Abstract
Objective:
This study had three goals: 1) to examine the association between racial discrimination and intimate partner violence (IPV) perpetration; 2) to determine whether this relationship is explained by mental health (MH) symptoms; and 3) to determine whether these associations vary by poverty status or gender.
Methods:
During the Wave 4 (2013-2017) visit of the Healthy Aging in Neighborhoods of Diversity Longitudinal Study (HANDLS), Black adults who were in a relationship (N = 433; mean age = 55.26, SD = 9.30; 51% men) provided self-report data on IPV perpetration; frequency of racial discrimination; and levels of anxiety, depression, and post-traumatic stress symptoms. Multi-group mediation models used these cross-sectional data to test whether racial discrimination was associated with MH symptoms, which in turn were associated with IPV perpetration, determining the significance of direct and indirect pathways and whether any pathways varied by poverty status or gender.
Results:
Racial discrimination was associated with more MH symptoms, which in turn was associated with IPV perpetration. The negative effect of discrimination on MH was stronger for Black women than Black men and for Black adults with household incomes below 125% of the Federal poverty line than those with incomes above this cutoff.
Discussion:
Efforts to prevent and treat IPV in the Black community should address the negative effects of racial discrimination experiences on mental health and partner aggression, especially among those with multiply marginalized identities. IPV prevention efforts may be enhanced through an overarching commitment to dismantle structural racism and intersectional forms of oppression.
Keywords: Racial discrimination, Intimate partner violence perpetration, Black/African American adults, mental health, poverty status, gender differences
Intimate partner violence (IPV) is a prevalent public health problem. However, it is understudied in the Black community. An early U.S. nationally representative study found that, in Black heterosexual relationships, 8% and 11% of females and males, respectively, reported beating their partner within the past year (Cazenave & Straus, 1979). Moreover, in a nationally representative sample of heterosexual couples, dyadic reports showed that 25% of Black couples were reporting IPV with 17% reporting mutual, 5% reporting female-to-male and 3% reporting male-to-female IPV (Caetano et al., 2008). Unfortunately, many nationally representative studies do not report IPV prevalence by race/ethnicity. This makes it difficult to have accurate estimates of prevalence within the Black community. Instead, many studies make relative comparisons, particularly to Whites, which may be misguided, especially given that these racial differences disappear when compared across similar contexts (Benson et al., 2004), and serves to further perpetuate stereotypes of Black individuals as violent. Nonetheless, the limited research on prevalence that does exist suggests that, as in other racial/ethnic communities, IPV is a public health problem within the Black community that merits further study and consideration.
To curb the perpetuation of harmful stereotypes, researchers have stated the importance of examining IPV within the Black community through a social ecological model that is specific to the Black experience in the U.S. (Powell, 2008; Hampton et al., 2003). To illustrate, although broader social ecological models of IPV state that social structures that maintain inequality (e.g., racism, classism, and sexism) can increase an individual’s risk for both IPV victimization (Heise, 1998) and perpetration (Centers for Disease Control and Prevention, 2015), these models are not specific to the Black experience and therefore do not detail the specific mechanisms that may be at play. On the other hand, Powell (2008) details numerous facets of racism and oppression, e.g., hate crimes, police brutality and discrimination, that coalesce to increase Black men’s risk of engaging in IPV against Black women. More specifically, Powell (2008) argues that it is the cumulative stressful and frustrating experience of these inequities and forms of oppression, which are experienced daily in nearly every facet of a Black person’s life (e.g., housing, education, and employment), that result in displaced anger and frustration against intimate partners. It follows that individuals with multiple marginalized identities (e.g., Black men living in poverty), would have greater accumulation of stress and frustration than others (e.g., Black men with more adequate financial standing) and would therefore be at greater risk for engaging in IPV.
Although most previous research and theoretical work has focused on male-perpetrated IPV, there are several important reasons to examine women’s use of partner violence as well. First and foremost, Black women, just like Black men, have an accumulation of stress and frustration and may potentially have a greater accumulation due to the multiple interlocking forms of oppression that they experience by virtue of being Black women, not just Black and women (Hill Collins, 2002; Crenshaw, 1991); therefore, like Black men, they may also be at an increased risk for engaging in IPV. More broadly, women engage in IPV at rates that are similar to, or slightly higher, than men (Archer, 2000). Second, although victims of male-perpetrated IPV, on average, incur more injuries and experience greater negative mental and physical health consequences than victims of female-perpetrated IPV (Black, 2011; Campbell, 2002), women’s IPV is also associated with negative mental health (MH) consequences for victims (Black et al., 2011; Tjaden & Thoennes, 2000). Finally, women’s use of IPV and its consequences may be different for individuals with multiple marginalized identities. For example, prior research has found that when Black women engage in IPV (compared to white women), it is more likely to occur in the context of mutual violence as opposed to unidirectional violence (Caetano et al., 2008). Some evidence indicates that mutual IPV is associated with greater risk of injury than unidirectional IPV (Whitaker et al., 2007).
Although researchers describe multiple factors that influence interpersonal violence in the Black community, the current study focuses on one factor, discrimination. Being the target of discrimination is one way oppressive social structures such as racism manifest at the individual level. Therefore, in understanding IPV in the Black community, racial discrimination, and the consequential negative MH symptoms associated with discrimination, may be especially salient. Furthermore, an intersectional lens suggests that the importance of these risk factors may depend on intersectional aspects of identity (Hill Collins, 2002; Crenshaw, 1991). Here, we focus on gender and SES as intersectional identities because they are commonly examined in the study of IPV.
Racial Discrimination as a Risk Factor for IPV Perpetration
Prior research, although limited, has identified racial discrimination as a potential risk factor for IPV perpetration among Black men age 18-65 (Reed et al., 2010), young Black women (Stueve & O’Donnell, 2008), and young Latino men and women (Forster et al., 2017). Reed and colleagues (2010) found that Black men, both U.S.-born and immigrants, who reported high levels of discrimination (above the median) were two times more likely than those who reported low levels of discrimination to engage in IPV perpetration. Reed and colleagues (2010) did not examine whether the association between discrimination and IPV perpetration varied by any of the SES indices included in their study, such as employment status, homelessness, or education level. Notably, the majority of Black men in that study who were recruited from urban community health centers were of lower SES (61% were unemployed, 22% were homeless, and 28% had less than a high school education) making it difficult to determine the generalizability of the results to Black men of less marginalized backgrounds. Stueve and O’Donnell (2008) also found that racial discrimination was associated with IPV perpetration among Black women. However, these studies examined only one gender, precluding comparisons across gender. Further research is needed to replicate the finding that discrimination is linked to increased risk for IPV among Black individuals in order to extend these findings to a broader range of Black people, including those with higher levels of education and SES, and to determine whether this association varies based on key intersectional factors including gender and poverty status.
Mental Health, Discrimination, and IPV
Although the limited research to date suggests that racial discrimination is a risk factor for IPV perpetration among minorities in the U.S., more work is also needed to examine the underlying mechanisms that may link racial discrimination to IPV perpetration. One key pathway may involve MH concerns that have been associated with both racial discrimination and IPV perpetration in past research. Previous studies have established a robust relationship between racial discrimination, a chronic stressor, and MH in ethnic minority populations. In a meta-analysis of cross-sectional studies, racial discrimination had significant associations, in the small-to-medium range of magnitude, with depressive symptoms, anxiety symptoms, and post-traumatic stress symptoms (PTSS) (Pascoe & Richman, 2009). In addition, experiences of racial discrimination have been shown to predict these MH outcomes more than one year later (Paradies et al., 2015). Although the association between racial discrimination and MH is well established, findings regarding gender differences in these associations are mixed, and little research has examined differences as a function of SES. Two meta-analyses found no gender differences in the association between racial discrimination and MH (including anxiety, depression, and PTSS) (Paradies et al., 2015; Pascoe & Richman, 2009). However, a third meta-analysis found a stronger association between racial discrimination and MH for women than men (Carter et al., 2019).
Moreover, although several studies include a poverty index (income and/or education), they typically control for this variable instead of examining it as a potential moderator (Paradies et al., 2015). One prior study examined differences in the relationship between racial discrimination and two MH outcomes (anxiety and depression) by gender and SES (i.e. parental educational attainment) in young Black adults (Neblett et al., 2016). Specifically, they found the strongest association between discrimination and anxiety among low SES Black men, followed by high SES Black women. There were no significant associations between discrimination and anxiety for the other two groups. In addition, although they found that discrimination was associated with depression, gender and SES did not moderate the association with depression.
The link between MH and IPV perpetration is also well established (Oram et al., 2014; Stith et al., 2004; Taft et al., 2011). Previous research on a nationally representative U.S. sample found that IPV perpetrators were more likely than non-perpetrators to have one or more diagnosable MH disorder, including, but not limited to, major depressive disorder (MDD), generalized anxiety disorder (GAD) and post-traumatic stress disorder (PTSD) (Okuda et al., 2015). Similarly, a summary of meta-analyses showed that IPV perpetration was associated with depression, anxiety, and PTSD as well as other MH conditions (Spencer et al., 2019).
Although the link between MH and IPV perpetration is well-established, there is mixed evidence on gender differences in this association and little or no research that examines differences by SES. For example, whereas some meta-analyses have found that there was a stronger relationship between MH (e.g. GAD, MDD and PTSD) and IPV perpetration among men than women (Oram et al., 2014; Taft et al., 2011), other meta-analyses have found no gender differences in these associations (Spencer et al., 2019). This discrepancy may be due to differences in methodologies, specifically, examining gender differences within specific MH conditions versus combining all MH conditions. Furthermore, although there are studies that examine SES in the context of IPV perpetration (e.g., Stith et al., 2004), to our knowledge, there are no studies that have compared the strength of the association between MH and IPV across SES. Therefore, it is important to examine the potential role of racial discrimination experiences and MH in IPV among Black individuals of different backgrounds.
Current Study
The current study builds on prior research that has identified racial discrimination as a potential risk factor for IPV perpetration in several ways. First, this study replicates earlier findings in an economically diverse sample of Black individuals living in urban neighborhoods. Second, unlike prior studies, both men and women are examined and compared. Finally, the current study expands on prior research by examining MH as a potential mechanism that may explain the links between experienced discrimination and IPV. In the current study, MH is assessed via anxiety symptoms, depressive symptoms and PTSS because these are common MH difficulties that have consistent and robust associations with both racial discrimination and IPV perpetration. Moreover, the current study examines whether any of the associations among racial discrimination, MH and IPV perpetration vary by poverty status or gender in urban-dwelling Black individuals.
The aims of the current study were to: 1) examine the association of racial discrimination with IPV perpetration; 2) determine whether this relationship can be explained by MH symptoms; and 3) determine whether these associations vary by poverty status or gender. Based on prior research, we predicted that: 1) racial discrimination will be positively associated with IPV perpetration; and 2) MH symptoms will mediate the relationship between racial discrimination and IPV perpetration. The hypotheses for the third aim were exploratory in nature. But, based on intersectional frameworks such as the doubly disadvantaged hypothesis (Dowd & Bengtson, 1978), which suggests that individuals with multiple marginalized identities experience poorer physical and mental health because they are exposed to multiple forms of discrimination, we hypothesized that the associations among racial discrimination, MH symptoms and IPV will be stronger for groups with intersectional identities of oppression (i.e. Black individuals living in poverty and Black women).
Method
Participants
This cross-sectional study used data from the Wave 4 (2013-2017) visit of the Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS). The current study was limited to cross-sectional analyses because the discrimination and IPV measures of interest were administered only at study Wave 4. Information on sample size determination, data exclusions, data manipulations, and measures included in the parent study is provided below. HANDLS (Evans et al., 2010) is a longitudinal investigation of health disparities in a cohort of 3,720 Non-Hispanic Black and Non-Hispanic white adults aged 30-64 ascertained through an area probability sample of Baltimore City, Maryland. The area probability sample was designed to recruit equally across 4 factors: 1) age via 7 five-year age groups between 30 and 64; 2) sex; 3) race (i.e., Black or white); and 4) SES, defined as either above or below 125% of the Federal poverty line for 2004. Participants for the current investigation were 433 Black participants who self-identified as currently married or partnered in Wave 4. Most participants (64%) had household incomes above the poverty line, which was determined at Wave 1, and approximately half (51%) were men. On average, participants were 55.26 years of age (SD = 9.30) and attained 12.6 years (SD = 2.64) of formal education.
Measures
Racial Discrimination
Racial discrimination was measured using the brief 17-item Perceived Ethnic Discrimination Questionnaire Community Version (Brief PEDQ-CV; Brondolo et al., 2005). On a 5-point scale from never (0) to very often (4), participants indicated how frequently they experienced each of 17 discrimination events due to their ethnicity or race (e.g., “how often have others hinted that you are dishonest or can’t be trusted because of your ethnicity or race?”). A sum score was created and had an observed range from 0 to 56. Seventy-eight participants (18%) were coded as missing because they did not provide valid responses for at least 75% of the PEDQ-CV items. This scale had excellent internal consistency (Cronbach’s α = .92).
Mental Health Symptoms
Anxiety symptoms.
Anxiety symptoms were measured using the 10-item Generalized Anxiety subscale from the Psychiatric Diagnostic Screening Questionnaire (PDSQ; Zimmerman & Mattia, 2001). Participants were asked whether they had experienced each of 10 anxiety symptoms during the past 6 months, e.g. “Did you worry a lot that bad things might happen to you or someone close to you?”. A sum score, which had an observed range from 0 to 10, was created for participants who provided valid responses to at least 75% of the items; 24 participants (6%) were coded as missing. The measure had good reliability (Cronbach’s α = .88).
Depressive symptoms.
Depressive symptoms were measured using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). Participants were asked how often they experienced each of the 20 depressive symptoms in the past week from rarely or not at all (less than one day) (0) to most or all of the time (5-7 days) (3), e.g. “I had crying spells”. A sum score, which had an observed range from 0 to 46, was created for participants who provided valid responses to at least 75% of the items; 11 participants (3%) were coded as missing. This measure had good reliability (Cronbach’s α = .86).
Post-traumatic stress symptoms.
Post-traumatic stress symptoms (PTSS) were measured using the 17-item PTSD Checklist (PCL; Blanchard et al., 1996) which maps onto the DSM-IV criteria for PTSD. Participants rated how much they were bothered by each symptom in the past month from not at all (1) to extremely (5), e.g., “repeated, disturbing dreams of a stressful experience from the past”. A sum score, which had an observed range from 17 to 70, was created for participants who provided valid responses to at least 75% of the items; 31 participants (7%) were coded as missing. This measure had excellent reliability (Cronbach’s α = .95)
Demographic Categories
Sex (i.e., male or female) and poverty status (i.e., household income above or below 125% of the federal poverty guideline), as determined at the wave 1 HANDLS visit, were used as demographic categories. These demographic categories were only assessed at wave 1. However, participants were asked to report their gender during wave 4. All the participants were cis-gendered and therefore the term “gender” as opposed to “sex” is used hereafter.
Intimate partner violence perpetration
The Conflict Tactics Scale Short-Form (CTS-SF; Straus & Douglas, 2004) was used to measure IPV perpetration (including psychological aggression, physical assault, injury, and sexual coercion). Participants answered two questions for how frequently (from “never” to “more than 20 times”) they perpetrated each form of IPV in the past year, e.g., “pushed, shoved or slapped,” and whether this had ever happened in the past for a total of 8 questions. Item responses were recoded to the midpoint of the frequency range for each response option, never (0), once (1), twice (2), three to five times (4), six to 10 times (8), 11 to 20 times (15), and more than 20 times (25). A total frequency score was computed. Because it was skewed and kurtotic (West et al., 1995), the frequency score was log-transformed after adding a constant of one. Participants who did not provide a valid response to at least 75% of the CTS2-SF items (n = 70, 16%) were coded as missing. Given the differing item variances, omega for the total scale was calculated (Dunn et al., 2014)
Data Analysis
The lavaan package (Rosseel, 2012) in R 3.6.1 (R Core Team, 2017) was used to obtain descriptive statistics and bivariate correlations; to test for measurement invariance; to test two separate multigroup mediation models in which racial discrimination predicts MH symptoms, which in turn predict IPV perpetration; and to determine whether the resulting pathway estimates varied by: 1) poverty status and 2) gender. Each background variable (poverty status or gender) was adjusted for in the model testing the other. MH symptoms were modeled as a latent construct with three observed indicators: anxiety symptoms, PTSS, and depressive symptoms (Figure 1). The indirect effects were tested using bootstrap 95% confidence intervals (CI) with 5,000 bootstrap samples. Maximum Likelihood was used to handle missing data (n = 70, 16%). Individuals who had missing data did not significantly differ from those with valid data on gender, poverty status, employment nor education level.
Figure 1.
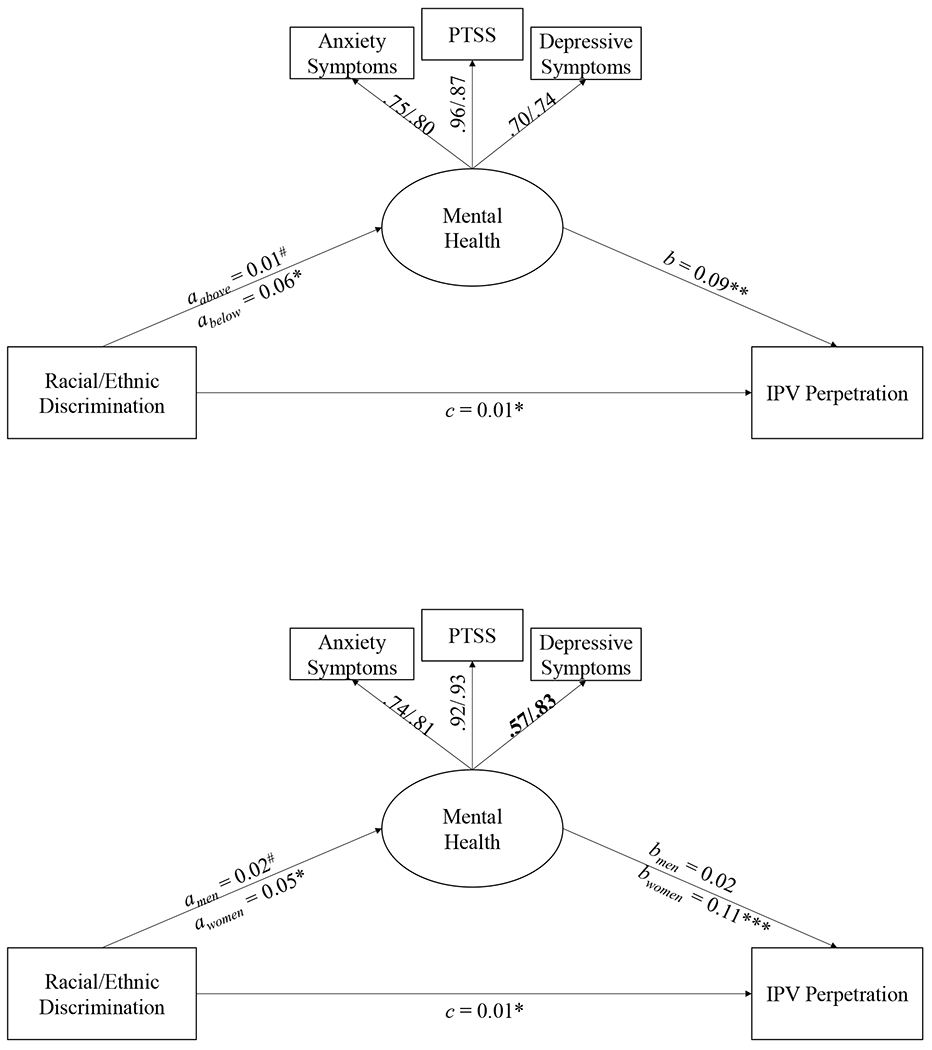
A. Structural Equation Model for Poverty Status
B. Structural Equation Model for Gender
Note. All pathways are adjusted for gender (Figure 1A) and poverty status (Figure 1B). PTSS = Post-traumatic stress symptoms. IPV = Intimate partner violence. In Figure 1B, the loadings for Black men are presented first followed by Black women. Note, only loadings for depressive symptoms vary significantly. All loadings were significant. Two separate standardized loadings are presented for depressive and PTSS due to different SE.
# p <.10. * p <.05. ** p < .01. *** p < .001.
Multigroup SEM was conducted only after establishing measurement invariance. To assess for invariance across poverty status and gender in both the measurement models and the structural models, we used the recommended guidelines of p > .05 for a chi-squared test of relative fit and ΔCFI < .01 (Cheung & Rensvold, 2002; Putnick & Bornstein, 2016). If these two indicators provided conflicting results, change in CFI was used because this metric is less biased by sample size than the chi-squared test. If invariance was violated, probing was then conducted to determine which loadings or path(s), if any, varied significantly at p < .05. To determine whether the structural equation models provided a good fit to the data, we used the following recommended cut-off values: CFI and TLI > 0.95, SRMR < 0.08 (Hu & Bentler, 1999), and RMSEA < 0.05 (Browne & Cudeck, 1992). Given the high correlations among IPV victimization and perpetration, we also provide additional models that further adjust for IPV victimization frequency scores, which were calculated as described for IPV perpetration except these scores were not log-transformed.
Given the cross-sectional nature of the data, we compared the fit of the current model, AIC = 6188.83 and BIC = 6226.48, to the fit of a reversed model, AIC = 8085.28 and BIC = 8122.93. Specifically, the current basic SEM model consisted of discrimination predicting mental health which in turn predicted IPV perpetration; the reversed model consisted of IPV perpetration predicting mental health which in turn predicted discrimination. We used Vuong’s non-nested Likelihood Ratio Test (Merkle et al., 2016) to compare the fit of these models and found that our current model had a significantly better fit than the reversed model, z = −40.43, p < .001, 95% CI of ΔAIC (1804.51, 1988.39) and 95% CI of ΔBIC (1804.51, 1988.39). Several models, including different order of variables and replacing IPV perpetration with IPV victimization, were tested (results not presented); however, all results revealed that the current model fit the data the best. The results of these tests, in tandem with theory, provide additional support for the current purported directionality of findings.
Data Availability
Per HHS requirements, HANDLS is registered with ClinicalTrials.gov: https://www.clinicaltrials.gov/ct2/show/NCT01323322?term=handls&draw=2&rank=1. Data are restricted but are available upon request due to ethical restrictions imposed by the National Institutes of Health Institutional Review Board. The IRB-approved consent forms that our study participants signed does not permit unrestricted public data sharing. However, it does permit data sharing through a Data Use Sharing Agreement. Data Use Sharing Agreements protect the privacy of human research participants and the confidentiality of their data. Our use of these agreements incorporates confidentiality standards to ensure data security at the agreement holder’s facility and prohibits manipulation of the data for the purpose of identifying study participants. The HANDLS website page labelled information for collaborators explains the process (https://handls.nih.gov/06Coll.htm). The contact for the study is our clinical study manager: Ms. Jennifer Norbeck, MSW, CCRC (norbeckje@grc.nia.nih.gov 410-558-8622). Analysis code in R is available upon request from the corresponding author.
Results
Sample Characteristics and Correlations
The majority of participants (71%) reported engaging in at least one form of IPV. Specifically, 70% reported engaging in psychological aggression, followed by physical assault (5%), injury (4%) and sexual coercion (4%). The majority of participants reported mutual IPV (68%) followed by no IPV (24%) and unidirectional IPV (8%). Based on the established cutoff of 16 or greater for the CES-D (Lewinsohn et al., 1997), 20% of participants were at risk for clinical depression. Similarly, 20% of participants had probable PTSD based on the established cutoff of 30 or greater among civilians in a community setting (Walker et al., 2002). Finally, based on the established cutoff of 7 or greater for the PDSQ (Zimmerman & Mattia, 2001), 11% of participants had probable generalized anxiety disorder.
On average, Black women reported significantly lower levels of racial discrimination, more depressive symptoms, and higher frequencies of IPV perpetration and victimization than Black men (Table 1). There were no other significant gender differences. On average, Black participants living below the poverty cutoff reported significantly higher levels of anxiety symptoms, depressive symptoms, and PTSS than those living above the poverty cutoff. Poverty status was not significantly associated with racial discrimination nor IPV. Further, racial discrimination was positively and significantly correlated with IPV, depressive symptoms, PTSS, but not with anxiety symptoms. Finally, the MH symptom scales were positively and significantly correlated with one another, and all three were positively and significantly correlated with IPV perpetration. Tables 2a and 2b report the bivariate correlations broken down by poverty status and gender, respectively.
Table 1.
Pairwise Bivariate Correlations and Descriptive Statistics of Overall Sample (N = 433)
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Gender | ||||||
| 2. Poverty Status | .05 | |||||
| 3. RD | − .28*** | −.05 | ||||
| 4. Anxiety symptoms | .07 | .14** | .09 | |||
| 5. Depressive symptoms | .10* | .15** | .16** | .55*** | ||
| 6. PTSS | .06 | .17*** | .14** | .73*** | .65*** | |
| 7. IPV perpetrationa | .17** | .02 | .11* | .20*** | .18*** | .20*** |
Note.
Variable was log-transformed after adding a constant of one.
Gender is coded as Women = 0 and Men = 1. Poverty status is coded as Above = 0 and Below = 1. RD = Racial discrimination. PTSS = Post-traumatic stress symptoms. IPV = Intimate partner violence.
p < .05.
p < .01.
p < .001.
Table 2a.
Pairwise Bivariate Correlations and Descriptive Statistics by Poverty Status
| 1 | 2 | 3 | 4 | 5 | M | SD | |
|---|---|---|---|---|---|---|---|
| 1. RD |
|
.05 | .13 | .07 | .07 | 7.65 | 9.33 |
| 2. Anxiety symptoms | .19* |
|
.54*** | .71*** | .27** | 1.72 | 2.55 |
| 3. Depressive symptoms | .26** | .54*** |
|
.69*** | .15* | 10.78 | 8.62 |
| 4. PTSS | .30*** | .75*** | .60*** |
|
.26*** | 23.38 | 25.45 |
| 5. IPV perpetrationa | .20* | .08 | .23* | .14 |
|
0.55 | 0.46 |
|
|
|||||||
| M | 6.71 | 2.51 | 13.67 | 27.00 | 0.58 | ||
| SD | 8.12 | 3.07 | 9.82 | 29.64 | 0.49 | ||
Note.
Variable was log-transformed after adding a constant of one.
The upper half and lower half of the matrix report data for Black participants living above (N = 235) and below (N = 119) poverty, respectively. RD = Racial discrimination. PTSS = Post-traumatic stress symptoms. IPV = Intimate partner violence.
p < .05.
p < .01.
p < .001.
Table 2b.
Pairwise Bivariate Correlations and Descriptives by Gender
| 1 | 2 | 3 | 4 | 5 | M | SD | |
|---|---|---|---|---|---|---|---|
| 1. RD |
|
.12 | .17* | .12 | .16* | 9.77 | 10.18 |
| 2. Anxiety symptoms | .12 |
|
.41*** | .71*** | .07 | 1.81 | 2.62 |
| 3. Depressive symptoms | .22** | .65*** |
|
.51*** | .09 | 10.88 | 8.41 |
| 4. PTSS | .26*** | .74*** | .74*** |
|
.01 | 24.05 | 26.23 |
| 5. IPV perpetrationa | .18* | .29*** | .24** | .33*** |
|
0.48 | 0.45 |
|
|
|||||||
| M | 4.85 | 2.19 | 12.69 | 25.22 | 0.64 | ||
| SD | 6.64 | 2.89 | 9.77 | 28.15 | 0.49 | ||
Note.
Variable was log-transformed after adding a constant of one.
The upper half and lower half of the matrix report data for Black men (N = 179) and women (N = 175), respectively. RD = Racial discrimination. PTSS = Post-traumatic stress symptoms. IPV = Intimate partner violence.
p < .05.
p < .01.
p < .001.
Measurement Invariance
To ensure that the groups could be compared across poverty status, measurement invariance was tested on the MH construct via confirmatory factor analysis (CFA). First, configural invariance was confirmed by imposing the same factor structure on both groups with factor loadings free to vary across groups. Next, weak invariance was tested by constraining factor loadings to be equal across groups. Although the results suggested that at least one of the loadings varied across poverty status (Δχ2[2, N = 433] = 6.33, p = .042), the change in CFI suggested that the difference between the configural invariance model and the weak invariance model was not meaningful, ΔCFI = .008. Therefore, measurement invariance for the MH construct was assumed across poverty status, and no further analyses were conducted to isolate differential factor loadings.
Applying the same steps to examine measurement invariance across gender, configural invariance was confirmed. However, weak invariance was not supported, Δχ2(2, N = 433) = 7.58, p = .023; ΔCFI = .011. Together, these findings suggested that at least one loading varied in a meaningful way across gender. Tests of partial weak invariance models revealed that only the depression factor loaded differently across gender groups, Δχ2(1, N = 433) = 7.45, p = .006. Therefore, a partial weak invariance model in which depression was allowed to vary across gender was used for subsequent analyses.
Structural Equation Modeling
Poverty Status
Figure 1A displays the multigroup mediational model results for poverty status adjusting for gender. Two models were compared: one in which all 3 pathways were constrained to be equal across poverty status and one in which the pathways were allowed to vary freely. The comparative fit results revealed that the models were significantly different, Δχ2(3, N = 433) = 9.89, p = .020. Further testing revealed that only path a, between racial discrimination and MH symptoms, varied significantly across poverty status, Δχ2(1, N = 433) = 6.48, p = .011.
The final model for poverty status, in which path a was allowed to vary, and all pathways were adjusted for gender, had excellent fit, CFI = .99, TLI = .99, RMSEA = .04, SRMR = .04. Higher levels of racial discrimination were associated with poorer MH only among Black participants with household incomes below the poverty cutoff, b = 0.06, z = 2.05, p = .040, than for those above the cutoff, b = 0.01, z = 1.86, p = .063. Next, regardless of poverty status, poorer MH was associated with higher frequencies of IPV perpetration, b = 0.09, z = 3.13, p = .002. Finally, racial discrimination was positively associated with IPV perpetration after adjusting for MH symptoms, b = 0.01, z = 2.06, p = .040. Overall, the indirect effect of racial discrimination on IPV perpetration was significant for Black participants living below the poverty cutoff, ab = 0.0048, 95% CI (0.0011, 0.0117), and for those living above the cutoff, ab = 0.0011, 95% CI (0.0002, 0.0031). Notably, after adjusting for victimization frequency, the associations of mental health and discrimination with IPV perpetration became non-significant. However, it is important to note that the fit notably worsened (CFI = .92, TLI = .88, RMSEA = .11 and SRMR = .10) and the strong correlation among perpetration and victimization partials out a large amount of variance, leaving little to be explained by other predictor variables.
Gender
Figure 1B displays the multigroup mediational model results for gender adjusting for poverty status. Two models were compared: one in which all 3 pathways were constrained to be equal across gender and one in which the pathways were allowed to vary freely. The comparative fit results revealed a significant difference in the models, Δχ2(3, N = 433) = 9.28, p = .026. Therefore, tests of pathway differences across gender were conducted. Further testing revealed that path a, between racial discrimination and MH symptoms, varied significantly across poverty status, Δχ2(1, N = 433) = 4.42, p = .036, as did path b, between MH symptoms and IPV perpetration, Δχ2(1, N = 433) = 4.60, p = .032.
The final model for gender had excellent fit, CFI = 1.00, TLI = 1.00, RMSEA = .00, SRMR = .03. First, higher levels of racial discrimination were associated with poorer only among Black women, b = 0.05, z = 2.31, p = .021; this association was non-significant for Black men, b = 0.02, z = 1.82, p = .068. A similar gender pattern was observed for the association between MH symptoms and IPV perpetration. Among Black women, more MH symptoms were associated with higher frequencies of IPV perpetration, b = 0.11, z = 3.44, p = .001; however, among Black men this association was non-significant, b = 0.02, z = 0.49, p = .624. Finally, racial discrimination was positively associated with IPV perpetration after adjusting for MH symptoms, b = 0.01, z = 2.16, p = .030. Overall, the indirect effect of racial discrimination on IPV perpetration was significant only for Black women, ab = 0.0055, 95% CI (0.0017, 0.0118), and not for Black men, ab = 0.0003, 95% CI (−0.0007, 0.0025). Notably, after adjusting for victimization frequency, the associations of mental health and discrimination with IPV perpetration became non-significant. However, it is important to note that the fit notably worsened (CFI = .95, TLI = .92, RMSEA = .09 and SRMR = .08) and the strong correlation among perpetration and victimization partials out a large amount of variance, leaving little to be explained by other predictor variables.
Discussion
The current study employed multi-group structural equation modeling to examine the association between racial discrimination and IPV perpetration (i.e. engaging in psychological aggression, physical assault, injury, or sexual coercion) in a community sample of middle-aged Black adults in a relationship, including whether this association can be explained by MH symptoms (depressive symptoms, anxiety symptoms and post-traumatic stress symptoms), and whether those associations vary by poverty status or gender. Regarding generalizability, the current sample has mental health symptomatology comparable to other community samples of Black adults (Davis et al., 2008; Long Foley et al., 2002; Williams et al., 2007). The rates of psychological aggression victimization in the current sample of Black urban adults (72% in the past year) were much higher than a nationally representative sample of U.S. adults (14% in past year) (Smith et al., 2017). However, the rates of physical violence and sexual coercion (11%) were similar (9.4%; 95% CI [7.8,11.3]) to nationally representative sample of Black adults (Smith et al., 2017).
Our descriptive findings showed that mutual violence was more common than unidirectional violence. In addition, IPV perpetration rates were different across gender, with Black women reporting higher rates than men. These rates did not differ across poverty status. It is important to consider the present findings in light of prior research has found that men, compared to women, tend to underreport their self-reported perpetration, particularly for severe violence (Stets & Straus, 1990). Consistent with prior research, the results indicate that greater experienced racial discrimination is associated with higher levels of MH symptoms (including depression, anxiety, and PTSS; Pascoe & Richman, 2009; Paradies et al., 2015). Moreover, as expected, poorer MH was associated with increased risk for IPV perpetration, which is consistent with previous research that has established a robust relationship between MH and IPV perpetration in both men and women (Spencer et al., 2019). Contrary to our hypothesis and previous research (Reed et al., 2010), experienced racial discrimination was not significantly correlated with IPV perpetration in simple bivariate analyses, and no significant direct effect between discrimination and IPV was present in model tests that included MH symptoms. However, after adjusting for sociodemographic factors, there was a significant indirect effect of discrimination on IPV perpetration via MH symptoms. This finding is consistent with recent studies using a nationally representative sample which have found that MH symptoms explain the association between experiences of sexist discrimination and use of physical IPV by women (Miles-McLean, Maldonado & Murphy, 2021) and the association between experiences of racial discrimination and use of physical IPV among US-born and immigrant Latino men (Maldonado, Cunradi & Nápoles, 2020). Together, these studies suggest that various forms of discrimination increase risk for IPV by operating as chronic stressors that contribute to MH symptoms.
A recent study by Sutton and colleagues (2019) indicates that the link between racial discrimination experiences and IPV may also involve more specific cognitive and emotional mechanisms. Using longitudinal data, they found that racial discrimination experienced in adolescence was indirectly linked to IPV perpetration in young adulthood through anger and hostile attribution biases reflecting appraisals of others as malicious. Their model explained nearly 18% of the variance in IPV perpetration, indicating that at a substantial portion of IPV perpetration that occurs among Black men can be explained by surviving racial discrimination.
Although the overall pattern of findings (direction and significance) in the current study was the same for all participants, the strength of the relationships between discrimination and MH varied by poverty status and gender. Groups with intersectional identities of oppression (i.e., Black participants with incomes below a poverty threshold cutoff and Black women) had a stronger association between racial discrimination and MH. The gender difference finding in the current study is consistent with previous research that has found that racial discrimination and everyday discrimination were more strongly associated with depressive symptoms and anxiety symptoms in Black women than Black men (Banks et al., 2006; Borrell et al., 2006). Moreover, these findings are consistent with a meta-analysis that found a stronger relationship between racial discrimination and MH among women than men (Carter et al., 2019), yet are inconsistent with two other meta-analyses that found no gender differences in the association between racial discrimination and MH (Paradies et al., 2015; Pascoe & Richman, 2009). The gender differences in the present model may be explained by the fact that women tend to express more internalizing symptoms, which were the focus of the MH assessment in the current study, whereas men tend to express more externalizing symptoms (Tolin & Foa, 2008). It may also be due to additional social vulnerabilities that women are exposed to, such as sexist discrimination and gender-related trauma (McLean & Anderson, 2009).
The finding that Black participants living below a poverty threshold, defined in HANDLS as 125% of the federal poverty level, had a stronger association between discrimination and MH than those living above this poverty threshold is consistent with a study that found that income moderated the effect of racial discrimination on self-rated MH, such that the relationship between these variables was stronger for Black women with lower, versus higher, incomes (Borrell et al., 2006). However, no differences by income were observed in Black men in that prior study. Furthermore, the current findings are consistent with another study that found that the effect of racial discrimination on anxiety was stronger for Black men of lower SES than those of higher SES (Neblett et al., 2016). However, the opposite pattern was found for Black women, with stronger effects of racial discrimination observed among those with higher SES than for those with lower SES. These mixed findings based on SES and gender indicate that further research with intersectional approaches is needed to elucidate the effects of experienced racial discrimination on MH among individuals with multiple marginalized and intersecting identities.
Taken as a whole, the current findings examining the associations between racial discrimination and MH by race and gender provide support for intersectional approaches (Beal, 2008; Hill Collins, 2002; King, 1988) and related research (Grollman, 2014). That is, the impact of racial discrimination on mental health is stronger among individuals with multiple marginalized identities (e.g., Black women). This may be due to the fact that multiple marginalized identities can be associated with a greater accumulation of stressors, in addition to discrimination and other forms of oppression, that further increase an individual’s vulnerability to mental health problems. Individuals with multiple marginalized identities are more likely than their more privileged counterparts to be exposed to adversities and are less likely to have access to resources to help mitigate the negative effects of these adversities. To illustrate, Black people living in poverty experience racism like wealthy Black people, but also require additional mental health resources to cope with the stressors that inherent in poverty, e.g., financial instability. Furthermore, the types of adversities experienced by individuals with multiple marginalized identities, particularly intersecting forms, e.g., sexualized racism, are different and, as such, may affect mental health differently (Cardyn, 2002). In brief, the present results suggest that multiple marginalized identities confer greater risk for negative MH outcomes associated with racial discrimination. This increased risk for negative MH outcomes in individuals with multiple marginalized identities suggests that they are in turn at an increased risk for IPV perpetration.
Limitations
The present study has several limitations. First, the models test the hypothesis that part of the reason individuals engage in IPV is due to the stress caused by discrimination, which leads to MH symptoms, and in turn increases risk for engaging in IPV. Nevertheless, because the study is cross-sectional, it is difficult to discern the direction of effects. It is possible that poor MH may increase the perception of discrimination given that individuals with MH conditions such as depression exhibit tendencies toward negative attributions of situations. However, prior longitudinal studies have shown that discrimination leads to more MH symptoms (Paradies et al., 2015). Despite this evidence, more longitudinal research is needed to confirm the implied directionality of the current models, particularly with respect to the prediction of IPV. The tests of non-nested models suggested that our purported directionality among our variables of interest were sound.
Importantly, the link between MH and IPV perpetration may exist, in part, because of the link between MH and IPV victimization and the interdependence of perpetration with victimization. When IPV victimization was included as a covariate in both models, the associations of mental health and discrimination with IPV perpetration became non-significant. Therefore, the current findings should be interpreted with caution. However, it is important to note that the fit notably worsened when victimization was included, suggesting that our current model fits the data better than analyses that included victimization. Due to the limited cross-sectional nature of self-report data, we were unable to fully disentangle these confounding relationships; dyadic data would be most appropriate. Similarly, as in any self-report measure the accuracy of self-reports, particularly, for undesirable behaviors comes into question, especially compared to partner’s reports. Although dyadic data is considered to provide a more complete assessment of IPV, self-report is also frequently used in the literature.
Another limitation of the current study is lack of data on the racial identity of participants’ relationship partners. Data from partners and on sociodemographic characteristics of partners (e.g., race) were not collected. It is possible that the effect of discrimination on IPV may differ based on the partner’s racial identity. For example, dynamics in interracial couples, including a White partner’s racial prejudices, may exacerbate the impact of racial discrimination on IPV. Future research should consider whether this relationship differs in interracial couples compared to same-race couples.
Next, the present analyses only looked at the intersection of race with two additional marginalized identities (poverty status and gender) and did not include the interaction of these two additional identities, which would have required comparisons across 4 groups (Black women and men with incomes above and below the poverty threshold). However, these analyses were not presented due to sample size considerations and because preliminary analyses revealed measurement variance in the MH latent construct across these 4 groups which violated the invariance assumption for multigroup structural equation modeling.
Further, the current models examine only one form of discrimination. It is possible that other experiences, including discrimination based on sex/gender, sexual orientation, or disability status, may have additive or interactive effects in combination with racial discrimination that influence MH and IPV risk. Indeed, multiple forms of discrimination have been found to partially explain the link between multiple marginalized identities and negative health outcomes (Grollman, 2014). In addition, future research should also examine different aspects of anti-Black racism and other race-related traumas and stressors. Racism is multi-level, interpersonal, structural, and multi-faceted (Clark et al., 1999). The experience of racism can vary in frequency, intensity, and severity. Common examples include daily microaggressions, experiences of discrimination in housing, education, and employment settings, racist depictions and language in media and popular culture, and collective experiences of racism at the community level, both historical and current (Harrell, 2000). It may be particularly important for future research to examine the impact of both interpersonal and structural forms of racism on IPV perpetration, as these distinctions may inform prevention and intervention efforts.
Furthermore, the current study was unable to explore other relevant sequelae of discrimination. One such relevant factor is substance use. There is robust evidence that racial discrimination is associated with substance use (Carter et al., 2019). For example, racial discrimination has been shown to predict alcohol use over time through an indirect path involving depression and anxiety (English et al., 2018). Moreover, substance use is associated with increased risk for engaging in IPV (Cafferky et al., 2018). Unfortunately, data available on the epidemiological sample analyzed in the current study were insufficient to examine the frequency or intensity of substance use, or the presence of substance use prior to specific acts of IPV, thus precluding a focus on this important variable. Another relevant factor for IPV perpetration that may occur following an experience of discrimination is anger, which is a known risk factor for IPV (Birkley & Eckhardt, 2015; Sutton et al., 2019). Anger is a common emotion that occurs following a stressful life event such as surviving racist acts. Although it is normal to feel anger, some research suggests that anger in the context of discrimination contributes to psychological distress and MH symptoms (Head & Seaborn Thompson, 2017; Pittman, 2011).
Finally, the community sample of middle-aged individuals in the current study is not a population that is traditionally considered to be at high-risk for engaging in IPV. As such, the generalizability of the findings to clinical samples, for example those receiving services at domestic violence agencies, is limited. However, researchers should still consider the role of discrimination and other race-based stressors, including race-based trauma (Carter, 2007), as potential risk factors for future violence in racial minority clinical populations.
Implications
Anti-Black racism manifests in a variety of ways. Racial discrimination is an interpersonal manifestation of anti-Black racism that merits consideration in the therapeutic treatment of Black people. Clinicians treating Black clients who present with internalizing symptoms, such as depression and anxiety, should be mindful that discrimination (among other race-related traumas and stressors) may be contributing to and exacerbating these MH conditions (Williams et al., 2019; Williams & Mohammed, 2009). In fact, pervasive or severe racial discrimination may be experienced as traumatic by some individuals (Chou et al., 2012) who may have clinical presentations similar to PTSD as a function of race-based traumatic stress (Carter, 2007). Our findings suggest that clients with multiple marginalized identities (e.g., Black clients living in poverty and Black women) may be particularly vulnerable to the negative effects of discrimination. Therefore, in addition to assessing racial discrimination, clinicians should assess other racial stressors and forms of discrimination, should consider this information in case formulations, and should provide treatment that is sensitive and responsive to these experiences.
In recognition of the devastating impact that anti-Black racism can have on the MH of Black people, clinical models have been developed to treat racial trauma and other race-related stressors (Bryant-Davis & Ocampo, 2006; Comas-Diaz, 2007; Dunbar, 2001). These models parallel PTSD treatments, while integrating racial trauma approaches. For instance, Comas-Diaz (2007) takes an ethnopolitical approach to treating race-related stress and trauma focused on “[decolonizing] people of color, [reformulating] their ethnic identity, and [promoting] racial reconciliation, personal transformation and sociopolitical change” (Comas-Diaz, 2016, pg. 254).
The findings may also have implications for treatment of individuals who have IPV as a presenting clinical problem. Specifically, programs or providers who serve Black individuals or members of other marginalized communities who have IPV as a presenting concern may have experienced exposure to chronic racial stressors, traumatic experiences, and other community factors that increase their risk to engage in IPV (Murphy et al., 2021; Williams, 1998). In recognition of these concerns, providers working with Black clients who use IPV in their relationships should be aware of how racial stressors and experiences of oppression may increase risk for IPV at the community level and may need to address these experiences directly in their intervention.
Furthermore, considering the fact that Black women had slightly higher rates of IPV perpetration than Black men, it is important to examine the multiplicative effects of racial stressors with sexist discrimination and gender-based traumas on their use of relationship aggression. These forms of oppression may interact and lead to greater MH symptoms (Grollman, 2014) which in turn may increase risk for engaging in IPV (Spencer et al., 2019). Notably, in the current study, we were unable to determine who initiated IPV, the motives for it, and whether IPV was done in self-defense. Although relationship dynamics play an important role in IPV, it is clear that there are other stressors that women face, outside the relationship, which may increase their own risk for engaging in these behaviors.
As mentioned, anti-Black racism is chronic and pervasive by nature. However, because it has been present the U.S. since chattel slavery, Black communities have created resources to help process and cope with anti-Black racism, including racial pride, religious/spiritual coping, and social and community supports (Brondolo et al., 2009; Carter, 2007; Utsey et al., 2008). Therefore, clinicians working with clients who are processing discriminatory experiences should assess clients’ access to these and other key resources and encourage clients to utilize and benefit from these resources. In terms of research, more studies are needed to identify these culturally relevant resources and strategies and determine the extent to which they can help alleviate the impact of anti-Black racism on MH and partner-aggressive behavior. However, attention must not only focus on helping Black people cope with discrimination and its effects on mental health, but also on eliminating the underlying sources of racial discrimination. Efforts to dismantle all forms anti-Black racism, including microaggressions, discriminatory practices, and the white supremacy that upholds such acts, remain the primary pathway towards alleviating racial health disparities in IPV.
Public health significance.
The current study indicates that racial discrimination is a risk factor for intimate partner violence perpetration among Black individuals living in urban neighborhoods due to its association with mental health symptoms (anxiety, depression, and PTSD). These associations are strongest for those with multiple marginalized identities, specifically Black women and those living in poverty.
Acknowledgments
This research was supported in part by the Intramural Research Program of the National Institutes of Health. The contents and views in this manuscript are those of the authors and should not be construed to represent the views of the National Institutes of Health. Data are restricted to available upon request due to ethical restrictions imposed by the National Institutes of Health Institutional Review Board. The HANDLS website page labelled information for collaborators explains the process for obtaining the data (https://handls.nih.gov/06Coll.htm). The contact for the study is our clinical study manager: Ms Jennifer Norbeck, MSW, CCRC (norbeckje@grc.nia.nih.gov 410-558-8622). Per HHS requirements, HANDLS is registered with ClinicalTrials.gov: https://www.clinicaltrials.gov/ct2/show/NCT01323322?term=handls&draw=2&rank=1. Analysis code in R is available upon request from the corresponding author.
Footnotes
All authors declare that they have no conflicts of interest.
References
- Archer J (2000). Sex differences in aggression between heterosexual partners: a meta-analytic review. Psychological Bulletin, 126(5), 651–680. 10.1037/0033-2909.126.5.651 [DOI] [PubMed] [Google Scholar]
- Banks KH, Kohn-Wood LP, & Spencer M (2006). An examination of the African American experience of everyday discrimination and symptoms of psychological distress. Community Mental Health Journal, 42(6), 555–570. 10.1007/s10597-006-9052-9 [DOI] [PubMed] [Google Scholar]
- Beal FM (2008). Double Jeopardy: To Be Black and Female. Meridians, 8(2), 166–176. 10.2979/mer.2008.8.2.166 [DOI] [Google Scholar]
- Birkley EL, & Eckhardt CI (2015). Anger, hostility, internalizing negative emotions, and intimate partner violence perpetration: A meta-analytic review. Clinical Psychology Review, 37, 40–56. 10.1016/_j.cpr.2015.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black MC (2011). Intimate Partner Violence and Adverse Health Consequences: Implications for Clinicians. American Journal of Lifestyle Medicine, 5(5), 428–439. 10.1177/1559827611410265 [DOI] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Chen J, & Stevens MR (2011). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–673. 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- Borrell LN, Kiefe CI, Williams DR, Diez-Roux AV, & Gordon-Larsen P (2006). Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Social Science & Medicine, 63(6), 1415–1427. 10.1016/j.socscimed.2006.04.008 [DOI] [PubMed] [Google Scholar]
- Brondolo E, Gallo LC, & Myers HF (2009). Race, racism and health: disparities, mechanisms, and interventions. Journal of behavioral medicine, 32(1), 1–8. 10.1007/s10865-008-9190-3 [DOI] [PubMed] [Google Scholar]
- Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, Cassells A, Tobin JN, Sweeney M, & Contrada RJ (2005). The Perceived Ethnic Discrimination Questionnaire: Development and Preliminary Validation of a Community Version. Journal of Applied Social Psychology, 35(2), 335–365. 10.1111/j.1559-1816.2005.tb02124.x [DOI] [Google Scholar]
- Browne MW, & Cudeck R (1992). Alternative Ways of Assessing Model Fit. Sociological Methods & Research, 21(2), 230–258. 10.1177/0049124192021002005 [DOI] [Google Scholar]
- Bryant-Davis T, & Ocampo C (2006). A therapeutic approach to the treatment of racist-incident-based trauma. Journal of Emotional Abuse, 6(4), 1–22. 10.1300/J135v06n04_01 [DOI] [Google Scholar]
- Caetano R, Vaeth PA, & Ramisetty-Mikler S (2008). Intimate partner violence victim and perpetrator characteristics among couples in the United States. Journal of Family Violence, 23(6), 507–518. 10.1007/s10896-008-9178-3 [DOI] [Google Scholar]
- Cafferky BM, Mendez M, Anderson JR, & Stith SM (2018). Substance use and intimate partner violence: A meta-analytic review. Psychology of Violence, 5(1), 110–131. 10.1037/vio0000074 [DOI] [Google Scholar]
- Campbell JC (2002). Health consequences of intimate partner violence. The Lancet, 359(9314), 1331–1336. 10.1016/S0140-6736(02)08336-8 [DOI] [PubMed] [Google Scholar]
- Cardyn L (2002). Sexualized Racism/Gendered Violence: Outraging the Body Politic in the Reconstruction South. Michigan Law Review, 100(4), 675–867. doi: 10.2307/1290425 [DOI] [Google Scholar]
- Carter RT (2007). Racism and psychological and emotional injury: Recognizing and assessing race-based traumatic stress. The Counseling Psychologist, 35(1), 13–105. 10.1177/0011000006292033 [DOI] [Google Scholar]
- Carter RT, Johnson VE, Kirkinis K, Roberson K, Muchow C, & Galgay C (2019). A meta-analytic review of racial discrimination: Relationships to health and culture. Race and Social Problems. 10.1007/s12552-018-9256-y [DOI] [Google Scholar]
- Cazenave NA, & Straus MA (1979). Race, Class, Network Embeddedness and Family Violence: A Search for Potent Support Systems. Journal of Comparative Family Studies, 10(3), 281–300. 10.3138/jcfs.10.3.281 [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. (2015). The Social-Ecological Model: A Framework for Prevention. https://www.cdc.gov/violenceprevention/publichealthissue/social-ecologicalmodel.html
- Cheung GW, & Rensvold RB (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling, 9(2), 233–255. 10.1207/S15328007SEM0902_5 [DOI] [Google Scholar]
- Chou T, Asnaani A, & Hofmann SG (2012). Perception of racial discrimination and psychopathology across three US ethnic minority groups. Cultural Diversity and Ethnic Minority Psychology, 18(1), 74–81. 10.1037/a0025432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, & Williams DR (1999). Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist, 54(10), 805–816. 10.1037/0003-066X.54.10.805 [DOI] [PubMed] [Google Scholar]
- Comas-Diaz L (2007). Ethnopolitical psychology: Healing and transformation. In Aldarondo E (Ed.), Advancing social justice through clinical practice (p. 91–118). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Comas-Díaz L (2016). Racial trauma recovery: A race-informed therapeutic approach to racial wounds. In Alvarez AN, Liang CTH, & Neville HA (Eds.), Cultural, racial, and ethnic psychology book series. The cost of racism for people of color: Contextualizing experiences of discrimination (p. 249–272). American Psychological Association. 10.1037/14852-012 [DOI] [Google Scholar]
- Crenshaw K (1991). Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color. Stanford Law Review, 43(6), 1241–1299. doi: 10.2307/1229039 [DOI] [Google Scholar]
- Davis RG, Ressler KJ, Schwartz AC, Stephens KJ, & Bradley RG (2008). Treatment barriers for low-income, urban African Americans with undiagnosed posttraumatic stress disorder. Journal of traumatic stress, 21(2), 218–222. 10.1002/jts.20313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd JJ, & Bengtson VL (1978). Aging in minority populations: an examination of the double jeopardy hypothesis. Journal of Gerontology, 33(3), 427–436. 10.1093/geronj/33.3.427 [DOI] [PubMed] [Google Scholar]
- Dunbar E (2001). Counseling practices to ameliorate the effects of discrimination and hate events: Toward a systematic approach to assessment and intervention. The Counseling Psychologist, 29(2), 279–307. 10.1177/0011000001292007 [DOI] [Google Scholar]
- Dunn TJ, Baguley T, & Brunsden V (2014). From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. British journal of psychology (London, England: 1953), 105(3), 399–412. 10.1111/bjop.12046 [DOI] [PubMed] [Google Scholar]
- English D, Rendina HJ, & Parsons JT (2018). The Effects of Intersecting Stigma: A Longitudinal Examination of Minority Stress, Mental Health, and Substance Use among Black, Latino, and Multiracial Gay and Bisexual Men. Psychology of Violence, 8(6), 669–679. 10.1037/vio0000218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans MK, Lepkowski JM, Powe NR, LaVeist T, Kuczmarski MF, & Zonderman AB (2010). Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS): Overcoming Barriers to Implementing a Longitudinal, Epidemiologic, Urban Study of Health, Race, and Socioeconomic Status. Ethnicity & disease, 20(3), 267–275. [PMC free article] [PubMed] [Google Scholar]
- Forster M, Grigsby TJ, Soto DW, Sussman SY, & Unger JB (2017). Perceived Discrimination, Cultural Identity Development, and Intimate Partner Violence Among a Sample of Hispanic Young Adults. Cultural Diversity and Ethnic Minority Psychology, 23(4), 576–582. 10.1037/cdp0000154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gondolf EW, & Williams OJ (2001). Culturally focused batterer counseling for African American men. Trauma, Violence, & Abuse, 2(4), 283–295. doi: 10.1177/1524838001002004001 [DOI] [Google Scholar]
- Grollman EA (2014). Multiple Disadvantaged Statuses and Health: The Role of Multiple Forms of Discrimination. Journal of health and social behavior, 55(1), 3–19. 10.1177/0022146514521215 [DOI] [PubMed] [Google Scholar]
- Harrell SP (2000). A multidimensional conceptualization of racism-related stress: Implications for the well-being of people of color. American journal of Orthopsychiatry, 70(1), 42–57. 10.1037/h0087722 [DOI] [PubMed] [Google Scholar]
- Head RN, & Seaborn Thompson M (2017). Discrimination-related anger, religion, and distress: differences between African Americans and Caribbean Black Americans. Society and mental health, 7(3), 159–174. 10.1177/2156869317711225 [DOI] [Google Scholar]
- Heise LL (1998). Violence against women: An integrated, ecological framework. Violence Against Women, 4(3), 262–290. 10.1177/1077801298004003002 [DOI] [PubMed] [Google Scholar]
- Hill Collins P (2002). Black feminist thought : knowledge, consciousness, and the politics of empowerment. Routledge. [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria Versus New Alternatives. Structural Equation Modeling, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- King DK (1988). Multiple Jeopardy, Multiple Consciousness: The Context of a Black Feminist Ideology. Signs: Journal of Women in Culture and Society, 14(1), 42–72. 10.1086/494491 [DOI] [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, & Allen NB (1997). Center for Epidemiological Studies-Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging, 12, 277–287. [DOI] [PubMed] [Google Scholar]
- Maldonado AI, Cunradi CB, & Nápoles AM (2020). Racial/Ethnic Discrimination and Intimate Partner Violence Perpetration in Latino Men: The Mediating Effects of Mental Health. International Journal of Environmental Research and Public Health, 77(21), 8148. doi: 10.3390/ijerphl7218148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles-McLean HA, Maldonado AI, & Murphy CM (2021). Sexist Discrimination and Women’s Use of Intimate Partner Aggression: Results From a Nationally Representative Sample of Women. Psychology of Women Quarterly, 45(1),50–60. 10.1177/0361684320974110 [DOI] [Google Scholar]
- Merkle EC, You D, & Preacher KJ (2016). Testing nonnested structural equation models. Psychological Methods, 21(2), 151–163. 10.1037/met0000038 [DOI] [PubMed] [Google Scholar]
- McLean CP, & Anderson ER (2009, 2009/08/01/). Brave men and timid women? A review of the gender differences in fear and anxiety. Clinical Psychology Review, 29(6), 496–505. 10.1016/_j.cpr.2009.05.003 [DOI] [PubMed] [Google Scholar]
- Murphy CM, Richards TN, Nitsch LJ, Green-Manning A, Brokmeier AM, LaMotte AD, & Holliday CN (2021). Community-informed relationship violence intervention in a high-stress, low-income urban context. Psychology of Violence, 11(6), 509–518. 10.1037/vio000038 [DOI] [Google Scholar]
- Neblett EW Jr., Bernard DL, & Banks KH (2016). The moderating roles of gender and socioeconomic status in the association between racial discrimination and psychological adjustment. Cognitive and Behavioral Practice, 23(3), 385–397. 10.1016/j.cbpra.2016.05.002 [DOI] [Google Scholar]
- Okuda M, Olfson M, Wang S, Rubio JM, Xu Y, & Blanco C (2015). Correlates of intimate partner violence perpetration: Results from a national epidemiologic survey. Journal of Traumatic Stress, 28(1), 49–56. 10.1002/jts.21986 [DOI] [PubMed] [Google Scholar]
- Oram S, Trevillion K, Khalifeh H, Feder G, & Howard LM (2014). Systematic review and meta-analysis of psychiatric disorder and the perpetration of partner violence. Epidemiology and Psychiatric Sciences, 23, 361–376. 10.1017/S2045796013000450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, & Gee G (2015). Racism as a Determinant of Health: A Systematic Review and Meta-Analysis. PLoS ONE, 10(9), 1–48. 10.1371/journal.pone.0138511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, & Richman LS (2009). Perceived Discrimination and Health: A Meta-Analytic Review. Psychological Bulletin, 135(4), 531–554. 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittman CT (2011). Getting mad but ending up sad: The mental health consequences for African Americans using anger to cope with racism. Journal of Black Studies, 42(7), 1106–1124. 10.1177/0021934711401737 [DOI] [PubMed] [Google Scholar]
- Putnick DL, & Bornstein MH (2016). Measurement invariance conventions and reporting: The state of the art and future directions for psychological research. Developmental Review, 41, 71–90. 10.1016/j.dr.2016.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2017). R: A language and environment for statistical computing. In R Foundation for Statistical Computing. https://www.R-project.org/. [Google Scholar]
- Radloff L (1977). The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Smith SG, Chen J, Basile KC, Gilbert LK, Merrick MT, Patel N, Walling M, & Jain A (2017). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010-2012 State Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Rosseel Y (2012). Lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48, 1–36. http://www.jstatsoft.org/v48/i02/. [Google Scholar]
- Spencer C, Mallory AB, Cafferky BM, Kimmes JG, Beck AR, & Stith SM (2019). Mental health factors and intimate partner violence perpetration and victimization: A meta-analysis. Psychology of Violence, 9(1), 1–17. 10.1037/vio0000156 [DOI] [Google Scholar]
- Stets J & Straus MA (1990). Gender differences in reporting marital violence and its medical and psychological consequences. In Straus MA & Gelles RJ (Eds.), Physical violence in American families (pp. 151–165). New Brunswick, NJ: Transaction Publishers. [Google Scholar]
- Stith SM, Smith DB, Penn CE, Ward DB, & Tritt D (2004). Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggression and Violent Behavior, 10(1), 65–98. 10.1016/j.avb.2003.09.001 [DOI] [Google Scholar]
- Straus MA, & Douglas EM (2004). A Short Form of the Revised Conflict Tactics Scales, and Typologies for Severity and Mutuality. Violence & Victims, 19(5), 507–520. 10.1891/vivi.19.5.507.63686 [DOI] [PubMed] [Google Scholar]
- Sutton TE, Gordon Simons L, Martin BT, Klopack ET, Gibbons FX, Beach SR, & Simons RL (2019). Racial Discrimination as a Risk Factor for African American Men’s Physical Partner Violence: A Longitudinal Test of Mediators and Moderators. Violence Against Women. [DOI] [PubMed] [Google Scholar]
- Taft CT, Watkins LE, Stafford J, Street AE, & Monson CM (2011). Posttraumatic Stress Disorder and Intimate Relationship Problems: A Meta-Analysis. Journal of consulting and clinical psychology, 79(1), 22–33. 10.1037/a0022196 [DOI] [PubMed] [Google Scholar]
- Tjaden P, & Thoennes N (2000). Prevalence and consequences of male-to-female and female-to-male intimate partner violence as measured by the National Violence Against Women Survey. Violence Against Women, 6(2), 142–161. 10.1177/10778010022181769 [DOI] [Google Scholar]
- Tolin DF, & Foa EB (2008). Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychological bulletin, 132(6), 959–992. 10.1037/0033-2909.132.6.959 [DOI] [PubMed] [Google Scholar]
- Utsey SO, Giesbrecht N, Hook J, & Stanard PM (2008). Cultural, sociofamilial, and psychological resources that inhibit psychological distress in African Americans exposed to stressful life events and race-related stress. Journal of Counseling Psychology, 55(1), 49–62. 10.1037/0022-0167.55.L49 [DOI] [Google Scholar]
- Walker EA, Newman E, Dobie DJ, Ciechanowski P, & Katon W (2002). Validation of the PTSD checklist in an HMO sample of women. General hospital psychiatry, 24(6), 375–380. 10.1016/s0163-8343(02)00203-7 [DOI] [PubMed] [Google Scholar]
- West SG, Finch JF, & Curran PJ (1995). Structural equation models with nonnormal variables: Problems and remedies. In Hoyle RH (Ed.), Structural equation modeling: Concepts, issues, and applications (p. 56–75). Sage Publications, Inc. [Google Scholar]
- Whitaker DJ, Haileyesus T, Swahn M, & Saltzman LS (2007). Differences in frequency of violence and reported injury between relationships with reciprocal and nonreciprocal intimate partner violence. American Journal of Public Health, 97(5), 941–947. 10.2105/AJPH.2005.079020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Lawrence JA, Davis BA, & Vu C (2019). Understanding how discrimination can affect health. Health services research, 54, 1374–1388. 10.1111/1475-6773.13222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2009). Discrimination and racial disparities in health: evidence and needed research. Journal of behavioral medicine, 32(1), 20–47. 10.1007/s10865-008-9185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CD, Taylor TR, Makambi K, Harrell J, Palmer JR, Rosenberg L, & Adams-Campbell LL (2007). CES-D four-factor structure is confirmed, but not invariant, in a large cohort of African American women. Psychiatry research, 150(2), 173–180. 10.1016/j.psychres.2006.02.007 [DOI] [PubMed] [Google Scholar]
- Williams OJ (1998). Healing and confronting the African America male who batterers. In Carrillo R & Tello J (Eds.), Family violence and men of color (pp. 74–94). New York: Springer. [Google Scholar]
- Zimmerman M, & Mattia JI (2001). A Self-Report Scale to Help Make Psychiatric Diagnoses: The Psychiatric Diagnostic Screening Questionnaire Archives of general psychiatry, 58(8), 787–794. 10.1001/archpsyc.58.8.787 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Per HHS requirements, HANDLS is registered with ClinicalTrials.gov: https://www.clinicaltrials.gov/ct2/show/NCT01323322?term=handls&draw=2&rank=1. Data are restricted but are available upon request due to ethical restrictions imposed by the National Institutes of Health Institutional Review Board. The IRB-approved consent forms that our study participants signed does not permit unrestricted public data sharing. However, it does permit data sharing through a Data Use Sharing Agreement. Data Use Sharing Agreements protect the privacy of human research participants and the confidentiality of their data. Our use of these agreements incorporates confidentiality standards to ensure data security at the agreement holder’s facility and prohibits manipulation of the data for the purpose of identifying study participants. The HANDLS website page labelled information for collaborators explains the process (https://handls.nih.gov/06Coll.htm). The contact for the study is our clinical study manager: Ms. Jennifer Norbeck, MSW, CCRC (norbeckje@grc.nia.nih.gov 410-558-8622). Analysis code in R is available upon request from the corresponding author.


