Abstract
Anaplastic thyroid cancer (ATC) is an aggressive and lethal malignancy having a dismal prognosis. Phytochemicals are bioactive components obtained from plants that have been proven useful to treat numerous diseases. Phytochemicals are also an important source of novel anticancer drugs and an important area of research due to the numerous available candidates that can potentially treat cancers. This review discusses naturally occurring phytochemicals and their derivatives that show promising anticancer effects in anaplastic thyroid cancer. Anticancer effects include cell growth inhibition, induction of apoptosis, promoting cell cycle arrest, suppressing angiogenesis, modulating autophagy, and increasing the production of reactive oxygen species. Phytochemicals are not only prospective candidates in the therapy of anaplastic thyroid cancer but also exhibit potential as adjuvants to improve the anticancer effects of other drugs. Although some phytochemicals have excellent anticancer properties, drug resistance observed during the use of resveratrol and artemisinin in different anaplastic thyroid cancer cell lines is still a problem. Anaplastic thyroid cancer cells have several biological, clinical, and drug-resistance features that differ from differentiated thyroid cancer cells. Phytochemicals such as resveratrol and quercetin exhibit different biological effects in anaplastic thyroid cancer and differentiated thyroid cancer. Tumor cells depend on increased aerobic glycolysis by mitochondrial oxidative phosphorylation to provide energy for their rapid growth, invasiveness, and drug resistance. Phytochemicals can alter signaling cascades, modulate the metabolic properties of cancer cells, and influence the mitochondrial membrane potential of anaplastic thyroid cancer cells. These findings enrich our knowledge of the anticancer effects of phytochemicals and highlight alternative therapies to prevent drug resistance in anaplastic thyroid cancer.
Keywords: phytochemicals, anaplastic thyroid cancer, drug resistance, adjuvant, resveratrol
1. Introduction
Anaplastic thyroid cancer (ATC) constitutes 1–2% of all thyroid cancers and has a poor prognosis with a median survival time of 6 months in 50% of patients and only a 1-year survival time in 20% of patients (1). The comprehensive treatment for ATC includes surgery and systematic chemotherapy combined with radioiodine therapy; however, the therapeutic outcomes are not promising owing to its rapid proliferation and aggressive nature and the lack of thyroid-specific role of iodine intake (2,3). Systemic chemotherapies based on combining paclitaxel or docetaxel with carboplatin or doxorubicin are adopted for patients with metastases (2,4,5). However, clinical data has revealed that serious adverse effects and drug resistance hinder combination treatment, posing difficulties in completing the course (5–7). A lack of reliable treatment for ATC due to resistance to chemotherapy leads to unlimited local growth and distal metastases in patients with ATC (8). All-trans-retinoic acid (ATRA) has been used to impel ATC cell redifferentiation with increased iodine uptake and improved radiosensitivity (9); however, the results are not promising and even exhibit the opposite effects in other ATC cell lines. Therefore, there is an urgent need to identify novel and safe drugs or redifferentiation agents with fewer side effects for ATC therapy.
Phytochemicals are effective in the management of inflammation and cancer (10). Dietary phytochemicals are potential modulators of immunological status and possess various pharmacological properties including anticancer, antioxidant, and anti-inflammatory effects (11). The therapeutic efficacy of phytochemicals shows promise in the management of several cancers (12). However, certain studies on the use of phytochemicals to treat ATC have exhibited some special features, which are presented in detail below. For example, ATRA induced redifferentiation in ATC cells (SW1736) and inhibited cell growth (9) but was ineffective in THJ-11T, THJ-16T, and THJ-21T cells (13). However, resveratrol reversed ATRA resistance in THJ-11T cells that were resistant to treatment only with resveratrol. These findings suggest that phytochemicals not only show promising antitumor effects in ATC cells but also exhibit the possibility to induce ATC cell redifferentiation in vivo. Further preclinical or clinical studies focusing on the treatment of ATC may face challenges of drug resistance. Phytochemicals may serve as prospective adjuvants to prevent drug resistance in ATC.
In the present review, some of the natural phytochemicals used to treat ATC were summarized and similar anticancer effects of other phytochemicals were listed. The references are mainly derived from searching internet databases such as Google Scholar, PubMed, and ScienceDirect. The search was restricted to studies published in English and those conducted on humans. Only articles and reviews were selected and symposium or conference papers were excluded. The present review focused on agents obtained from plants that exhibit a potential role in the treatment of ATC. Compounds obtained from other organisms were excluded.
2. Phytochemicals effective in ATC cells
Aloperine
Aloperine is a quinolizidine alkaloid extracted from Sophora alopecuroides L., commonly used to treat infections, rheumatism, heart disorders, and gastrointestinal diseases (14). To date, the anticancer effects of aloperine include inhibition of cell growth, induction of apoptosis, activation of reactive oxygen species (ROS), and modulation of autophagy in several cancers, such as breast, prostate, ovarian, and thyroid cancer (15–18). Aloperine was revealed to inhibit the proliferation of ATC cells (8505C and KMH-2) and tumorigenesis in vivo. It also promoted caspase-dependent apoptosis in 8505C and KMH-2 cells by intrinsic or extrinsic pathways (19). Moreover, aloperine promoted the activation of autophagy in KMH-2 ATC cells by suppressing the activation of the Akt/mammalian target of rapamycin (mTOR) pathway. The cytotoxic effect of aloperine in KMH-2 ATC cells resulted from aloperine-mediated autophagy (18).
Apigenin (APG)
APG is a flavone widely found in fruit, vegetables, and seasoning herbs, such as artichoke, onions, and dried chamomile flowers (20). APG exerts anticancer effects by altering cell viability, migration and invasion potential, dendrite morphology, G2/M phase arrest, and apoptosis by inactivation of the extracellular signal-regulated protein kinase (ERK) and the Akt/mTOR signaling pathway (21). In 1999, it was reported that APG exerted anticancer effects on ATC cells (ARO) that lack antiestrogen binding sites or estrogen receptors (22). APG also induced apoptosis in ATC cells (FRO) by increasing c-Myc levels and phosphorylation of both p38 and p53. c-Myc may act as a core regulator in the progression of APG-induced apoptosis of ATC cells (23). In addition, APG exerted growth-inhibition effects in ATC cells (ARO), inhibited both autophosphorylation of epidermal growth factor receptor (EGFR) tyrosine and phosphorylation of its downstream effector mitogen-activated protein kinase (MAPK) and decreased c-Myc phosphorylation (24). PLX4032 is a BRAFV600E inhibitor that can enhance the effects of APG in ATC cells (8505C and FRO) harboring BRAFV600E (25). The outcomes of using APG and PLX4032 include the decreasing of cell viability, increasing the dead cell percentage, promoting the expression of cleaved poly-ADP ribose polymerase (PARP)-1 and cleaved caspase-3 protein, and decreasing phosphorylated (p)-ERK expression. However, treatment with APG and PLX4032 failed to alter the protein levels of p-ERK in FRO cells. Additionally, treatment with APG and tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL) decreased the viability of ATC cells (8505C and CAL-62) and Bcl-2 protein levels, and increased the protein levels of cleaved PARP and p-ERK1/2. Suppression of Akt signaling enhanced the effects of APG and TRAIL treatment by modulation of Bcl-2 family protein levels in 8505C and CAL-62 cells (26).
Artemisinin (ART)
ART is a sesquiterpene isolated from Artemisia annua L. It is known as qinghao (a herb with a long history of use in China), and as a sesquiterpene with a unique peroxide structure, ART exhibits excellent activity against malaria (27). ART and its derivatives are potential candidates that have been demonstrated to increase the apoptosis and autophagy of cancer cells, promote cell cycle arrest, suppress the invasion and migration of cancer cells, and induce ferroptosis in cancer cells (28). It was revealed that ART could suppress cell growth, induce arrest in the G2/M phase, and increase cyclin D1 in BHT-101 ATC cells but not in CAL-62 ATC cells. Using RNA-seq, it was determined that ART-resistant CAL-62 cells were associated to the abnormal activation of WNT signaling. Lastly, the issue of ART resistance was overcome by co-treating cells with ART and pyrvinium pamoate, which is a WNT signaling inhibitor (29).
Baicalein
Baicalein is a flavone extracted from Scutellaria (S.) baicalensis Georgi or S. lateriflora L. It has several anticancer properties including the inhibition of cell proliferation, invasiveness, migration, and EMT progression; and an increase in apoptosis and autophagy (30–32). Some studies have demonstrated that treatment with baicalein (50 or 100 µM) and docetaxel (10 nM) can significantly enhance the anticancer effects of docetaxel by the suppression of proliferation and induction of apoptosis, and by significantly inhibiting the expression of transforming growth factor (TGF)-β1, vascular endothelial growth factor (VEGF), caspase-3, Bax, E-cadherin, N-cadherin, and mTOR. Moreover, baicalein and docetaxel significantly reduced Bcl-2 expression and the phosphorylation of ERK and Akt in 8505C ATC cells (33). Furthermore, baicalein treatment inhibited the proliferation of FRO ATC cells and induced apoptosis with increased DNA fragmentation. Baicalein at concentrations of 50 and 100 µM was demonstrated to decrease the expression of Bax, PARP, cytochrome c, cleaved caspase-3, and Cox-2, and increase Bcl-2 expression. Baicalein exerted anticancer effects in FRO ATC cells mainly by promoting the phosphorylation of ERK, p38, MAPK, and Akt (34). Additionally, baicalein decreased cell viability and the number of cell colonies, and increased cell apoptosis, cell cycle arrest, and autophagy in FRO ATC cells. It significantly increased the expression of Beclin-1, Atg5, p62, Atg12, caspase-3, and caspase-8. Furthermore, it significantly decreased the ratios of caspase-3 and caspase-8, p-ERK/ERK, and p-Akt/Akt, suggesting its potential in suppressing ERK and phosphatidylinositol 3-kinase/protein kinase B (PI3K/Akt) signaling (32).
Chrysin
Chrysin is a phytochemical widely present in Matricaria chamomilla L., Oroxylum Indicum (L.) Kurz, Passiflora edulis Sims, and P. caerulea L. It is also found in honey, passion fruit, and mushrooms (35,36). Chrysin has been demonstrated to inhibit the growth of cancer cells through the induction of apoptosis, cell cycle arrest, suppression of angiogenesis, and inhibition of invasion and metastasis, without causing toxicity or undesirable side effects to normal cells both in vivo and in vitro. Chrysin exerts these effects by selectively modulating multiple cell signaling pathways related to inflammation, proliferation, angiogenesis, invasion and metastasis, and survival of cancer cells (37). Chrysin exerted anticancer effects in ATC cells (HTH7 and KAT18) such as inhibition of cell growth, alteration of protein levels, and increasing the ratio of Bax to Bcl-2 expression (38). Changes in protein levels included a decrease in the expression of cyclin D1, Mcl-1, and XIAP, and a significant increase in the expression of cleaved caspase-3 and cleaved PARP. In addition, chrysin was revealed as a potential Notch activator in ATC cells (HTh7 and KAT18) (39). Chrysin treatment resulted in cell growth inhibition and increased the protein and mRNA expression of Notch 1 and hairy/enhancer of split 1 (Hes1). The proliferation-inhibition effect of chrysin in ATC cells was due to apoptosis resulting from Notch1 activation and an increase in cleaved PARP protein in vivo. Moreover, chrysin suppressed the growth of ATC xenografts and delayed the calculated median time to tumor progression in vivo (39).
Curcumin
Curcumin is a polyphenol obtained from the rhizomes of Curcuma longa. It is one of the most promising naturally occurring compounds used to treat cancers, including breast, lung, gastric, colorectal, pancreatic, and hepatic cancers (40). Curcumin intervention was demonstrated to result in a decrease in cell viability, suppression of aggressiveness, and an increase in apoptosis in the ATC cell lines SW1736 and 8505C. It also decreased the mRNA expression of PAX8, TTF1, TTF2, and TPO in SW1736 cells while decreasing the miRNA expression of hsa-miR-221, hsa-miR-222, hsa-miR-21, and hsa-miR-146b in both SW1736 and 8505C (41). Curcumin was revealed to significantly reduce the oxidative stress index in ATC cells (CAL-62) accumulating in the G0/1 phase, and also suppress spheroid formation and cellular motility in Matrigel (42). Moreover, curcumin increased the therapeutic efficacy of drugs used to treat ATC. Curcumin combined with docetaxel decreased the viability of ATC cells and induced apoptosis. It improved the anticancer effect of docetaxel in ATC cells by inhibiting p65 activation and COX2 expression and decreasing the threshold of cell apoptosis by docetaxel (43). Thus, the role of curcumin as an adjuvant in ATC chemotherapy should be further explored.
Deguelin
Deguelin is one of the four natural rotenoids obtained from the bark, roots, and leaves of plants from the Leguminosae family. It is an NADH:ubiquinone oxidoreductase (complex I) inhibitor (44,45). Low doses of deguelin have been demonstrated to result in cell cycle arrest, induction of tumor apoptosis, and suppression of angiogenesis and metastasis. Its anticancer effects are related to the protein levels of PI3K, MAPK, Akt, mTOR, NF-κB, caspase-3/8/9, matrix metalloproteinase (MMP)-2, and MMP-9 (45). Deguelin enhanced superoxide dismutase (SOD) activity and effectively induced apoptosis (similar to docetaxel) in CAL-62 ATC cells. It has been shown to play similar roles as that of curcumin, such as blocking spheroid formation and cellular motility in Matrigel and cell cycle arrest (42).
Epigallocatechin-3-gallate (EGCG)
EGCG is one of the most abundant ingredients in green tea that has been widely studied as a phytochemical and nutraceutical (46). EGCG has been demonstrated to induce ROS generation and upregulate AMPK. Through the increase in liver kinase B1 (LKB1) and Ca2+/calmodulin-dependent protein kinase kinase (CaMKK), it caused a decrease in mTOR expression, which finally led to anticancer effects (47). A previous study revealed that EGCG inhibited the proliferation, viability, cell cycle progression, migration, and invasion of ARO ATC cells, and induced apoptosis in ARO cells by reducing the protein levels of H-RAS, p-RAF, p-MEK1/2, p-EGFR, and p-ERK1/2. In vivo, EGCG inhibited the growth of ARO cell carcinoma xenografts by increasing apoptosis and blocking angiogenesis (48). Furthermore, EGCG significantly inhibited epithelial-mesenchymal transition (EMT), invasion, and migration in 8505C ATC cells by regulating the TGF-β/Smad signaling pathways in vivo. The regulatory mechanism of TGF-β/Smad signaling pathways includes E-cadherin reduction and vimentin induction, and the inhibition of Smad2/3 phosphorylation and Smad4 translocation (49).
Evodiamine (EVO)
EVO is an important alkaloid isolated from the fruit of Tetradium ruticarpum (A.Juss.) T.G. Hartley, and is one of the most important components of the Chinese herb ‘Wu-Zhu-Yu’ (50). EVO has been revealed to exert its anticancer effects by inhibiting cell growth, invasion, and metastasis, and inducing apoptosis in cancer cells in colon cancer, lung cancer, hepatocellular carcinoma, and melanoma (51). Mechanisms of the anticancer effects of EVO in ARO ATC cells include the inhibition of cell proliferation, increase in DNA fragmentation, induction of apoptosis, and G2/M phase arrest. Moreover, EVO was demonstrated to change the protein levels and activity in ARO ATC cells, which included increasing the levels of cdc25C, cyclin B1, and cdc2-p161; decreasing the level of cdc2-p15; and promoting caspase-3/8/9 activation and PARP cleavage (52). Results from a proteomic strategy indicated that the anticancer effects of EVO in ARO ATC cells were due to the differentially expressed proteins involved in transcription control, signal transduction/calcium regulation, protein folding, and lipid metabolism (53). Furthermore, EVO was shown to decrease cell viability and the protein levels of Bcl-2 and p-Akt, and increase cytotoxicity and the percentage of apoptotic cells in SW1736 ATC cells. EVO exhibited synergistic effects when used with other anticancer agents such as wortmannin, TGF-β, and PXD101 (a histone deacetylase inhibitor). Co-treatment with EVO and wortmannin decreased cell viability and the levels of p-Akt and Bcl-2, and promoted cytotoxicity. Additionally, following treatment with TGF-β, EVO decreased variations in morphology, growth, and migration by increasing p21 and p53, and decreasing the protein levels of β-catenin, N-cadherin, vimentin, p-Akt, and MMP-2/9 (54). A previous study demonstrated that co-treatment of SW1736 ATC cells with EVO and PXD101 decreased cell viability, the percentage of viable cells, and Bcl-2 expression, while increasing cytotoxicity, the percentage of apoptotic cells, and the expression of γH2AX, acetyl histone H3, and cleaved PARP. Moreover, EVO increased PXD101 cytotoxicity, ROS production, the expression of γH2AX and cleaved PARP, and the Bcl-2/Bax ratio (55). Different ATC cell lines (SW1736 and KAT4B) have different sensitivities to EVO (56). Previous research revealed that EVO treatment induced a higher apoptotic percentage in SW1736 cells than in KAT4B cells (56). Mechanistic studies demonstrated that the activation of p53 and its downstream proteins, the blockage of MMP, and an increase in intracellular peroxide production leads to EVO-induced G2/M arrest and apoptosis in SW1736 cells. However, in KAT4B cells, EVO induced only a few apoptotic events and only cell accumulation in the G2/M phase. Notably, the alkylation of EVO at position 14 may be crucial in inducing apoptosis in SW1736 cells (56).
Indirubin
Indirubin is a bis-indole alkaloid and the main active constituent of Danggui Longhui Wan, a Chinese traditional medicine used to treat chronic myeloid leukemia treatment (57). It has been reported that indirubin and its derivatives compete with ATP binding and suppress cyclin-dependent kinases (CDKs), resulting in apoptosis and G2/M arrest in cancer cells (58). A previous has shown that 7-bromoindirubin-3′-oxime (7BIO; an indirubin derivative) can impel DNA fragmentation and lactate dehydrogenase liberation in ATC cells (BHT-101, SW1736, HTh7, and C643). However, 7BIO failed to promote caspase activation in these ATC cell lines and increased cleaved PARP fragments only in C643 cells. Moreover, all ATC cell lines except for C643 exhibited a significant increase in the proportion of cells in the G1 phase after treatment with 7BIO. Notably, caspase suppression did not affect the viability of cells after incubation with 7BIO. The authors of the study suggest that 7BIO may be a potential candidate to treat ATC treatment; however, the mechanisms of 7BIO in exerting an effect in different ATC cells require further research (59).
Isoflavones [genistein (Gen) and daidzein]
Gen is an isoflavone that is abundantly present in legumes, lupine, coffee, soybeans, fava bean, and kudzu. Gen exerts its antitumor effects through cell growth inhibition, alteration of the cell cycle, apoptosis induction, angiogenesis suppression, invasion and metastasis suppression, and modulation of epigenetic changes (60). The anticancer effect of Gen in ATC cells (UCLA RO-81-A-1) has been shown as early as 1999 (22). The concurrent treatment of Gen and photodynamic therapy (PDT) mediated by photofrin revealed promising antitumor effects in SUN-80 ATC cells. Treatment using this combination led to antitumor effects including cell growth inhibition, mitochondrial membrane depolarization, apoptosis induction, promotion of ROS production, and alterations in the protein levels of caspase-3/8/9/12, cytochrome c, and other apoptosis-related proteins (61). In addition, it has been reported that Gen suppresses cell viability and promotes apoptosis in ATC cells (SW1736 and 8505C). Additionally, Gen was demonstrated to increase the expression of genes related to the thyroid-differentiated phenotype, such as TG, sodium-iodine symporter (NIS), TPO, TSHR, and TTF2 in both SW1736 and 8505C cells. Notably, Gen reduced colony formation only in 8505C cells but not in SW1736 cells (41). Moreover, co-treatment with thymoquinone and Gen suggests promising anticancer effects in ATC cells. Co-treatment using thymoquinone and Gen is detailed in a subsequent section.
Myricetin
Numerous studies have confirmed the potent anticancer effects of myricetin on cancers such as those of the breast, liver, ovary, colon, and thyroid (62–66). Myricetin has been demonstrated to decrease the growth of ATC cells (SNU-80 HATC) and induce a significant increase in DNA condensation and the proportion of cells in the sub-G1 phase (66). Myricetin was shown to induce ATC cell death by an increase in the activation of caspase cascades and the Bax:Bcl-2 ratio (66). Myricetin was also revealed to alter the mitochondrial membrane potential and increase the release of apoptosis-inducing factor (AIF) from mitochondria to the cytosol (66).
Quercetin
Quercetin is a natural flavonoid that is abundant in the daily diet. Several in vivo and in vitro studies have revealed that quercetin exerts anticancer effects by inhibiting cell proliferation, affecting cell cycle progression, promoting apoptosis, inhibiting angiogenesis and metastasis, and even affecting autophagy (67). Quercetin has been shown to suppress the growth of ATC cells (FRO and ARO) and reduce CD97 expression (68). CD97 is a dedifferentiation marker relevant to cancer progression and metastasis. It was decreased by certain redifferentiating agents such as ATRA in CD97-positive human follicular thyroid carcinoma (FTC-133) cells (69). Quercetin has been demonstrated to increase or induce NIS in FRO cells, but it failed to increase NIS expression in ARO cells (68).
Resveratrol. Resveratrol (trans−3,5,4¢-trihydroxystilbene) was first isolated from the roots of Veratrum album (white hellebore) and Polygonum cuspidatum (Japanese knotweed) and is abundantly present in grapes, berries, and peanuts (70). Resveratrol exhibits potential in the treatment of cancers, such as those of the head and neck, thyroid, breast, lung, stomach, colon, kidney, cervix, bladder, ovary, and skin in humans (71). Resveratrol treatment was demonstrated to suppress the growth of ATC cells (HTh7 and 8505C) by apoptosis induction and S-phase cell cycle arrest. It also increased Notch1 protein expression and activated the Notch1 pathway and upregulated the protein levels of thyroid-specific genes, such as Pax8, NIS, TTF1, and TTF2 (72). A previous study by the authors revealed that resveratrol decreased the total ATC cell count (THJ-16T and THJ-21T) by decreasing cyclin D1 expression, increasing the apoptotic cell fractions, and activation of caspase-3. Resveratrol was not able to suppress the growth of THJ-11T ATC cells; however, it promoted ATRA sensitivity in THJ-11T ATC cells by suppressing peroxisome proliferator-activated receptor-β/δ and increasing cellular retinoic acid receptor-β and cellular retinoic acid-binding protein (CRABP)2. In addition, the efficacy of resveratrol in increasing thyroglobulin and E-cadherin levels was manifested by the appearance of membranous E-cadherin in THJ-11T ATC cells (13). Liu et al researched the ability of resveratrol in improving ATRA sensitivity in THJ-11T ATC cells. Resveratrol abolished CRABP2 methylation through demethylation of three CpG methylation sites on the promoter of CRABP2 and due to its suppressive effect on DNA methyltransferase (DNMT1 and DNMT3A) protein levels (73). Wu et al explored the association between the activation of STAT3 signaling and the antitumor effect of resveratrol in ATC cells (THJ-11T, THJ-16T, and THJ-21T). In this study it was revealed that resveratrol suppressed LIF and STAT3 expression and inhibited p-STAT3 nuclear translocation in THJ-16T and THJ-21T cells but not in THJ-11T cells, indicating LIF upregulation and more frequent p-STAT3 nuclear translocation. A STAT3 inhibitor, AG490, which significantly prevents p-STAT3 nuclear translocation, reversed the resveratrol toleration of THJ-11T cells (74). Another study by Zheng et al demonstrated that the molecular mechanisms of the anticancer effects of resveratrol are associated to resveratrol-induced oxidative damage due to increased ROS and oxidative stress-induced mitochondrial swelling. Compared with untreated THJ-11T cells, resveratrol-treated THJ-16T cells exhibited a marked increase in ROS generation, a decrease in catalase (CAT) and SOD2 levels, stronger activation of caspase-9/caspase-3, and more impaired mitochondrial function. In addition, co-treatment with antioxidants such as N-acetylcysteine attenuated the antitumor effects of resveratrol in THJ-16T cells (75). Xiong et al explored the redifferentiating effect of resveratrol in THJ-16T and THJ-21T ATC cells and determined that resveratrol increased phosphatase and tensin homolog (PTEN) levels, resulting in distinct NIS and PTEN nuclear co-translocation in THJ-16T and THJ-21T ATC cells. However, NIS did not appear on the ATC cell membrane (76). In addition, resveratrol in different delivery systems has also exhibited potential in treating ATC. Resveratrol sustained-release targeting nanoparticles successfully suppressed ATC cell growth in vivo. Resveratrol overcame the side effects and secondary drug resistance of docetaxel/doxorubicin in treating ATC xenograft models (77).
Thymoquinone (TQ)
TQ (2-isopropyl-5-methyl-1,4-benzoquinone) is a bioactive substance isolated from Nigella sativa seeds (78). TQ exerts anticancer effects on several types of cancers, such as skin cancer, glioblastoma, breast cancer, pancreatic cancer, colorectal carcinoma, bladder cancer, and cervical squamous carcinoma (79). The combined intervention of TQ and Gen has been demonstrated to suppress cell survival, angiogenesis, telomerase activation, and increase pro-apoptotic protein expression in ATC cells (CAL-62 and ACC 448). The anticancer effects of the combination of TQ and Gen were attributed to a reduction of NF-κB, VEGF, and human telomerase reverse transcriptase (hTERT) and suppression of p21 and PTEN. Moreover, co-treatment with TQ and Gen was more effective in ATC cells than in FTC cells (80).
Triptolide (TPL)
TPL is a diterpenoid trioxide isolated from a perennial vine-like Chinese herb Tripterygium wilfordii Hook. f. (81). TPL inhibits cancer cell growth and shows promising antitumor effects in cancers such as prostate cancer, ovarian cancer, breast cancer, neuroblastoma, lung cancer, acute myeloid leukemia, and multiple gastrointestinal cancers in preclinical studies (82). Previous research revealed the anticancer effects of TPL in ATC cells (TA-K), including the inhibition of cell growth and induction of apoptosis by suppression of the NF-κB pathway but not the p53 signaling pathway (83). Inhibition of the transcriptional activation of NF-κB by TPL in TA-K cells was due to the blocking between the p65 subunit and CREB-binding protein (CBP)/p300 in the early stages and a decrease in p65 expression in the later stage. In addition, TPL decreased the protein levels of proliferation, angiogenesis, and invasion targets such as cyclin D1, VEGF, and urokinase-type plasminogen activator in ATC cells (TA-K and 8505C) (84). A previous study revealed that TPL has an angiogenesis-suppressive effect in both TK-A cells and human umbilical vein endothelial cells; these findings were also reported in vivo studies (85). Furthermore, TPL may be considered an adjuvant in the treatment of 8505C ATC cells. When used as an adjuvant, BIIB021, a novel heat shock protein 90 inhibitor, exhibited improved anticancer effects in decreasing cell viability and dead cell percentage and increasing cytotoxicity compared with BIIB021 treatment alone. Co-treatment with BIIB021 and TPL increased cytotoxicity in 8505C ATC cells through activation of DNA damage response, suppression of the NF-κB and PI3K/Akt/mTOR pathways, and a decrease in surviving (86).
3. Discussion
Phytochemicals have five broad unique aspects and limitations. First, some phytochemicals promote the activation of ROS in ATC cells. The anticancer effects of phytochemicals in ATC cells, including cell growth inhibition, suppression of angiogenesis, and autophagy modulation, promotion of apoptosis cell cycle arrest, and ROS activation are presented in Table I. Phytochemicals are generally considered to have the ability to reduce ROS activity in other cancers (87–89). It is unusual for phytochemicals to have the capacity to increase the activation of ROS in ATC cells. Second, unlike other anticancer agents, phytochemicals exert therapeutic effects on numerous cancers and are associated only with a few side effects (90). Third, phytochemicals exhibit promise as adjuvants in enhancing the sensitivities of other anticancer agents such as PLX4032, TRAIL, docetaxel, TGF-β, wortmannin, PXD101, ATRA, and BIIB021 (25,26,43,54,55,73,86). However, the varying sensitivities of different ATC cell lines often restrict phytochemical use (13,59,68). Moreover, drug resistance exhibited by ATC cells continues to pose a serious challenge. Fourth, the active metabolites of phytochemicals cannot always reach the target tissue at therapeutic concentrations. Furthermore, urinary excretion, short elimination half-life, and water solubility decrease the bioavailability of phytochemicals (91). Some research groups have improved the bioavailability of phytochemicals (92), thereby increasing the possibility of their use as biomedicine. Fifth, clinical trials are seldom conducted on phytochemicals; therefore, data on their efficacy in treating patients with ATC are lacking. The majority of references presented in this review are studies on the anticancer effects of phytochemicals in ATC cells. In animal models, daidzein, evodiamine, and resveratrol have been demonstrated to be effective as anticancer or chemopreventive agents (93,94). Only a few studies have reported that curcumin decreases the genotoxicity of 131I therapy in patients with differentiated thyroid cancer (DTC) (95). A supplement containing spirulina, curcumin, and Boswellia has been shown to reduce the size of thyroid nodules in euthyroid patients with benign thyroid nodules (96).
Table I.
Anticancer effects of different phytochemicals in ATC cells.
| Phytochemicals | Cell growth inhibition | Apoptosis induction | Cell cycle arrest | Angiogenesis suppression | Autophagy modulation | ROS activation |
|---|---|---|---|---|---|---|
| Aloperine | √ | √ | 0 | 0 | √ | 0 |
| Apigenin | √ | √ | 0 | 0 | 0 | 0 |
| Artemisinin | √ | 0 | √ | 0 | 0 | 0 |
| Baicalein | √ | √ | √ | 0 | √ | 0 |
| Chrysin | √ | √ | 0 | 0 | 0 | 0 |
| Curcumin | √ | √ | √ | 0 | 0 | 0 |
| Deguelin | √ | √ | √ | √ | 0 | 0 |
| Epigallocatechin-3-gallate | √ | √ | √ | √ | 0 | |
| Evodiamine | √ | √ | √ | 0 | 0 | √ |
| Indirubin | √ | √ | √ | 0 | 0 | 0 |
| Isoflavones (genistein and daidzein) | √ | √ | 0 | 0 | 0 | √ |
| Myricetin | √ | √ | √ | 0 | 0 | 0 |
| Quercetin | √ | √ | √ | √ | √ | 0 |
| Resveratrol | √ | √ | √ | 0 | 0 | √ |
| Thymoquinone | √ | √ | 0 | √ | 0 | 0 |
| Triptolide | √ | √ | 0 | √ | 0 | 0 |
ATC, anaplastic thyroid cancer; ROS, reactive oxygen species.
There are five types of thyroid cancer including ATC, medullary thyroid carcinoma DTC, poorly differentiated thyroid carcinoma, and Hurthle cell thyroid carcinoma (97). ATC is one of the most aggressive human carcinomas, which arises from the follicular cells in the thyroid gland. Although both ATC and DTC originate from thyroid follicular cells, their clinical and biological features vary considerably. The primary differences are shown in Table II. i) Incidence: ATC only accounts for <1% of the total cases of thyroid tumors (98), whereas DTC accounts for >95% of cases (99). ii) Gender ratio: DTC patients have a female:male ratio of 3:1 (100), whereas this ratio in ATC is 1.5:2 (101). iii) Mortality: Although the incidence of ATC is quite low (3.6% of all cases of thyroid cancer in different areas) (102), deaths due to ATC account for 14–39% of all deaths due to thyroid cancer. The average survival time of patients with ATC was 5–6 months (101). iv) Migration and invasiveness: ATC is more prone to aggressive local disease and distant metastasis than DTC. Approximately 97% of patients with ATC present with a rapidly enlarging thyroid mass (103). Almost 50% of patients with ATC were found to have distant metastasis at diagnosis. Metastasis also occurred in approximately 25% of patients during their disease course (104). Metastases mainly involve the cervical lymph nodes in patients with DTC. v) Biological features: ATC cells lose some biological features such as iodine-uptake capacity and TSH dependence, which are characteristic features of normal follicular cells (101). These features are still present in DTC, and radioiodine ablation and TSH suppression are necessary components of DTC treatment (98). vi) Sensitivity to chemotherapy drugs: ATC is resistant to numerous first-line anticancer drugs such as sorafenib and lenvatinib used in a clinical setting to treat DTC (98,105).
Table II.
Differences between ATC and DTC.
| Type of cancer | Incidence (of total cases) | Sex ratio (F:M) | Lethality rate | Migration and invasiveness | Thyroid-specific features | Sensitivity to chemotherapy drugs |
|---|---|---|---|---|---|---|
| DTC | >95% | 3:1 | Normal | Normal | Partly | Normal |
| ATC | <1% | 1.5:2 | High | Easily appearing | None | Poor |
ATC, anaplastic thyroid cancer; DTC, differentiated thyroid cancer.
The anticancer effects of phytochemicals in DTC and ATC differ. In DTC cells, resveratrol treatment led to cell growth suppression, induction of apoptosis, cell cycle arrest, and redifferentiation (68,106). Treatment with resveratrol (1–10 µM), was demonstrated to increase the activation of MAPK and the protein levels of nuclear p53 protein, c-Fos, c-Jun, and p21 in DTC cells (107). Moreover, resveratrol enhanced the activation of Notch1, which is considered a regulator of thyroid-specific gene expression (99) and the cause of autophagic flux in DTC cells (108,109). However, this effect of resveratrol was not observed in ATC cells. For example, resveratrol promoted the apoptosis of ATC cells but did not increase MAPK activation and p53 expression. Resveratrol also increased the activation of Notch1 signaling and the protein expression of thyroid-specific genes. Unfortunately, the location of important thyroid-specific proteins, such as NIS, differs from that in normal thyroid cells and is accompanied by a loss of function (72,76). Quercetin was revealed to impel NIS protein expression and decrease CD97 protein levels, a de-differentiation marker, in DTC cells (68). However, while quercetin decreased CD expression in both FRO and ARO ATC cells, it only induced NIS protein expression in FRO ATC cells (68). These studies suggest that ATC, but not DTC, may have unique drug-resistance mechanisms. Therefore, effective drugs and therapies are urgently required for undifferentiated thyroid cancer.
The mechanisms of drug resistance in ATC are poorly understood. Some studies have hypothesized and found evidence for the following aspects: i) STAT3 activation: Wu et al reported that activation of STAT3 signaling is associated with the resistance of ATC cells to resveratrol (74). Wang et al established the connection between STAT3 and ATC resistance to BRAF inhibition (110). ii) Drug- efflux pumps: Abbasifarid et al suggested that ATP-binding cassette (ABC) transporters ABCC1, ABCG2, and ABCB1 are the key determinants of the resistance of ATC to chemotherapy (8). ABC transporters efflux anticancer drugs and play a role in the development of drug resistance in cancer cells (111). In addition, signal transduction pathways such as PI3K/Akt (112), MAPK (113) and Notch (114) not only regulate the expression of ABCC1, ABCG2, and ABCB1 but also participate in the development of drug resistance. iii) Energy metabolism: Ma and Cheng demonstrated that metabolic reprogramming in ATC cells confers upon them a capacity of resistance to doxorubicin. Targeting 6-phosphogluconate dehydrogenase overcame this drug resistance (115). A previous study by one of the authors determined that PDH activity plays a role in the transient resistance of ATC to artemisinin (116).
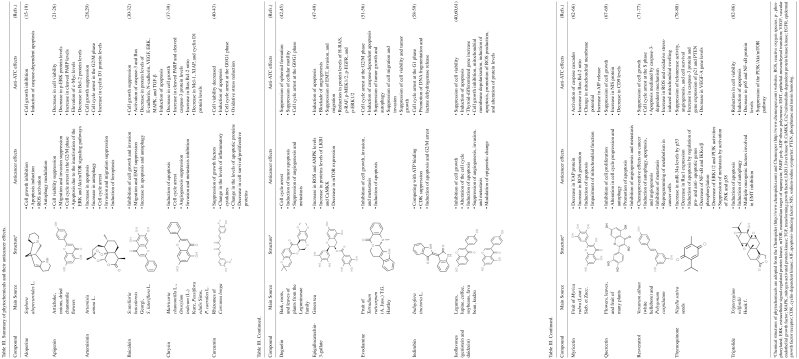
Phytochemicals such as resveratrol affect the phosphorylation and nuclear translocation of STAT3 (74). Furthermore, they regulate some signaling pathways that participate in drug resistance in ATC. For example, aloperine, APG and baicalein were demonstrated to suppress Akt activation in ATC cells (19,26,32). Baicalein inhibited MAPK phosphorylation (34) and chysin increased Notch1 expression. Cancer is a metabolic disease with a special metabolic profile in tumor cells (117). Tumor cells depend on increased aerobic glycolysis by mitochondrial oxidative phosphorylation to provide energy for their rapid growth, invasion, and drug resistance. There are three major interferences in tumor therapy, namely, dynamic cancer ecosystems, profitable temporal and spatial diversity of environmental conditions, and heritable cell phenotypes (118). The evolution phenomenon known as competitive release explains how drug-resistant cells attain a better opportunity to rapidly proliferate by eliminating the drug-sensitive cells (118). It reveals that traditional anticancer therapy to kill the majority of tumor cells as a strategy to treat metastatic cancer is unreasonable from the point of evolution. However, some alternative strategies have focused on evolution-based methods that yield more benefits in the long-term control compared with traditional therapy by only eliminating tumor cells. Treatment with phytochemicals can alter several signaling cascades and the modulation of the metabolic properties of cancer cells (119). However, they also influence the mitochondrial membrane potential and regulate the mitochondrial metabolic pathways (120). For example, resveratrol not only exerts its antitumor effects on ATC cells alone but can also reverse drug resistance in these cells. Treatment of resveratrol-sensitive ATC cells with resveratrol alone, leads to changes in the morphological characteristics of mitochondria and an increase in ROS production (75). These results indicate that resveratrol suppresses ATC cell growth and drug resistance through an impaired effect on mitochondria. In a previous study by one of the authors, it was determined that treatment with ART significantly changed mitochondrial protein levels including the downregulation of COX7A2 and COX2 and the upregulation of YEM1L1, ALAS1, COX14, and OAT after 48 h of treatment. CAL-62 cells showed a transient and reversible resistance to ART (only at 48 h), which was correlated to the time-dependent changes in PDK1, HIF1a, and PDHA levels (117). These results suggest that improved mitochondrial function may strongly be associated to drug resistance in ATC cells. The inhibitory effect of phytochemicals of ATC cells is important in overcoming drug resistance. The findings of the present review (Table III) may improve the utility of phytochemicals as adjuvants in the therapy of ATC, help prevent drug resistance, and provide a novel perspective for further research on ATC therapy.
Table III.
Summary of phytochemicals and their anticancer effects.
Acknowledgements
We are thankful for the generous support of Shandong Provincial Natural Science Foundation.
Funding Statement
This review was financially supported by the Shandong Provincial Natural Science Foundation, China (grant no. ZR2020QC075).
Availability of data and materials
Not applicable.
Authors' contributions
JZ and YL contributed to the conception of the present review. All authors (YL, JZ, HZ and ZD) contributed to the resources, data curation, and writing of the manuscript as well as the literature review analysis. ZD and YL reviewed and edited the manuscript. Data authentication is not applicable. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.O'Neill JP, Shaha AR. Anaplastic thyroid cancer. Oral Oncol. 2013;49:702–706. doi: 10.1016/j.oraloncology.2013.03.440. [DOI] [PubMed] [Google Scholar]
- 2.Saini S, Tulla K, Maker AV, Burman KD, Prabhakar BS. Therapeutic advances in anaplastic thyroid cancer: A current perspective. Mol Cancer. 2018;17:154. doi: 10.1186/s12943-018-0903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tesselaar MH, Crezee T, Schuurmans I, Gerrits D, Nagarajah J, Boerman OC, van Engen-van Grunsven I, Smit JWA, Netea-Maier RT, Plantinga TS. Digitalislike compounds restore hNIS expression and iodide uptake capacity in anaplastic thyroid cancer. J Nucl Med. 2018;59:780–786. doi: 10.2967/jnumed.117.200675. [DOI] [PubMed] [Google Scholar]
- 4.Haugen BR, Sawka AM, Alexander EK, Bible KC, Caturegli P, Doherty GM, Mandel SJ, Morris JC, Nassar A, Pacini F, et al. American thyroid association guidelines on the management of thyroid nodules and differentiated thyroid cancer task force review and recommendation on the proposed renaming of encapsulated follicular variant papillary thyroid carcinoma without invasion to noninvasive follicular thyroid neoplasm with papillary-like nuclear features. Thyroid. 2017;27:481–483. doi: 10.1089/thy.2016.0628. [DOI] [PubMed] [Google Scholar]
- 5.Haddad RI, Nasr C, Bischoff L, Busaidy NL, Byrd D, Callender G, Dickson P, Duh QY, Ehya H, Goldner W, et al. NCCN guidelines insights: Thyroid carcinoma, version 2.2018. J Natl Compr Cancer Netw. 2018;16:1429–1440. doi: 10.6004/jnccn.2018.0089. [DOI] [PubMed] [Google Scholar]
- 6.Zheng X, Cui D, Xu S, Brabant G, Derwahl M. Doxorubicin fails to eradicate cancer stem cells derived from anaplastic thyroid carcinoma cells: Characterization of resistant cells. Int J Oncol. 2010;37:307–315. doi: 10.3892/ijo_00000679. [DOI] [PubMed] [Google Scholar]
- 7.Xu Y, Han YF, Ye B, Zhang YL, Dong JD, Zhu SJ, Chen J. MiR-27b-3p is involved in doxorubicin resistance of human anaplastic thyroid cancer cells via targeting peroxisome proliferator-activated receptor gamma. Basic Clin Pharmacol Toxicol. 2018;123:670–677. doi: 10.1111/bcpt.13076. [DOI] [PubMed] [Google Scholar]
- 8.Abbasifarid E, Sajjadi-Jazi SM, Beheshtian M, Samimi H, Larijani B, Haghpanah V. The role of ATP-binding cassette transporters in the chemoresistance of anaplastic thyroid cancer: A systematic review. Endocrinology. 2019;160:2015–2023. doi: 10.1210/en.2019-00241. [DOI] [PubMed] [Google Scholar]
- 9.Lan L, Basourakos S, Cui D, Zuo X, Deng W, Huo L, Chen H, Zhang G, Deng L, Shi B, Luo Y. ATRA increases iodine uptake and inhibits the proliferation and invasiveness of human anaplastic thyroid carcinoma SW1736 cells: Involvement of β-catenin phosphorylation inhibition. Oncol Lett. 2017;14:7733–7738. doi: 10.3892/ol.2017.7225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Avila-Carrasco L, Majano P, Sánchez-Toméro JA, Selgas R, López-Cabrera M, Aguilera A, Mateo GG. Natural plants compounds as modulators of epithelial-to-mesenchymal transition. Front Pharmacol. 2019;10:715. doi: 10.3389/fphar.2019.00715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen CY, Kao CL, Liu CM. The cancer prevention, anti-inflammatory and anti-oxidation of bioactive phytochemicals targeting the TLR4 signaling pathway. Int J Mol Sci. 2018;19:2729. doi: 10.3390/ijms19092729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asadi-Samani M, Kooti W, Aslani E, Shirzad H. A systematic review of Iran's medicinal plants with anticancer effects. J Evid Based Complement Altern Med. 2016;21:143–153. doi: 10.1177/2156587215600873. [DOI] [PubMed] [Google Scholar]
- 13.Li YT, Tian XT, Wu ML, Zheng X, Kong QY, Cheng XX, Zhu GW, Liu J, Li H. Resveratrol suppresses the growth and enhances retinoic acid sensitivity of anaplastic thyroid cancer cells. Int J Mol Sci. 2018;19:1030. doi: 10.3390/ijms19041030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang R, Deng X, Gao Q, Wu X, Han L, Gao X, Zhao S, Chen W, Zhou R, Li Z, Bai C. Sophora alopecuroides L: An ethnopharmacological, phytochemical, and pharmacological review. J Ethnopharmacol. 2020;248:112172. doi: 10.1016/j.jep.2019.112172. [DOI] [PubMed] [Google Scholar]
- 15.Tian D, Li Y, Li X, Tian Z. Aloperine inhibits proliferation, migration and invasion and induces apoptosis by blocking the Ras signaling pathway in human breast cancer cells. Mol Med Rep. 2018;18:3699–3710. doi: 10.3892/mmr.2018.9419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ling Z, Guan H, You Z, Wang C, Hu L, Zhang L, Wang Y, Chen S, Xu B, Chen M. Aloperine executes antitumor effects through the induction of apoptosis and cell cycle arrest in prostate cancer in vitro and in vivo. Onco Targets Ther. 2018;11:2735–2743. doi: 10.2147/OTT.S165262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu M, Liu J, Su Y, Liu J, Wu C, Zhao B. Aloperine induces apoptosis by a reactive oxygen species activation mechanism in human ovarian cancer cells. Protein Pept Lett. 2020;27:860–869. doi: 10.2174/0929866527666200320094313. [DOI] [PubMed] [Google Scholar]
- 18.Yu HI, Shen HC, Chen SH, Lim YP, Chuang HH, Tai TS, Kung FP, Lu CH, Hou CY, Lee YR, et al. Autophagy modulation in human thyroid cancer cells following aloperine treatment. Int J Mol Sci. 2019;20:5315. doi: 10.3390/ijms20215315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee YR, Chen SH, Lin CY, Chao WY, Lim YP, Yu HI, Lu CH. In vitro antitumor activity of aloperine on human thyroid cancer cells through caspase-dependent apoptosis. Int J Mol Sci. 2018;19:312. doi: 10.3390/ijms19010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharma A, Ghani A, Sak K, Tuli HS, Sharma AK, Setzer WN, Sharma S, Das AK. Probing into therapeutic anti-cancer potential of apigenin: Recent trends and future directions. Recent Pat Inflamm Allergy Drug Discov. 2019;13:124–133. doi: 10.2174/1872213X13666190816160240. [DOI] [PubMed] [Google Scholar]
- 21.Zhao G, Han X, Cheng W, Ni J, Zhang Y, Lin J, Song Z. Apigenin inhibits proliferation and invasion, and induces apoptosis and cell cycle arrest in human melanoma cells. Oncol Rep. 2017;37:2277–2285. doi: 10.3892/or.2017.5450. [DOI] [PubMed] [Google Scholar]
- 22.Yin F, Giuliano AE, Van Herle AJ. Growth inhibitory effects of flavonoids in human thyroid cancer cell lines. Thyroid. 1999;9:369–376. doi: 10.1089/thy.1999.9.369. [DOI] [PubMed] [Google Scholar]
- 23.Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG, Yoo HJ, Lee SJ. Apigenin induces c-Myc-mediated apoptosis in FRO anaplastic thyroid carcinoma cells. Mol Cell Endocrinol. 2013;369:130–139. doi: 10.1016/j.mce.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 24.Yin F, Giuliano AE, Van Herle AJ. Signal pathways involved in apigenin inhibition of growth and induction of apoptosis of human anaplastic thyroid cancer cells (ARO) Anticancer Res. 1999;19:4297–4303. [PubMed] [Google Scholar]
- 25.Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG, Yoo HJ, Lee SJ. Akt inhibition enhances the cytotoxic effect of apigenin in combination with PLX4032 in anaplastic thyroid carcinoma cells harboring BRAFV600E. J Endocrinol Invest. 2013;36:1099–1104. doi: 10.3275/9099. [DOI] [PubMed] [Google Scholar]
- 26.Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG, Yoo HJ, Lee SJ. Suppression of AKT potentiates synergistic cytotoxicity of apigenin with trail in anaplastic thyroid carcinoma cells. Anticancer Res. 2015;35:6529–6537. [PubMed] [Google Scholar]
- 27.Ma N, Zhang Z, Liao F, Jiang T, Tu Y. The birth of artemisinin. Pharmacol Ther. 2020;216:107658. doi: 10.1016/j.pharmthera.2020.107658. [DOI] [PubMed] [Google Scholar]
- 28.Zhu S, Yu Q, Huo C, Li Y, He L, Ran B, Chen J, Li Y, Liu W. Ferroptosis: A novel mechanism of artemisinin and its derivatives in cancer therapy. Curr Med Chem. 2021;28:329–345. doi: 10.2174/0929867327666200121124404. [DOI] [PubMed] [Google Scholar]
- 29.Li Y. Pyrvinium pamoate can overcome artemisinin's resistance in anaplastic thyroid cancer. BMC Complement Med Ther. 2021;21:156. doi: 10.1186/s12906-021-03332-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zeng Q, Zhang Y, Zhang W, Guo Q. Baicalein suppresses the proliferation and invasiveness of colorectal cancer cells by inhibiting snail-induced epithelial-mesenchymal transition. Mol Med Rep. 2020;21:2544–2552. doi: 10.3892/mmr.2020.11051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu G, Chen L, Hu Y, Yuan Z, Luo Y, Xiong Y. Antitumor effects of baicalein and its mechanism via TGFβ pathway in cervical cancer hela cells. Evid Based Complement Altern Med. 2021;2021:5527190. doi: 10.1155/2021/5527190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yan W, Ma X, Zhao X, Zhang S. Baicalein induces apoptosis and autophagy of breast cancer cells via inhibiting PI3K/AKT pathway in vivo and vitro. Drug Des Devel Ther. 2018;12:3961–3972. doi: 10.2147/DDDT.S181939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Park CH, Han SE, Nam-Goong IS, Kim YI, Kim ES. Combined effects of baicalein and docetaxel on apoptosis in 8505c anaplastic thyroid cancer cells via downregulation of the ERK and Akt/mTOR pathways. Endocrinol Metab (Seoul) 2018;33:121–132. doi: 10.3803/EnM.2018.33.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Han SE, Park CH, Nam-Goong IS, Kim YI, Kim ES. Anticancer effects of baicalein in FRO thyroid cancer cells through the up-regulation of ERK/p38 MAPK and Akt pathway. In Vivo. 2019;33:375–382. doi: 10.21873/invivo.11484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Naz S, Imran M, Rauf A, Orhan IE, Shariati MA, Iahtisham-Ul-Haq, IqraYasmin, Shahbaz M, Qaisrani TB, Shah ZA, et al. Chrysin: Pharmacological and therapeutic properties. Life Sci. 2019;235:116797. doi: 10.1016/j.lfs.2019.116797. [DOI] [PubMed] [Google Scholar]
- 36.Jung J. Emerging utilization of chrysin using nanoscale modification. J Nanomater. 2016;2016:e2894089. doi: 10.1155/2016/2894089. [DOI] [Google Scholar]
- 37.Kasala ER, Bodduluru LN, Madana RM, Athira KV, Gogoi R, Barua CC. Chemopreventive and therapeutic potential of chrysin in cancer: Mechanistic perspectives. Toxicol Lett. 2015;233:214–225. doi: 10.1016/j.toxlet.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 38.Phan T, Yu XM, Kunnimalaiyaan M, Chen H. Antiproliferative effect of chrysin on anaplastic thyroid cancer. J Surg Res. 2011;170:84–88. doi: 10.1016/j.jss.2011.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yu XM, Phan T, Patel PN, Jaskula-Sztul R, Chen H. Chrysin activates notch1 signaling and suppresses tumor growth of anaplastic thyroid carcinoma in vitro and in vivo. Cancer. 2013;119:774–781. doi: 10.1002/cncr.27742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giordano A, Tommonaro G. Curcumin and cancer. Nutrients. 2019;11:2376. doi: 10.3390/nu11102376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allegri L, Rosignolo F, Mio C, Filetti S, Baldan F, Damante G. Effects of nutraceuticals on anaplastic thyroid cancer cells. J Cancer Res Clin Oncol. 2018;144:285–294. doi: 10.1007/s00432-017-2555-7. [DOI] [PubMed] [Google Scholar]
- 42.Kocdor MA, Cengiz H, Ates H, Kocdor H. Inhibition of cancer stem-like phenotype by curcumin and deguelin in CAL-62 anaplastic thyroid cancer cells. Anticancer Agents Med Chem. 2019;19:1887–1898. doi: 10.2174/1871520619666191004144025. [DOI] [PubMed] [Google Scholar]
- 43.Hong JM, Park CS, Nam-Goong IS, Kim YS, Lee JC, Han MW, Choi JI, Kim YI, Kim ES. Curcumin enhances docetaxel-induced apoptosis of 8505C anaplastic thyroid carcinoma cells. Endocrinol Metab (Seoul) 2014;29:54–61. doi: 10.3803/EnM.2014.29.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boyd J, Han A. Deguelin and its role in chronic diseases. Adv Exp Med Biol. 2016;929:363–375. doi: 10.1007/978-3-319-41342-6_16. [DOI] [PubMed] [Google Scholar]
- 45.Tuli HS, Mittal S, Loka M, Aggarwal V, Aggarwal D, Masurkar A, Kaur G, Varol M, Sak K, Kumar M, et al. Deguelin targets multiple oncogenic signaling pathways to combat human malignancies. Pharmacol Res. 2021;166:105487. doi: 10.1016/j.phrs.2021.105487. [DOI] [PubMed] [Google Scholar]
- 46.Kim HS, Quon MJ, Kim JA. New insights into the mechanisms of polyphenols beyond antioxidant properties; lessons from the green tea polyphenol, epigallocatechin 3-gallate. Redox Biol. 2014;2:187–195. doi: 10.1016/j.redox.2013.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hayakawa S, Ohishi T, Miyoshi N, Oishi Y, Nakamura Y, Isemura M. Anti-cancer effects of green tea epigallocatchin–3-gallate and coffee chlorogenic acid. Molecules. 2020;25:4553. doi: 10.3390/molecules25194553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu D, Liu Z, Li J, Zhang Q, Zhong P, Teng T, Chen M, Xie Z, Ji A, Li Y. Epigallocatechin-3-gallate inhibits the growth and increases the apoptosis of human thyroid carcinoma cells through suppression of EGFR/RAS/RAF/MEK/ERK signaling pathway. Cancer Cell Int. 2019;19:43. doi: 10.1186/s12935-019-0762-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li T, Zhao N, Lu J, Zhu Q, Liu X, Hao F, Jiao X. Epigallocatechin gallate (EGCG) suppresses epithelial-mesenchymal transition (EMT) and invasion in anaplastic thyroid carcinoma cells through blocking of TGF-β1/smad signaling pathways. Bioengineered. 2019;10:282–291. doi: 10.1080/21655979.2019.1632669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jiang ZB, Huang JM, Xie YJ, Zhang YZ, Chang C, Lai HL, Wang W, Yao XJ, Fan XX, Wu QB, et al. Evodiamine suppresses non-small cell lung cancer by elevating CD8+ T cells and downregulating the MUC1-C/PD-L1 axis. J Exp Clin Cancer Res. 2020;39:249. doi: 10.1186/s13046-020-01741-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Luo C, Ai J, Ren E, Li J, Feng C, Li X, Luo X. Research progress on evodiamine, a bioactive alkaloid of Evodiae fructus: Focus on its anti-cancer activity and bioavailability (Review) Exp Ther Med. 2021;22:1327. doi: 10.3892/etm.2021.10762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen MC, Yu CH, Wang SW, Pu HF, Kan SF, Lin LC, Chi CW, Ho LLT, Lee CH, Wang PS. Anti-proliferative effects of evodiamine on human thyroid cancer cell line ARO. J Cell Biochem. 2010;110:1495–1503. doi: 10.1002/jcb.22716. [DOI] [PubMed] [Google Scholar]
- 53.Yu HI, Chou HC, Su YC, Lin LH, Lu CH, Chuang HH, Tsai YT, Liao EC, Wei YS, Yang YT, et al. Proteomic analysis of evodiamine-induced cytotoxicity in thyroid cancer cells. J Pharm Biomed Anal. 2018;160:344–350. doi: 10.1016/j.jpba.2018.08.008. [DOI] [PubMed] [Google Scholar]
- 54.Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG, Lee SJ. Evodiamine suppresses survival, proliferation, migration and epithelial-mesenchymal transition of thyroid carcinoma cells. Anticancer Res. 2018;38:6339–6352. doi: 10.21873/anticanres.12992. [DOI] [PubMed] [Google Scholar]
- 55.Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG, Lee SJ. Evodiamine in combination with histone deacetylase inhibitors has synergistic cytotoxicity in thyroid carcinoma cells. Endocrine. 2019;65:110–120. doi: 10.1007/s12020-019-01885-1. [DOI] [PubMed] [Google Scholar]
- 56.Chien CC, Wu MS, Chou SW, Jargalsaikhan G, Chen YC. Roles of reactive oxygen species, mitochondrial membrane potential, and p53 in evodiamine-induced apoptosis and G2/M arrest of human anaplastic thyroid carcinoma cells. Chin Med. 2021;16:134. doi: 10.1186/s13020-021-00505-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xiao Z, Hao Y, Liu B, Qian L. Indirubin and meisoindigo in the treatment of chronic myelogenous leukemia in China. Leuk Lymphoma. 2002;43:1763–1768. doi: 10.1080/1042819021000006295. [DOI] [PubMed] [Google Scholar]
- 58.Hoessel R, Leclerc S, Endicott JA, Nobel ME, Lawrie A, Tunnah P, Leost M, Damiens E, Marie D, Marko D, et al. Indirubin, the active constituent of a Chinese antileukaemia medicine, inhibits cyclin-dependent kinases. Nat Cell Biol. 1999;1:60–67. doi: 10.1038/9035. [DOI] [PubMed] [Google Scholar]
- 59.Broecker-Preuss M, Becher-Boveleth N, Gall S, Rehmann K, Schenke S, Mann K. Induction of atypical cell death in thyroid carcinoma cells by the indirubin derivative 7-bromoindirubin-3′-oxime (7BIO) Cancer Cell Int. 2015;15:97. doi: 10.1186/s12935-015-0251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mukund V, Mukund D, Sharma V, Mannarapu M, Alam A. Genistein: Its role in metabolic diseases and cancer. Crit Rev Oncol Hematol. 2017;119:13–22. doi: 10.1016/j.critrevonc.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 61.Ahn JC, Biswas R, Chung PS. Combination with genistein enhances the efficacy of photodynamic therapy against human anaplastic thyroid cancer cells. Lasers Surg Med. 2012;44:840–849. doi: 10.1002/lsm.22095. [DOI] [PubMed] [Google Scholar]
- 62.Li M, Chen J, Yu X, Xu S, Li D, Zheng Q, Yin Y. Myricetin suppresses the propagation of hepatocellular carcinoma via down-regulating expression of YAP. Cells. 2019;8:358. doi: 10.3390/cells8040358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Knickle A, Fernando W, Greenshields AL, Rupasinghe HPV, Hoskin DW. Myricetin-induced apoptosis of triple-negative breast cancer cells is mediated by the iron-dependent generation of reactive oxygen species from hydrogen peroxide. Food Chem Toxicol. 2018;118:154–167. doi: 10.1016/j.fct.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 64.Xu Y, Xie Q, Wu S, Yi D, Yu Y, Liu S, Li S, Li Z. Myricetin induces apoptosis via endoplasmic reticulum stress and DNA double-strand breaks in human ovarian cancer cells. Mol Med Rep. 2016;13:2094–2100. doi: 10.3892/mmr.2016.4763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ma L, Cao X, Wang H, Lu K, Wang Y, Tu C, Dai Y, Meng Y, Li Y, Yu P, et al. Discovery of Myricetin as a potent inhibitor of human flap endonuclease 1, which potentially can be used as sensitizing agent against HT-29 human colon cancer cells. J Agric Food Chem. 2019;67:1656–1665. doi: 10.1021/acs.jafc.8b05447. [DOI] [PubMed] [Google Scholar]
- 66.Jo S, Ha TK, Han SH, Kim ME, Jung I, Lee HW, Bae SK, Lee JS. Myricetin induces apoptosis of human anaplastic thyroid cancer cells via mitochondria dysfunction. Anticancer Res. 2017;37:1705–1710. doi: 10.21873/anticanres.11502. [DOI] [PubMed] [Google Scholar]
- 67.Tang SM, Deng XT, Zhou J, Li QP, Ge XX, Miao L. Pharmacological basis and new insights of quercetin action in respect to its anti-cancer effects. Biomed Pharmacother. 2020;121:109604. doi: 10.1016/j.biopha.2019.109604. [DOI] [PubMed] [Google Scholar]
- 68.Kang HJ, Youn YK, Hong MK, Kim LS. Antiproliferation and redifferentiation in thyroid cancer cell lines by polyphenol phytochemicals. J Korean Med Sci. 2011;26:893–899. doi: 10.3346/jkms.2011.26.10.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hoang-Vu C, Bull K, Schwarz I, Krause G, Schmutzler C, Aust G, Köhrle J, Dralle H. Regulation of CD97 protein in thyroid carcinoma. J Clin Endocrinol Metab. 1999;84:1104–1109. doi: 10.1210/jcem.84.3.5557. [DOI] [PubMed] [Google Scholar]
- 70.Ren B, Kwah MXY, Liu C, Ma Z, Shanmugam MK, Ding L, Xiang X, Ho PCL, Wang L, Ong PS, Goh BC. Resveratrol for cancer therapy: Challenges and future perspectives. Cancer Lett. 2021;515:63–72. doi: 10.1016/j.canlet.2021.05.001. [DOI] [PubMed] [Google Scholar]
- 71.Rauf A, Imran M, Butt MS, Nadeem M, Peters DG, Mubarak MS. Resveratrol as an anti-cancer agent: A review. Crit Rev Food Sci Nutr. 2018;58:1428–1447. doi: 10.1080/10408398.2016.1263597. [DOI] [PubMed] [Google Scholar]
- 72.Yu XM, Jaskula-Sztul R, Ahmed K, Harrison AD, Kunnimalaiyaan M, Chen H. Resveratrol induces differentiation markers expression in anaplastic thyroid carcinoma via activation of notch1 signaling and suppresses cell growth. Mol Cancer Ther. 2013;12:1276–1287. doi: 10.1158/1535-7163.MCT-12-0841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liu X, Li H, Wu ML, Wu J, Sun Y, Zhang KL, Liu J. Resveratrol reverses retinoic acid resistance of anaplastic thyroid cancer cells via demethylating CRABP2 gene. Front Endocrinol (Lausanne) 2019;10:734. doi: 10.3389/fendo.2019.00734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wu J, Li YT, Tian XT, Liu YS, Wu ML, Li PN, Liu J. STAT3 signaling statuses determine the fate of resveratrol-treated anaplastic thyroid cancer cells. Cancer Biomark Sect Dis Markers. 2020;27:461–469. doi: 10.3233/CBM-191010. [DOI] [PubMed] [Google Scholar]
- 75.Zheng X, Jia B, Tian XT, Song X, Wu ML, Kong QY, Li H, Liu J. Correlation of reactive oxygen species levels with resveratrol sensitivities of anaplastic thyroid cancer cells. Oxid Med Cell Longev. 2018;2018:6235417. doi: 10.1155/2018/6235417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Xiong L, Nie JH, Lin XM, Wu JB, Chen Z, Xu B, Liu J. Biological implications of PTEN upregulation and altered sodium/iodide symporter intracellular distribution in resveratrol-suppressed anaplastic thyroid cancer cells. J Cancer. 2020;11:6883–6891. doi: 10.7150/jca.48180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Xiong L, Lin XM, Nie JH, Ye HS, Liu J. Resveratrol and its nanoparticle suppress doxorubicin/docetaxel-resistant anaplastic thyroid cancer cells in vitro and in vivo. Nanotheranostics. 2021;5:143–154. doi: 10.7150/ntno.53844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Imran M, Rauf A, Khan IA, Shahbaz M, Qaisrani TB, Fatmawati S, Abu-Izneid T, Imran A, Rahman KU, Gondal TA. Thymoquinone: A novel strategy to combat cancer: A review. Biomed Pharmacother Biomedecine Pharmacother. 2018;106:390–402. doi: 10.1016/j.biopha.2018.06.159. [DOI] [PubMed] [Google Scholar]
- 79.Zhang M, Du H, Wang L, Yue Y, Zhang P, Huang Z, Lv W, Ma J, Shao Q, Ma M, et al. Thymoquinone suppresses invasion and metastasis in bladder cancer cells by reversing EMT through the Wnt/β-catenin signaling pathway. Chem Biol Interact. 2020;320:109022. doi: 10.1016/j.cbi.2020.109022. [DOI] [PubMed] [Google Scholar]
- 80.Ozturk SA, Alp E, Saglam ASY, Konac E, Menevse ES. The effects of thymoquinone and genistein treatment on telomerase activity, apoptosis, angiogenesis, and survival in thyroid cancer cell lines. J Cancer Res Ther. 2018;14:328–334. doi: 10.4103/0973-1482.202886. [DOI] [PubMed] [Google Scholar]
- 81.Kupchan SM, Court WA, Dailey RG, Jr, Gilmore CJ, Bryan RF. Triptolide and tripdiolide, novel antileukemic diterpenoid triepoxides from Tripterygium wilfordii. J Am Chem Soc. 1972;94:7194–7195. doi: 10.1021/ja00775a078. [DOI] [PubMed] [Google Scholar]
- 82.Noel P, Von Hoff DD, Saluja AK, Velagapudi M, Borazanci E, Han H. Triptolide and its derivatives as cancer therapies. Trends Pharmacol Sci. 2019;40:327–341. doi: 10.1016/j.tips.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 83.Zhu W, Hu H, Qiu P, Yan G. Triptolide induces apoptosis in human anaplastic thyroid carcinoma cells by a p53-independent but NF-kappaB-related mechanism. Oncol Rep. 2009;22:1397–1401. doi: 10.3892/or_00000580. [DOI] [PubMed] [Google Scholar]
- 84.Zhu W, Ou Y, Li Y, Xiao R, Shu M, Zhou Y, Xie J, He S, Qiu P, Yan G. A small-molecule triptolide suppresses angiogenesis and invasion of human anaplastic thyroid carcinoma cells via down-regulation of the nuclear factor-kappa B pathway. Mol Pharmacol. 2009;75:812–819. doi: 10.1124/mol.108.052605. [DOI] [PubMed] [Google Scholar]
- 85.Zhu W, He S, Li Y, Qiu P, Shu M, Ou Y, Zhou Y, Leng T, Xie J, Zheng X, et al. Anti-angiogenic activity of triptolide in anaplastic thyroid carcinoma is mediated by targeting vascular endothelial and tumor cells. Vascul Pharmacol. 2010;52:46–54. doi: 10.1016/j.vph.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 86.Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG, Yoo HJ, Lee SJ. Synergistic cytotoxicity of BIIB021 with triptolide through suppression of PI3K/Akt/mTOR and NF-κB signal pathways in thyroid carcinoma cells. Biomed Pharmacother. 2016;83:22–32. doi: 10.1016/j.biopha.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 87.Chikara S, Nagaprashantha LD, Singhal J, Horne D, Awasthi S, Singhal SS. Oxidative stress and dietary phytochemicals: Role in cancer chemoprevention and treatment. Cancer Lett. 2018;413:122–134. doi: 10.1016/j.canlet.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 88.Ahmad SS, Waheed T, Rozeen S, Mahmood S, Kamal MA. Therapeutic study of phytochemicals against cancer and Alzheimer's disease management. Curr Drug Metab. 2019;20:1006–1013. doi: 10.2174/1389200221666200103092719. [DOI] [PubMed] [Google Scholar]
- 89.Tendulkar S, Dodamani S. Chemoresistance in ovarian cancer: Prospects for new drugs. Anticancer Agents Med Chem. 2021;21:668–678. doi: 10.2174/1871520620666200908104835. [DOI] [PubMed] [Google Scholar]
- 90.Shin HJ, Hwang KA, Choi KC. Antitumor effect of various phytochemicals on diverse types of thyroid cancers. Nutrients. 2019;11:125. doi: 10.3390/nu11010125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Manach C, Williamson G, Morand C, Scalbert A, Rémésy C. Bioavailability and bioefficacy of polyphenols in humans. I. Review of 97 bioavailability studies. Am J Clin Nutr. 2005;81((1 Suppl)):230S–242S. doi: 10.1093/ajcn/81.1.230S. [DOI] [PubMed] [Google Scholar]
- 92.Pannu N, Bhatnagar A. Resveratrol: From enhanced biosynthesis and bioavailability to multitargeting chronic diseases. Biomed Pharmacother. 2019;109:2237–2251. doi: 10.1016/j.biopha.2018.11.075. [DOI] [PubMed] [Google Scholar]
- 93.Somjen D, Grafi-Cohen M, Katzburg S, Weisinger G, Izkhakov E, Nevo N, Sharon O, Kraiem Z, Kohen F, Stern N. Anti-thyroid cancer properties of a novel isoflavone derivative, 7-(O)-carboxymethyl daidzein conjugated to N-t-Boc-hexylenediamine in vitro and in vivo. J Steroid Biochem Mol Biol. 2011;126:95–103. doi: 10.1016/j.jsbmb.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 94.Zheng X, Jia B, Song X, Kong QY, Wu ML, Qiu ZW, Li H, Liu J. Preventive potential of resveratrol in carcinogen-induced rat thyroid tumorigenesis. Nutrients. 2018;10:279. doi: 10.3390/nu10030279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jafarpour SM, Safaei M, Mohseni M, Salimian M, Aliasgharzadeh A, Farhood B. The radioprotective effects of curcumin and trehalose against genetic damage caused by I-131. Indian J Nucl Med. 2018;33:99–104. doi: 10.4103/ijnm.IJNM_158_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Stancioiu F, Mihai D, Papadakis GZ, Tsatsakis A, Spandidos DA, Badiu C. Treatment for benign thyroid nodules with a combination of natural extracts. Mol Med Rep. 2019;20:2332–2338. doi: 10.3892/mmr.2019.10453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chmielik E, Rusinek D, Oczko-Wojciechowska M, Jarzab M, Krajewska J, Czarniecka A, Jarzab B. Heterogeneity of thyroid cancer. Pathobiolgy. 2018;85:117–129. doi: 10.1159/000486422. [DOI] [PubMed] [Google Scholar]
- 98.Cabanillas ME, McFadden DG, Durante C. Thyroid cancer. Lancet. 2016;388:2783–2795. doi: 10.1016/S0140-6736(16)30172-6. [DOI] [PubMed] [Google Scholar]
- 99.Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA, editors. National Cancer Institute; Bethesda, MD: 2018. SEER Cancer Statistics Review, 1975–2018. [Google Scholar]
- 100.La Vecchia C, Malvezzi M, Bosetti C, Garavello W, Bertuccio P, Levi F, Negri E. Thyroid cancer mortality and incidence: A global overview. Int J Cancer. 2015;136:2187–2195. doi: 10.1002/ijc.29251. [DOI] [PubMed] [Google Scholar]
- 101.Molinaro E, Romei C, Biagini A, Sabini E, Agate L, Mazzeo S, Materazzi G, Sellari-Franceschini S, Ribechini A, Torregrossa L, et al. Anaplastic thyroid carcinoma: From clinicopathology to genetics and advanced therapies. Nat Rev Endocrinol. 2017;13:644–660. doi: 10.1038/nrendo.2017.76. [DOI] [PubMed] [Google Scholar]
- 102.Smallridge RC, Copland JA. Anaplastic thyroid carcinoma: Pathogenesis and emerging therapies. Clin Oncol (R Coll Radiol) 2010;22:486–497. doi: 10.1016/j.clon.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ain KB. Anaplastic thyroid carcinoma: Behavior, biology, and therapeutic approaches. Thyroid. 1998;8:715–726. doi: 10.1089/thy.1998.8.715. [DOI] [PubMed] [Google Scholar]
- 104.Glaser SM, Mandish SF, Gill BS, Balasubramani GK, Clump DA, Beriwal S. Anaplastic thyroid cancer: Prognostic factors, patterns of care, and overall survival. Head Neck. 2016;38((Suppl 1)):E2083–E2090. doi: 10.1002/hed.24384. [DOI] [PubMed] [Google Scholar]
- 105.Ferrari SM, Elia G, Ragusa F, Ruffilli I, Motta CL, Paparo SR, Patrizio A, Vita R, Benvenga S, Materazzi G, et al. Novel treatments for anaplastic thyroid carcinoma. Gland Surg. 2020;9((Suppl 1)):S28–S42. doi: 10.21037/gs.2019.10.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Xu G, Chen J, Wang G, Xiao J, Zhang N, Chen Y, Yu H, Wang G, Zhao Y. Resveratrol inhibits the tumorigenesis of follicular thyroid cancer via ST6GAL2-regulated activation of the hippo signaling pathway. Mol Ther Oncolytics. 2020;16:124–133. doi: 10.1016/j.omto.2019.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Shih A, Davis FB, Lin HY, Davis PJ. Resveratrol induces apoptosis in thyroid cancer cell lines via a MAPK- and p53-dependent mechanism. J Clin Endocrinol Metab. 2002;87:1223–1232. doi: 10.1210/jcem.87.3.8345. [DOI] [PubMed] [Google Scholar]
- 108.Ferretti E, Tosi E, Po A, Scipioni A, Morisi R, Espinola MS, Russo D, Durante C, Schlumberger M, Screpanti I, et al. Notch signaling is involved in expression of thyrocyte differentiation markers and is down-regulated in thyroid tumors. J Clin Endocrinol Metab. 2008;93:4080–4087. doi: 10.1210/jc.2008-0528. [DOI] [PubMed] [Google Scholar]
- 109.Davis RJ, Pinchot S, Jarjour S, Kunnimalaiyaan M, Chen H. Resveratrol-induced notch activation potentially mediates autophagy in human follicular thyroid cancer cells. J Surg Res. 2010;2:331–332. doi: 10.1016/j.jss.2009.11.440. [DOI] [Google Scholar]
- 110.Wang Y, Hu Z, Ma W, Niu Y, Su J, Zhang L, Zhao P. Signal transducer and activator of transcription 3 inhibition alleviates resistance to BRAF inhibition in anaplastic thyroid cancer. Invest New Drugs. 2021;39:764–774. doi: 10.1007/s10637-020-01024-y. [DOI] [PubMed] [Google Scholar]
- 111.Kartal-Yandim M, Adan-Gokbulut A, Baran Y. Molecular mechanisms of drug resistance and its reversal in cancer. Crit Rev Biotechnol. 2016;36:716–726. doi: 10.3109/07388551.2015.1015957. [DOI] [PubMed] [Google Scholar]
- 112.Pick A, Wiese M. Tyrosine kinase inhibitors influence ABCG2 expression in EGFR-positive MDCK BCRP cells via the PI3K/Akt signaling pathway. ChemMedChem. 2012;7:650–662. doi: 10.1002/cmdc.201100543. [DOI] [PubMed] [Google Scholar]
- 113.Hoffmann K, Shibo L, Xiao Z, Longerich T, Büchler MW, Schemmer P. Correlation of gene expression of ATP-binding cassette protein and tyrosine kinase signaling pathway in patients with hepatocellular carcinoma. Anticancer Res. 2011;31:3883–3890. [PubMed] [Google Scholar]
- 114.Wang Z, Li Y, Ahmad A, Azmi AS, Banerjee S, Kong D, Sarkar FH. Targeting notch signaling pathway to overcome drug resistance for cancer therapy. Biochim Biophys Acta. 2010;1806:258–267. doi: 10.1016/j.bbcan.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ma L, Cheng Q. Inhibiting 6-phosphogluconate dehydrogenase reverses doxorubicin resistance in anaplastic thyroid cancer via inhibiting NADPH-dependent metabolic reprogramming. Biochem Biophys Res Commun. 2018;498:912–917. doi: 10.1016/j.bbrc.2018.03.079. [DOI] [PubMed] [Google Scholar]
- 116.Li Y. Inactivation of PDH can reduce anaplastic thyroid cancer cells' sensitivity to artemisinin. Anticancer Agents Med Chem. 2021;22:1753–1760. doi: 10.2174/1871520621666210910100803. [DOI] [PubMed] [Google Scholar]
- 117.Warburg O. On the origin of cancer cells. Science. 1956;123:309–314. doi: 10.1126/science.123.3191.309. [DOI] [PubMed] [Google Scholar]
- 118.Enriquez-Navas PM, Wojtkowiak JW, Gatenby RA. Application of evolutionary principles to cancer therapy. Cancer Res. 2015;75:4675–4680. doi: 10.1158/0008-5472.CAN-15-1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Siddiqui FA, Prakasam G, Chattopadhyay S, Rehman AU, Padder RA, Ansari MA, Irshad R, Mangalhara K, Bamezai RNK, Husain M, et al. Curcumin decreases Warburg effect in cancer cells by down-regulating pyruvate kinase M2 via mTOR-HIF1α inhibition. Sci Rep. 2018;8:8323. doi: 10.1038/s41598-018-25524-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gibellini L, Bianchini E, De Biasi S, Nasi M, Cossarizza A, Pinti M. Natural compounds modulating mitochondrial functions. Evid Based Complement Altern Med. 2015;2015:527209. doi: 10.1155/2015/527209. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.