Abstract
Background:
Periapical intraoral radiographs are useful in assessing periapical pathologies; essential information often is not extracted owing to difficult interpretation and two-dimensional presentation of three-dimensional structures focusing on using cone beam CT (CBCT) and other advanced imaging modalities.
Aims:
The present study was conducted to comparatively assess the digital intraoral radiography to CBCT in the diagnosis of periapical pathologies.
Materials and Methods:
In 50 teeth, CBCT and digital imaging were compared in assessing periapical pathologies using CBCTPA and six-point scoring. The scores obtained were assessed and compared with statistical evaluation. The data were expressed in percentage and number and mean and standard deviation. The level of significance was kept at P < 0.05.
Results:
On comparing 3D CBCT and 2D digital imaging for assessing the study parameters, it was seen that resorption was seen in 33, 30, and 9 teeth, respectively, on 3, 2, and 1 rooted tooth on CBCT and 13, 16, and 7 teeth on digital radiography. The numbers of roots and root canals on CBCT were 45, 34, and 18 in 3, 2, and 1 rooted tooth and 50, 32, and 18 on digital imaging. Lesions were detected on CBCT in 16, 18, and 18 teeth on CBCT in 3, 2, and 1 rooted tooth, respectively, and in 14, 14, and 16 teeth on digital imaging. Comparing the five-point scale for lesions and CBPAI index for CBCT and digital imaging, the difference was statistically significant with P = 0.004 and <0.0001, respectively.
Conclusion:
The present study concludes that 3D CBCT is superior in accuracy to 2D imaging in diagnosing the periapical lesions, especially concerning multirooted teeth. Owing to its high radiation exposure and cost, 2D imaging can be incorporated in assessing periapical pathology for the single-rooted tooth.
KEYWORDS: Computed tomography [CT scan], cone beam computed tomography [CBCT], digital radiography, periapical pathologies
INTRODUCTION
Periapical tissue destruction following periodontitis and pulpal necrosis can lead to local bone response around the root apex and result in the formation of inflammatory lesions in the periapical region. However, sometimes, periapical lesions in the bone may be detected using imaging in asymptomatic subjects with apical periodontitis. Detection of such lesion radiographically is governed by various factors including radiation geometry, mineralization and thickness of the surrounding bone, imaging system resolution, and/or extent of the lesion concerned.[1]
Accurate early detection of these lesions is vital in diagnosis, treatment planning, and follow-up of the subjects and warrants information including lesion extent, the number of root canals and roots involved, and lesion connection from different roots. Commonly used periapical intraoral radiographs are useful in assessing periapical pathologies; essential information often is not extracted owing to difficult interpretation and two-dimensional presentation of three-dimensional structures.[2]
Digital imaging has certain advantages over conventional radiography including no wet processing, comparable resolution, less dose, fast image.[3] 3D imaging modality, CBCT (cone beam CT), was introduced in 2000 for assessing jaw bones and associated pathologies utilizing the tomosynthesis principle and cone-shaped X-ray beam. The CBCT images are captured in raw format and undergo 3D reconstruction to reconstruct desired anatomic structure with 0.07–0.05 voxels.
CBCT in dentistry is used widely to assess temporomandibular joint and associated disorders, impacted tooth and related anatomical structures, and planning of dental implants. CBCT is advantageous over conventional CT concerning compact size, hard tissue display, low exposure, undistorted images, low cost, and high resolution.[4] However, the use of CBCT is limited compared to conventional dental digital radiography with both having their limitations and advantages in detecting periapical pathologies. The data concerning the comparison of the two is limited in the literature. Hence, the present study was conducted to comparatively evaluate the digital intraoral radiography to CBCT in the diagnosis of periapical pathologies.
MATERIALS AND METHODS
The present study was conducted to comparatively assess the digital intraoral radiography to CBCT in the diagnosis of periapical pathologies. The study was conducted after obtaining clearance from the concerned Ethical committee. The study population was comprised of subjects visiting the Outpatient Department of Oral Medicine and Radiology. The study included a total of 38 subjects having periapical lesions on previous radiographs. The study had both males (n = 27) and females (n = 11) within the age range of 17–72 years and the mean age of 48.7 ± 3.86 years. In 38 subjects, 50 teeth were evaluated. The detailed study design was explained and consent was taken verbally and in written format from all the subjects. The lesions were assessed on digital intraoral radiography [Figure 1] and CBCT.
Figure 1.

Periapical lesion assessment radiographically
Digital intraoral radiographs were taken by a single expert using the same exposure parameter (60–64 kV, 0.32 s, and 8 mA) and a single X-ray machine using paralleling technique and position holding device with the sensor placed parallel to concerning teeth. CBCT evaluation was done by a single examiner blinded to the study using constant parameters (70–74 kV, 10.6 s, and 10 mA) at a voxel size of 76.5. To better visualize the images, manipulation was allowed concerning zoom, contrast, brightness, inversion, edge-enhancement, and pseudocolors using the same software that was used to capture the image. 3D slicing was done for CBCT images. Periapical pathology was assessed on the X-, Y-, and Z-axis analyzing each slice separately [Figure 2]. All images were evaluated by three examiners, and disagreement was followed as suggested by the majority.
Figure 2.
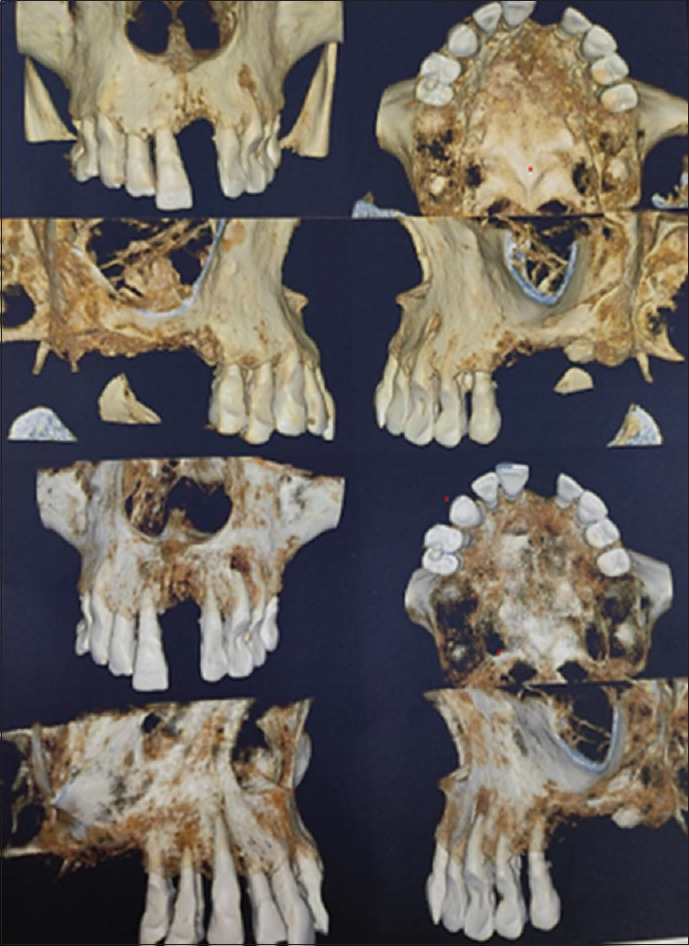
Periapical lesion assessment on CBCT
Any periapical radiolucency attached to root apex with extension to a minimum to twice the periodontal ligament space width was defined as a periapical lesion. On CBCT, the lesion was considered present if it was visible on more than one image plane. Scoring lesions assigned to the periapical lesion were as follows: 1: lesion absent, 2: probable absence of the lesion, 3: uncertainty about lesion presence, 4: lesion probably present, and 5: lesion present. Apical marginal communication was affirmative with PDL space was twice or more of normal width.
In CBCT and digital imaging lesion extent and location, maxillary sinus, cortical bone, mandibular canal, root canal, and root number, external root resorption, and root fractures were assessed. In both the arches, distance from root apices to mandibular canal, nasal fossa, and maxillary sinus was measured with inbuilt software and tools. For CBCT and digital radiography, CBCT periapical index was used[5] along with six-point scoring. The scores obtained were assessed and compared.
The collected data were subjected to the statistical evaluation using SPSS software version 21 (Chicago, IL, USA) for results formulation. The data were expressed in percentage and number and mean and standard deviation. The level of significance was kept at P < 0.05.
RESULTS
The present study was conducted to comparatively assess the digital intraoral radiography to CBCT in the diagnosis of periapical pathologies. The present study included a total of 38 subjects having periapical lesions on previous radiographs. The study had both males (n = 27) and females (n = 11) within the age range of 17–72 years and the mean age of 48.7 ± 3.86 years. In 38 subjects, 50 teeth were evaluated. The demographic characteristics of the study subjects are listed in Table 1. Among 50 evaluated teeth, there were 15 (30%) incisors from maxilla, 8% (n = 4) premolars from maxilla, and 6% (n = 3) from the mandible, and 30% (n = 15) molars were from maxilla and 26% (n = 13) molars were from mandible.
Table 1.
Demographic characteristics of the study subjects
| Characteristic | n | % |
|---|---|---|
| Mean age (years) | 48.7±3.86 | |
| Age range (years) | 17-72 | |
| Gender | ||
| Males | 27 | 71.05 |
| Females | 11 | 28.94 |
| The total number of teeth evaluated | 50 | 100 |
| Teeth Involved | ||
| Incisors | ||
| Maxilla | 15 | 30 |
| Mandible | 0 | 0 |
| Premolars | ||
| Maxilla | 4 | 8 |
| Mandible | 3 | 6 |
| Molars | ||
| Maxilla | 15 | 30 |
| Mandible | 13 | 26 |
On comparing 3D CBCT and 2D digital imaging for assessing the study parameters, it was seen that coincidental involvement of other teeth on CBCT was seen in two cases and was not seen in any teeth on digital imaging, whereas in single-rooted teeth, 10 teeth had this involvement on CBCT and 1 on digital radiography. Root fractures were seen in 4, 2, and 1 tooth on CBCT in 3, 2, and 1 rooted tooth and on 1 tooth in 2 and 1 rooted teeth in digital imaging. Lesion extension to anatomic landmark was not seen in any teeth in digital imaging and seven teeth on CBCT. Root resorption was seen in 33, 30, and 9 teeth, respectively, on 3, 2, and 1 rooted tooth on CBCT and 13, 16, and 7 teeth on digital radiography. The numbers of roots and root canals on CBCT were 45, 34, and 18 in 3, 2, and 1 rooted tooth and 50, 32, and 18 on digital imaging. Lesions were detected on CBCT in 16, 18, and 18 teeth on CBCT in 3, 2, and 1 rooted tooth, respectively, and in 14, 14, and 16 teeth on digital imaging [Table 2].
Table 2.
Comparison of CBCT and digital radiography in assessing study parameters
| Parameter | CBCT | Digital radiography | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| 3 rooted teeth | 2 rooted teeth | Single-rooted tooth | 3 rooted teeth | 2 rooted teeth | Single-rooted tooth | |
| Coincidental other teeth involvement | 2 | 1 | 10 | 0 | 0 | 1 |
| Root fracture | 4 | 2 | 1 | 0 | 1 | 1 |
| Apical communication to margin | 9 | 11 | 16 | 5 | 6 | 3 |
| Root resorption | 33 | 30 | 9 | 13 | 16 | 7 |
| Sinus mucosal thickening | 9 | 3 | 1 | 3 | 1 | 0 |
| Lesion extension to an anatomic landmark | 4 | 1 | 2 | 0 | 0 | 0 |
| Root canals number | 45 | 34 | 18 | 50 | 32 | 18 |
| Root number | 45 | 34 | 18 | 50 | 32 | 18 |
| Roots involved | 38 | 31 | 18 | 20 | 23 | 16 |
| Lesion detection | 16 | 18 | 18 | 14 | 14 | 16 |
In study variables, comparing five-point scale for lesions on CBCT, the mean was 4.8186 ± 0.5679 and for digital imaging; it was significantly lesser as 4.3058 ± 1.2488 with P = 0.004. Concerning CBPAI index, the value for CBCT was 3.3943 ± 1.5578 and for the digital radiography was 2.0365 ± 1.9292. This difference was statistically significant with P < 0.0001 [Table 3].
Table 3.
Comparison of five-point scale and CBPAI index in CBCT and diagnostic imaging
| Variable | (Mean±S.D) | P |
|---|---|---|
| Five-point scale for assessing lesion | ||
| CBCT | 4.8186±0.5679 | 0.004 |
| Digital radiography | 4.3058±1.2488 | |
| CBPAI index for assessing lesion | ||
| CBCT | 3.3943±1.5578 | <0.0001 |
| Digital radiography | 2.0365±1.9292 |
DISCUSSION
The present study was conducted to comparatively assess the digital intraoral radiography to CBCT in the diagnosis of periapical pathologies. The present study included a total of 38 subjects having periapical lesions on previous radiographs. The study had both males (n = 27) and females (n = 11) within the age range of 17–72 years and the mean age of 48.7 ± 3.86 years. In 38 subjects, 50 teeth were evaluated. Among 50 evaluated teeth, there were 15 (30%) incisors from maxilla, 8% (n = 4) premolars from maxilla, and 6% (n = 3) from the mandible, and 30% (n = 15) molars were from maxilla and 26% (n = 13) molars were from mandible. These demographics were comparable to the results of Sogur E et al.[6] in 2012, where authors assessed comparable study populations.
3D CBCT and 2D digital imaging were compared for assessing the study parameters; it was seen that coincidental involvement of other teeth on CBCT was seen in two cases and was not seen in any teeth on digital imaging, whereas in single-rooted teeth, 10 teeth had this involvement on CBCT and 1 on digital radiography. The numbers of roots and root canals on CBCT were 45, 34, and 18 in 3, 2, and 1 rooted tooth and 50, 32, and 18 on digital imaging. Lesions were detected on CBCT in 16, 18, and 18 teeth on CBCT in 3, 2, and 1 rooted tooth, respectively, and in 14, 14, and 16 teeth on digital imaging. These results showed that CBCT was better in diagnosing periapical lesions compared to 2D digital imaging. These findings were in agreement with the findings of Lorenzoni DC et al.[7] in 2012 and MM Bornstein et al.[8] in 2011, where authors reported better accuracy with CBCT compared to 2D imaging modalities.
On assessing the study variables in the present study, and on comparing the five-point scale for lesions on CBCT, the mean was 4.8186 ± 0.5679, and for digital imaging, it was significantly lesser as 4.3058 ± 1.2488 with P = 0.004. Concerning CBPAI index, the value for CBCT was 3.3943 ± 1.5578 and for the digital radiography was 2.0365 ± 1.9292. This difference was statistically significant with P < 0.0001. These findings were comparable to the studies of Vandenberghe B et al.[9] in 2008 and Bender P et al.[10] in 2017, where authors reported results as in the present study concerning CBCT and digital radiography.
CONCLUSION
Within its limitations, the present study concludes that 3D CBCT is superior in accuracy to 2D imaging in diagnosing the periapical lesions, especially concerning multirooted teeth. Owing to its high radiation exposure and cost, 2D imaging can be incorporated in assessing periapical pathology for the single-rooted tooth. However, the present study had few limitations including a smaller sample size, geographical area biases, and single-institution nature. Hence, more studies in vivo are warranted to reach a definitive conclusion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dewangan A, Dewangan D, Tiwari M, Singh A, Singh A, Singh RK, et al. The effect of dentate, partial dentate, and non-dentate jaw on mandibular morphology- A radiographic retrospective study. Int J Med Sci Cur Res. 2018;1:172–9. [Google Scholar]
- 2.Antony D, Thomas T, Nivedhitha MS. Two-dimensional periapical, panoramic radiography versus three-dimensional cone-beam computed tomography in the detection of periapical lesion after endodontic treatment: A systematic review. Cureus. 2020;12:7736. doi: 10.7759/cureus.7736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akarslan ZZ, Peker I. Advances in Radiographic Techniques used in Dentistry. Emerging Trends in Oral Health Sciences and Dentistry. IntechOpen. 2015 [Google Scholar]
- 4.Venkatesh E, Elluru SV. Cone-beam computed tomography: Basics and applications in dentistry. J Istanb Univ Fac Dent. 2017;51:102–21. doi: 10.17096/jiufd.00289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pécora JD. A new periapical index based on cone beam computed tomography. J Endod. 2008;34:1325–31. doi: 10.1016/j.joen.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 6.Sogur E, Grondahl HG, Baksi BG, Mert A. Does a combination of two radiographs increase accuracy in detecting acid-induced periapical lesions and does it approach the accuracy of cone-beam computed tomography scanning.? J Endod. 2012;38:131–6. doi: 10.1016/j.joen.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 7.Lorenzoni DC, Bolognese AM, Garib DG, Guedes FR, Sant’ Anna EF. Cone-beam computed tomography and radiographs in dentistry: Aspects related to radiation dose. Int J Dent. 2012;2012:813768. doi: 10.1155/2012/813768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bornstein MM, Lauber R, Sendi P, von Arx T. Comparison of periapical radiography and limited cone-beam computed tomography in mandibular molars for analysis of anatomical landmarks before apical surgery. J Endod. 2011;37:151–7. doi: 10.1016/j.joen.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 9.Vandenberghe B, Jacobs R, Yang J. Detection of periodontal bone loss using digital intraoral and cone-beam computed tomography images: An in vitro assessment of bony and/or infrabony defects. Dentomaxillofac Radiol. 2008;37:252–60. doi: 10.1259/dmfr/57711133. [DOI] [PubMed] [Google Scholar]
- 10.Bender P, Salvi GE, Buser D, Sculean A, Bornstein MM. Correlation of three-dimensional radiologic data with subsequent treatment approach in patients with peri-implantitis: A retrospective analysis. Int J Periodontics Restor Dent. 2017;37:481–9. doi: 10.11607/prd.2844. [DOI] [PubMed] [Google Scholar]


