Abstract
Although recent studies have examined the bidirectional associations between physical activity and sleep parameters, few have focused on older adults utilizing objective assessments, such as polysomnography. This micro-longitudinal observational study included 92 Japanese older adults (aged 65–86 years) who underwent objective evaluations of sleep quality using polysomnography and completed subjective sleep-related questionnaires. Activity levels were assessed using an accelerometer. Polysomnography, subjective sleep-related questionnaires, and accelerometer were administered for 7 consecutive days. Multilevel models (participant-, day-level) were used to examine the temporal associations of objective and subjective sleep parameters with sedentary behavior and physical activity. In the day-level analysis, higher levels of sedentary behavior during daytime were associated with longer rapid eye movement (REM) sleep, shorter REM latency, lower levels of non-REM sleep (stage N3), and reduced delta power during daytime. Higher levels of low-intensity physical activity during daytime were associated with lower levels of REM sleep, longer REM latency, and increased stage N3 sleep in the day-level analysis. Higher levels of moderate-to-vigorous physical activity were associated with increased REM latency. Longer subjective sleep time was associated with increased next-day moderate-to-vigorous physical activity. Thus, low-intensity physical activity may provide objective benefits related to deep sleep parameters in older adults.
Subject terms: Geriatrics, Public health, Quality of life
Introduction
Non-restorative sleep and difficulties initiating or maintaining sleep have been reported in approximately 50% of older adults1. Several studies have demonstrated that these disturbances are caused by age-related factors, such as decreased physical activity, social isolation, increased levels of depressive symptoms, and circadian rhythm alterations2–5.
The prevalence of insomnia is lower among older adults who engage in daily physical activity6, which exerts distinct effects on sleep quality depending on its intensity (e.g., sedentary behavior, low- or moderate-to-vigorous intensity)7; in particular, daily low-intensity physical activity (e.g., light walking, stretching, lifting hand weights, etc.) is associated with improved sleep quality7,8. Moreover, engaging in moderate-to-vigorous intensity aerobic exercise (e.g., cycling, running, etc.) also improves sleep quality9,10. Although the effects of exercise on sleep quality vary in magnitude depending on the type of activity11, daily physical activities, such as housework and work-related activities, are also positively associated with sleep quality in older adults12. Physical activity affects sleep quality by several mechanisms, including energy conservation, increases in body and central nervous system temperature, and decreases in anxiety13–15.
Several methods can be used to assess sleep quality, including validated questionnaires, wrist actigraphy, and polysomnography5. However, previous studies have reported low correlations between objective and subjective assessments of sleep quality16,17 as the two measures appear to reflect different aspects of sleep quality17. Subjective sleep quality is mainly measured via qualitative evaluation of the monthly average sleep quality (e.g., using the Pittsburgh Sleep Quality Index). In contrast, objective sleep quality is measured by actigraphy or polysomnography. Moreover, polysomnography can provide more detailed information on different sleep stages (e.g., shallow or deep sleep) in addition to other objective sleep parameters (e.g., total sleep time and sleep latency). Sleep architecture is related to collapsed circadian rhythm and the presence of depression, dementia, and mortality18,19. For example, rapid eye movement (REM) sleep is thought to reset the brain and has been associated with improvement in cognitive function the next day18. Specifically, while cholinergic neurons are important modulators of REM sleep, REM sleep itself has a positive recovery effect on cholinergic network impairments and on the imbalance between cholinergic and orexinergic systems18. Furthermore, a shorter REM sleep duration has been associated with higher mortality among older adults19.
Actigraphy can be used to assess sleep habits in daily life. Recent epidemiological studies have objectively examined the relationship between physical activity and sleep using accelerometer and actigraphy data7,20,21. Thirty minutes of sedentary behavior per day with an equal period of low-intensity physical activity was associated with decreased wakefulness after sleep onset and greater sleep efficiency among older adults7.
Technological developments in assessment methods have led to the development of various statistical methods, such as multilevel analysis. Continuous physical activity and sleep data are structured based on each participant, and multilevel analysis allows one to assess bidirectional relationships both between (level 2: participant-level) and within participants (level 1: day-level)22. Multilevel analysis can therefore be used to examine temporal directionality, both between and within participants, between sleep and physical activity throughout the week. This approach provides insight into the temporal directionality between physical activity and sleep and the mutual correlation after considering between-participant differences22. However, a common limitation among these studies is that they could not assess relationships based on sleep stage23–26.
Some previous studies have attempted to achieve more accurate quantitative and qualitative evaluations based on estimated sleep stages and delta power (0.75–4.00 Hz)27,28. Delta power refers to the scalp surface representation of a highly complex ensemble of oscillatory activity during non-REM sleep, including the cortical up and down states that comprise the slow oscillation29,30.
Actigraphy allows for quantitative evaluation but cannot provide qualitative data concerning sleep stage or delta power. However, polysomnography allows for both quantitative (e.g., total sleep time and sleep latency) and qualitative evaluations (e.g., shallow or deep sleep). To date, previous studies have not used continuous polysomnography due to the burden of unfamiliar sleep environments (e.g., laboratory and/or medical facilities) in older adults. In addition, skilled staff are required to attach polysomnography electrodes. Therefore, consecutive daily measurements using ordinary polysomnography are almost impossible, especially for older adults. To overcome these limitations, some studies have used simple home-based polysomnography devices under participants’ free-living home conditions31,32.
Several studies have demonstrated a bidirectional relationship between physical activity and sleep quality as measured using actigraphy or recorded using sleep diaries22,23,26,33. However, few such studies have utilized polysomnography, and the day-to-day bidirectional relationship between daily physical activity and objectively measured sleep depth (e.g., sleep stage) remains unknown. Based on previous evidence7,8, we hypothesized that increased day-to-day physical activity performed at low intensity would exhibit a linear relationship with objective parameters that are positively related to deep sleep (e.g., sleep stage 3 and delta power) and with REM sleep parameters. To evaluate our hypothesis, we examined the bidirectional associations between the objectively measured day-to-day intensity of physical activities and both objective and subjective sleep quality in older adults.
Results
Participant characteristics
We analyzed accelerometer and polysomnography data for 92 participants. The average number of days with valid actigraphy and polysomnography data was 6.5 ± 0.9 days. Further, the number of days for the self-report questionnaire (OSA-MA version) was 6.7 ± 1.0 days.
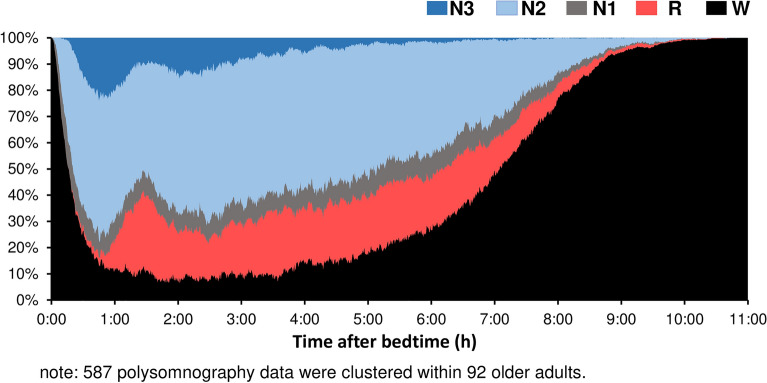
Participant characteristics are presented in Table 1, and the cumulative display of sleep architecture for all 92 participants is shown in Fig. 1. Time in bed and total sleep time among all participants were 7.7 and 6.2 h per day, respectively. The durations of daily sedentary behavior, low-intensity physical activities, and moderate-to-vigorous-intensity physical activities were 533.4 min per day (58.2% of wear time), 316.7 min per day (34.7% of wear time), and 64.6 min per day (7.1% of wear time), respectively (Table 1). We confirmed the intercorrelations among polysomnography and the OSA-MA version parameters. The sleep onset latency measured by polysomnography was significantly negatively related with sleepiness on rising (r = − 0.218), initiation and maintenance of sleep (r = − 0.277), and the OSA total score (r = − 0.255). The REM latency was significantly negatively related with initiation and maintenance of sleep (r = − 0.357). Additionally, the total sleep time was negatively related with frequent dreaming (r = − 0.217) and positively related with sleep length (r = 0.244) (all P values < 0.05).
Table 1.
Characteristics of participants.
| Mean ± SD | Min | Max | |
|---|---|---|---|
| Age, years | 73.9 ± 5.0 | 65 | 86 |
| Female, n (%) | 73 (79.3) | ||
| Body mass index, kg/m2 | 23.7 ± 3.2 | 16.9 | 38.3 |
| Smoking history, n (%) | 1 (1.1) | ||
| Alcohol consumption (drinker), n (%) | 35 (38.0) | ||
| Caffeine consumption (drinker), n (%) | 84 (91.3) | ||
| Medical history | |||
| Hypertension, n (%) | 35 (38.0) | ||
| Hyperlipidemia, n (%) | 18 (19.6) | ||
| Diabetes, n (%) | 4 (4.3) | ||
| GDS score, points | 3.2 ± 2.8 | 0 | 14 |
| Objective sleep parameters | |||
| Time in bed, min | 459 ± 62.3 | 243.6 | 612.1 |
| Total sleep time, min | 373.6 ± 44.6 | 208.9 | 452.9 |
| Sleep latency, min | 19.7 ± 11.0 | 4.3 | 60.6 |
| WASO, min | 68.1 ± 30.3 | 21.2 | 149.8 |
| Sleep efficiency, % | 81.4 ± 6.2 | 64.8 | 91.7 |
| REM latency, min | 96.7 ± 34.3 | 48.4 | 240.8 |
| N1, % | 10.5 ± 4.2 | 2.6 | 25.3 |
| N2, % | 58.3 ± 7.0 | 43.0 | 75.6 |
| N3, % | 7.9 ± 7.3 | 0 | 27.8 |
| REM, % | 23.3 ± 4.1 | 13.3 | 33.1 |
| Sum of delta power, μV2/night | 115,306 ± 9223 | 25,768 | 272,428 |
| Subjective sleep parameters | |||
| Sleepiness on rising, pts | 51.8 ± 7.5 | 30.1 | 65.0 |
| Initiation and maintenance of sleep, pts | 46.8 ± 7.4 | 19.4 | 62.5 |
| Frequent dreaming, pts | 52.5 ± 6.2 | 38.8 | 58.4 |
| Refreshing, pts | 53.2 ± 7.0 | 37.4 | 65.6 |
| Sleep length, pts | 48.3 ± 6.7 | 28.8 | 63.5 |
| OSA-MA total score, pts | 252.6 ± 25.4 | 197.4 | 303.8 |
| Habitual physical activity | |||
| Wear time, hour | 15.2 ± 1.4 | 11.8 | 18.3 |
| SB, hour (% of wear time) | 8.9 (58.2) | 5.0 | 12.7 |
| LPA, hour (% of wear time) | 5.3 (34.7) | 2.1 | 7.4 |
| MVPA, hour (% of wear time) | 1.1 (7.1) | 0.1 | 3.5 |
SD standard deviation, GDS Geriatric Depression Scale (Sheikh JI and Yesavage, 1986), WASO wake after sleep onset, N non-REM sleep stage, REM rapid eye movement, SB sedentary behavior, LPA low-intensity physical activity, MVPA moderate-vigorous-intensity physical activity. n = 92.
Figure 1.
Cumulative display of sleep architecture in all 92 participants. The percentage of participants in each sleep stage is shown for stages W (black), N1 (gray), N2 (light blue), N3 (blue), and R (red). W awake, R rapid eye movement sleep, N non-rapid eye movement sleep. A total of 587 polysomnography data points were clustered in 92 older adults.
Temporal associations between daytime physical activity and predicted sleep quality that night
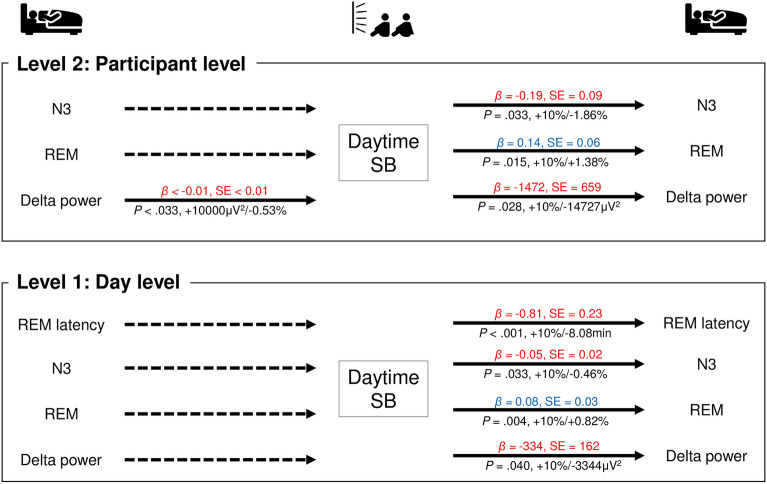
Same-day daytime sedentary behavior exhibited significant negative associations with REM latency (B = − 0.81, P < 0.001), stage N3 sleep (B = − 0.05, P = 0.033), and delta power (B = − 334.4, P = 0.040). Same-day daytime sedentary behavior also exhibited a significant positive association with REM sleep (B = 0.08, P = 0.004). As in the day-level analysis, analyses at the participant level indicated that daytime sedentary behavior was significantly and negatively associated with stage N3 sleep (B = − 0.19, P = 0.033) and delta power (B = − 1472.7, P = 0.028) that night. Daytime sedentary behavior also exhibited a significant positive association with REM sleep in the participant-level analysis (B = 0.14, P = 0.015) (Fig. 2, Supplementary Tables S1 and S2).
Figure 2.
Bidirectional associations between sleep parameters and sedentary behavior. Adjusted for age; sex; BMI; history of smoking, alcohol consumption, and caffeine consumption; and medical history of hypertension, hyperlipidemia, and depressive symptoms. SB sedentary behavior; the solid line represents significant relevance. A solid line on both sides indicates bidirectionally related parameters, and a solid line on one side and a dashed line on the other side indicate only temporally related parameters. Blue text indicates a positive relationship, and red text indicates a negative relationship.
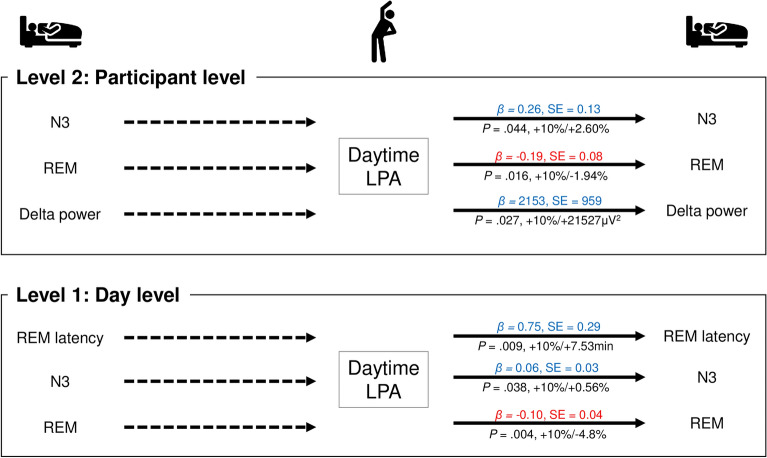
Same-day daytime low-intensity physical activity exhibited a significant positive association with nighttime REM latency (B = 0.75, P = 0.009) and stage N3 sleep (B = 0.06, P = 0.038), as well as a significant negative association with REM sleep (B = − 0.10, P = 0.004). In the participant-level analysis, daytime low-intensity physical activity exhibited a significant positive association with stage N3 sleep (B = 0.26, P = 0.044) and delta power (B = 2152.7, P = 0.027) at night, as well as a significant negative association with REM sleep (B = − 0.19, P = 0.016) (Fig. 3, Supplementary Tables S3 and S4).
Figure 3.
Bidirectional associations between sleep parameters and low-intensity physical activity. Adjusted for age; sex; BMI; history of smoking, alcohol consumption, and caffeine consumption; and medical history of hypertension, hyperlipidemia, and depressive symptoms. LPA low-intensity physical activity. The solid line represents significant relevance. A solid line on both sides indicates bidirectionally related parameters, and a solid line on one side and a dashed line on the other side indicate only temporally related parameters. Blue text indicates a positive relationship, and red text indicates a negative relationship.
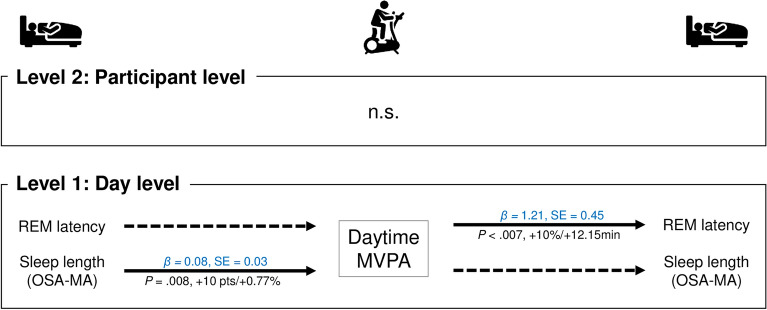
Same-day daytime moderate-to-vigorous-intensity physical activity was significantly and positively associated with nighttime REM latency (B = 1.21, P = 0.007). However, there were no significant associations of daytime moderate-to-vigorous-intensity physical activity at the participant level (Fig. 4, Supplementary Tables S5 and S6).
Figure 4.
Bidirectional associations between sleep parameters and moderate-to-vigorous-intensity physical activity. Adjusted for age; sex; BMI; history of smoking, alcohol consumption, and caffeine consumption; and medical history of hypertension, hyperlipidemia, and depressive symptoms. MVPA, moderate-to-vigorous-intensity physical activity. The solid line represents significant relevance. A solid line on both sides means that they are bidirectionally related parameters, and a solid line on one side and a dashed line on the other side means that they are only temporally related to each parameter. Blue text means a positive relationship, and red text means a negative relationship.
Temporal associations between nighttime sleep and predicted physical activity the next day
The participant-level delta power was significantly and negatively associated with daytime sedentary behavior (B < − 0.01, P = 0.033) (Fig. 2, Supplementary Table S7). Additionally, same-day subjective sleep duration was significantly and positively associated with daytime moderate-to-vigorous-intensity physical activity (B = 0.08, P = 0.008) (Fig. 4, Supplementary Table S8). However, there were no significant relationships between next-day physical activity and other sleep parameters (Figs. 2, 3, 4, Supplementary Tables S9–S21).
Discussion
In the present study, we examined the bidirectional associations between physical activity and both objective and subjective sleep quality in older adults. Our analysis revealed that the characteristics of stage N3 sleep were better among our participants than among those included in a previous epidemiological study28. In 80% of younger adults, changes in sleep structure related to stage N3 appear within approximately 1 h after falling asleep34; however, such changes occurred in only 20% of older adults in the current study (Fig. 1). Compared to American, Swiss, and Brazilian older adults, the Japanese participants showed short total time in bed; however, a similar sleep structure has been reported in older adults from other countries19,35,36. Overall, compared with the National Sleep Foundation’s sleep quality recommendations37, the participants seemed to be relatively healthy in terms of sleep composition.
Previous studies have focused on the bidirectional association between physical activity and sleep; however, these studies primarily assessed physical activity and/or sleep using subjective measures33,38,39, and most quantitative evaluations of sleep have been performed using actigraphy only22,23,26. These studies suggested qualitative assessment of sleep as a direction for future research22,24,40 and commonly mentioned that future studies should use polysomnography data for both qualitative and quantitative estimation24,33,41. Moreover, few studies have focused on the bidirectional association between daily physical activity and sleep in older adults23,26,41.
In the day-level analysis (level 1), we observed that 10% increase in daytime sedentary behavior was associated with 0.82% increase in REM sleep that night. Furthermore, the participant-level (level 2) analysis revealed that REM latency, stage N3 sleep, and delta power were lower by 8.08 min, 0.46%, and 3344.1 μV2, respectively (Fig. 2). However, when low-intensity physical activity during the daytime was higher by 10%, REM sleep duration was lower by 4.80%, and REM latency and the duration of stage N3 sleep were higher by 7.53 min and 0.56% at the day level (level 1), respectively (Fig. 3). In addition, when moderate-to-vigorous-intensity physical activity during daytime was higher by 10%, REM latency was lower by 12.15 min at the day level (level 1). Furthermore, for every 10-point increase in subjective sleep length, daytime moderate-to-vigorous-intensity physical activity during the next day was higher by 0.77% at the day level (level 1) (Fig. 4).
The participant-level (level 2) analysis indicated that higher levels of daytime sedentary behavior are negatively associated with deep sleep parameters (e.g., N3, delta power), while higher low-intensity physical activity during the daytime is positively associated with these parameters. These analyses also revealed that higher delta power during the prior day is negatively associated with daytime sedentary behavior the next day. These findings are in accordance with those of our previous study, which demonstrated that replacing 30 min of sedentary behavior per day with an equal period of low-intensity physical activity may favorably influence objective and subjective sleep parameters7. Furthermore, the positive associations between low-intensity physical activity and deep sleep parameters (N3 and delta power) in this study were based on complete polysomnography data.
Although we examined different sleep parameters using actigraphy, a previous study suggests that greater sleep efficiency and lower sleep fragmentation are related to greater levels of moderate-to-vigorous-intensity physical activity the following day23. The present study did not show significant differences in the relationship between moderate-to-vigorous-intensity physical activity that resulted in sleep efficiency (B = 0.02, P = 0.914 in Model 2; B = − 0.14, P = 0.084 in Model 1; Supplementary Table S5) and wake after sleep onset (B = − 0.89, P = 0.239 in Model 2; B = − 0.36, P = 0.314 in Model 1; Supplementary Table S5). In contrast to the objective sleep parameters, the subjectively long sleep length resulted in increased next-day moderate-vigorous-intensity physical activity (Fig. 4). Unfortunately, the underlying mechanism remains unclear, but depressive symptoms may mediate the relationship between good subjective sleep length and higher moderate-to-vigorous-intensity physical activity (e.g., exercise)42. Future studies should consider interventional designs to examine the effect of increasing subjective sleep length on moderate-to-vigorous-intensity physical activity.
Low-intensity aerobic exercise induces an increase in delta power during the first hour of sleep time when compared with sedentary behavior11. Although our previous study demonstrated that the same low-intensity level of housework could not induce delta oscillations during sleep among older adults, the current study suggests that higher levels of low-intensity physical activity during the daytime are associated with increases in delta power. Furthermore, combining low-intensity physical activity with social interaction has been found to increase the prevalence of slow-wave sleep43. Some researchers have postulated that engaging in low-intensity physical activity in the context of social relationships increases blood flow to the brain, improves neuronal function, and facilitates deep sleep6,43. These results suggest that, when compared with moderate-to-vigorous-intensity physical activity, low-intensity physical activity induces positive effects on deep sleep among older adults. Moreover, previous studies have argued for the effects of exercise duration (e.g., acute and chronic effects) on sleep quality27,44. This study suggests that low-intensity physical activity, including exercise, has both acute and chronic positive effects on sleep quality in older adults at both the participant and day levels.
Additionally, when compared with objective sleep parameters, sedentary behavior and the intensity of physical activity are associated with fewer predictive factors related to subjective sleep parameters (e.g., OSA-MA). As mentioned above, some studies have argued that there is a mismatch between subjective and objective sleep assessments, proposing that observation periods should last for at least 14 days to resolve these inconsistencies17,26.
Although the precise mechanisms underlying the relationship between sedentary behavior and sleep quality remain unclear, previous studies have demonstrated a negative correlation between sedentary behavior and total sleep time/sleep efficiency44,45. In addition, the results regarding the appropriate intensity of physical activity remain inconclusive. An epidemiological study has demonstrated that lower-intensity physical activity is better than moderate-to-vigorous-intensity physical activity for slowing or halting the degradation of sleep quality8. Our previous epidemiological study also indicated that physically active older adults with robust social networks have a lower prevalence of sleep disorders6. Low-intensity physical activity may be positively associated with social relationships since it often involves routine daily social activities, such as caring for grandchildren and walking while having a conversation with others46.
However, the present results show a contrary hypothesis that sedentary behavior is positively associated with REM sleep, while the opposite was observed for low-intensity physical activity. In terms of REM latency, sedentary behavior shifted REM sleep forward, while low- and moderate-to-vigorous-intensity physical activity delayed the onset of REM. One meta-analysis concluded that acute physical activity delays REM latency and decreases REM sleep duration, and these changes are the mechanism through which antidepressant treatments work47.
An individual’s discretionary time is limited to 24 h per day, meaning that each activity (e.g., sedentary behavior, low-intensity physical activity, moderate-to-vigorous-intensity physical activity, and sleep period) is mutually exclusive. Sedentary behavior and physical activity may exhibit an interdependent relationship with REM latency and REM sleep duration. Indeed, in the present study, REM sleep accounted for 23.3% of the total sleep time, which is similar to the proportion observed among younger people48.
The above-mentioned REM sleep among older adults was divided into the following categories: (1) Q1: < 14.8%; (2) Q2: 14.8–19.4%; (3) Q3: 19.5–23.6%; and (4) Q4: > 23.6%19. Notably, REM sleep is fundamentally different from non-REM sleep given that it is associated with a higher metabolic rate, higher heart rate, activation of the sympathetic nervous system, and patterns of global brain activity similar to those observed during wakefulness49,50. Indeed, the duration of REM sleep exhibited a significant negative correlation with the self-reported frequency of dreaming (r = − 0.211, P = 0.044) in this study. Furthermore, patients with depression exhibit early appearance of REM latency and a higher rate of REM sleep51, and REM sleep of ≥ 41% of the total sleep time indicates bad sleep quality among older adults37. Since human sleep time is also limited, the present study suggests that low-intensity physical activity could shift REM sleep to a deep N3 sleep stage, and both low- and moderate-to-vigorous-intensity physical activity could delay REM onset. There was also no significant association between depressive symptoms and REM latency or REM sleep in the current study (Supplementary Tables S1–S21). However, as this study included only healthy older adults, future studies should focus on patients with depression and/or insomnia.
The present study overcomes the limitations of previous studies using polysomnography; however, it has other limitations. First, this micro-longitudinal observational study was conducted during the coronavirus disease 2019 (COVID-19) pandemic. It is possible that restrictions on or avoidance of physical activity due to the COVID-19 pandemic affected physical activity patterns, although the levels of physical activity observed appear similar to those reported among US and Japanese older adults prior to the COVID-19 pandemic52,53. Second, a previous study reported that there are sex-based differences in sleep quality54. Additionally, we could not investigate the participants’ educational levels. Although our analyses were adjusted for sex and other potential confounders, future studies should focus on individual differences, including sex and education level. Moreover, a similar study has considered the weekday/weekend sleep patterns among students22. However, no significant differences were noted between the midpoint of sleep time on weekday and that on weekend (e.g., social jet lag) in the older adults in the present study (Supplementary Fig. S1). Third, the sample size was small, despite the use of objective data obtained using accelerometers and polysomnography. Fourth, as mentioned above, every physical activity has strong relevance to each other. Our previous study showed the influence of replacing sedentary behavior with engaging or other intensities of physical activities (e.g., low- and moderate-to-vigorous intensity physical activity) on sleep quality7. However, autocorrelation could not be considered in our study because there is multi-collinearity when multi-level analysis inserting the level 1 and level 2 variables of activities was undertaken. In addition, this study examined bidirectional associations in two separate models. Although our models tested two temporal directions (sedentary/physical activities to sleep that night, and sleep to next-day sedentary/physical activities), these associations are likely to be correlational. We do not yet know whether each variable (physical activity or sleep) is associated with change in the other. Future studies may need to use more rigorous models that control for the prior day’s behavior (physical activity and/or sleep). Finally, although we excluded participants who had taken sleeping medications, some patients in our study may have had obstructive sleep apnea despite a lack of subjective symptoms. To verify our results, future investigations with larger sample sizes in older adults are necessary.
In conclusion, our results suggest that there are bidirectionally negative associations between sedentary behavior and delta power at the participant level. Contrarily, more low-intensity physical activity during the daytime is associated with greater deep sleep. Moreover, longer subjective sleep length is associated with higher moderate-to-vigorous-intensity physical activity the next day. However, the number of parameters related to next-day physical activity predicted by sleep in the present study was fewer than in previous studies. Meanwhile, the results of the present study suggest that regardless of intensity, engaging in physical activity will increase REM latency, while low-intensity physical activity will increase deep sleep and decrease REM sleep in older adults.
Methods
Participants
This micro-longitudinal observational study was conducted from February to June 2021. A total of 112 older adults were recruited from January to May 2021 through advertisements and snowball sampling in Ibaraki Prefecture, Japan. The inclusion criteria were age over 65 years and having no restrictions on exercise as imposed by a physician. The participants were required to wear an accelerometer during the daytime for 7 consecutive days and to undergo polysomnography during the sleep period. In addition, to assess self-reported sleep quality, the participants were instructed to complete a detailed questionnaire after waking up for 7 consecutive days. For the assessment of usual daily physical activity and sleep habits, the participants were required to spend the day how they normally would have, and we did not control the total sleep time, bedtime, and awake time.
We excluded individuals who were taking sleeping medication (n = 7) and those who provided less than 3 days of paired accelerometer and polysomnography data (n = 13). Finally, daily physical activity and polysomnography data were analyzed for 92 participants (Table 1). Except for that in alcohol consumption, no significant differences were noted in the characteristics between the included and excluded participants (Supplementary Table S22). All participants provided written informed consent and were compensated with 4000 Japanese yen. This study was performed in accordance with the principles of the Declaration of Helsinki and the Ethics Committee of the University of Tsukuba approved this study (reference no. R02-211).
Measurements
Polysomnography assessment and self-reported sleep parameters
Objective daily sleep parameters were recorded using a wearable polysomnography device (Insomnograf K1; S’UIMIN Inc., Tokyo, Japan), which is light (162 g) and easy to attach and remove due to the soft sticking electrodes, making it easy to use in older adults. A pilot study found an 86.9% concordance rate and 0.80 kappa coefficient with a typical polysomnography device. Participants were instructed to attach electrodes to their head after showering and to push the record button immediately before going to bed and after waking up. The time to bed and last awakening in the morning were determined using these data. The participants pushed the power button or inserted the cable for charge, and the recording ended. We cross-checked the bedtime and wake-up time recorded by polysomnography and the self-reported questionnaires. The two instruments were used together to ensure that data were collected even in cases when participants forgot to push the button immediately after waking up. Although, some minor differences were noted in bedtime and waketime, there was a high correlation between the polysomnography and self-reported questionnaires on bedtime (r = 0.935, P < 0.001), waketime (r = 0.933, P < 0.001), and midpoint of sleep time (r = 0.967, P < 0.001).
This device’s recording system consisted of five electroencephalogram derivations (Fp1–M2, Fp2–M1, Fp1–average M, Fp2–average M, and Fp1–Fp2). The records were scored every 30 s to classify sleep stages as wakefulness (stage W); non-REM (stage N); N1, N2, and N3; and REM. Measurements during sleep onset latency were classified as stage W. Moreover, REM latency was measured until the first REM stage that appeared after sleep onset. Waking after sleep onset was defined according to standard criteria55. The Fp1 to average M recording was analyzed using discrete fast Fourier transform techniques, as previously described27. The total delta [0.75–4.00 Hz] power was calculated during non-REM sleep; the power content of the delta band was reported as a 5-s epoch of the sleep phase27 in μV2. We calculated the sum of delta power during the night because we could not control participants’ total sleep time in their home environment.
The Oguri–Shirakawa–Azumi sleep inventory, Middle-Aged and Aged version (OSA-MA) is a questionnaire designed to assess self-reported sleep quality the next morning56. The participants used a pen to write in a printed form due to the difficulty encountered by older adults in using and/or the absence of a smartphone. This questionnaire consists of bedtime/waketime and 16 components, each of which is graded into four levels (1–4 score) and divided into five categories: sleepiness on rising, initiation and maintenance of sleep, frequent dreaming, feeling refreshed, and sleep length. The sum of the scores for each category is used to determine the global score. Higher scores indicate better sleep quality. The reliability and reproducibility of the OSA-MA have been confirmed in a previous study56.
Daily sedentary behavior and intensity of physical activity
Sedentary behavior and physical activity were measured using a triaxial accelerometer (GT3X-BT; ActiGraph, Pensacola, FL). Participants wore an accelerometer on their waist during all waking hours, except when either changing clothes or bathing. Accelerometer data were collected at a sampling rate of 30 Hz, aggregated over 60-s intervals, and analyzed using ActiLife (version 6.13.4). The time spent not wearing the device (non-wearing time) was recorded at intervals of at least 60 consecutive minutes of zero counts. Wearing time was determined by subtracting the total non-wearing time from 24 h. Based on a previous study32, the count per minute (cpm) data were divided into three levels: (1) sedentary behavior (less than 50 cpm), (2) low-intensity physical activity (51–1040 cpm), and (3) moderate-to-vigorous-intensity physical activity (more than 1041 cpm)53,57. Days with over 10 h of wearing time were considered valid7.
Potential confounders
Based on previous studies58, we included age (continuous variable), sex (male or female), body mass index (BMI) (continuous variable), medical history (hypertension, hyperlipidemia; yes or no), caffeine consumption (daily or 1–6 times per week/less than 1–3 times per month), alcohol consumption (daily or 1–6 times per week/less than 1–3 times per month), tobacco smoking status (current or past/never), and depressive symptoms as confounders. Interviews and BMI assessments were conducted during the study visit by trained students. Depressive symptoms were assessed using the Japanese version of the 15-item Geriatric Depression Scale59 (continuous variable).
Temporal alignment of sleep and physical activity measures
To examine the bidirectional associations between sedentary/physical activities and sleep, we developed two datasets. First, when we tested temporal associations of sedentary/physical activities predicting that night’s sleep, the data set consisted of data on physical activity and sleep parameters of that day (587 daily observations were clustered from 92 older adults). Second, when we confirmed the temporal associations of each night’s sleep predicting the next day sedentary/physical activities, the data set consisted of sleep parameters coupled with the next day sedentary/physical activity data (489 daily observations were clustered within 92 older adults).
Statistical analysis
Multilevel models with lagged effects were analyzed using R software (R Foundation for Statistical Computing, Vienna, Austria). First, the precondition of the multilevel model analysis was a hierarchical model of all the variables. Thus, the null model was used to confirm the intra-class correlation (ICC) for all variables. The ICC was 0.36–0.83 through sedentary/physical activities and sleep variables (Table 2). We developed a two-level model to examine the associations between daily physical activity and nighttime sleep measures according to between-participant (participant level: level 2) and within-participant (day level: level 1) levels. The independent variables were centered at the sample mean for the between-participant variables, and the within-participant variables were centered at the person mean. Additionally, to investigate the bidirectional associations between daily physical activity and nighttime sleep measures, we used the two datasets mentioned above. Potential confounders were included in all models (Supplementary Tables S1–S21). Statistical significance was set at P < 0.05 (two-tailed test).
Table 2.
Null model without independent variables on objective sleep parameters.
| Variables | β Coefficients | |||
|---|---|---|---|---|
| Intercept | Within participant | Between participant | ICC | |
| Polysomnography | ||||
| Total sleep time, min | 373.8 | 2361.5 | 1582.2 | 0.40 |
| Sleep latency, min | 19.7 | 162.4 | 92.8 | 0.36 |
| Sleep efficiency, % | 81.4 | 48.6 | 30.5 | 0.39 |
| WASO, min | 68.1 | 889.4 | 781.4 | 0.47 |
| REM latency, min | 96.8 | 1371.1 | 969.8 | 0.41 |
| N1, % | 10.5 | 7.9 | 16.1 | 0.67 |
| N2, % | 58.3 | 25.7 | 44.6 | 0.63 |
| N3, % | 7.9 | 12.1 | 51.6 | 0.81 |
| REM, % | 23.3 | 20.5 | 13.3 | 0.39 |
| Sum of delta power, μV2/night | 115,386 | 678,567,863 | 2,891,874,440 | 0.83 |
| OSA-MA | ||||
| Sleepiness on rising, pts | 51.8 | 31.1 | 51.4 | 0.62 |
| Initiation and maintenance of sleep, pts | 46.8 | 65.4 | 44.4 | 0.40 |
| Frequent dreaming, pts | 52.5 | 44.3 | 31.7 | 0.42 |
| Refreshing, pts | 53.2 | 45.8 | 42.6 | 0.48 |
| Sleep length, pts | 48.3 | 48.8 | 38.1 | 0.44 |
| Total score, pts | 252.6 | 527.6 | 569.8 | 0.52 |
| Physical activity | ||||
| SB, % | 58.2 | 54.7 | 87.2 | 0.61 |
| LPA, % | 34.7 | 33.7 | 46.7 | 0.58 |
| MVPA, % | 7.1 | 16.1 | 20.2 | 0.56 |
ICC intraclass correlation coefficients, WASO wake after sleep onset, REM rapid eye movement, N non-REM sleep stage, OSA-MA Oguri–Shirakawa–Azumi sleep inventory, Middle-Aged and Aged version, SB sedentary behavior, LPA low-intensity physical activity, MVPA moderate-vigorous-intensity physical activity. 587 polysomnography data were clustered within 92 older adults.
Supplementary Information
Acknowledgements
The authors would like to thank Editage (http://www.editage.jp) for English language editing.
Author contributions
J.S., S.F., T.K., and T.O. designed research; J.S., J.L., and T.O. contributed to data collection; J.S., J.L. and I.P. analyzed data; J.S., and J.L. wrote the first draft of the paper; J.S., J.L., K.T., S.F., T.K., M.Y., and T.O. wrote the paper.
Funding
This work was supported by a grant from collaborative research between the University of Tsukuba and Toyota Motor Corporation, AMED (grand number: JP21zf0127005), JST-Mirai Program (grant number: JPMJMI19D8), JSPS KAKENHI (grant number: 21F21110), and the COI STREAM launched in 2013 by the Ministry of Education, Culture, Sports, Science and Technology (MEXT), the COI-NEXT (grant number: JPMJPF2017) launched in 2020 by the MEXT. The sponsors played no role in the preparation of the manuscript.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author (seol.jaehoon.ge@u.tsukuba.ac.jp) on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Jaehoon Seol and Jaehee Lee.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-19841-x.
References
- 1.Miner B, Kryger MH. Sleep in the aging population. Sleep Med. Clin. 2017;12:31–38. doi: 10.1016/j.jsmc.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Achttien RJ, van Lieshout J, Wensing M, Nijhuis-van der Sanden M, Staal JB. The decline in physical activity in aging people is not modified by gender or the presence of cardiovascular disease. Eur. J. Public Health. 2020;30:333–339. doi: 10.1093/eurpub/ckz159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang YC, et al. Social relationships and physiological determinants of longevity across the human life span. Proc. Natl Acad. Sci. U.S.A. 2016;113:578–583. doi: 10.1073/pnas.1511085112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee SL, et al. The association between loneliness and depressive symptoms among adults aged 50 years and older: A 12-year population-based cohort study. Lancet Psychiatry. 2021;8:48–57. doi: 10.1016/S2215-0366(20)30383-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel D, Steinberg J, Patel P. Insomnia in the elderly: A review. J. Clin. Sleep Med. 2018;14:1017–1024. doi: 10.5664/jcsm.7172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seol J, et al. Combined effect of daily physical activity and social relationships on sleep disorder among older adults: Cross-sectional and longitudinal study based on data from the Kasama study. BMC Geriatr. 2021;21:623. doi: 10.1186/s12877-021-02589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seol J, Abe T, Fujii Y, Joho K, Okura T. Effects of sedentary behavior and physical activity on sleep quality in older people: A cross-sectional study. Nurs. Health Sci. 2020;22:64–71. doi: 10.1111/nhs.12647. [DOI] [PubMed] [Google Scholar]
- 8.Tsunoda K, et al. Prospective study of physical activity and sleep in middle-aged and older adults. Am. J. Prev. Med. 2015;48:662–673. doi: 10.1016/j.amepre.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Bullock A, Kovacevic A, Kuhn T, Heisz JJ. Optimizing sleep in older adults: Where does high-intensity interval training fit? Front. Psychol. 2020;11:576316. doi: 10.3389/fpsyg.2020.576316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.King AC, et al. Effects of moderate-intensity exercise on polysomnographic and subjective sleep quality in older adults with mild to moderate sleep complaints. J. Gerontol. A Biol. Sci. Med. Sci. 2008;63:997–1004. doi: 10.1093/gerona/63.9.997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seol J, et al. Distinct effects of low-intensity physical activity in the evening on sleep quality in older women: A comparison of exercise and housework. Exp. Gerontol. 2021;143:111165. doi: 10.1016/j.exger.2020.111165. [DOI] [PubMed] [Google Scholar]
- 12.Zheng B, et al. Associations of domain-specific physical activities with insomnia symptoms among 0.5 million Chinese adults. J. Sleep Res. 2017;26:330–337. doi: 10.1111/jsr.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stutz J, Eiholzer R, Spengler CM. Effects of evening exercise on sleep in healthy participants: A systematic review and meta-analysis. Sports Med. 2019;49:269–287. doi: 10.1007/s40279-018-1015-0. [DOI] [PubMed] [Google Scholar]
- 14.St-Onge MP. The role of sleep duration in the regulation of energy balance: Effects on energy intakes and expenditure. J. Clin. Sleep Med. 2013;9:73–80. doi: 10.5664/jcsm.2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor AH, et al. Physical activity and older adults: A review of health benefits and the effectiveness of interventions. J. Sports Sci. 2004;22:703–725. doi: 10.1080/02640410410001712421. [DOI] [PubMed] [Google Scholar]
- 16.Zavecz Z, Nagy T, Galkó A, Nemeth D, Janacsek K. The relationship between subjective sleep quality and cognitive performance in healthy young adults: Evidence from three empirical studies. Sci. Rep. 2020;10:4855. doi: 10.1038/s41598-020-61627-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Landry GJ, Best JR, Liu-Ambrose T. Measuring sleep quality in older adults: A comparison using subjective and objective methods. Front. Aging Neurosci. 2015;7:166. doi: 10.3389/fnagi.2015.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Djonlagic I, et al. Macro and micro sleep architecture and cognitive performance in older adults. Nat. Hum. Behav. 2021;5:123–145. doi: 10.1038/s41562-020-00964-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leary EB, et al. Association of rapid eye movement sleep with mortality in middle-aged and older adults. JAMA Neurol. 2020;77:1241–1251. doi: 10.1001/jamaneurol.2020.2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vietheer A, Kiserud T, Lie RT, Haaland ØA, Kessler J. Sleep and physical activity from before conception to the end of pregnancy in healthy women: A longitudinal actigraphy study. Sleep Med. 2021;83:89–98. doi: 10.1016/j.sleep.2021.04.028. [DOI] [PubMed] [Google Scholar]
- 21.Reimers AK, Heidenreich V, Bittermann HJ, Knapp G, Reimers CD. Accelerometer-measured physical activity and its impact on sleep quality in patients suffering from restless legs syndrome. BMC Neurol. 2021;21:90. doi: 10.1186/s12883-021-02115-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Master L, et al. Bidirectional, daily temporal associations between sleep and physical activity in adolescents. Sci. Rep. 2019;9:7732. doi: 10.1038/s41598-019-44059-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lambiase MJ, Gabriel KP, Kuller LH, Matthews KA. Temporal relationships between physical activity and sleep in older women. Med. Sci. Sports Exerc. 2013;45:2362–2368. doi: 10.1249/MSS.0b013e31829e4cea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Plekhanova T, et al. Effect of exercise on sleep and bi-directional associations with accelerometer-assessed physical activity in men with obesity. Appl. Physiol. Nutr. Metab. 2021;46:597–605. doi: 10.1139/apnm-2020-0361. [DOI] [PubMed] [Google Scholar]
- 25.Lin Y, et al. Temporal and bi-directional associations between sleep duration and physical activity/sedentary time in children: An international comparison. Prev. Med. 2018;111:436–441. doi: 10.1016/j.ypmed.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Best JR, Falck RS, Landry GJ, Liu-Ambrose T. Analysis of dynamic, bidirectional associations in older adult physical activity and sleep quality. J. Sleep Res. 2019;28:e12769. doi: 10.1111/jsr.12769. [DOI] [PubMed] [Google Scholar]
- 27.Park I, et al. Exercise improves the quality of slow-wave sleep by increasing slow-wave stability. Sci. Rep. 2021;11:4410. doi: 10.1038/s41598-021-83817-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoon JE, et al. Sleep structure and electroencephalographic spectral power of middle-aged or older adults: Normative values by age and sex in the Korean population. J. Sleep Res. 2021;30:e13358. doi: 10.1111/jsr.13358. [DOI] [PubMed] [Google Scholar]
- 29.Thomas RJ, et al. Relationship between delta power and the electrocardiogram-derived cardiopulmonary spectrogram: Possible implications for assessing the effectiveness of sleep. Sleep Med. 2014;15:125–131. doi: 10.1016/j.sleep.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chauvette S, Volgushev M, Timofeev I. Origin of active states in local neocortical networks during slow sleep oscillation. Cereb. Cortex. 2010;20:2660–2674. doi: 10.1093/cercor/bhq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hof Zum Berge A, Kellmann M, Jakowski S. The first-night effect in elite sports: An initial glance on polysomnography in home-based settings. Front. Psychol. 2021;12:641451. doi: 10.3389/fpsyg.2021.641451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matsushita C, et al. Linkage of lower urinary tract symptoms to sleep quality in elderly men with nocturia: A community based study using home measured electroencephalogram data. J. Urol. 2017;197:204–209. doi: 10.1016/j.juro.2016.07.088. [DOI] [PubMed] [Google Scholar]
- 33.Kim Y, Umeda M, Lochbaum M, Sloan RA. Examining the day-to-day bidirectional associations between physical activity, sedentary behavior, screen time, and sleep health during school days in adolescents. PLoS One. 2020;15:e0238721. doi: 10.1371/journal.pone.0238721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang S, et al. Metabolic flexibility during sleep. Sci. Rep. 2021;11:17849. doi: 10.1038/s41598-021-97301-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lustenberger C, et al. Auditory deep sleep stimulation in older adults at home: A randomized crossover trial. Commun. Med. (Lond.) 2022;2:30. doi: 10.1038/s43856-022-00096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pires GN, et al. Sleep in older adults and its possible relations with COVID-19. Front. Aging Neurosci. 2021;13:647875. doi: 10.3389/fnagi.2021.647875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ohayon M, et al. National Sleep Foundation's sleep quality recommendations: First report. Sleep Health. 2017;3:6–19. doi: 10.1016/j.sleh.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 38.Huang BH, Hamer M, Duncan MJ, Cistulli PA, Stamatakis E. The bidirectional association between sleep and physical activity: A 6.9 years longitudinal analysis of 38,601 UK Biobank participants. Prev. Med. 2021;143:106315. doi: 10.1016/j.ypmed.2020.106315. [DOI] [PubMed] [Google Scholar]
- 39.Mesas AE, Hagen EW, Peppard PE. The bidirectional association between physical activity and sleep in middle-aged and older adults: A prospective study based on polysomnography. Sleep. 2018;41:zsy114. doi: 10.1093/sleep/zsy114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Madden KM, Ashe MC, Lockhart C, Chase JM. Sedentary behavior and sleep efficiency in active community-dwelling older adults. Sleep Sci. 2014;7:82–88. doi: 10.1016/j.slsci.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bruijel J, et al. The bidirectional relationship between sleep and physical activity following traumatic brain injury. J. Sleep Res. 2021;30:e13334. doi: 10.1111/jsr.13334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.De Wild-Hartmann JA, et al. Day-to-day associations between subjective sleep and affect in regard to future depression in a female population-based sample. Br. J. Psychiatry. 2013;202:407–412. doi: 10.1192/bjp.bp.112.123794. [DOI] [PubMed] [Google Scholar]
- 43.Naylor E, et al. Daily social and physical activity increases slow-wave sleep and daytime neuropsychological performance in the elderly. Sleep. 2000;23:87–95. doi: 10.1093/sleep/23.1.1f. [DOI] [PubMed] [Google Scholar]
- 44.Santos RV, Tufik S, De Mello MT. Exercise, sleep and cytokines: Is there a relation? Sleep Med. Rev. 2007;11:231–239. doi: 10.1016/j.smrv.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 45.Mochón-Benguigui S, Carneiro-Barrera A, Castillo MJ, Amaro-Gahete FJ. Role of physical activity and fitness on sleep in sedentary middle-aged adults: The FIT-AGEING study. Sci. Rep. 2021;11:539. doi: 10.1038/s41598-020-79355-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Varma VR, et al. Low-intensity walking activity is associated with better health. J. Appl. Gerontol. 2014;33:870–887. doi: 10.1177/0733464813512896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Youngstedt SD. Does exercise truly enhance sleep? Phys. Sports Med. 1997;25:72–82. doi: 10.3810/psm.1997.10.1473. [DOI] [PubMed] [Google Scholar]
- 48.Shrivastava D, Jung S, Saadat M, Sirohi R, Crewson K. How to interpret the results of a sleep study. J. Community Hosp. Intern. Med. Perspect. 2014;4:24983. doi: 10.3402/jchimp.v4.24983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kayaba M, et al. Energy metabolism differs between sleep stages and begins to increase prior to awakening. Metabolism. 2017;69:14–23. doi: 10.1016/j.metabol.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 50.Chouchou F, Desseilles M. Heart rate variability: A tool to explore the sleeping brain? Front. Neurosci. 2014;8:402. doi: 10.3389/fnins.2014.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Palagini L, Baglioni C, Ciapparelli A, Gemignani A, Riemann D. REM sleep dysregulation in depression: State of the art. Sleep Med. Rev. 2013;17:377–390. doi: 10.1016/j.smrv.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 52.Rosenberg D, et al. Device-assessed physical activity and sedentary behavior in a community-based cohort of older adults. BMC Public Health. 2020;20:1256. doi: 10.1186/s12889-020-09330-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nagata K, Fujii Y, Seol J, Monma T, Okura T. Associations of objectively measured sedentary behavior and physical activity with cognitive function among older Japanese adults: An isotemporal substitution model. Tairyoku Kagaku. 2021;70:149–156. doi: 10.7600/jspfsm.70.149. [DOI] [Google Scholar]
- 54.Jonasdottir SS, Minor K, Lehmann S. Gender differences in nighttime sleep patterns and variability across the adult lifespan: A global-scale wearables study. Sleep. 2021;44:zsaa169. doi: 10.1093/sleep/zsaa169. [DOI] [PubMed] [Google Scholar]
- 55.Berry RB, et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, version 2.4. American Academy of Sleep Medicine; 2017. [Google Scholar]
- 56.Yamamoto Y, et al. Standardization of revised version of OSA sleep inventory for middle age and aged. Brain Sci. Ment. Disord. 1999;10:401–409. [Google Scholar]
- 57.Copeland JL, Esliger DW. Accelerometer assessment of physical activity in active, healthy older adults. J. Aging Phys. Act. 2009;17:17–30. doi: 10.1123/japa.17.1.17. [DOI] [PubMed] [Google Scholar]
- 58.Ancoli-Israel S. Sleep and aging: prevalence of disturbed sleep and treatment considerations in older adults. J. Clin. Psychiatry. 2005;66:24–30. [PubMed] [Google Scholar]
- 59.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS) recent evidence and development of a shorter version. Clin. Gerontol. 1986;5:165–173. doi: 10.1300/J018v05n01_09. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author (seol.jaehoon.ge@u.tsukuba.ac.jp) on reasonable request.