Graphical Abstract
To the Editor:
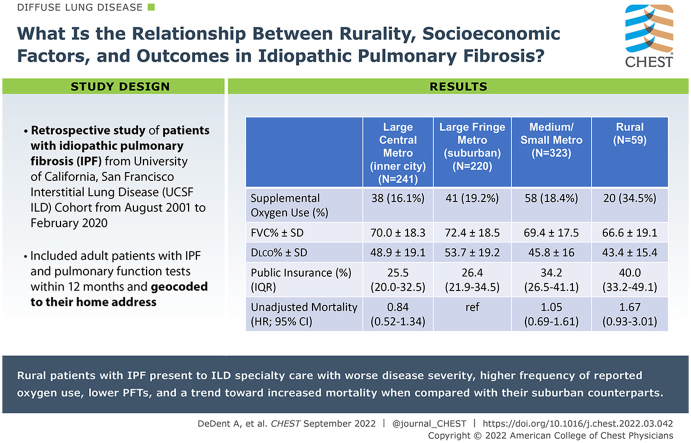
Idiopathic pulmonary fibrosis (IPF) is a chronic interstitial lung disease (ILD) characterized by a progressive decline in lung function.1 Early diagnosis and treatment are essential to slow lung function decline.2,3 Rural populations experience socioeconomic disadvantage and fractured access to care, both of which contribute to worse health outcomes.4 The relationship between rurality, socioeconomic factors that may impair care access, and outcomes in IPF has not been previously explored. We investigated the association between rurality and IPF disease severity, measured by pulmonary function at presentation to ILD specialty care, and mortality rates. We hypothesized that rurality would be associated with worse pulmonary function at presentation and death and that these relationships would be explained by neighborhood-level socioeconomic factors.
Methods
For this retrospective study, consenting participants with IPF were identified from the University of California, San Francisco (UCSF) ILD Cohort between August 2001 and February 2020 (UCSF institutional review board #10-01592). Eligibility criteria included age ≥18 years, pulmonary function tests within 12 months of the clinic visit date, and a home address that could be geocoded.
Rurality was categorized with the use of the 2013 National Center for Health Statistics Urban-Rural Classification Scheme for Counties: rural (micropolitan/noncore), medium/small metro (combined), large fringe metro (ie, suburban), and large central metro (ie, inner cities).5 Some categories were collapsed because of the small sample sizes. Large fringe metro was chosen as the reference region because they often experience better health outcomes and socioeconomic advantage compared to the other regions.5 Outcomes included FVC percent predicted and diffusion capacity for carbon monoxide (Dlco) percent predicted, which were standardized with the use of the Global Lung Initiative reference equations,6,7 and death, which was verified with the use of the National Death Index. Participants were censored at lung transplantation or the end of the study period. Time to death or censoring was measured from the initial clinic visit. We measured the association between geographic region and FVC and Dlco percent predicted at presentation using stepwise multivariate linear regression, first adjusting for individual-level covariates, which included age, sex, race/ethnicity, COPD diagnosis, smoking history, and antifibrotic use (nintedanib/pirfenidone) and then for neighborhood-level socioeconomic variables with a known relationship to rurality, which included the percent of the population with a bachelor’s degree or greater, percent with no insurance, percent with public insurance, and the percent of the population ≥ 65 years old who were living below the federal poverty line, which was obtained from the American Community Survey 5-year estimates.8 Immunosuppression use was not included because of nonsignificant differences between geographic regions before and after the approval of antifibrotics. Robust SEs were used because the constant variance assumption was violated; all other assumptions of the linear models were met. The association with death was assessed with the use of stepwise Cox proportional hazards regression, first adjusting for individual-level covariates and then for FVC and Dlco percent predicted at presentation, and last for neighborhood-level socioeconomic variables. Follow-up time was stratified into 0 to 1 and ≥ 1 years to meet the proportional hazards assumption. Models were run with the use of the Stata software statistical package, version 16.1/SE (StataCorporation). Probability values ≤.05 were considered statistically significant.
Results
Eight hundred forty-three participants were included in the analysis. Rural participants had the highest frequency of reported shortness of breath and supplemental oxygen use and the lowest frequency of antifibrotic use at presentation (Table 1). Compared with suburban participants, rurality was associated with lower mean FVC % predicted (˗8.19%; 95% CI, ˗14.20% to ˗2.19%) and Dlco percent predicted (˗7.99%; 95% CI, ˗12.58% to ˗3.40%) after adjustment for individual-level covariates with attenuation in both measures after adjustment for neighborhood-level variables (˗4.82%; 95% CI, ˗11.30% to 1.65%; and ˗4.95%; 95% CI, ˗9.83% to ˗0.06%, respectively).
Table 1.
Baseline Characteristics of Participants with Idiopathic Pulmonary Fibrosis by Geographic Region
| Characteristic | Large Central Metro (inner city) (n = 241) | Large Fringe Metro (suburban) (n = 220) | Medium/Small Metro (n = 323) | Rural (n = 59) | P value |
|---|---|---|---|---|---|
| Individual variables | |||||
| Age, mean (SD), years | 71.4 (8.7) | 71.8 (8.4) | 71.0 (8.6) | 69.9 (8.5) | .5 |
| Sex, No. (%), male | 177 (73.4) | 175 (79.5) | 227 (70.3) | 46 (78.0) | .095 |
| Supplemental oxygen use, No. (%) | 38 (16.1) | 41 (19.2) | 58 (18.4) | 20 (34.5) | .016 |
| Cough, No. (%) | 201 (84.5) | 186 (84.9) | 279 (86.6) | 53 (89.8) | .7 |
| Dyspnea, No. (%), | 198 (87.2) | 184 (90.2) | 294 (93.6) | 56 (98.2) | .014 |
| FVC percent predicted, mean (SD) | 70.0 (18.3) | 72.4 (18.5) | 69.4 (17.5) | 66.6 (19.1) | .11 |
| Diffusion capacity for carbon monoxide percent predicted, mean (SD) | 48.9 (19.1) | 53.7 (19.2) | 45.8 (16.0) | 43.4 (15.4) | <.001 |
| Antifibrotic use after 10/31/2014, No. (%)a | 23/108 (21.3) | 26/101 (25.7) | 20/140 (14.3) | 2/20 (10.0) | .10 |
| Immunosuppression use after 10/31/2014, No. (%)b | 17/103 (16.5) | 18/96 (18.8) | 19/134 (14.2) | 3/19 (15.8) | .8 |
| Referring pulmonary provider, No. (%) | 144 (67.0) | 178 (84.0) | 274 (87.8) | 43 (75.4) | <.001 |
| Neighborhood variables | |||||
| Educational attainment | |||||
| Less than high school, median (IQR), % | 3.1 (1.1-6.4) | 1.8 (0.6-4.1) | 3.7 (1.4-7.7) | 2.7 (1.4-4.8) | <.001c |
| High school graduate, mean (SD), % | 14.4 (8.5) | 15.6 (8.8) | 20.3 (6.5) | 24.3 (7.1) | <.001 |
| Bachelor’s degree, mean (SD), % | 29.1 (9.6) | 28.5 (10.3) | 20.6 (9.1) | 18.2 (8.2) | <.001 |
| Graduate or professional degree, median (IQR), % | 19.2 (10.1-31.9) | 19.5 (9.1-31.2) | 11.1 (6.6-17.9) | 8.1 (5.4-12.4) | <.001c |
| Insurance status | |||||
| Private insurance, median (IQR), % | 81.1 (70.0-88.1) | 82.7 (75.6-88.7) | 72.9 (61.6-81.3) | 63.0 (55.3-71.7) | <.001c |
| Public insurance, median (IQR), % | 25.5 (20.0-32.5) | 26.4 (21.9-34.5) | 34.2 (26.5-41.1) | 40.0 (33.2-49.1) | <.001c |
| Uninsured, median (IQR), % | 5.7 (2.6-10.1) | 4.4 (2.2-8.4) | 8.2 (4.8-13.4) | 12.3 (7.5-16.7) | <.001c |
| Poverty: below the poverty level at age ≥ 65 years, median (IQR), % | 6.4 (2.6-12.2) | 5.0 (2.1-8.3) | 6.5 (3.2-10.2) | 6.7 (3.4-10.2) | .009c |
Data are presented as mean ± SD; No. (%); median (interquartile range: 25%, 75%), or categoric statistical analyses that were performed with the use of analysis of variance, unless otherwise specified.
Antifibrotic use defined as use of pirfenidone or nintedanib at initial presentation.
Immunosuppression use defined as use of prednisone, azathioprine, or mycophenolate at presentation, alone or in combination.
Categoric statistical analyses performed with the use of Kruskal-Wallis testing because of skewed distribution.
Median survival time for the cohort was 1,330 days (Fig 1). In the first year of follow up, we observed a trend towards an increased mortality rate for participants from rural regions (hazard ratio = 1.80; 95% CI, 0.98 to 3.31; P = .06) (Table 2) after adjustment for individual-level variables. This finding was attenuated after adjustment for FVC and Dlco percent predicted at presentation (hazard ratio = 0.87; 95% CI, 0.39 to 1.91; P = .7). These results were not changed qualitatively after further adjustment for neighborhood-level socioeconomic variables (results not shown).
Figure 1.
Survival time estimates by geographic region are displayed up to 2,000 days or 5.48 years of follow-up time. Median survival time by geographic region as follows: rural = 927 days; medium/small metro = 1,347 days; large fringe metro (suburban) = 1,304 days, and large central metro (inner city) = 1,348 days.
Table 2.
Unadjusted and Adjusted Hazard Ratio for Death by Geographic Region
| Geographic region | Model 1a |
Model 2b |
Model 3c |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Hazard ratio | CI | P value | Hazard ratio | CI | P value | Hazard ratio | CI | P value | |
| Large fringe metro (suburban) | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Large central metro (inner city) | |||||||||
| 0-1 years | 0.84 | 0.52-1.34 | .5 | 0.92 | 0.57-1.49 | .7 | 0.84 | 0.50-1.43 | .5 |
| ≥1 years | 0.99 | 0.74-1.32 | > .9 | 1.02 | 0.76-1.37 | .9 | 0.84 | 0.61-1.17 | .3 |
| Medium/small metro | |||||||||
| 0-1 years | 1.05 | 0.69-1.61 | .8 | 1.19 | 0.77-1.82 | .4 | 0.88 | 0.55-1.40 | .6 |
| ≥1 years | 1.03 | 0.79-1.36 | .8 | 1.14 | 0.86-1.51 | .4 | 0.74 | 0.54-1.01 | .06 |
| Rural | |||||||||
| 0-1 years | 1.67 | 0.93-3.01 | .09 | 1.80 | 0.98-3.31 | .06 | 0.87 | 0.39-1.91 | .7 |
| ≥ 1 years | 1.0 | 0.62-1.60 | > .9 | 1.18 | 0.73-1.92 | .5 | 0.79 | 0.47-1.35 | .4 |
Unadjusted analysis.
Adjusted for individual-level covariates: age, gender, race/ethnicity, COPD diagnosis, smoking history, antifibrotic use.
Adjusted for individual-level characteristics and pulmonary function at time of referral: age, gender, race/ethnicity, COPD diagnosis, smoking history, antifibrotic use, FVC % predicted with the use of the Global Lung Initiative “Other” reference equation, diffusion capacity for carbon monoxide percent predicted with the use of the Global Lung Initiative reference equation.
Discussion
We found that rural participants with IPF present to ILD specialty care with worse disease severity, which included a higher frequency of reported oxygen use and lower pulmonary function (the latter of which was largely explained by neighborhood-level socioeconomic factors), compared to their suburban counterparts. Though we found no statistically significant difference in survival between rural and suburban participants, the resolution of the increased hazard ratio at 1 year after adjustment for pulmonary function measures observed at the initial visit suggests that delayed presentation may be one explanatory pathway for worse short-term outcomes for rural populations with IPF.
Larger prospective studies are needed to further assess this potential pathway. We did not observe differences in survival between groups after the first year of follow up, possibly because the survival curve for suburban participants after this time more closely followed that of rural participants, and the sample size of rural participants was small. These findings support rurality as a barrier to ILD specialty care,4 which is highlighted by the small proportion of rural participants with IPF in our cohort (7% of population) compared with the proportion of the US population that lives in rural areas (approximately 20%), where IPF prevalence is greater and the populations is disproportionately older.8 Potential rural barriers to care include possible lack of access to local pulmonary care, or if accessing local pulmonary care, possibly only those who have the most severe or complicated disease are referred to ILD specialty care. Additional barriers include lack of adequate health insurance or other resources, logistical challenges (eg, distance from UCSF), and increased overall morbidity/competing priorities. Our study was not designed to address these questions. Limitations of this study include a low sample size of rural participants that limited the power to detect differences in mortality rates and the lack of a universally accepted definition of rurality.9 Given the health disparities experienced by rural populations more generally, further studies are warranted to validate and expand on our findings.
Acknowledgments
Funding/support: This study was funded by grants from the NHLBI/NIH (K24HL12131 and 5T32HL007185-43,44,45).
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: A. M. D. reports grants from the National Institutes of Health. H. R. C. reports grants from the National Institutes of Health, personal fees from Boehringer Ingelheim, grants from the Pulmonary Fibrosis Foundation, grants and personal fees from Three Lakes Partners, personal fees from Advance Medical, and personal fees from Polarean outside the submitted work. None declared (N. T.).
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: The authors thank Jane Berkeley, BA, for her assistance with data management, retrieval, and geocoding; Ann Lazar, PhD, for statistical support; the providers, staff, and coordinators of the University of California, San Francisco, Interstitial Lung Disease Clinic, and the patients who agreed to participate in this cohort study.
Footnotes
Part of this article was previously presented in abstract form at the American Thoracic Society Virtual Conference, May 16, 2021.
References
- 1.Raghu G., Collard H.R., Egan J.J., et al. ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.King T.E., Jr., Bradford W.Z., Castro-Bernardini S., et al. ASCEND Study Group A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2083–2092. doi: 10.1056/NEJMoa1402582. [DOI] [PubMed] [Google Scholar]
- 3.Richeldi L., du Bois R.M., Raghu G., et al. INPULSIS Trial Investigators Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2071–2082. doi: 10.1056/NEJMoa1402584. [DOI] [PubMed] [Google Scholar]
- 4.Douthit N., Kiv S., Dwolatzky T., Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–620. doi: 10.1016/j.puhe.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Ingram D.D., Franco S.J. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat 2. 2014;(166):1–73. [PubMed] [Google Scholar]
- 6.Quanjer P.H., Stanojevic S., Cole T.J., et al. ERS Global Lung Function Initiative Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–1343. doi: 10.1183/09031936.00080312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stanojevic S., Graham B.L., Cooper B.G., et al. Global Lung Function Initiative TLCO working group. Global Lung Function Initiative (GLI) TLCO Official ERS technical standards: Global Lung Function Initiative reference values for the carbon monoxide transfer factor for Caucasians. Eur Respir J. 2017;50(3) doi: 10.1183/13993003.00010-2017. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Census Bureau. American Community Survey, 2012 and 2017 American Community Survey 5-year estimates, Tables DP02, DP03, S1701; generated by Alison DeDent; using data.census.gov. Accessed July 13, 2020. https://data.census.gov/cedsci/
- 9.Bennett K.J., Borders T.F., Holmes G.M., Kozhimannil K.B., Ziller E. What is rural? Challenges and implications of definitions that inadequately encompass rural people and places. Health Aff (Millwood) 2019;38(12):1985–1992. doi: 10.1377/hlthaff.2019.00910. [DOI] [PubMed] [Google Scholar]