Abstract
Aim:
The aim of the current study was to assess the clinical success of immediate loading implant in the esthetic zone.
Materials and Methods:
20 patients with 20 teeth to get replaced were selected for the study. All patients underwent a pre-surgical preparation followed by draping. Following stringent asepsis, necessary precaution was taken to not to injure the socket wall while removal of tooth. After removal, socket was thoroughly cleaned and curetted with saline and betadine. Using physiodispenser and drills, socket was properly prepared for implant insertion taking care of irrigation with saline to avoid heating of socket while drilling. Implants were then placed with initial stability with hand motion followed by complete insertion with hand ratchet. Black silk sutures were used to close the socket. Patients underwent the first control one week after surgery. They were recalled at the 1st, 3rd and 6th months to evaluate the following parameters to assess the success of immediate implant placement: mobility, soft tissue conditions (gingival index and probing pocket depth (PPD)), and a graded scale ranging from “very satisfied” to “very unsatisfied” were employed to subjectively evaluate patient contentedness.
Results:
During the 1st and 3rd months, 100% mobility was absent. But on the 6th month, the implant of 3 patients (15%) was mobile. The maximum gingival index score was noted in the 1st month (1.02 ± 0.01) and reduced more in the 3rd month (0.74 ± 0.08). The probing depth was more in the 1st month (3.88 ± 0.10) and it was reduced in the 3rd month (3.02 ± 0.12). Significant difference was not found between different times of intervals. 14 patients were very satisfied, 5 patients were fairly satisfied, and 1 was fairly unsatisfied.
Conclusion:
The current study concluded that immediate implant placement in the esthetic zone has a better success rate with good patient acceptance.
KEYWORDS: Aesthetic zone, clinical success extraction sockets, immediate implant
INTRODUCTION
Modern dentistry has witnessed, over the last decades, a rapid and continuing evolution of techniques in different fields. Concerning the implant-rehabilitation protocols, they have been redefined over the years as a result of new knowledge in implant surgery and in order to satisfy patients' increasing expectations in terms of comfort, esthetic, and shorter treatment period.[1]
Loss of teeth involves a physiological remodeling of the alveolar bone with subsequent soft-tissue modification. Bone atrophy are often adequate to 50% when 5–6 months moving principally in the horizontal dimension, predominantly on the buccal aspect, with relation to the vertical dimension, continued slowly, however steady throughout life. Bone resorption could cause a narrower and shorter ridge, thereby compromising the purposeful and esthetic rehabilitation.[2]
Concerning the implant-rehabilitation protocols, many protocols for implant placement have been proposed to overcome this time gap and the associated loss of tissue. These protocols for implant placement include: immediate placement, that is, immediate implant placement in an extraction socket; early placement, that is, early implant placement 4 to 8 weeks after tooth removal; delayed placement, that is, early implant placement (delayed) 12 to 16 weeks after tooth removal; and late placement, that is, late implant placement more than 6 months after extraction.[3] To provide rapid replacement of the tooth, prevent alveolar bone collapse during healing period, shorten treatment protocol, and reduce patient discomfort or inconvenience, immediate implants were introduced as a protocol for implant placement.[4] Hence the present study was conducted to assess the clinical success of immediate loading implant in the esthetic zone.
MATERIALS AND METHODS
Selection of patients
The present study was performed in the department of periodontics, Kalinga institute of Dental Sciences, Bhubaneswar, India. 20 patients with 20 teeth scheduled to be replaced were selected for the study. Inclusion criteria included: presence of a minimum of one poor prognosis anterior tooth (caries, root resorption, endodontic failure); presence of good gingival architecture with surrounding dentition, systemically healthy subjects; presence of at least 4 mm of bone beyond root apex at the sites planned for implant placement; and maintenance of good oral hygiene. Chronic smokers, patients with cardiac pacemakers, patients with bleeding disorders, patients with parafunctional habits such as bruxism were excluded from the study.
Sample size calculation and surgical procedure
The sample size calculation was done by using 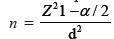 formula. “n” was the required sample size, “z1 – α/2” was a constant; its value for a two-sided test was 1.96 for 95%, “d” was the absolute precision at 20% = 0.2. All patients underwent a pre-surgical preparation followed by draping. Following stringent asepsis, local anesthesia was administered by infiltration employing 2% lignocaine hydrochloride containing 1:200000 adrenaline, which was injected both buccally and on the lingual or palatal side to attain anesthetic effects. After giving anesthesia, atraumatic extraction was done with help of luxators and other instruments. Necessary precaution was taken to not to injure the socket wall while removing the tooth, and avoid excessive force with conservation of gingival margins.
formula. “n” was the required sample size, “z1 – α/2” was a constant; its value for a two-sided test was 1.96 for 95%, “d” was the absolute precision at 20% = 0.2. All patients underwent a pre-surgical preparation followed by draping. Following stringent asepsis, local anesthesia was administered by infiltration employing 2% lignocaine hydrochloride containing 1:200000 adrenaline, which was injected both buccally and on the lingual or palatal side to attain anesthetic effects. After giving anesthesia, atraumatic extraction was done with help of luxators and other instruments. Necessary precaution was taken to not to injure the socket wall while removing the tooth, and avoid excessive force with conservation of gingival margins.
After removal of tooth, socket was thoroughly curetted and cleaned with saline and betadine. Using physiodispenser and drills, socket was properly prepared for implant insertion taking care of irrigation with saline to avoid heating of socket while drilling. Implants were then placed with initial stability with hand motion followed by complete insertion with hand ratchet. Black silk sutures were used to close the socket. Postoperative instruction and medications were given and recalled after one week for suture removal. After implant placement, the provisional restoration was prepared. After four months, with adequate tissue healing and the emergence profile correctly created, the final impression was taken and crown was fixed.
Postoperative phase
In the postoperative phase, the patients were instructed to take an antibiotic regimen for five days and to take analgesics as required. They were also informed to rinse the wound area with 0.2% chlorhexidine, three times a day for the first two weeks, then to brush for the next six weeks with a soft bristle toothbrush. Patients were also asked to take a soft diet and avoid mastication at the newly rehabilitated sites for eight weeks.
Intraoral periapical radiographs (IOPAR) were taken at the site of the inserted implant and patients underwent the first control, one week after surgery. They were recalled in the 1st, 3rd and 6th months to assess the following parameters in order to assess the success of immediate implant placement: mobility (present and absent), soft tissue conditions (gingival index, and probing pocket depth (PPD)), and a graded scale ranging from “very satisfied” to “very unsatisfied,” employed to subjectively evaluate patient contentedness.
Statistical analysis
Data were presented as means ± standard deviation. SPSS software version 20.0 was used to analyze the gathered data. Quantitative data was assessed with t test while Chi-squared test as well as Fischer's exact test were used to analyze qualitative data. A P value lower than 0.05 indicated statistical significance.
RESULTS
Table 1 reveals the evaluation of the implant's mobility at different intervals. In the 1st and 3rd month, 100% mobility was absent, but in the 6th month the implant of 3 patients (15%) was mobile. However, no statistically significant difference was found.
Table 1.
Evaluation of implant mobility at different intervals
| Intervals | Mobility | |||
|---|---|---|---|---|
|
| ||||
| Present | Absent | |||
|
|
|
|||
| No | % | No | % | |
| 1st Month | 0 | 0 | 20 | 100% |
| 3rd Month | 0 | 0 | 20 | 100% |
| 6th Month | 3 | 15% | 17 | 85% |
| Fischer exact test χ2=8.184, P value=0.864 | ||||
Table 2 shows the intra group comparison of gingival index between different time of intervals. The maximum gingival index score was noted in the 1st month (1.02 ± 0.01) and reduced further in the 3rd month (0.74 ± 0.08). There was no significant difference found between different times of intervals.
Table 2.
Intra group comparison of gingival index between different time of intervals
| Different times of Intervals | Mean±SD | t | P |
|---|---|---|---|
| 1st Month | 1.02±0.01 | 9.256 | 0.348 |
| 3rd Month | 0.74±0.08 | ||
| 6th Month | 0.82±0.06 |
The probing depth was more in the 1st month (3.88 ± 0.10) and reduced in the 3rd month (3.02 ± 0.12). No significant difference was found between different times of intervals [Table 3].
Table 3.
Intra group comparison of probing depth between different time intervals
| Different times of Intervals | Mean±SD | t | P |
|---|---|---|---|
| 1st Month | 3.88±0.10 | 10.190 | 0.819 |
| 3rd Month | 3.02±0.12 | ||
| 6th Month | 3.46±0.16 |
Overall patient satisfaction was assessed in Table 4. 14 patients were very satisfied, 5 patients were fairly satisfied, and 1 was fairly unsatisfied.
Table 4.
Assessment of overall patient satisfaction
| Patient satisfaction level | ||||
|---|---|---|---|---|
|
| ||||
| Very satisfied | Fairly satisfied | Fairly unsatisfied | Very unsatisfied | |
| Immediate implant placement | 14 | 5 | 1 | 0 |
χ2=2.814, P=0.664
DISCUSSION
In recent times, there has been a tremendous change in the treatment modalities and outlook used in dentistry. Dental implants are to this day considered to be a major advance in the relief of misplaced and missing teeth, as it has a huge number of benefits. The timing of implant placement after tooth removal has been a matter of discussion in dental implant treatment. 12 months of waiting period or more than that to allow socket healing has been the gold standard protocol. Various alternatives to this approach may be considered in order to reduce the waiting time.[5]
Different authors have tried to improve this bone implant contact so as to improve the long-term prognosis of implant therapy by way of constantly changing the nature of various implant surfaces, and have achieved variable success with each of these modifications. Immediate loading of implant is taught with its own risks. The initial healing time is very important for the success of the implant and one of the very important factors to be considered is the bone implant contact during this period.[6]
In the present study, clinical mobility of the implant was evaluated. Except for 3 implants (15%) which endured mobility of Grade 1 at 6th month of follow-up, no mobility was endured by any of the implants at all the three follow-up visits that were listed in the 1st, 3rd, and 6th months. Micro movements of the implant was found because of subject has applied forces on the implant system in the early healing time. The presence of micro movements at the interface between bone and implant can, in fact, affect the bone healing period and osseointegration, leading to a slight rallying of the implant.[7]
Sekine H et al.[8] mentioned that the movement of healthy implant should be lower than 75 micrometers and that it is considered as zero clinical mobility. A study by Winkler S et al.[9] stated that the presence of connective tissue between the implant and bone was considered as clinical failure for an endosteal root-form implant.
Though, all studies demonstrated that immediate implant placement into infected extraction sockets can be successful, (provided that proper antiseptic protocols are followed), the literature also suggests that there are factors such as primary stability at the time of implant placement, implant positioning, socket anatomy, soft tissue morphology, tooth position, implant system used, and administration of antiseptic protocols which could change the predictability of success of immediate placement of implants into infected extraction sockets.[10]
CONCLUSION
The current study concluded that immediate implant placement in the esthetic zone has a better success rate with good patient acceptance.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tettamanti L, Andrisani C, Bassi MA, Vinci R, Silvestre-Rangil J, Tagliabue A. Immediate loading implants: Review of the critical aspects. Oral Implantol (Rome) 2017;10:129–39. doi: 10.11138/orl/2017.10.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ariano V, Mancini M, Cardi A, Condò R, Cerroni L, Pasquantonio G. Immediate nonfunctional loading of two single-maxillary postextractive implants: 6-year postloading results of two case reports. Case Rep Dent. 2016;2016:6816907. doi: 10.1155/2016/6816907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hammerle CH, Chen ST, Wilson TG., Jr Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants. 2004;19:272–8. [PubMed] [Google Scholar]
- 4.Kaur J, Chahal GS, Grover V, Bansal D, Jain A. Immediate implant placement in periodontally infected sites- A systematic review and meta-analysis. J Int Acad Periodontol. 2021;23:115–37. [PubMed] [Google Scholar]
- 5.Diwakar D, Ebenezer V. Comparative analysis of peri-implant bone levels in immediate and delayed implants – A retrospective study. Int J Curr Res. 2021;13:16918–22. [Google Scholar]
- 6.Anand U, Mehta DS. Evaluation of immediately loaded dental implants bioactivated with platelet-rich plasma placed in the mandibular posterior region: A clinico-radiographic study. J Indian Soc Periodontol. 2012;16:89–95. doi: 10.4103/0972-124X.94612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sathe S, Gufran K, Hamza MO, Gowdar IM, Elqomsan MA, Mirza MB. Success of immediate implants in anterior esthetic zone: One year prospective study. World J Dent. 2018;9:451–6. [Google Scholar]
- 8.Sekine H, Komiyama Y, Hotta H, Yoshida K. “Van Steenberghe”. Amsterdam: Elservier; 1986. Mobility characteristics and tactile sensitivity of osseointegrated fixture-supporting systems. Tissue integration in oral maxillofacial reconstruction; pp. 326–32. [Google Scholar]
- 9.Winkler S, Morris HF, Spray JR. Stability of implants and natural teeth as determined by the Perio test over 60 months of function. J Oral Implantol. 2001;27:198–203. doi: 10.1563/1548-1336(2001)027<0198:SOIANT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Marconcini S, Barone A, Gelpi F, Briguglio F, Covani U. Immediate implant placement in infected sites: A case series. J Periodontol. 2013;84:196–202. doi: 10.1902/jop.2012.110279. [DOI] [PubMed] [Google Scholar]


