Abstract
Oral mucoceles or mucoceles are communal minor salivary gland lesions, and they are clinically categorized by the presence of single or multiple, spherical-shaped fluctuant nodules which are asymptomatic and pain free. Application of diode laser for removal of mucosal lesions in the oral cavity is relatively new and viably better alternative to its precedent methods. The added advantage of using a laser includes lesser bleeding, improved or reduced healing time, and its affinity to melatonin that prevents further or recurrent pigmentation.
KEYWORDS: Diode laser, less bleeding, mucocele
INTRODUCTION
Oral mucoceles or mucoceles are communal minor salivary gland lesions, and they are clinically categorized by the presence of single or multiple, spherical-shaped fluctuant nodules which are asymptomatic and pain free.[1] The literature suggests that the occurrence rate is higher in the lower lip when compared to other sites.[2,3,4] The other affected areas include tongue, palate, cheek, and floor of the mouth.[4,5] Mucocele arises from mechanical trauma to the excretory duct of the salivary glands. This causes duct rupture that leads to extravasation of mucin to the connective tissue stroma (mucus extravasation phenomenon).[6,7]
Treatment procedures for mucocele removal include not only conventional surgical technique which is most widely performed but also electrosurgery, cryosurgery, micromarsupialization, and marsupialization. Steroids injections were also reported.[8,9,10] Application of diode laser for removal of mucosal lesions in the oral cavity is a relatively new and viably better alternative to its precedent methods.[11] The added advantage of using a laser includes lesser bleeding, improved or reduced healing time, and its affinity to melatonin that prevents further or recurrent pigmentation.[12]
CASE REPORT
A 27-year-old man presented to the emergency department with swelling on his lower lip. The patient was free of any pain; however, he was complaining about the growing swelling and its effect on the overall facial profile of his face. The swelling has been growing in size for the past 3 months and sometimes causes obstruction while biting or chewing. On being examined clinically, a swelling appearing 10 mm was found on the lower left lip [Figures 1 and 2]. The patient was suggested for diode laser excision of the swelling and the patient agreed.
Figure 1.
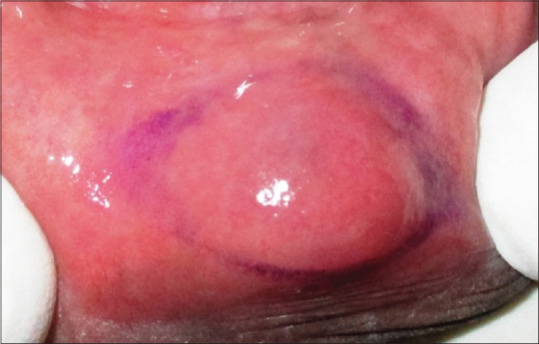
Preoperative image of the lesion
Figure 2.

Preoperative image of the lesion facial view
The lesion was excised with a diode laser with a wavelength of 980 ± 10 nm in continuous wave, with output energy of 1 W. Minimal infiltration of local anesthesia, of concentration 1:2,00,000 Xylocaine, was given and the circumferential incision was placed around the swelling Figures 3-7. There was an absence of bleeding during the procedure. 3-0 silk sutures were placed. The utilization of sutures was efficacious because of the larger area of the surgical site Figures 8-10.
Figure 3.
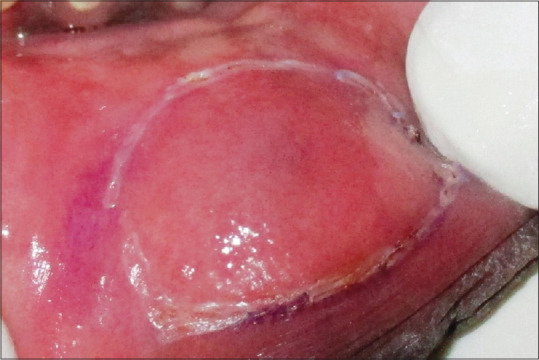
Circumferential incision given
Figure 7.
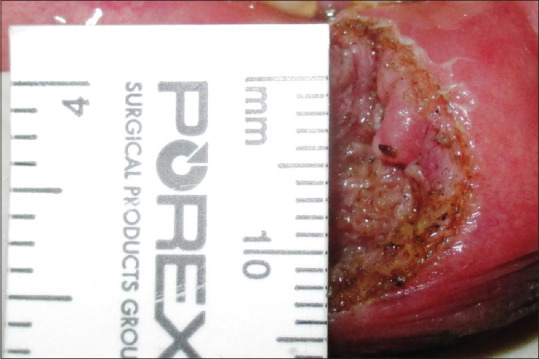
Surgical site calibration
Figure 8.

Sutures placed
Figure 10.

Postoperative after 2 months (facial view)
Figure 4.

Circumferential incision given
Figure 5.
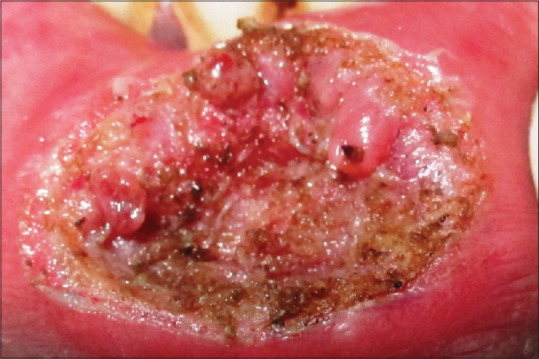
Mucocele excised
Figure 6.

Excised mucocele sample
Figure 9.

Postoperative after 2 months
DISCUSSION
Blood, lymphatic vessels, related muscles, nerves, and salivary gland tissues, which can be serous or mucous in type, make up oral tissues on surfaces subjected to abrasion during mastication, such as the roof of the mouth (palate) and gums, a stratified squamous keratinized epithelium is observed (gingiva). The stratified squamous keratinized epithelium serves as the body's first line of defense against traumatic abnormalities. Tissue fluids, compounded proteins, chromophoric chemicals, and the heme group of blood hemoglobin species are among the components of an oral tissue bio-sample that are required for application of laser.
The oral cavity's mucocele is the second most common lesion. In the age bracket of 10–29 years, the rate of occurrence is higher. Mucocele is characterized by a mucin buildup.[13] It has a dome-like form to it. They usually have a bluish color to them.[14,15,16] Mucocele is most commonly found on the lower lip, followed by the buccal mucosa and mouth floor.[17] Traditional scalpel incision and/or surgical excision, marsupialization, micromarsupialization, corticosteroid injection, sclerosing agent, cryosurgery, electrosurgery, and laser are all validated procedures for treating mucocele in the literature.[16]
Diode lasers provide a faster wound healing and recovery rate than their rivals. Due to its antibacterial and anti-inflammatory qualities, this laser therapy has the extra benefit of improving wound healing without infection or edema.[18]
Soft-tissue laser-assisted procedures have the advantages of minimum intraoperative bleeding, edema, and postoperative pain, besides very little surgical time, scarring, and coagulation. The size of a surgical site determines whether or not sutures are used. Procedures involving small or significant soft-tissue excision, implant exposure with or without bone trimming, can be performed in patients with bleeding problems.[19]
This instance is consistent with prior reports of mucocele excision using a diode laser. The huge amount of tissue removed and the level of patient comfort further supports the novel fact that it can be employed for big mucocele as well.
CONCLUSION
Diode laser is an inevitable boon for future dentistry. Its ease of avail, atraumatic nature, and integrated advantage over conventional methods spur today's clinical practitioners for their routine work.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Anastassov GE, Haiavy J, Solodnik P, Lee H, Lumerman H. Submandibular gland mucocele: Diagnosis and management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:159–63. doi: 10.1067/moe.2000.102771. [DOI] [PubMed] [Google Scholar]
- 2.Singh N, Chandra P, Agarwal S. Oral mucocele: A case report. J Dentofac Sci. 2014;3:47–50. [Google Scholar]
- 3.Mott J, Morrison JA. Blackwell's Five-Minute Veterinary Consult Clinical Companion. Hoboken, NJ, USA: John Wiley & Sons, Inc; 2019. Salivary mucocele; pp. 164–71. [Google Scholar]
- 4.Paglia M, Crippa R, Ferrante F, Angiero F. Mucocele of the minor salivary glands in an infant: Treatment with diode laser. Eur J Paediatr Dent. 2015;16:139–42. [PubMed] [Google Scholar]
- 5.Huang IY, Chen CM, Kao YH, Worthington P. Treatment of mucocele of the lower lip with carbon dioxide laser. J Oral Maxillofac Surg. 2007;65:855–8. doi: 10.1016/j.joms.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 6.Granholm C, Olsson Bergland K, Walhjalt H, Magnusson B. Oral mucoceles; Extravasation cysts and retention cysts. A study of 298 cases. Swed Dent J. 2009;33:125–30. [PubMed] [Google Scholar]
- 7.Dent CD, Svirsky JA, Kenny KF. Large mucous retention phenomenon (mucocele) of the upper lip: Case report and review of the literature. Virginia Dent J. 1997;74:8–9. [PubMed] [Google Scholar]
- 8.Ata-Ali J, Carrillo C, Bonet C, Balaguer J, Penarrocha M, Penarrocha M. Oral mucocele: Review of the literature. J Clin Exp Dent. 2010;2:e18–21. [Google Scholar]
- 9.Oka M, Nishioka E, Miyachi R, Terashima M, Nishigori C. Case of superficial mucocele of the lower lip. J Dermatol. 2007;34:754–6. doi: 10.1111/j.1346-8138.2007.00377.x. [DOI] [PubMed] [Google Scholar]
- 10.Chaitanya P, Praveen D, Reddy M. Mucocele on lower lip: A case series. Indian Dermatol Online J. 2017;8:205–7. doi: 10.4103/idoj.IDOJ_151_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ortega-Concepción D, Cano-Durán JA, Peña-Cardelles JF, Paredes-Rodríguez VM, González-Serrano J, López-Quiles J. The application of diode laser in the treatment of oral soft tissues lesions. A literature review. J Clin Exp Dent. 2017;9:e925–8. doi: 10.4317/jced.53795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahad A, Tandon S, Lamba AK, Faraz F, Anand P, Aleem A. Diode laser assisted excision and low level laser therapy in the management of mucus extravasation cysts: A case series. J Lasers Med Sci. 2017;8:155–9. doi: 10.15171/jlms.2017.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crippa R, Fruili S, Parker S, Angiero F, Benedicenti S, Berne E. Management of intraoral venous malformations using laser-assisted forced dehydration induced photocoagulation. IL Dent Mod. 2013;9:80–97. [Google Scholar]
- 14.Neville BW, Damm DD, Allen M, Bouqot JE, editors. 2nd ed. Philadelphia, PA, USA: Saunders; 2002. Oral and Maxillofacial Pathology. [Google Scholar]
- 15.Re Cecconi D, Achilli A, Tarozzi M, Lodi G, Demarosi F, Sardella A, et al. Mucoceles of the oral cavity: A large case series (1994-2008) and a literature review. Med Oral Patol Oral Cir Bucal. 2010;15:e551–6. doi: 10.4317/medoral.15.e551. [DOI] [PubMed] [Google Scholar]
- 16.Yagüe-García J, España-Tost AJ, Berini-Aytés L, Gay-Escoda C. Treatment of oral mucocele-scalpel versus CO2 laser. Med Oral Patol Oral Cir Bucal. 2009;14:e469–74. [PubMed] [Google Scholar]
- 17.Chawla K, Lamba AK, Faraz F, Tandon S, Arora S, Gupta M. Treatment of lower lip mucocele with Er, Cr: YSGG laser – A case report. J Oral Laser Appl. 2010;10:181–5. [Google Scholar]
- 18.Boj JR, Poirier C, Hernandez M, Espassa E, Espanya A. Review: Laser soft tissue treatments for paediatric dental patients. Eur Arch Paediatr Dent. 2011;12:100–5. doi: 10.1007/BF03262788. [DOI] [PubMed] [Google Scholar]
- 19.Azma E, Safavi N. Diode laser application in soft tissue oral surgery. J Lasers Med Sci. 2013;4:206–11. [PMC free article] [PubMed] [Google Scholar]


