Front Pediatr. 2019;7:360. doi: 10.3389/fped.2019.00360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Park J, Shin DA, Lee S, Cho YJ, Jheon S, Lee JC, Kim HC. Investigation of key circuit constituents affecting drug sequestration during extracorporeal membrane oxygenation treatment. ASAIO J. 2017;63:293–298. doi: 10.1097/MAT.0000000000000489. [DOI] [PubMed] [Google Scholar]
- 40.Lemaitre F, Hasni N, Leprince P, Corvol E, Belhabib G, Fillâtre P, Luyt CE, Leven C, Farinotti R, Fernandez C, Combes A. Propofol, midazolam, vancomycin and cyclosporine therapeutic drug monitoring in extracorporeal membrane oxygenation circuits primed with whole human blood. Crit Care. 2015;19:40. doi: 10.1186/s13054-015-0772-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shekar K, Roberts JA, Barnett AG, Diab S, Wallis SC, Fung YL, Fraser JF. Can physicochemical properties of antimicrobials be used to predict their pharmacokinetics during extracorporeal membrane oxygenation? Illustrative data from ovine models. Crit Care. 2015;19:437. doi: 10.1186/s13054-015-1151-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Spriet I, Annaert P, Meersseman P, Hermans G, Meersseman W, Verbesselt R, Willems L. Pharmacokinetics of caspofungin and voriconazole in critically ill patients during extracorporeal membrane oxygenation. J Antimicrob Chemother. 2009;63:767–770. doi: 10.1093/jac/dkp026. [DOI] [PubMed] [Google Scholar]
- 43.Preston TJ, Ratliff TM, Gomez D, Olshove VE, Jr, Nicol KK, Sargel CL, Chicoine LG. Modified surface coatings and their effect on drug adsorption within the extracorporeal life support circuit. J Extra Corpor Technol. 2010;42:199–202. [PMC free article] [PubMed] [Google Scholar]
- 44.Bhatt-Meht V, Annich G. Sedative clearance during extracorporeal membrane oxygenation. Perfusion. 2005;20:309–315. doi: 10.1191/0267659105pf827oa. [DOI] [PubMed] [Google Scholar]
- 45.Mehta NM, Halwick DR, Dodson BL, Thompson JE, Arnold JH. Potential drug sequestration during extracorporeal membrane oxygenation: results from an ex vivo experiment. Intensive Care Med. 2007;33:1018–1024. doi: 10.1007/s00134-007-0606-2. [DOI] [PubMed] [Google Scholar]
- 46.Harthan AA, Buckley KW, Heger ML, Fortuna RS, Mays K. Medication adsorption into contemporary extracorporeal membrane oxygenator circuits. J Pediatr Pharmacol Ther. 2014;19:288–295. doi: 10.5863/1551-6776-19.4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stanke-Labesque F, Gautier-Veyret E, Chhun S, Guilhaumou R. Inflammation is a major regulator of drug metabolizing enzymes and transporters: consequences for the personalization of drug treatment. Pharmacol Ther. 2020;215:107627. doi: 10.1016/j.pharmthera.2020.107627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen YC, Tsai FC, Fang JT, Yang CW. Acute kidney injury in adults receiving extracorporeal membrane oxygenation. J Formos Med Assoc. 2014;113:778–785. doi: 10.1016/j.jfma.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 49.Watt KM, Cohen-Wolkowiez M, Barrett JS, Sevestre M, Zhao P, Brouwer KLR, Edginton AN. Physiologically based pharmacokinetic approach to determine dosing on extracorporeal life support: fluconazole in children on ECMO. CPT Pharmacometrics Syst Pharmacol. 2018;7:629–637. doi: 10.1002/psp4.12338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Autmizguine J, Hornik CP, Benjamin DK, Jr, Brouwer KL, Hupp SR, Cohen-Wolkowiez M, Watt KM. Pharmacokinetics and safety of micafungin in infants supported with extracorporeal membrane oxygenation. Pediatr Infect Dis J. 2016;35:1204–1210. doi: 10.1097/INF.0000000000001268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Watt KM, Benjamin DK, Jr, Cheifetz IM, Moorthy G, Wade KC, Smith PB, Brouwer KL, Capparelli EV, Cohen-Wolkowiez M. Pharmacokinetics and safety of fluconazole in young infants supported with extracorporeal membrane oxygenation. Pediatr Infect Dis J. 2012;31:1042–1047. doi: 10.1097/INF.0b013e31825d3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dagan O, Klein J, Gruenwald C, Bohn D, Barker G, Koren G. Preliminary studies of the effects of extracorporeal membrane oxygenator on the disposition of common pediatric drugs. Ther Drug Monit. 1993;15:263–266. doi: 10.1097/00007691-199308000-00001. [DOI] [PubMed] [Google Scholar]
- 53.Kim YK, Kim HS, Park S, Kim HI, Lee SH, Lee DH. Population pharmacokinetics of piperacillin/tazobactam in critically ill Korean patients and the effects of extracorporeal membrane oxygenation. J Antimicrob Chemother. 2022;77:1353–1364. doi: 10.1093/jac/dkac059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alihodzic D, Wicha SG, Frey OR, König C, Baehr M, Jarczak D, Kluge S, Langebrake C. Ciprofloxacin in patients undergoing extracorporeal membrane oxygenation (ECMO): a population pharmacokinetic study. Pharmaceutics. 2022;14(5):965. doi: 10.3390/pharmaceutics14050965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kois AK, Gluck JA, Nicolau DP, Kuti JL. Pharmacokinetics and time above the MIC exposure of cefepime in critically ill patients receiving extracorporeal membrane oxygenation (ECMO) Int J Antimicrob Agents. 2022;60:106603. doi: 10.1016/j.ijantimicag.2022.106603. [DOI] [PubMed] [Google Scholar]
- 56.Cheng V, Abdul-Aziz MH, Burrows F, Buscher H, Cho YJ, Corley A, Diehl A, Gilder E, Jakob SM, Kim HS, Levkovich BJ, Lim SY, McGuinness S, Parke R, Pellegrino V, Que YA, Reynolds C, Rudham S, Wallis SC, Welch SA, Zacharias D, Fraser JF, Shekar K, Roberts JA, Investigators AE. Population pharmacokinetics of vancomycin in critically ill adult patients receiving extracorporeal membrane oxygenation (an ASAP ECMO Study) Antimicrob Agents Chemother. 2022;66:e0137721. doi: 10.1128/AAC.01377-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cheng V, Abdul-Aziz MH, Burrows F, Buscher H, Cho YJ, Corley A, Gilder E, Kim HS, Lim SY, McGuinness S, Parke R, Reynolds C, Rudham S, Wallis SC, Welch SA, Fraser JF, Shekar K, Roberts JA (2022) Population pharmacokinetics and dosing simulations of ceftriaxone in critically ill patients receiving extracorporeal membrane oxygenation (An ASAP ECMO Study). Clin Pharmacokinet 61(6):847–856 [DOI] [PMC free article] [PubMed]
- 58.Jung Y, Lee DH, Kim HS (2021) Prospective cohort study of population pharmacokinetics and pharmacodynamic target attainment of vancomycin in adults on extracorporeal membrane oxygenation. Antimicrob Agents Chemother 65(2):e02408–20 [DOI] [PMC free article] [PubMed]
- 59.Cheng V, Abdul-Aziz MH, Burrows F, Buscher H, Corley A, Diehl A, Jakob SM, Levkovich BJ, Pellegrino V, Que YA, Reynolds C, Rudham S, Wallis SC, Welch SA, Zacharias D, Roberts JA, Shekar K, Fraser JF. Population pharmacokinetics of cefepime in critically ill patients receiving extracorporeal membrane oxygenation (an ASAP ECMO study) Int J Antimicrob Agents. 2021;58:106466. doi: 10.1016/j.ijantimicag.2021.106466. [DOI] [PubMed] [Google Scholar]
- 60.Cheng V, Abdul-Aziz MH, Burrows F, Buscher H, Cho YJ, Corley A, Diehl A, Gilder E, Jakob SM, Kim HS, Levkovich BJ, Lim SY, McGuinness S, Parke R, Pellegrino V, Que YA, Reynolds C, Rudham S, Wallis SC, Welch SA, Zacharias D, Fraser JF, Shekar K, Roberts JA, Investigators AE. Population Pharmacokinetics of piperacillin and tazobactam in critically ill patients receiving extracorporeal membrane oxygenation: an ASAP ECMO Study. Antimicrob Agents Chemother. 2021;65:e0143821. doi: 10.1128/AAC.01438-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gijsen M, Dreesen E, Annaert P, Nicolai J, Debaveye Y, Wauters J, Spriet I (2021) Meropenem pharmacokinetics and target attainment in critically ill patients are not affected by extracorporeal membrane oxygenation: a matched cohort analysis. Microorganisms 9(6):1310 [DOI] [PMC free article] [PubMed]
- 62.Van Daele R, Bekkers B, Lindfors M, Broman LM, Schauwvlieghe A, Rijnders B, Hunfeld NGM, Juffermans NP, Taccone FS, Coimbra Sousa CA, Jacquet LM, Laterre PF, Nulens E, Grootaert V, Lyster H, Reed A, Patel B, Meersseman P, Debaveye Y, Wauters J, Vandenbriele C, Spriet I (2021) A large retrospective assessment of voriconazole exposure in patients treated with extracorporeal membrane oxygenation. Microorganisms 9(7):1543 [DOI] [PMC free article] [PubMed]
- 63.Touchard C, Aubry A, Eloy P, Brechot N, Lebreton G, Franchineau G, Besset S, Hekimian G, Nieszkowska A, Leprince P, Luyt CE, Combes A, Schmidt M. Predictors of insufficient peak amikacin concentration in critically ill patients on extracorporeal membrane oxygenation. Crit Care. 2018;22:199. doi: 10.1186/s13054-018-2122-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cheng V, Abdul-Aziz MH, Burrows F, Buscher H, Corley A, Diehl A, Levkovich BJ, Pellegrino V, Reynolds C, Rudham S, Wallis SC, Welch SA, Roberts JA, Shekar K, Fraser JF. Population pharmacokinetics of ciprofloxacin in critically ill patients receiving extracorporeal membrane oxygenation (an ASAP ECMO study) Anaesth Crit Care Pain Med. 2022;41:101080. doi: 10.1016/j.accpm.2022.101080. [DOI] [PubMed] [Google Scholar]
- 65.Sinnah F, Shekar K, Abdul-Aziz MH, Buscher H, Diab SD, Fisquet S, Fung YL, McDonald CI, Reynolds C, Rudham S, Wallis SC, Welch S, Xie J, Fraser JF, Roberts JA, investigators AE Incremental research approach to describing the pharmacokinetics of ciprofloxacin during extracorporeal membrane oxygenation. Crit Care Resusc. 2017;19:8–14. [PubMed] [Google Scholar]
- 66.Shekar K, Roberts JA, McDonald CI, Ghassabian S, Anstey C, Wallis SC, Mullany DV, Fung YL, Fraser JF. Protein-bound drugs are prone to sequestration in the extracorporeal membrane oxygenation circuit: results from an ex vivo study. Crit Care. 2015;19:164. doi: 10.1186/s13054-015-0891-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shekar K, Roberts JA, Smith MT, Fung YL, Fraser JF. The ECMO PK Project: an incremental research approach to advance understanding of the pharmacokinetic alterations and improve patient outcomes during extracorporeal membrane oxygenation. BMC Anesthesiol. 2013;13:7. doi: 10.1186/1471-2253-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shekar K, Roberts JA, Welch S, Buscher H, Rudham S, Burrows F, Ghassabian S, Wallis SC, Levkovich B, Pellegrino V, McGuinness S, Parke R, Gilder E, Barnett AG, Walsham J, Mullany DV, Fung YL, Smith MT, Fraser JF. ASAP ECMO: antibiotic, sedative and analgesic pharmacokinetics during extracorporeal membrane oxygenation: a multi-centre study to optimise drug therapy during ECMO. BMC Anesthesiol. 2012;12:29. doi: 10.1186/1471-2253-12-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cies JJ, Moore WS, 2nd, Conley SB, Dickerman MJ, Small C, Carella D, Shea P, Parker J, Chopra A. Pharmacokinetics of continuous infusion meropenem with concurrent extracorporeal life support and continuous renal replacement therapy: a case report. J Pediatr Pharmacol Ther. 2016;21:92–97. doi: 10.5863/1551-6776-21.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nordmann P, Picazo JJ, Mutters R, Korten V, Quintana A, Laeuffer JM, Seak JC, Flamm RK, Morrissey I. Comparative activity of carbapenem testing: the COMPACT study. J Antimicrob Chemother. 2011;66:1070–1078. doi: 10.1093/jac/dkr056. [DOI] [PubMed] [Google Scholar]
- 71.McKinnon PS, Paladino JA, Schentag JJ. Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T>MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents. 2008;31:345–351. doi: 10.1016/j.ijantimicag.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 72.Moise-Broder PA, Forrest A, Birmingham MC, Schentag JJ. Pharmacodynamics of vancomycin and other antimicrobials in patients with Staphylococcus aureus lower respiratory tract infections. Clin Pharmacokinet. 2004;43:925–942. doi: 10.2165/00003088-200443130-00005. [DOI] [PubMed] [Google Scholar]
- 73.Imani S, Alffenaar JW, Cotta MO, Daveson K, van Hal S, Lau C, Marriott D, Penm J, Roberts JA, Tabah A, Trethewy N, Williams P, Sandaradura I (2020) Therapeutic drug monitoring of commonly used anti-infective agents: A nationwide cross-sectional survey of Australian hospital practices. Int J Antimicrob Agents, 56(6):106180 [DOI] [PubMed]
- 74.Tabah A, De Waele J, Lipman J, Zahar JR, Cotta MO, Barton G, Timsit JF, Roberts JA, Working Group for Antimicrobial Use in the ICUwtISotESoICM The ADMIN-ICU survey: a survey on antimicrobial dosing and monitoring in ICUs. J Antimicrob Chemother. 2015;70:2671–2677. doi: 10.1093/jac/dkv165. [DOI] [PubMed] [Google Scholar]
- 75.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 76.Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Kumar A, Cheang M. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 77.Ates HC, Roberts JA, Lipman J, Cass AEG, Urban GA, Dincer C. On-site therapeutic drug monitoring. Trends Biotechnol. 2020;38:1262–1277. doi: 10.1016/j.tibtech.2020.03.001. [DOI] [PubMed] [Google Scholar]
- 78.Rawson TM, O'Hare D, Herrero P, Sharma S, Moore LSP, de Barra E, Roberts JA, Gordon AC, Hope W, Georgiou P, Cass AEG, Holmes AH. Delivering precision antimicrobial therapy through closed-loop control systems. J Antimicrob Chemother. 2018;73:835–843. doi: 10.1093/jac/dkx458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Visser EWA, Yan J, van IJzendoorn LJ, Prins MWJ. Continuous biomarker monitoring by particle mobility sensing with single molecule resolution. Nat Commun. 2018;9:2541. doi: 10.1038/s41467-018-04802-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bian S, Zhu B, Rong G, Sawan M. Towards wearable and implantable continuous drug monitoring: a review. J Pharm Anal. 2021;11:1–14. doi: 10.1016/j.jpha.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Heil EL, Nicolau DP, Farkas A, Roberts JA, Thom KA (2018) Pharmacodynamic target attainment for cefepime, meropenem, and piperacillin-tazobactam using a pharmacokinetic/pharmacodynamic-based dosing calculator in critically ill patients. Antimicrob Agents Chemother 62(9):e01008–18 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


