Key Points
Question
Are nonpharmacological interventions effective in lengthening sleep duration in healthy children, and if so, what are the key elements?
Findings
In this systematic review and meta-analysis of 45 trials, interventions to improve sleep in healthy children were associated with a small increase in sleep duration (by 10 minutes per night). Face-to-face delivery was an important component of interventions, but interventions that included earlier bedtimes were associated with 47 minutes longer sleep duration per night.
Meaning
Supporting children to go to bed earlier can increase sleep duration in healthy children, and interventions to encourage earlier bedtimes should be included.
This systematic review and meta-analysis evaluates whether nonpharmaceutical interventions to improve sleep duration in healthy children are effective and identifies the key components of these interventions.
Abstract
Importance
Adequate sleep duration is necessary for many aspects of child health, development, and well-being, yet sleep durations for children are declining, and effective strategies to increase sleep in healthy children remain to be elucidated.
Objective
To determine whether nonpharmaceutical interventions to improve sleep duration in healthy children are effective and to identify the key components of these interventions.
Data Sources
CENTRAL, MEDLINE, Embase, PsycINFO, Web of Science Core collection, ClinicalTrials.gov, and WHO trials databases were searched from inception to November 15, 2021.
Study Selection
Randomized clinical trials of interventions to improve sleep duration in healthy children were independently screened by 2 researchers. A total of 28 478 studies were identified.
Data Extraction and Synthesis
Data were processed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) reporting guideline. Random-effects meta-analytic models were used to estimate pooled effect sizes.
Main Outcomes and Measures
Difference in sleep duration, measured in minutes.
Results
A total of 13 539 child participants from 45 randomized clinical trials were included. Of these, 6897 (50.9%) were in the intervention group and 6642 (49.1%) in the control group, and the mean age ranged from 18 months to 19 years. Pooled results indicate that sleep interventions were associated with 10.5 minutes (95% CI, 5.6-15.4) longer nocturnal sleep duration. There was substantial variation between trials. Sources of variation that were not associated with the study effect size included age group, whether the population was identified as having a sleep problem or being at a socioeconomic disadvantage (eg, coming from a low-income family or area), method of assessment of sleep duration (objective vs subjective), location of intervention delivery (home vs school), whether interventions were delivered in person or used parental involvement, whether behavioral theory was used, environmental change, or had greater or lower intensity. Interventions that included earlier bedtimes were associated with a 47-minute sleep extension (95% CI, 18.9-75.0; 3 trials) compared with remaining studies (7.4 minutes; 95% CI, 2.9-11.8; 42 trials) (P = .006 for group difference). Trials of shorter duration (6 months or less) had larger effects.
Conclusions and Relevance
Interventions focused on earlier bedtimes may offer a simple, pragmatic, effective way to meaningfully increase sleep duration that could have important benefits for child health.
Introduction
Early childhood experiences and development can have a significant impact on subsequent health, and adequate sleep during childhood is a critical component of well-being. Healthy sleep involves a combination of appropriate sleep timing, quality, and duration.1,2 Sleep in children is vital for appropriate growth, cognitive processing, mental well-being, effective social interactions, and metabolic health.3,4,5,6
Marked differences in sleep patterns are observed through childhood, with declines in sleep duration with increasing age. Guidance from the US National Sleep Foundation recommends that toddlers age 1 to 2 years should sleep 11 to 14 hours per night, preschool-aged children age 3 to 5 years should sleep 10 to 13 hours, school-aged children age 6 to 13 years should sleep 9 to 11 hours, and teenagers age 14 to 17 years should sleep 8 to 10 hours,1 with similar decreasing sleep durations with increasing child age in the UK,7 reflecting the changes in circadian rhythm and homeostatic sleep processes during child development. While these recommendations are not derived from systematic reviews and meta-analysis of the evidence, they represent the best available consensus from a multidisciplinary expert panel.1 Unfortunately, fewer children are achieving these recommendations, with a trend toward shorter sleep durations,8,9,10,11 where currently one-third or less of younger children and adolescents are achieving adequate sleep durations.8,9,10 These short sleep durations have been attributed to increased screen time, electronic media use, stimulant intake (particularly caffeine),12,13,14,15,16,17,18,19 and increasing emergence of unhealthy sleep behaviors, including poor bedtime routines (such as irregular sleep timings and unsupportive environments).20,21
Effective strategies are therefore needed to encourage healthy sleep and optimize sleep behavior in children. Recent systematic reviews and meta-analyses largely of intervention studies have focused on those with sleep problems and/or medical issues22,23,24 restricted to narrow age groups,21,25,26,27,28 including infants and preschoolers where circadian sleep patterns are not yet fully established,26,27,28 have also considered suboptimal nonexperimental studies26 and have lacked sufficient evidence to unravel the role of single component vs multicomponent interventions as part of broader health improvement agendas.21 Most reviews to date have also been narrative, which may reflect a lack of standardization in reporting sleep-related outcomes, particularly sleep duration.25 Of the few meta-analyses that have quantified overall intervention effects, pooled estimates have been modest at best.26 Increasingly, objective measurements are being used, which limits comparisons with previously reported self-reported or parent-reported sleep.26
Interventions in school-aged children may offer an ideal age group to alter nocturnal sleep behavior, given circadian sleep patterns are well established, and scope to deliver interventions within both school and home settings. Hence, we have carried out an up-to-date systematic review of intervention studies to promote optimal sleep patterns in all children, including those of school age (aged 1 to 18 years).
The main aim of this systematic review and meta-analysis was to estimate the effectiveness of sleep-related interventions in healthy children. Secondary aims included subgroup exploration to identify which sleep-related intervention components are most or least effective and to estimate the effect size of these different elements.
Methods
This systematic review and meta-analysis was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline,29 aligned with the EQUATOR reporting guidelines. The protocol was registered on PROSPERO (CRD42019160089).
Eligibility Criteria
Eligible studies were both individual and cluster randomized clinical trials (RCTs) at both the class and school level investigating interventions to affect sleep duration in children aged 1 to 18 years without a known medical condition or disability. Studies were excluded if they included infants younger than 1 year, those with a formal diagnosis of a sleep disorder, or use of pharmacological interventions. Pharmacological interventions are not recommended as first-line therapy for sleep improvement and differ from behavioral interventions.30
The sleep-related intervention could be stand-alone or part of a multicomponent health promotion strategy, eg, addressing obesity. The comparator group could be delayed intervention, alternative child health or safety advice, or usual care. The primary outcome was change in mean self-reported, parent-reported, or objectively measured daily total sleep time (in minutes) in children receiving the intervention compared with controls. Non-English language studies were excluded at the full-text screening stage.
Additional proposed outcomes were change in measures of sleep quality (based on study-specific subjective scales) and sleep hygiene (based on study-specific sleep hygiene scales). However, due to the heterogeneity of these measures and lack of consistency between studies, it was not possible to meaningfully synthesize these outcomes.
Search Strategy
We carried out searches using both text words and Medical Subject Headings/index terms in 7 databases: CENTRAL, MEDLINE (Ovid), Embase (Ovid), PsycINFO (Ovid), Web of Science Core Collection, ClinicalTrials.gov, and World Health Organization trials databases. Searches were carried out from database inception to November 15, 2021. The search strategy used is provided in eTable 1 in the Supplement.
We used the Cochrane RCT Classifier31 for an initial assessment of the results. Following this, all remaining titles and abstracts were screened independently by 2 reviewers using Covidence version 1.0,32 with discrepancies resolved by a third reviewer (L.M., U.A.R.C., A.S.D., C.W., C.M.N., A.R.R., C.G.O.). Full-text screening was carried out independently by 2 reviewers in the research group, and disagreements were resolved with a third reviewer (L.M., A.S.D., C.W.).
Data Extraction
Study information was extracted using the Covidence data extraction form, edited to include relevant fields specific to this review, including details about the study population, intervention design, and delivery. Use of theory in the interventions was assessed using a framework33 that has been used in previous systematic reviews,34,35 assessed against 4 levels: informed by theory, applied theory, testing theory, and building theory. Data were extracted by 2 reviewers independently, with discrepancies discussed and resolved with a third reviewer (L. M., A. S. D., and C. W.), as necessary.
Quantitative data were extracted using a structured data extraction sheet in Microsoft Excel version 2205. The data extraction sheet was piloted on 6 trials by 2 of us (U. A. R. C. and C. G. O.). Extraction included data in different forms (eg, means at end point or change-on-change), using different measurement methods (eg, actigraphy or self-report/parent-report) related to sleep at different times of the week (eg, weekend or weekday) and at different follow-up periods. Quantitative data extraction was undertaken independently by 2 reviewers, with discrepancies discussed and resolved with a third reviewer where necessary (U. A. R. C., L. P. G., and A. R. R.). Due to reporting inconsistency of intervention length and follow-up period, these were combined under study period.
Study Quality
Cochrane’s Risk of Bias tool36 was chosen over alternative instruments, as it is sensitive to variation in the quality of RCTs. Two reviewers independently scored the domains (selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases) prior to data analysis, with discrepancies resolved by a third reviewer (L. M., C. W., and A. S. D.).
Statistical Analysis
We used Cochrane’s Review Manager version 5.4 to calculate effect estimates (in minutes) and associated 95% CI, using a random-effects mean difference model. Trials were excluded if the number of participants at follow-up could not be established. The comparator group was split to avoid double counting in 3-arm trials, and where a study did not report pooled results for the entire sample, effects reported were combined using a fixed-effects meta-analysis. Adjusted effect estimates were preferred over unadjusted estimates, and the longest follow-up period was selected for inclusion where multiple follow-up periods were reported. Data for weekday sleep were used in preference to weekend sleep.
Further analyses were performed in Stata version 17 (StataCorp) using metan and metareg commands. Subgroup analyses, examining differences in effect estimates for different populations (eg, by age group, continent, reported social deprivation, self-identified sleep problem), and study design features (eg, method of measuring of sleep duration, length of intervention, location, and mode of delivery) were performed using 2-tailed z tests with statistical significance defined as P < .05. Statistical heterogeneity was assessed using the I2 statistic and P values. An I2 value of 50% to 75% suggested moderate heterogeneity and of 75% or greater suggested high heterogeneity.37 We assessed publication bias by visual examination of funnel plots, and using Begg and Egger tests, overall and by subgroups.
Results
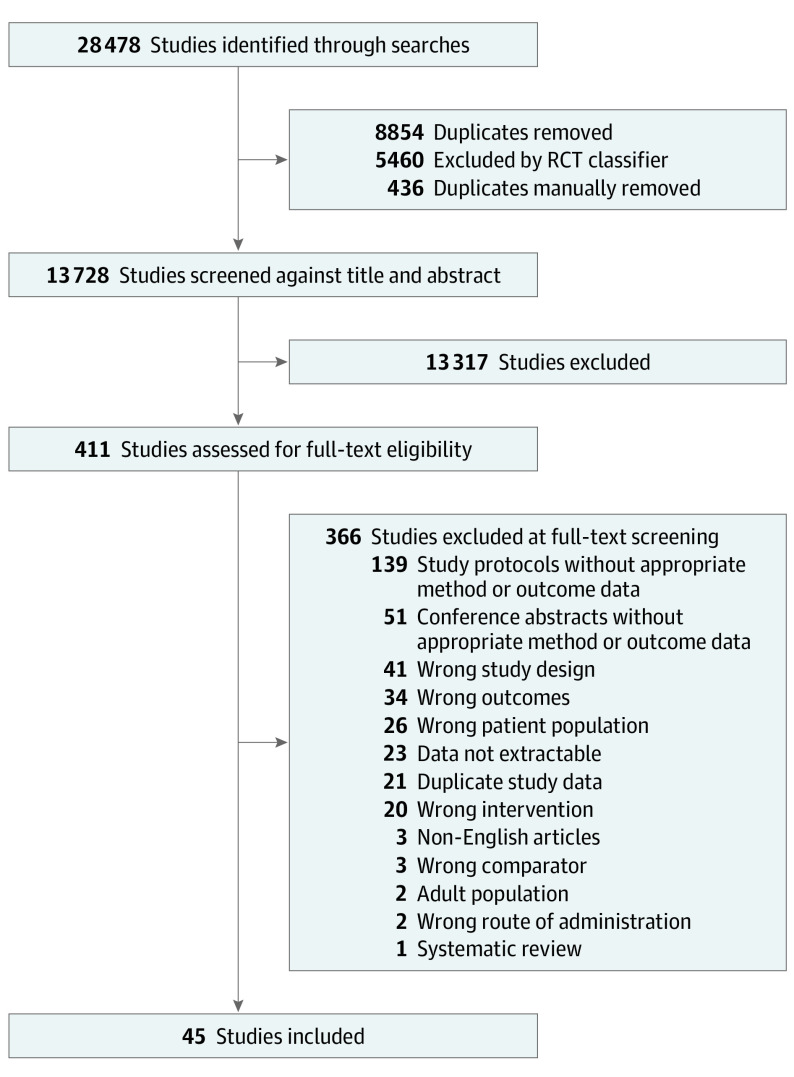
A total of 28 478 studies were identified, of which 8854 were duplicates. The RCT Classifier excluded 5460 records and a further 436 duplicates were identified, resulting in 13 728 studies to be screened. After screening of titles and abstracts, 411 potentially relevant full-text articles were screened. Figure 1 shows the article selection process. In total, 13 539 child participants from 45 RCTs with 47 estimates of mean differences in sleep duration between intervention and control groups were included in the analyses. Of these, 6897 (50.9%) were in the intervention group and 6642 (49.1%) in the control group, and the mean age ranged from 18 months to 19 years. The key characteristics of selected trials and interventions are shown in Table 1; more detailed characteristics can be seen in eTable 2 in the Supplement and study estimates can be seen in eTable 3 in the Supplement. Of 45 trials, 10 were in preschool-aged children, 11 in primary school–aged children, and 26 in secondary school–aged children.
Figure 1. Study Selection Process.
Table 1. Study Characteristics.
| Source | Age | Target population | Settinga | Inclusion criteria | Mode of delivery | Intervention overview b,c | Dose | Intervention duration | Study duration |
|---|---|---|---|---|---|---|---|---|---|
| Beijamini and Louzada,38 2012 | Range, 13-14 y | School students in public high schools | School | General population | Face-to-face | Educational program of 4 themed lessons on sleepb | 4× 50-min Lessons over 5 d | <1 wk | 3 wk |
| Blake et al,39 2016d | Range, 12-16 y | Students in year 7-10 at risk of major depressive disorder | Secondary schools | High levels of anxiety and sleeping difficulties but without a depressive disorder | Face-to-face | Sleep education program, including 7 sessions and information book | 7× 90-min Sessions | 7 wk | 9 wk |
| Delli Bovi et al,40 2021 | Range, 6-14 y | Obese children | Pediatric obesity clinic in university hospital | BMI >95th percentile for age and sex according to the CDC 2000 growth curves | Face-to-face group sessions and WhatsApp texts | Clinician-led group sessions on health, including nutrition and physical activity | Group session with 3 messages a week for 24 wk or as above plus monthly in-person visits (4× over 6 mo) | 24 wk | 9 mo |
| Cain et al,41 2011 | Range, 16-17 y | Psychology students | Secondary schools | Students with discrepant weekday-weekend out-of-bed times (>2 h) and insufficient sleep on school nights (<8 h) | Face-to-face | Sleep education classes and motivational interviewing frameworkb | 4× 50-min Sessions | 4 wk | 6 wk |
| Cepni et al,42 2021 | Range, 12-36 mo | Parent-toddler dyads | Home environment | Low-income and ethnically diverse general population | Face-to-face, text reminders | Trained facilitators and health workers delivered health information and positive parenting coaching | 10× 90-min Sessions, delivered weekly | 10 wk | 12 wk |
| Dewald-Kaufmann et al,43 2013 | Range, 12-19 y | Adolescents with chronic sleep reduction | School with home phone calls | Adolescents with a Chronic Sleep Reduction Questionnaire (CSRQ) score ≥40 | Face-to-face and telephone | Personal sleep schedule to gradually extend sleep by 10 min per night | Daily sleep schedule provided for 2 wk | 2 wk | 3 wk |
| Dong et al,44 2020 | Range, 10-18 y | Adolescents with eveningness chronotype | University-based clinic | Reported eveningness and 7-d sleep diary with late sleep time | Face-to-face | Promoting behavior change via 4 cross-cutting modules (functional analysis, goal setting, motivational interviewing, and education) | 6× 50-min Sessions, delivered weekly | 6 wk | 6 mo |
| Haines et al,45 2013 | Range, 2-5 y | Ethnic minority and low-income families | Community health centers in deprived areas | Low-income and ethnically diverse general population with a television in their room | Face-to-face, phone calls, texts, and printed information | Motivational coaching to adopt healthy routines to reduce obesity | 4× Home visits, 4× phone calls, weekly text messages | 24 wk | 24 wk |
| Hammersley et al,46 2019 | Range, 2-5 y | Parent-child dyads | Home environment | General population (healthy weight and overweight) | Online | Online modules targeting multiple behaviors, including sleep | 6× 30-min Modules to complete over 11 wk, weekly email reminders | 23 wk | 24 wk |
| Hammersely et al,47 2021 | Range, 2-6 y | Children aged 2-6 y | Home environment | General population | Telephone and online | Modules targeting multiple behaviors including sleep via telephone calls or online modules | 6× 30-min Telephone calls or 6 online modules | 3 mo | 9 mo |
| Hart et al,48 2017, and Hart et al,49 2016 | Range, 8-11 y | Children aged 8-11 y | Not stated | General population | Face to face, telephone | Behavioral strategies (eg, goal setting, stimulus control, positive reinforcement) to increase time in bed by 1.5 h | 4 Sessions over 8 wk (week 1, 60 min; week 2, 30 min; telephone week 4 and week 6) | 8 wk | 8 wk |
| Hiscock et al,50 2019 | Range, 5-6 y | Children with sleep problems in the first year of schooling | Primary schools | Parent report of moderate or severe sleep problems | Face-to-face, follow-up phone call | Nurse-led consultation, providing information on good sleep practice and new sleep routine | 1× 45-min Consultation, 10-min follow-up phone call, optional 20-min consultation | 4 wk | 52 wk |
| Kalak et al,51 2012 | Range, 17-19 y | School students | Secondary school | General population | Face-to-face | Daily morning run at school in small groups | 30-min Run weekdays for 3 wk | 3 wk | 3 wk |
| Kira et al,52 2014 | Range, 13-16 y | School students | Secondary school | General population | Face-to-face plus workbook | A sleep educational program, including small group discussionsb | 4× 50-min Sessions | 4 wk | 10 wk |
| Knebel et al,53 2020 | Range, 11-15 y | School students | Secondary school | General population | Face-to-face | Program to increase physical activity and reduce sedentary time, teacher training, environmental improvements, and health educationc | Structures created and equipment provided to encourage physical activity and teachers encouraged to use | 39 wk | 39 wk |
| Lin et al,54 2018 | Median, 15 y | School students | Secondary school | General population | Face-to-face | A sleep education program, encouraging behavior change with individual plan and parental involvement | 4× 1-h Sessions every 2 wk | 8 wk | 24 wk |
| Lufi et al,55 2011 | Range, 13-14 y | School students | Secondary school | General population | Restructure environment | School start time delayed for 1 hb | Daily for 1 wk | 1 wk | 2 wk |
| Marsh et al,56 2020 | Range, 2-4 y | Parent-child dyads | Clinic and home | Children whose daily screen use exceeded recommendations (≥1 h per day) | Face-to-face and online | Workshop and online materials aimed to promote positive parent-child interactions at bedtime, mealtimes, and when restricting screen time | A half-day workshop and subsequent access to the study website over a 6-wk period | 6 wk | 12 wk |
| Mindell et al,57 2009 | Range, 18-36 mo | Mother-child dyads | Home | Mother reported small to severe sleep problem, but not a sleep disorder | Face-to-face | A nightly 3-step bedtime routine (bath, massage, quiet activities), lights out within 30 min of end of bath | Everyday | 2 wk | 3 wk |
| Mindell et al,58 2016 | Range, 2-12 y | Socioeconomically disadvantaged children | Home | Children from low income households without proper bedding | Face-to-face and restructured environment | Sleep education messages for parents | Messages provided twice: week 1 and week 4 | 4 wk | 4 wk |
| Mitchell et al,59 2021 | Range, 10-12 y | Children aged 10-12 y | Home | Parent/guardian report of typically 8-9 h in bed | Online | Mobile health platform used to send goal achievement messages around bedtimes | Daily messages over a 7-wk period | 7 wk | 9 wk |
| Moore et al,60 2019 | Range, 11-12 y | Low-income children, racial minority children, and children with overweight or obesity | Middle school | Children with BMI ≥85th percentile, entering 6th grade | Face-to-face and telephone | 2 Active arms: healthy change, behavioral strategies used in CBT and motivational interviewing; system change, emphasis on restructuring family daily routines | 25 Face-to-face sessions in year 1, alternating monthly face-to-face and phone sessions year 2, 4 face-to-face sessions and 8 phone sessions in year 3 | 156 wk | 3 y (annual data collection) |
| Morell-Azanza et al,61 2019 | Range, 7-16 y | Children with abdominal obesity | Clinical | Waist circumference >90th percentile, according to national data | Face-to-face | Family-based lifestyle program with education sessions around diet | 6× 30-min Sessions | 8 wk | 8 wk |
| Moseley and Gradisar,62 2009 | Median, 15.6 y | Year 11 psychology students with delayed sleep | Secondary school | Adolescents with discrepant out-of-bed times (school vs weekend mornings >2 h) and insufficient sleep on school nights | Face-to-face | Education sessions promoting and maintaining a healthy lifestyle using a CBT frameworkb | 4× 50-min Sessions | 4 wk | 6 wk |
| Moula et al,63 2020 | Range, 7-10 y | Primary school children | Primary school | Children with mild emotional and behavioral difficulties | Face-to-face | Art therapies | 1-h per wk for 8 wk | 8 wk | 8 wk |
| Mousarrezaei et al,64 2020 | Range, 7-12 y | Mother-child dyads | Home | Children with sleep inadequacy based on sleep duration | Mobile phone | Educational messages sent to mothers via phone about sleep | Daily messages for 4 wk | 4 wk | 13 wk |
| Pablos et al,65 2018 | Range, 11-12 y | Students attending Spanish primary schools in eastern Valencia | Primary school | General population | Face-to-face | Education sessions around diet, physical activity, sleep, and hygiene plus a practical physical activity sessionb | Twice weekly sessions lasting 150 min | 32 wk | 32 wk |
| Puder et al,66 2011 | Median, 5.1 y | Children at school in high migrant population areas in Switzerland | Preschool | General population with >40% migrant children | Face-to-face and take-home resources and restructured environment | Multidimensional lifestyle intervention, focused on physical activity, nutrition, media use, sleep, and adaptation of the built environment of the preschool classb | Children: 4× 45-min sessions a week plus 22 additional sessions; teachers: 2× workshops; parents: 3× evening lessons | 42 wk | 42 wk |
| Quach et al,67 2018 | Range, 6-7 y | Students in the second year (grade 1) with low working memory | Primary schools | Children with low verbal and/or visuospatial working memory scores relative to their peers | Face-to-face | The Cogmed Working Memory training tasks on temporary storage and manipulation of verbal and/or visuospatial information | 20-25 Sessions, 25 min each, over 5-7 wk | 5-7 wk | 26 wk |
| Rigney et al,68 2015 | Range, 11-13 y | Students in year 6 and 7 from 12 south Australian schools | Secondary schools | General population | Face-to-face and take-home resources | Education sessions on sleep physiology and sleep hygienec | 4× Weekly lessons then a group project on sleep, which students then presented to parents | 4 wk | 18 wk |
| Santiago et al,69 2022 | Range, 14-19 y | Students aged 14-19 y | Secondary schools | Adolescents reporting poor sleep quality or sleep disturbance and daytime sleepiness | Face-to-face | Strength training sessions | 55-min Sessions 3× times a week for 12 wk | 12 wk | 12 wk |
| Sousa et al,70 2013 | Median, 16.8 y | 12th-Grade students | Secondary schools | General population | Face-to-face | Education program about physiological and behavioral processes of sleep and healthy lifestyle | 5× 50-min Classes | 5 d | 4 wk |
| Sundgot-Borgen et al,71 2020 | Median, 16.8 y | 12th-Grade students | Secondary schools | General population | Face-to-face | Interactive workshops, with 3 themes related to body image, social media literacy, and lifestylec | 3× 90-min Interactive workshops | 13 wk | 52 wk |
| Tamura and Tanaka,72 2014 | Range, 9-11 y | Children in year 4-6 | Elementary schools | General population | Face-to-face | Education session with quiz about sleep habits, then monitored practicing target sleep behavior for 2 wkb | 1× 40-min Session, then performing sleep behavior for 2 wk | 2 wk | 2 wk |
| Tamura and Tanaka,73 2016 | Range, 12-13 y | Adolescents in grade 7 public junior high schools | Junior high schools | General population | Face to face | Education session, then monitored practicing a target sleep behavior for 2 wkb | 1× 45-min Session, then the sleep behavior for 2 wk | 2 wk | 2 wk |
| Taylor et al,74 2015 | Median, 6.5 y | Families with children aged 4-8 y with overweight and obesity | Clinical setting | Children with BMI ≥85th percentile | Face to face, phone calls | Families attended 1 multidisciplinary session to develop specific goals, then met with a mentor | Initial session (1-2 h), then meet mentor monthly in year 1 and 3 visits in year 2 | 104 wk | 104 wk |
| Tomayko et al,75 2018 | Range, 2-5 y | American Indian parent-child dyads living on tribal reservations | Home | General population from American Indian communities | Mail, text reminders, social media | 12 Healthy lifestyle lessons (1 mailed each month) | 12 Lessons (1 each mo for 1 y) | 52 wk | 52 wk |
| Uhlig et al,76 2019 | Range, 8-13 y | Adolescents in 8th grade | Public primary school | General population | Face-to-face | Rap and sing music therapy sessionsb | 16× 45-min Sessions weekly over 4 mo | 16 wk | 16 wk |
| Van Dyk et al,77 2017 | Range, 14-18 y | High school students who sleep 5-7 h on school nights | Home | General population with reduced sleep | Face to face | Increase time in bed on school nights | Increase time in bed by 1.5 h/night for 2 wk | 5 wk | 5 wk |
| van Rijn et al,78 2020 | Median, 14.0 y | 8th-Grade secondary school students from an all-boys school in Singapore | Secondary school | General population | Face-to-face | Education program about the importance of sleep, barriers to getting enough sleep, and improving their opportunities for sleepb | 4× 1-h Lessons delivered over 4 wk | 4 wk | 11 wk |
| Walton et al,79 2016 | Range, 2-5 y | Parents of children age 2-5 y attending early-years centers | Ontario early-years centers | General population | Face to face | Group discussions about weight-related topics, sometimes stimulated by videos of vignettes | 9× 120-min Weekly group sessions | 9 wk | 36 wk |
| Wilson et al,80 2014 | Median, 4.3 y | Low-income preschool children and their families | Head Start preschools | General population | Face to face | Education sessions for children with a 20-min daily lesson followed by 20 min of related activityb | 8× 40-min Sessions for children; 1× 45-min presentation for parents | 2 wk | 4 wk |
| Wing et al,81 2015 | Median, 14.86 y | 7th- to 11th-Grade students aged 12-18 y | Secondary schools | General population | Face to face | Didactic teaching with sleep hygiene tips, followed by small group discussions with casesb | 1× 60-min Town hall seminar, 2× 40-min small workshops, 1 mo apart | 12.2 wk | 17.2 wk |
| Wolfson et al,82 2015 | Median, 12.5 y | 7th Graders and their parents | Public middle schools | General population | Face to face | Didactic information on adolescent sleep and specific strategies for establishing healthy sleep hygiene practicesc | 8× 40-min Sessions over 4 wk, then 4× booster sessions at 2 mo and 12 mo postintervention | 52 wk | 12 mo (full results at 4 wk only) |
| Yoong et al,83 2019 | Range, 3-6 y | Parents of children aged 3-6 y at a convenience sample of childcare centers | Home | General population | Video, phone, text message | Video targeting key behavioral beliefs about sleep practices and a telephone call using motivational interview techniques | 1× 12-min Video, 1-3× phone calls 2-4 wk later, 2× text messages 1 wk after call | 12 wk | 12 wk |
Abbreviations: BMI, body mass index; CBT, cognitive behavioral therapy.
Setting includes where participants were recruited and tested and not necessarily where the intervention has taken place.
Study reported cluster randomization at the class level.
Study reported cluster randomization at the school level.
The primary analysis found that sleep interventions were associated with 10.5 minutes (95% CI, 5.6-15.4; P < .001) longer nocturnal sleep duration compared with the control condition. Figure 2 shows the primary meta-analysis forest plot, with quality assessments.38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83 There was marked heterogeneity across study estimates (I2 = 87.2%). All subgroup comparisons by population characteristics, study design features, and intervention features are summarized in Table 2.
Figure 2. Forest Plot Showing Mean Differences in Sleep Duration in 45 Studies, Comparing Sleep Intervention Groups With Control.
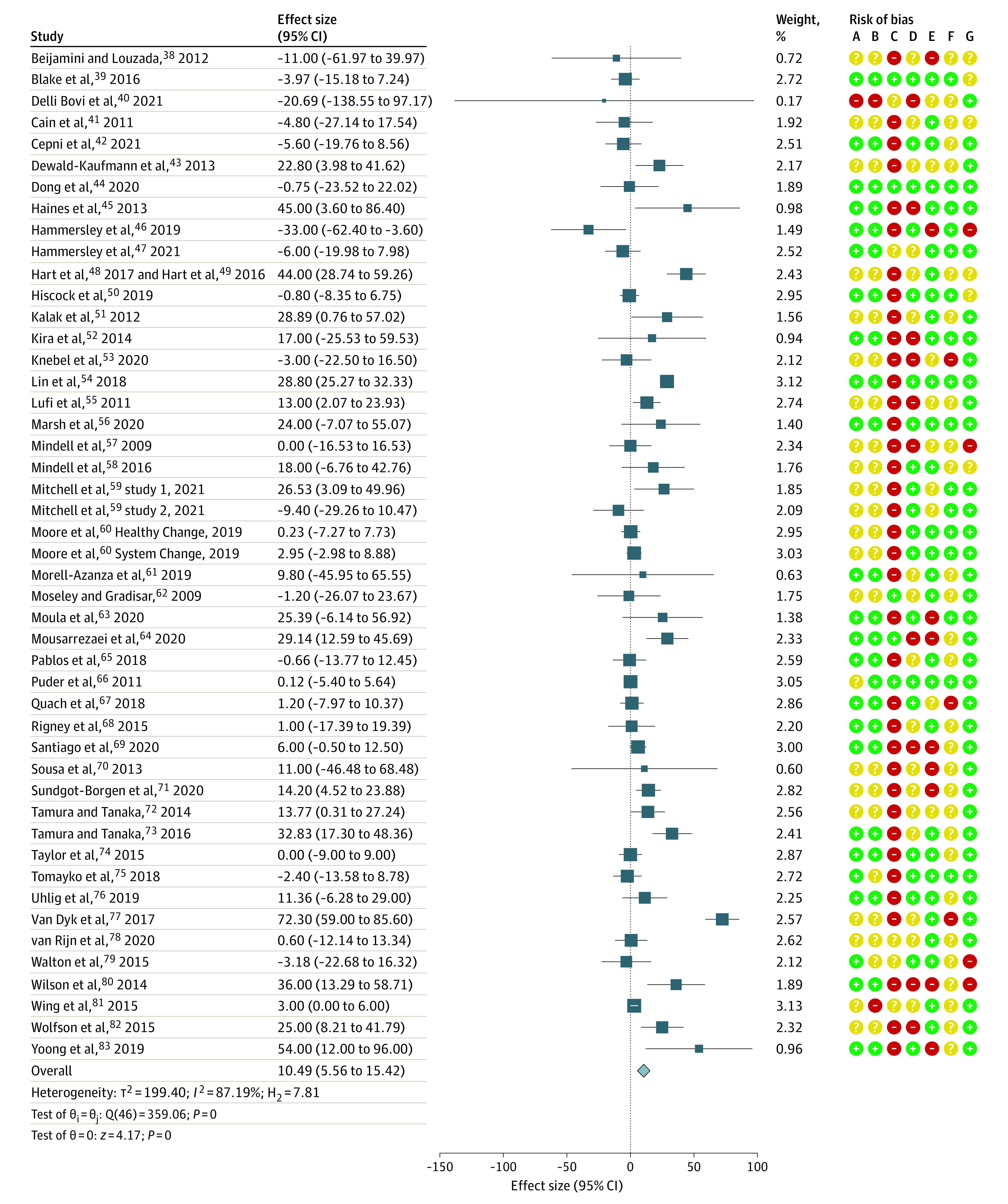
Mean differences in sleep duration (in minutes) for each study, comparing duration in those receiving a sleep intervention vs control. Point estimates are shown by blue solid squares, with horizontal lines showing the 95% CI. The pooled estimate based on a random-effects model is shown with a blue diamond. In the risk of bias column, category A indicates random sequence generation (selection bias); category B, allocation concealment (selection bias); category C, blinding of participants and personnel (performance bias); category D, blinding of outcome assessment (detection bias); category E, incomplete outcome data (attrition bias); category F, selective reporting (reporting bias); and category G, other bias. Risk of bias criteria graded from low risk (green), unclear risk (yellow), or high risk (red).
Table 2. Results of Subgroup Comparisons.
| Subgroup comparison | Studies, No. | Pooled estimate for subgroup, min (95% CI) | P value | Heterogeneity | Difference in subgroup estimates, P value | |
|---|---|---|---|---|---|---|
| I2, % | P value | |||||
| Combined estimate, no subgroups | 47 | 10.49 (5.56 to 15.42) | <.001 | 87.2 | <.001 | NA |
| Population characteristics | ||||||
| Age group | ||||||
| Preschool (1-5 y) | 10 | 5.73 (−5.81 to 17.26) | .33 | 69.1 | .001 | .68 |
| Primary school (6-11 y) | 11 | 11.56 (3.34 to 19.78) | .006 | 77.9 | <.001 | |
| Secondary school (>11 y) | 26 | 11.36 (4.45 to 18.27) | .001 | 90.5 | <.001 | |
| Continent | ||||||
| North America | 15 | 15.63 (3.76 to 27.50) | .01 | 90.4 | <.001 | .02 |
| Australasia | 12 | −0.56 (−5.82 to 4.70) | .83 | 28.9 | .16 | |
| Europe | 9 | 9.97 (2.06 to 17.88) | .01 | 49.0 | .047 | |
| Asia | 7 | 16.93 (4.47 to 29.38) | .008 | 95.5 | <.001 | |
| South America | 4 | 4.96 (−1.15 to 11.02) | .11 | 0 | .76 | |
| Socioeconomic disadvantagea | ||||||
| Population reported to be disadvantaged | 6 | 7.90 (−3.28 to 19.09) | .17 | 69.7 | .006 | .67 |
| Population not reported to be disadvantaged | 41 | 10.64 (5.23 to 16.04) | <.001 | 87.9 | <.001 | |
| Population has a sleep problem | ||||||
| No | 37 | 9.73 (4.46 to 15.00) | <.001 | 85.5 | <.001 | .75 |
| Yes | 10 | 12.26 (−2.20 to 26.73) | .10 | 91.9 | .10 | |
| Study design features | ||||||
| Measure of sleep duration | ||||||
| Objective (actigraphy, EEG) | 19 | 11.00 (1.42 to 20.58) | .02 | 88.1 | <.001 | .86 |
| Subjective (child/parent report or sleep diary) | 28 | 9.95 (3.98 to 15.91) | .001 | 86.9 | <.001 | |
| Subjective measures | ||||||
| Child self-report | 11 | 7.76 (−2.31 to 17.65) | .13 | 92.8 | <.001 | <.001 |
| Parent report | 10 | 0.43 (−3.41 to 4.27) | .83 | 9.3 | .36 | |
| Sleep diary | 7 | 26.44 (17.69 to 35.19) | <.001 | 13.5 | .33 | |
| Nights used for data collection | ||||||
| Weekend nights | 2 | 2.86 (−0.10 to 5.83) | .06 | 0 | .56 | .04 |
| Weekday nights | 19 | 10.34 (2.50 to 18.19) | .01 | 88.1 | <.001 | |
| All weeknights | 26 | 11.86 (4.04 to 19.68) | .003 | 87.2 | <.001 | |
| Study period for participants (including intervention length and follow-up) | ||||||
| ≤1 mo | 12 | 15.22 (7.55 to 22.89) | <.001 | 39.6 | .08 | <.001 |
| 1-<6 mo | 24 | 14.61 (6.21 to 23.01) | .001 | 91.6 | <.001 | |
| 6-<12 mo | 6 | 1.64 (−4.65 to 7.93) | .61 | 41.0 | .13 | |
| ≥1 y | 5 | 0.65 (−2.80 to 4.10) | .71 | 0 | .90 | |
| Intervention features | ||||||
| Location of intervention delivery | ||||||
| Home | 13 | 16.42 (−1.21 to 34.05) | .07 | 89.9 | <.001 | .49 |
| School | 23 | 9.85 (3.50 to 16.20) | .002 | 88.1 | <.001 | |
| Combination of locations/other/unspecified | 11 | 5.84 (−1.57 to 13.25) | .12 | 72.9 | <.001 | |
| Mode of delivery | ||||||
| Face-to-face | 31 | 12.86 (6.16 to 19.55) | <.001 | 89.1 | <.001 | .046 |
| Telephone, text message, and/or online | 14 | 4.00 (−1.67 to 9.59) | .17 | 66.9 | <.001 | |
| Parental involvement in delivery | ||||||
| No | 19 | 10.61 (5.20 to 16.02) | <.001 | 69.5 | <.001 | .96 |
| Yes | 28 | 10.39 (2.71 to 18.09) | <.001 | 90.5 | <.001 | |
| Physical activity component | ||||||
| No | 36 | 13.39 (7.14 to 19.64) | <.001 | 88.7 | <.001 | .001 |
| Yes | 11 | 1.64 (−1.21 to 4.49) | .26 | 0 | .56 | |
| Intervention aims to improve sleep only | ||||||
| No | 18 | 1.25 (−2.54 to 5.03) | .52 | 30.3 | .11 | <.001 |
| Yes | 29 | 15.76 (8.90 to 22.62) | <.001 | 90.2 | <.001 | |
| Intervention focused on obesity | ||||||
| No | 35 | 12.82 (6.97 to 18.68) | <.001 | 88.5 | <.001 | .06 |
| Yes | 12 | 3.29 (−4.78 to 11.35) | .43 | 73.6 | <.001 | |
| Behavior models used | ||||||
| No | 29 | 11.33 (5.78 to 16.88) | <.001 | 83.8 | <.001 | .65 |
| Yes | 18 | 8.79 (−0.62 to 18.19) | .07 | 87.8 | <.001 | |
| Environmental change | ||||||
| No | 41 | 11.06 (5.55 to 16.58) | <.001 | 88.3 | <.001 | .22 |
| Yes | 6 | 5.34 (−2.01 to 12.68) | .15 | 36.8 | .16 | |
| Intervention involves an earlier bedtime | ||||||
| No | 44 | 7.37 (2.93 to 11.82) | .001 | 82.8 | <.001 | .006 |
| Yes | 3 | 46.97 (18.94 to 75.00) | .001 | 89.6 | <.001 | |
| Earlier bedtime in younger vs older children | ||||||
| Primary school (6 to 11 y) | 1 | 44.00 28.74 to 59.26) | <.001 | .88 | ||
| Secondary school (>11 y) | 2 | 48.01 (−0.48 to 96.52) | .05 | 94.4 | <.001 | |
| Intensity | ||||||
| Low/unclear | 23 | 11.13 (4.78 to 17.48) | .001 | 87.9 | <.001 | .64 |
| Medium | 11 | 11.83 (0.74 to 22.93) | .04 | 77.3 | <.001 | |
| High | 13 | 7.01 (−0.11 to 14.12) | .05 | 54.4 | .01 | |
Abbreviations: EEG, electroencephalogram; NA, not applicable.
Socioeconomic disadvantage was defined differently in different studies, but primarily includes individuals from low-income areas or families.
Differences in Sleep Duration by Study Population Characteristics
There were no significant differences in sleep duration estimates across preschool, primary school, and secondary school age groups, presence of social disadvantage (eg, coming from a low-income family or low-income area), or whether the study population included those reporting sleep problems. Most trials were carried out in high-income countries in children of largely White European ancestry (ie, 15 trials were carried out in North America, 12 trials in Australasia, 9 in Europe); the remaining trials were carried out in Asia (7 trials) and South America (4 trials). There were significant differences in the effect size estimates by study geography; pooled estimates from North American (15.6 minutes; 95% CI, 3.8-27.5) and Asian (16.9 minutes; 95% CI, 4.5-29.4) trials appeared to show the largest difference in sleep duration compared with pooled trials from Australasia (−0.6 minutes; 95% CI, −5.8 to 4.7) and South America (5.0 minutes; 95% CI, −1.2 to 11.0), which showed no change with wide CIs (P = .02) (Table 2).
Differences in Sleep Duration by Study Design Features
There were no overall differences in sleep duration when measured using objective (accelerometer or electroencephalography) vs subjective (sleep diaries, child or parental report) methods. However, there were considerable differences in sleep duration among the trials relying on subjective reports, where those using parent report were associated with very small changes in sleep duration (0.4 minutes; 95% CI, −3.4 to 4.3) and those relying on child report were associated with a nonsignificant difference in sleep duration (7.8 minutes; 95% CI, −2.3 to 17.7), whereas trials using sleep diaries were associated with a large difference in sleep duration (26.4 minutes; 95% CI, 17.7-35.2) (P < .001). Estimates from trials recording data on 7 nights per week (all weeknights; 11.9 minutes; 95% CI, 4.0-19.7) ) were similar to those recording data 5 nights per week (weekday nights; 10.3 minutes; 95% CI, 2.5-18.2). Two trials only reported data for weekend nights, reporting a lower effect estimate (2.9 minutes; 95% CI, −0.1 to 5.8); the difference between subgroups was significant (P = .04). Trials that reported final follow-up data within 6 months of the baseline reported significantly greater effect sizes than those reporting final follow-up beyond 6 months.
Differences in Sleep Duration by Intervention Features
There were no statistically significant differences in sleep duration estimates by the location of intervention delivery (eg, home or school), with parental involvement in the intervention, or in whether the intervention was delivered face-to-face. Trials that focused on lengthening sleep alone showed significantly more change in sleep duration (15.8 minutes; 95% CI, 8.9-22.6) than interventions with broader aims (1.2 minutes; 95% CI, −2.5 to 5.0; P < .001). There were no statistically significant differences in the effects of trials by intensity of intervention delivery, use of environmental change to support longer sleep, or whether behavioral theory was used to inform intervention design.
Trials that focused on obesity had a smaller effect (3.3 minutes; 95% CI, −4.8 to 11.3) compared with other trials (12.8 minutes; 95% CI, 7.0-18.7; P = .06). Similarly, trials with a physical activity component (1.6 minutes; 95% CI, −1.2 to 4.5) had a significantly smaller effect size compared with those with no physical activity component (13.4 minutes ;95% CI, 7.1-19.6; P = .001). Trials that involved an earlier bedtime had a significant and substantially greater effect estimate (47.0 minutes; 95% CI, 18.9-75.0) compared with the effect of trials that did not encourage participants to go to bed earlier (7.4 minutes; 95% CI, 2.9-11.8; P = .006). The effect of early bedtimes was in fewer studies (3 trials), but the effect appeared similar in studies carried out in primary school–aged children, and 2 studies solely in secondary school–aged children. Heterogeneity in subgroup analyses varied between 0% and 95.5%.
Possible Association of Bias and Other Factors With Differences in Estimates of Sleep Duration
Visual inspection did not reveal any clear pattern of small study or publication bias overall (Egger test = 0.85); there was no clear pattern of small study bias by subgroups. Equally, risk of bias assessments, including selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases, did not provide notable patterns in the data (Figure 2). There was no evidence that differences in sleep duration between intervention and control differed by quartile groups of baseline levels of sleep duration. Moreover, there was no evidence of a systematic difference in unadjusted vs adjusted sleep duration analyses, both at a study level (n = 45) or estimate level (n = 58).
Discussion
This systematic review found that sleep interventions in children aged 1 to 18 years were associated with 10.5 minutes longer sleep duration per night. Many intervention components have small effects on sleep duration. Substantial increases in sleep duration were observed in a subgroup of trials encouraging earlier bedtimes, with objectively measured sleep durations increasing by 47 minutes. Interventions that have a broader focus (eg, interventions that focus on obesity) were ineffective in increasing sleep duration, extending sleep by 1.2 minutes compared with 16 minutes in interventions focused on sleep only.
The pooled effect estimate of 10.5 minutes longer sleep duration per night is similar to previous reviews that included fewer trials with correspondingly fewer participants26 or narrower age groups (eg, infants, or infants and preschool-aged children only).26,27,28 While a 2020 meta-analysis85 of older children and young adults (12 to 25 years) found a larger intervention effect (35 minutes), the pooled estimate was associated with wide CIs (95% CI, 8.70-61.14), inclusive of our overall finding. Notably, the pooled effect estimate from that review is similar to the estimate reported in the present review for trials that encouraged earlier bedtimes and importantly used objective actigraphy measurement of sleep duration (with 2 trials being used in both reviews43,77), which limits well-known biases associated with self-reported or parent-reported sleep times.26 While prior qualitative reviews have suggested that multicomponent interventions underpinned by behavioral theory might be more effective,25 our findings (in agreement with another previous review26) demonstrate that simple sleep-focused interventions are more effective.
We included a large number of RCTs (45 trials with 13 539 participants), which provide the best available evidence of potential intervention. This review spans the entirety of childhood (excluding infants younger than 1 year) and finds no clear evidence of differences in overall intervention effects by age. Most trials included in this review were carried out in primary school–aged and secondary school–aged children, where circadian sleep patterns and nocturnal sleep behavior are well established. The trials included delivered interventions in both school and home settings, and no difference was found in the effect sizes of interventions in either setting. These findings suggest that reinforcement of interventions in both settings could be used for future implementation. Differences in individual study results were reflected by high levels of heterogeneity in both the main and subgroup analyses.
There were inconsistencies measuring sleep-related outcomes across trials. Sleep duration was the most commonly reported outcome, but there was variation in the analytical approach, with some trials reporting mean sleep durations by intervention and control groups and others reporting mean differences in sleep duration between groups at follow-up or differences-in-differences (with differing levels of adjustment); notably, there was no evidence of systematic differences across these groups. Other important sleep-related outcomes beyond duration, such as sleep quality and latency (not reported here), were inconsistently and less frequently reported, which presents challenges for appropriately pooling results. Similarly, other intervention characteristics were not routinely reported, and while interventions underpinned by theory did not appear to be associated with longer sleep durations, more detailed reporting of the use of theory (including behavioral models underpinning proposed interventions) and study fidelity (including uptake and compliance with a given intervention) could usefully contribute to the evidence by allowing effective components to be more readily identified, which would support the development of novel interventions.
While an overall 10-minute increase in sleep duration would have a modest effect in addressing declining sleep durations in children,8,9,10,11 a 47-minute increase associated with earlier bedtimes would substantially affect this population-level problem. However, while the difference in sleep duration among trials using earlier bedtimes was much larger, this was only based on 3 studies (1 trial in primary school–aged children48 and 2 trials in secondary school–aged children43,77), largely in the US,48,77 and these findings need to be replicated in further studies and settings. If confirmed, earlier bedtimes are needed given wake-up times are less changeable, especially on schooldays. While one RCT from Israel55 included in our review showed 55 minutes longer sleep duration by delaying school start times by 1 hour within the first week, this was not sustained. Further high-quality experimental evidence is needed,86 especially as interventions to shift wake-up times by delaying school start times in a UK context have been shown to be impractical.87 However, recent observational evidence from the US has shown that increased sleep duration (by as much as 40 minutes) could be achieved by delaying school start times, suggesting that such an approach might be feasible.88,89 In our study, control group children achieved only 8.6 hours of sleep overall, with 10.4 hours in 10 trials of preschool-aged children, 9.2 hours in 9 trials of primary school–aged children, and as little as 7.6 hours in 22 trials of secondary school–aged children. These durations are much shorter than current recommended levels of 10 to 11 hours in those aged 4 to 12 years and of 8 to 10 hours in those aged 3 to 18 years.1 Lengthening time asleep by 47 minutes among those with inadequate sleep duration could not only address these shortfalls but could also have important benefits for child health. Observational evidence in those aged 8 to 10 years suggests that such increases could have an appreciable effect on cardiometabolic health (eg, 0.1 lower body mass index [calculated as weight in kilograms divided by height in meters squared] and 2% reduction in insulin resistance),90 as well as having potential benefits for mental health and well-being.6 Patterning sleep behavior from early age could also track into adulthood, with potential benefits for health in later life. Currently, the only studies encouraging earlier bedtimes within the age ranges of this study were conducted largely in adolescents. Further research is urgently needed to establish whether similarly large effect sizes are observed in sleep interventions encouraging earlier bedtimes in younger children, and, moving beyond this, to establish whether the effects can be sustained. Additional research is also needed to clarify the long-term benefits of such interventions on health outcomes.
Limitations
This study has limitations. Reasons for high levels of heterogeneity in effect sizes remain unclear, and further studies confirming the large increase in sleep duration associated with earlier bedtimes are needed in different age groups and population settings.
Conclusions
Typically, nonpharmacological interventions increase sleep by a small amount (10.5 minutes). Intervention elements, such as a narrow focus on sleep including earlier bedtimes, should be taken forward in terms of study design to help children achieve adequate sleep to support growth, cognitive development, mental well-being, and metabolic health. Based on the best available evidence to date, earlier bedtimes offer a simple, pragmatic strategy to meaningfully increase sleep duration.
eTable 1. Search Strategy Used in Medline
eTable 2. Detailed Table of Study Characteristics
eTable 3. Spreadsheet of Study Estimates Used
References
- 1.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40-43. doi: 10.1016/j.sleh.2014.12.010 [DOI] [PubMed] [Google Scholar]
- 2.Ohayon M, Wickwire EM, Hirshkowitz M, et al. National Sleep Foundation’s sleep quality recommendations: first report. Sleep Health. 2017;3(1):6-19. doi: 10.1016/j.sleh.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 3.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414-420. doi: 10.2337/dc09-1124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fallone G, Owens JA, Deane J. Sleepiness in children and adolescents: clinical implications. Sleep Med Rev. 2002;6(4):287-306. doi: 10.1053/smrv.2001.0192 [DOI] [PubMed] [Google Scholar]
- 5.Gozal D, Kheirandish-Gozal L. Neurocognitive and behavioral morbidity in children with sleep disorders. Curr Opin Pulm Med. 2007;13(6):505-509. doi: 10.1097/MCP.0b013e3282ef6880 [DOI] [PubMed] [Google Scholar]
- 6.Short MA, Bartel K, Carskadon MA. Sleep and mental health in children and adolescents. In: Grandner MA, ed. Sleep and Health. Academic Press; 2019:435-445. [Google Scholar]
- 7.The Sleep Charity . How much sleep does my child need? Accessed August 16, 2022. https://thesleepcharity.org.uk/how-much-sleep-does-my-child-need/
- 8.Guan H, Zhang Z, Wang B, et al. Proportion of kindergarten children meeting the WHO guidelines on physical activity, sedentary behaviour and sleep and associations with adiposity in urban Beijing. BMC Pediatr. 2020;20(1):70. doi: 10.1186/s12887-020-1969-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The great sleep recession: changes in sleep duration among US adolescents, 1991-2012. Pediatrics. 2015;135(3):460-468. doi: 10.1542/peds.2014-2707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaput J-P, Janssen I. Sleep duration estimates of Canadian children and adolescents. J Sleep Res. 2016;25(5):541-548. doi: 10.1111/jsr.12410 [DOI] [PubMed] [Google Scholar]
- 11.Singh GK, Kenney MK. Rising prevalence and neighborhood, social, and behavioral determinants of sleep problems in US children and adolescents, 2003-2012. Sleep Disord. 2013;2013:394320. doi: 10.1155/2013/394320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hysing M, Pallesen S, Stormark KM, Jakobsen R, Lundervold AJ, Sivertsen B. Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open. 2015;5(1):e006748. doi: 10.1136/bmjopen-2014-006748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dube N, Khan K, Loehr S, Chu Y, Veugelers P. The use of entertainment and communication technologies before sleep could affect sleep and weight status: a population-based study among children. Int J Behav Nutr Phys Act. 2017;14(1):97. doi: 10.1186/s12966-017-0547-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50-58. doi: 10.1016/j.smrv.2014.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med. 2010;11(8):735-742. doi: 10.1016/j.sleep.2010.02.006 [DOI] [PubMed] [Google Scholar]
- 16.Bruni O, Sette S, Fontanesi L, Baiocco R, Laghi F, Baumgartner E. Technology use and sleep quality in preadolescence and adolescence. J Clin Sleep Med. 2015;11(12):1433-1441. doi: 10.5664/jcsm.5282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gamble AL, D’Rozario AL, Bartlett DJ, et al. Adolescent sleep patterns and night-time technology use: results of the Australian Broadcasting Corporation’s Big Sleep Survey. PLoS One. 2014;9(11):e111700. doi: 10.1371/journal.pone.0111700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahluwalia N, Herrick K, Moshfegh A, Rybak M. Caffeine intake in children in the United States and 10-y trends: 2001-2010. Am J Clin Nutr. 2014;100(4):1124-1132. doi: 10.3945/ajcn.113.082172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Temple JL. Review: trends, safety, and recommendations for caffeine use in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2019;58(1):36-45. doi: 10.1016/j.jaac.2018.06.030 [DOI] [PubMed] [Google Scholar]
- 20.Allen SL, Howlett MD, Coulombe JA, Corkum PV. ABCs of SLEEPING: a review of the evidence behind pediatric sleep practice recommendations. Sleep Med Rev. 2016;29:1-14. doi: 10.1016/j.smrv.2015.08.006 [DOI] [PubMed] [Google Scholar]
- 21.Belmon LS, van Stralen MM, Busch V, Harmsen IA, Chinapaw MJM. What are the determinants of children’s sleep behavior? a systematic review of longitudinal studies. Sleep Med Rev. 2019;43:60-70. doi: 10.1016/j.smrv.2018.09.007 [DOI] [PubMed] [Google Scholar]
- 22.Meltzer LJ, Mindell JA. Systematic review and meta-analysis of behavioral interventions for pediatric insomnia. J Pediatr Psychol. 2014;39(8):932-948. doi: 10.1093/jpepsy/jsu041 [DOI] [PubMed] [Google Scholar]
- 23.Nikles J, Mitchell GK, de Miranda Araújo R, et al. A systematic review of the effectiveness of sleep hygiene in children with ADHD. Psychol Health Med. 2020;25(4):497-518. doi: 10.1080/13548506.2020.1732431 [DOI] [PubMed] [Google Scholar]
- 24.Keogh S, Bridle C, Siriwardena NA, et al. Effectiveness of non-pharmacological interventions for insomnia in children with autism spectrum disorder: a systematic review and meta-analysis. PLoS One. 2019;14(8):e0221428-e0221428. doi: 10.1371/journal.pone.0221428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Busch V, Altenburg TM, Harmsen IA, Chinapaw MJ. Interventions that stimulate healthy sleep in school-aged children: a systematic literature review. Eur J Public Health. 2017;27(1):53-65. doi: 10.1093/eurpub/ckw140 [DOI] [PubMed] [Google Scholar]
- 26.Fangupo LJ, Haszard JJ, Reynolds AN, et al. Do sleep interventions change sleep duration in children aged 0-5 years? a systematic review and meta-analysis of randomised controlled trials. Sleep Med Rev. 2021;59:101498. doi: 10.1016/j.smrv.2021.101498 [DOI] [PubMed] [Google Scholar]
- 27.Kempler L, Sharpe L, Miller CB, Bartlett DJ. Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? a systematic review and meta-analysis of randomised controlled trials. Sleep Med Rev. 2016;29:15-22. doi: 10.1016/j.smrv.2015.08.002 [DOI] [PubMed] [Google Scholar]
- 28.Bryanton J, Beck CT, Montelpare W. Postnatal parental education for optimizing infant general health and parent-infant relationships. Cochrane Database Syst Rev. 2013;(11):CD004068. doi: 10.1002/14651858.CD004068.pub4 [DOI] [PubMed] [Google Scholar]
- 29.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71):n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson S, Anderson K, Baldwin D, et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders: an update. J Psychopharmacol. 2019;33(8):923-947. doi: 10.1177/0269881119855343 [DOI] [PubMed] [Google Scholar]
- 31.Wallace BC, Noel-Storr A, Marshall IJ, Cohen AM, Smalheiser NR, Thomas J. Identifying reports of randomized controlled trials (RCTs) via a hybrid machine learning and crowdsourcing approach. J Am Med Inform Assoc. 2017;24(6):1165-1168. doi: 10.1093/jamia/ocx053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Covidence. Homepage. Accessed August 8, 2022. http://www.covidence.org
- 33.Painter JE, Borba CP, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med. 2008;35(3):358-362. doi: 10.1007/s12160-008-9042-y [DOI] [PubMed] [Google Scholar]
- 34.Pang B, Kubacki K, Rundle-Thiele S. Promoting active travel to school: a systematic review (2010-2016). BMC Public Health. 2017;17(1):638. doi: 10.1186/s12889-017-4648-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hurley E, Dietrich T, Rundle-Thiele S. A systematic review of parent based programs to prevent or reduce alcohol consumption in adolescents. BMC Public Health. 2019;19(1):1451. doi: 10.1186/s12889-019-7733-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgins JPT, Altman DG, Gøtzsche PC, et al. ; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beijamini F, Louzada FM. Are educational interventions able to prevent excessive daytime sleepiness in adolescents? Biol Rhythm Res. 2012;43(6):603-613. doi: 10.1080/09291016.2011.630183 [DOI] [Google Scholar]
- 39.Blake M, Waloszek JM, Schwartz O, et al. The SENSE study: post intervention effects of a randomized controlled trial of a cognitive-behavioral and mindfulness-based group sleep improvement intervention among at-risk adolescents. J Consult Clin Psychol. 2016;84(12):1039-1051. doi: 10.1037/ccp0000142 [DOI] [PubMed] [Google Scholar]
- 40.Delli Bovi AP, Manco Cesari G, Rocco MC, et al. Healthy lifestyle management of pediatric obesity with a hybrid system of customized mobile technology: the PediaFit pilot project. Nutrients. 2021;13(2):631. doi: 10.3390/nu13020631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cain N, Gradisar M, Moseley L. A motivational school-based intervention for adolescent sleep problems. Sleep Med. 2011;12(3):246-251. doi: 10.1016/j.sleep.2010.06.008 [DOI] [PubMed] [Google Scholar]
- 42.Cepni AB, Taylor A, Crumbley C, et al. Feasibility and efficacy of the “FUNPALs Playgroup” intervention to improve toddler dietary and activity behaviors: a pilot randomized controlled trial. Int J Environ Res Public Health. 2021;18(15):7828. doi: 10.3390/ijerph18157828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension on sleep and cognitive performance in adolescents with chronic sleep reduction: an experimental study. Sleep Med. 2013;14(6):510-517. doi: 10.1016/j.sleep.2013.01.012 [DOI] [PubMed] [Google Scholar]
- 44.Dong L, Dolsen MR, Martinez AJ, Notsu H, Harvey AG. A transdiagnostic sleep and circadian intervention for adolescents: six-month follow-up of a randomized controlled trial. J Child Psychol Psychiatry. 2020;61(6):653-661. doi: 10.1111/jcpp.13154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haines J, McDonald J, O’Brien A, et al. Healthy habits, happy homes: randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatr. 2013;167(11):1072-1079. doi: 10.1001/jamapediatrics.2013.2356 [DOI] [PubMed] [Google Scholar]
- 46.Hammersley ML, Okely AD, Batterham MJ, Jones RA. An internet-based childhood obesity prevention program (Time2bHealthy) for parents of preschool-aged children: randomized controlled trial. J Med Internet Res. 2019;21(2):e11964. doi: 10.2196/11964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hammersley ML, Wyse RJ, Jones RA, et al. Translation of two healthy eating and active living support programs for parents of 2-6-year-old children: outcomes of the ‘Time for Healthy Habits’ parallel partially randomised preference trial. Nutrients. 2021;13(10):3348. doi: 10.3390/nu13103348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hart C, Hawley N, Egleston B, et al. 0995 Brief behavioral intervention enhances children’s sleep and improves weight status. Sleep (Basel). 2017;40(suppl 1):A370-A370. doi: 10.1093/sleepj/zsx050.994 [DOI] [Google Scholar]
- 49.Hart CN, Hawley NL, Wing RR. Development of a behavioral sleep intervention as a novel approach for pediatric obesity in school-aged children. Pediatr Clin North Am. 2016;63(3):511-523. doi: 10.1016/j.pcl.2016.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hiscock H, Quach J, Paton K, et al. Impact of a behavioral sleep intervention on new school entrants’ social emotional functioning and sleep: a translational randomized trial. Behav Sleep Med. 2019;17(6):698-712. doi: 10.1080/15402002.2018.1469493 [DOI] [PubMed] [Google Scholar]
- 51.Kalak N, Gerber M, Kirov R, et al. Daily morning running for 3 weeks improved sleep and psychological functioning in healthy adolescents compared with controls. J Adolesc Health. 2012;51(6):615-622. [DOI] [PubMed] [Google Scholar]
- 52.Kira G, Maddison R, Hull M, Blunden S, Olds T. Sleep education improves the sleep duration of adolescents: a randomized controlled pilot study. J Clin Sleep Med. 2014;10(7):787-792. doi: 10.5664/jcsm.3874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Knebel MTG, Borgatto AF, Lopes MVV, et al. Mediating role of screen media use on adolescents’ total sleep time: a cluster-randomized controlled trial for physical activity and sedentary behaviour. Child Care Health Dev. 2020;46(3):381-389. doi: 10.1111/cch.12755 [DOI] [PubMed] [Google Scholar]
- 54.Lin CY, Strong C, Scott AJ, Broström A, Pakpour AH, Webb TL. A cluster randomized controlled trial of a theory-based sleep hygiene intervention for adolescents. Sleep. Published online November 1, 2018. doi: 10.1093/sleep/zsy170 [DOI] [PubMed] [Google Scholar]
- 55.Lufi D, Tzischinsky O, Hadar S. Delaying school starting time by one hour: some effects on attention levels in adolescents. J Clin Sleep Med. 2011;7(2):137-143. doi: 10.5664/jcsm.28100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marsh S, Taylor R, Galland B, Gerritsen S, Parag V, Maddison R. Results of the 3 Pillars Study (3PS), a relationship-based programme targeting parent-child interactions, healthy lifestyle behaviours, and the home environment in parents of preschool-aged children: a pilot randomised controlled trial. PLoS One. 2020;15(9):e0238977. doi: 10.1371/journal.pone.0238977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mindell JA, Telofski LS, Wiegand B, Kurtz ES. A nightly bedtime routine: impact on sleep in young children and maternal mood. Sleep. 2009;32(5):599-606. doi: 10.1093/sleep/32.5.599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mindell JA, Sedmak R, Boyle JT, Butler R, Williamson AA. Sleep Well!: a pilot study of an education campaign to improve sleep of socioeconomically disadvantaged children. J Clin Sleep Med. 2016;12(12):1593-1599. doi: 10.5664/jcsm.6338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mitchell JA, Morales KH, Williamson AA, et al. Engineering a mobile platform to promote sleep in the pediatric primary care setting. Sleep Adv. 2021;2(1):zpab006. doi: 10.1093/sleepadvances/zpab006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moore SM, Borawski EA, Love TE, et al. Two family interventions to reduce BMI in low-income urban youth: a randomized trial. Pediatrics. 2019;143(6):e20182185. doi: 10.1542/peds.2018-2185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Morell-Azanza L, Ojeda-Rodríguez A, Ochotorena-Elicegui A, et al. Changes in objectively measured physical activity after a multidisciplinary lifestyle intervention in children with abdominal obesity: a randomized control trial. BMC Pediatr. 2019;19(1):90. doi: 10.1186/s12887-019-1468-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Moseley L, Gradisar M. Evaluation of a school-based intervention for adolescent sleep problems. Sleep. 2009;32(3):334-341. doi: 10.1093/sleep/32.3.334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Moula Z, Powell J, Karkou V. An investigation of the effectiveness of arts therapies interventions on measures of quality of life and wellbeing: a pilot randomized controlled study in primary schools. Front Psychol. 2020;11:586134. doi: 10.3389/fpsyg.2020.586134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mousarrezaei Z, Valizadeh L, Alizadeh M, Aghajari P, Jafarabadi MA, Janani R. The effects of education through short message service for mothers on sleep duration among school-aged children: a randomized trial. Nurs Midwifery Stud. 2020;9(1):9-15. doi: 10.4103/nms.nms_93_18 [DOI] [Google Scholar]
- 65.Pablos A, Nebot V, Vañó-Vicent V, Ceca D, Elvira L. Effectiveness of a school-based program focusing on diet and health habits taught through physical exercise. Appl Physiol Nutr Metab. 2018;43(4):331-337. doi: 10.1139/apnm-2017-0348 [DOI] [PubMed] [Google Scholar]
- 66.Puder JJ, Marques-Vidal P, Schindler C, et al. Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): cluster randomised controlled trial. BMJ. 2011;343:d6195. doi: 10.1136/bmj.d6195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Quach J, Spencer-Smith M, Anderson PJ, Roberts G. Can working memory training improve children’s sleep? Sleep Med. 2018;47:113-116. doi: 10.1016/j.sleep.2017.11.1143 [DOI] [PubMed] [Google Scholar]
- 68.Rigney G, Blunden S, Maher C, et al. Can a school-based sleep education programme improve sleep knowledge, hygiene and behaviours using a randomised controlled trial. Sleep Med. 2015;16(6):736-745. doi: 10.1016/j.sleep.2015.02.534 [DOI] [PubMed] [Google Scholar]
- 69.Santiago LCS, Lyra MJ, Germano-Soares AH, et al. Effects of strength training on sleep parameters of adolescents: a randomized controlled trial. J Strength Cond Res. 2022;36(5):1222-1227. [DOI] [PubMed] [Google Scholar]
- 70.Sousa IC, Souza JC, Louzada FM, Azevedo CVM. Changes in sleep habits and knowledge after an educational sleep program in 12th grade students. Sleep Biol Rhythms. 2013;11(3):144-153. doi: 10.1111/sbr.12016 [DOI] [Google Scholar]
- 71.Sundgot-Borgen C, Friborg O, Kolle E, et al. Does the Healthy Body Image program improve lifestyle habits among high school students? a randomized controlled trial with 12-month follow-up. J Int Med Res. 2020;48(3):300060519889453. doi: 10.1177/0300060519889453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tamura N, Tanaka H. Effects of sleep education with self-help treatment for elementary schoolchild with nocturnal lifestyle and irritability. Sleep Biol Rhythms. 2014;12(3):169-179. doi: 10.1111/sbr.12055 [DOI] [Google Scholar]
- 73.Tamura N, Tanaka H. Effects of a sleep education program with self-help treatment on sleeping patterns and daytime sleepiness in Japanese adolescents: a cluster randomized trial. Chronobiol Int. 2016;33(8):1073-1085. doi: 10.1080/07420528.2016.1199561 [DOI] [PubMed] [Google Scholar]
- 74.Taylor RW, Cox A, Knight L, et al. A tailored family-based obesity intervention: a randomized trial. Pediatrics. 2015;136(2):281-289. doi: 10.1542/peds.2015-0595 [DOI] [PubMed] [Google Scholar]
- 75.Tomayko EJ, Prince RJ, Cronin KA, Kim K, Parker T, Adams AK. The Healthy Children, Strong Families 2 (HCSF2) randomized controlled trial improved healthy behaviors in American Indian families with young children. Curr Dev Nutr. 2018;3(suppl 2):53-62. doi: 10.1093/cdn/nzy087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Uhlig S, Groot J, Jansen E, Scherder E. Rap & Sing Music Therapy and sleep in adolescents: a single-blind cluster randomized controlled trial. Nord J Music Ther. 2019;28(1):60-70. doi: 10.1080/08098131.2018.1542613 [DOI] [Google Scholar]
- 77.Van Dyk TR, Zhang N, Catlin PA, et al. Feasibility and emotional impact of experimentally extending sleep in short-sleeping adolescents. Sleep. 2017;40(9). doi: 10.1093/sleep/zsx123 [DOI] [PubMed] [Google Scholar]
- 78.van Rijn E, Koh SYJ, Ng ASC, et al. Evaluation of an interactive school-based sleep education program: a cluster-randomized controlled trial. Sleep Health. 2020;6(2):137-144. doi: 10.1016/j.sleh.2019.10.006 [DOI] [PubMed] [Google Scholar]
- 79.Walton K, Filion AJ, Gross D, et al. Parents and Tots Together: pilot randomized controlled trial of a family-based obesity prevention intervention in Canada. Can J Public Health. 2016;106(8):e555-e562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wilson KE, Miller AL, Bonuck K, Lumeng JC, Chervin RD. Evaluation of a sleep education program for low-income preschool children and their families. Sleep. 2014;37(6):1117-1125. doi: 10.5665/sleep.3774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wing YK, Chan NY, Man Yu MW, et al. A school-based sleep education program for adolescents: a cluster randomized trial. Pediatrics. 2015;135(3):e635-e643. doi: 10.1542/peds.2014-2419 [DOI] [PubMed] [Google Scholar]
- 82.Wolfson AR, Harkins E, Johnson M, Marco C. Effects of the Young Adolescent Sleep Smart Program on sleep hygiene practices, sleep health efficacy, and behavioral well-being. Sleep Health. 2015;1(3):197-204. doi: 10.1016/j.sleh.2015.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yoong SL, Grady A, Stacey F, et al. A pilot randomized controlled trial examining the impact of a sleep intervention targeting home routines on young children’s (3-6 years) physical activity. Pediatr Obes. 2019;14(4):e12481. doi: 10.1111/ijpo.12481 [DOI] [PubMed] [Google Scholar]
- 84.Blake MJ, Blake LM, Schwartz O, et al. Who benefits from adolescent sleep interventions? moderators of treatment efficacy in a randomized controlled trial of a cognitive-behavioral and mindfulness-based group sleep intervention for at-risk adolescents. J Child Psychol Psychiatry. 2018;59(6):637-649. doi: 10.1111/jcpp.12842 [DOI] [PubMed] [Google Scholar]
- 85.Griggs S, Conley S, Batten J, Grey M. A systematic review and meta-analysis of behavioral sleep interventions for adolescents and emerging adults. Sleep Med Rev. 2020;54:101356. doi: 10.1016/j.smrv.2020.101356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Minges KE, Redeker NS. Delayed school start times and adolescent sleep: a systematic review of the experimental evidence. Sleep Med Rev. 2016;28:86-95. doi: 10.1016/j.smrv.2015.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Illingworth G, Sharman R, Jowett A, Harvey CJ, Foster RG, Espie CA. Challenges in implementing and assessing outcomes of school start time change in the UK: experience of the Oxford Teensleep study. Sleep Med. 2019;60:89-95. doi: 10.1016/j.sleep.2018.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Widome R, Berger AT, Iber C, et al. Association of delaying school start time with sleep duration, timing, and quality among adolescents. JAMA Pediatr. 2020;174(7):697-704. doi: 10.1001/jamapediatrics.2020.0344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bowers JM, Moyer A. Effects of school start time on students’ sleep duration, daytime sleepiness, and attendance: a meta-analysis. Sleep Health. 2017;3(6):423-431. doi: 10.1016/j.sleh.2017.08.004 [DOI] [PubMed] [Google Scholar]
- 90.Rudnicka AR, Nightingale CM, Donin AS, et al. Sleep duration and risk of type 2 diabetes. Pediatrics. 2017;140(3):e20170338. doi: 10.1542/peds.2017-0338 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Search Strategy Used in Medline
eTable 2. Detailed Table of Study Characteristics
eTable 3. Spreadsheet of Study Estimates Used