Abstract
Background
It is great of significance to figure the time-trend of esophageal cancer (EC) and its current status for effective prevention and control, especially in EC high risk areas. As one of world-renowned high-risk areas, the epidemiology of EC in Henan has not been recently updated. Therefore, we aimed to depict the status quo of EC and analyze its time-trend in Henan.
Methods
The EC data were extracted from the Henan Provincial Cancer registry database derived from the population based cancer registry system, which covered 30.51% of the whole population in Henan and were qualified according to national and international guidelines. The incidence and mortality of EC were estimated by area (rural/urban), gender, and age groups. The age-standardized rates (ASRs) were calculated according to the Segi’s population. Joinpoint regression was used to calculate annual percentage change (APC) and average annual percentage change (AAPC) to evaluate the time-trend of EC.
Results
As estimated, there were 29,913 new EC cases in Henan, 2018. The crude incidence and the age-standardized incidence rate by world standard population (ASIRW) was 27.43/105 and 19.96/105, respectively. The incidence in males and rural was 1.83 and 1.51 times higher than that in females and urban areas, respectively. Meanwhile, it was estimated that 22,688 deaths occurred in 2018. The crude mortality and the age-standardized mortality rate by world standard population (ASMRW) were 20.80/105 and 14.47/105, respectively. Similarly, males and rural areas had higher mortality compared with females and urban areas. The age-specific incidence and mortality of EC showed significant increasing after 60–64 years group. In general, the time-trend of incidence (APC: −8.9, P<0.001) and mortality (APC: −7.6, P<0.001) of EC showed a significant decreasing trend since 2014, and downward trend were also observed in rural areas for incidence (APC: −5.2, P<0.001) and mortality (APC: −3.9, P<0.001) from 2010 to 2018.
Conclusions
The EC incidence and mortality in Henan has exhibited a significant declining trend in past years. Nonetheless, the disease burden remains high, especially in males and rural areas. Therefore, the ongoing prevention and control strategies of EC should be maintained alongside the establishment of more effective strategies.
Keywords: Esophageal cancer (EC), incidence, mortality, trend, Henan
Introduction
Esophageal cancer (EC) is the eighth most common cancer worldwide and constitutes the sixth leading cause of cancer deaths (1). It is characterized by its high mortality rate, poor prognosis due to late-stage diagnosis, and geographic variability of incidence (2,3). According to the estimation by the World Health Organization/International Agency for Research on Cancer (WHO/IARC), there were 604,100 new cases and 544,000 deaths from EC globally in 2020 although decline time-trend of EC incidence and mortality reported worldwide (1). The incidence varied remarkably by more than 21-fold among different regions, with the highest rates in eastern Asia, and eastern and southern Africa, and the lowest rate in western Africa (4,5). The predominant histopathological type of EC is esophageal squamous cell carcinoma (ESCC), of which most cases occur in China (6-9).
In the last decades, although the incidence and mortality of EC in China have reduced dramatically, the figures remain much higher than the average level worldwide (10), warranting characterization of the trend so that policy makers can modify the prevention and control strategies promptly and effectively. Henan is one of the EC high-risk areas in China, within which Linxian County (now named Linzhou City) has been acknowledged worldwide as a high-risk area because of pickled vegetables popular, micronutrients deficiency and consumption of hot food and beverages (11,12). Numerous studies have been conducted in this area, and EC incidence has decreased from more than 80/105 to less than 20/105 between 1983 and 1997 through countless efforts towards comprehensive prevention and treatment (4,13).
In last decades, the socioeconomic status has improved substantially in China and the EC prevention and control strategies were optimized and performed well. In Henan, endoscopy screening program (opportunistic/organized) has been conducted since 2005. Furthermore, various ways of health education promotion were carried out every year. It is of great importance to retain the currency of EC incidence and mortality in Henan. Meanwhile, it is imperative to determine if the trend continues to decline or is reversed. Therefore, this study was designed to analyze the current incidence and mortality of EC in Henan, and to further present the updated essential data to medical policymakers for prompt and effective modification even optimization of the prevention and control strategy. We present the following article in accordance with the STROBE reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4027/rc).
Methods
Data source
The EC incidence and mortality data were extracted from the Henan Cancer Registry Database from 2010 to 2018, which were established based on the Henan Cancer Registry system and coded according to the International Classification of Diseases-10 (ICD-10). In briefly, Henan Cancer Registry system was launched in Linzhou city in 1988 and then expanded gradually to other five areas as of 2008. The number of local cancer registry increased rapidly since 2010 and achieved 42 in 2018. The incident and death data were collected by local cancer registry from hospitals, community healthcare center, village doctors, insurance system and vital statistical system and then submitted to Henan Provincial Cancer Registry for quality control and management. In 2018, there were 42 local cancer registries submitted cancer incidence and mortality data. After quality check, three local cancer registries (Gushi, Anyang, and Xinxiang counties) was excluded from the database due to a lack of completeness. Finally, data from 39 cancer registries were included for analysis, including 10 urban registries and 29 rural registries, and comprised a total of 33,271,234 people (17,055,226 males and 16,216,008 females) accounting for 30.51% of the whole population in Henan. In urban and rural areas, there were 24,331,311 (73.13%) and 8,939,923 (26.87%) individuals, respectively (Figure 1).
Figure 1.
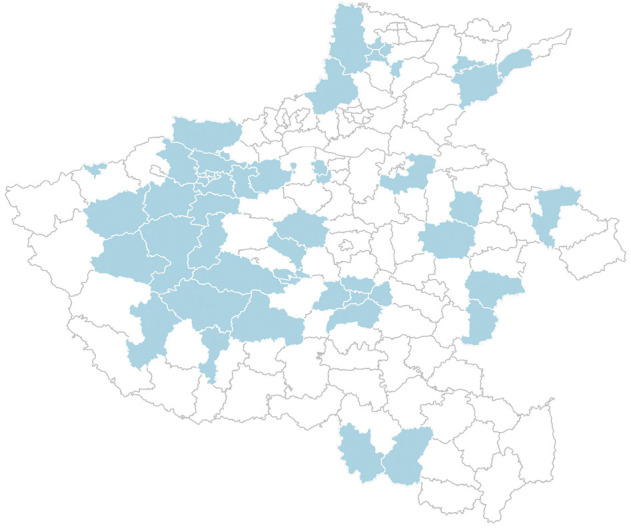
Distribution of local cancer registries in Henan, 2018.
In the current study, the population data in local cancer registry was collected from government institute. The standard Chinese population were estimated based on the 5th National Population Census data published by the National Bureau of statistics (NBS) and the changes of urban-rural ratio and age structure of the population. And the standard world population was Segi’s population. The population were stratified by area (urban and rural), gender (male/female), and age groups (0~,1–4, 5–9, 10–14, … 80–84, and 85+ years old). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Quality control
The data quality control was performed according to the “Chinese Guideline for Cancer Registration” (14) and the principles of quality control for cancer registration published by IARC and International Association for Cancer Registries (IACR). The cancer registry data quality in this study was systematically evaluated from three aspects: comparability, completeness, and validity. All data were evaluated by mortality to incidence ratio (M/I), morphological verification (MV%), death certification only (DCO%), and unknown basis of diagnosis (UB%). Among these indicators, M/I, MV%, and DCO% are important indicators to evaluate the integrity and validity of cancer registry data. The M/I was usually 0.6–0.8. An M/I <0.6 indicated that death may have been underreported; 0.8 indicated that the incidence may have been underreported. Furthermore, the incidence and mortality of cancers in each local cancer registry were also checked year by year to ensure them didn’t fluctuate drastically. Both the incidence and mortality were relatively stable from 2010 to 2018 indicated that the quality of database was acceptable. A summary of different quality control indicators in 2018 is displayed in Table 1.
Table 1. Quality control of EC in Henan, 2018.
| Areas | Gender | M/I | MV (%) | DCO (%) | UB (%) |
|---|---|---|---|---|---|
| All | Male | 0.77 | 80.03 | 1.19 | 0 |
| Female | 0.74 | 79.99 | 1.23 | 0 | |
| Both | 0.76 | 80.02 | 1.21 | 0 | |
| Urban | Male | 0.74 | 77.98 | 2.27 | 0 |
| Female | 0.71 | 80.09 | 2.08 | 0 | |
| Both | 0.73 | 78.72 | 2.2 | 0 | |
| Rural | Male | 0.78 | 80.55 | 0.92 | 0 |
| Female | 0.75 | 79.97 | 1.03 | 0 | |
| Both | 0.77 | 80.33 | 0.97 | 0 |
EC, esophageal cancer; M/I, mortality to incidence ratio; MV, morphological verification; DCO, death certification only; UB, unknown basis of diagnosis.
Outcomes and measurement
In this study, the primary outcomes included incidence rates, mortality rates, cumulative rates (0–74 years) and the annual percentage change (APC) of incidence and mortality. More specifically, the incidence and mortality rates included crude incidence and mortality, and age-standardized incidence and mortality adjusted by the Chinese standard population and world Segi’s population. The formula for crude incidence and mortality was as follow:
| [1] |
The cumulative rates indicated the possibility of individual had specific disease onset during birth and a specific age. The EC cumulative rate from 0 to 74 years was calculated as follows:
| [2] |
When calculating the APC based on age-standardized rate (ASR), the calendar year is an independent variable that is used to fit the regression line of the natural logarithm of ASR. The formula was used as follows:
| [3] |
where β is the estimated value of the slope b. By analyzing ASR and APC, the effectiveness of current prevention strategies can be established, and more targeted strategies can be formulated when necessary.
Statistical analysis
The incidence and mortality of EC were calculated by areas, gender, and age group. The numbers of incident cases and deaths were estimated based on the incidence, mortality, and corresponding populations. The age-standardized incidence and mortality were calculated according to Segi’s population and the Chinese population (5th National Population Census in 2000). More importantly, the APC and average annual percentage change (AAPC) and corresponding 95% confidence interval (CI) were calculated to depict the trend of ASR. If the estimates of APC or AAPC and corresponding lower boundary of the 95% CI were both >0, the ASR was considered on the rise. On the contrary, if the estimates of APC and its upper boundary of the 95% CI were both <0, the ASR was considered in a downward trend. Otherwise, the ASR was considered stable over time. In the present study, APC, AAPC, and 95% CI were calculated by Joinpoint 4.8 (National Cancer Institute, Rockville, MD, USA). Meanwhile, age-trend of incidence and mortality was also evaluated by Joinpoint linear regression. Other analyses were performed using the software SAS 9.4 (SAS Institute, Cary, NC, USA) and GraphPad Prism 8 (GraphPad Software, San Diego, CA, USA). The level of statistical significance was set as two-sided P<0.05.
Results
Incidence and mortality of EC in 2018
Table 2 shows the incidence rates of EC by areas in Henan, 2018. There was an estimated total of 29,913 new cases, including 22,809 cases in rural areas, with 3.21 times as many cases in rural areas than in urban areas (7,104 cases). The crude incidence of EC was 27.43/105, and the age-standardized incidence rate by world standard population (ASIRW) was 19.96/105. The cumulative incidence rate was 2.55% for individuals aged 0–74 years. More specifically, above rates in rural areas were 30.37/105, 22.35/105, and 2.88%. In contrast, they were 20.92/105, 14.84/105, and 1.85%, respectively, in urban areas, which were lower than those in rural areas. Therefore, the burden of EC in rural areas was more severe than that in urban areas.
Table 2. Incidence of esophageal cancer in Henan Province, 2018.
| Areas | Gender | Cases | Incidence (1/105) | ASIRW (1/105) | ASIRC (1/105) | Cumulative rate (0–74 years, %) |
|---|---|---|---|---|---|---|
| All | Both | 29,913 | 27.43 | 19.96 | 19.75 | 2.55 |
| Male | 18,715 | 33.07 | 26.00 | 25.63 | 3.30 | |
| Female | 11,198 | 21.34 | 14.17 | 14.10 | 1.79 | |
| Urban | Both | 7,104 | 20.92 | 14.84 | 14.58 | 1.85 |
| Male | 4,601 | 26.43 | 20.21 | 19.84 | 2.51 | |
| Female | 2,503 | 15.13 | 9.75 | 9.60 | 1.20 | |
| Rural | Both | 22,809 | 30.37 | 22.35 | 22.16 | 2.88 |
| Male | 14,114 | 36.02 | 28.66 | 28.29 | 3.67 | |
| Female | 8,695 | 24.2 | 16.26 | 16.23 | 2.07 |
ASIRW, age-standardized incidence rate by world standard population; ASIRC, age-standardized incidence rate by Chinese standard population.
Table 3 shows the mortality rates of EC in Henan. In 2018, the number of deaths in Henan was 22,688, including 14,353 male cases and 8,335 female cases. The crude mortality rate of EC was 20.80/105. The age-standardized mortality rate by world standard population (ASMRW) was 14.47/105, respectively. The crude mortality rate of EC was higher in rural areas (23.25/105) than that in urban areas (15.39/105). The ASMRW in rural areas (16.36/105) was 1.57 times higher than that in urban areas (10.44/105).
Table 3. Mortality of esophageal cancer in Henan, 2018.
| Areas | Gender | Cases | Mortality (1/105) | ASMRW (1/105) | ASMRC (1/105) | Cumulative rate 0–74 (%) |
|---|---|---|---|---|---|---|
| All | Both | 22,688 | 20.80 | 14.47 | 14.36 | 1.71 |
| Male | 14,353 | 25.36 | 19.64 | 19.42 | 2.36 | |
| Female | 8,335 | 15.89 | 9.61 | 9.59 | 1.07 | |
| Urban | Both | 5,226 | 15.39 | 10.44 | 10.22 | 1.16 |
| Male | 3,427 | 19.68 | 14.79 | 14.44 | 1.69 | |
| Female | 1,799 | 10.88 | 6.38 | 6.29 | 0.64 | |
| Rural | Both | 17,462 | 23.25 | 16.36 | 16.32 | 1.97 |
| Male | 10,926 | 27.89 | 21.89 | 21.73 | 2.66 | |
| Female | 6,536 | 18.19 | 11.14 | 11.17 | 1.27 |
ASMRW, age-standardized mortality rate by world standard population; ASMRC, age-standardized mortality rate by Chinese standard population.
Age-specific incidence rates and mortality rates of EC in 2018
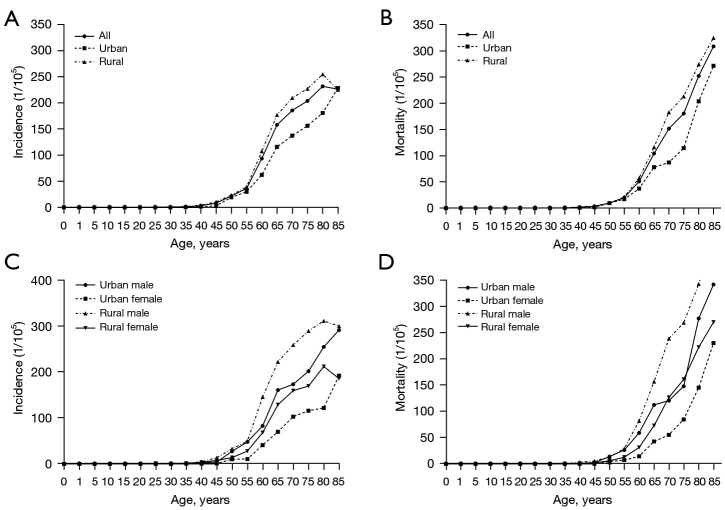
Overall, the age-specific incidence rates of EC were relatively low among individuals aged <44 years. An upward trend was revealed after 45 years, which peaked in the 80–84 age group. Similarly, an increasing trend was observed among individuals aged >45 years in both urban and rural areas. However, the incidence rates of EC decreased sharply after reaching its peak in the 80–84 years group in rural females and rural males. The age-specific mortality rates of EC were relatively low before age 44 years yet dramatically increased with age among individuals after age 45. Similarly, the trend was found in both urban and rural individuals and the mortality rates in all age groups in rural areas were higher than those in urban areas. However, the mortality rates in females in all age groups were lower than those in males in both urban and rural areas (Figure 2, Tables 4,5).
Figure 2.
Age-specific incidence and mortality of EC in Henan, 2018. EC, esophageal cancer.
Table 4. Joinpoint linear regression analysis on age-specific incidence for esophageal cancer in Henan, 2018.
| Areas | Gender | Segment 1 (slope) | Segment 2 (slope) | Segment 3 (slope) | Segment 4 (slope) |
|---|---|---|---|---|---|
| All | Both | 0–44 (0.01) | 45–59 (2.54) | 60–74 (10.54*) | 75–85+ (2.38*) |
| Male | 0–54 (0.28*) | 55–74 (11.62*) | 75–85+ (4.05*) | ||
| Female | 0–44 (0.03) | 45–59 (1.39) | 60–74 (8.10*) | 75–85+ (3.23*) | |
| Urban | Both | 0–44 (−0.04) | 45–59 (2.37) | 60–85+ (6.34*) | |
| Male | 0–39 (0.05) | 40–54 (1.37) | 55–85+ (7.83*) | ||
| Female | 0–44 (0.00) | 45–59 (0.87) | 60–85+ (5.38*) | ||
| Rural | Both | 0–54 (0.17) | 55–74 (10.58*) | 75–85+ (1.44) | |
| Male | 0–54 (0.28*) | 55–74 (13.11*) | 75–85+ (2.51*) | ||
| Female | 0–59 (0.37*) | 60–74 (10.25*) | 75–85+ (1.97) |
*, P<0.05.
Table 5. Joinpoint linear regression analysis on age-specific mortality for esophageal cancer in Henan, 2018.
| Areas | Gender | Segment 1 (slope) | Segment 2 (slope) | Segment 3 (slope) | Segment 4 (slope) |
|---|---|---|---|---|---|
| All | Both | 0–44 (0.01) | 45–59 (1.05*) | 60–79 (8.55*) | 80–85+ (12.33*) |
| Male | 0–44 (-0.01) | 45–59 (1.84*) | 60–79 (10.75*) | 80–85+ (15.98*) | |
| Female | 0–49 (0.00) | 50–64 (1.62*) | 65–79 (7.61*) | 80–85+ (12.06*) | |
| Urban | Both | 0–54 (0.02) | 55–79 (4.55*) | 79–85+ (16.07*) | |
| Male | 0–54 (0.10) | 55–79 (6.21*) | 79–85+ (19.42*) | ||
| Female | 0–59 (0.05) | 59–79 (3.81*) | 79–85+ (14.87*) | ||
| Rural | Both | 0–44 (0.02) | 45–59 (0.96) | 60–85+ (10.31*) | |
| Male | 0–44(0.02) | 45–59 (1.52) | 60–85+ (13.17*) | ||
| Female | 0–49 (0.00) | 46–64 (1.72) | 65–85+ (9.70*) |
*, P<0.05
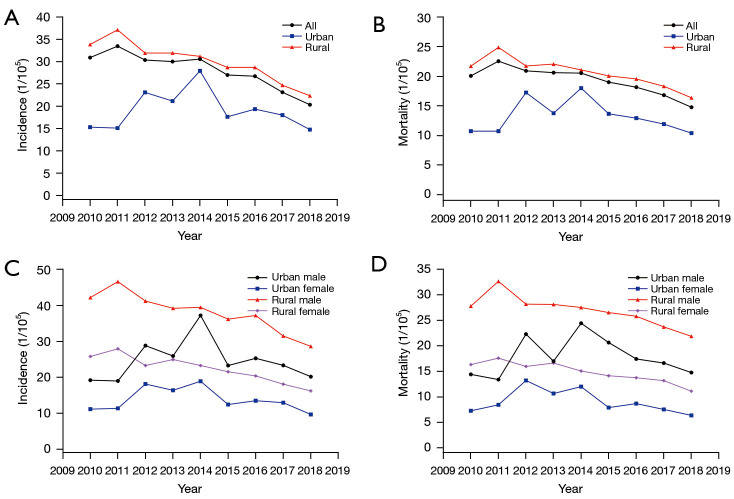
Trends of EC incidence and mortality rates during 2010–2018
From 2010 to 2018, the incidence rates of EC in Henan showed a downward trend, in which the decline during the period 2014–2018 was significant (APC =−8.9, 95% CI: −14.5 to −3, P<0.001). The incidence rates of EC in females also exhibited a similar downward trend in this period (APC =−10.1, 95% CI: −15 to −4.8, P<0.001). Similarly, the overall incidence rate of EC in rural areas also showed a significant downward trend from 2010 to 2018 (APC =−5.2, 95% CI: −6.9 to −3.4, P<0.001). During the same period, there were also significant downward trends for incidence rates in males and females (males: APC =−4.9, 95% CI: −6.7 to −3, P<0.001; females: APC =−5.8, 95% CI: −7.6 to −3.9, P<0.001) (Table 6, Figure 3). Meanwhile, the mortality rate of EC in Henan also showed a downward trend, in which the decline was significant during 2014–2018 (APC =−7.6, 95% CI: −13 to −2, P<0.001). In males and females, the mortality rates of EC both exhibited an obvious downward trend from 2010 to 2018 (APC =−3.5, 95% CI: −5.5 to −1.5, P<0.001) and from 2013 to 2018 (APC =−8.1, 95% CI: −11.8 to −4.3, P<0.001), respectively. In rural areas, the overall mortality rates of EC showed significant downward trends from 2010 to 2018 (APC =−3.9, 95% CI: −5.6 to −2.1, P<0.001), and similar trends were observed among males and females during the same period (Table 7, Figure 3).
Table 6. The trend of incidence of esophageal cancer in Henan, 2010–2018.
| Areas | Gender | Period | APC (95% CI) | P value | AAPC (95% CI) |
|---|---|---|---|---|---|
| All | Both | 2010–2014 | −1.1 (−7.1, 5.3) | 0.7 | −5.1 (−8, −2.1) |
| 2014–2018 | −8.9 (−14.5, −3) | <0.001 | |||
| Male | 2010–2016 | −2.7 (−6.2, 1) | 0.1 | −5.4 (−9.4, −1.2) | |
| 2016–2018 | −13.1 (−30.2, 8.1) | 0.1 | |||
| Female | 2010–2014 | −1.4 (−6.8, 4.4) | 0.5 | −5.8 (−8.5, −3.1) | |
| 2014–2018 | −10.1 (−15, −4.8) | <0.001 | |||
| Urban | Both | 2010–2014 | 13.4 (−3.5, 33.2) | 0.1 | −0.3 (−8, 8.1) |
| 2014–2018 | −12.2 (−25.3, 3.1) | 0.1 | |||
| Male | 2010–2014 | 14.5 (−1.7, 33.4) | 0.1 | 0.7 (−6.6, 8.7) | |
| 2014–2018 | −11.4 (−23.9, 3.3) | 0.1 | |||
| Female | 2010–2013 | 19.3 (−11.6, 60.9) | 0.2 | −0.5 (−9.9, 9.8) | |
| 2013–2018 | −10.8 (−22, 2) | 0.1 | |||
| Rural | Both | 2010–2018 | −5.2 (−6.9, −3.4) | <0.001 | −5.2 (−6.9, −3.4) |
| Male | 2010–2018 | −4.9 (−6.7, −3) | <0.001 | −4.9 (−6.7, −3) | |
| Female | 2010–2018 | −5.8 (−7.6, −3.9) | <0.001 | −5.8 (−7.6, −3.9) |
APC, average percentage change; AAPC, annual average percentage change; CI, confidence interval.
Figure 3.
Trends of the incidence and mortality of EC by area and gender in Henan, 2010–2018. EC, esophageal cancer.
Table 7. The trend of mortality of esophageal cancer in Henan, 2010–2018.
| Areas | Gender | Period | APC (95% CI) | P value | AAPC (95% CI) |
|---|---|---|---|---|---|
| All | Both | 2010–2014 | −0.3 (−6.1, 5.9) | 0.9 | −4.0 (−6.9, −1.1) |
| 2014–2018 | −7.6 (−13, −2) | <0.001 | |||
| Male | 2010–2018 | −3.5 (−5.5, −1.5) | <0.001 | −3.5 (−5.5, −1.5) | |
| Female | 2010–2013 | 1.2 (−7.6, 10.8) | 0.7 | −4.7 (−7.5, −1.8) | |
| 2013–2018 | −8.1 (−11.8, −4.3) | <0.001 | |||
| Urban | Both | 2010–2014 | 12 (−6.4, 34) | 0.2 | −0.6 (−9.2, 8.7) |
| 2014–2018 | −11.9 (−26.4, 5.5) | 0.1 | |||
| Male | 2010–2014 | 13.5 (−7.2, 38.9) | 0.2 | 0.8 (−8.9, 11.4) | |
| 2014–2018 | −10.6 (−26.9, 9.4) | 0.2 | |||
| Female | 2010–2012 | 35.3 (−15.3, 116) | 0.1 | −0.6 (−9.4, 9) | |
| 2012–2018 | −10.3 (−17.1, −2.9) | <0.001 | |||
| Rural | Both | 2010–2018 | −3.9 (−5.6, −2.1) | <0.001 | −3.9 (−5.6, −2.1) |
| Male | 2010–2018 | −3.5 (−5.3, −1.7) | <0.001 | −3.5 (−5.3, −1.7) | |
| Female | 2010–2018 | −4.7 (−6.4, −2.9) | <0.001 | −4.7 (−6.4, −2.9) |
APC, average percentage change; AAPC, annual average percentage; CI, confidence interval.
Discussion
The current study extrapolated the epidemiology of EC in Henan during 2010 to 2018 based on Cancer registry data. The incidence and mortality of EC showed decreasing trends, especially in rural areas. Nonetheless, the burden of EC in Henan was still high. Thus, it is essential to maintain, even strengthen and optimize the ongoing EC prevention and control strategies.
In 2018, the ASIRW and ASMRW of EC in Henan were still higher than the average rates in China (11.13/105, 8.28/105) (15) and the globe (6.3/105, 5.6/105) (1). This implied that the disease burden of EC in Henan was still high and effective prevention and control strategies required extended effective implementation. Meanwhile, the male predominance observed in incidence and mortality was also in line with that in China, the United Kingdom, the United States, and other regions (10,16,17), which indicated these regions may have similarly distributed risk factors. Regarding male predominance, alcohol use and tobacco smoking/exposure were clearly established risk factors for EC development (2). Thus, the higher use of alcohol and tobacco in males than that in females may be one explanation. In Henan, the active smoking prevalence among males was as high as 57.5% in adults aged 30 years and older, in contrast to that of only 0.6% in females (18). As for alcohol use, 33.8% of men reported drinking alcohol regularly, which was also significantly correlated with an increased risk of EC, especially among those who reported flushing after alcohol consumption, whereas the proportion of women reporting alcohol drinking was very low (19). In addition, hormonal factors may inhibit the development of EC; there is evidence that estrogen may lower the risk of EC in women (20). Besides, the higher incidence and mortality in rural areas than that in urban areas had been reported before in China (21). This phenomenon reflected the heterogeneity of EC risk factors, and allocation of unbalanced medical resources across areas (17).
The age specific-incidence and mortality increased rapidly from the 45–54 age group onwards and reached the peak in the 80–84 and older group. Thus, population aging contributed substantially to the increase of incidence and mortality (22). An important implication of these figures was the identification of the target population for intervention in EC prevention and control. For primary prevention, although the whole population is expected to be targeted, some subgroups including males, rural dwellers, and individuals aged 45 and older should receive higher priority for limited medical resources, because they would face a higher risk of EC. For secondary prevention, it was observed that age-specific incidence gradually increased after 40 years of age, supporting that high-risk individuals should be screened by endoscopy after 40 years of age which had been recommended by guidelines. However, endoscopy and biopsy are traumatic and a well-trained technologist is required, which might reduce the compliance of population screening and limit its widespread application. Meanwhile, the effectiveness of large-scale endoscopic screening for EC had not been clarified (23). Therefore, a risk prediction model was proposed to identify the high-risk individuals so that the screening population could be consolidated, circumventing unnecessary examinations and expenses (24), which will be of great significance to improve the coverage and efficacy of EC screening in China.
From 2010 to 2018, the incidence and mortality of EC in Henan decreased year by year, and the downward trend was significant between 2014 and 2018. Similar decreasing trends were also observed throughout China (15,21). On the one hand, tobacco smoking is one of the established factors for EC (12), and thus, effective tobacco smoking control could reduce the incidence of EC (25). In the past years, China has implemented broad smoking bans, and consequently, the prevalence of smoking and second-hand smoking in public places has dropped significantly over time (26), which contributed to the decreasing incidence of EC. Meanwhile, the public awareness of cancer prevention and control was improved after a series of plans and policies on cancer control were released by government in 2015. In turn, a higher level of cancer prevention awareness was also associated with a relatively lower risk of developing EC (27), which could be explained by the fact that cancer prevention awareness was an independent factor to facilitate healthy lifestyles, and increase their compliance of EC screening (28). On the other hand, starting in 2007, Henan conducted an organized EC endoscopy-based screening program in high-risk areas and populations. Screening could identify lesions early and improve patient’s prognosis. Thereafter, the incidence and mortality of EC showed reductions. In addition, the decreasing trend of incidence and mortality further validated the efficacy of endoscopy-based cancer screening in China (29,30). The mortality reduction also reflected the improvement in the quality of cancer care, including the access to, quality, and funding of such services (31). Nevertheless, the incidence and mortality of EC in Henan have remained at a high level, and effective prevention and control strategies require ongoing implementation.
For the first time, the current study depicted the updated epidemiology and trends of EC in Henan and internationally, using data from cancer registry system which covered 30.51% of the whole population. Our findings are significant for EC prevention and control in China, even in the world. However, as mentioned before, the current study was conducted based on the cancer registry, which was launched officially in 2009. The cancer registry has been on track since 2010 and scaled up gradually. Thus, the current study had following inevitable shortfalls. First, we were unable to analyze the trend change over a longer time period due to the relatively recent implementation of the cancer registry. Second, with the scaling up, the number of cancer registries enrolled in the current analysis was increasing with time. To minimize the influence of data sources, the current study used the same quality control criteria for the database from 2010 to 2018. Third, due to limitations of the cancer registry system, the clinical characteristics of EC were unable to be obtained in detail, which made it difficult to stratify the data to perform some interesting analyses, such as the distribution of tumor stage and tumor size.
Conclusions
The incidence and mortality of EC in Henan were much higher than the average level of China and the globe. Decreasing trends were observed for ASIRW and ASMRW during the period from 2010 to 2018. However, the trends in urban areas were relatively stable as compared with those in rural areas. Male predominance was found in both urban and rural areas for the incidence and mortality of EC.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: This study was funded by Key Project of Intergovernmental International Scientific and Technological Innovation Cooperation of National Key R&D Program (No. 2021YFE0106000).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-4027/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-4027/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4027/coif). The authors have no conflicts of interest to declare.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 2.Uhlenhopp DJ, Then EO, Sunkara T, et al. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol 2020;13:1010-21. 10.1007/s12328-020-01237-x [DOI] [PubMed] [Google Scholar]
- 3.Short MW, Burgers KG, Fry VT. Esophageal Cancer. Am Fam Physician 2017;95:22-8. [PubMed] [Google Scholar]
- 4.DiSiena M, Perelman A, Birk J, et al. Esophageal Cancer: An Updated Review. South Med J 2021;114:161-8. 10.14423/SMJ.0000000000001226 [DOI] [PubMed] [Google Scholar]
- 5.Thrift AP. Global burden and epidemiology of Barrett oesophagus and oesophageal cancer. Nat Rev Gastroenterol Hepatol 2021;18:432-43. 10.1038/s41575-021-00419-3 [DOI] [PubMed] [Google Scholar]
- 6.Huang FL, Yu SJ. Esophageal cancer: Risk factors, genetic association, and treatment. Asian J Surg 2018;41:210-5. 10.1016/j.asjsur.2016.10.005 [DOI] [PubMed] [Google Scholar]
- 7.Zhang W, Yan C, Gao X, et al. Safety and Feasibility of Radiotherapy Plus Camrelizumab for Locally Advanced Esophageal Squamous Cell Carcinoma. Oncologist 2021;26:e1110-24. 10.1002/onco.13797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coleman HG, Xie SH, Lagergren J. The Epidemiology of Esophageal Adenocarcinoma. Gastroenterology 2018;154:390-405. 10.1053/j.gastro.2017.07.046 [DOI] [PubMed] [Google Scholar]
- 9.Yang CS, Chen XL. Research on esophageal cancer: With personal perspectives from studies in China and Kenya. Int J Cancer 2021;149:264-76. 10.1002/ijc.33421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang S, Lin S, Li N, et al. Burden, trends, and risk factors of esophageal cancer in China from 1990 to 2017: an up-to-date overview and comparison with those in Japan and South Korea. J Hematol Oncol 2020;13:146. 10.1186/s13045-020-00981-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blot WJ, Li JY, Taylor PR, et al. Nutrition intervention trials in Linxian, China: supplementation with specific vitamin/mineral combinations, cancer incidence, and disease-specific mortality in the general population. J Natl Cancer Inst 1993;85:1483-92. 10.1093/jnci/85.18.1483 [DOI] [PubMed] [Google Scholar]
- 12.Abnet CC, Arnold M, Wei WQ. Epidemiology of Esophageal Squamous Cell Carcinoma. Gastroenterology 2018;154:360-73. 10.1053/j.gastro.2017.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang CS. Research on esophageal cancer in China: a review. Cancer Res 1980;40:2633-44. [PubMed] [Google Scholar]
- 14.Center NC. Chinese Guideline for Cancer Registration[in Chinese]. Beijing: People’s Medical Publishing House Co., LTD; 2016. [Google Scholar]
- 15.Zheng R, Zhang S, Zeng H, et al. Cancer incidence and mortality in China, 2016. Journal of the National Cancer Center 2022. [DOI] [PMC free article] [PubMed]
- 16.Xi Y, Dong W, Qiao L, et al. Trends in incidence and mortality of esophageal cancer in Inner Mongolia, 2010-2015. Thorac Cancer 2020;11:2440-8. 10.1111/1759-7714.13552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu H, Cao S, Xu R. Cancer incidence, mortality, and burden in China: a time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun (Lond) 2021;41:1037-48. 10.1002/cac2.12197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xia C, Zheng R, Zeng H, et al. Provincial-level cancer burden attributable to active and second-hand smoking in China. Tob Control 2019;28:669-75. 10.1136/tobaccocontrol-2018-054583 [DOI] [PubMed] [Google Scholar]
- 19.Im PK, Millwood IY, Kartsonaki C, et al. Alcohol drinking and risks of total and site-specific cancers in China: A 10-year prospective study of 0.5 million adults. Int J Cancer 2021;149:522-34. 10.1002/ijc.33538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang BJ, Zhang B, Yan SS, et al. Hormonal and reproductive factors and risk of esophageal cancer in women: a meta-analysis. Dis Esophagus 2016;29:448-54. 10.1111/dote.12349 [DOI] [PubMed] [Google Scholar]
- 21.He F, Wang J, Liu L, et al. Esophageal cancer: trends in incidence and mortality in China from 2005 to 2015. Cancer Med 2021;10:1839-47. 10.1002/cam4.3647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Global Burden of Disease Cancer Collaboration ; Fitzmaurice C, Allen C, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2017;3:524-48. 10.1001/jamaoncol.2016.5688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang N, Li Y, Chang X, et al. Long-term effectiveness of one-time endoscopic screening for esophageal cancer: A community-based study in rural China. Cancer 2020;126:4511-20. 10.1002/cncr.33119 [DOI] [PubMed] [Google Scholar]
- 24.Li H, Sun D, Cao M, et al. Risk prediction models for esophageal cancer: A systematic review and critical appraisal. Cancer Med 2021;10:7265-76. 10.1002/cam4.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Islami F, DeSantis CE, Jemal A. Incidence Trends of Esophageal and Gastric Cancer Subtypes by Race, Ethnicity, and Age in the United States, 1997-2014. Clin Gastroenterol Hepatol 2019;17:429-39. 10.1016/j.cgh.2018.05.044 [DOI] [PubMed] [Google Scholar]
- 26.Sansone G, Fong GT, Yan M, et al. Secondhand smoke exposure and support for smoke-free policies in cities and rural areas of China from 2009 to 2015: a population-based cohort study (the ITC China Survey). BMJ Open 2019;9:e031891. 10.1136/bmjopen-2019-031891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li H, Zeng H, Zheng R, et al. Association of cancer awareness levels with the risk of cancer in rural China: A population-based cohort study. Cancer 2020;126:4563-71. 10.1002/cncr.33029 [DOI] [PubMed] [Google Scholar]
- 28.Jia S, Li H, Zeng H, et al. Association of cancer prevention awareness with esophageal cancer screening participation rates: Results from a population-based cancer screening program in rural China. Chin J Cancer Res 2019;31:601-8. 10.21147/j.issn.1000-9604.2019.04.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen R, Liu Y, Song G, et al. Effectiveness of one-time endoscopic screening programme in prevention of upper gastrointestinal cancer in China: a multicentre population-based cohort study. Gut 2021;70:251-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wei WQ, Chen ZF, He YT, et al. Long-Term Follow-Up of a Community Assignment, One-Time Endoscopic Screening Study of Esophageal Cancer in China. J Clin Oncol 2015;33:1951-7. 10.1200/JCO.2014.58.0423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zeng H, Chen W, Zheng R, et al. Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health 2018;6:e555-67. 10.1016/S2214-109X(18)30127-X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as