Abstract
Mesenchymal stem cells (MSCs) are multipotent stromal cells that can be obtained from various human tissues and organs. They can differentiate into a wide range of cell types, including osteoblasts, adipocytes and chondrocytes, thus exhibiting great potential in regenerative medicine. Numerous studies have indicated that MSCs play critical roles in cancer biology. The crosstalk between tumour cells and MSCs has been found to regulate many tumour behaviours, such as proliferation, metastasis and epithelial-mesenchymal transition (EMT). Multiple lines of evidence have demonstrated that MSCs can secrete exosomes that can modulate the tumour microenvironment and play important roles in tumour development. Notably, very recent works have shown that mesenchymal stem cell-derived exosomes (MSC-derived exosomes) are critically involved in cancer resistance to chemotherapy agents, targeted-therapy drugs, radiotherapy and immunotherapy. In this review, we systematically summarized the emerging roles and detailed molecular mechanisms of MSC-derived exosomes in mediating cancer therapy resistance, thus providing novel insights into the clinical applications of MSC-derived exosomes in cancer management.
Keywords: Mesenchymal stem cell, Exosome, Therapy resistance, Cancer
Background
Cancer is a major disease and the leading cause of mortality worldwide [1]. Although several treatment approaches, including surgery, chemotherapy, radiotherapy, targeted therapy, and immunotherapy have been developed and effectively improved patients’ prognoses, both intrinsic and acquired therapy resistance contribute to the reduction of therapeutic effectiveness, thus resulting in poor outcomes of cancer patients [2, 3]. The mechanisms of cancer therapy resistance are complicated and multifaceted, including decreased uptake and/or increased efflux of drugs, the inhibition of apoptosis-related signalling pathways, activation of cancer stem cells (CSCs), enhanced DNA damage repair, loss of cell cycle control, as well as physical barriers preventing therapeutic drugs from entering the tissue and exerting their effects [4–6]. Nevertheless, the detailed mechanisms underlying anticancer therapy resistance are still unclear. Identifying the key mediators of cancer therapy resistance could help us to understand the development of therapy resistance, and these mediators play considerable roles in the prediction and reversion of anticancer therapy resistance.
Mesenchymal stem cells (MSCs) are multipotent stem cells that can self-renew and differentiate into multilineage cells [7]. MSCs can be obtained from a variety of human tissues and organs, such as the bone marrow, fat tissue, brain, lung, and pancreas [7]. Moreover, emerging evidence has highlighted the regulatory roles of MSCs in both physiological and pathological conditions [8]. MSCs have the innate affinity to home to tumour sites and can modulate multiple biological processes related to cancer, such as metastasis, angiogenesis and epithelial-mesenchymal transition (EMT) [9, 10]. Notably, MSCs can secrete exosomes that can interact with diverse recipient cells to affect diverse biological behaviours of targeted cells, thereby modulating physiological homeostasis and/or the progression of human diseases [11]. Exosomes are nanosized membrane vesicles 40–160 nm in diameter that can be secreted by diverse cell types [12, 13]. Exosomes comprise complex contents, such as nucleic acids including DNA, mRNAs, and noncoding RNAs (ncRNAs), lipids, and various proteins [14, 15]. The major function of exosomes is modulating intercellular communication between diverse cell types by transferring multiple molecules, which mediate various cellular processes in both physiological and pathological conditions [16, 17]. Notably, numerous works have found that MSC-derived exosomes can function as critical modulators in the tumour microenvironment, and mediate the pathogenesis of various human cancers [18, 19]. Interestingly, MSC-derived exosomes have been found to play an essential role in cancer therapy resistance, including chemoresistance, targeted therapy resistance, radiotherapy resistance and immunotherapy resistance [20–22]. Furthermore, MSC-derived exosomes have been exploited as a novel therapeutic strategy in antitumour treatment due to their various advantages, such as biocompatibility, promising potential for modification, and lack of cytotoxicity [20–22]. For instance, MSC-derived exosomes show great potential for the delivery of anticancer agents because they can enhance their efficacy with low toxicity. Additionally, a great number of investigations have indicated that MSC-derived exosomes transfected with synthetic miRNAs can effectively enhance the sensitivity of cancer cells to chemotherapeutic drugs [18, 20].
In this review, we performed a systematic review of the pivotal roles of MSC-derived exosomes in mediating cancer therapy resistance as well as the complex mechanisms by which MSC-derived exosomes enhance or weaken anticancer-therapy resistance. Meanwhile, we also discussed the clinical applications of MSC-derived exosomes as novel therapeutic strategies for enhancing drug sensitivity, drug delivery vehicles and radiation-induced damage repair in cancer management.
Overview of MSC-derived exosomes
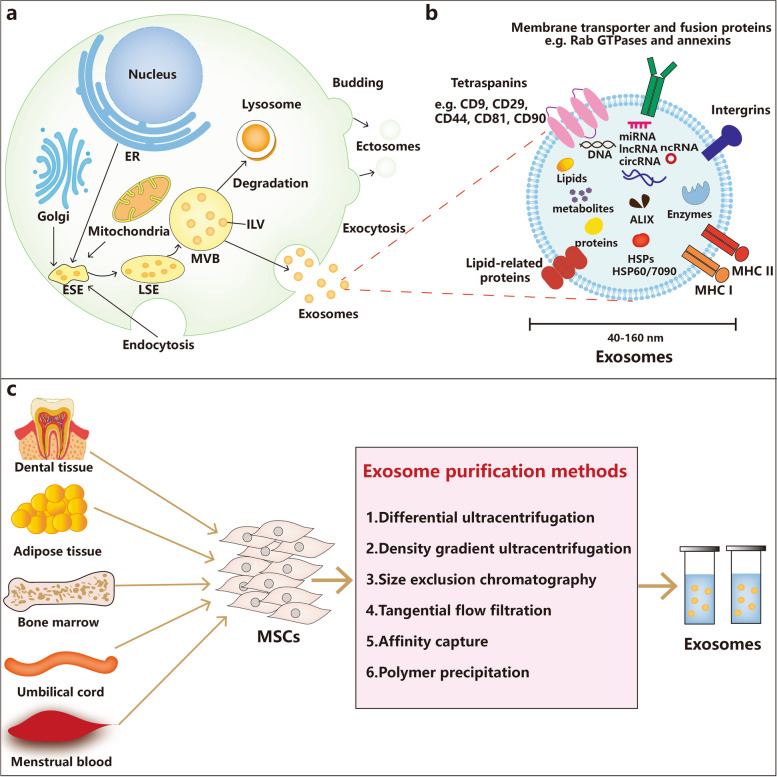
Biogenesis of exosomes
Exosomes are of endosomal origin and derived from lipid raft microdomains in the plasma membrane, with a diameter ranging in size from 40 to 160 nm and a density of 1.15–1.19 g/mL in sucrose gradients [23–25]. Exosomes are characterized as having a round morphology with heterogeneous sizes under a transmission electron microscope [26]. Exosomes are derived from a sequential process, mainly including the dual invagination of the plasma membrane, and the formation of intracellular multivesicular bodies (MVBs) that contain intraluminal vesicles (ILVs) (Fig. 1a) [27]. The biogenesis of exosomes starts with the invagination of primary endocytic vesicles encysting proteins from the cell surface and extracellular environments, which form the early-sorting endosomes (ESEs). Some ESEs are returned to the plasma membrane by endosome recycling, whereas other ESEs can induce the formation of late sorting endosomes (LSEs), and invagination of LSEs gives rise to ILVs [27]. This process contributes to the modification of cargos in the future resulting exosomes and the subsequent formation of MVBs. While some MVBs will be degraded by autophagosomes or lysosomes, others can fuse with the plasma membrane and then release ILVs into the extracellular environment as exosomes [28].
Fig. 1.
Overview of MSC-derived exosomes. A Biogenesis of exosomes. The biogenesis of exosomes comprises endocytosis, MVB formation, and exosome secretion into the extracellular microenvironment through merging with the plasma membrane. B Characteristics and contents of exosomes. C Exosome purification methods
A variety of proteins have been found to modulate the biogenesis of exosomes. Endosomal-sorting complex required for transport (ESCRT) proteins (ESCRT-0, ESCRT-I, ESCRT-II and ESCRT-III) are recognized as crucial mediators of ILV formation [29]. They can sort protein cargoes, induce membrane budding and sever membrane necks from their inner face with accessory proteins including Alix, VPS4 and VTA1 [30]. During the process of ILV biogenesis, protein cargoes captured into ILVs are principally characterized by ubiquitin, and the ESCRT-0 complex recognizes and obtains ubiquitinated proteins in the late endosome membrane [31, 32]. Then, cargoes are handed over to ESCRT-I, followed by the recruitment of ESCRT-II, which comprises a ubiquitin-binding and PtdIns3P-binding GLUE domain [29]. ESCRT-I and ESCRT-II complexes have strong recognition domains with high affinity for ubiquitinated substrates, and are responsible for shapping the membrane into buds, but it is still unknown whether ESCRT-I and ESCRT-II bind ubiquitylated cargoes sequentially or coordinately [33, 34]. ESCRT-III separates the vesicles from the cytoplasmic membrane to form MVBs, and promotes the deubiquitination of cargo proteins by deubiquitylating enzymes (DUBs) before ILV formation [14, 35]. Finally, ATPase induces the membrane scission and vacuolar protein sorting 4 (VPS4) participates in recycling all ESCRT molecules [36, 37]. The ubiquitinated proteins are critically involved in ESCRT-dependent cargo sorting and ILV formation, and E3 ubiquitin ligases and deubiquitylating enzymes have been identified to modulate the localization and functions of ESCRTs [38, 39]. In addition to ESCRT-dependent biogenesis of exosomes, recent reports have emphasized the importance of ESCRT-independent pathways involving ceramides, ADP ribosylation factor 6 (ARF6), and tetraspanin proteins (CD9, CD81 and CD82) in exosome biogenesis [40]. There also exists a non-MVB-specific pathway that regulates ILV formation through protein–protein interactions, in which syntenin-1 can bind to the cytosolic domain of syndecan-1 to recruit Alix in synergy with ESCRTs [41]. In terms of the fusion of MVBs with the plasma membrane and exosome secretion, RAB family small GTPase proteins, including Rab27a, Rab27b, Rab35 and Rab7, as well as membrane fusion soluble N-ethylmaleimide-sensitive factor attachment protein receptor (SNARE) complex proteins have been demonstrated to play critical roles in vesicular sorting and trafficking towards secretory organelles [42]. Interestingly, it has been reported that the mechanism of exosome secretion modulated by various RAB family proteins is dependent on cellular types. For instance, Rab27a and Rab27b are involved in controlling exosome release in HeLa cells, while exosome release in MCF-7 breast cancer cells is mediated by Rab7 [43]. Although progress in understanding the numerous proteins controlling the origin and biogenesis of exosomes has been achieved, the underlying mechanisms by which these proteins exert precise rate-limiting effects on exosome biogenesis warrant further in-depth exploration, especially in vivo research.
Contents of exosomes
Exosomes carry a variety of substances, including proteins, lipids, nucleic acids (DNA, mRNAs, and ncRNAs) and metabolites (Fig. 1b) [18]. There are thousands of exosome cargos, such as proteins, mRNAs, and miRNAs, according to the ExoCarta database (http://exocarta.org/) [44]. These cargos are critically involved in regulating diverse biological processes in both physiological and pathological conditions, and can be employed as biomarkers and effective therapeutic targets for human diseases. Over 1600 proteins participating in different biological functions, such as signal transduction, structural dynamics and metabolism modulation, are carried in exosomes [23]. Multiple exosomal proteins have been found to be associated with membrane transport and fusion, such as RAB GTPases, ESCRTs, heat shock proteins (HSPs) such as Hsp60, Hsp70, and Hsp90 and the accessory factors Alix and VPS4 [23, 45, 46]. Tetraspanins including CD9, CD63, CD81, CD82, and Tspan8, are the most common membrane proteins in exosomes, and have been found to facilitate the packaging of specific cargos into exosomes [47]. Notably, several exosomal proteins that are nonspecific molecules are usually regarded as markers for the identification of exosomes, such as CD9, CD63, CD81, HSP70 and Alix [14, 48]. Lipids are also a key component in exosomes, and play an indispensable role in exosome biogenesis, shape maintenance and homeostasis regulation in recipient cells [14]. For example, lysobisphosphatidic acid and ceramide are crucial mediators during exosome release from the cytoplasm [49, 50]. In addition, growing evidence has shown that ceramide participates in the regulation of autophagy, which may influence MVB homeostasis indirectly [51]. Moreover, the lipid composition of target cells has been found to change after fusing with exosomes, which subsequently affects the homeostasis of exosomes in recipient cells [14]. Notably, nucleic acids, especially RNAs make up the most significant fraction of functional components in exosomes and significantly facilitate the roles of exosomes as critical modulators of intracellular communication and diverse signalling pathways [52]. Exosomal RNA packaging is a specific process, as indicated by the preferential accumulation of certain exosomal RNAs that can be transferred to recipient cells to exert their effects [43]. RNAs in exosomes can modulate the biological behaviours of recipient cells in various ways, and exosomal RNAs in different body fluids can function as diagnostic and prognostic biomarkers in various human diseases [53]. In addition to proteins, lipids and RNAs, exosomes also carry several types of DNA, including single-stranded DNA (ssDNA), double stranded DNA (dsDNA) and mitochondrial DNA (mtDNA). KRAS and p53 mutations can be identified in genomic DNA from exosomal DNA for pancreatic cancer prediction [54]. The transfer of exosomal DNA into recipient cells can also endow recipient cells with diverse biological functions. For example, topotecan-treated cancer cell-derived exosomal DNA can trigger the activation of dendritic cells and subsequent CD8+ T-cell activation through the CGAS-STING signalling pathway [55].
Isolation of exosomes
In general, exosomes can be isolated from various body fluids, such as blood, urine, and synovial fluid, and conditioned cell culture media. Various techniques have been utilized for exosome isolation, such as differential ultracentrifugation, density-gradient ultracentrifugation, and tangential flow filtration (Fig. 1c) [56]. Differential high-speed ultracentrifugation is the most widely utilized and traditional method due to its simple protocol, efficiency and high purity [57]. Additionally, it has been found that density-gradient ultracentrifugation can isolate exosomes with a higher purity by isolating particles by layers of biocompatible medium with different densities, in comparison with classic ultracentrifugation [58]. However, all these methods, including density-gradient ultracentrifugation, size exclusion chromatography, and tangential flow filtration, have the same limitation in that they fail to distinguish particles with overlapping ranges, such as exosomes and microvesicles (extracellular vesicles with similar properties to exosomes) [20]. Notably, affinity capture can well distinguish a wide range of exosomes with high purity by surface markers of extracellular vesicles with the capture molecules attached to different carriers instead of depending on the density or size of extracellular vesicles; however, it has the disadvantage of low yield [20, 59]. Many novel techniques have emerged in recent years, including polyethylene glycol-based low-speed centrifugation, antibody- and filter-based enrichment methods, methods incorporating acoustics and microfluidics. In addition, many commercial kits have been put into use for exosome isolation. However, their isolation effectiveness has yet to be fully assessed [58, 60–62]. Although there is currently no consensus on a “gold standard” method for exosome isolation, it is recommended to utilize more than one technique combined for optimal outcomes in exosome isolation [63].
Characteristics of MSC-derived exosomes
MSCs have been demonstrated to be the most prolific producers of mass exosomes in humans [64]. MSC-derived exosomes were first investigated in the myocardial ischemia/reperfusion injury in vivo in 2010, followed by numerous works focusing on the roles of MSC-derived exosomes in a variety of diseases [65]. MSC-derived exosomes have the same morphological characteristics and isolation and storage methods as exosomes from other sources [19]. In terms of the identification of exosomes, MSC-derived exosomes not only express common surface biomarkers such as CD81 and CD9, but also express MSC surface markers, such as CD29, CD44, CD73 and CD90. MSC-derived exosomes are also enriched in diverse contents similar to exosomes from other cellular sources [66]. A previous study identified 730 functional proteins in bone marrow mesenchymal stem cell (BMSC)-derived exosomes, which play important roles in regulating the cellular growth, proliferation, migration and morphogenesis capacities of MSCs [67]. RNAs also make up critical components of MSC-derived exosomes. It has been found that MSC-derived exosomes are mainly enriched in short RNAs (< 300 nt), whereas 28S and 18S RNAs are not visible by utilizing ethidium bromide staining [66]. The enrichment of miRNAs in MSC-derived exosomes has been extensively investigated. It has been reported that exosomal miRNAs from MSCs are predominantly in the precursor form, and an ample amount of passenger miRNA has been found in MSC-derived exosomes [68]. Furthermore, comparative analysis of MSC-derived exosomal miRNAs with miRNAs in MSCs have found that 106 miRNAs in MSCs were not detected in MSC-derived exosomes, indicating that the packaging of miRNAs into exosomes is not a random but a regulated process [69]. The mechanisms by which exosomes selectively package miRNAs remain largely unknown. Previous studies have confirmed the critical correlation between RNAs and RNA-binding proteins (RBPs) outside cells, indicative of the importance of RBPs in the transfer and maintenance of RNAs in the extracellular space [70–72]. Emerging evidence has indicated that various RBPs are critically involved in sorting miRNAs into exosomes, making RBPs critical candidates for the fate and function of exosomal miRNAs [71, 73]. Notably, very recent work has demonstrated that special sorting sequences of miRNAs are required to determine their secretion in small extracellular vesicles (EXO-motifs) or cellular retention (CELL-motifs) [74]. Moreover, Alyref and Fus are two important RBPs involved in miRNA sequence recognition and the packaging of miRNA in exosomes [74]. Multiple lines of evidence have identified that the biological functions of MSC-derived exosomes are similar to those of MSCs, such as tissue regeneration, immune regulatory effects, and anti-inflammatory effects [75]. Notably, the unique characteristics of MSC-derived exosomes, including small size, long circulation half-life, low immunogenicity, excellent penetration capability, and ideal biocompatibility, make them promising candidates for the treatment of diverse human diseases, especially as newly-developed tools to be exploited in anticancer therapy [66].
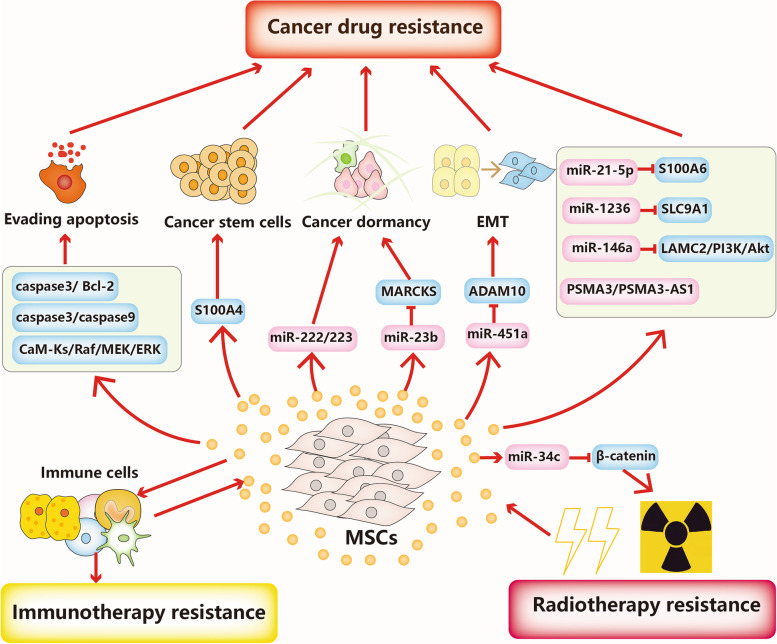
MSC-derived exosomes in cancer therapy resistance
Therapeutic resistance is a daunting challenge in achieving cures in patients with cancer. Cancer therapy resistance can be categorized into primary resistance and acquired resistance. Primary resistance means that tumour cells are initially resistant to standard therapy due to genetic or phenotypic alterations, while acquired resistance occurs after the initial successful therapeutic responses [76]. Hence, elucidating the detailed mechanisms involved in cancer therapy resistance is critical for developing optimal therapeutic strategies and improving the prognosis of cancer patients. Critical roles played by MSC-derived exosomes in multiple aspects of cancer progression, particularly therapy resistance have been increasingly demonstrated. The involvement of MSC-derived exosomes in cancer resistance to chemotherapy, targeted-therapy, immunotherapy and radiotherapy is summarized below (Fig. 2).
Fig. 2.
MSC-derived exosomes in cancer therapy resistance. MSC-derived exosomes participate in cancer drug resistance, immunotherapy and radiotherapy resistance through complex mechanisms, including evasion of apoptosis, modulation of cancer stem cells, and regulation of cancer dormancy
MSC-derived exosomes in chemotherapy resistance
Currently, chemotherapy is the first-line therapeutic strategy for a series of malignancies. Multiple chemotherapeutic agents with different properties and targets have been effectively applied to improve the clinical outcomes of patients with advanced cancers, such as platinum drugs, adriamycin (ADR), and 5-fluorouracil (5-FU) [77, 78]. However, the development of multidrug resistance (MDR) has remained the major challenge for the success of chemotherapy [79]. Multiple lines of evidence have demonstrated that MSC-derived exosomes are deeply involved in cancer chemotherapy resistance because they directly deliver functional proteins and RNAs (Table 1). Apoptosis avoidance has been identified as one of the major causes of chemoresistance, and MSC-derived exosomes can modulate apoptosis-related proteins to mediate chemoresistance. It has been found that MSC-derived exosomes enhance the resistance to 5-FU in gastric cancer both in vitro and in vivo. Mechanistically, MSC-derived exosomes prevent 5-FU-induced apoptosis by activating the CaM-Ks/Raf/MEK/ERK signalling cascade and MDR associated proteins by transferring functional proteins [80]. Tumour dormancy means that tumour cells can remain in the G0 phase of the cell cycle at the metastatic site after the resection of the primary tumour. Tumour dormancy is critically involved in cancer recurrence, metastasis and chemoresistance, and breast cancer cells exhibit particularly extensive tumour dormancy [81]. There is overwhelming evidence indicating that breast cancer recurrence and chemoresistance are correlated with the prolonged dormancy and successful survival of tumour cells in the bone marrow microenvironment. MSC-derived exosomes induced by breast cancer cells promoted breast cancer dormancy by transferring miR-222/223 in vitro and in vivo, and this dormancy was linked to carboplatin resistance. Furthermore, MSC-derived exosomes delivering antagomiRs enhanced the sensitivity to carboplatin and prevented cellular dormancy in breast cancer [22]. MSCs derived from human umbilical cord (hUCMSCs) are known for their promising self-renewal and proliferation capacities and their multipotent ability to differentiate into diverse cell lineages of the three germ layers [82]. hUCMSCs can also secrete diverse biologically active molecules through exosomes to interact with other cells, such as immune cells, thereby showing promising therapeutic potential in human diseases [82]. The antitumour effects of hUCMSCs have been confirmed in several neoplasms, such as breast cancer, lung cancer and osteosarcoma [83, 84]. Notably, however, hUCMSCs have been found to transdifferentiate into cancer-associated mesenchymal stem cells in tumour microenvironment, and have the capability to facilitate cancer progression and metastasis [85, 86]. Therefore, it is still largely unclear whether hUCMSCs promote or inhibit tumour progression, and the roles of hUCMSC-derived exosomes in cancer initiation and development are also uncertain and controversial. It has been found that hUCMSC-derived exosomes can promote dormancy initiation and confer resistance to conventional chemotherapy by inducing the expression of MMP-2 and ecto-5′-nucleotidase by transferring miRNAs in metastatic breast cancer [87]. Nevertheless, several studies have indicated hUCMSC-derived exosomes can inhibit breast cancer progression through complex mechanisms and deliver different cargoes. More studies are needed to clarify the controversial findings regarding the functions of hUCMSC-derived exosomes during breast cancer progression. It has been found that BMSC-derived exosomes can promote dormancy and docetaxel resistance in a bone marrow–metastatic human breast cancer cell line (BM2). Mechanistically, remarkable upregulation of miR-23b was detected in BMSC-derived exosomes compared with adult fibroblasts, and BMSC-derived exosomal miR-23b enhanced dormancy phenotypes and docetaxel resistance in BM2 cells by suppressing the expression of MARCKS, which encodes a protein that facilitates cell cycling and motility [88]. Similarly, MSCs-secreted exosomes have been found to promote doxorubicin (DOX) resistance by inducing S100A6 expression in MDA-MB-231 breast cancer cells. Upregulation of miR-21-5p has been detected in both MSCs and MSC-secreted exosomes after exposure to DOX, and MSCs-secreted exosomes could potentiate DOX resistance via miR-21-5p-mediated induction of S100A6 expression in breast cancer in vitro and in vivo [89]. CSCs, characterized by self-renewal and differentiation capacities and high tumorigenic potency, can differentiate into various subpopulations of cells within tumours [90]. It has been suggested that MSC-derived exosomes can regulate CSCs to mediate cancer therapy resistance. Exosomes from BMSCs have been found to upregulate stemness genes, such as OCT4, NANOG and SOX2, and promote the stemness of acute myeloid leukaemia (AML) cells. In addition, BMSC-derived exosomes can reduce the sensitivity to Ara-C by stimulating the expression of S100A4, a typical member of the S100 family of calcium-binding proteins in AML cells. Furthermore, knockdown of S100A4 reversed chemoresistance of AML cells [21].
Table 1.
MSC-derived exosomes in chemotherapy resistance
| Exosome source | Cancer type | Method | Key cargo | Genes and pathways | Drug | Drug resistance | Ref |
|---|---|---|---|---|---|---|---|
| hBMSCs | Gastric cancer | In vitro and in vivo | CaM-Ks/Raf/MEK/ERK | 5-FU | ↑ | [80] | |
| hBMSCs | Breast cancer | In vitro and in vivo | miR-222/223 | Carboplatin | ↑ | [22] | |
| hUMSCs | Breast cancer | In vitro | MMP-2 and ecto-5′-nucleotidase | Conventional chemotherapy | ↑ | [87] | |
| hBMSCs | Breast cancer | In vitro | miR-23b | MARCKS | DOX | ↑ | [88] |
| hBMSCs | Breast cancer | In vitro | miR-21-5p | S100A6 | DOX | ↑ | [89] |
| hBMSCs | Acute myeloid leukemia | In vitro | OCT4, NANOG and SOX2 | Ara-C | ↑ | [21] | |
| ADMSCs | Breast cancer | In vitro | miR-1236 | Wnt/β-Catenin | DDP | ↓ | [91] |
| hUCMSCs | Ovarian cancer | In vitro | miR-146a | LAMC2/PI3K/Akt | DOX | ↓ | [92] |
| hUCMSCs | Hepatocellular carcinoma | In vitro | miR-451a | ADAM10 | PTX | ↓ | [93] |
In contrast, a number of studies have identified that MSC-derived exosomes can enhance chemosensitivity in various cancers. Adipose-derived mesenchymal stem cell (ADMSC)-derived exosomes have been reported to can impair cisplatin (DDP) resistance in both parental and DDP-resistant breast cancer cell lines. Mechanistic investigation demonstrated that ADMSC-derived exosomes enhanced sensitivity to DDP by downregulating SLC9A1 via miR-1236 in breast cancer. Furthermore, overexpression of SLC9A1 reversed the inhibitory effects of ADMSC-derived exosomal miR-1236 on DDP resistance by activating the Wnt/β-Catenin signalling pathway in breast cancer [91]. Exosomal miR-146a from hUCMSCs has been reported to reverse the resistance of ovarian cancer cells to docetaxel and taxane by modulating the expression of LAMC2 and the PI3K/Akt signalling pathway in vitro [92]. EMT is a biological process, in which cells lose their epithelial characteristics, such as apical-basal polarity and cell junctions, and transform into a mesenchymal phenotype [94]. Increasing evidence has confirmed that cancer cells can undergo EMT to acquire chemoresistance in various cancer types, indicating inhibiting that EMT is a feasible strategy for reversing chemoresistance [94]. Xu et al. confirmed that hUCMSC-derived exosomal miR-451a could inhibit the EMT of hepatocellular carcinoma Hep3B and SMMC-7721 cell lines through the inhibition of ADAM10, thus increasing the paclitaxel (PTX) sensitivity of hepatocellular carcinoma cells in vitro [93].
MSC-derived exosomes in targeted therapy resistance
Recent advances in the understanding of the molecular biology of cancer development have given rise to numerous targeted-therapy drugs. Multiple targeted therapy drugs have been applied in the treatment of diverse cancers, such as cetuximab and panitumumab targeting the epidermal growth factor receptor (EGFR), and trastuzumab targeting HER-2 [95, 96]. Although these targeted-therapy drugs have been found to effectively improve the prognosis of cancer patients, the inevitable emergence of targeted-therapy resistance is a major hurdle for the long-term survival of patients [97]. Emerging evidence has indicated that MSC-derived exosomes critically participate in mediating targeted-therapy resistance (Table 2). For instance, Viola et al. have indicated that alterations in the contents of BMSC-derived exosomes were significantly correlated with tyrosine kinase inhibitor (TKI) resistance in AML [98]. Human BMSC (hBMSC)-derived exosomes have been reported to inhibit cellular proliferation via transferring miR-15a in chronic myeloid leukaemia (CML) in vitro. In addition, hBMSC-derived exosomes have also been confirmed to be involved in CML targeted-therapy resistance. hBMSC-derived exosomes can enhance cellular apoptosis resistance to TKIs by silencing caspase3 and Bcl-2 both in vitro and in vivo [99]. The proteasome inhibitor (PI) bortezomib has shown impressive efficacy in the treatment of patients with multiple myeloma [100]. However, its therapeutic effectiveness is highly impaired by drug resistance and the mechanism underlying PI resistance has not been completely revealed. A recent study suggested that MSC-derived exosomes play a critical role in multiple myeloma PI resistance. Furthermore, researchers identified that PSMA3 and lnc PSMA3-AS1 which were markedly upregulated in bortezomib-resistant samples in comparison to bortezomib-sensitive samples, were present in MSC-derived exosomes in multiple myeloma. Mechanistically, MSC-derived exosomes conferred bortezomib resistance by transferring PSMA3 and lnc PSMA3-AS1 to multiple myeloma cells, and lnc PSMA3-AS1 impaired the sensitivity of multiple myeloma cells to bortezomib by upregulating PSMA3 expression by forming an RNA duplex with PSMA3-AS1 pre-mRNA in vitro. Further in vivo studies confirmed that PSMA3-AS1 siRNA efficiently enhanced carfilzomib sensitivity in multiple myeloma xenografts, thereby identifying the therapeutic potential of exosomal PSMA3-AS1 from MSCs [101]. Conversely, MSC-derived exosomes can also reverse cancer targeted therapy resistance. Imatinib (IM), a TKI targeting the BCR-ABL oncoprotein, is a front-line therapeutic strategy for patients with early-stage CML [102]. However, approximately 20% CML patients develop IM resistance, resulting in unfavourable long-term survival. hUCMSC-derived exosomes have been found to enhance the sensitivity of K562 cells to IM through inhibition of proliferation and induction of apoptosis. Mechanistically, the combination of hUCMSC-derived exosomes with IM activated caspase-9 and caspase-3 in vitro in CML [103].
Table 2.
MSC-derived exosomes in targeted therapy resistance
| Exosome source | Cancer type | Method | Key cargo | Genes and pathways | Drugs | Drug resistance | Ref |
|---|---|---|---|---|---|---|---|
| BMSCs | AML | In vitro | TKIs | ↑ | [98] | ||
| hBMSCs | CML | In vivo and vitro | Caspase3 and Bcl-2 | TKIs | ↑ | [99] | |
| hBMSCs | Multiple myeloma | In vitro and in vivo | PSMA3 and Psma3-as1 | Bortezomib | ↑ | [101] | |
| hUMSCs | CML | In vitro | Caspase-9 and Caspase-3 | IM | ↓ | [103] |
MSC-derived exosomes in radiotherapy resistance
Radiation therapy is also a critical component of cancer therapeutic strategies, and has been widely utilized in diverse cancer types, such as prostate cancer, lung cancer and head and neck cancer [104]. It has been reported that approximately 50% of patients with cancer receive radiation therapy during their treatment, and radiation therapy accounts for approximately 40% of curative treatment for cancer patients [105]. However, cancer patients often develop radioresistance via complex mechanisms, resulting in limited effectiveness and cancer metastasis and recurrence. Emerging evidence has demonstrated that radiation therapy can affect the contents and secretion of exosomes, and radiation-derived exosomes can confer radioresistance and facilitate radiation-induced bystander effects [106]. For example, exosomal miR-340-5p from hypoxic oesophageal squamous cell carcinoma (OSCC) cells potentiated radioresistance by preventing radiation-induced apoptosis and promoting DNA damage repair by directly targeting KLF10 [107]. Notably, MSC-derived exosomes also participate in mediating cancer radiotherapy resistance. miR-34c, which is downregulated in both nasopharyngeal carcinoma tissues and cell lines, has been found to impair radioresistance by promoting radiotherapy-induced cell apoptosis by slicing β-catenin in vitro and in vivo. Furthermore, miR-34c-overexpressing exosomes derived from MSCs drastically facilitated radiation-induced cellular apoptosis in nasopharyngeal carcinoma [108]. In addition, MSC-derived exosomes could enhance the effectiveness of radiotherapy in inhibiting tumour growth and metastasis in a melanoma mouse model, thus suggesting the utility of combining radiotherapy with MSC-derived exosomes in the treatment of cancer patients [109].
MSC-derived exosomes in immunotherapy resistance
Recent breakthroughs in exploring the tumour immune microenvironment have opened new avenues for the development of immunotherapies [110]. Immunotherapy, which aims to kill cancer cells by modulating the host immune system, has been applied in the clinical treatment along with surgery, chemotherapy and radiotherapy in cancers such as melanoma [111]. Currently, the commonly used immunotherapeutic agents include immune checkpoint inhibitors, such as nivolumab and pembrolizumab (anti-PD-1), and ipilimumab and tremelimumab (anti-CTLA-4), chimeric antigen receptor (CAR) T cells and monoclonal antibodies [111–115]. Despite the unprecedented durable response rates of cancer patients to immunotherapies, a large portion of patients do not respond to immunotherapies due to primary, adaptive or acquired resistance [116]. Exosomes can play an immunoregulatory role by modulating the functions of different types of immune cells such as natural killer (NK) cells, T- and B-lymphocytes in the tumour immune microenvironment. Moreover, exosomes can transfer diverse cellular components and express molecules such as PD-L1 to stimulate or suppress the tumour immune response [117]. For example, hepatocellular carcinoma-derived exosomal circUHRF1 has been confirmed to inhibit the functions of NK cells by regulating the miR-449c-5p/TIM-3 pathway and can impair the sensitivity of hepatocellular carcinoma cells to anti-PD1 therapy [118]. In melanoma, it has been found that exosomal PD-L1 levels are associated with the tumour burden and immunotherapy sensitivity after patients receive PD-1 inhibitors, indicating the potential role of exosomal PD-L1 as a predictive biomarker for anti-PD-1 therapy. Notably, ongoing studies indicate that MSC-derived exosomes also critically participate in immunomodulation, mainly by regulating the functions of immune cells and altering the secretion of inflammatory factors, such as TNF-α and IL-1β [119]. MSC-derived exosomes can facilitate the differentiation of monocytic myeloid-derived suppressor cells (M-MDSCs) into highly immunosuppressive M2-polarized macrophages. In addition, MSC-derived exosomes can impair protective antitumour immunity through the upregulation of PD-L1 in myeloid cells and the downregulation of PD-1 in T cells in breast cancer in vivo [120]. In pancreatic ductal adenocarcinoma, BMSC-derived exosomes carrying galectin-9 siRNA and oxaliplatin (OXA) prodrug can induce immunogenic cell death (ICD), and reverse the suppressive tumour immune microenvironment, for example, inhibiting M2 macrophage polarization and the recruitment of cytotoxic T lymphocytes, thus enhancing immunotherapy effectiveness in vitro and in vivo [121]. Future studies are needed to elucidate whether MSC-derived exosomes play an immune-suppressive or immune-promoting role in the tumour microenvironment, as well as their functions in mediating cancer immunotherapy resistance.
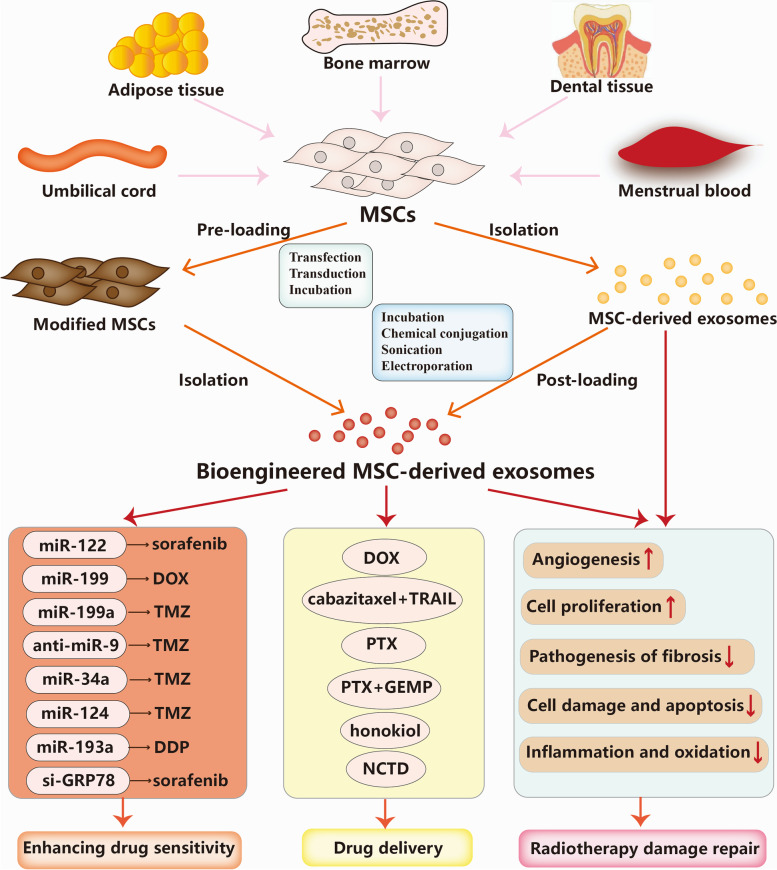
Therapeutic potential of MSC-derived exosomes in cancer
In the previous sections, we summarized the detailed mechanisms by which MSC-derived exosomes intensify or weaken cancer therapy resistance. Based on these mechanisms, in this section, we will discuss the promising potential of MSC-derived exosomes as a novel therapeutic strategy for enhancing therapeutic sensitivity, delivering various anticancer cargoes, and repairing radiotherapy-induced damage in cancer treatment (Fig. 3).
Fig. 3.
Applications of MSC-derived exosomes in cancer therapy. MSC-derived exosomes can be employed to deliver functional RNAs including miRNAs and siRNA to enhance the drug sensitivity, and deliver anticancer drugs such as chemotherapeutic agents. Moreover, MSC-derived exosomes are capable of repairing radiotherapy-induced damage through complex mechanisms, including promotion of cellular proliferation, promotion of angiogenesis capability, inhibition of inflammation and oxidation, and reduction of the pathogenesis of fibrosis
MSC-derived exosomes for enhancing drug sensitivity
Recent progress in understanding the roles of MSC-derived exosomes in mediating cancer therapy resistance has highlighted the promising potential of MSC-derived exosome-based therapy for enhancing therapeutic sensitivity. Because of their natural intercellular communication function, strong tumour tropism, low immunogenicity, low toxicity, biodegradable characteristics, and capability to escape from clearance and cross biological barriers, MSC-derived exosomes have emerged as promising carriers of various biomolecules and chemical agents in cancer treatment. Bioengineered MSC-derived exosomes can encapsulate desired therapeutic cargoes, such as miRNAs, proteins and drugs. There are two main anti-cancer cargo loading approaches, including preloading (before exosome isolation) and post-loading (after exosome isolation). It has been observed that MSCs transfected with synthetic miRNAs can enhance the chemosensitivity of cancer cells by transferring specific miRNAs via exosomes. For instance, ADMSCs transfected with miR-122, which can effectively transfer miR-122 to hepatocellular carcinoma cells and have been found to sensitize hepatocellular carcinoma cells to 5-FU and sorafenib by negatively regulating the expression of miR-122 target genes. Furthermore, intratumour injection of ADMSC-derived miR-122-carrying exosomes can significantly enhance the antitumour efficacy of sorafenib and inhibit tumour growth in hepatocellular carcinoma in vivo [122]. Similarly, exosomes derived from miR-199-modified ADMSCs can improve sensitivity to DOX via the inhibition of the mTOR signalling pathway in hepatocellular carcinoma in vitro and in vivo [123]. In glioma, miR-199a, a downregulated miRNA in both glioma tissues and cells, has been found to inhibit the proliferation, invasion and migration of U251 cells in vitro. Furthermore, miR-199a-overexpressing MSC-derived exosomes inhibited glioma progression and enhanced sensitivity to temozolomide (TMZ) by suppressing AGAP2 expression in vitro and in vivo [124]. Exosomes from MSCs-labelled with anti-miR-9-Cy5 can transfer anti-miR-9 to weaken the TMZ resistance of glioblastoma cells. Mechanistically, anti-miR-9 delivered by MSC-derived exosomes can promote caspase activity and induce cell death in response to TMZ by suppressing the expression of the drug transporter MDR1 [125]. Likewise, it has been found that hBMSC-secreted exosomes overexpressing miR-34a can increase the sensitivity to TMZ, and inhibit the proliferation, migration and invasion of glioblastoma cells by downregulating MYCN both in vitro and in vivo [126]. Wharton’s jelly-derived MSC (WJ-MSC)-derived exosomes transfected with miR-124 have been confirmed to sensitize glioblastoma cells to TMZ and inhibit glioblastoma cell proliferation and migration of by directly targeting CDK6 in vitro [127]. It has been observed that miR-193a expression was downregulated whereas LRRC1 expression was upregulated in both DDP-resistant NSCLC tissues and cells, and BMSC-derived exosomes could inhibit NSCLC progression through upregulating miR-193a and downregulating LRRC1 in vitro and in vivo. Furthermore, BMSC-derived exosomes transfected with miR-193a mimic impaired DDP resistance and inhibited proliferation, migration and invasion by inhibiting LRRC expression in NSCLC [128]. Additionally, MSC-derived exosomes-delivered small interfering RNA (siRNA) is another novel therapeutic strategy for enhancing drug sensitivity in the treatment of many cancers. Grp78, which is upregulated in multiple cancer types, have been reported to confer sorafenib resistance in hepatocellular carcinoma. Exosomes derived from GRP7-siRNA-modified BMSCs can sensitize hepatocellular carcinoma cells to sorafenib, and combination of si-GRP78-modified BMSC-derived exosomes and sorafenib can suppress the growth and invasion of the hepatocellular carcinoma cells in vitro [129].
MSC-derived exosomes for drug delivery
MSC-derived exosomes possess broad application prospects for delivering chemotherapeutic agents in cancer treatment and can effectively improve the inhibitory effects on tumour growth and selectivity for targeting tumour sites of the chemotherapeutic agents. Compared with conventional chemotherapy. Besides, MSC-derived exosomes can easily permeate through various physical barriers at a high speed, such as the blood–brain barrier (BBB), and transcytosis is the main underlying mechanism, thus helping drugs reach therapeutic concentrations [130]. In drug-resistant oral squamous cell carcinoma MSC-derived exosomes can deliver cabazitaxel/tumour necrosis factor-related apoptosis-inducing ligand (TRAIL) combinations and enhance cabazitaxel-induced apoptosis by inhibiting the PI3K/Akt/mTOR signalling pathway in vitro and vivo [131]. It has been found that MSC-derived exosomes carrying DOX can inhibit osteosarcoma cell growth with higher effectiveness and lower cytotoxicity than free DOX in vitro [132]. Similarly, Bagheri et al. reported that MSC-derived exosomes carrying DOX could be transported to MUC1-positive colorectal cancer cells with high efficiency in vitro. Further in vivo studies found that DOX carried in MSC-derived exosomes could highly accumulate in tumour site and remarkedly inhibit tumour growth with faster liver clearance than free DOX [133]. It has been found that mouse BMSCs could be loaded with PTX through exposure to very-high-dose PTX in vitro. Then, these BMSCs can secrete exosomes containing a high amount of PTX, which exert strong anti-proliferative effects on pancreatic cancer cells [134]. Similarly, PTX-loaded MSC-derived exosomes have been found to effectively inhibit tumour growth and distant organs metastasis with a 1000-fold reduced PTX amount compared with the application of free PTX [135]. Recent research has found that BMSC-derived exosomes loaded with PTX and gemcitabine monophosphate (GEMP), an intermediate product of gemcitabine metabolism, exhibited superior homing and penetrating abilities both in vitro and in vivo in pancreatic cancer. Meanwhile, both the in vitro and in vivo antitumour efficacy of BMSC-derived exosomes loaded with PTX and GEMP were significantly high. These findings indicated that BMSC-derived exosomes loaded with PTX and GEMP may play an important role in overcoming chemoresistance and penetrating pathological barriers, and could function well as a promising strategy for targeted therapy in pancreatic cancer [136]. Honokiol is a pleiotropic compound that has been specified as a novel antitumour agent in various cancer types [137]. Kanchanapally et al. loaded MSC-derived exosomes with honokiol by utilizing the sonication method, and the results showed that MSC-derived exosomes-loaded honokiol had superior antitumour effects than the free honokiol resulting from the efficient cellular uptake [138]. Norcantharidin, is a demethylated derivative of cantharidin and has strong bioactivity in anti-cancer and light side-effects, which has been currently applied as a routine anti-cancer agent clinically in China [139]. A recent study has found that norcantharidin loaded in BMSC-derived exosomes have significant antitumour effects and an in-situ homing effect on the tumour sites with no body toxicity in the treatment for hepatocellular carcinoma. Furthermore, BMSC-derived exosomes-loaded norcantharidin can repair damaged liver tissues through promoting cellular proliferation and suppressing liver cell oxidation [140].
MSC-derived exosomes for radiotherapy damage repair
Despite remarkable advances in radiotherapy techniques, cancer patients often suffer from radiation-induced damage during or after receiving radiotherapy [141]. MSC-derived exosomes have been shown to exert effects on regenerating tissue injuries in different diseases and clinical scenarios models, such as wound healing, cardiovascular disease, and COVID-19 [68]. Multiple lines of evidence have identified that MSC-derived exosomes have promising potential to repair radiation-induced tissue damage by various mechanisms, including promoting cellular proliferation and survival, enhancing angiogenesis, inhibiting inflammation and oxidation, and reducing the pathogenesis of fibrosis [142]. For instance, intravenous delivery of human BMSC-derived extracellular vesicles, including exosomes and microvesicles, can recover the normal counts of peripheral blood cells because the exosomes transfer various miRNAs in mice after receipt of whole-body irradiation [67]. Mechanistically, exosomal miR-221, miR-451, and miR-654-3p can enhance the proliferation of irradiated bone marrow cells, and exosomal miR210-5p, miR-106b-3p and miR-155-5p can prevent the radiation-induced apoptosis of haematopoietic cells [67]. It has also been reported that MSC-derived exosomes can recover radiation-induced haematopoiesis in a mouse model by secreting human haematopoiesis-related cytokines, such as IL-6/8, G-CSF, and MCP-1 [143]. Additionally, MSC-derived exosomes can protect the skin, respiratory system and other systems against radiation-induced damage. BMSC-derived exosomes have been reported to alleviate radiation-induced bone loss in a rat model. This effect is achieved by recovering the cellular proliferative capability, alleviating DNA and oxidative stress damage, and restoring the balance between adipogenesis and osteogenesis of irradiated BMSCs [144]. Radiotherapy-induced lung fibrosis is a common complication of thoracic radiotherapy and strongly limits the increasing radiation doses and influences the cancer patients’ clinical outcomes. Mouse MSC-derived exosomal miR-466f-3p can efficiently relieve radiation-induced lung fibrosis through reversing EMT by inhibiting the AKT/GSK3β signaling pathway via c-MET [145].
Perspectives and challenges
MSC-derived exosomes are critical mediators of every mentioned category of therapy resistance in various human malignancies. Multiple bioactivators in MSC-derived exosomes may have potential as optimal candidates for noninvasive biomarkers associated with cancer therapy resistance and therapeutic efficacy for cancer patients. Therefore, dynamic monitoring of these bioactivators may be a promising approach to effectively evaluate therapeutic responses, thus enabling clinicians to choose the most suitable therapy strategy for individual patient. Moreover, the identification of exosomes, especially MSC-derived exosomes, as a cell-free material that can exert inherently beneficial therapeutic effects provides a novel avenue for their application in cancer treatment. Bioengineered MSC-derived exosomes can function as delivery vehicles for anticancer agents and diverse synthetic biomolecules, thus exerting excellent anticancer effects. To date, a total of 15 clinical trials employing MSC-derived exosomes as therapeutic agents have been designed or conducted (www.clinicaltrials.gov). Although substantial progress has been achieved in the investigation of MSC-derived exosomes, many crucial unanswered questions and limitations of MSC-derived exosome have slowed down their clinical application, and should be addressed in future studies.
First, standard classifications for MSC-derived exosomes remain elusive. A recent study presented isolation and characterization protocols for six different extracellular vesicle subpopulations from tissues [146]. However, the classification of MSC-derived extracellular vesicles still lacks uniform international standards, and whether previous results have been affected by inconsistent isolation and purification techniques remains unclear. Future studies should distinguish different MSC-derived extracellular vesicle subpopulations and then assess their antitumour activity. Moreover, systematic standards and protocols for the extraction, purification, and storage of MSC-derived exosomes have not been established, which is a problem for the clinical application of MSC-derived exosomes. The use of different isolation and purification methods contribute to different subpopulations of MSC-derived extracellular vesicles with different contents, characteristics and biological functions [66]. Therefore, novel standardized strategies for extraction, purification, and storage techniques that meet good manufacturing practice (GMP) standards need to be developed for MSC-derived exosomes research.
The efficiency of the large-scale production of MSC-derived exosomes also clearly hinders the potential translation of MSC-derived exosomes into clinical practice. Currently, several effective and exosome isolation techniques have been developed, such as the polyethylene glycol (PEG) isolation approach, dielectrophoretic (DEP) separation, and deterministic lateral displacement (DLD) separation, and the combination of two or more isolation techniques presents a plausible strategy for efficient and high purity exosome isolation [147–149]. Nonetheless, combined isolation strategies contribute to high cost and procedure complexity. Developing real-time exosome quantification and analysis strategies and devices is also of great importance for further in-depth investigation and clinical translation of MSC-derived exosomes. It also seems necessary to improve the unsatisfactory efficiency of antitumour cargo loading and delivery in engineered exosomes. Recently, an increasing number of studies have focused on developing artificial exosomes as prominent drug delivery systems. Artificial exosomes possess similar characteristics and therapeutic potential to exosomes with higher pharmaceutical acceptability and the capability of much larger-scale production [150, 151]. Employing MSC-derived exosome mimetics in cancer management is a promising future direction with a wide clinical application view. For instance, hBMSC-derived exosome mimetics mixed with PTX via extrusion can exert promising antitumour effects in breast cancer in vitro and in vivo [152].
Despite their native tumour-homing properties, MSC-derived exosomes can be taken up by different cell types, and achieving promising targeting specificity and to prevent side effects caused by targeting of nontargeted cells is of great importance. Researchers are now exploring and developing novel strategies for attaching specific peptides or ligands to the exosome membrane by surface engineering to improve targeting specificity. Lysosomal-associated membrane protein 2 (Lamp2b), which can be appended with various targeting ligands, has become the most extensively employed exosome membrane protein for exosome surface engineering to improve the selectivity for specific targeted cells [153, 154]. Furthermore, several other exosome membrane proteins, such as the transmembrane protein platelet-derived growth factor receptor (PDGFR), the tetraspanin superfamily members, CD63, CD9, and CD81 (with their two extracellular loops), and lactadherin (with its C1C2 domain) can also be engineered to confer cancer cell targeting specificity [155, 156]. However, novel cancer cell-targeting biomolecules with high binding affinity and targeting specificity are still lacking, and strategies to the problems caused by surface engineering, such as immune activation and host protein deficiency are needed.
Finally, challenges also exist regarding the uncertain biosafety of MSC-derived exosomes in the clinic. There are multiple functional and harmful contents in MSC-derived exosomes; thus, further studies should focus on developing effective and novel engineering strategies to remove or deactivate unwanted and harmful substances in MSC-derived exosomes to ensure the safety of exosomal therapy [157]. In addition, the instability of MSC-derived exosomal contents in recipients is another challenge for the future application of MSC-derived exosomes in cancer management. Previous studies have found that the amount of miRNA cargo secreted by exosomes can be highly influenced by environmental conditions, such as the pH value and hypoxic status of the culture medium [66]. Thus, more efforts should be made to improve the stability of antitumour cargoes in MSC-derived exosomes in the human body. Furthermore, a comprehensive evaluation of the optimal dose, drug distribution, therapeutic routine and biological safety of MSC-derived exosomes in cancer treatment is urgently required. To date, most research focusing on MSC-derived exosomes has been conducted in cellular experiments; thus, the biosafety and efficacy of MSC-derived exosome-associated applications should be examined with long-term monitoring platforms and in vivo models. There is also an urgent need for larger, multicentre, and longer-term studies to achieve the clinical use of MSC-derived exosomes, including clinical trials.
Conclusions
Overall, we discussed and summarized recent discoveries and research progress related to the roles of MSC-derived exosomes in mediating cancer therapy resistance, and further emphasized the potential of MSC-derived exosomes in clinical applications as novel antitumour agents, which provides a novel direction for reversing therapy resistance and improving prognoses for cancer patients. Due to the key role of MSC-derived exosomes in mediating cancer therapy resistance, further investigations are needed to explore the underlying mechanisms of MSC-derived exosomes in cancer therapy resistance and develop novel MSC-derived exosome-related therapeutic strategies to overcome cancer therapy resistance in the clinic.
Acknowledgments
Not applicable.
Abbreviations
- MSCs
mesenchymal stem cells
- EMT
epithelial-mesenchymal transition
- MSC-derived exosomes
mesenchymal stem cell-derived exosomes
- CSCs
cancer stem cells
- ncRNAs
noncoding RNAs
- MVBs
multivesicular bodies
- ILVs
intraluminal vesicles
- ESEs
early-sorting endosomes
- LSEs
late sorting endosomes
- ESCRT
Endosomal-sorting complex required for transport
- DUBs
de-ubiquitylating enzymes
- VPS4
vacuolar protein sorting 4
- ARF6
ADP ribosylation factor 6
- SNARE
soluble N-ethylmaleimide-sensitive factor attachment protein receptor
- HSPs
heat shock proteins
- ssDNA
single-stranded DNA
- dsDNA
double stranded DNA
- mtDNA
mitochondrial DNA
- BMSC
bone marrow mesenchymal stem cell
- RBPs
RNA-binding proteins
- ADR
adriamycin
- 5-FU
5-fluorouracil
- MDR
multi-drug resistance
- hUCMSCs
MSCs derived from the human umbilical cord
- BM2
bone marrow–metastatic human breast cancer cell line
- DOX
doxorubicin
- AML
acute myeloid leukemia
- ADMSC
adipose mesenchymal stem cell
- DDP
cisplatin
- PTX
paclitaxel
- EFGR
epidermal growth factor receptor
- TKIs
tyrosine kinase inhibitors
- CML
chronic myeloid leukemia
- EGFR
epidermal growth factor receptor
- PI
proteasome inhibitor
- IM
Imatinib
- OSCC
oesophageal squamous cell carcinoma
- CAR
chimaeric antigen receptor
- NK
natural killer
- M-MDSCs
monocytic myeloid-derived suppressor cells
- OXA
oxaliplatin
- ICD
immunogenic cell death
- TMZ
temozolomide
- WJ-MSCs
Wharton’s jelly-MSCs
- siRNA
small interfering RNA
- BBB
blood–brain barrier
- TRAIL
factor-related apoptosis-inducing ligand
- GEMP
gemcitabine monophosphate
- PEG
polyethylene glycol (PEG)
- DEP
dielectrophoretic
- DLD
deterministic lateral displacement
- Lamp2b
lysosomal-associated membrane protein 2
- PDGFR
platelet-derived growth factor receptor
Authors’ contributions
ZJL, YLW and TL contributed to conceive, design and revision of the manuscript sections. ZJL, YTX and GQL wrote the manuscript. YTX and GQL designed figures and created Tables. ZHL and TL supervised the manuscript by providing critical feedbacks and revisions. The authors read and approved the final manuscript.
Funding
This study was supported by grants from National Natural Science Foundation of China (NO. 81871783 and 82072441), Hunan Outstanding Youth Fund (NO. 2022JJ10095).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors consent to publication.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zhihong Li, Email: lizhihong@csu.edu.cn.
Tang Liu, Email: liutang1204@csu.edu.cn.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 2.Gatenby RA, Brown JS. Integrating evolutionary dynamics into cancer therapy. Nat Rev Clin Oncol. 2020;17:675–686. doi: 10.1038/s41571-020-0411-1. [DOI] [PubMed] [Google Scholar]
- 3.Shahar N, Larisch S. Inhibiting the inhibitors: targeting anti-apoptotic proteins in cancer and therapy resistance. Drug Resist Updat. 2020;52:100712. doi: 10.1016/j.drup.2020.100712. [DOI] [PubMed] [Google Scholar]
- 4.Wei L, Sun J, Zhang N, Zheng Y, Wang X, Lv L, Liu J, Xu Y, Shen Y, Yang M. Noncoding RNAs in gastric cancer: implications for drug resistance. Mol Cancer. 2020;19:62. doi: 10.1186/s12943-020-01185-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vasan N, Baselga J, Hyman DM. A view on drug resistance in cancer. Nature. 2019;575:299–309. doi: 10.1038/s41586-019-1730-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arvanitis CD, Ferraro GB, Jain RK. The blood-brain barrier and blood-tumour barrier in brain tumours and metastases. Nat Rev Cancer. 2020;20:26–41. doi: 10.1038/s41568-019-0205-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salem HK, Thiemermann C. Mesenchymal stromal cells: current understanding and clinical status. Stem Cells. 2010;28:585–596. doi: 10.1002/stem.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uccelli A, Moretta L, Pistoia V. Mesenchymal stem cells in health and disease. Nat Rev Immunol. 2008;8:726–736. doi: 10.1038/nri2395. [DOI] [PubMed] [Google Scholar]
- 9.Ridge SM, Sullivan FJ, Glynn SA. Mesenchymal stem cells: key players in cancer progression. Mol Cancer. 2017;16:31. doi: 10.1186/s12943-017-0597-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meng L, Zhao Y, Bu W, Li X, Liu X, Zhou D, Chen Y, Zheng S, Lin Q, Liu Q, Sun H. Bone mesenchymal stem cells are recruited via CXCL8-CXCR2 and promote EMT through TGF-beta signal pathways in oral squamous carcinoma. Cell Prolif. 2020;53:e12859. doi: 10.1111/cpr.12859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xunian Z, Kalluri R. Biology and therapeutic potential of mesenchymal stem cell-derived exosomes. Cancer Sci. 2020;111:3100–3110. doi: 10.1111/cas.14563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Camussi G, Deregibus MC, Bruno S, Grange C, Fonsato V, Tetta C. Exosome/microvesicle-mediated epigenetic reprogramming of cells. Am J Cancer Res. 2011;1:98–110. [PMC free article] [PubMed] [Google Scholar]
- 13.Azmi AS, Bao B, Sarkar FH. Exosomes in cancer development, metastasis, and drug resistance: a comprehensive review. Cancer Metastasis Rev. 2013;32:623–642. doi: 10.1007/s10555-013-9441-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mashouri L, Yousefi H, Aref AR, Ahadi AM, Molaei F, Alahari SK. Exosomes: composition, biogenesis, and mechanisms in cancer metastasis and drug resistance. Mol Cancer. 2019;18:75. doi: 10.1186/s12943-019-0991-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mathivanan S, Ji H, Simpson RJ. Exosomes: extracellular organelles important in intercellular communication. J Proteome. 2010;73:1907–1920. doi: 10.1016/j.jprot.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 16.Li I, Nabet BY. Exosomes in the tumor microenvironment as mediators of cancer therapy resistance. Mol Cancer. 2019;18:32. doi: 10.1186/s12943-019-0975-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Record M, Subra C, Silvente-Poirot S, Poirot M. Exosomes as intercellular signalosomes and pharmacological effectors. Biochem Pharmacol. 2011;81:1171–1182. doi: 10.1016/j.bcp.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 18.Vakhshiteh F, Atyabi F, Ostad SN. Mesenchymal stem cell exosomes: a two-edged sword in cancer therapy. Int J Nanomedicine. 2019;14:2847–2859. doi: 10.2147/IJN.S200036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lai RC, Yeo RW, Lim SK. Mesenchymal stem cell exosomes. Semin Cell Dev Biol. 2015;40:82–88. doi: 10.1016/j.semcdb.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 20.Weng Z, Zhang B, Wu C, Yu F, Han B, Li B, Li L. Therapeutic roles of mesenchymal stem cell-derived extracellular vesicles in cancer. J Hematol Oncol. 2021;14:136. doi: 10.1186/s13045-021-01141-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lyu T, Wang Y, Li D, Yang H, Qin B, Zhang W, Li Z, Cheng C, Zhang B, Guo R, Song Y. Exosomes from BM-MSCs promote acute myeloid leukemia cell proliferation, invasion and chemoresistance via upregulation of S100A4. Exp Hematol Oncol. 2021;10:24. doi: 10.1186/s40164-021-00220-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bliss SA, Sinha G, Sandiford OA, Williams LM, Engelberth DJ, Guiro K, Isenalumhe LL, Greco SJ, Ayer S, Bryan M, et al. Mesenchymal stem cell-derived Exosomes stimulate cycling quiescence and early breast Cancer dormancy in bone marrow. Cancer Res. 2016;76:5832–5844. doi: 10.1158/0008-5472.CAN-16-1092. [DOI] [PubMed] [Google Scholar]
- 23.Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367:eaau6977. [DOI] [PMC free article] [PubMed]
- 24.Tan SS, Yin Y, Lee T, Lai RC, Yeo RW, Zhang B, et al. Therapeutic MSC exosomes are derived from lipid raft microdomains in the plasma membrane. J Extracell Vesicles. 2013;2:22614. doi: 10.3402/jev.v2i0.22614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Théry C, Amigorena S, Raposo G, Clayton A. Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Curr Protoc Cell Biol. 2006;Chapter 3:Unit 3.22. doi: 10.1002/0471143030.cb0322s30. [DOI] [PubMed] [Google Scholar]
- 26.Gong M, Yu B, Wang J, Wang Y, Liu M, Paul C, Millard RW, Xiao DS, Ashraf M, Xu M. Mesenchymal stem cells release exosomes that transfer miRNAs to endothelial cells and promote angiogenesis. Oncotarget. 2017;8:45200–45212. doi: 10.18632/oncotarget.16778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ibrahim A, Marban E. Exosomes: fundamental biology and roles in cardiovascular physiology. Annu Rev Physiol. 2016;78:67–83. doi: 10.1146/annurev-physiol-021115-104929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hessvik NP, Llorente A. Current knowledge on exosome biogenesis and release. Cell Mol Life Sci. 2018;75:193–208. doi: 10.1007/s00018-017-2595-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vietri M, Radulovic M, Stenmark H. The many functions of ESCRTs. Nat Rev Mol Cell Biol. 2020;21:25–42. doi: 10.1038/s41580-019-0177-4. [DOI] [PubMed] [Google Scholar]
- 30.Henne WM, Buchkovich NJ, Emr SD. The ESCRT pathway. Dev Cell. 2011;21:77–91. doi: 10.1016/j.devcel.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 31.Hanson PI, Cashikar A. Multivesicular body morphogenesis. Annu Rev Cell Dev Biol. 2012;28:337–362. doi: 10.1146/annurev-cellbio-092910-154152. [DOI] [PubMed] [Google Scholar]
- 32.Raiborg C, Stenmark H. The ESCRT machinery in endosomal sorting of ubiquitylated membrane proteins. Nature. 2009;458:445–452. doi: 10.1038/nature07961. [DOI] [PubMed] [Google Scholar]
- 33.Wollert T, Hurley JH. Molecular mechanism of multivesicular body biogenesis by ESCRT complexes. Nature. 2010;464:864–869. doi: 10.1038/nature08849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stefani F, Zhang L, Taylor S, Donovan J, Rollinson S, Doyotte A, Brownhill K, Bennion J, Pickering-Brown S, Woodman P. UBAP1 is a component of an endosome-specific ESCRT-I complex that is essential for MVB sorting. Curr Biol. 2011;21:1245–1250. doi: 10.1016/j.cub.2011.06.028. [DOI] [PubMed] [Google Scholar]
- 35.Yeates EF, Tesco G. The endosome-associated Deubiquitinating enzyme USP8 regulates BACE1 enzyme Ubiquitination and degradation. J Biol Chem. 2016;291:15753–15766. doi: 10.1074/jbc.M116.718023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adell MAY, Migliano SM, Upadhyayula S, Bykov YS, Sprenger S, Pakdel M, et al. Recruitment dynamics of ESCRT-III and Vps4 to endosomes and implications for reverse membrane budding. Elife. 2017;6:e31652. [DOI] [PMC free article] [PubMed]
- 37.Urbanelli L, Magini A, Buratta S, Brozzi A, Sagini K, Polchi A, Tancini B, Emiliani C. Signaling pathways in exosomes biogenesis, secretion and fate. Genes (Basel) 2013;4:152–170. doi: 10.3390/genes4020152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hoeller D, Crosetto N, Blagoev B, Raiborg C, Tikkanen R, Wagner S, Kowanetz K, Breitling R, Mann M, Stenmark H, Dikic I. Regulation of ubiquitin-binding proteins by monoubiquitination. Nat Cell Biol. 2006;8:163–169. doi: 10.1038/ncb1354. [DOI] [PubMed] [Google Scholar]
- 39.Clague MJ, Liu H, Urbe S. Governance of endocytic trafficking and signaling by reversible ubiquitylation. Dev Cell. 2012;23:457–467. doi: 10.1016/j.devcel.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 40.Henne WM, Stenmark H, Emr SD. Molecular mechanisms of the membrane sculpting ESCRT pathway. Cold Spring Harb Perspect Biol. 2013;5:a016766. [DOI] [PMC free article] [PubMed]
- 41.Mathieu M, Martin-Jaular L, Lavieu G, Théry C. Specificities of secretion and uptake of exosomes and other extracellular vesicles for cell-to-cell communication. Nat Cell Biol. 2019;21:9–17. doi: 10.1038/s41556-018-0250-9. [DOI] [PubMed] [Google Scholar]
- 42.Zhen Y, Stenmark H. Cellular functions of Rab GTPases at a glance. J Cell Sci. 2015;128:3171–3176. doi: 10.1242/jcs.166074. [DOI] [PubMed] [Google Scholar]
- 43.Liu J, Ren L, Li S, Li W, Zheng X, Yang Y, Fu W, Yi J, Wang J, Du G. The biology, function, and applications of exosomes in cancer. Acta Pharm Sin B. 2021;11:2783–2797. doi: 10.1016/j.apsb.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Keerthikumar S, Chisanga D, Ariyaratne D, Al Saffar H, Anand S, Zhao K, Samuel M, Pathan M, Jois M, Chilamkurti N, et al. ExoCarta: a web-based compendium of Exosomal cargo. J Mol Biol. 2016;428:688–692. doi: 10.1016/j.jmb.2015.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lauwers E, Wang YC, Gallardo R, Van der Kant R, Michiels E, Swerts J, Baatsen P, Zaiter SS, McAlpine SR, Gounko NV, et al. Hsp90 mediates membrane deformation and exosome release. Mol Cell. 2018;71(689–702):e689. doi: 10.1016/j.molcel.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 46.Moreno-Gonzalo O, Fernandez-Delgado I, Sanchez-Madrid F. Post-translational add-ons mark the path in exosomal protein sorting. Cell Mol Life Sci. 2018;75:1–19. doi: 10.1007/s00018-017-2690-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kalluri R. The biology and function of exosomes in cancer. J Clin Invest. 2016;126:1208–1215. doi: 10.1172/JCI81135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thery C, Zitvogel L, Amigorena S. Exosomes: composition, biogenesis and function. Nat Rev Immunol. 2002;2:569–579. doi: 10.1038/nri855. [DOI] [PubMed] [Google Scholar]
- 49.Trajkovic K, Hsu C, Chiantia S, Rajendran L, Wenzel D, Wieland F, Schwille P, Brügger B, Simons M. Ceramide triggers budding of exosome vesicles into multivesicular endosomes. Science. 2008;319:1244–1247. doi: 10.1126/science.1153124. [DOI] [PubMed] [Google Scholar]
- 50.Chu Z, Witte DP, Qi X. Saposin C-LBPA interaction in late-endosomes/lysosomes. Exp Cell Res. 2005;303:300–307. doi: 10.1016/j.yexcr.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 51.Scarlatti F, Bauvy C, Ventruti A, Sala G, Cluzeaud F, Vandewalle A, Ghidoni R, Codogno P. Ceramide-mediated macroautophagy involves inhibition of protein kinase B and up-regulation of beclin 1. J Biol Chem. 2004;279:18384–18391. doi: 10.1074/jbc.M313561200. [DOI] [PubMed] [Google Scholar]
- 52.Dai J, Su Y, Zhong S, Cong L, Liu B, Yang J, Tao Y, He Z, Chen C, Jiang Y. Exosomes: key players in cancer and potential therapeutic strategy. Signal Transduct Target Ther. 2020;5:145. doi: 10.1038/s41392-020-00261-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhu L, Li J, Gong Y, Wu Q, Tan S, Sun D, Xu X, Zuo Y, Zhao Y, Wei YQ, et al. Exosomal tRNA-derived small RNA as a promising biomarker for cancer diagnosis. Mol Cancer. 2019;18:74. doi: 10.1186/s12943-019-1000-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kahlert C, Melo SA, Protopopov A, Tang J, Seth S, Koch M, Zhang J, Weitz J, Chin L, Futreal A, Kalluri R. Identification of double-stranded genomic DNA spanning all chromosomes with mutated KRAS and p53 DNA in the serum exosomes of patients with pancreatic cancer. J Biol Chem. 2014;289:3869–3875. doi: 10.1074/jbc.C113.532267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kitai Y, Kawasaki T, Sueyoshi T, Kobiyama K, Ishii KJ, Zou J, Akira S, Matsuda T, Kawai T. DNA-containing Exosomes derived from Cancer cells treated with Topotecan activate a STING-dependent pathway and reinforce antitumor immunity. J Immunol. 2017;198:1649–1659. doi: 10.4049/jimmunol.1601694. [DOI] [PubMed] [Google Scholar]
- 56.Wang J, Chen D, Ho EA. Challenges in the development and establishment of exosome-based drug delivery systems. J Control Release. 2021;329:894–906. doi: 10.1016/j.jconrel.2020.10.020. [DOI] [PubMed] [Google Scholar]
- 57.Gardiner C, Di Vizio D, Sahoo S, Théry C, Witwer KW, Wauben M, Hill AF. Techniques used for the isolation and characterization of extracellular vesicles: results of a worldwide survey. J Extracell Vesicles. 2016;5:32945. doi: 10.3402/jev.v5.32945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li P, Kaslan M, Lee SH, Yao J, Gao Z. Progress in Exosome Isolation Techniques. Theranostics. 2017;7:789–804. doi: 10.7150/thno.18133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhu L, Sun HT, Wang S, Huang SL, Zheng Y, Wang CQ, Hu BY, Qin W, Zou TT, Fu Y, et al. Isolation and characterization of exosomes for cancer research. J Hematol Oncol. 2020;13:152. doi: 10.1186/s13045-020-00987-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rider MA, Hurwitz SN, Meckes DG., Jr ExtraPEG: a polyethylene glycol-based method for enrichment of extracellular vesicles. Sci Rep. 2016;6:23978. doi: 10.1038/srep23978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu M, Ouyang Y, Wang Z, Zhang R, Huang PH, Chen C, Li H, Li P, Quinn D, Dao M, et al. Isolation of exosomes from whole blood by integrating acoustics and microfluidics. Proc Natl Acad Sci U S A. 2017;114:10584–10589. doi: 10.1073/pnas.1709210114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu F, Vermesh O, Mani V, Ge TJ, Madsen SJ, Sabour A, Hsu EC, Gowrishankar G, Kanada M, Jokerst JV, et al. The exosome Total isolation Chip. ACS Nano. 2017;11:10712–10723. doi: 10.1021/acsnano.7b04878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Théry C, Witwer KW, Aikawa E, Alcaraz MJ, Anderson JD, Andriantsitohaina R, Antoniou A, Arab T, Archer F, Atkin-Smith GK, et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2018;7:1535750. doi: 10.1080/20013078.2018.1535750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yeo RW, Lai RC, Zhang B, Tan SS, Yin Y, Teh BJ, Lim SK. Mesenchymal stem cell: an efficient mass producer of exosomes for drug delivery. Adv Drug Deliv Rev. 2013;65:336–341. doi: 10.1016/j.addr.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 65.Lai RC, Arslan F, Lee MM, Sze NS, Choo A, Chen TS, Salto-Tellez M, Timmers L, Lee CN, El Oakley RM, et al. Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury. Stem Cell Res. 2010;4:214–222. doi: 10.1016/j.scr.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 66.Luo T, von der Ohe J, Hass R. MSC-derived extracellular vesicles in tumors and therapy. Cancers (Basel) 2021;13:5212. doi: 10.3390/cancers13205212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wen S, Dooner M, Cheng Y, Papa E, Del Tatto M, Pereira M, Deng Y, Goldberg L, Aliotta J, Chatterjee D, et al. Mesenchymal stromal cell-derived extracellular vesicles rescue radiation damage to murine marrow hematopoietic cells. Leukemia. 2016;30:2221–2231. doi: 10.1038/leu.2016.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hade MD, Suire CN, Suo Z. Mesenchymal stem cell-derived Exosomes: applications in regenerative medicine. Cells. 2021;10:1959. doi: 10.3390/cells10081959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu T, Zhang Q, Zhang J, Li C, Miao YR, Lei Q, Li Q, Guo AY. EVmiRNA: a database of miRNA profiling in extracellular vesicles. Nucleic Acids Res. 2019;47:D89–D93. doi: 10.1093/nar/gky985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Statello L, Maugeri M, Garre E, Nawaz M, Wahlgren J, Papadimitriou A, Lundqvist C, Lindfors L, Collen A, Sunnerhagen P, et al. Identification of RNA-binding proteins in exosomes capable of interacting with different types of RNA: RBP-facilitated transport of RNAs into exosomes. PLoS One. 2018;13:e0195969. doi: 10.1371/journal.pone.0195969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Squadrito ML, Baer C, Burdet F, Maderna C, Gilfillan GD, Lyle R, Ibberson M, De Palma M. Endogenous RNAs modulate microRNA sorting to exosomes and transfer to acceptor cells. Cell Rep. 2014;8:1432–1446. doi: 10.1016/j.celrep.2014.07.035. [DOI] [PubMed] [Google Scholar]
- 72.Wani S, Man Law IK, Pothoulakis C. Role and mechanisms of exosomal miRNAs in IBD pathophysiology. Am J Physiol Gastrointest Liver Physiol. 2020;319:G646–G654. doi: 10.1152/ajpgi.00295.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.O'Grady T, Njock MS, Lion M, Bruyr J, Mariavelle E, Galvan B, Boeckx A, Struman I, Dequiedt F. Sorting and packaging of RNA into extracellular vesicles shape intracellular transcript levels. BMC Biol. 2022;20:72. doi: 10.1186/s12915-022-01277-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Garcia-Martin R, Wang G, Brandao BB, Zanotto TM, Shah S, Kumar Patel S, Schilling B, Kahn CR. MicroRNA sequence codes for small extracellular vesicle release and cellular retention. Nature. 2022;601:446–451. doi: 10.1038/s41586-021-04234-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rani S, Ryan AE, Griffin MD, Ritter T. Mesenchymal stem cell-derived extracellular vesicles: toward cell-free therapeutic applications. Mol Ther. 2015;23:812–823. doi: 10.1038/mt.2015.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Baguley BC. Multiple drug resistance mechanisms in cancer. Mol Biotechnol. 2010;46:308–316. doi: 10.1007/s12033-010-9321-2. [DOI] [PubMed] [Google Scholar]
- 77.Weaver BA, Cleveland DW. Decoding the links between mitosis, cancer, and chemotherapy: the mitotic checkpoint, adaptation, and cell death. Cancer Cell. 2005;8:7–12. doi: 10.1016/j.ccr.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 78.Ghosh S. Cisplatin: the first metal based anticancer drug. Bioorg Chem. 2019;88:102925. doi: 10.1016/j.bioorg.2019.102925. [DOI] [PubMed] [Google Scholar]
- 79.Guerra F, Arbini AA, Moro L. Mitochondria and cancer chemoresistance. Biochim Biophys Acta Bioenerg. 2017;1858:686–699. doi: 10.1016/j.bbabio.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 80.Ji R, Zhang B, Zhang X, Xue J, Yuan X, Yan Y, Wang M, Zhu W, Qian H, Xu W. Exosomes derived from human mesenchymal stem cells confer drug resistance in gastric cancer. Cell Cycle. 2015;14:2473–2483. doi: 10.1080/15384101.2015.1005530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Phan TG, Croucher PI. The dormant cancer cell life cycle. Nat Rev Cancer. 2020;20:398–411. doi: 10.1038/s41568-020-0263-0. [DOI] [PubMed] [Google Scholar]
- 82.Ding DC, Chang YH, Shyu WC, Lin SZ. Human umbilical cord mesenchymal stem cells: a new era for stem cell therapy. Cell Transplant. 2015;24:339–347. doi: 10.3727/096368915X686841. [DOI] [PubMed] [Google Scholar]
- 83.Ohta N, Ishiguro S, Kawabata A, Uppalapati D, Pyle M, Troyer D, De S, Zhang Y, Becker KG, Tamura M. Human umbilical cord matrix mesenchymal stem cells suppress the growth of breast cancer by expression of tumor suppressor genes. PLoS One. 2015;10:e0123756. doi: 10.1371/journal.pone.0123756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li T, Xia M, Gao Y, Chen Y, Xu Y. Human umbilical cord mesenchymal stem cells: an overview of their potential in cell-based therapy. Expert Opin Biol Ther. 2015;15:1293–1306. doi: 10.1517/14712598.2015.1051528. [DOI] [PubMed] [Google Scholar]
- 85.Ma F, Chen D, Chen F, Chi Y, Han Z, Feng X, Li X, Han Z. Human umbilical cord Mesenchymal stem cells promote breast Cancer metastasis by Interleukin-8- and Interleukin-6-dependent induction of CD44(+)/CD24(−) cells. Cell Transplant. 2015;24:2585–2599. doi: 10.3727/096368915X687462. [DOI] [PubMed] [Google Scholar]
- 86.Yang J, Miao Y, Chang Y, Zhang F, Wang Y, Zheng S. Condition medium of HepG-2 cells induces the transdifferentiation of human umbilical cord mesenchymal stem cells into cancerous mesenchymal stem cells. Am J Transl Res. 2016;8:3429–3438. [PMC free article] [PubMed] [Google Scholar]
- 87.Yang Y, Bucan V, Baehre H, von der Ohe J, Otte A, Hass R. Acquisition of new tumor cell properties by MSC-derived exosomes. Int J Oncol. 2015;47:244–252. doi: 10.3892/ijo.2015.3001. [DOI] [PubMed] [Google Scholar]
- 88.Ono M, Kosaka N, Tominaga N, Yoshioka Y, Takeshita F, Takahashi RU, et al. Exosomes from bone marrow mesenchymal stem cells contain a microRNA that promotes dormancy in metastatic breast cancer cells. Sci Signal. 2014;7:ra63. [DOI] [PubMed]
- 89.Luo T, Liu Q, Tan A, Duan L, Jia Y, Nong L, Tang J, Zhou W, Xie W, Lu Y, et al. Mesenchymal stem cell-secreted exosome promotes Chemoresistance in breast Cancer via enhancing miR-21-5p-mediated S100A6 expression. Mol Ther Oncolytics. 2020;19:283–293. doi: 10.1016/j.omto.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Henkin RI. Clinical and therapeutic implications of Cancer stem cells. N Engl J Med. 2019;381:e19. doi: 10.1056/NEJMc1908886. [DOI] [PubMed] [Google Scholar]
- 91.Jia Z, Zhu H, Sun H, Hua Y, Zhang G, Jiang J, Wang X. Adipose Mesenchymal stem cell-derived Exosomal microRNA-1236 reduces resistance of breast Cancer cells to Cisplatin by suppressing SLC9A1 and the Wnt/beta-catenin signaling. Cancer Manag Res. 2020;12:8733–8744. doi: 10.2147/CMAR.S270200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Qiu L, Wang J, Chen M, Chen F, Tu W. Exosomal microRNA146a derived from mesenchymal stem cells increases the sensitivity of ovarian cancer cells to docetaxel and taxane via a LAMC2mediated PI3K/Akt axis. Int J Mol Med. 2020;46:609–620. doi: 10.3892/ijmm.2020.4634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dong B, Li S, Zhu S, Yi M, Luo S, Wu K. MiRNA-mediated EMT and CSCs in cancer chemoresistance. Exp Hematol Oncol. 2021;10:12. doi: 10.1186/s40164-021-00206-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Xu Y, Lai Y, Cao L, Li Y, Chen G, Chen L, et al. Human umbilical cord mesenchymal stem cells-derived exosomal microRNA-451a represses epithelial-mesenchymal transition of hepatocellular carcinoma cells by inhibiting ADAM10. RNA Biol. 2021;18:1408–1423. doi: 10.1080/15476286.2020.1851540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lee YT, Tan YJ, Oon CE. Molecular targeted therapy: treating cancer with specificity. Eur J Pharmacol. 2018;834:188–196. doi: 10.1016/j.ejphar.2018.07.034. [DOI] [PubMed] [Google Scholar]
- 96.Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376:687–697. doi: 10.1016/S0140-6736(10)61121-X. [DOI] [PubMed] [Google Scholar]
- 97.Chatterjee N, Bivona TG. Polytherapy and targeted Cancer drug resistance. Trends Cancer. 2019;5:170–182. doi: 10.1016/j.trecan.2019.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Viola S, Traer E, Huan J, Hornick NI, Tyner JW, Agarwal A, Loriaux M, Johnstone B, Kurre P. Alterations in acute myeloid leukaemia bone marrow stromal cell exosome content coincide with gains in tyrosine kinase inhibitor resistance. Br J Haematol. 2016;172:983–986. doi: 10.1111/bjh.13551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhang X, Yang Y, Yang Y, Chen H, Tu H, Li J. Exosomes from bone marrow microenvironment-derived Mesenchymal stem cells affect CML cells growth and promote drug resistance to tyrosine kinase inhibitors. Stem Cells Int. 2020;2020:8890201. doi: 10.1155/2020/8890201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hideshima T, Chauhan D, Richardson P, Anderson KC. Identification and validation of novel therapeutic targets for multiple myeloma. J Clin Oncol. 2005;23:6345–6350. doi: 10.1200/JCO.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 101.Xu H, Han H, Song S, Yi N, Qian C, Qiu Y, Zhou W, Hong Y, Zhuang W, Li Z, et al. Exosome-transmitted PSMA3 and PSMA3-AS1 promote proteasome inhibitor resistance in multiple myeloma. Clin Cancer Res. 2019;25:1923–1935. doi: 10.1158/1078-0432.CCR-18-2363. [DOI] [PubMed] [Google Scholar]
- 102.Berman E. How I treat chronic-phase chronic myelogenous leukemia. Blood. 2022;139:3138–3147. doi: 10.1182/blood.2021011722. [DOI] [PubMed] [Google Scholar]
- 103.Liu Y, Song B, Wei Y, Chen F, Chi Y, Fan H, Liu N, Li Z, Han Z, Ma F. Exosomes from mesenchymal stromal cells enhance imatinib-induced apoptosis in human leukemia cells via activation of caspase signaling pathway. Cytotherapy. 2018;20:181–188. doi: 10.1016/j.jcyt.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 104.Schaue D, McBride WH. Opportunities and challenges of radiotherapy for treating cancer. Nat Rev Clin Oncol. 2015;12:527–540. doi: 10.1038/nrclinonc.2015.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Barton MB, Jacob S, Shafiq J, Wong K, Thompson SR, Hanna TP, Delaney GP. Estimating the demand for radiotherapy from the evidence: a review of changes from 2003 to 2012. Radiother Oncol. 2014;112:140–144. doi: 10.1016/j.radonc.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 106.Ni J, Bucci J, Malouf D, Knox M, Graham P, Li Y. Exosomes in Cancer Radioresistance. Front Oncol. 2019;9:869. doi: 10.3389/fonc.2019.00869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chen F, Xu B, Li J, Yang X, Gu J, Yao X, Sun X. Hypoxic tumour cell-derived exosomal miR-340-5p promotes radioresistance of oesophageal squamous cell carcinoma via KLF10. J Exp Clin Cancer Res. 2021;40:38. doi: 10.1186/s13046-021-01834-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wan FZ, Chen KH, Sun YC, Chen XC, Liang RB, Chen L, Zhu XD. Exosomes overexpressing miR-34c inhibit malignant behavior and reverse the radioresistance of nasopharyngeal carcinoma. J Transl Med. 2020;18:12. doi: 10.1186/s12967-019-02203-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.de Araujo FV, O'Valle F, Serrano-Saenz S, Anderson P, Andres E, Lopez-Penalver J, Tovar I, Nieto A, Santos A, Martin F, et al. Exosomes derived from mesenchymal stem cells enhance radiotherapy-induced cell death in tumor and metastatic tumor foci. Mol Cancer. 2018;17:122. doi: 10.1186/s12943-018-0867-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Li X, Wenes M, Romero P, Huang SC, Fendt SM, Ho PC. Navigating metabolic pathways to enhance antitumour immunity and immunotherapy. Nat Rev Clin Oncol. 2019;16:425–441. doi: 10.1038/s41571-019-0203-7. [DOI] [PubMed] [Google Scholar]
- 111.van den Bulk J, Verdegaal EM, de Miranda NF. Cancer immunotherapy: broadening the scope of targetable tumours. Open Biol. 2018;8:180037. [DOI] [PMC free article] [PubMed]
- 112.Kochenderfer JN, Wilson WH, Janik JE, Dudley ME, Stetler-Stevenson M, Feldman SA, Maric I, Raffeld M, Nathan DA, Lanier BJ, et al. Eradication of B-lineage cells and regression of lymphoma in a patient treated with autologous T cells genetically engineered to recognize CD19. Blood. 2010;116:4099–4102. doi: 10.1182/blood-2010-04-281931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.McGranahan N, Furness AJ, Rosenthal R, Ramskov S, Lyngaa R, Saini SK, Jamal-Hanjani M, Wilson GA, Birkbak NJ, Hiley CT, et al. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science. 2016;351:1463–1469. doi: 10.1126/science.aaf1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, Lu S, Kemberling H, Wilt C, Luber BS, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–413. doi: 10.1126/science.aan6733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chan TA, Wolchok JD, Snyder A. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 1984;2015:373. doi: 10.1056/NEJMc1508163. [DOI] [PubMed] [Google Scholar]
- 116.Sharma P, Hu-Lieskovan S, Wargo JA, Ribas A. Primary, adaptive, and acquired resistance to Cancer immunotherapy. Cell. 2017;168:707–723. doi: 10.1016/j.cell.2017.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Thery C, Ostrowski M, Segura E. Membrane vesicles as conveyors of immune responses. Nat Rev Immunol. 2009;9:581–593. doi: 10.1038/nri2567. [DOI] [PubMed] [Google Scholar]
- 118.Zhang PF, Gao C, Huang XY, Lu JC, Guo XJ, Shi GM, Cai JB, Ke AW. Cancer cell-derived exosomal circUHRF1 induces natural killer cell exhaustion and may cause resistance to anti-PD1 therapy in hepatocellular carcinoma. Mol Cancer. 2020;19:110. doi: 10.1186/s12943-020-01222-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Liu H, Liang Z, Wang F, Zhou C, Zheng X, Hu T, et al. Exosomes from mesenchymal stromal cells reduce murine colonic inflammation via a macrophage-dependent mechanism. JCI Insight. 2019;4:e131273. [DOI] [PMC free article] [PubMed]
- 120.Biswas S, Mandal G, Roy Chowdhury S, Purohit S, Payne KK, Anadon C, Gupta A, Swanson P, Yu X, Conejo-Garcia JR, Bhattacharyya A. Exosomes produced by Mesenchymal stem cells drive differentiation of myeloid cells into immunosuppressive M2-polarized macrophages in breast Cancer. J Immunol. 2019;203:3447–3460. doi: 10.4049/jimmunol.1900692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhou W, Zhou Y, Chen X, Ning T, Chen H, Guo Q, Zhang Y, Liu P, Zhang Y, Li C, et al. Pancreatic cancer-targeting exosomes for enhancing immunotherapy and reprogramming tumor microenvironment. Biomaterials. 2021;268:120546. doi: 10.1016/j.biomaterials.2020.120546. [DOI] [PubMed] [Google Scholar]
- 122.Lou G, Song X, Yang F, Wu S, Wang J, Chen Z, Liu Y. Exosomes derived from miR-122-modified adipose tissue-derived MSCs increase chemosensitivity of hepatocellular carcinoma. J Hematol Oncol. 2015;8:122. doi: 10.1186/s13045-015-0220-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lou G, Chen L, Xia C, Wang W, Qi J, Li A, Zhao L, Chen Z, Zheng M, Liu Y. MiR-199a-modified exosomes from adipose tissue-derived mesenchymal stem cells improve hepatocellular carcinoma chemosensitivity through mTOR pathway. J Exp Clin Cancer Res. 2020;39:4. doi: 10.1186/s13046-019-1512-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yu L, Gui S, Liu Y, Qiu X, Zhang G, Zhang X, Pan J, Fan J, Qi S, Qiu B. Exosomes derived from microRNA-199a-overexpressing mesenchymal stem cells inhibit glioma progression by down-regulating AGAP2. Aging (Albany NY) 2019;11:5300–5318. doi: 10.18632/aging.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Munoz JL, Bliss SA, Greco SJ, Ramkissoon SH, Ligon KL, Rameshwar P. Delivery of functional anti-miR-9 by Mesenchymal stem cell-derived Exosomes to Glioblastoma Multiforme cells conferred Chemosensitivity. Mol Ther Nucleic Acids. 2013;2:e126. doi: 10.1038/mtna.2013.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wang B, Wu ZH, Lou PY, Chai C, Han SY, Ning JF, Li M. Human bone marrow-derived mesenchymal stem cell-secreted exosomes overexpressing microRNA-34a ameliorate glioblastoma development via down-regulating MYCN. Cell Oncol (Dordr) 2019;42:783–799. doi: 10.1007/s13402-019-00461-z. [DOI] [PubMed] [Google Scholar]
- 127.Sharif S, Ghahremani MH, Soleimani M. Delivery of exogenous miR-124 to Glioblastoma multiform cells by Wharton’s jelly Mesenchymal stem cells decreases cell proliferation and migration, and confers Chemosensitivity. Stem Cell Rev Rep. 2017;14:236–246. doi: 10.1007/s12015-017-9788-3. [DOI] [PubMed] [Google Scholar]
- 128.Wu H, Mu X, Liu L, Wu H, Hu X, Chen L, Liu J, Mu Y, Yuan F, Liu W, Zhao Y. Bone marrow mesenchymal stem cells-derived exosomal microRNA-193a reduces cisplatin resistance of non-small cell lung cancer cells via targeting LRRC1. Cell Death Dis. 2020;11:801. doi: 10.1038/s41419-020-02962-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Li H, Yang C, Shi Y, Zhao L. Exosomes derived from siRNA against GRP78 modified bone-marrow-derived mesenchymal stem cells suppress Sorafenib resistance in hepatocellular carcinoma. J Nanobiotechnology. 2018;16:103. doi: 10.1186/s12951-018-0429-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Sun Y, Liu G, Zhang K, Cao Q, Liu T, Li J. Mesenchymal stem cells-derived exosomes for drug delivery. Stem Cell Res Ther. 2021;12:561. doi: 10.1186/s13287-021-02629-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Qiu Y, Sun J, Qiu J, Chen G, Wang X, Mu Y, Li K, Wang W. Antitumor activity of Cabazitaxel and MSC-TRAIL derived extracellular vesicles in drug-resistant Oral squamous cell carcinoma. Cancer Manag Res. 2020;12:10809–10820. doi: 10.2147/CMAR.S277324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wei HX, Chen JY, Wang SL, Fu FH, Zhu X, Wu CY, Liu ZJ, Zhong GX, Lin JH. A Nanodrug consisting of doxorubicin and exosome derived from Mesenchymal stem cells for osteosarcoma treatment in vitro. Int J Nanomedicine. 2019;14:8603–8610. doi: 10.2147/IJN.S218988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bagheri E, Abnous K, Farzad SA, Taghdisi SM, Ramezani M, Alibolandi M. Targeted doxorubicin-loaded mesenchymal stem cells-derived exosomes as a versatile platform for fighting against colorectal cancer. Life Sci. 2020;261:118369. [DOI] [PubMed]
- 134.Pascucci L, Cocce V, Bonomi A, Ami D, Ceccarelli P, Ciusani E, Vigano L, Locatelli A, Sisto F, Doglia SM, et al. Paclitaxel is incorporated by mesenchymal stromal cells and released in exosomes that inhibit in vitro tumor growth: a new approach for drug delivery. J Control Release. 2014;192:262–270. doi: 10.1016/j.jconrel.2014.07.042. [DOI] [PubMed] [Google Scholar]
- 135.Melzer C, Rehn V, Yang Y, Bahre H, von der Ohe J, Hass R. Taxol-loaded MSC-derived Exosomes provide a therapeutic vehicle to target metastatic breast cancer and other carcinoma cells. Cancers (Basel) 2019;11:798. doi: 10.3390/cancers11060798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zhou Y, Zhou W, Chen X, Wang Q, Li C, Chen Q, Zhang Y, Lu Y, Ding X, Jiang C. Bone marrow mesenchymal stem cells-derived exosomes for penetrating and targeted chemotherapy of pancreatic cancer. Acta Pharm Sin B. 2020;10:1563–1575. doi: 10.1016/j.apsb.2019.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Rauf A, Patel S, Imran M, Maalik A, Arshad MU, Saeed F, Mabkhot YN, Al-Showiman SS, Ahmad N, Elsharkawy E. Honokiol: An anticancer lignan. Biomed Pharmacother. 2018;107:555–562. doi: 10.1016/j.biopha.2018.08.054. [DOI] [PubMed] [Google Scholar]
- 138.Kanchanapally R, Khan MA, Deshmukh SK, Srivastava SK, Khushman M, Singh S, Singh AP. Exosomal formulation escalates cellular uptake of Honokiol leading to the enhancement of its antitumor efficacy. ACS Omega. 2020;5:23299–23307. doi: 10.1021/acsomega.0c03136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zhou J, Ren Y, Tan L, Song X, Wang M, Li Y, Cao Z, Guo C. Norcantharidin: research advances in pharmaceutical activities and derivatives in recent years. Biomed Pharmacother. 2020;131:110755. doi: 10.1016/j.biopha.2020.110755. [DOI] [PubMed] [Google Scholar]
- 140.Liang L, Zhao L, Wang Y, Wang Y. Treatment for hepatocellular carcinoma is enhanced when Norcantharidin is encapsulated in Exosomes derived from bone marrow Mesenchymal stem cells. Mol Pharm. 2021;18:1003–1013. doi: 10.1021/acs.molpharmaceut.0c00976. [DOI] [PubMed] [Google Scholar]
- 141.De Ruysscher D, Niedermann G, Burnet NG, Siva S, Lee AWM, Hegi-Johnson F. Radiotherapy toxicity. Nat Rev Dis Primers. 2019;5:13. doi: 10.1038/s41572-019-0064-5. [DOI] [PubMed] [Google Scholar]
- 142.Rodgers K, Jadhav SS. The application of mesenchymal stem cells to treat thermal and radiation burns. Adv Drug Deliv Rev. 2018;123:75–81. doi: 10.1016/j.addr.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 143.Kink JA, Forsberg MH, Reshetylo S, Besharat S, Childs CJ, Pederson JD, Gendron-Fitzpatrick A, Graham M, Bates PD, Schmuck EG, et al. Macrophages educated with Exosomes from primed Mesenchymal stem cells treat acute radiation syndrome by promoting hematopoietic recovery. Biol Blood Marrow Transplant. 2019;25:2124–2133. doi: 10.1016/j.bbmt.2019.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zuo R, Liu M, Wang Y, Li J, Wang W, Wu J, Sun C, Li B, Wang Z, Lan W, et al. BM-MSC-derived exosomes alleviate radiation-induced bone loss by restoring the function of recipient BM-MSCs and activating Wnt/beta-catenin signaling. Stem Cell Res Ther. 2019;10:30. doi: 10.1186/s13287-018-1121-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Li Y, Shen Z, Jiang X, Wang Y, Yang Z, Mao Y, Wu Z, Li G, Chen H. Mouse mesenchymal stem cell-derived exosomal miR-466f-3p reverses EMT process through inhibiting AKT/GSK3beta pathway via c-MET in radiation-induced lung injury. J Exp Clin Cancer Res. 2022;41:128. doi: 10.1186/s13046-022-02351-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Crescitelli R, Lasser C, Lotvall J. Isolation and characterization of extracellular vesicle subpopulations from tissues. Nat Protoc. 2021;16:1548–1580. doi: 10.1038/s41596-020-00466-1. [DOI] [PubMed] [Google Scholar]
- 147.Yang D, Zhang W, Zhang H, Zhang F, Chen L, Ma L, Larcher LM, Chen S, Liu N, Zhao Q, et al. Progress, opportunity, and perspective on exosome isolation - efforts for efficient exosome-based theranostics. Theranostics. 2020;10:3684–3707. doi: 10.7150/thno.41580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ibsen SD, Wright J, Lewis JM, Kim S, Ko SY, Ong J, Manouchehri S, Vyas A, Akers J, Chen CC, et al. Rapid isolation and detection of Exosomes and associated biomarkers from plasma. ACS Nano. 2017;11:6641–6651. doi: 10.1021/acsnano.7b00549. [DOI] [PubMed] [Google Scholar]
- 149.Zhou H, Zhu L, Song J, Wang G, Li P, Li W, Luo P, Sun X, Wu J, Liu Y, et al. Liquid biopsy at the frontier of detection, prognosis and progression monitoring in colorectal cancer. Mol Cancer. 2022;21:86. doi: 10.1186/s12943-022-01556-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lu M, Huang Y. Bioinspired exosome-like therapeutics and delivery nanoplatforms. Biomaterials. 2020;242:119925. doi: 10.1016/j.biomaterials.2020.119925. [DOI] [PubMed] [Google Scholar]
- 151.Li YJ, Wu JY, Liu J, Xu W, Qiu X, Huang S, Hu XB, Xiang DX. Artificial exosomes for translational nanomedicine. J Nanobiotechnology. 2021;19:242. doi: 10.1186/s12951-021-00986-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kalimuthu S, Gangadaran P, Rajendran RL, Zhu L, Oh JM, Lee HW, Gopal A, Baek SH, Jeong SY, Lee SW, et al. A new approach for loading anticancer drugs into Mesenchymal stem cell-derived exosome Mimetics for Cancer therapy. Front Pharmacol. 2018;9:1116. doi: 10.3389/fphar.2018.01116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Li Z, Zhou X, Gao X, Bai D, Dong Y, Sun W, Zhao L, Wei M, Yang X, Yang G, Yuan L. Fusion protein engineered exosomes for targeted degradation of specific RNAs in lysosomes: a proof-of-concept study. J Extracell Vesicles. 2020;9:1816710. doi: 10.1080/20013078.2020.1816710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29:341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 155.Ohno S, Takanashi M, Sudo K, Ueda S, Ishikawa A, Matsuyama N, Fujita K, Mizutani T, Ohgi T, Ochiya T, et al. Systemically injected exosomes targeted to EGFR deliver antitumor microRNA to breast cancer cells. Mol Ther. 2013;21:185–191. doi: 10.1038/mt.2012.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Liang Y, Duan L, Lu J, Xia J. Engineering exosomes for targeted drug delivery. Theranostics. 2021;11:3183–3195. doi: 10.7150/thno.52570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.de Abreu RC, Fernandes H, da Costa Martins PA, Sahoo S, Emanueli C, Ferreira L. Native and bioengineered extracellular vesicles for cardiovascular therapeutics. Nat Rev Cardiol. 2020;17:685–697. doi: 10.1038/s41569-020-0389-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.