OBJECTIVES:
To determine the association of prior use of renin-angiotensin-aldosterone system inhibitors (RAASIs) with mortality and outcomes in hospitalized patients with COVID-19.
DESIGN:
Retrospective observational study.
SETTING:
Multicenter, international COVID-19 registry.
Subjects:
Adult hospitalized COVID-19 patients on antihypertensive agents (AHAs) prior to admission, admitted from March 31, 2020, to March 10, 2021.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
Data were compared between three groups: patients on RAASIs only, other AHAs only, and those on both medications. Multivariable logistic and linear regressions were performed after controlling for prehospitalization characteristics to estimate the effect of RAASIs on mortality and other outcomes during hospitalization. Of 26,652 patients, 7,975 patients were on AHAs prior to hospitalization. Of these, 1,542 patients (19.3%) were on RAASIs only, 3,765 patients (47.2%) were on other AHAs only, and 2,668 (33.5%) patients were on both medications. Compared with those taking other AHAs only, patients on RAASIs only were younger (mean age 63.3 vs 66.9 yr; p < 0.0001), more often male (58.2% vs 52.4%; p = 0.0001) and more often White (55.1% vs 47.2%; p < 0.0001). After adjusting for age, gender, race, location, and comorbidities, patients on combination of RAASIs and other AHAs had higher in-hospital mortality than those on RAASIs only (odds ratio [OR] = 1.28; 95% CI [1.19–1.38]; p < 0.0001) and higher mortality than those on other AHAs only (OR = 1.09; 95% CI [1.03–1.15]; p = 0.0017). Patients on RAASIs only had lower mortality than those on other AHAs only (OR = 0.87; 95% CI [0.81–0.94]; p = 0.0003). Patients on ACEIs only had higher mortality compared with those on ARBs only (OR = 1.37; 95% CI [1.20–1.56]; p < 0.0001).
CONCLUSIONS:
Among patients hospitalized for COVID-19 who were taking AHAs, prior use of a combination of RAASIs and other AHAs was associated with higher in-hospital mortality than the use of RAASIs alone. When compared with ARBs, ACEIs were associated with significantly higher mortality in hospitalized COVID-19 patients.
Keywords: antihypertensive agents, COVID-19, mortality, outcome, renin-angiotensin-aldosterone system inhibitors
Over the course of the pandemic caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), there have been numerous triumphs for the scientific community as well as a surplus of misinformation released to the public with potentially life-threatening implications. In the early stages of the pandemic, research showed that SARS-CoV-2 invades the host cells through the receptor angiotensin-converting enzyme (ACE)–2. This well-known enzyme is highly expressed in the vascular endothelium and the lungs, particularly in endothelial and type 2 alveolar epithelial cells (1). Common medications used to treat hypertension, ACE inhibitors (ACEIs), and angiotensin receptor blockers (ARBs) that are collectively known as renin-angiotensin-aldosterone system inhibitors (RAASIs) came into question as experimental studies with animal models showed these medications up-regulate ACE-2 expression leading to increased risk of severe illness (2).
Research suggests that the use of ACEIs and ARBs does not increase the risk of COVID-19, instead, comorbidities such as hypertension, obesity, diabetes mellitus (DM), and cardiovascular disease are risk factors for severe COVID-19 (3, 4). Recent literature does not show increased risk of COVID-19 or hospital outcomes with use of these medications (5, 6). Lopes et al (7) reported that in hospitalized patients with COVID-19, discontinuation of RAASIs did not affect the number of days alive and out of the hospital. Another study showed that discontinuation of RAASIs in patients with COVID-19 may lead to faster and better recovery (8). Additional research has shown that the interaction between SARS-CoV-2 and ACE-2 can lead to dysregulation of RAAS which results in an accumulation of angiotensin II and can have potentially negative effects, such as inflammation, coagulation, and fibrosis (9). Therefore, the use of RAASIs could potentially decrease angiotensin II proinflammatory effects and be beneficial in patients infected with COVID-19. A prospective cohort study by Hippisley-Cox reported reduced risk of COVID-19 in patients receiving RAASIs (10).
With this contrasting evidence, it remains unclear whether use of RAASIs affects the outcomes of hospitalized patients with COVID-19. Society of Critical Care Medicine (SCCM) Discovery Viral Infection and Respiratory Illness Universal Study (VIRUS) COVID-19 Registry is a multicenter, international registry developed by SCCM’s Discovery network (11). The aim of this study was to determine the effect of prior use of RAASIs on outcomes of patients hospitalized with laboratory-confirmed SARS-CoV-2 infection included in the VIRUS: COVID-19 Registry database.
MATERIALS AND METHODS
Design, Setting, and Study Population
This is a retrospective observational study of adult patients hospitalized with laboratory-confirmed SARS-CoV-2 infection included in the VIRUS: COVID-19 Registry database (11) from 181 sites in 19 countries between March 31, 2020, and March 10, 2021. A confirmed case of COVID-19 was defined by a positive result on a reverse-transcriptase–polymerase chain reaction assay. For patients with multiple hospital admissions for COVID-19, only the first hospital admission was included in this analysis. Patients under the age of 18 years, those with no recorded discharge status, and those without research authorization to access medical records were excluded. Patients who were not admitted for COVID-19 but were incidentally found to be positive for SARS-CoV-2 were also excluded. Patients on any antihypertensive agents (AHAs) prior to admission were included in the analysis. Patients were followed until hospital discharge or death.
Data Collection
Extensive data were collected by the registry for each patient; however, only a subset was requested for this analysis. Demographic data requested included age, gender, race, and geographical location. Clinical data requested included admission diagnosis, location of initial admission, comorbidities, other prehospitalization medications, smoking status, and Acute Physiology and Chronic Health Evaluation (APACHE) II scores. Outcome data included in-hospital mortality, admission to ICU, hospital and ICU length of stay (LOS), development of complications (e.g., respiratory failure, septic shock, congestive heart failure, etc.), need for organ support therapy such as mechanical ventilation, continuous renal replacement therapy (CRRT), hemodialysis, and extracorporeal membrane oxygenation (ECMO). Patients who were missing data on prehospitalization medications, comorbidities, admission diagnosis, or outcomes were excluded.
The patients were divided into three groups according to the AHAs they were taking prior to admission: 1) patients on RAASIs only, 2) patients on other AHAs only, and 3) patients on both medication classes together. The RAASIs only group included patients on ACEIs and/or ARBs. Other AHAs included non-RAASI medications such as beta blockers, calcium channel blockers, and diuretics. These groups were compared to eliminate many strong sources of bias including prevalent user bias, confounding by hypertension, and age.
Outcome Measures
The primary outcome was in-hospital mortality. Secondary outcomes included hospital and ICU LOS, development of complications, and need for organ support therapy.
Data Management
Study data were recorded and managed using the Mayo Clinic Research Electronic Data Capture (REDCap) system (12). The study was approved by the Mayo Clinic Institutional Review Board (no. 20-002610). The study is registered on ClinicalTrials.gov: NCT04323787. Each study site obtained approval from their local review board with a waiver of informed consent and signed a data use agreement before being granted permission to enter deidentified data from their medical records into the registry.
Statistical Analysis
Group statistics are expressed as mean ± sd for continuous measures (e.g., age, LOS) or as number (percentage) for categorical measures (e.g., race, prevalence of comorbidities). Group characteristics were compared using chi-square test for categorical variables and t test or Wilcoxon rank test for continuous variables depending on normality of sample distributions. Appropriateness of assumption of normal distributions for the continuous measures was confirmed by D’Agostino-Pearson omnibus normality test. Multivariable logistic and linear regressions were performed to evaluate the association of RAASIs with mortality and other outcomes during hospitalization after adjusting for other factors: age, gender, race, location (United States vs non-United States), and comorbidities (chronic kidney disease [CKD], chronic pulmonary disease [CPD], congestive heart failure [CHF], DM, hypertension, asthma, coronary artery disease, and cardiac arrhythmia). Cox proportional hazard regression was used to compare the survival curves between the three groups with right censoring of time to event at discharge from hospital. A secondary comparison was made between patients on ACEIs only versus ARBs only. Statistical analysis was performed using R statistical software (R Version 4.0.3 [2020; R Core Team, Vienna, Austria] using packages tidyverse 1.3.1 and survival 3.2-7). A p value of less than 0.05 was considered statistically significant for comparing demographics and primary outcome. For the secondary outcomes (n = 15)‚ p < 0.0033 was considered statistically significant after using Bonferroni correction (p = 0.05/15 = 0.0033).
RESULTS
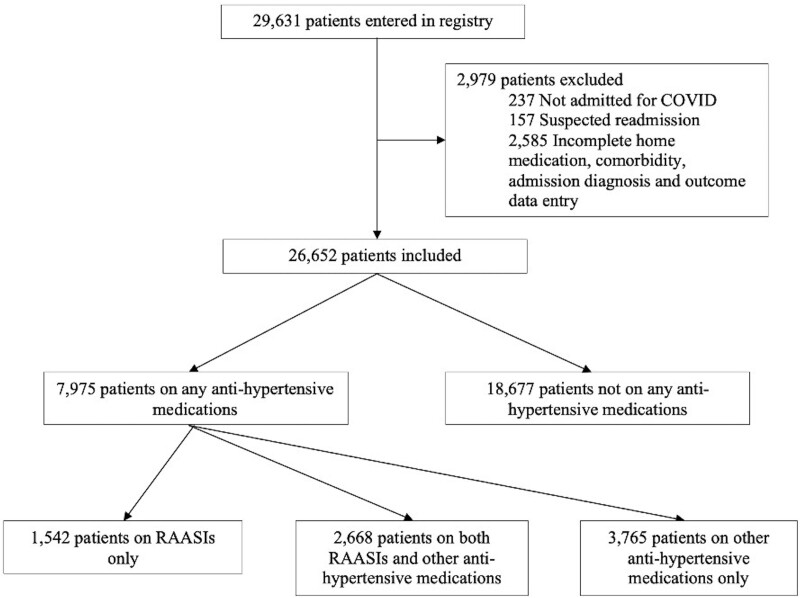
A total of 29,631 patients were entered into the registry. Two thousand nine hundred seventy-nine patients were excluded from the study as shown in Figure 1. Of 26,652 patients, 7,975 patients were on AHAs. Of these, 1,542 patients (19.3%) were on RAASIs only and 3,765 patients (47.2%) were on other AHAs only prior to hospitalization, whereas the remainder were on both of these medications (Fig. 1). For both 26,652 and 7,975 patients, less than 1% of data were missing for age, gender, race, mortality, and hospital LOS. For most of the remaining variables, estimating the percentage of missing data cannot be done directly because of how the data were entered into the REDCap.
Figure 1.
Flow chart of patients in each group after applying exclusion and inclusion criteria.
Demographic and clinical characteristics of patients with SARS-CoV-2 infection at admission are given in Table 1 (Supplemental Digital Content, http://links.lww.com/CCM/H154), grouped by use of RAASI only, RAASIs and other AHAs, and other AHAs only. Compared with patients on both medications and those on other AHAs only, patients on RAASIs only were younger (mean age 63.3 vs 67.4 yr in combined RAASIs and other AHAs group and 66.9 yr in other AHAs only group; p < 0.0001), were more often male (58.2% vs 55.9% in combined RAASIs and other AHAs group and 52.4% in other AHAs only group; p = 0.0002), and were more often White (55.1% vs 50.0% in combined RAASIs and other AHAs group and 47.2% in other AHAs only group, p < 0.0001). Patients on RAASIs were more likely to be admitted with diagnosis of acute respiratory distress syndrome (ARDS) (10.2% vs 7.5% in combined RAASIs and other AHAs group and 7.9% in other AHAs only group, p = 0.0043), whereas patients on both RAASIs and other AHAs were more likely to have admission diagnosis of acute hypoxic respiratory failure (non-ARDS), acute renal failure/injury, bacterial pneumonia, cardiac arrhythmia/failure, or shock. Even though patients in all groups were on one or more AHAs (RAASIs or others), only 85.4% of patients had a diagnosis of hypertension at admission. Hypertension, DM, obesity, and CHF were more prevalent in patients on combination of RAASIs and other AHAs. Other comorbidities including asthma, CKD, and CPD were significantly higher in the other AHAs only group. There was no difference in the prevalence of smoking between the groups. Mean APACHE II scores were significantly higher in group on both RAASIs and other AHAs (19 vs 16 in RAASIs only group and 18.6 in other AHAs only; p = 0.010); however, APACHE II score data were only available for 651 (8.2%) patients.
Group statistics for the outcomes is shown in Table 1 for all three groups. Table 2 (Supplemental Digital Content, http://links.lww.com/CCM/H155) shows the comparison of outcomes between these three groups after adjusting for demographics and prehospital comorbidities. Multivariable logistic (for categorical outcomes) or linear (for continuous outcomes) regression models were fit to estimate whether there was a significant effect of RAASIs on outcomes after adjusting for demographics (age, gender, race, and geographical location) and prehospitalization comorbidities (CHF, CPD, CKD, DM, hypertension, asthma, coronary artery disease, and cardiac arrhythmia). Patients on combination of RAASIs and other AHAs had higher in-hospital mortality than those on RAASIs only (odds ratio [OR] = 1.28; 95% CI [1.19–1.38]; p < 0.0001) and higher mortality than those on other AHAs only (OR = 1.09; 95% CI [1.03–1.15]; p = 0.0017). Patients on RAASIs only had significantly lower mortality than those on other AHAs only (OR = 0.87; 95% CI [0.81–0.94]; p = 0.0003). For the secondary outcomes, there was no difference, after adjustment, in the use of CRRT/hemodialysis, admission to ICU, hospital LOS, use of mechanical ventilation or development of complications including respiratory failure, septic shock, CHF, cardiac arrhythmia, stroke, and secondary infections between the groups. ICU LOS was significantly shorter in patients on combination of RAASIs and other AHAs when compared with those on RAASIs only (β = –2.1; 95% CI [–2.9 to –1.3]; p < 0.0001). Table 3 (Supplemental Digital Content, http://links.lww.com/CCM/H156) lists all complications during hospitalization for which the registry gathered data, comparing patients on RAASIs only, RAASIs and other AHAs, and other AHAs only, after adjusting for patient demographics. Patients on combined RAASIs and other AHAs had higher odds of developing acute kidney injury during hospitalization when compared with those on RAASIs only (OR = 1.40; 95% CI [1.19–1.66]; p < 0.0001). Even though there were no differences in odds of developing other major complications between the groups, patients on combined medications had lower odds of not having complications compared with those on RAASIs only (OR = 0.74; 95% CI [0.64–0.86]; p < 0.0001).
TABLE 1.
Group Statistics for Outcomes of Patients on Renin-Angiotensin-Aldosterone System Inhibitors Only, Renin-Angiotensin-Aldosterone System Inhibitors and Other Antihypertensive Agents and Other Antihypertensive Agents Only
| Outcomes | RAASIs Only (N = 1,542) | RAASIs and Other AHAs (N = 2,668) | Other AHAs Only (N = 3,765) | p | |||
|---|---|---|---|---|---|---|---|
| Analysis of Variance | RAASIs Only vs Both Medications | Both Medications vs Other AHAs Only | RAASIs vs Other AHAs Only | ||||
| In-hospital mortality, n (%) | 286 (18.5) | 640 (24.0) | 884 (23.5) | < 0.0001 | < 0.0001 | 0.66 | < 0.0001 |
| Use of CRRT/hemodialysis, n (%) | 66 (4.2) | 207 (7.5) | 230 (5.9) | < 0.0001 | < 0.0001 | 0.013 | 0.012 |
| Time on CRRT (d), mean ± sd | 10.0 ± 9.3 | 9.4 ± 10.1 | 10.7 ± 11.5 | 0.42 | 0.63 | 0.20 | 0.60 |
| Use of extracorporeal membrane oxygenation, n (%) | 19 (1.2) | 24 (0.9) | 27 (0.7) | 0.19 | 0.38 | 0.50 | 0.094 |
| Admitted to ICU, n (%) | 713 (46.4) | 1,241 (47.1) | 1,669 (46.9) | 0.92 | 0.71 | 0.93 | 0.77 |
| ICU length of stay (d), mean ± sd | 14.3 ± 15.3 | 12.7 ± 12.8 | 12.0 ± 12.7 | < 0.0001 | < 0.0001 | 0.0003 | < 0.0001 |
| Hospital length of stay (d), mean ± sd | 15.9 ± 19.7 | 15.1 ± 14.3 | 15.0 ± 16.7 | 0.0011 | 0.0027 | 0.56 | 0.0007 |
| Use of mechanical ventilation, n (%) | 424 (27.5) | 786 (29.5) | 1,004 (26.7) | 0.046 | 0.19 | 0.015 | 0.56 |
| Time on ventilator (d), mean ± sd | 14.9 ± 14.8 | 13.1 ± 12.1 | 13.2 ± 14.9 | 0.072 | 0.024 | 0.87 | 0.052 |
| Complications during hospitalization, n (%) | |||||||
| Respiratory failure (acute respiratory distress syndrome) | 320 (20.8) | 576 (21.6) | 729 (19.4) | 0.085 | 0.55 | 0.031 | 0.26 |
| Mild (P:F 200–300) | 21 (8.1) | 60 (12.5) | 62 (10.5) | 0.31 | 0.10 | 0.60 | 0.32 |
| Moderate (P:F 100–199) | 73 (28.1) | 146 (30.4) | 181 (30.7) | ||||
| Severe (P:F < 100) | 166 (63.8) | 275 (57.2) | 347 (58.8) | ||||
| Septic shock | 170 (11.0) | 355 (13.3) | 435 (11.6) | 0.041 | 0.035 | 0.038 | 0.61 |
| Congestive heart failure | 24 (1.6) | 93 (3.5) | 116 (3.1) | 0.0012 | 0.0004 | 0.41 | 0.0023 |
| Cardiac arrhythmia | 78 (5.1) | 202 (7.6) | 232 (6.2) | 0.0040 | 0.0020 | 0.030 | 0.14 |
| Stroke | 15 (1.0) | 47 (1.8) | 39 (1.0) | 0.019 | 0.056 | 0.017 | 0.95 |
| Co- or secondary infection | 66 (4.3) | 139 (5.2) | 156 (4.1) | 0.11 | 0.20 | 0.051 | 0.88 |
AHAs = antihypertensive agents, CRRT = continuous renal replacement therapy, P:F = Pao2:Fio2 ratio, RAASIs = renin-angiotensin-aldosterone system inhibitors.
Boldface values indicate statistical significance.
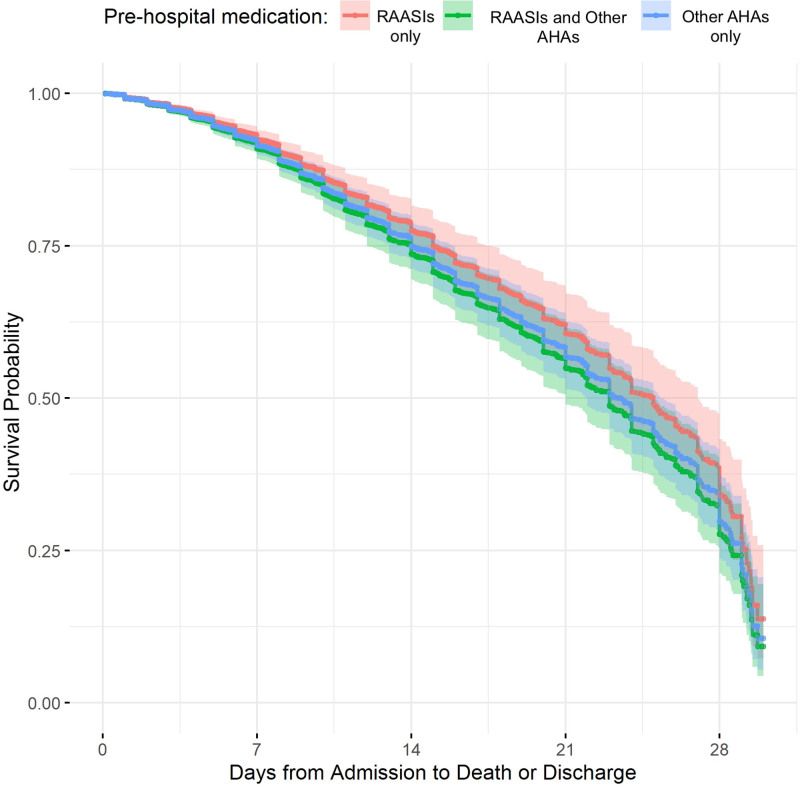
Cox proportional hazard regression analysis was used to compare the survival curves between the three groups (Fig. 2) while adjusting for age, gender, race, and comorbidities: CHF, CPD, CKD, DM, hypertension, asthma, coronary artery disease, and cardiac arrhythmia. When comparing all three groups, we did not find a significant difference in the in-hospital mortality (p = 0.073). On pairwise Cox proportional hazard analysis, combined use of RAASIs and other AHAs, compared with use of RAASIs alone, was associated with a significantly higher in-hospital mortality and shorter survival times (p = 0.023). When compared with RAASIs only, use of other AHAs only was associated with significantly higher mortality (p = 0.021). There was no difference in mortality when comparing use of AHAs only versus combined use of RAASIs and other AHAs (p = 0.97).
Figure 2.
Cox proportional-hazards model comparing survival probability of patients on renin-angiotensin-aldosterone system inhibitors (RAASIs) only, RAASIs and other antihypertensive agents (AHAs) and other AHAs only. Survival time is from hospital admission to death; if the patient did not die, then survival time is right censored at time of discharge from hospital.
Secondary analysis was performed to compare group statistics and outcomes for patients on ACEIs only versus ARBs only (Table 4 [Supplemental Digital Content, http://links.lww.com/CCM/H157], Table 5 [Supplemental Digital Content, http://links.lww.com/CCM/H158], and Table 6 [Supplemental Digital Content, http://links.lww.com/CCM/H159], respectively). Of the 1,517 patients on a single RAASI agent, 958 patients (63.2%) were on ACEIs only, whereas 559 patients (36.8%) were on ARBs only. Compared with patients on ARBs only, patients on ACEIs only were significantly younger (mean age 62.6 vs 64.4 yr; p = 0.012), more likely to be male (61.3% vs 53.1%; p = 0.0021), and more often White (56.4% vs 53.5%; p = 0.010). Compared with those on ARBs only, patients on ACEIs only had higher prevalence of DM (56.5% in ACEIs vs 45.3% in ARBs group; p < 0.0001) and lower prevalence of hypertension (86.2% in ACEIs vs 92.1% in ARBs group; p = 0.0007) and asthma (6.3% in ACEIs vs 10.0% in ARBs group; p = 0.011). There were no differences in admission diagnoses or APACHE II scores in both the groups. On comparing the outcomes, patients on ACEIs only had significantly higher in-hospital mortality compared with those on ARBs only (OR = 1.37; 95% CI [1.20–1.56]; p < 0.0001). Patients on ACEIs only also had significantly longer hospital LOS compared with ARBs only group (β = 2.9; 95% CI [1.9–3.8]; p < 0.0001). For the secondary outcomes, there was no difference, after adjustment, in the use of CRRT/hemodialysis, time on CRRT, admission to ICU, ICU LOS, use of mechanical ventilation, time on ventilator, or development of complications between the two groups. Table 7 (Supplemental Digital Content, http://links.lww.com/CCM/H160) lists all complications during hospitalization for which the registry gathered data, comparing patients on ACEIs only and ARBs only, after adjusting for patient demographics.
DISCUSSION
Our study suggests that hospitalized patients on RAASIs prior to COVID-19 are at lower risk of mortality during hospitalization when compared with patients who were on other AHAs only prior to admission. Furthermore, mortality risk was also significantly increased for patients on both RAASIs and other AHAs prior to hospitalization compared with those on RAASIs only. To our knowledge, this is the first international study looking at the impact of combined use of RAASIs and other AHAs on mortality in hospitalized COVID-19 patients.
Recently, many studies have shown that RAASIs are not associated with increased risk of having COVID-19 (4, 10). A study by Khera et al (13) showed 40% lower rate of hospitalization in COVID-19 patients using RAASIs. However, for patients who are already hospitalized with COVID-19, there are contradictory data for association of RAASI use prior to hospitalization and mortality. A recent study by Ip et al (14) has shown no association between mortality and use of RAASIs in patients with COVID-19. A systematic review looking at association of mortality with ACEIs use in patients with COVID-19 showed increased mortality in ACEI group in some settings, whereas these findings were not seen in other settings (15). Another study by Bauer et al (8) showed that discontinuation of RAASIs in COVID-19 was associated with faster and better recovery. However, these studies varied with respect to patient ages and mortality and were restricted to one geographical region.
A single-center study conducted in Italy reported lower mortality in patients on RAASIs compared with other AHAs with OR equals to 0.56; however, it did not reach statistical significance, possibly due to their small sample size (16). A meta-analysis by Zhang et al (17) among COVID-19 patients with hypertension also reported a protective effect of the use of RAASIs against mortality, severity/mortality, hospitalization, and rate of transfer to ICU compared with those on non-RAASI AHAs. Some of the other recent systematic reviews and meta-analyses also showed lower mortality in hypertensive patients on RAASIs compared with those on other or no treatment (18–21). However, these studies did not account for whether patients in the RAASI groups were on RAASI only or they were on other AHAs as well. Our study shows lower risk of in-hospital mortality in patients taking only RAASIs prior to admission compared with those who were taking a combination of RAASIs and other AHAs or other AHAs only. Our study results are consistent with another study by Yuan et al (22) that reported that hypertensive COVID-19 patients on RAASIs had a lower risk of mortality, while patients on beta blockers, calcium channel blockers, and diuretics did not show any significant difference when compared with patients with uncontrolled blood pressure. Contradictory to the above studies, we did not notice any association between use of RAASIs and risk of ICU admission in our study. Even though the risk of in-hospital mortality for patients on RAASIs only was lower compared with patients on combination of RAASIs and other AHAs, they had longer ICU LOS. Competing risk of death might have shortened ICU LOS in patients on both RAASIs and other AHAs.
We believe that this higher in-hospital mortality with combined use of RAASIs and other AHAs prior to hospitalization is an interesting and novel finding. As shown in Table 1 (Supplemental Digital Content, http://links.lww.com/CCM/H154), these patients represent a higher comorbid group especially compared with patients on RAASIs only; however, they maintained an independent association with in-hospital mortality even after controlling for these prehospital comorbidities (Table 2, Supplemental Digital Content, http://links.lww.com/CCM/H155). It is possible that patients on both medications may have presented sicker to the hospital. Given that APACHE II scores were only available for about 8.2% patients included in the study, it is difficult to make an interpretation from these data. Another hypothesis is that the combination of different medications with RAASIs like beta blockers, calcium channel blockers, or diuretics may have inadvertent side effects in patients especially when they are sick. For example, the combination of medications could have hindered heart rate response in COVID-19 or altered pulmonary shunt and thus oxygenation requirements. However, most published literature shows that combination therapy for hypertension is not only more effective in controlling blood pressure but also has fewer side effects due to lower doses of medications required to control blood pressure compared with higher dose monotherapy (23). Besides, the rate of most complications and use of organ support therapy was similar across all the groups which makes this hypothesis less likely. We also noticed that patients on combined RAASIs and other AHAs had significantly higher mortality than those on other AHAs only on logistic regression analysis (Table 2, Supplemental Digital Content, http://links.lww.com/CCM/H155). However, there was no difference in mortality between the two groups on Cox proportional hazard regression analysis. It is possible that other AHAs (even in combination with RAASIs) took away the protective effect of RAASIs.
With respect to RAASIs, ACEIs and ARBs have different mechanisms in the pathogenesis of COVID-19 (24). Therefore, we decided to compare the outcomes of patients on ACEIs versus ARBs prior to hospitalization as our secondary analysis. Most published literature compared patients on ACEIs and/or ARBs with nonusers. However, there are paucity of data on comparison of these two classes of RAASIs and association with mortality. A study by Derington et al (25) evaluated association of mortality among inpatients and outpatients on ARBs versus ACEIs. This study did not find a significant association between ARB or ACEI use and all-cause mortality in inpatients with COVID-19, whereas a significantly lower risk of all-cause hospitalization or mortality was seen among ARB users compared with ACEI users in outpatients. We found a significantly higher mortality in patients on ACEIs compared with those on ARBs in hospitalized COVID-19 patients.
This study has limitations inherent to retrospective registry analyses. A complete case analysis such as ours assumes data are missing completely at random (26). The VIRUS: COVID-19 Registry employs extensive data missingness review and cross-validation process to detect any errors (27). However, there is still a possibility of data entry errors. Patients with incidentally positive SARS-CoV-2 PCR on hospitalization were excluded from the registry. However, the distinction of incidental diagnosis versus an admission for illness due to SARS-CoV-2 was made by the site investigators. Due to the evolving understanding of the varied COVID-19 presentations, this may have resulted in slight over- and/or under-inclusion of patients. Our study included all patients on AHAs prior to hospitalization irrespective of the indication of medication use. However, we have controlled for the most common indications in the multivariable regression model to prevent bias. Since it is a retrospective database study, we could not account for compliance of the patients with these medications and for patients whose home antihypertensive medications were discontinued during hospitalization. It was also unknown how long the patients had been on these medications prior to hospitalization. Lastly‚ given the observational nature of the analysis and the uncertain mechanisms of causal influence, there is a considerable risk of residual confounding.
CONCLUSIONS
In this multicenter observational study, patients on both RAASIs and other AHAs prior to admission had higher in-hospital mortality than patients on RAASIs only. When compared with ARBs, ACEIs were associated with significantly higher mortality in hospitalized COVID-19 patients. These findings may help in early identification of patients who are at higher risk of morbidity and mortality from COVID-19.
ACKNOWLEDGMENT
We would like to thank the VIRUS: COVID-19 Registry and the collaborative co‐authors listed in Appendix 1 for providing and maintaining the database of hospitalized COVID‐19 patients which made this study possible. We are grateful to the Society of Critical Care Medicine colleagues for their internal review and feedback on this study.
Supplementary Material
APPENDIX 1. LIST OF SOCIETY OF CRITICAL CARE MEDICINE DISCOVERY VIRAL INFECTION AND RESPIRATORY ILLNESS UNIVERSAL STUDY (VIRUS): COVID-19 REGISTRY INVESTIGATOR GROUP
Belgium: Centre Hospitalier Jolimont: Jean-Baptiste Mesland, Pierre Henin, Hélène Petre, Isabelle Buelens, Anne-Catherine Gerard; The Brugmann University hospital, Bruxelles: Philippe Clevenbergh. Bolvia: Clinica Los Olivos: Rolando Claure-Del Granado, Jose A. Mercado, Esdenka Vega-Terrazas, Maria F. Iturricha-Caceres. Canada: Mackenzie Health, Richmond Hill: Ruben Garza, Eric Chu, Victoria Chan. Columbia: Clinica Medical SAS: Oscar Y. Gavidia, Felipe Pachon, Yeimy A. Sanchez. Croatia: Clinical Hospital Center Rijeka, Rijeka, Croatia: Danijel knežević. Egypt: Helwan University: Mohamed El Kassas, Mohamed Badr, Ahmed Tawheed, Ahmed Tawheed, Hend Yahia. Greece: ICU University Hospital of Ioannina: Dimitrios Kantas, Vasileios Koulouras. Hondurus: CEMESA Hospital: Estela Pineda; Honduras Medical Center: Gabina María Reyes Guillen, Helin Archaga Soto, Ana Karen Vallecillo Lizardo. Hungary: Uzsoki Teaching Hospital: Csaba Kopitkó, Agnes Bencze, István Méhész, Zsófia Gerendai. India: ACSR Govt. Medical College and Hospital: Phaneendra Doddaga, Neethi Chandra; Bangalore Medical College and Research Institute: Smitha S. Segu, Tuhin Chakraborty, Epcebha Joyce; BSES MG Hospital, Mumbai: Girish Vadgaonkar, Rekha Ediga, Shilpa Basety, Shwetha Dammareddy, Phani Sreeharsha Kasumalla; Gandhi Medical College and Hospital, Hyderabad: Umamaheswara Raju, Janaki Manduva, Naresh Kolakani, Shreeja Sripathi, Sheetal Chaitanya; Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry: Anusha Cherian, Sreejith Parameswaran, Magesh Parthiban, Menu Priya A.; KLEs Dr. Prabhakar Kore Hospital: Madhav Prabhu, Vishal Jakati; Mahatma Gandhi Hospital, Jaipur: Puneet Rijhwani, Ashish Jain, Aviral Gupta, Ram Mohan Jaiswal, Ambika Tyagi, Nimish Mathur; Maulana Azad Medical College and Lok Nayak hospital: Mradul Kumar Daga, Munisha Agarwal, Ishan Rohtagi; Medicover Hospitals: Sridhar Papani, Mahesh Kamuram; Om Superspeciality Hospital, Raipur: Kamlesh Kumar Agrawal, Vijendra Baghel, Kirti Kumar Patel; Panimalar Medical College Hospital & Research Institute: Surapaneni Krishna Mohan, Ekambaram Jyothisree; Tristar Hospital: Mukur Petrolwala, Bharat Ladva. Iran: Labbafinejad Medical Center, Shahid Beheshti University of Medical Sciences, Tehran: Nooshin Dalili, Mohsen Nafa. Japan: Center Hospital of the National Center for Global Health and Medicine: Wataru Matsuda, Reina Suzuki; Hiroshima University: Michihito Kyo; Hokkaido University Hospital, Sapporo: Shu Tahara, Mineji Hayakawa, Kunihiko Maekawa; Jichi Medical University Saitama Medical Center: Reina Suzuki, Masamitsu Sanui, Sho Horikita; Sapporo City General Hospital: Yuki Itagaki, Akira Kodate, Reina Suzuki, Akira Kodate, Yuki Takahashi, Koyo Moriki; Tohoku university hospital, Sendai: Takuya Shiga, Yudai Iwasaki; Tokyo Medical and Dental University: Hidenobu Shigemitsu, Yuka Mishima, Nobuyuki Nosaka, Michio Nagashima.Kuwait: Al-Amiri and Jaber Al-Ahmed Hospitals, Kuwait Extracorporeal Life Support Program: Abdulrahman Al-Fares. Mexico: Centenario Hospital Miguel Hidalgo, Aguascalientes: Mariana Janeth Hermosillo Ulloa; Hospital Universitario, Universidad Autonoma de Nuevo León: Rene Rodriguez-Gutierrez, Jose Gerardo Gonzalez- Gonzalez, Alejandro Salcido-Montenegro, Adrian Camacho-Ortiz. Nigeria: Aminu Kano Teaching Hospital/Bayero University, Kano: Fatimah Hassan- Hanga, Hadiza Galadanci, Abubakar Shehu Gezawa, Halima M. S. Kabara, Taiwo Gboluwaga Amole, Halima Kabir, Dalha Gwarzo Haliru, Abdullahi S. Ibrahim. Pakistan: Dow University Hospital: Muhammad Sohaib Asghar, Mashaal Syed, Syed Anosh Ali Naqvi. Russia: Kuban State Medical University with affiliation Territorial Hospital #2: Igor Borisovich Zabolotskikh, Konstantin Dmitrievich Zybin, Sergey Vasilevich Sinkov, Tatiana Sergeevna Musaeva. Saudi Arabia: King Fahad Armed Forces Hospital: Razan K. Alamoudi, Hassan M. AlSharif, Sarah A. Almazwaghi, Mohammed S. Elsakran, Mohamed A. Aid, Mouaz A. Darwich, Omnia M. Hagag, Salah A. Ali, Alona rocacorba, Kathrine Supeña, Efren Ray Juane, Jenalyn Medina, Jowany Baduria; King Faisal Specialist Hospital & Research Centre - Riyadh: Marwa Ridha Amer, Mohammed Abdullah Bawazeer, Talal I. Dahhan, Eiad Kseibi, Abid Shahzad Butt, Syed Moazzum Khurshid, Muath Rabee, Mohammed Abujazar, Razan Alghunaim, Maal Abualkhair, Abeer Turki AlFirm, Eiad Kseibi, Syed Moazzum Khurshid, Muath Rabee, Mohammed Abujazar, Razan Alghunaim; King Saud bin Abdulaziz University for Health Sciences and King Abdullah International Medical Research Center: Yaseen M Arabi, Sheryl Ann Abdukahil; King Saud University: Mohammed A. Almazyad, Mohammed I. Alarifi, Jara M. Macarambon, Ahmad Abdullah Bukhari, Hussain A. Albahrani, Kazi N. Asfina, Kaltham M. Aldossary. Serbia: CHC Bezanijska kosa, Belgrade: Marija Zdravkovic. Zoran Todorovic, Viseslav Popadic, Slobodan Klasnja; Institute for Pulmonary Diseases of Vojvodina, Sremska Kamenica: Ana Andrijevic, Srdjan Gavrilovic, Vladimir Carapic; UMC Zvezdara, Belgrad: Bojan Kovacevic, Jovana Bojicic; University Clinical Centre of the Republic of Srpska, Banja Luka, Bosnia And Herzegovina: Pedja Kovacevic; University Hospital Center “Dr Dragisa Misovic-Dedinje”: Stevanovic Predrag, Dejan S. Stojakov, Duska K. Ignjatovic, Suzana C. Bojic, Marina M. Bobos, Irina B. Nenadic, Milica S. Zaric, Marko D. Djuric, Vladimir R. Djukic. Spain: Hospital Universitario La Paz: Santiago Y. Teruel, Belen C. Martin, Santiago Y. Teruel. Turkey: Marmara University: Uluhan Sili, Huseyin Bilgin, Pinar Ay. United States: Advocate Children’s Hospital, IL: Varsha P Gharpure, Usman Raheemi; Advocate Christ Medical Center: Kenneth W. Dodd, Nicholas Goodmanson, Kathleen Hesse, Paige Bird, Chauncey Weinert, Nathan Schoenrade, Abdulrahman Altaher, Esmael Mayar, Matthew Aronson, Tyler Cooper, Monica Logan, Brianna Miner, Gisele Papo; Advocate/Aurora St Luke’s Medical Center: Eric M. Siegal, Phyllis Runningen; Albany Medical Center: Suzanne Barry, Christopher Woll, Gregory Wu, Erin Carrole, Kathryn Burke, Mustafa Mohammed; Allina Health (Abbott Northwestern Hospital, United Hospital and Mercy Hospital in Minnesota): Roman R. Melamed, David M. Tierney, Love A. Patel, Vino S. Raj, Barite U. Dawud, Narayana Mazumder, Abbey Sidebottom, Alena M. Guenther, Benjamin D. Krehbiel, Nova J. Schmitz, Stacy L. Jepsen, Lynn Sipsey, Anna Schulte, Whitney Wunderlich, Cecely Hoyt; AnMed Health: Abhijit A Raval, Andrea Franks; Arkansas Children’s Hospital: Katherine Irby, Ronald C. Sanders Jr., Glenda Hefley; Ascension St. Mary’s Hospital: Jennifer M. Jarvis; Ascension St.Vincent Hospital: Anmol Kharbanda, Sunil Jhajhria, Zachary Fyffe; Ascension/St. Thomas Research Institute West Campus: Stephen Capizzi, Bethany Alicie, Martha Green, Lori Crockarell, Amelia Drennan, Kathleen Dubuque, Tonya Fambrough, Nikole Gasaway, Briana Krantz, Peiman Nebi, Jan Orga, Margaret Serfass, Alina Simion, Kimberly Warren, Cassie Wheeler, CJ Woolman; Atrium Health Navicent: Amy B. Christie, Dennis W. Ashley, Rajani Adiga; Augusta Health: Andrew S. Moyer, George M. Verghese; Augusta University Medical Center: Andrea Sikora Newsome, Christy C. Forehand, Rebecca Bruning, Timothy W. Jones; Aultman Hospital: Moldovan Sabov, Fatema Zaidi, Fiona Tissavirasingham, Dhatri Malipeddi.Banner University Medical Center-Tucson: Jarrod M Mosier, Karen Lutrick, Beth Salvagio Campbell, Cathleen Wilson, Patrick Rivers, Jonathan Brinks, Mokenge Ndiva Mongoh, Boris Gilson; Baptist Health South Florida: Donna Lee Armaignac, Don Parris, Maria Pilar Zuniga, Ilea Vargas, Viviana Boronat, Anneka Hutton, Navneet Kaur, Prashank Neupane, Nohemi Sadule-Rios, Lourdes M. Rojas, Aashish Neupane, Priscilla Rivera, Carlos Valle Carlos, Gregory Vincent; BayCare Health System: Mahesh Amin, Mary E Schelle, Amanda Steadham.Baylor College of Medicine, Baylor St. Lukes Medical Center: Christopher M. Howard, Cameron McBride, Jocelyn Abraham, Orlando Garner, Katherine Richards, Keegan Collins, Preethi Antony, Sindhu Mathew; Baylor Scott & White Health: Valerie C. Danesh, Gueorgui Dubrocq, Amber L. Davis, Marissa J Hammers, Jill M. McGahey, Amanda C. Farris, Elisa Priest, Robyn Korsmo, Lorie Fares, Kathy Skiles, Susan M. Shor, Kenya Burns, Corrie A. Dowell, Gabriela “Hope” Gonzales, Melody Flores, Lindsay Newman, Debora A. Wilk, Jason Ettlinger, Jaccallene Bomar, Himani Darji, Alejandro Arroliga, Alejandro C. Arroliga, Corrie A. Dowell, Gabriela Hope Conzales, Melody Flores, Lindsay Newman, Debora A. Wilk, Jason Ettlinger, Himani Darji, Jaccallene Bomar; Beaumont Children’s Hospital: Paras B. Khandhar, Elizabeth Kring; Beth Israel Deaconess Medical Center: Valerie M. Banner-Goodspeed, Somnath Bose, Lauren E. Kelly, Melisa Joseph, Marie McGourty, Krystal Capers, Benjamin Hoenig, Maria C. Karamourtopoulos, Anica C. Law, Elias N. Baedorf Kassis; Boston University School of Medicine, Boston, MA: Allan J. Walkey, Sushrut S. Waikar, Michael A. Garcia, Mia Colona, Zoe Kibbelaar, Michael Leong, Daniel Wallman, Kanupriya Soni, Jennifer Maccarone, Joshua Gilman, Ycar Devis, Joseph Chung, Munizay Paracha, David N. Lumelsky, Madeline DiLorenzo, Najla Abdurrahman, Shelsey Johnson; Brooke Army Medical Center: Maj Andrew M. Hersh, CPT Stephanie L. Wachs, Brittany S. Swigger, CPT Stephanie L Wachs, Capt Lauren A. Sattler, Capt Michael N. Moulton; Buffalo General Medical Center: Kimberly Zammit Patrick J. McGrath, William Loeffler, Maya R. Chilbert; Cardinal Glennon Children’s Hospital: Aaron S. Miller, Edwin L. Anderson, Rosemary Nagy, Ravali R. Inja; Cedars Sinai Medical Center: Pooja A. Nawathe, Isabel Pedraza, Jennifer Tsing, Karen Carr, Anila Chaudhary, Kathleen Guglielmino; Chambersburg Hospital: Raghavendra Tirupathi, Alymer Tang, Arshad Safi, Cindy Green, Jackie Newell; Chandler Regional Medical Center, Chandler AZ: Francis Maguire, Kris Roach, Jack Short, Jessica Mullins, Angela Roumain; Charleston Area Medical Center: Rayan E. Ihle, Shelda A. Martin, Elaine A. Davis; Children’s Hospital Colorado, University of Colorado Anschutz Medical Campus: Katja M. Gist, Imran A Sayed, John Brinton, Larisa Strom; Children’s Hospital of Philadelphia: Kathleen Chiotos, Allison M. Blatz, Giyoung Lee, Ryan H. Burnett, Guy I. Sydney, Danielle M. Traynor; CHRISTUS Santa Rosa Health System: Karissa Nauert, Annika Gonzalez, Mariel Bagley, Anita Santpurkar; Christus Spohn Shoreline Corpus Christi: Salim Surani, Joshua White, Aftab Khan, Rahul Dhahwal; Clements University Hospital at UT Southwestern Medical Center: Sreekanth Cheruku, Farzin Ahmed, Christopher Deonarine, Ashley Jones, Mohammad-Ali Shaikh, David Preston, Jeanette Chin; Cleveland Clinic (Main Campus, Fairview Hospital, Florida- Weston, Hillcrest Hospital, Marymount Hospital): Vidula Vachharajani, Abhijit Duggal, Prabalini Rajendram, Omar Mehkri, Siddharth Dugar, Michelle Biehl, Gretchen Sacha, Stuart Houltham, Alexander King, Kiran Ashok, Bryan Poynter, Mary Beukemann, Richard Rice, Susan Gole, Valerie Shaner, Adarsh Conjeevaram, Michelle Ferrari, Narendrakumar Alappan, Steven Minear, Jaime Hernandez-Montfort, Syed Sohaib Nasim, Ravi Sunderkrishnan, DebasisSahoo; Community Health Network Indianapolis: Patrick S. Milligan, Sandeep K. Gupta, Joy M. Koglin, Regina Gibson, Lana Johnson, Felicia Preston, Crimson Scott, Bethany Nungester; Cooper University Healthcare: Dana D Byrne, Christa A Schorr, Katie Grant, Katherine L Doktor, Maura C. Porto, Olga Kaplan, James E. Siegler, III, Brian Schonewald, Ashley Woodford, Alan Tsai, Savina Reid, Kuntal Bhowmick, Saba Daneshpooy, Cyrus Mowdawalla, Trishna Akshay Dave, Wilhemina Kennedy Connor Crudeli, Christopher Ferry, Long Nguyen, Sneha Modi, Niharika Padala, Pavan Jitendra Patel, Belle Lin, Lena Chatterjee, Jamie Qiuyun, Fan Mandi Liu, Rasagna Kota, Annesha Banerjee; Cox Medical Center Springfield: Steven K. Daugherty, Sam Atkinson, Kelly Shrimpton; Detar Family Medicine residency: Sidney Ontai, Brian Contreras, MD, Uzoma Obinwanko, Nneka Amamasi, Amir Sharafi; Detroit Medical Centre: Sarah Lee, Zahia Esber, Chetna Jinjvadia; Duke University Hospital: Raquel R Bartz, Vijay Krishnamoorthy, Bryan Kraft, Aaron Pulsipher, Eugene Friedman, Sachin Mehta; Englewood Health: Margit Kaufman, Gregg Lobel, Nisha Gandhi, Amr Abdelaty, Elizabeth Shaji, Kiana Lim, Juan Marte, Dani Ashley Sosa; George Washington University: David P. Yamane, Ivy Benjenk, Nivedita Prasanna; Greenville Memorial Hospital: Nicholas Perkins, Prera J. Roth, Banu Sivaraj, Haley Fulton, Madison G Herin, Marissa Crum, Morgan E. Fretwell, Emily-Rose Zhou; Gundersen Health System La Crosse Wisconsin: Christine Waller, Kara Kallies, Christine Waller, Jonean Thorsen, Alec Fitzsimmons, Haley Olsen; Hassenfeld Children’s Hospital at NYU Langone: Heda R. Dapul, Sourabh Verma, Alan Salas, Ariel Daube, Michelle Korn, Michelle Ramirez, Logi Rajagopalan, Laura Santos; Hospital Auxilio Mutuo: Hector Collazo Santiago, Ricardo Alan Hernandez; Howard University Hospital: Norma Smalls; Jacobi Medical Center: Asher G Bercow, Mark Shlomovich; John R. Oishei Children’s Hospital: Christine Crandall, Sasko Stojanovski, Kristin Johnson, Kelly Michienzi; JPS Health Network: Steven Q. Davis, Valentina Jovic, Valentina Jovic, Max Masuda, Amanda Hayes; Lahey Hospital & Medical Center: Katharine Nault; Lakes Region General Hospital: Michael Smith, William Snow, Riley Liptak, Hannah Durant, Valerie Pendleton, Alay Nanavati, Risa Mrozowsk; LifeBridge Health/Sinai and Northwest Hospitals: Namrata Nag, Jeff Brauer, Ashwin Dharmadhikari, Sahib Singh, Franco Laghi, Ghania Naeem, Andrew Wang, Kevin Bliden, Amit Rout, Jaime Barnes, Martin Gesheff, Asha Thomas, Melbin Thomas, Alicia R. Liendo, Jovan Milosavljevic, Kenan Abbasi, Nicholas B. Burley, Nicole Rapista, Samuel Amankwah, Sanjay K. Poudel, Saroj Timilsina, Sauradeep Sarkar, Oluwasayo Akinyosoye, Shashi K. Yalamanchili, Sheena Moorthy, Sonia Sugumar, Jonathan Ford, Martin C. Taylor, Charlotte Dunderdale, Alyssa Henshaw, Mary K. Brunk, Jessica Hagy, Shehryar Masood, Sushrutha Sridhar; Lincoln Medical and Mental Health Center: Manoj K. Gupta, Franscene E. Oulds, Akshay Nandavar; Loyola University Medical Center: Yuk Ming Liu, Sarah Zavala, Sarah Zavala, Esther Shim; M Health-Fairview, University of Minnesota: Ronald A. Reilkoff, Julia A. Heneghan, Sarah Eichen, Lexie Goertzen, Scott Rajala, Ghislaine Feussom, Ben Tang; MacNeal Hospital Loyola Medicine: Christine C. Junia, Robert Lichtenberg, Hasrat Sidhu, Diana Espinoza, Shelden Rodrigues, Maria Jose Zabala, Daniela Goyes, Ammu Susheela, Buddhi Hatharaliyadda, Naveen Rameshkumar, Amulya Kasireddy, Genessis Maldonado, Lisseth Beltran, Akshata Chaugule, Hassan Khan; Mass General Brigham Hospital: Namrata Patil, Ruhi Patil; Mayo Clinic Arizona: Rodrigo Cartin-Ceba, Ayan Sen, Fahimeh Talaei; Mayo Clinic Rochester: Rahul Kashyap, Juan Pablo Domecq, Ognjen Gajic, Vikas Bansal, Aysun Tekin, Amos Lal, John C. O’Horo, Neha N. Deo, Mayank Sharma, Shahraz Qamar, Romil Singh, Diana J. Valencia Morales; Mayo Clinic, Eau Claire: Abigail T. La Nou, Marija Bogojevic, Simon Zec; Mayo Clinic, Florida: Devang Sanghavi, Pramod Guru, Pablo Moreno Franco, Karthik Gnanapandithan, Hollie Saunders, Zachary Fleissner, Juan Garcia, Alejandra Yu Lee Mateus, Siva Naga Yarrarapu, Nirmaljot Kaur, Abhisekh Giri, Mohammed Mustafa Hasan, Ashrita Donepudi; Mayo Clinic, Mankato: Syed Anjum Khan, Nitesh Kumar Jain, Thoyaja Koritala; Medical Center Health System, Odessa: Alexander Bastidas, Gabriela Orellana, Adriana Briceno Bierwirth, Eliana Milazzo, Juan Guillermo Sierra, Thao Dang; Medical College of Wisconsin: Rahul S Nanchal, Paul A Bergl, Jennifer L Peterson; Mercy Gilbert Medical Center: Jessica Timmer, Kimberly Welker; Mercy Hospital and Medical Center, Chicago: Travis Yamanaka, Nicholas A. Barreras, Michael Markos, Anita Fareeduddin, Rohan Mehta; Mercy Hospital, Saint Louis: Chakradhar Venkata, Miriam Engemann, Annamarie Mantese; MetroHealth Medical Center: Yasir Tarabichi, Adam Perzynski, Christine Wang, Dhatri Kotekal; Midland Memorial Hospital, Texas Tech University Health Sciences Center: Adriana C Briceno Bierwirth, Gabriela M Orellana, Gerardo Catalasan, Shohana Ahmed, Carlos F Matute, Ahmad Hamdan, Ivania Salinas, Genesis Del Nogal, Angel Tejada; Millard Fillmore Suburban Hospital: Anna Eschler, Mary Hejna, Emily Lewandowski, Kristen Kusmierski, Clare Martin; Montefiore Medical Center The Bronx: Jen-Ting Chen, Aluko Hope, Zoe Tsagaris, Elise Ruen, Aram Hambardzumyan; New Hanover Regional Medical Center: Nasar A. Siddiqi, Lesly Jurado, Lindsey Tincher, Carolyn Brown; Nicklaus Children’s Hospital: Prithvi Sendi, Meghana Nadiger, Balagangadhar Totapally; OSF Saint Francis Medical Center: Bhagat S. Aulakh, Sandeep Tripathi, Jennifer A. Bandy, Lisa M. Kreps, Dawn R. Bollinger, Jennifer A. Bandy; OU Medical Center: Neha Gupta, Brent R Brown, Tracy L Jones, Kassidy Malone, Lauren A. Sinko, Amy B. Harrell, Shonda C. Ayers, Lisa M. Settle, Taylor J. Sears; Parkview Health System, Fort Wayne: Roger Scott Stienecker, Andre G. Melendez, Tressa A. Brunner, Sue M Budzon, Jessica L. Heffernan, Janelle M. Souder, Tracy L. Miller, Andrea G. Maisonneuve; ProMedica Toledo Hospital: Roberta E. Redfern, Jessica Shoemaker, Jennifer Micham, Lynn Kenney, Gabriel Naimy; Ridgecrest Regional Hospital: Victoria Schauf; Roper St. Francis Healthcare Charleston: Sara Utley, Holly Balcer; Saint Alphonsus Regional Medical Center: Kerry P. J. Pulver, Jennifer Yehle, Alicia Weeks, Terra Inman; Saint Luke’s Hospital: Majdi Hamarshi, Jeannette Ploetz, Nick Bennett, Kyle Klindworth, Moustafa Younis, Adham Mohamed; Samaritan Health Services: Brian L. Delmonaco, Anthony Franklin, Mitchell Heath; Santa Barbara Cottage Hospital: Diane Barkas; Sarasota Memorial Hospital: Antonia L. Vilella, Sara B. Kutner, Kacie Clark, Danielle Moore; Seattle Children’s Hospital: Shina Menon, John K McGuire, Deana Rich; St. Joseph Mercy Ann Arbor, Ann Arbor: Harry L. Anderson, III, Dixy Rajkumar, Ali Abunayla, Jerrilyn Heiter; St. Joseph’s Candler Health System: Howard A. Zaren, Stephanie J. Smith, Grant C. Lewis, Lauren Seames, Cheryl Farlow, Judy Miller, Gloria Broadstreet; St. Louis Children’s Hospital: John Lin, Cindy Terrill, Brock Montgomery, Sydney Reyes, Summer Reyes, Alex Plattner; St.Agnes Hospital: Anthony Martinez, Micheal Allison, Aniket Mittal, Rafael Ruiz, Aleta Skaanland, Robert Ross . St.Mary Medical Center, Langhorne: Umang Patel, Jordesha Hodge, Krunal Kumar Patel, Shivani Dalal, Himanshu Kavani, Sam Joseph; Stamford Health: Michael A. Bernstein, Ian K. Goff, Matthew Naftilan, Amal Mathew, Deborah Williams, Sue Murdock, RN, Maryanne Ducey, Kerianne Nelson; Stanford Hospital and Clinics: Paul K Mohabir, Connor G O’Brien, Komal Dasani; SUNY Upstate Medical University: William Marx, Ioana Amzuta, Asad J. Choudhry, Mohammad T. Azam; Texas Health Resources, Arlington: Kristina L Carter, PharmD, Michael A Olmos, Brittany M Parker, Julio Quintanilla, Tara A Craig, Brendon J Clough, Jeffrey T Jameson; The Children’s Hospital at OU Medicine: Neha Gupta, Tracy L Jones, Shonda C Ayers, Amy B Harrell, Brent R Brown; The Children’s Hospital of San Antonio, Baylor College of Medicine: Utpal S. Bhalala, Joshua Kuehne, Melinda Garcia, Morgan Beebe, Heather Herrera; The Queen’s Medical Center: Chris Fiack, Stephanie Guo, May Vawer, Beth Blackburn; The University of Tennessee Medical Center: Caleb Darby, Kristy Page, Amanda Brown, Jessie McAbee; Thomas Jefferson University Hospital: Katherine A. Belden, Michael Baram, Devin M. Weber, Rosalie DePaola, Yuwei Xia, Hudson Carter, Aaron Tolley, Mary Ferranti; Truman Medical Centers: Mark Steele, Laurie Kemble; Tulane University Medical Center and University Medical Center New Orleans: Joshua L. Denson, A. Scott Gillet, Margo Brown, Rachael Stevens, Andrew Wetherbie, Kevin Tea, Mathew Moore; UC San Diego Medical Center—Hillcrest: Abdurrahman Husain, Atul Malhotra, Qais Zawaydeh; UNC Medical Center: Benjamin J Sines, Thomas J Bice; University Clinical Hospital, Mostar, Bosnia and Herzegovina: Dragana Markotić, Ivana Bošnjak; University Hospital San Antonio: Emily A. Vail, Susannah Nicholson, Rachelle B. Jonas, AnnaRose E. Dement, William Tang, Mark DeRosa, Robert E. Villarreal; University Medical Center (University Medical Center of Southern Nevada Las Vegas): Rajany V. Dy, Alfredo Iardino, Jill Sharma, Richard Czieki, Julia Christopher, Ryan Lacey, Marwan Mashina, Kushal Patel; University of Alabama at Birmingham: Erica C. Bjornstad, Nancy M. Tofil, Scott House, Isabella Aldana; University of Arkansas for Medical Sciences: Nikhil K. Meena, Jose D. Caceres, Nikhil K Meena, Sarenthia M. Epps, Harmeen Goraya, Kelsey R. Besett, MD, Ryan James, Lana Y. Abusalem, Akash K. Patel, Lana S Hasan; University of Cincinnati: Dina Gomaa B.S., Michael Goodman, Devin Wakefield, Anthony Spuzzillo, John O. Shinn II; University of Colorado Hospital: Robert MacLaren; University of Florida Health Shands Hospital: Azra Bihorac, Tezcan Ozrazgat Baslanti, George Omalay, Haleh Hashemighouchani, Julie S. Cupka, Matthew M Ruppert; University of Iowa Carver College of Medicine: Patrick W. McGonagill, Colette Galet, Janice Hubbard, David Wang, Lauren Allan, Aditya Badheka, Madhuradhar Chegondi; University of Kansas Medical Center: Usman Nazir, Garrett Rampon, Jake Riggle, Nathan Dismang; University of Louisville and Norton Children’s Hospital: Vicki Montgomery, Janice Sullivan, Sarah Morris, Jennifer Nason; University of Louisville Hospital: Ozan Akca, Rainer Lenhardt, Rodrigo S. Cavallazzi, Ann Jerde, Alexa Black, Allison Polidori, Haily Griffey, Justin Winkler, Thomas Brenzel; University of Miami Miller School of Medicine: Roger A. Alvarez, Amarilys Alarcon-Calderon, Marie Anne Sosa, Sunita K. Mahabir, Mausam J. Patel; University of Michigan Health System: Pauline Park, Andrew Admon, Sinan Hanna, Rishi Chanderraj, Maria Pliakas, Ann Wolski, Jennifer Cirino; University of Missouri, Columbia: Dima Dandachi, Hariharan Regunath, Maraya N. Camazine, Grant. E. Geiger, Abdoulie O. Njai, Baraa M. Saad; University of Pittsburgh: Faraaz Ali Shah, Byron Chuan, Sagar L. Rawal, Manal Piracha; University of Utah Health: Joseph E. Tonna, Nicholas M. Levin, Kayte Suslavich, Rachel Tsolinas, Zachary T. Fica, Chloe R. Skidmore; University of Vermont Larner College of Medicine: Renee D. Stapleton, Anne E. Dixon, Olivia Johnson, Sara S. Ardren, Stephanie Burns, Anna Raymond, Erika Gonyaw, Kevin Hodgdon, Chloe Housenger, Benjamin Lin, Karen McQuesten, Heidi Pecott-Grimm, Julie Sweet, Sebastian Ventrone; University of Washington–Northwest: Nita Khandelwal, T. Eoin West, Ellen S. Caldwell, Lara Lovelace-Macon, Navya Garimella, Denisse B. Dow; UT Southwestern Medical Center: Sreekanth R. Cheruku, Catherine Chen, Farzin Ahmed, Christopher Deonarine, Ashley Jones, David Preston, Mohammad-Ali Shaikh, Jeanette Chin; Valleywise Health (formerly Maricopa Medical Center): Murtaza Akhter, Rania Abdul Rahman, Mary Mulrow; Vanderbilt University Medical Center: Erin M. Wilfong, Kelsi Vela; Wake Forest University School of Medicine; Wake Forest Baptist Health Network: Ashish K. Khanna, Lynne Harris, Bruce Cusson, Jacob Fowler, David Vaneenenaam, Glen McKinney, Imoh Udoh, Kathleen Johnson; Washington University School of Medicine and Barnes-Jewish Hospital: Patrick G. Lyons, Andrew P Michelson, Sara S. Haluf, Lauren M. Lynch, Nguyet M. Nguyen, Aaron Steinberg; William S. Middleton Memorial VA Hospital: Nicholas Braus; Wyoming Medical Center: Vishwanath Pattan, Jessica Papke, Ismail Jimada, Nida Mhid, Samuel Chakola; Yale New Haven Health New Haven: Kevin Sheth, Abdalla Ammar, Mahmoud Ammar, Victor Torres Lopez, Charles Dela Cruz, Akhil Khosla, Samir Madeline Gautam.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Supported, in part, by National Institutes of Health/ National Center for Research Resources/National Center for Advancing Translational Sciences' Clinical and Translational Science Award Grant Number UL1 TR002377 (Research Electronic Data Capture), U54 GM104940 which funds the Louisiana Clinical and Translational Science Center Roadmap Scholars Award (to Dr. Denson), American Diabetes Association COVID-19 Research Award 7-20-COVID-053 (to Dr. Denson), the Society of Critical Care Medicine (to Dr. Denson), the Gordon and Betty Moore Foundation (to Dr. Denson), and Janssen Research & Development, LLC (to Drs. Boman, Kumar, and Kashyap).
Dr. Perkins received funding from TelmedIQ. Dr. Kaufman’s institution received funding from the Society of Critical Care Medicine, and she received funding from consulting for Mendaera. Dr. Christie’s institution received funding from Navicent Health Foundation. Ms. Boman, Drs. Kumar’s, Walkey’s, and Kashyap’s institutions received funding from the Gordon and Betty Moore Foundation. Ms. Boman, Drs. Kumar’s, and Kashyap’s institutions received funding from Janssen R & D. Dr. Aston’s institution received funding from the National Institutes of Health. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. The funders had no influence on analysis, interpretation and reporting of pooled data.
List of collaborative co-authors for the Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study (VIRUS): COVID-19 Registry Investigator Group are listed in Appendix 1.
Contributor Information
Collaborators: Jean-Baptiste Mesland, Pierre Henin, Hélène Petre, Isabelle Buelens, Anne-Catherine Gerard, Philippe Clevenbergh, Rolando Claure-Del Granado, Jose A. Mercado, Esdenka Vega-Terrazas, Maria F. Iturricha-Caceres, Ruben Garza, Eric Chu, Victoria Chan, Oscar Y. Gavidia, Felipe Pachon, Yeimy A. Sanchez, Danijel knežević, Mohamed El Kassas, Mohamed Badr, Ahmed Tawheed, Ahmed Tawheed, Hend Yahia, Dimitrios Kantas, Vasileios Koulouras, Estela Pineda, Gabina María Reyes Guillen, Helin Archaga Soto, Ana Karen Vallecillo Lizardo, Csaba Kopitkó, Ágnes Bencze, István Méhész, Zsófia Gerendai, Phaneendra Doddaga, Neethi Chandra, Smitha S. Segu, Tuhin Chakraborty, Epcebha Joyce, Girish Vadgaonkar, Rekha Ediga, Shilpa Basety, Shwetha Dammareddy, Phani Sreeharsha Kasumalla, Umamaheswara Raju, Janaki Manduva, Naresh Kolakani, Shreeja Sripathi, Sheetal Chaitanya, Anusha Cherian, Sreejith Parameswaran, Magesh Parthiban, Menu Priya A., Madhav Prabhu, Vishal Jakati, Puneet Rijhwani, Ashish Jain, Aviral Gupta, Ram Mohan Jaiswal, Ambika Tyagi, Nimish Mathur, Mradul Kumar Daga, Munisha Agarwal, Ishan Rohtagi, Sridhar Papani, Mahesh Kamuram, Kamlesh Kumar Agrawal, Vijendra Baghel, Kirti Kumar Patel, Surapaneni Krishna Mohan, Ekambaram Jyothisree, Mukur Petrolwala, Bharat Ladva, Nooshin Dalili, Mohsen Nafa, Wataru Matsuda, Reina Suzuki, Shu Tahara, Reina Suzuki, Masamitsu Sanui, Sho Horikita, Yuki Itagaki, Akira Kodate, Reina Suzuki, Akira Kodate, Yuki Takahashi, Koyo Moriki, Takuya Shiga, Yudai Iwasaki, Hidenobu Shigemitsu, Yuka Mishima, Nobuyuki Nosaka, Michio Nagashima, Abdulrahman Al-Fares, Mariana Janeth Hermosillo Ulloa, Rene Rodriguez-Gutierrez, Jose Gerardo Gonzalez-Gonzalez, Alejandro Salcido-Montenegro, Adrian Camacho-Ortiz, Fatimah Hassan-Hanga, Hadiza Galadanci, Abubakar Shehu Gezawa, Halima M. S. Kabara, Taiwo Gboluwaga Amole, Halima Kabir, Dalha Gwarzo Haliru, Abdullahi S. Ibrahim, Muhammad Sohaib Asghar, Mashaal Syed, Syed Anosh Ali Naqvi, Igor Borisovich Zabolotskikh, Konstantin Dmitrievich Zybin, Sergey Vasilevich Sinkov, Tatiana Sergeevna Musaeva, Razan K. Alamoudi, Hassan M. AlSharif, Sarah A. Almazwaghi, Mohammed S. Elsakran, Mohamed A. Aid, Mouaz A. Darwich, Omnia M. Hagag, Salah A. Ali, Alona rocacorba, Kathrine Supeña, Efren Ray Juane, Jenalyn Medina, Jowany Baduria, Marwa Ridha Amer, Mohammed Abdullah Bawazeer, Talal I. Dahhan, Eiad Kseibi, Abid Shahzad Butt, Syed Moazzum Khurshid, Muath Rabee, Mohammed Abujazar, Razan Alghunaim, Maal Abualkhair, Abeer Turki AlFirm, Eiad Kseibi, Syed Moazzum Khurshid, Muath Rabee, Mohammed Abujazar, Razan Alghunaim, Yaseen M Arabi, Sheryl Ann Abdukahil, Mohammed A. Almazyad, Mohammed I. Alarifi, Jara M. Macarambon, Ahmad Abdullah Bukhari, Hussain A. Albahrani, Kazi N. Asfina, Kaltham M. Aldossary, Marija Zdravkovic, Zoran Todorovic, Viseslav Popadic, Slobodan Klasnja, Ana Andrijevic, Srdjan Gavrilovic, Vladimir Carapic, Bojan Kovacevic, Jovana Bojicic, Pedja Kovacevic, Stevanovic Predrag, Dejan S. Stojakov, Duska K. Ignjatovic, Suzana C. Bojic, Marina M. Bobos, Irina B. Nenadic, Milica S. Zaric, Marko D. Djuric, Vladimir R. Djukic, Santiago Y. Teruel, Belen C. Martin, Santiago Y. Teruel, Uluhan Sili, Huseyin Bilgin, Pinar Ay, Varsha P Gharpure, Usman Raheemi, Kenneth W. Dodd, Nicholas Goodmanson, Kathleen Hesse, Paige Bird, Chauncey Weinert, Nathan Schoenrade, Abdulrahman Altaher, Esmael Mayar, Matthew Aronson, Tyler Cooper, Monica Logan, Brianna Miner, Gisele Papo, Eric M. Siegal, Phyllis Runningen, Suzanne Barry, Christopher Woll, Gregory Wu, Erin Carrole, Kathryn Burke, Mustafa Mohammed, Roman R. Melamed, David M. Tierney, Love A. Patel, Vino S. Raj, Barite U. Dawud, Narayana Mazumder, Abbey Sidebottom, Alena M. Guenther, Benjamin D. Krehbiel, Nova J. Schmitz, Stacy L. Jepsen, Lynn Sipsey, Anna Schulte, Whitney Wunderlich, Cecely Hoyt, Abhijit A Raval, Andrea Franks, Katherine Irby, Ronald C. Sanders, Jr., Glenda Hefley, Jennifer M. Jarvis, Anmol Kharbanda, Sunil Jhajhria, Zachary Fyffe, Stephen Capizzi, Bethany Alicie, Martha Green, Lori Crockarell, Amelia Drennan, Kathleen Dubuque, Tonya Fambrough, Nikole Gasaway, Briana Krantz, Peiman Nebi, Jan Orga, Margaret Serfass, Alina Simion, Kimberly Warren, Cassie Wheeler, CJ Woolman, Amy B. Christie, Dennis W. Ashley, Rajani Adiga, Andrew S. Moyer, George M. Verghese, Andrea Sikora Newsome, Christy C. Forehand, Rebecca Bruning, Timothy W. Jones, Moldovan Sabov, Fatema Zaidi, Fiona Tissavirasingham, Dhatri Malipeddi, Jarrod M Mosier, Karen Lutrick, Beth Salvagio Campbell, Cathleen Wilson, Patrick Rivers, Jonathan Brinks, Mokenge Ndiva Mongoh, Boris Gilson, Donna Lee Armaignac, Don Parris, Maria Pilar Zuniga, Ilea Vargas, Viviana Boronat, Anneka Hutton, Navneet Kaur, Prashank Neupane, Nohemi Sadule-Rios, Lourdes M. Rojas, Aashish Neupane, Priscilla Rivera, Carlos Valle Carlos, Gregory Vincent, Mahesh Amin, Mary E Schelle, Amanda Steadham, Christopher M. Howard, Cameron McBride, Jocelyn Abraham, Orlando Garner, Katherine Richards, Keegan Collins, Preethi Antony, Sindhu Mathew, Valerie C. Danesh, Gueorgui Dubrocq, Amber L. Davis, Marissa J Hammers, Jill M. McGahey, Amanda C. Farris, Elisa Priest, Robyn Korsmo, Lorie Fares, Kathy Skiles, Susan M. Shor, Kenya Burns, Corrie A. Dowell, Melody Flores, Lindsay Newman, Debora A. Wilk, Jason Ettlinger, Jaccallene Bomar, Himani Darji, Alejandro Arroliga, Alejandro C. Arroliga, Corrie A. Dowell, Gabriela Hope Conzales, Melody Flores, Lindsay Newman, Debora A. Wilk, Jason Ettlinger, Himani Darji, Jaccallene Bomar, Paras B. Khandhar, Elizabeth Kring, Valerie M. Banner-Goodspeed, Somnath Bose, Lauren E. Kelly, Melisa Joseph, Marie McGourty, Krystal Capers, Benjamin Hoenig, Maria C. Karamourtopoulos, Anica C. Law, Elias N. Baedorf Kassis, Allan J. Walkey, Sushrut S. Waikar, Michael A. Garcia, Mia Colona, Zoe Kibbelaar, Michael Leong, Daniel Wallman, Kanupriya Soni, Jennifer Maccarone, Joshua Gilman, Ycar Devis, Joseph Chung, Munizay Paracha, David N. Lumelsky, Madeline DiLorenzo, Najla Abdurrahman, Shelsey Johnson, Maj Andrew M. Hersh, CPT Stephanie L. Wachs, Brittany S. Swigger, CPT Stephanie L Wachs, Capt Lauren A. Sattler, Capt Michael N. Moulton, Kimberly Zammit, Patrick J. McGrath, William Loeffler, Maya R. Chilbert, Aaron S. Miller, Edwin L. Anderson, Rosemary Nagy, Ravali R. Inja, Pooja A. Nawathe, Isabel Pedraza, Jennifer Tsing, Karen Carr, Anila Chaudhary, Kathleen Guglielmino, Raghavendra Tirupathi, Alymer Tang, Arshad Safi, Cindy Green, Jackie Newell, Francis Maguire, Kris Roach, Jack Short, Jessica Mullins, Angela Roumain, Rayan E. Ihle, Shelda A. Martin, Elaine A. Davis, Katja M. Gist, Imran A Sayed, John Brinton, Larisa Strom, Kathleen Chiotos, Allison M. Blatz, Giyoung Lee, Ryan H. Burnett, Guy I. Sydney, Danielle M. Traynor, Karissa Nauert, Annika Gonzalez, Mariel Bagley, Anita Santpurkar, Salim Surani, Joshua White, Aftab Khan, Rahul Dhahwal, Sreekanth Cheruku, Farzin Ahmed, Christopher Deonarine, Ashley Jones, Mohammad-Ali Shaikh, David Preston, Jeanette Chin, Vidula Vachharajani, Abhijit Duggal, Prabalini Rajendram, Omar Mehkri, Siddharth Dugar, Michelle Biehl, Gretchen Sacha, Stuart Houltham, Alexander King, Kiran Ashok, Bryan Poynter, Mary Beukemann, Richard Rice, Susan Gole, Valerie Shaner, Adarsh Conjeevaram, Michelle Ferrari, Narendrakumar Alappan, Steven Minear, Jaime Hernandez-Montfort, Syed Sohaib Nasim, Ravi Sunderkrishnan, Patrick S. Milligan, Sandeep K. Gupta, Joy M. Koglin, Regina Gibson, Lana Johnson, Felicia Preston, Crimson Scott, Bethany Nungester, Dana D Byrne, Christa A Schorr, Katie Grant, Katherine L Doktor, Maura C. Porto, Olga Kaplan, James E. Siegler, Brian Schonewald, Ashley Woodford, Alan Tsai, Savina Reid, Kuntal Bhowmick, Saba Daneshpooy, Cyrus Mowdawalla, Trishna Akshay Dave, Wilhemina Kennedy Connor Crudeli, Christopher Ferry, Long Nguyen, Sneha Modi, Niharika Padala, Pavan Jitendra Patel, Belle Lin, Lena Chatterjee, Jamie Qiuyun, Fan Mandi Liu, Rasagna Kota, Annesha Banerjee, Steven K. Daugherty, Sam Atkinson, Kelly Shrimpton, Sidney Ontai, Brian Contreras, Uzoma Obinwanko, Nneka Amamasi, Amir Sharafi, Sarah Lee, Zahia Esber, Chetna Jinjvadia, Raquel R Bartz, Vijay Krishnamoorthy, Bryan Kraft, Aaron Pulsipher, Eugene Friedman, Sachin Mehta, Margit Kaufman, Gregg Lobel, Nisha Gandhi, Amr Abdelaty, Elizabeth Shaji, Kiana Lim, Juan Marte, Dani Ashley Sosa, David P. Yamane, Ivy Benjenk, Nivedita Prasanna, Nicholas Perkins, Prera J. Roth, Banu Sivaraj, Haley Fulton, Madison G Herin, Marissa Crum, Morgan E. Fretwell, Emily-Rose Zhou, Christine Waller, Kara Kallies, Christine Waller, Jonean Thorsen, Alec Fitzsimmons, Haley Olsen, Heda R. Dapul, Sourabh Verma, Alan Salas, Ariel Daube, Michelle Korn, Michelle Ramirez, Logi Rajagopalan, Laura Santos, Hector Collazo Santiago, Ricardo Alan Hernandez, Norma Smalls, Asher G Bercow, Mark Shlomovich, Christine Crandall, Sasko Stojanovski, Kristin Johnson, Kelly Michienzi, Steven Q. Davis, Valentina Jovic, Valentina Jovic, Max Masuda, Amanda Hayes, Katharine Nault, Michael Smith, William Snow, Riley Liptak, Hannah Durant, Valerie Pendleton, Alay Nanavati, Risa Mrozowsk, Namrata Nag, Jeff Brauer, Ashwin Dharmadhikari, Sahib Singh, Franco Laghi, Ghania Naeem, Andrew Wang, Kevin Bliden, Amit Rout, Jaime Barnes, Martin Gesheff, Asha Thomas, Melbin Thomas, Alicia R. Liendo, Jovan Milosavljevic, Kenan Abbasi, Nicholas B. Burley, Nicole Rapista, Samuel Amankwah, Sanjay K. Poudel, Saroj Timilsina, Sauradeep Sarkar, Oluwasayo Akinyosoye, Shashi K. Yalamanchili, Sheena Moorthy, Sonia Sugumar, Jonathan Ford, Martin C. Taylor, Charlotte Dunderdale, Alyssa Henshaw, Mary K. Brunk, Jessica Hagy, Shehryar Masood, Sushrutha Sridhar, Manoj K. Gupta, Franscene E. Oulds, Akshay Nandavar, Yuk Ming Liu, Sarah Zavala, Sarah Zavala, Esther Shim, Ronald A. Reilkoff, Julia A. Heneghan, Sarah Eichen, Lexie Goertzen, Scott Rajala, Ghislaine Feussom, Ben Tang, Christine C. Junia, Robert Lichtenberg, Hasrat Sidhu, Diana Espinoza, Shelden Rodrigues, Maria Jose Zabala, Daniela Goyes, Ammu Susheela, Buddhi Hatharaliyadda, Naveen Rameshkumar, Amulya Kasireddy, Genessis Maldonado, Lisseth Beltran, Akshata Chaugule, Hassan Khan, Namrata Patil, Ruhi Patil, Rodrigo Cartin-Ceba, Ayan Sen, Fahimeh Talaei, Rahul Kashyap, Juan Pablo Domecq, Ognjen Gajic, Vikas Bansal, Aysun Tekin, Amos Lal, John C. O’Horo, Neha N. Deo, Mayank Sharma, Shahraz Qamar, Romil Singh, Diana J. Valencia Morales, Abigail T. La Nou, Marija Bogojevic, Simon Zec, Devang Sanghavi, Pramod Guru, Pablo Moreno Franco, Karthik Gnanapandithan, Hollie Saunders, Zachary Fleissner, Juan Garcia, Alejandra Yu Lee Mateus, Siva Naga Yarrarapu, Nirmaljot Kaur, Abhisekh Giri, Mohammed Mustafa Hasan, Ashrita Donepudi, Syed Anjum Khan, Nitesh Kumar Jain, Thoyaja Koritala, Alexander Bastidas, Gabriela Orellana, Adriana Briceno Bierwirth, Eliana Milazzo, Juan Guillermo Sierra, Thao Dang, Rahul S Nanchal, Paul A Bergl, Jennifer L Peterson, Jessica Timmer, Kimberly Welker, Travis Yamanaka, Nicholas A. Barreras, Michael Markos, Anita Fareeduddin, Rohan Mehta, Chakradhar Venkata, Miriam Engemann, Annamarie Mantese, Yasir Tarabichi, Adam Perzynski, Christine Wang, Dhatri Kotekal, Adriana C Briceno Bierwirth, Gabriela M Orellana, Gerardo Catalasan, Shohana Ahmed, Carlos F Matute, Ahmad Hamdan, Ivania Salinas, Genesis Del Nogal, Angel Tejada, Anna Eschler, Mary Hejna, Emily Lewandowski, Kristen Kusmierski, Clare Martin, Jen-Ting Chen, Aluko Hope, Zoe Tsagaris, Elise Ruen, Aram Hambardzumyan, Nasar A. Siddiqi, Lesly Jurado, Lindsey Tincher, Carolyn Brown, Prithvi Sendi, Meghana Nadiger, Balagangadhar Totapally, Bhagat S. Aulakh, Sandeep Tripathi, Jennifer A. Bandy, Lisa M. Kreps, Dawn R. Bollinger, Jennifer A. Bandy, Neha Gupta, Brent R Brown, Tracy L Jones, Kassidy Malone, Lauren A. Sinko, Amy B. Harrell, Shonda C. Ayers, Lisa M. Settle, Taylor J. Sears, Roger Scott Stienecker, Andre G. Melendez, Tressa A. Brunner, Sue M Budzon, Jessica L. Heffernan, Janelle M. Souder, Tracy L. Miller, Andrea G. Maisonneuve, Roberta E. Redfern, Jessica Shoemaker, Jennifer Micham, Lynn Kenney, Gabriel Naimy, Victoria Schauf, Sara Utley, Holly Balcer, Kerry P. J. Pulver, Jennifer Yehle, Alicia Weeks, Terra Inman, Majdi Hamarshi, Jeannette Ploetz, Nick Bennett, Kyle Klindworth, Moustafa Younis, Adham Mohamed, Brian L. Delmonaco, Anthony Franklin, Mitchell Heath, Diane Barkas, Antonia L. Vilella, Sara B. Kutner, Kacie Clark, Danielle Moore, Shina Menon, John K McGuire, Deana Rich, Harry L. Anderson, III, Dixy Rajkumar, Ali Abunayla, Jerrilyn Heiter, Howard A. Zaren, Stephanie J. Smith, Grant C. Lewis, Lauren Seames, Cheryl Farlow, Judy Miller, Gloria Broadstreet, John Lin, Cindy Terrill, Brock Montgomery, Sydney Reyes, Summer Reyes, Alex Plattner, Anthony Martinez, Micheal Allison, Aniket Mittal, Rafael Ruiz, Aleta Skaanland, Robert Ross, Umang Patel, Jordesha Hodge, Krunal Kumar Patel, Shivani Dalal, Himanshu Kavani, Sam Joseph, Michael A. Bernstein, Ian K. Goff, Matthew Naftilan, Amal Mathew, Deborah Williams, Sue Murdock, Maryanne Ducey, Kerianne Nelson, Paul K Mohabir, Connor G O’Brien, Komal Dasani, William Marx, Ioana Amzuta, Asad J. Choudhry, Mohammad T. Azam, Kristina L Carter, Michael A Olmos, Brittany M Parker, Julio Quintanilla, Tara A Craig, Brendon J Clough, Jeffrey T Jameson, Neha Gupta, Tracy L Jones, Shonda C Ayers, Amy B Harrell, Brent R Brown, Utpal S. Bhalala, Joshua Kuehne, Melinda Garcia, Morgan Beebe, Heather Herrera, Chris Fiack, Stephanie Guo, May Vawer, Beth Blackburn, Caleb Darby, Kristy Page, Amanda Brown, Jessie McAbee, Katherine A. Belden, Michael Baram, Devin M. Weber, Rosalie DePaola, Yuwei Xia, Hudson Carter, Aaron Tolley, Mary Ferranti, Mark Steele, Laurie Kemble, Joshua L. Denson, A. Scott Gillet, Margo Brown, Rachael Stevens, Andrew Wetherbie, Kevin Tea, Mathew Moore, Abdurrahman Husain, Atul Malhotra, Qais Zawaydeh, Benjamin J Sines, Thomas J Bice, Dragana Markotić, Ivana Bošnjak, Emily A. Vail, Susannah Nicholson, Rachelle B. Jonas, AnnaRose E. Dement, William Tang, Mark DeRosa, Robert E. Villarreal, Rajany V. Dy, Alfredo Iardino, Jill Sharma, Richard Czieki, Julia Christopher, Ryan Lacey, Marwan Mashina, Kushal Patel, Erica C. Bjornstad, Nancy M. Tofil, Scott House, Isabella Aldana, Nikhil K. Meena, Jose D. Caceres, Nikhil K Meena, Sarenthia M. Epps, Harmeen Goraya, Kelsey R. Besett, Ryan James, Lana Y. Abusalem, Akash K. Patel, Lana S Hasan, Dina Gomaa, Michael Goodman, Devin Wakefield, Anthony Spuzzillo, John O. Shinn, II, Robert MacLaren, Azra Bihorac, Tezcan Ozrazgat Baslanti, George Omalay, Haleh Hashemighouchani, Julie S. Cupka, Matthew M Ruppert, Patrick W. McGonagill, Colette Galet, Janice Hubbard, David Wang, Lauren Allan, Aditya Badheka, Madhuradhar Chegondi, Usman Nazir, Garrett Rampon, Jake Riggle, Nathan Dismang, Vicki Montgomery, Janice Sullivan, Sarah Morris, Jennifer Nason, Ozan Akca, Rainer Lenhardt, Rodrigo S. Cavallazzi, Ann Jerde, Alexa Black, Allison Polidori, Haily Griffey, Justin Winkler, Thomas Brenzel, Roger A. Alvarez, Amarilys Alarcon-Calderon, Marie Anne Sosa, Sunita K. Mahabir, Mausam J. Patel, Pauline Park, Andrew Admon, Sinan Hanna, Rishi Chanderraj, Maria Pliakas, Ann Wolski, Jennifer Cirino, Dima Dandachi, Hariharan Regunath, Maraya N. Camazine, Grant. E. Geiger, Abdoulie O. Njai, Baraa M. Saad, Faraaz Ali Shah, Byron Chuan, Sagar L. Rawal, Manal Piracha, Joseph E. Tonna, Nicholas M. Levin, Kayte Suslavich, Rachel Tsolinas, Zachary T. Fica, Chloe R. Skidmore, Renee D. Stapleton, Anne E. Dixon, Olivia Johnson, Sara S. Ardren, Stephanie Burns, Anna Raymond, Erika Gonyaw, Kevin Hodgdon, Chloe Housenger, Benjamin Lin, Karen McQuesten, Heidi Pecott-Grimm, Julie Sweet, Sebastian Ventrone, Nita Khandelwal, T. Eoin West, Ellen S. Caldwell, Lara Lovelace-Macon, Navya Garimella, Denisse B. Dow, Sreekanth R. Cheruku, Catherine Chen, Farzin Ahmed, Christopher Deonarine, Ashley Jones, David Preston, Mohammad-Ali Shaikh, Jeanette Chin, Murtaza Akhter, Rania Abdul Rahman, Mary Mulrow, Erin M. Wilfong, Kelsi Vela, Ashish K. Khanna, Lynne Harris, Bruce Cusson, Jacob Fowler, David Vaneenenaam, Glen McKinney, Imoh Udoh, Kathleen Johnson, Patrick G. Lyons, Andrew P Michelson, Sara S. Haluf, Lauren M. Lynch, Nguyet M. Nguyen, Aaron Steinberg, Nicholas Braus, Vishwanath Pattan, Jessica Papke, Ismail Jimada, Nida Mhid, Samuel Chakola, Kevin Sheth, Abdalla Ammar, Mahmoud Ammar, Victor Torres Lopez, Charles Dela Cruz, Akhil Khosla, and Samir Madeline Gautam
REFERENCES
- 1.Rossi GP, Sanga V, Barton M: Potential harmful effects of discontinuing ACE-inhibitors and ARBs in COVID-19 patients. Elife 2020; 9:e57278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Furuhashi M, Moniwa N, Mita T, et al. : Urinary angiotensin-converting enzyme 2 in hypertensive patients may be increased by olmesartan, an angiotensin II receptor blocker. Am J Hypertens 2015; 28:15–21 [DOI] [PubMed] [Google Scholar]
- 3.Zheng Z, Peng F, Xu B, et al. : Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis J Infect 2020; 81:e16–e25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fernández-Ruiz I: RAAS inhibitors do not increase the risk of COVID-19. Nat Rev Cardiol 2020; 17:383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morales DR, Conover MM, You SC, et al. : Renin-angiotensin system blockers and susceptibility to COVID-19: An international, open science, cohort analysis. Lancet Digit Health 2021; 3:e98-e114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.An J, Wei R, Zhou H, et al. : Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers use and COVID-19 infection among 824 650 patients with hypertension from a US integrated healthcare system. J Am Heart Assoc 2021; 10:e019669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lopes RD, Macedo AVS, de Barros E Silva PGM, et al. ; BRACE CORONA Investigators: Effect of discontinuing vs continuing angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on days alive and out of the hospital in patients admitted with COVID-19: A randomized clinical trial. JAMA 2021; 325:254–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bauer A, Schreinlechner M, Sappler N, et al. ; ACEI-COVID investigators: Discontinuation versus continuation of renin-angiotensin-system inhibitors in COVID-19 (ACEI-COVID): A prospective, parallel group, randomised, controlled, open-label trial. Lancet Respir Med 2021; 9:863–872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scialo F, Daniele A, Amato F, et al. : ACE2: The major cell entry receptor for SARS-CoV-2. Lung 2020; 198:867–877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hippisley-Cox J, Young D, Coupland C, et al. : Risk of severe COVID-19 disease with ACE inhibitors and angiotensin receptor blockers: Cohort study including 8.3 million people. Heart 2020; 106:1503–1511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walkey AJ, Kumar VK, Harhay MO, et al. : The viral infection and respiratory illness universal study (VIRUS): An international registry of coronavirus 2019-related critical illness. Crit Care Explor 2020; 2:e0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris PA, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)–A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khera R, Clark C, Lu Y, et al. : Association of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers with the risk of hospitalization and death in hypertensive patients with coronavirus disease-19. medRxiv 2020; 2020.05.17.20104943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ip A, Parikh K, Parrillo JE, et al. : Hypertension and renin-angiotensin-aldosterone system inhibitors in patients with Covid-19. medRxiv 2020; 2020.04.24.20077388 [Google Scholar]
- 15.Nunes JPL: Mortality and use of angiotensin-converting enzyme inhibitors in COVID 19 disease: A systematic review. Porto Biomed J 2020; 5:e085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Felice C, Nardin C, Di Tanna GL, et al. : Use of RAAS inhibitors and risk of clinical deterioration in COVID-19: Results from an Italian cohort of 133 hypertensives. Am J Hypertens 2020; 33:944–948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang G, Wu Y, Xu R, et al. : Effects of renin-angiotensin-aldosterone system inhibitors on disease severity and mortality in patients with COVID-19: A meta-analysis. J Med Virol 2021; 93:2287–2300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y, Chen B, Li Y, et al. : The use of renin-angiotensin-aldosterone system (RAAS) inhibitors is associated with a lower risk of mortality in hypertensive COVID-19 patients: A systematic review and meta-analysis. J Med Virol 2021; 93:1370–1377 [DOI] [PubMed] [Google Scholar]
- 19.Baral R, White M, Vassiliou VS: Effect of renin-angiotensin-aldosterone system inhibitors in patients with COVID-19: A systematic review and meta-analysis of 28,872 patients. Curr Atheroscler Rep 2020; 22:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barochiner J, Martínez R: Use of inhibitors of the renin-angiotensin system in hypertensive patients and COVID-19 severity: A systematic review and meta-analysis. J Clin Pharm Ther 2020; 45:1244–1252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu X, Long C, Xiong Q, et al. : Association of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with risk of COVID-19, inflammation level, severity, and death in patients with COVID-19: A rapid systematic review and meta-analysis. Clin Cardiol 2020;10.1002/clc.23421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yuan Y, Liu D, Zeng S, et al. : In-hospital use of ACEI/ARB is associated with lower risk of mortality and critic illness in COVID-19 patients with hypertension. J Infect 2020; 81:816–846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mancia G, Rea F, Corrao G, et al. : Two-drug combinations as first-step antihypertensive treatment. Circ Res 2019; 124:1113–1123 [DOI] [PubMed] [Google Scholar]
- 24.Yehualashet AS, Belachew TF: ACEIs and ARBs and their correlation with COVID-19: A review. Infect Drug Resist 2020; 13:3217–3224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Derington CG, Cohen JB, Mohanty AF, et al. : Angiotensin II receptor blocker or angiotensin-converting enzyme inhibitor use and COVID-19-related outcomes among US Veterans. PLoS One 2021; 16:e0248080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vandenbroucke JP, von Elm E, Altman DG, et al. ; STROBE Initiative: Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. PLoS Med 2007; 4:e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walkey AJ, Sheldrick RC, Kashyap R, et al. : Guiding principles for the conduct of observational critical care research for coronavirus disease 2019 pandemics and beyond: The Society of Critical Care Medicine discovery viral infection and respiratory illness universal study registry. Crit Care Med 2020; 48:e1038–e1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.