Abstract
Objectives
The COVID-19 pandemic caused an unprecedented health crisis resulting in over 6 million deaths worldwide, a figure, which continues to grow. In addition to the excess mortality, there are individuals who recovered from the acute stages, but suffered long-term changes in their health post COVID-19, commonly referred to as long COVID. It is estimated there are currently 1.8 million long COVID sufferers by May 2022 in the UK alone. The aim of this narrative literature review is to explore the signs, symptoms and diagnosis of long COVID and the potential impact on imaging services.
Key findings
Long COVID is estimated to occur in 9.5% of those with two doses of vaccination and 14.6% if those with a single dose or no vaccination. Long COVID is defined by ongoing symptoms lasting for 12 or more weeks post acute infection. Symptoms are associated with reductions in the quality of daily life and may involve multisystem manifestations or present as a single symptom.
Conclusion
The full impact of long COVID on imaging services is yet to be realised, but there is likely to be significant increased demand for imaging, particularly in CT for the assessment of lung disease. Educators will need to include aspects related to long COVID pathophysiology and imaging presentations in curricula, underpinned by the rapidly evolving evidence base.
Implications for practice
Symptoms relating to long COVID are likely to become a common reason for imaging, with a particular burden on Computed Tomography services. Planning, education and updating protocols in line with a rapidly emerging evidence base is going to be essential.
Keywords: Long-covid, COVID-19, Imaging, Computed tomography, Magnetic resonance imaging, Radiography
Introduction
Medical imaging played and continues to play an essential role during the COVID-19 pandemic for patient diagnostics and assessment. High-resolution chest computed tomography (CT) was established as the gold standard for identifying subtle changes within the lung fields caused in response to COVID-19 infection with 90% sensitivity and 91% specificity.1 In comparison, chest X-rays have a sensitivity and specificity estimated at 89% and 41%–66% due to their reliance on reader experience and ability.2 Magnetic resonance imaging (MRI), particularly ultrashort echo time MRI (UTE-MRI), is recommended as an alternative to CT to evaluate COVID-19.3 While some imaging increased during the initial waves of COVID-19, some non-urgent imaging was postponed, and some services, such as dual-energy X-ray absorptiometry (DXA) and the mammography screening programme,4, 5, 6 were closed in many hospitals, resulting in waiting list increases, which remain two years later.7 , 8
With each wave of COVID-19, significant pressure was put on the NHS and imaging services, not just from patient volume, but also increasingly due to staff sickness with COVID-19.9 , 10 Vaccination against SARS-CoV-2 limits the severity of symptoms, reduces the number of hospitalisations and is currently seen as the route out of the pandemic.11
As the acute phase of the pandemic recedes, however, there is a greater awareness, that many individuals who have recovered from the acute stages of the disease have reported prolonged changes in their physical health and wellbeing post-COVID-19.12 The term “long COVID”, alongside the term “long haulers”, was first used by Dr. Elisa Perego on 20 May 2020 in a social media post describing the disease experience in Italy.13 In mid-March 2021, more than 50,000 mentions of long COVID were noted on social media, indicating an increase of 140%. Callard and Perego14 concluded that “long COVID has a strong claim to be considered the first illness to be collectively made by patients finding one another through Twitter and other social media.”
The UK National Health Service (NHS) continues to be severely challenged as it commences the recovery program to combat the built-up waiting lists for routine procedures and imaging at record levels. As such, the NHS must adapt to also diagnose and treat the estimated 2 million15 people suffering with long COVID, a disease that did not exist 3 years ago. This paper aims to outline the presentations of long COVID and explore the impact on imaging services along with the rapid adjustments in education needed to underpin the diagnosis, treatment, and treatment monitoring of this new disease. As more becomes known about long-COVID and therapeutic interventions are explored, diagnostic pathways will develop. It is important for radiographers to understand the presentations of long-COVID so that they can make informed decisions relating to imaging this patient group.
What is long COVID?
Many definitions and classifications have been established for long COVID. The term “long COVID” remains the patient-preferred name for this condition,14 although the National Institute for Health Excellence (NICE) uses the term “Post COVID-19 Syndrome” defined as: Signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis.16 The World Health Organization has further refined this definition to a condition which “… occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis”. The Americans with Disability Act classified long COVID count as disability in July 2021,17 then at 1st of October 2021, the CDC and National Centre for Health Statistics (NCHS) developed a new code for post-COVID-19 conditions.18 The CDC and NICE have indicated that persistent symptoms of long COVID can be experienced even by non-hospitalised individuals, of any age group, with a history of confirmed acute COVID-19, even if that initial infection was asymptomatic.19 , 20
Varying reports have noted the rates of developing long COVID with little insight and knowledge about known determinants. The Office for National Statistics (ONS) estimate that long COVID is 9.5% in people who self-reported two doses of vaccination and 14.6% for both single vaccinated and unvaccinated.21 Other studies estimate greater prevalence.22 , 23 Over the 6 months after their acute infection, a Norwegian study evaluated 312 patients who contracted COVID-19 during the first wave. Some of these cases were milder (247 home-isolated) whilst 65 were hospitalised due to their more severe disease.24 Rates of long-COVID in this population was 61%, much higher than the current ONS self-reporting estimates in the UK. Other data indicates that most patients requiring hospitalisation for COVID-19 still have persistent symptoms, even after a year.25 , 26 Care must be taken when interpreting these estimates as they vary depending in study methodologies. Currently, the ONS and The Solve ME/CFS Initiative (Solve M.E.) state that about 3% of the UK and 7% of the U.S. population has reported experiencing long COVID symptoms.15 , 27
Long COVID subtypes
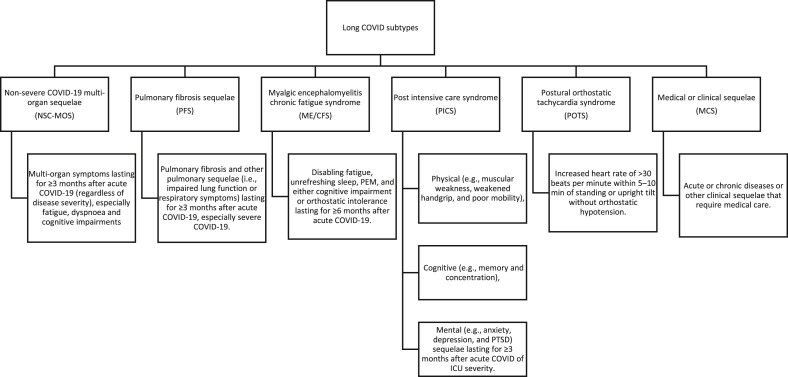
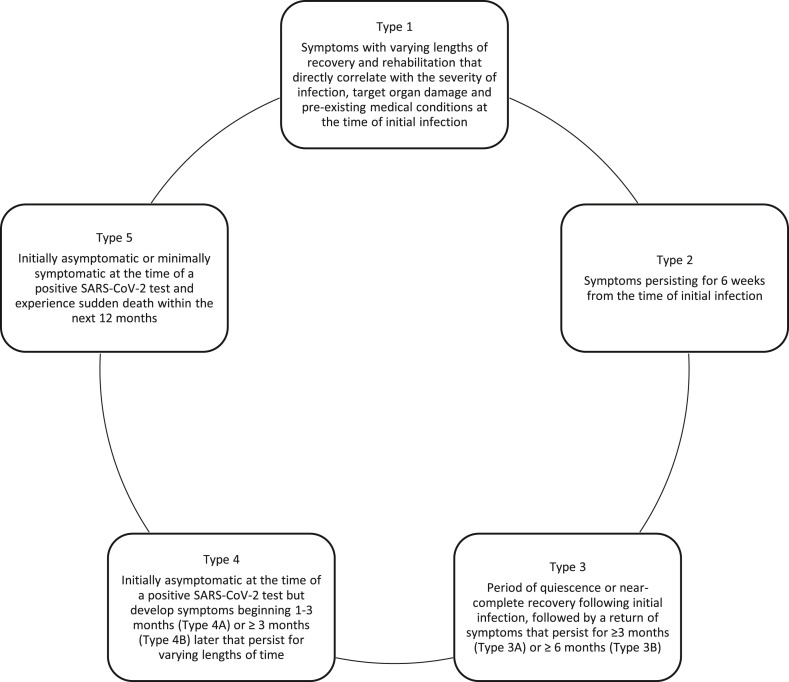
The acute phase of COVID-19, characterised based on symptoms severity as: asymptomatic, mild, moderate, severe, and critical has been well described [27]. The early-stage clinical examination or specific diagnostic criteria for post-COVID syndrome is still unclear and the persistence of symptoms fluctuates. Furthermore, the heterogeneity of long COVID makes it challenging to characterise specific subdivisions of the condition. Long COVID may be classified into four syndromes: post-intensive care syndrome, post-viral fatigue syndrome, permanent organ damage, and long-term COVID syndrome.28 Alternatively, Yong and Liu, based on the literature, suggested six post COVID syndrome subsets including: non-severe COVID-19 multiorgan sequelae (NSC-MOS), pulmonary fibrosis sequelae (PFS), myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), postural orthostatic tachycardia syndrome (POTS), post intensive care syndrome (PICS), and medical or clinical sequelae (MCS) (Fig. 1 ).29 Furthermore, Becker developed five classifications of long COVID based on the initial symptoms, their period, inactivation duration, and onset (Fig. 2 ).30 Finally, Boix and Merino, from their practical perspective, sorted long COVID into five types: post-acute COVID body organ impairment sequelae, post-COVID derived from the hospitalisation itself (post-ICU syndrome), decompensation of previous chronic diseases, onset of a new disease triggered by COVID-19, and pharmacological toxicity from COVID-19 treatment.31
Figure 1.
Long COVID subtypes (adapted from Yong SJ, Liu S, 2021).29
Figure 2.
Alternative classification of long COVID subtypes (adapted from Becker RC, 2021).30
Symptoms of long COVID
The duration of COVID-19 recovery is highly variable; some individuals will take only a couple of days, whereas others may take up to 12 weeks for a full recovery. Ongoing symptoms lasting over 12 weeks after positive COVID-19 testing is considered long COVID.25 , 32 In general, symptoms are associated with reductions in the quality of daily life and may involve multisystem manifestations or present as a single symptom.33 , 34 Many low-risk individuals with mild COVID-19 have been shown to present with diverse long-term symptoms with subsequent disruption of work, social, and home life.35 Therefore, patients understandably wish to adapt or treat any remaining symptoms that cause difficulty in daily life to eventually reach a stage of full recovery.
The pathological and mechanistic basis behind the persistence of long COVID symptoms has not yet been determined. However, proposed hypotheses include an ongoing healing process (the convalescent phase) after organ damage from the acute phase,36 an autoimmune response,37 ongoing infection, mini infection,38 or post-intensive care syndrome.39 It is suggested that COVID develops a cytotoxic memory immune T cell that affects the autoimmune response.40 Another cause of long COVID may be that the immune system does not attack the virus, in cases where COVID-19 is replicated in a protected anatomical location, such as the central nervous system (CNS) or the gut-associated lymphoid tissue (GALT).40 This was demonstrated by the remnants of SARS-CoV-2-RNA on the faecal samples post-acute phase,41 which resulted in long COVID effects. It is difficult to determine the pathophysiological mechanism behind long COVID without further cohort investigations.
Whilst there has been much focus on the symptoms of long COVID using different methods, evidence based on diagnostic imaging reports revealed biological changes in long COVID that could explain some of the symptoms experienced by patients. Therefore, it is important to explore symptoms of long COVID and the various imaging modalities involved in its management to plan strategies to address the demand.
Cardiovascular symptoms in long COVID
The formation of microclots and other cardiovascular conditions have been identified in people with long COVID. Pre-existing cardiovascular disease was highlighted early as a risk factor for having severe COVID-19 symptoms, with an increased risk of hospitalisation and mortality.42 COVID-19 infection may exacerbate cardiovascular disease, causing dysfunction, coagulopathies and thrombocytopenia, hypercoagulation, pulmonary intravascular coagulation, microangiopathy, venous thromboembolism or arterial thrombosis, myocardial injury, acute coronary syndromes (ACS), cardiomyopathy, acute cor pulmonale, arrhythmias, and cardiogenic shock.43 , 44 For those with no pre-existing disease, long COVID may be present with a cardiovascular disorder. The exact aetiopathogenesis is unknown, although the leading hypothesis includes this being a result of persistent SARS-CoV-2 infection in immune-privileged tissue triggering persistent inflammation and micro-emboli that block micro-capillary and prohibit oxygen exchange, eventually leading to tissue hypoxia.44 The immune system may aggressively respond to COVID-19 through the cardiopulmonary system both directly and indirectly. Vessel inflammation may lead to thromboembolism development, affecting vital organs function as it circulates through the bloodstream.45 One study investigating ongoing breathlessness symptoms using XeMRI for discharged patients with long COVID found that the symptoms were caused by alveolar-capillary thrombosis. They reported alveolar capillary diffusion limitation in all of the nine participants despite normal or relatively normal CT results.46 Further, a study using [18F] FDG-PET/CT on 13 adults with long COVID showed signs of brain hypometabolism. There was also poor metabolism in some areas related to long COVID symptoms, such as anosmia/ageusia, fatigue, and vascular uptake, and several participants still had lung abnormalities.47 FDG PET scans in three long COVID patients with brain fog showed an association with the brainstem, with hypometabolic conditions particularly at the pons.48
Respiratory symptoms in long COVID
The epithelium in the respiratory tract is the front-line of the COVID-19 infection following inhalation of the virus.49 Respiratory symptoms and severity following a COVID-19 infection are broad with mild upper respiratory tract symptoms such as a sore throat and cough regularly reported.50 However, patients can develop more severe illness, commonly viral pneumonia, which can result in acute respiratory disorder syndrome (ARDS), which requires intense treatment and is linked to poor patient outcomes and/or mortality.51 Whilst data on the short-term respiratory sequelae is still emerging, and longer-term follow-up studies remain scarce; 1370 pulmonary CT scans of 188 SARS-CoV2 patients identified the presence of pleural effusion, which was linked to increased risk of cardio-respiratory complications and hospital mortality.52 Interstitial lung disease has been demonstrated in patients post COVID-19 infection and it is probable that with such prevalent infections in the UK, an increasing burden will be placed on Computed Tomography (CT) services for diagnosis and monitoring of this disease.53 Wells et al. recommend longer-term follow-up of patients at or beyond a year to determine whether CT abnormalities regress or persist.54 In this regard, it may be important to distinguish between post-ARDS abnormalities (including ventilator-induced injury) and auto-inflammatory and/or autoimmune pathways triggered by COVID-19, perhaps giving rise to progressive fibrotic lung disease in a small minority of patients. Whilst there is a need for more detailed investigations and longitudinal cohort analysis, the presence of pulmonary effusion in hospitalised patients might serve as a clinical indicator to COVID-19 severity and post-COVID-19 outcomes. There is also evidence that the acute effects of COVID-19 leads to reduced pulmonary diffusing capacity55 which is largely related to increased disease severity, with abnormally low pulmonary diffusing capacity55 (<80% predicted) reported in ∼60% of patients with severe disease, ∼32% in moderate disease and ∼20% in mild disease.56 COVID-19 has little impact on spirometry measures, with lung volumes close to normative values, particularly in those with milder disease.57 Arguably one of the most reported symptoms 3 months post-infection is chronic dyspnoea, with some data highlighting this as a key symptom in over half of the patients.50 Chronic dyspnoea is associated with greater restriction on spirometry, lower pulmonary diffusing capacity,55 reduced functional status, and greater desaturation during exertion than those without persistent dyspnoea,58 suggestive of an underlying physiological mechanism that is responsible for this. Whilst the details of this have yet to be determined, early suggestions attribute pulmonary emboli59 and potential vagus nerve dysfunction as possible explanations for various systemic symptoms, however more mechanistic insight is required.
Musculoskeletal (MSK) symptoms in long COVID
Though studies have identified MSK-related conditions associated with long COVID, this aspect remains unclear. An early paper identified “profound fatigue” as a common symptom in many patients with long COVID60 and fatigue is the most common self-reported symptom of long COVID.61 Furthermore, studies of MSK-related long COVID symptoms have reported fatigue as one of the main manifestations, followed by myalgia and arthralgia, which are as ambiguous as other long COVID symptoms.62, 63, 64, 65 These symptoms may result from inflammatory,66 neurological67 and psychological68 factors, or from the negative impact of extended lockdown associated with the COVID-19 pandemic.69
Other infrequent MSK related signs and symptoms of long COVID include bone density reduction and muscle weakness. These may be in part caused by the sedentary condition and limited mobility imposed by quarantine measures. The long lockdown period that the COVID pandemic forced into countries led to people staying indoors with functional limitations and reduced exposure to sunlight. Similar to astronauts, who suffer from a reduction in bone mass on the weight-bearing bones,70 certain at-risk individuals may have experienced similar conditions during the COVID pandemic, leading to bone turnover system disruptions and systemic osteoporosis.71 , 72 Indeed, many investigations have studied the effect of physical activity reduction on the function of bone and muscle,73 and in patients with total knee replacement74 and stroke75 showing low muscle mass and increased bone loss with slow recovery even after one year.76 Moreover, a study in hamsters found that SARS-CoV-2 disturbs bone turnover.77 This bone mechanism disruption may be expected due to the systemic inflammation caused by the cytokine storm.78 Bone mineral density did not attract that much attention during that pandemic, other than it may be a dangerous severity indicator for COVID patients if it is low.79 In addition, the use of corticosteroids as COVID therapy80 may affect the balance of bone density, and resulting in bone loss and an increased chance of fracture.81
Likewise, myalgia or joint pain have been recorded with other MSK symptoms. A study found that almost two in every five long COVID patients report extensive spreading pain in joints and muscles,62 likely induced by the acute COVID phase,82 in which it has been reported that 15% of patients experience arthralgia,83 and 19% experience myalgia.84 However, 45% of post-hospitalised patients with long COVID will experience generalised muscle pain, frequently at the lower extremity.85 Some studies have reported MSK-related biological changes, which could explain some of the symptoms. A recent review showed one study found an association between MSK related COVID-19 symptoms and imaging hematoma, nerves injuries, thickening, and compression, muscle oedema and myositis, multi-joint rheumatoid arthritis, synovitis and other findings,86 which may be linked with the post COVID syndrome theme. Furthermore, CT findings on COVID patients at 24 h and 20 days following ICU admission show a loss of lean body mass,87 which has been linked with fatigue and reduced neuromuscular function.88 In addition, utilising dual-energy X-ray (DXA) may provide further information regarding bone mineral density in long COVID,89 and MSK ultrasound can determine abnormal articular changes in long COVID.90
Current diagnosis of long COVID and the impact on imaging services
The current understanding of long COVID is still developing. The health sector is supposed to be in a post-pandemic recovery period following the COVID-19 overload, as elective medical procedures were postponed during the pandemic. Additionally, the number of long COVID patients is increasing, and they require reliable clinical, imaging and laboratory biomarkers to diagnose and monitor their disease and any future treatments. The multidisciplinary community needs more studies to help better understand the mechanisms underlying multiorgan persistent symptoms of COVID-19. The Health-Related Quality of Life (HRQOL) EQ-5D-5L questionnaire with visual analogue scale,91 , 92 and the Newcastle post-COVID syndrome follow-up screening questionnaire,93 have been utilised in some studies. Significantly, the COVID-19 Yorkshire Rehabilitation Scale C19-YRS was developed to assess the severity of long COVID-19 symptoms during screening, aligning with The International Classification of Functioning of the WHO,94 and recommended by the NHS Clinical Guidance.91 These techniques were used to help triage suspected long COVID patients, were key tools in initial studies investigating ongoing COVID symptoms and are trusted as part of the initial clinical examination for long COVID.
The NHS has already committed £145 million, establishing more than 80 long COVID assessment clinics around the nation,95 however, this still equates to less than £100 per person. These clinics primarily act as an investigation hub (to exclude alternative diagnoses) and then signpost people to existing services.96
Several protocols and guidelines have been proposed throughout the literature. One suggested diagnostic algorithm indicates that there should be three successive primary care visits to cover long COVID, which encompasses both ongoing and post-COVID syndrome, starting from COVID-19 diagnosis. The purpose of the initial visit aims to gather patient medical history, COVID-19 screening, complete physical examination, lab tests and complementary tests. After the initial assessment, when alternative diagnoses are considered, it is recommended to schedule the second visit between 8 and 10 weeks. Finally, to determine any further symptom development, the third appointment is recommended between weeks 12–14.97 In cases of post-hospitalisation COVID-19 survival with lung complications, a 4-week post-discharge phone call check is recommended, followed by a 12-week clinic appointment assessment accompanied by a number of standardised tests. If any of the results were abnormal, more advanced tests would be performed, such as a chest X-ray, chest CT or CT angiography.98 NICE guidelines recommend a holistic assessment that focuses on the overall health of the patient, requesting tests deemed necessary for physical, psychological, social and spiritual wellbeing.20 In cases of long COVID, a chest X-ray may be required with another medical test34 , 99 especially with 12-week post-positive COVID-19 pneumonia, or ongoing respiratory symptoms.100 , 101 Specific medical imaging scans are also recommended for dealing with long COVID patients based on symptoms, body system or sequelae (Table 1 ).97 , 102
Table 1.
Imaging recommendation for long COVID patients (adapted from Sisó-Almirall et al. and Riccardo Cau et al.).97,102
| Imaging modality | Imaging test | Evaluation | System/symptoms/sequelae |
|---|---|---|---|
| X-ray | Chest X-ray |
|
Pulmonary |
| CT | Chest high resolution CT or angio-CT |
|
Pulmonary Cardiac |
| CT Abdomen |
|
Abdominal | |
| CT Brain |
|
Neurological | |
| MRI | Cardiac MRI/CMR |
|
Pulmonary Cardiac |
| Brain MRI |
|
Neurological | |
| Hepatic/Pancreatic MRI |
|
Abdominal | |
| Ultrasound | Joint ultrasound |
|
Musculoskeletal |
| Abdominal ultrasound |
|
Abdominal | |
| Duplex ultrasound |
|
Vascular | |
| Lung ultrasound |
|
Pulmonary | |
| Chest ultrasound |
|
Pulmonary | |
| Echocardiography |
|
Cardiac |
During the pandemic, unprecedented delays in patients attending routine screening appointments have been seen. An additional estimated 2 million people suffer from long COVID, a number likely to grow with further infections and repeat infections. Radiology departments will face a significant amount of catching-up; they will need to account for this increased workload in their plans. In addition, there will be potential for trials tackling the need for imaging to help clinical differential diagnoses and follow-up patients. Strengthen research training by the field experts and increase research radiographer roles within the departments, which is more weight than adding to a sort of managers trying to get those signing rolls to facilitate. Likewise, it is important for radiography educators to include long COVID in their curricula to know the presentation and justification of imaging in patients presenting with long COVID. As the evidence base evolves, protocols for imaging and monitoring will need to be developed and as therapeutics enter the market, imaging is likely to play an integral part in evaluating the efficacy and longer term effectiveness of these treatments. It is also possible that imaging may play a role in identifying candidates for appropriate therapeutic intervention in the future.
Conclusion
The COVID-19 pandemic has significantly affected the world over the past 2 years, but its impact will be felt for longer in patients with long COVID. Healthcare communities and governments have gained support for research on long COVID. Therefore, there is an opportunity to investigate the causes of these persistent symptoms and methods to cure or avert them. The percentage of people suffering from long COVID is growing, and action is needed. The full impact of long COVID on imaging services is yet to be realised, but there is likely to be significant increased demand for imaging, particularly in CT for the assessment of lung disease. Educators will need to include aspects related to long COVID pathophysiology and imaging presentations in curricula, underpinned by the rapidly evolving evidence base.
Conflict of interest statement
The authors have no conflict of interest to declare.
References
- 1.Li J., Long X., Wang X., Fang F., Lv X., Zhang D., et al. Radiology indispensable for tracking COVID-19. Diagn Interv Imaging. 2021;102:69–75. doi: 10.1016/j.diii.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cozzi A., Schiaffino S., Arpaia F., Della Pepa G., Tritella S., Bertolotti P., et al. Chest x-ray in the COVID-19 pandemic: radiologists' real-world reader performance. Eur J Radiol. 2020;132 doi: 10.1016/j.ejrad.2020.109272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang S., Zhang Y., Shen J., Dai Y., Ling Y., Lu H., et al. Clinical potential of UTE-MRI for assessing COVID-19: patient-and lesion-based comparative analysis. J Magn Reson Imaging. 2020;52:397–406. doi: 10.1002/jmri.27208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peng S.M., Yang K.C., Chan W.P., Wang Y.W., Lin L.J., Yen A.M.F., et al. Impact of the COVID-19 pandemic on a population-based breast cancer screening program. Cancer. 2020;126:5202–5205. doi: 10.1002/cncr.33180. [DOI] [PubMed] [Google Scholar]
- 5.DeGroff A., Miller J., Sharma K., Sun J., Helsel W., Kammerer W., et al. COVID-19 impact on screening test volume through the National Breast and Cervical Cancer early detection program, January–June 2020, in the United States. Prev Med. 2021;151 doi: 10.1016/j.ypmed.2021.106559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eijkelboom A.H., de Munck L., Lobbes M.B., van Gils C.H., Wesseling J., Westenend P.J., et al. Impact of the suspension and restart of the Dutch breast cancer screening program on breast cancer incidence and stage during the COVID-19 pandemic. Prev Med. 2021;151 doi: 10.1016/j.ypmed.2021.106602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leite H., Lindsay C., Kumar M. COVID-19 outbreak: implications on healthcare operations. TQM J. 2020;33(1):247–256. doi: 10.1108/TQM-05-2020-0111. [DOI] [Google Scholar]
- 8.National Health Service England NHS Improvement . NHS; 2019. NHS diagnostic waiting times and activity data. [Google Scholar]
- 9.Thakur V., Bhola S., Thakur P., Patel S.K.S., Kulshrestha S., Ratho R.K., et al. Waves and variants of SARS-CoV-2: understanding the causes and effect of the COVID-19 catastrophe. Infection. 2021:1–16. doi: 10.1007/s15010-021-01734-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burki T.K. Omicron variant and booster COVID-19 vaccines. Lancet Respir Med. 2022;10:e17. doi: 10.1016/S2213-2600(21)00559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Health Service Coronavirus (COVID-19) vaccine for people with a severely weakened immune system. 2022. https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/coronavirus-vaccine-people-with-severely-weakened-immune-system/ [Online]. Available:
- 12.Mahase E. Covid-19: what do we know about “long covid”? BMJ. 2020;370:m2815. doi: 10.1136/bmj.m2815. [DOI] [PubMed] [Google Scholar]
- 13.Garg M., Maralakunte M., Garg S., Dhooria S., Sehgal I., Bhalla A.S., et al. The conundrum of ‘long-COVID-19’: a narrative review. Int J Gen Med. 2021;14:2491–2506. doi: 10.2147/IJGM.S316708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Callard F., Perego E. How and why patients made long Covid. Soc Sci Med. 2021;268 doi: 10.1016/j.socscimed.2020.113426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Office for National Statistics Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 7 July 2022. 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/7july2022 [Online]. Available:
- 16.NICE . National Institute of Health Care Excellence; 2020. COVID-19 rapid guideline: managing the long-term effects of COVID-19 NICE guideline [NG188] [PubMed] [Google Scholar]
- 17.U.S. Department of Health & Human Services Guidance on “long COVID” as a disability under the ADA, section 504, and section 1557. 2021. https://www.hhs.gov/civil-rights/for-providers/civil-rights-covid19/guidance-long-covid-disability/index.html#footnote10_0ac8mdc [Online]. Available:
- 18.Centers for Disease Control and Prevention New ICD-10-CM code for post-COVID conditions, following the 2019 novel coronavirus (COVID-19) 2021. https://www.cdc.gov/nchs/icd/icd10cm.htm [Online]. Available:
- 19.Centers for Disease Control and Prevention . 2021. Post-COVID conditions. [Online] [Google Scholar]
- 20.National Institute for Health and Care Excellence COVID-19 rapid guideline: managing the longterm effects of COVID-19. 2021. https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742 [Online]. Available: [PubMed]
- 21.Office for National Statistics Self-reported long COVID after two doses of a coronavirus (COVID-19) vaccine in the UK: 26 January 2022. 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/selfreportedlongcovidaftertwodosesofacoronaviruscovid19vaccineintheuk/26january2022 [Online]. Available:
- 22.Huang C., Huang L., Wang Y., Li X., Ren L., Gu X., et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weerahandi H., Hochman K.A., Simon E., Blaum C., Chodosh J., Duan E., et al. Post-discharge health status and symptoms in patients with severe COVID-19. J Gen Intern Med. 2021;36:738–745. doi: 10.1007/s11606-020-06338-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blomberg B., Mohn K.G., Brokstad K.A., Zhou F., Linchausen D.W., Hansen B.A., et al. Long COVID in a prospective cohort of home-isolated patients. Nat Med. 2021;27:1607–1613. doi: 10.1038/s41591-021-01433-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evans R.A., Leavy O.C., Richardson M., Elneima O., McAuley H.J., Shikotra A., et al. medRxiv; 2021. Clinical characteristics with inflammation profiling of Long-COVID and association with one-year recovery following hospitalisation in the UK: a prospective observational study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garrigues E., Janvier P., Kherabi Y., Le Bot A., Hamon A., Gouze H., et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020;81:e4–e6. doi: 10.1016/j.jinf.2020.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Solve M.E. Long COVID: nearly 7% of U.S. Adults suffering symptoms; personal financial burden estimated at $386 billion. 2022. https://www.prnewswire.com/news-releases/long-covid-nearly-7-of-us-adults-suffering-symptoms-personal-financial-burden--estimated-at-386-billion-301517095.html [Online]. Available:
- 28.National Institute for Health Research Living with Covid19. A dynamic review of the evidence around ongoing Covid19 symptoms (often called Long Covid) 2020. https://evidence.nihr.ac.uk/themedreview/living-with-covid19/ [Online]. Available:
- 29.Yong S.J., Liu S. Proposed subtypes of post-COVID-19 syndrome (or long-COVID) and their respective potential therapies. Rev Med Virol. 2021:e2315. doi: 10.1002/rmv.2315. [DOI] [PubMed] [Google Scholar]
- 30.Becker R.C. Springer; 2021. COVID-19 and its sequelae: a platform for optimal patient care, discovery and training. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boix V., Merino E. Post-COVID syndrome. The never ending challenge. Med Clin. 2022;158:178–180. doi: 10.1016/j.medcle.2021.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raveendran A., Jayadevan R., Sashidharan S. Long COVID: an overview. Diabetes Metabol Syndr Clin Res Rev. 2021;15:869–875. doi: 10.1016/j.dsx.2022.102660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hayes L.D., Ingram J., Sculthorpe N.F. More than 100 persistent symptoms of SARS-CoV-2 (long COVID): a scoping review. Front Med. 2021;2028 doi: 10.3389/fmed.2021.750378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Health Service Long-term effects of coronavirus (long COVID) https://www.nhs.uk/conditions/coronavirus-covid-19/long-term-effects-of-coronavirus-long-covid/ [Online]. Available:
- 35.Havervall S., Rosell A., Phillipson M., Mangsbo S.M., Nilsson P., Hober S., et al. Symptoms and functional impairment assessed 8 Months after mild COVID-19 among health care workers. JAMA. 2021;325:2015–2016. doi: 10.1001/jama.2021.5612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pierce J.D., Shen Q., Cintron S.A., Hiebert J.B. Post-COVID-19 syndrome. Nurs Res. 2022;71:164–174. doi: 10.1097/NNR.0000000000000565. [DOI] [PubMed] [Google Scholar]
- 37.Tay M.Z., Poh C.M., Rénia L., MacAry P.A., Ng L.F. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tehrani H.A., Darnahal M., Nadji S.A., Haghighi S. COVID-19 re-infection or persistent infection in patient with acute myeloid leukaemia M3: a mini review. New Microbes New infect. 2021;39 doi: 10.1016/j.nmni.2020.100830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stam H., Stucki G., Bickenbach J. Covid-19 and post intensive care syndrome: a call for action. J Rehabil Med. 2020;52(4):1–4. doi: 10.2340/16501977-2677. [DOI] [PubMed] [Google Scholar]
- 40.Galán M., Vigón L., Fuertes D., Murciano-Antón M.A., Casado G., Domínguez-Mateos S., et al. Persistent overactive cytotoxic immune response in a Spanish cohort of individuals with Long-COVID: Identification of diagnostic biomarkers. Front Immunol. 2022;13:1129. doi: 10.3389/fimmu.2022.848886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Arostegui D., Castro K., Schwarz S., Vaidy K., Rabinowitz S., Wallach T. Persistent SARS-CoV-2 nucleocapsid protein presence in the intestinal epithelium of a pediatric patient 3 months after acute infection. JPGN Rep. 2022;3:e152. doi: 10.1097/PG9.0000000000000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 43.Gupta A., Madhavan M.V., Sehgal K., Nair N., Mahajan S., Sehrawat T.S., et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26:1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PubMed] [Google Scholar]
- 44.Pretorius E., Vlok M., Venter C., Bezuidenhout J.A., Laubscher G.J., Steenkamp J., et al. Persistent clotting protein pathology in long COVID/post-acute sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc Diabetol. 2021;20:1–18. doi: 10.1186/s12933-021-01359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Silva Andrade B., Siqueira S., de Assis Soares W.R., de Souza Rangel F., Santos N.O., dos Santos Freitas A., et al. Long-COVID and post-COVID health complications: an up-to-date review on clinical conditions and their possible molecular mechanisms. Viruses. 2021;13:700. doi: 10.3390/v13040700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grist J.T., Chen M., Collier G.J., Raman B., AbuEid G., McIntyre A., et al. Hyperpolarized 129Xe MRI abnormalities in dyspneic patients 3 Months after COVID-19 pneumonia: preliminary results. Radiology. 2021;301:E353–E360. doi: 10.1148/radiol.2021210033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sollini M., Morbelli S., Ciccarelli M., Cecconi M., Aghemo A., Morelli P., et al. Long COVID hallmarks on [18F] FDG-PET/CT: a case-control study. Eur J Nucl Med Mol Imaging. 2021;48:3187–3197. doi: 10.1007/s00259-021-05294-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jacques Hugon M.Q., Sanchez Ortiz Marta, Flore Msika Eva, Farid Karim, Paquet Claire. Cognitive decline and brainstem hypometabolism in long COVID: a case series. Brain Behav. 2022;12(4):1–5. doi: 10.1002/brb3.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brosnahan S.B., Jonkman A.H., Kugler M.C., Munger J.S., Kaufman D.A. COVID-19 and respiratory system disorders: current knowledge, future clinical and translational research questions. Arterioscler Thromb Vasc Biol. 2020;40:2586–2597. doi: 10.1161/ATVBAHA.120.314515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Faghy M.A., Maden-Wilkinson T., Arena R., Copeland R.J., Owen R., Hodgkins H., et al. COVID-19 patients require multi-disciplinary rehabilitation approaches to address persisting symptom profiles and restore pre-COVID quality of life. Expet Rev Respir Med. 2022;16:1–6. doi: 10.1080/17476348.2022.2063843. [DOI] [PubMed] [Google Scholar]
- 51.Wang F., Kream R.M., Stefano G.B. Long-term respiratory and neurological sequelae of COVID-19. Med Sci Monit. 2020;26 doi: 10.12659/MSM.928996. e928996-928991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cereda A., Toselli M., Palmisano A., Leone R., Vignale D., Nicoletti V., et al. Is pleural effusion in COVID-19 interstitial pneumonia related to in-hospital mortality? Ital J Med. 2021;15 [Google Scholar]
- 53.Eapen M.S., Lu W., Gaikwad A.V., Bhattarai P., Chia C., Hardikar A., et al. Endothelial to mesenchymal transition: a precursor to post-COVID-19 interstitial pulmonary fibrosis and vascular obliteration? Eur Respir J. 2020;56 doi: 10.1183/13993003.03167-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wells A.U., Devaraj A., Desai S.R. Radiological Society of North America; 2021. Interstitial lung disease after COVID-19 infection: a catalog of uncertainties. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barisione G., Brusasco V. Lung diffusing capacity for nitric oxide and carbon monoxide following mild-to-severe COVID-19. Physiol Rep. 2021;9 doi: 10.14814/phy2.14748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thomas M., Price O.J., Hull J.H. Pulmonary function and COVID-19. Curr Opin Physiol. 2021;21:29–35. doi: 10.1016/j.cophys.2021.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Froidure A., Mahsouli A., Liistro G., De Greef J., Belkhir L., Gérard L., et al. Integrative respiratory follow-up of severe COVID-19 reveals common functional and lung imaging sequelae. Respir Med. 2021;181 doi: 10.1016/j.rmed.2021.106383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cortés-Telles A., López-Romero S., Figueroa-Hurtado E., Pou-Aguilar Y.N., Wong A.W., Milne K.M., et al. Pulmonary function and functional capacity in COVID-19 survivors with persistent dyspnoea. Respir Physiol Neurobiol. 2021;288 doi: 10.1016/j.resp.2021.103644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Timurkaan M., Altuntas G., Kalayci M., Timurkaan E.S., Ayyildiz H. Early warning triad for pulmonary microemboli in COVID-19 pneumonia: pulmonary artery diameter, D-dimer and NT-proBNP. Medicine. 2022;11:775–779. [Google Scholar]
- 60.Nabavi N. Long covid: how to define it and how to manage it. BMJ. 2020;370:m3489. doi: 10.1136/bmj.m3489. [DOI] [PubMed] [Google Scholar]
- 61.Sykes D.L., Holdsworth L., Jawad N., Gunasekera P., Morice A.H., Crooks M.G. Post-COVID-19 symptom burden: what is long-COVID and how should we manage it? Lung. 2021;199:113–119. doi: 10.1007/s00408-021-00423-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Karaarslan F., Guneri F.D., Kardes S. Long COVID: rheumatologic/musculoskeletal symptoms in hospitalized COVID-19 survivors at 3 and 6 months. Clin Rheumatol. 2022;41:289–296. doi: 10.1007/s10067-021-05942-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Peghin M., Palese A., Venturini M., De Martino M., Gerussi V., Graziano E., et al. Post-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin Microbiol Infect. 2021;27:1507–1513. doi: 10.1016/j.cmi.2021.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ghosn J., Piroth L., Epaulard O., Le Turnier P., Mentré F., Bachelet D., et al. Persistent COVID-19 symptoms are highly prevalent 6 months after hospitalization: results from a large prospective cohort. Clin Microbiol Infect. 2021;27:1041. doi: 10.1016/j.cmi.2021.03.012. 1041.e1-1041.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vaishya R., Jain V.K., Iyengar K.P. Musculoskeletal manifestations of COVID-19. J Clin Orthop Trauma. 2021;17:280–281. doi: 10.1016/j.jcot.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Guedj E., Million M., Dudouet P., Tissot-Dupont H., Bregeon F., Cammilleri S., et al. 18F-FDG brain PET hypometabolism in post-SARS-CoV-2 infection: substrate for persistent/delayed disorders? Eur J Nucl Med Mol Imaging. 2021;48:592–595. doi: 10.1007/s00259-020-04973-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wostyn P. COVID-19 and chronic fatigue syndrome: is the worst yet to come? Med Hypotheses. 2021;146 doi: 10.1016/j.mehy.2020.110469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ahmed S., Akter R., Islam M.J., Muthalib A.A., Sadia A.A. Impact of lockdown on musculoskeletal health due to COVID-19 outbreak in Bangladesh: a cross sectional survey study. Heliyon. 2021;7 doi: 10.1016/j.heliyon.2021.e07335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Collet P., Uebelhart D., Vico L., Moro L., Hartmann D., Roth M., et al. Effects of 1-and 6-month spaceflight on bone mass and biochemistry in two humans. Bone. 1997;20:547–551. doi: 10.1016/s8756-3282(97)00052-5. [DOI] [PubMed] [Google Scholar]
- 71.Iwamoto J., Takeda T., Sato Y. Interventions to prevent bone loss in astronauts during space flight. Keio J Med. 2005;54:55–59. doi: 10.2302/kjm.54.55. [DOI] [PubMed] [Google Scholar]
- 72.Sibonga J.D., Spector E.R., Johnston S.L., Tarver W.J. Evaluating bone loss in ISS astronauts. Aerosp Med Hum Perform. 2015;86:A38–A44. doi: 10.3357/AMHP.EC06.2015. [DOI] [PubMed] [Google Scholar]
- 73.Knapp K.M., Rowlands A.V., Welsman J.R., MacLeod K.M. Prolonged unilateral disuse osteopenia 14 years post external fixator removal: a case history and critical review. Case Rep Med. 2010;2010 doi: 10.1155/2010/629020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gundry M., Hopkins S., Knapp K. A review on bone mineral density loss in total knee replacements leading to increased fracture risk. Clin Rev Bone Miner Metabol. 2017;15:162–174. doi: 10.1007/s12018-017-9238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Poole K.E., Warburton E.A., Reeve J. Rapid long-term bone loss following stroke in a man with osteoporosis and atherosclerosis. Osteoporos Int. 2005;16:302–305. doi: 10.1007/s00198-004-1682-6. [DOI] [PubMed] [Google Scholar]
- 76.Hopkins S., Toms A., Brown M., Welsman J., Ukoumunne O., Knapp K. A study investigating short-and medium-term effects on function, bone mineral density and lean tissue mass post-total knee replacement in a Caucasian female post-menopausal population: implications for hip fracture risk. Osteoporos Int. 2016;27:2567–2576. doi: 10.1007/s00198-016-3546-2. [DOI] [PubMed] [Google Scholar]
- 77.Qiao W., Lau H.E., Xie H., Poon V.K.M., Chan C.C.S., Chu H., et al. SARS-CoV-2 infection induces inflammatory bone loss in golden Syrian hamsters. Nat Commun. 2022;13(1):1–16. doi: 10.1038/s41467-022-30195-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tao H., Ge G., Li W., Liang X., Wang H., Li N., et al. Dysimmunity and inflammatory storm: watch out for bone lesions in COVID-19 infection. Med Hypotheses. 2020;145 doi: 10.1016/j.mehy.2020.110332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kottlors J., Hokamp N.G., Fervers P., Bremm J., Fichter F., Persigehl T., et al. Early extrapulmonary prognostic features in chest computed tomography in COVID-19 pneumonia: bone mineral density is a relevant predictor for the clinical outcome – a multicenter feasibility study. Bone. 2021;144 doi: 10.1016/j.bone.2020.115790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Buckley L., Humphrey M.B. Glucocorticoid-induced osteoporosis. N Engl J Med. 2018;379:2547–2556. doi: 10.1056/NEJMcp1800214. [DOI] [PubMed] [Google Scholar]
- 81.Tang J. What can we learn about corticosteroid therapy as a treatment for COVID-19? Osteoporos Int. 2020;vol. 31 doi: 10.1007/s00198-020-05487-w. 1595-1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Baimukhamedov C., Barskova T., Matucci-Cerinic M. Arthritis after SARS-CoV-2 infection. Lancet Rheumatol. 2021;3:e324–e325. doi: 10.1016/S2665-9913(21)00067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mukarram M.S., Ishaq Ghauri M., Sethar S., Afsar N., Riaz A., Ishaq K. COVID-19: an emerging culprit of inflammatory arthritis. Case Rep Rheumatol. 2021;2021 doi: 10.1155/2021/6610340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Abdullahi A., Candan S.A., Abba M.A., Bello A.H., Alshehri M.A., Afamefuna Victor E., et al. Neurological and musculoskeletal features of COVID-19: a systematic review and meta-analysis. Front Neurol. 2020;687 doi: 10.3389/fneur.2020.00687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fernandez-de-Las-Penas C., de-la-Llave-Rincon A.I., Ortega-Santiago R., Ambite-Quesada S., Gomez-Mayordomo V., Cuadrado M.L., et al. Prevalence and risk factors of musculoskeletal pain symptoms as long-term post-COVID sequelae in hospitalized COVID-19 survivors: a multicenter study. Pain. 2021;163(9):e989–e996. doi: 10.1097/j.pain.0000000000002564. [DOI] [PubMed] [Google Scholar]
- 86.Ramani S.L., Samet J., Franz C.K., Hsieh C., Nguyen C.V., Horbinski C., et al. Musculoskeletal involvement of COVID-19: review of imaging. Skeletal Radiol. 2021;50:1763–1773. doi: 10.1007/s00256-021-03734-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gualtieri P., Falcone C., Romano L., Macheda S., Correale P., Arciello P., et al. Body composition findings by computed tomography in SARS-CoV-2 patients: increased risk of muscle wasting in obesity. Int J Mol Sci. 2020;21:4670. doi: 10.3390/ijms21134670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Willoughby D., Hewlings S., Kalman D. Body composition changes in weight loss: strategies and supplementation for maintaining lean body mass, a brief review. Nutrients. 2018;10:1876. doi: 10.3390/nu10121876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Knapp K. Dual energy X-ray absorptiometry: beyond bone mineral density. Imaging Ther Pract. 2015;5 [Google Scholar]
- 90.Backhaus T.M., Ohrndorf S., Kellner H., Strunk J., Hartung W., Sattler H., et al. The US7 score is sensitive to change in a large cohort of patients with rheumatoid arthritis over 12 months of therapy. Ann Rheum Dis. 2013;72:1163–1169. doi: 10.1136/annrheumdis-2012-201397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.National Health Service England and NHS Improvement coronavirus National Guidance for post-COVID syndrome assessment clinics. 2021. https://www.england.nhs.uk/coronavirus/documents/national-guidance-for-post-covid-syndrome-assessment-clinics/ [Online]. 2022. Available: [accessed March, 22]
- 92.Han J.H., Womack K.N., Tenforde M.W., Files D.C., Gibbs K.W., Shapiro N.I., et al. Associations between persistent symptoms after mild COVID-19 and long-term health status, quality of life, and psychological distress. Influenza Other Respir Viruses. 2022;16(4):680–689. doi: 10.1111/irv.12980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Alkodaymi M.S., Omrani O.A., Fawzy N.A., Abou Shaar B., Almamlouk R., Riaz M., et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect. 2022;28(5):657–666. doi: 10.1016/j.cmi.2022.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sivan M., Halpin S., Gee J. Assessing long-term rehabilitation needs in COVID-19 survivors using a telephone screening tool (C19-YRS tool) Adv Clin Neurosci Rehabil. 2020;19:14–17. [Google Scholar]
- 95.Baraniuk C. Covid-19: how Europe is approaching long covid. BMJ. 2022:376. doi: 10.1136/bmj.o158. [DOI] [PubMed] [Google Scholar]
- 96.National Health Service Long COVID patients to get help at more than 60 clinics. 2020. https://www.england.nhs.uk/2020/12/long-covid-patients-to-get-help-at-more-than-60-clinics/ [Online]. Available:
- 97.Sisó-Almirall A., Brito-Zerón P., Conangla Ferrín L., Kostov B., Moragas Moreno A., Mestres J., et al. Long Covid-19: proposed primary care clinical guidelines for diagnosis and disease management. Int J Environ Res Public Health. 2021;18:4350. doi: 10.3390/ijerph18084350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Alarcón-Rodríguez J., Fernández-Velilla M., Ureña-Vacas A., Martín-Pinacho J., Rigual-Bobillo J., Jaureguízar-Oriol A., et al. Radiological management and follow-up of post-COVID-19 patients. Radiología. 2021;63:258–269. doi: 10.1016/j.rx.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Greenhalgh T., Knight M., Buxton M., Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020:370. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 100.Society B.T. British Thoracic Society guidance on respiratory follow up of patients with a clinico-radiological diagnosis of COVID-19 pneumonia. Br Thorac Soc. 2020:1–15. [Google Scholar]
- 101.National Institute for Health and Care Excellence COVID-19 rapid guideline: managing the longterm effects of COVID-19. 2022. https://www.nice.org.uk/guidance/ng188 [Online]. Available: [PubMed]
- 102.Cau R., Faa G., Nardi V., Balestrieri A., Puig J., Suri J.S., et al. Long-COVID diagnosis: from diagnostic to advanced AI-driven models. Eur J Radiol. 2022;148 doi: 10.1016/j.ejrad.2022.110164. [DOI] [PMC free article] [PubMed] [Google Scholar]