Abstract
Recent policy changes have required health care delivery organizations provide patients electronic access to their clinical notes free of charge. There is concern that this could have an unintended consequence of increased electronic health record (EHR) work as clinicians may feel the need to adapt their documentation practices in light of their notes being accessible to patients, potentially exacerbating EHR-induced clinician burnout. Using a national, longitudinal data set consisting of all ambulatory care physicians and advance practice providers using an Epic Systems EHR, we used an interrupted time-series analysis to evaluate the immediate impact of the policy change on clinician note length and time spent documenting in the EHR. We found no evidence of a change in note length or time spent writing notes following the implementation of the policy, suggesting patient access to clinical notes did not increase documentation workload for clinicians.
Keywords: electronic health records, documentation burden, clinician well-being, patient portals
INTRODUCTION
The Office of the National Coordinator for Health Information Technology (ONC) implemented part of the 21st Century Cures Act final rule on April 5, 2021 mandating care delivery organizations provide patients with no-cost access to their electronic health information, including clinical notes.1 While this represents an important step forward for patient access to data, there are concerns that allowing patient access to clinical notes could change documentation patterns, requiring clinicians to spend more time and effort documenting to ensure clinical notes are intelligible to patients and potentially engaging in “shadow charting,” the practice of maintaining separate notes inaccessible to patients when legal to do so.2,3 This could potentially result in an increase in electronic health record (EHR) workload for clinicians as they adapt to a new socio-technical environment and exacerbate EHR-driven burnout.4
Given growing concerns over clinician burnout,4–6 and an increased policy focus on reducing documentation burden,7 there is a clear demand from policymakers to understand how aspects of policy drives EHR work.8 Evaluating the impact of changes to the regulations that govern how patients and clinicians interact with the EHR with a focus on determining whether there are unintended consequences resulting in increased clinician documentation burden is critical to building an understanding of how policy creates EHR work. It is especially important to rapidly evaluate the immediate impact of policy changes that have the potential to significantly disrupt existing clinician workflows, such as the potential impact of allowing patients access to clinical notes on clinician EHR documentation.
However, to-date, there have been no large-scale studies of the impact of mandating patient access to their electronic health data, including clinical notes, on documentation length and time spent writing notes in the EHR. To address this, we evaluated the immediate impact of the policy using national EHR metadata for ambulatory care clinicians, to assess changes in progress note length and time spent documenting in the EHR following the implementation of the rule.
MATERIALS AND METHODS
Data
Our sample included all physicians and advance practice providers using Epic as their ambulatory EHR in the United States. Our data were deidentified clinician-week level EHR audit log metadata extracted by Epic’s Signal software. The software tracks all user activity in the EHR and aggregates the data into clinician-level means for each week, from January 3, 2021 to May 29, 2021. Details of Epic’s Signal data collection can be found in prior published work.9,10
Our sample included 341 234 unique clinicians through 21 weeks for 5 518 574 clinician-week observations. This represents Epic’s entire US clinician user-base during this period. All measures are specific to ambulatory care EHR use only; any work on inpatient data is excluded from the analytic data set. All data were deidentified prior to receipt of the data, and the University of Pennsylvania Institutional Review Board deemed this study exempt as nonhuman subjects research.
Measures
Our primary independent variable of interest was the implementation of mandatory patient access to their electronic health information, including clinical notes. We used the week beginning April 4, 2021 as our posttreatment period, as the policy took effect April 5, 2021.
Our dependent variables of interest were EHR use variables related to clinician documentation. These were mean progress note length, measured as number of characters per note, and mean time spent documenting in the Notes section of the EHR, per visit and per progress notes written (as not all visits generate progress notes), measured in minutes.
Statistical analyses
We calculated means before (January 3, 2021 to April 3, 2021) and after (April 4, 2021 to May 29, 2021) the policy was implemented. We then used interrupted time-series regression analyses to identify the immediate impact of the policy as well as compare trends before and after for our outcomes.11 We also plotted weekly estimates to observe any potential anticipation effect of health systems enabling patient access to notes prior to the deadline. Models included controls for number of visits per week, clinician-level fixed effects to control for potential unobserved time invariant omitted variable bias, and robust standard errors clustered at the clinician level. We also conducted robustness tests with a subsample of our data evaluating only primary care clinicians, as evidence shows they face the highest burden of EHR documentation time,12,13 as well as comparing physicians and advance practice providers.
RESULTS
Prior to April 4, 2021, mean progress note length was 5520 characters and documentation time was 10.5 min per appointment and 12.6 min per progress note. From April 4, 2021 through May 29, 2021, mean note length was 5522 characters and documentation time was 10.2 min per visit and 12.2 min per note (Table 1).
Table 1.
Clinician note length and documentation time per appointment
| January 3, 2021 to April 3, 2021 | April 4, 2021 to May 29, 2021 | Adjusted difference | Change in slope | |
|---|---|---|---|---|
| Mean | Mean | β [95% CI] | β [95% CI] | |
| Progress note length (number of characters) | 5520 | 5522 | 27.3*** [13.5; 41.1] | −3.38*** [−4.27; −2.49] |
| Time in notes per visit (min) | 10.5 | 10.2 | 0.29*** [0.14; 0.43] | −0.03*** [−0.04; −0.02] |
| Time in notes per progress notes written (min) | 12.6 | 12.2 | 0.13 [−0.05; 0.31] | −0.02*** [−0.03; −0.01] |
Note: P < .05; **P < .01; ***P < .001.
Adjusted difference represents the immediate change in the week of policy implementation, change in slope represents difference between slope of fitted linear model on either side of policy implementation, both from interrupted time-series analyses with controls for weekly volume, clinician-level fixed effects, and robust standard errors clustered at the clinician level.
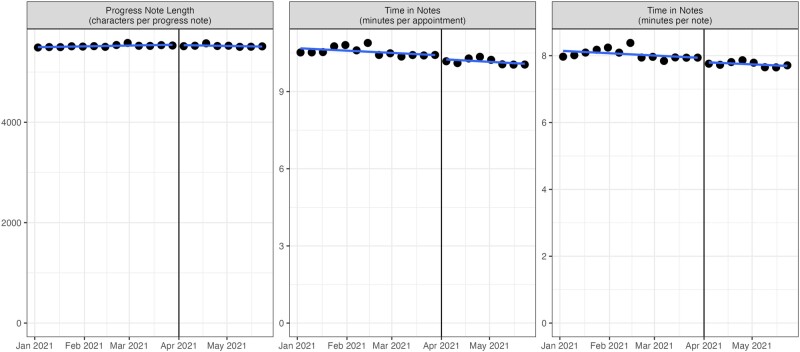
In our interrupted time-series analyses, immediately following the change note length increased by 27.3 characters (95% CI, 13.5–41.1) and time in notes per visit increased by 0.29 min (95% CI, 0.14–0.43), while time in notes per note was unchanged (β = 0.13; 95% CI, −0.05 to 0.31). In the weeks following the policy implementation, note length (β = −3.38; 95% CI, −4.27 to −2.49), documentation time per visit (β = −0.03; 95% CI, −0.04 to −0.02) and per note (β = −0.02; 95% CI, −0.03 to −0.01) saw statistically significant downward trends relative to the preperiod (Figure 1). We found similar results in our robustness tests focusing on primary care physicians and separately on advance practice providers (Supplementary Appendix Exhibit S1).
Figure 1.
Mean note length and documentation time before and after patient electronic health information access rules. Vertical line represents week beginning April 4, 2021. ONC Information Blocking rules pertaining to patient access to electronic health information were implemented April 5, 2021. Blue lines represent linear best fit on each side of policy implementation. Gray areas represent 95% confidence intervals. Dots represent sample mean in each week.
DISCUSSION
We found that recently implemented ONC rules mandating patient access to clinical notes did not meaningfully increase documentation length or time spent documenting in the EHR. Rather, our results show decreases in the slope of both note length and documentation time, though the effect sizes are miniscule. Our results are consistent with studies on clinicians that opted into patient access to notes through the OpenNotes initiative, which found most clinicians had a positive impression of patient note access.14
Our results show no short-term increase in EHR documentation work due to the implementation of rules stipulating no-cost patient access to electronic health information. Future research should evaluate the longer-term impact of policy on EHR burden to better understand how policy impacts clinician work, productivity, and well-being. While EHR time and note length did not increase, the quality of notes for clinical purposes may have decreased, or clinicians had to otherwise alter their documentation practices in light of the new policy. Finally, it is important to note that the policy change required significant effort on the part of care delivery organizations and other health care stakeholders to prepare for and facilitate patient access to notes, including any technical work to enable patient access, educating clinicians, understanding the allowed exceptions, and creating workflows to implement them, and more. Our findings showing no increase in EHR documentation length or time reflects the significant efforts invested in the leadup to the policy implementation.
Limitations
Our study should be interpreted with some limitations in mind. First, our results are an average treatment effect of the policy implementation—some individual clinicians or groups may have experienced increased documentation burden even if the policy did not have an impact on the average clinician. Second, our study evaluates the policy change mandating patient access to electronic notes, rather than the impact of patients actually viewing the notes, which we are unable to observe in our data. Additionally, some organizations may have implemented patient access prior to the policy deadline of April 5. However, in plotting our dependent variables over time, we do not see an uptick in documentation burden in the months leading up to the policy change, which suggests even if this were the case we do not observe an increase in documentation burden. Third, the policy change was implemented during the COVID-19 pandemic, which could potentially bias our results. However, our findings on time spent in notes are similar to prepandemic data,12,15 and previous research has found that the disruptive impact of COVID on clinician EHR use had reached a steady state by August 2020.16 Additionally, other EHR metadata research has shown trends in EHR documentation and use have been stable in the period leading up to the implementation of patient note access.7 To assess evidence of COVID-induced bias, we conducted several “control” analyses using our interrupted time-series framework on outcomes we would expect to show large changes if a COVID surge were disrupting normal operations. These included total weekly visits, number of weekly visits with new patients and weekly visits with existing patients for E/M encounters, and average patient age. In all of our models we found no clinically significant changes in the aftermath of the April 5th policy implementation date (Supplementary Appendix Table S2). However, we cannot completely rule out bias from other contemporaneous phenomena that could impact documentation practices. Fourth, due to data limitations, we were only able to evaluate the immediate impact of the policy change. While our data are able to address our main research question as to whether the implementation of the policy increased EHR documentation time and length, future studies should evaluate long-term impacts on other aspects of documentation as clinician behavior can change slowly. Additionally, our study used data from a single electronic health record vendor, Epic Systems. However, Epic is the largest ambulatory care EHR vendor in the United States,17 serving care delivery organizations ranging from academic medical centers to safety-net providers,18 and to our knowledge our sample constitutes one of the largest studies of clinician EHR work to-date. Finally, patient access to notes may generate other forms of EHR work outside of documentation, such as increased messages received from patients that our data do not capture.19
CONCLUSION
We found no increase in EHR documentation work measured by length of progress note or documentation time in our evaluation of the possibility of increased clinician documentation in the immediate aftermath of the recent policy change mandating patient no-cost access to their electronic health information using a national, longitudinal evaluation of clinician EHR metadata from all outpatient physicians and advance practice providers using Epic in the United States. Changes to policy and regulation of electronic health information may create unintended consequences, such as increasing documentation burden for clinicians. Policymakers and health system leaders interested in addressing EHR burden should continue to investigate other drivers of documentation work to address the impacts of EHRs on clinician well-being.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
AUTHOR CONTRIBUTIONS
AJH conceived the study and wrote the first draft of the manuscript. NCA acquired the data and performed the analysis. Both authors contributed equally to the design of the analysis and critical revisions of the manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
CONFLICT OF INTEREST STATEMENT
None declared.
Supplementary Material
Contributor Information
A Jay Holmgren, Center for Clinical Informatics and Improvement Research, University of California San Francisco, San Francisco, California, USA.
Nate C Apathy, Perelman School of Medicine, Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
Data Availability
All data used in the study are available upon request from the data provider, Epic Systems.
REFERENCES
- 1. About ONC’s Cures Act Final Rule. Office of the National Coordinator for Health Information Technology. 2020. https://www.healthit.gov/curesrule/overview/about-oncs-cures-act-final-rule Accessed August 1, 2021.
- 2. American Medical Association. How Doctors Can Adjust to New Reality—Opening Notes to Patients. 2021. https://www.ama-assn.org/practice-management/digital/how-doctors-can-adjust-new-reality-opening-notes-patients Accessed October 11, 2021.
- 3. Arvisais-Anhalt S, Lau M, Lehmann CU, et al. The 21st century cures act and multiuser electronic health record access: potential pitfalls of information release. J Med Internet Res 2022; 24 (2): e34085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Adler-Milstein J, Zhao W, Willard-Grace R, et al. Electronic health records and burnout: time spent on the electronic health record after hours and message volume associated with exhaustion but not with cynicism among primary care clinicians. J Am Med Inform Assoc 2020; 27 (4): 531–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc 2019; 26 (2): 106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hilliard RW, Haskell J, Gardner RL.. Are specific elements of electronic health record use associated with clinician burnout more than others? J Am Med Inform Assoc 2020; 27 (9): 1401–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Apathy NC, Hare AJ, Fendrich S, et al. Early changes in billing and notes after evaluation and management guideline change. Ann Intern Med 2022; 175 (4): 499–504. [DOI] [PubMed] [Google Scholar]
- 8. Holmgren AJ, Rotenstein L, Downing NL, et al. Association between state-level malpractice environment and clinician electronic health record (EHR) time. J Am Med Inform Assoc 2022; 29 (6): 1069–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Baxter SL, Apathy NC, Cross DA, et al. Measures of electronic health record use in outpatient settings across vendors. J Am Med Inform Assoc 2021; 28 (5): 955–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Holmgren AJ, Downing NL, Bates DW, et al. Assessment of electronic health record use between US and non-US health systems. JAMA Intern Med 2021; 181 (2): 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J 2015; 15 (2): 480–500. [Google Scholar]
- 12. Rotenstein LS, Holmgren AJ, Downing NL, et al. Differences in total and after-hours electronic health record time across ambulatory specialties. JAMA Intern Med 2021; 181 (6): 863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rotenstein LS, Holmgren AJ, Downing NL, et al. Differences in clinician electronic health record use across adult and pediatric primary care specialties. JAMA Netw Open 2021; 4 (7): e2116375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. DesRoches CM, Leveille S, Bell SK, et al. The views and experiences of clinicians sharing medical record notes with patients. JAMA Netw Open 2020; 3 (3): e201753. [DOI] [PubMed] [Google Scholar]
- 15. Overhage JM, McCallie D.. Physician time spent using the electronic health record during outpatient encounters: a descriptive study. Ann Intern Med 2020; 172 (3): 169. [DOI] [PubMed] [Google Scholar]
- 16. Holmgren AJ, Downing NL, Tang M, et al. Assessing the impact of the COVID-19 pandemic on clinician ambulatory electronic health record use. J Am Med Inform Assoc 2022; 29 (3): 453–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Top 10 Ambulatory EHR Vendors by 2019 Market Share. Definitive Healthcare. 2019. https://blog.definitivehc.com/top-ambulatory-ehr-systems Accessed June 27, 2020.
- 18. OCHIN Epic EHR. OCHIN. https://ochin.org/hosted-epic-ehr Accessed September 21, 2021.
- 19. Steitz BD, Sulieman L, Wright A, et al. Association of immediate release of test results to patients with implications for clinical workflow. JAMA Netw Open 2021; 4 (10): e2129553. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data used in the study are available upon request from the data provider, Epic Systems.