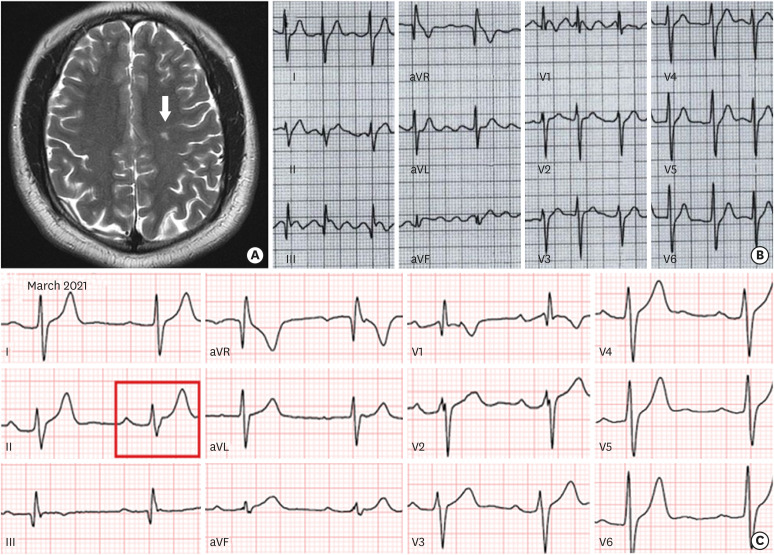
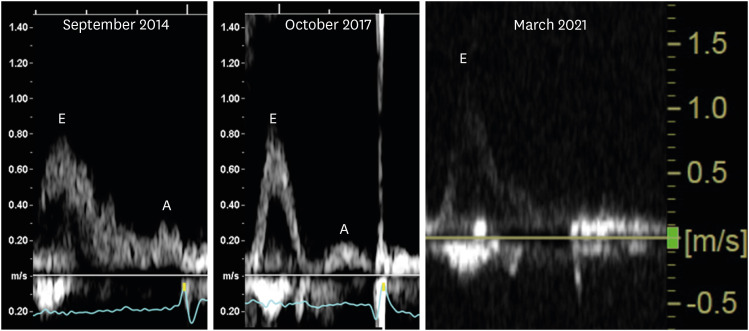
A 26-year-old man experienced paroxysmal atrial fibrillation (AF) and cerebral infarction without significant head and neck angiopathy or coagulopathy in April 2020 (Figure 1A and B). The patient has a history of recurrent syncope and was referred to manage a flecainide-resistant paroxysmal AF in July 2020. Electrocardiography and echocardiography revealed PR prolongation (Figure 1C) and progressive disappearance of mitral inflow A-wave (Figure 2), respectively. Other echocardiography parameters are shown in Supplementary Figure 1A and B.
Figure 1. Examinations which were conducted prior to electrophysiological study. Cerebral magnetic resonance imaging in April 2020 (A). Documented paroxysmal atrial fibrillation in July 2020 (B). Electrocardiogram in March 2021. The red square showed PR interval 240 ms (C).
aVF = augmented vector foot; aVL = augmented vector left; aVR = augmented vector right.
Figure 2. Echocardiography which was conducted in March 2021. Serial change of mitral inflow pattern and loss of A-wave since September 2014.
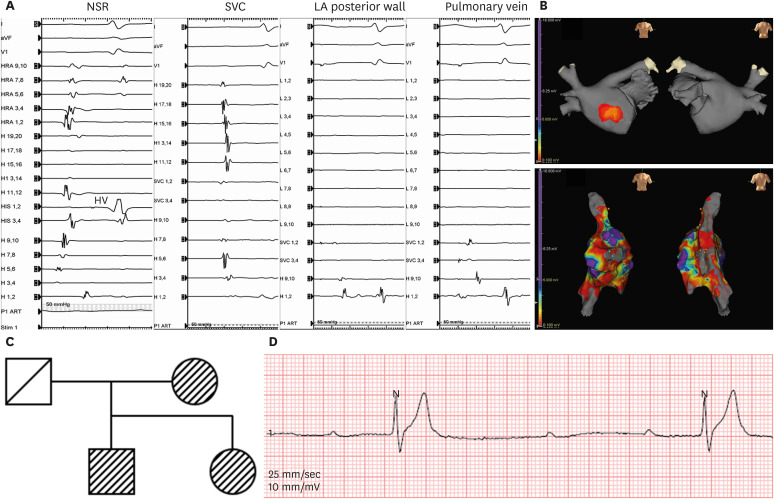
The patient underwent an electrophysiological study in March 2021. At a baseline sinus cycle length of 700 ms, the HV interval was 73 ms (Figure 3A). LA pressure was measured at 33 mmHg. Intracardiac echocardiography was performed after trans-septal puncture (Supplementary Figure 1C). In contrast to the absence of endocardial bipolar voltage signals in the entire LA and pulmonary veins except for a small area at the anteroseptal LA (a bipolar voltage cut-off of 0.1mV, Figure 3B), right atrium (RA) showed relatively preserved voltage with localized scar on the septum in a 3D-electroanatomical map. The intracardiac electrograms showed consistent results (Figure 3A). We performed linear ablations of the superior vena cava to the RA septum and cavotricuspid isthmus without LA ablation.
Figure 3. Electrophysiologic study and ECG. Intracardiac electrogram during sinus rhythm with HV interval 73 ms. In contrast to the absence of endocardial signals in LA posterior wall and pulmonary vein, SVC showed relatively preserved signals in intracardiac electrograms (A). The left atrial voltage map with final ablation site at RA (B). A genotype pedigree representing first-degree relatives (C). Follow-up Holter showing paroxysmal complete AV block in November 2021 (D).
AV = atrioventricular; aVF = augmented vector foot; HV = His-ventricular; LA = left atrial; NSR = normal sinus rhythm; RA = right atrium; SVC = superior vena cava.
Two months after the procedure, an SCN5A mutation (c.3823G>A[p.Asp1275Asn], likely pathogenic) was found in the proband and his mother and sister (Figure 3C). Paroxysmal complete atrioventricular block was revealed in the Holter during follow-up (Figure 3D). Eventually, the patient underwent a dual-chamber pacemaker implantation eight months after electrophysiology procedure.
Our patient had an SCN5A-D1275N mutation associated with isolated LA standstill and progressive AV conduction disease requiring permanent pacemaker implantation.1),2) Although this patient did not show any evidence for ventricular arrhythmia, careful observation and follow-up are warranted for this potentially progressive genetic arrhythmia disease.
Written informed consent was obtained from the patient.
Footnotes
Funding: This work was supported by a grant (HI21C0011) from the Ministry of Health and Welfare, a grant (NRF-2020R1A2B5B01001695) from the Basic Science Research Program run by the National Research Foundation of Korea (NRF) which is funded by the Ministry of Science, ICT & Future Planning (MSIP), and a grant (RS-2022-00141473) from Cross-ministerial tasks.
Conflict of Interest: The authors have no financial conflicts of interest.
Data Sharing Statement: The data generated in this study is available from the corresponding author upon reasonable request.
- Conceptualization: Oh J, Pak HN.
- Data curation: Kang DS, Khmao P, Oh J, Pak HN.
- Formal analysis: Kang DS, Khmao P, Pak HN.
- Investigation: Kang DS, Khmao P, Oh J, Pak HN.
- Methodology: Kang DS, Khmao P, Pak HN.
- Project administration: Pak HN.
- Supervision: Oh J, Pak HN.
- Writing - original draft: Kang DS, Khmao P.
- Writing - review & editing: Oh J, Pak HN.
SUPPLEMENTARY MATERIAL
Additional results of examinations which was conducted prior to or during electrophysiological study. Transthoracic echocardiography conducted in March 2021 identified an enlarged left ventricle with preserved systolic function (A). Other parameters of the transthoracic echocardiography (B). Intracardiac echocardiography showed decreased emptying and filling velocity of left atrial appendage (C).
References
- 1.Shaw TR, Northridge DB, Francis CM. Left atrial standstill in a patient with mitral stenosis and sinus rhythm: a risk of thrombus hidden by left and right atrial electrical dissociation. Heart. 2003;89:1173. doi: 10.1136/heart.89.10.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duncan E, Schilling RJ, Earley M. Isolated left atrial standstill identified during catheter ablation. Pacing Clin Electrophysiol. 2013;36:e120–e124. doi: 10.1111/j.1540-8159.2010.02957.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional results of examinations which was conducted prior to or during electrophysiological study. Transthoracic echocardiography conducted in March 2021 identified an enlarged left ventricle with preserved systolic function (A). Other parameters of the transthoracic echocardiography (B). Intracardiac echocardiography showed decreased emptying and filling velocity of left atrial appendage (C).