Abstract
This study assesses governments' long-term non-pharmaceutical interventions upon the coronavirus disease 2019 (COVID-19) pandemic in East Asia. It advances the literature towards a better understanding of when and which control measures are effective. We (1) provide time-varying case fatality ratios and focus on the elderly's mortality and case fatality ratios, (2) measure the correlations between daily new cases (daily new deaths) and each index based on multiple domestic pandemic waves and (3) examine the lead–lag relationship between daily new cases (daily new deaths) and each index via the cross-correlation functions on the pre-whitened series. Our results show that the interventions reduce COVID-19 infections for some periods before the period of the Omicron variant. Moreover, there is no COVID-19 policy lag in Taiwan between daily new confirmed cases and each index. As of March 2022, the case fatality ratios of the elderly group in Japan, Hong Kong and South Korea are 4.69%, 4.72% and 1.48%, respectively, while the case fatality ratio of the elderly group in Taiwan is 25.01%. A government's COVID-19 vaccination distribution and prioritisation policies are pivotal for the elderly group to reduce the number of deaths. Immunising this specific group as best as possible should undoubtedly be a top priority.
Key words: Case fatality ratio, COVID-19, non-pharmaceutical interventions, elderly group, Spearman's rank correlation
Introduction
Ever since the onset of the coronavirus disease 2019 (COVID-19) pandemic, many governments have implemented massive containment and other policies to preserve lives and enhance safety as well as introduced travel restrictions [1, 2] and numerous non-pharmaceutical interventions [3, 4] to bring down virus-related infections and deaths. Such interventions have also covered school closings, travel restrictions, bans on public gatherings and stay-at-home orders [5]. Many contemporary studies have thus examined government effectiveness targeting the COVID-19 pandemic at specific time points [6–8].
With COVID-19 already prevailing for almost 3 years, it is critical to assess government policies and their impact and effectiveness during this time. The present study assesses governments' long-term non-pharmaceutical interventions upon the COVID-19 pandemic in East Asia based on defined multiple pandemic waves. The study moves the literature towards a better understanding of when and which control measures are effective. We employ the Oxford COVID-19 Government Response Tracker (OxCGRT) datasets and narrow them down to East Asia for several reasons. First, the development of the COVID-19 pandemic in this region is very different from what has happened in Western countries. Second, this study offers a greater in-depth look and uncovers insightful information. Lastly, we investigate the proportion of new confirmed cases (new cases for short), new deaths and case fatality ratios of the elderly group.
Data description
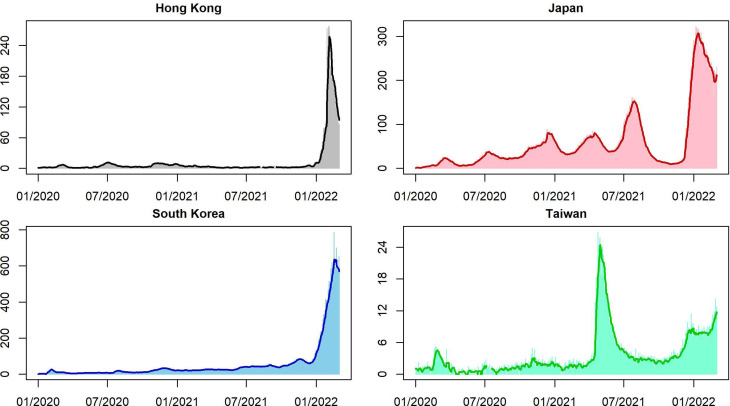
We collect the daily numbers of confirmed cases, numbers of deaths, containment and health index, stringency index, and government response index from Oxford COVID-19 Government Response Tracker [5] and further calculate daily confirmed cases and daily deaths by the 7-day moving average (MA) to allocate uncertain cases on the correct dates of the pandemic onset for some countries and region (Fig. 1). OxCGRT tracks individual policy measures across 20 indicators, producing four indices that aggregate daily information into a single number from 0 to 100. It measures how many relevant indicators a government has acted upon and to what degree. An index is an ordinal variable that is unable to provide whether a government's policy has been implemented effectively. This study scrutinises these indices associated with other information and uncovers insightful information. We describe the three indices as follows.
Containment and health index (CHI): the index integrates information on lockdown restrictions and related healthcare investments due to the pandemic. It relies on all ordinal containment/closure and health system policy indicators.
Stringency index (SI): the index measures the strictness of various lockdown policies that aim to reduce social activities and human contact. It covers all ordinal containment/closure policy indicators and an indicator on public information campaigns.
Government response index (GRI): the index records how government responses result in varying overall indicators in the OxCGRT database that become stronger or weaker throughout the outbreak. This index comes from all ordinal indicators. GRI provides a dynamic benchmarking measure for the speed of government responses globally to COVID-19.
Fig. 1.
Square root of daily new confirmed cases (on the vertical line) and the square root of daily new confirmed cases smoothed by 7-day MA.
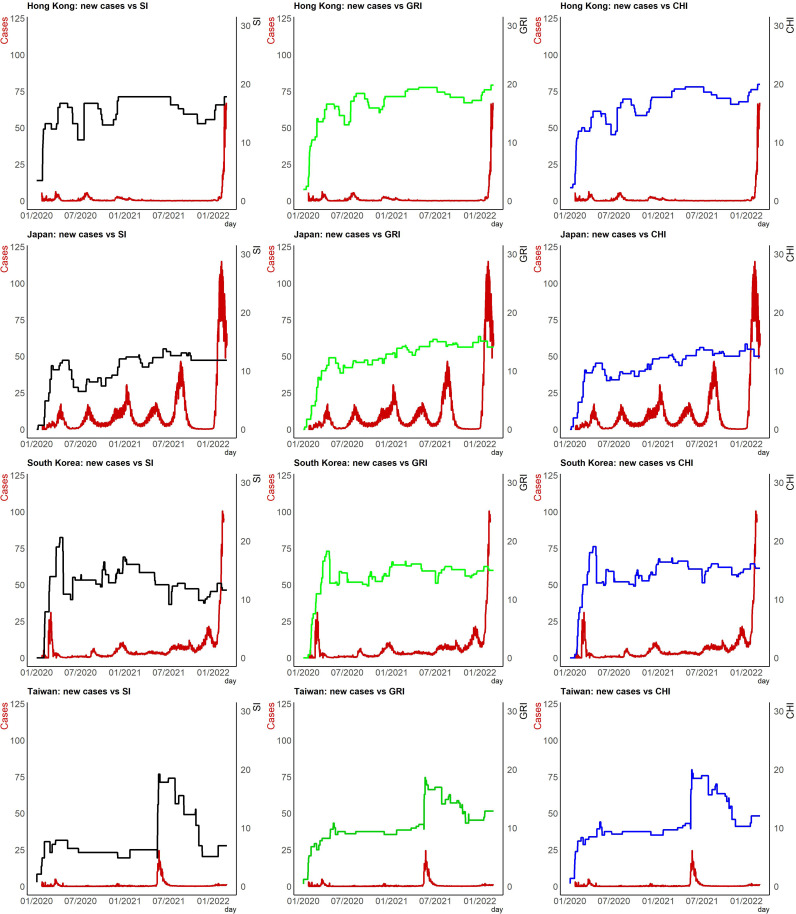
Figure 2 illustrates the time plots of daily confirmed cases as of March 2022 associated with Japan, Hong Kong, South Korea and Taiwan indices. We rescale confirmed cases in the figure since the magnitudes are pretty large, as we cannot show their trend with the index in the same frame without doing so. The latest severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) Omicron variant has spread worldwide since being first detected in South Africa on 9 November 2021. We clearly see that governments in East Asia have maintained or reintroduced strict measures designed in response to this variant's surge in 2022 to limit COVID-19's spread domestically. Population disparities among different countries and region are of course enormous. To conduct international comparisons, we collect total confirmed cases (deaths) of COVID-19 per million people and the proportion of the elderly group from ‘Our World in Data’ [9].
Fig. 2.
Time plots for rescaled daily confirmed cases associated with the indices.
Methodology
We examine the pairwise association between daily new cases (daily new deaths) and the indices. An appropriate measure is Kendall's coefficient of rank correlation or Spearman's rank correlation coefficient to evaluate the strength of linkage between two variables [10] when one variable is continuous and the other is ordinal. We use Spearman's rank correlation coefficient to see the strength of association between daily new cases (daily new deaths) and each index, because the index is a discrete variable having an order associated with its large number of levels. This helps us evaluate the effectiveness of governments' policies through the three indices.
We divide the whole sample period into several waves based on multiple domestic COVID-19 pandemic surges. As of 31 March 2022, Hong Kong has experienced five waves (see the appendix in [11] for the first four waves), while South Korea has dealt with four waves (see [12] for the periods of the first three waves). Japan has encountered its sixth wave ([13, 14] define the periods from the first wave to the fifth wave of the COVID-19 pandemic), while Taiwan has faced four waves based on the period of level 3.
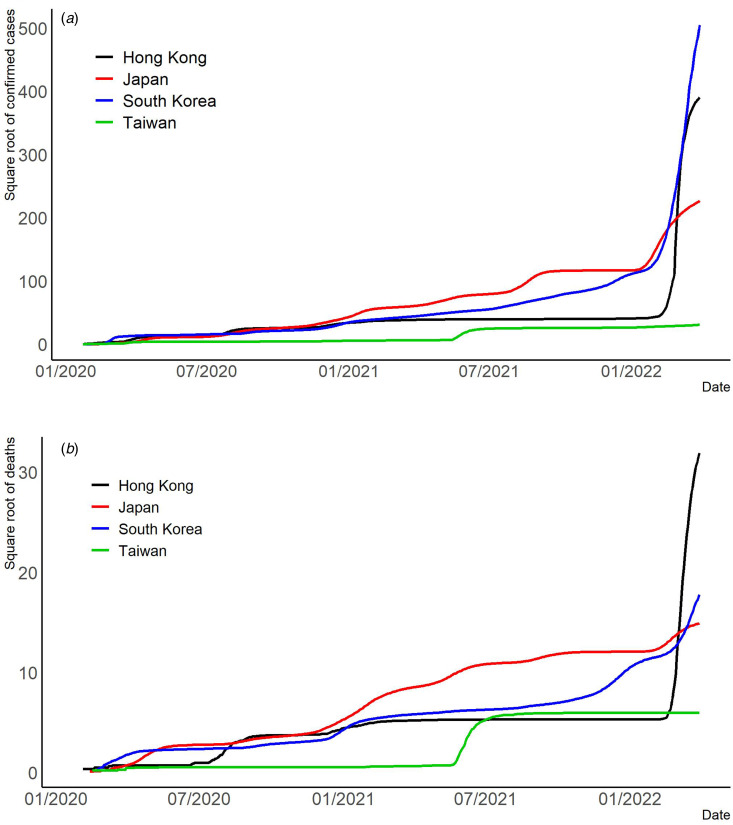
We employ visualisation to help understand different aspects of the pandemic in East Asia. We also provide (1) time-varying rescaled (but the same scale for each country or region) daily new cases vs. each index (Fig. 2); (2) time-varying total confirmed cases of COVID-19 per million people (Fig. 3a); (3) time-varying total confirmed deaths of COVID-19 per million people (Fig. 3b) and (4) time-varying dynamic case fatality ratios (Fig. 4). We rescale confirmed cases in Figures 1–3 since their magnitudes are quite large.
Fig. 3.
(a) Square root of the total confirmed cases of COVID-19 per million people. (b) Square root of the total deaths of COVID-19 per million people.
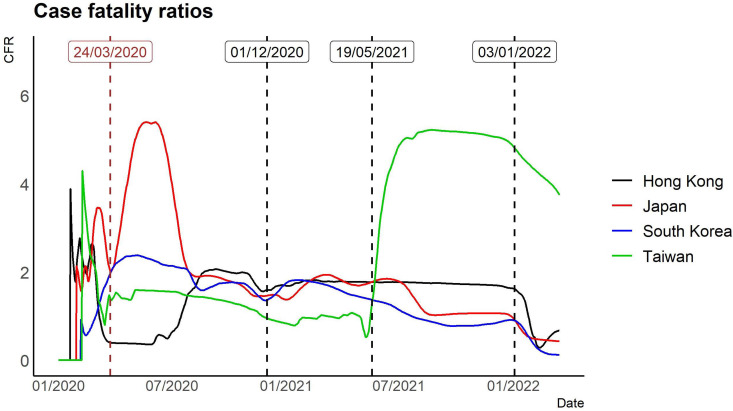
Fig. 4.
COVID-19 time-varying case fatality ratios based on the 7-day MA of confirmed cases and deaths.
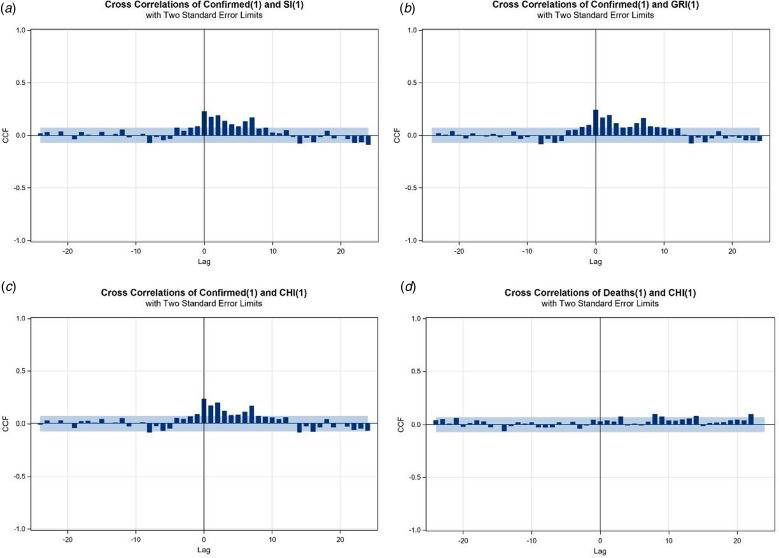
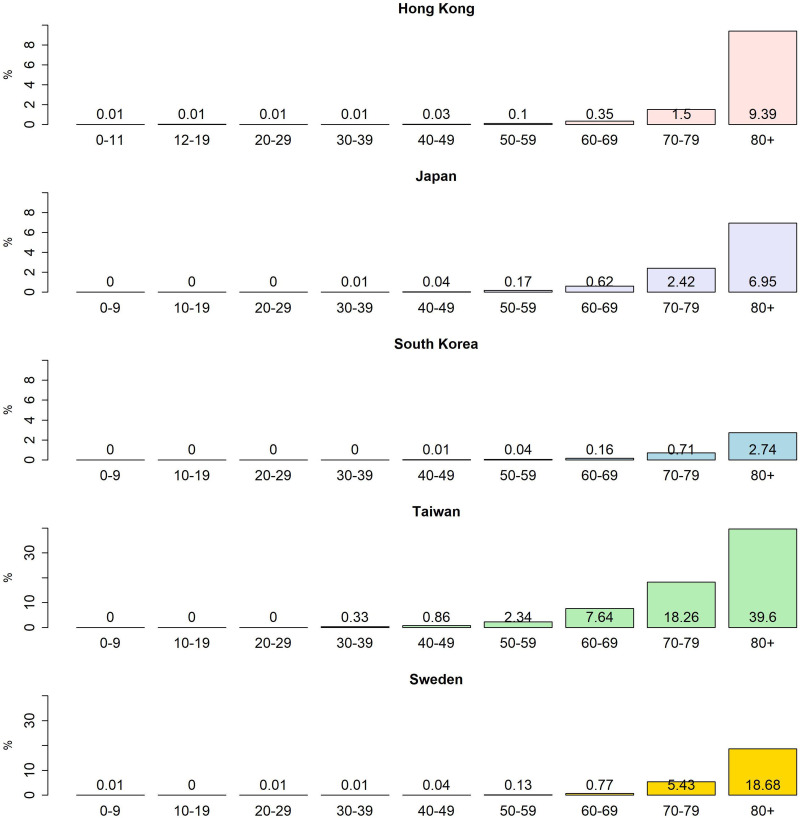
To explore the relationship between the series of SI, CHI or GRI and confirmed cases (deaths) of COVID-19, we apply the cross-correlation function (CCF) as an aid to identify the pattern of correlations. First, we conduct the first-differenced series of a considered policy index, named index changes, as a pre-whitening process. We then filter the 7-day MA of confirmed cases based on the model of the index changes. Following this strategy, the patterns of CCF between the daily new confirmed (daily new death) cases and index changes are easily identifiable (Fig. 5). The study calculates the age group-specific case fatality ratios by dividing the deaths from COVID-19 over a defined period by the number of confirmed cases during that time, especially focusing on the elderly group (Fig. 6).
Fig. 5.
CCF plots based on pre-whitened series. (a)–(c) 7-day MA of confirmed cases vs. SI, GRI and CHI changes for Taiwan, respectively. (d) 7-day MA of deaths vs. CHI changes for Taiwan. The grey areas are the bands of two standard errors.
Fig. 6.
Case fatality ratios by age group in Japan, Hong Kong, South Korea, Taiwan and Sweden as of March 2022.
Results and discussion
To observe the co-movement of policy indices and rescaled daily confirmed cases, we provide the time series plots of these two variables together. We observe that the statuses of policy indices are associated with daily new cases in countries and region. We provide illustrative descriptions that appear in Figure 2.
Hong Kong: To stop the transmission of COVID-19 from overseas to Hong Kong, a mandatory quarantine was imposed for travellers from mainland China and South Korea in February 2020 and for travellers from Iran, Italy and other regions in March 2020 [15]. There were also restrictions on public gatherings implemented in April 2020. Therefore, it is not surprising that SI, GRI and CHI increased rapidly in the first 3 months of 2020. Since then, various hygiene measures for controlling the transmission of the disease have been introduced, and there was a slight upward trend in GRI and CHI after mid-2020. Early 2022 presented a sharp increase in confirmed cases, because of the transmission of the Omicron variant in Hong Kong. A few months before the spreading of Omicron, the three indices had increased slowly, probably indicating that there was a tightening of hygiene control measures in late-2021 after recording a few imported Omicron cases.
Japan: The number of confirmed cases surged, exceeding 200 across Japan as of 27 February 2020, excluding the over 700 confirmed cases from the Diamond Princess cruise ship. The Japan government adopted various measures to limit or prevent the outbreak in the first half of 2020, which included inaugurating a Joint Research Coronavirus Task Force to supervise its response to the pandemic and the suspension of all Japanese schooling from elementary to high schools from 27 February until early April 2020 [16]. On 7 April 2020, the Japan government proclaimed a 1-month state of emergency for Tokyo and several prefectures. The state of emergency was lifted for an increasing number of prefectures during May 2020, extending to the whole country by 25 May 2020 [17]. That is why we observe growth and a drop-down in Japan for SI, GRI and CHI in the first 6 months.
South Korea: After 18 February 2020, when the virus was initially confirmed in Daegu, the number of patients with COVID-19 increased rapidly. To respond to the rapid rise in the number of COVID-19 cases, the South Korea government puts the COVID-19 alert level at the highest (level 4) on 23 February 2020, enhanced social distancing measures and infection control measures in hospitals, imposed travel restrictions, cancelled social events and delayed the school start time [18]. We observe that SI, GRI and CHI shot up rapidly in the first 3 months of 2020. In February 2022, new confirmed cases surged to six-digit figures in South Korea.
Taiwan: COVID-19 infections cropped up only sporadically before May 2021. However, daily new confirmed case numbers soared into the triple digits on 15 May 2021. The Central Epidemic Command Center (CECC) raised level 3 COVID-19 alert for Taipei City and New Taipei City, strengthened national restrictions and measures, effective from 15 May, and further raised the epidemic warning to level 3 nationwide from 19 May 2021. Heightened measures and regulations were introduced across Taiwan to reduce community transmission [19, 20]. The government has implemented a mandatory wearing-mask policy, stringent restrictions on all kinds of gatherings, closure of entertainment venues and limiting restaurants to take-out service. CECC partially lifted certain restrictions for level 3 (starting on 13 July 2021 and ending on 26 July 2021). All these related policies reveal the rising and then plummeting SI, GRI and CHI during this period.
The Omicron variant was the predominant variant in Hong Kong, Japan and South Korea from late January 2022. We observe steep increase curves for daily new confirmed cases, while the Omicron outbreak in Taiwan is still in its early stages. The daily count of new cases surged as high as a few multiples of 10 000 outside this study's period (January 2020 to March 2022).
As the 7-day MA removes the fluctuation and derives a more stable trend, we provide Spearman's rank correlation coefficient to measure the association between the 7-day MA of new cases (new deaths) and each index (Tables 1–4). The results indicate the effectiveness of government policies through the specified range when the negative correlation is significant. Findings show significantly negative association measurements during different waves for Hong Kong, Japan, South Korea and Taiwan, but most effects are on confirmed cases with only a few situations on deaths. The exceptions appear on the fourth wave (1 July 2021 to 26 March 2022) in South Korea. Both confirmed and death cases in South Korea have significantly negative associations with the three indices (SI, GRI and CHI) during this period.
Table 1.
Spearman's correlations between 7-day MA of new cases (new deaths) and policy indices for Hong Kong
| Index | COVID-19 new | Whole period 28 January 2020–26 March 2022 |
First wave 28 January 2020–3 March 2020 |
Second wave 4 March 2020–21 June 2020 |
Third wave 22 June 2020–19 November 2020 |
Fourth wave 20 November 2020–6 April 2021 |
Fifth wave 31 December 2021–26 March 2022 |
|---|---|---|---|---|---|---|---|
| SI | Case | −0.2278*** | 0.1363 | −0.4827*** | −0.3007*** | −0.4446*** | −0.3166** |
| Death | 0.0445 | −0.1934 | −0.0755 | 0.0277 | −0.0738 | 0.2272* | |
| GRI | Case | −0.1415*** | 0.0315 | −0.5147*** | −0.4264*** | −0.1504 | −0.2600* |
| Death | 0.0760* | −0.1394 | −0.0748 | −0.0162 | −0.0406 | 0.2327* | |
| CHI | Case | −0.1115** | 0.1069 | −0.5147*** | −0.4280*** | −0.1504 | −0.2600* |
| Death | 0.0764* | −0.0811 | −0.0748 | −0.0293 | −0.0406 | 0.2327* |
*, **, and *** denote significance at the 5%, 1%, and 0.1% levels, respectively.
Table 2.
Spearman's correlations between 7-day MA of new cases (new deaths) and policy indices for Japan
| Index | COVID-19 new | Whole period 28 January 2020–26 March 2022 |
First wave 1 March 2020–30 June 2020 |
Second wave 1 July 2020–31 October 2020 |
Third wave 1 November 2020–28 February 2021 |
Fourth wave 1 March 2021–24 June 2021 |
Fifth wave 25 June 2021–30 September 2021 |
Sixth wave 6 January 2022–26 March 2022 |
|---|---|---|---|---|---|---|---|---|
| SI | Case | −0.1314*** | −0.3489*** | −0.1700 | −0.4970*** | −0.4951*** | −0.4807*** | NA |
| Death | −0.0210 | 0.2364** | −0.0079 | −0.0696 | −0.1294 | −0.1689 | NA | |
| GRI | Case | 0.0165 | −0.4952*** | −0.1700 | −0.4558*** | −0.4901*** | 0.2529* | 0.6442*** |
| Death | −0.0304 | 0.0193 | −0.0079 | −0.1776 | −0.1253 | −0.4810*** | 0.2834* | |
| CHI | Case | 0.0206 | −0.4040*** | −0.1700 | −0.4641*** | −0.4901*** | 0.2529* | 0.6442*** |
| Death | −0.0070 | 0.1892* | −0.0079 | −0.1294 | −0.1253 | −0.4810*** | 0.2834* |
*, **, and *** denote significance at the 5%, 1%, and 0.1% levels, respectively.
Table 3.
Spearman's correlations between 7-day MA of new cases (new deaths) and policy indices for South Korea
| Index | COVID-19 new | Whole period 28 January 2020–26 March 2022 |
First wave 1 February 2020–31 March 2020 |
Second wave 13 August 2020–18 September 2020 |
Third wave 4 November 2020–31 January 2021 |
Fourth wave 1 July 2021–26 March 2022 |
|---|---|---|---|---|---|---|
| SI | Case | −0.2290*** | −0.0173 | 0.7060*** | −0.4876*** | −0.1461* |
| Death | −0.1734*** | 0.1114 | −0.0434 | −0.0949 | −0.3055*** | |
| GRI | Case | −0.0732* | −0.0717 | 0.7060*** | −0.5573*** | −0.1364* |
| Death | −0.1018** | 0.0883 | −0.0434 | −0.1953 | −0.2909*** | |
| CHI | Case | −0.0836* | −0.0843 | 0.7060*** | −0.5573*** | −0.1364* |
| Death | −0.1060** | 0.0827 | −0.0434 | −0.1953 | −0.2909*** |
*, **, and *** denote significance at the 5%, 1%, and 0.1% levels, respectively.
Table 4.
Spearman's correlations between 7-day MA of new cases (new deaths) and policy indices for Taiwan
| Index | COVID-19 new | Whole period 28 January 2020–22 March 2022 | First wave 28 January 2020–22 April 2021 | Second wave 23 April 2021–26 July 2021 | Third wave 27 July 2021–2 January 2022 | Fourth wave 3 January 2022–22 March 2022 |
|---|---|---|---|---|---|---|
| SI | Case | −0.1989*** | −0.0618 | −0.1162 | −0.2540** | −0.2131 |
| Death | −0.0328 | 0.0000 | −0.0517 | −0.1111 | 0.0000 | |
| GRI | Case | −0.0755* | 0.0281 | −0.0355 | −0.1607* | −0.2392* |
| Death | −0.0285 | 0.0259 | 0.1413 | −0.1118 | −0.0248 | |
| CHI | Case | −0.0814* | 0.0264 | −0.1163 | −0.1828* | −0.2392* |
| Death | −0.0342 | 0.0259 | −0.0524 | −0.1118 | −0.0248 |
*, **, and *** denote significance at the 5%, 1%, and 0.1% levels, respectively.
Governments did enforce stringent measures in the second and third quarters of 2020 after the COVID-19 virus broke out and quickly responded to the outbreak, encompassing restrictions on business activities, suspension of schooling, travel restrictions and social distancing rules (Fig. 3a). Interventions, such as enforced isolation, in Hong Kong did work truly well in the early pandemic to contain the virus over the second and third waves in terms of reducing confirmed cases (Table 1), as we find significantly negative associations between the three indices (SI, GRI and CHI) and daily confirmed cases. Since early 2022, Hong Kong has been experiencing huge and fatal virus surges via the highest total confirmed deaths of COVID-19 per million people in our study ([21] and Fig. 3b).
The number of confirmed cases increased substantially across Japan in late-February 2020. The Japan government adopted various hygiene measures to limit or prevent the outbreak in the first half of 2020. These could explain why we observe a significantly negative association between new confirmed cases and policy in the first wave in Table 2 for this country.
We observe evidence of the impact of non-pharmaceutical measures in controlling the spread of the virus in Japan during the whole study period except during the second and sixth waves (Table 2). The ‘Go To Travel’ campaign originally ran in the second half of 2020 to support the travel industry in Japan. We do not observe any significant association between new cases and the index in the second wave (Table 2). The subsidy programme was suspended on 28 December 2020, complicating government efforts to address the economic fallout from the pandemic and extending the State of Emergency during the third wave. This may explain the negative association between new cases and SI, GRI and CHI during the third and fourth waves. Daily new cases in Japan soared following the start of the Olympics in the last week of July and in early August of 2021. Consequently, the policy indices of GRI and CHI fail to show effective prevention of confirmed cases in the fifth wave. Because of a state of emergency declaration and a spectator-less Tokyo 2020 Olympic Games, the number of confirmed cases in Tokyo dropped after the fifth wave. The negative association between new cases and SI also confirms this fact. Currently, in the sixth wave Japan has seen a rapid increase in new confirmed cases by more than three times over the previous wave, fuelled by the surge of Omicron. None of the indices negatively affect new confirmed cases in the sixth wave.
The economic reactivation and public health control of the COVID-19 pandemic have been asymmetric. When social activities were reactivated to boost the economy, the second and third waves in South Korea started, but there were differences in the public health response [12]. Our results of the second and third waves in Table 3 confirm a negative association between new cases and each index in the third wave, while a positive association exists between new cases and each index in the second wave. The results reveal South Korea's trending down of new death cases in the fourth wave and the entire period (Table 3). South Korea presents two seemingly contradictory pandemic indicators. It recorded over 100 000 new confirmed cases every day from 17 February 2022 to March 2022, as seen from the trend in Figure 3a. At the same time, the country has one of the lowest virus death rates globally (https://covid19.who.int/table).
During the first wave, Taiwan had nearly unblemished success at keeping the COVID-19 pandemic at bay with the world's longest track of case-free days. Due to the outbreak of infections derived from tea houses in the red-light district of Wanhua in Taipei on 23 April 2021, Taiwan was in the grip of its first major COVID-19 surge. The CECC announced a nationwide level 3 epidemic alert on 19 May 2021, but later eased some restrictions for level 3 from 13 July to 26 July 2021. The intervention results during the second wave seem to have been not so effective, showing insignificant associations between cases (deaths) and each index. The intervention during the third wave by Taiwan was relatively significant compared to the previous waves (Table 4).
A lead–lag effect, especially in economics, describes when one (leading) variable cross-correlates with the values of another (lagging) variable at later times. This study aims to quantify the time-lag effect reflected in new confirmed cases from authorities' response to the COVID-19 pandemic using SI (GRI or CHI) as an indicator of policy effectiveness. From the healthcare perspective, there are COVID-19-related studies that do investigate the time lag between the mobility response and government policy [22] and the lead–lag relationship between physical and mental health [23]. Our findings show no policy lag in Taiwan (Fig. 5). At the same time, there is no significant relationship between new confirmed cases and each index for Hong Kong, Japan and South Korea.
In May 2020 14% (79 out of 557) of COVID-19-related deaths in Japan took place in long-term care facilities [24]. Long-term care facilities with elderly residents are especially high-risk facilities in the event of COVID-19 viral transmissions. This may explain why the case fatality ratio of Japan is relatively higher than in other East Asia countries during the first wave (Fig. 4). For comparison, we also include the case fatality ratio of the elderly group for Sweden in Table 5. By the beginning of December 2020, more than 7000 people had died of COVID-19 in Sweden. Of these, almost 90% were 70 years or older, half were living in a long-term residential care facility, and just under 30% received home help services [25].
Table 5.
Information on the elderly group and test (per 1000) for all ages
| Confirmed cases | Deaths | Case fatality ratio | Test (per 1k) | Proportion of elderly | |
|---|---|---|---|---|---|
| Age ≥70 (%) | Age ≥70 (%) | Age ≥70 (%) | All ages | Age ≥65 (%) | |
| Hong Kong | 11.63 | 87.51 | 4.72 | 5954.47 | 19.60 |
| Japan | 8.18 | 86.53 | 4.69 | 328.57 | 29.79 |
| South Korea | 6.93 | 81.21 | 1.48 | 1683.60 | 16.65 |
| Taiwan | 13.27 | 61.62 | 25.01 | 292.77 | 15.96 |
| Sweden | 5.66 | 88.75 | 11.50 | 1788.10 | 20.10 |
The case fatality ratios by age group in Japan, Hong Kong, South Korea and Taiwan as of March 2022 appear in Figure 6.1 This confirms an earlier report [25] that case fatality ratios exhibit age group-specific disparity and a high percentage of deaths in elderly people. It shows that the case fatality ratios of the elderly group (age ≥70) in Japan, Hong Kong and South Korea are 4.69%, 4.72% and 1.48%, respectively, while the case fatality ratio of the elderly group (age ≥70) in Taiwan is 25.01% (Table 5). The proportion of deaths in the elderly group (age ≥70) of Japan as of March 2022 is 86.53% of confirmed deaths, in which the first wave may dominate. The reason for elderly deaths could be that some countries performed mass testing or initiated substantial prevention measures, which helped avoid a large number of potential deaths; it could also be that insufficient vaccinations led to them being unable to prevent these issues or families abandoning their elderly amid this pandemic [26].
We also provide total tests per thousand (total tests/population × 1000) as of March 2022 in the fifth column of Table 5. Hong Kong and South Korea have undergone mass testing compared to Japan and Taiwan. At the start of the pandemic in 2020, South Korea was hit by some of the worst early COVID-19 outbreaks, but it appeared to have brought them under control through mass testing and aggressive contact tracing. However, the South Korea government announced on 7 February 2022 that it was abandoning the test-and-trace system in the face of a surge of Omicron cases that threatened to overwhelm the country's health system [27]. Authorities of South Korea prioritise tests for people aged 60 or older.
We add the proportion of elderly in East Asia and Sweden in the last column of Table 5. Unfortunately, we only can provide the proportion of people aged over 65 in 2021 instead of the elderly group aged over 70. We observe that the proportion of elderly people in 2021 ranges from around 15% to 30% and also note that the proportion of the elderly in Japan is the highest in this study. There is clearly no obvious association between this proportion and the case fatality ratio for the elderly group.
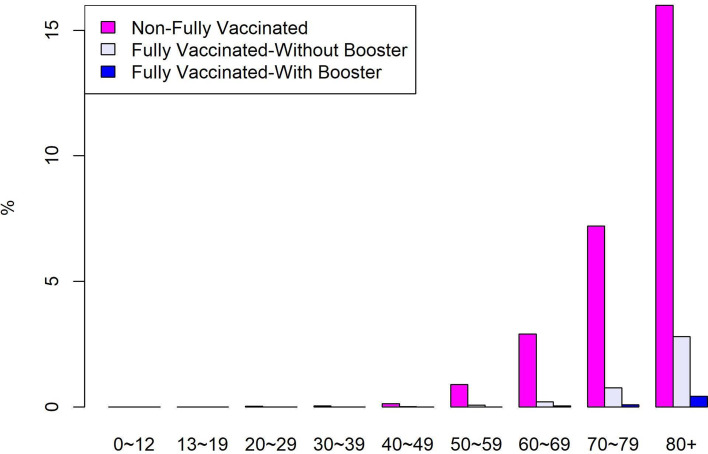
It is impossible to examine how the Hong Kong and Taiwan governments are responding to COVID-19 without considering their past experience with the SARS epidemic in 2003. Hong Kong and Taiwan both faced severe consequences from the SARS outbreak [28, 29]. Both governments have effectively provided non-pharmaceutical interventions in terms of the negative association between COVID-19 confirmed cases and the indices. Table 1 reveals such negative associations between COVID-19 confirmed cases and the indices of Hong Kong during the second, third and fifth waves. However, the proportion of deaths in the elderly group (age ≥70) of Hong Kong is 87.51% of confirmed deaths, which is similar to Sweden's elderly group at 88.75% (Table 5). As of 25 March 2022, the proportion of people aged over 80 in Hong Kong who have received two vaccine doses or more is 53.19% [30]. Around one-half of people aged 80 and over in Hong Kong have been given two doses or more of a vaccine before the Omicron surge, compared to over 90% in Singapore. A recent report (accessed 27 March 2022) by the Ministry of Health, Singapore shows that 16% of confirmed death in those aged 80 and over in Singapore were non-fully vaccinated, while 2.8% and 0.42% were fully vaccinated-without booster and fully vaccinated-with booster, respectively (Fig. 7).
Fig. 7.
Proportion of COVID-19 cases in Singapore who died, by age and vaccination status.
There is a steep case fatality ratio for Taiwan after May 2021. The case fatality ratio of March 2022 in the elderly group (age ≥70) is 25.01%, which is the highest case fatality ratio for the elderly group in our study. Taiwan began Oxford-AstraZeneca COVID-19 vaccinations on 22 March 2021, while the Moderna COVID-19 vaccine rollout started on 9 June 2021. Its CECC announced a COVID-19 vaccine distribution strategy on 20 June 2021. Table 6 presents the 10 approved priority groups.
Table 6.
COVID-19 vaccination rollout in Taiwan announced by the CECC on 20 June 2021
| Group | Vaccination target | Estimated number of peoplea | Cumulative number of peoplea |
|---|---|---|---|
| 1 | Healthcare workers | 50.6 | 50.6 |
| 2 | Central and local government epidemic prevention personnel | 13.9 | 64.5 |
| 3 | Frontline workers with a high risk of COVID-19; e.g. domestic aviation industry flight crew, etc. | 6.1 | 70.6 |
| 4 | Those who need to travel abroad | 0.2 | 70.8 |
| 5 | Law enforcement officers and firefighters | 46.7 | 117.5 |
| 6 | Elderly people aged 75 and over and pregnant women | 168 | 285.5 |
| 7 | National security personnel | 86 | 371.5 |
| 8 | Those aged 65–74 | 198.5 | 570 |
| 9 | Adults aged 19–65 with life-threatening conditions, rare diseases or a history of serious illness | 387.5 | 957.5 |
| 10 | Adults between the ages of 50 and 64 | 530 | 1487.5 |
Unit is 10 000 people.
The elderly people aged 75 and over and pregnant women rank in the sixth priority group, while those aged 65–74 ranked as the eighth priority, and adults aged 50–64 with the largest number rank at tenth priority. This may explain the highest case fatality ratio of March 2022 in Taiwan in the elderly group, as they are insufficiently vaccinated. Based on the death rate of Hong Kong's largely unvaccinated elderly group [21] and the lower priority order for Taiwan's elderly group after vaccines rolled out, we draw a conclusion that a fully vaccinated person with a booster is presently the best strategy for reducing deaths from COVID-19 in the elderly group.
Limitations
This study has two limitations. First, the information provided in this study relates to current evidence but may be modified as more information becomes available. Second, the number of confirmed cases may be lower than the true number of infections due to limited testing.
Conclusion
Our results show that non-pharmaceutical interventions have significant effects on reducing COVID-19 infections for some periods before the rise of the Omicron variant, offering evidence of a significantly negative association between confirmed cases and the study's indices. The three indices do not include an evaluation of vaccination, and CHI only covers investments in vaccines. Our conclusion agrees with some recent studies [8, 31] in which advances in the prevention and effective management of COVID-19 will require basic and clinical investigation and public health and clinical interventions. A government's COVID-19 vaccination distribution and prioritisation policies are pivotal for the elderly group. The study offers a particularly profound lesson, whereby if the vaccination rate for the elderly is low, then their death rate tends to be high. Immunising the elderly group as best as possible and managing their ‘long COVID’ after infection [32] have undoubtedly become top priorities.
Acknowledgements
The authors thank the editor, the academic editor and anonymous referees for their precious time and helpful comments, which have improved this paper.
Footnotes
All age group data sources are from government official websites as of 25–27 March 2022.
Supplementary material
For supplementary material accompanying this paper visit http://doi.org/10.1017/S0950268822001388.
click here to view supplementary material
Data availability statement
The dataset underlying the results described in this paper can be found in the ‘Data description’ section. Details of all data sources can be found in the Supplementary material.
References
- 1.Chu AMY et al. (2020) Analysis of travel restrictions for COVID-19 control in Latin America through network connectedness. Journal of Travel Medicine 27, taaa176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chu AMY et al. (2021) Are travel restrictions helpful to control the global COVID-19 outbreak? Travel Medicine and Infectious Disease 41, 102021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cowling BJ et al. (2020) Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health 5, e279–e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perra N (2021) Non-pharmaceutical interventions during the COVID-19 pandemic: a review. Physics Reports 913, 1–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hale T et al. (2021) A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nature Human Behaviour 5, 529–538. [DOI] [PubMed] [Google Scholar]
- 6.Chisadza C, Clance M and Gupta R (2021) Government effectiveness and the COVID-19 pandemic. Sustainability 1313, 3042. [Google Scholar]
- 7.Chen CWS et al. (2021) What factors drive the satisfaction of citizens on governments’ responses to COVID-19? International Journal of Infectious Diseases 102, 327–331. [DOI] [PubMed] [Google Scholar]
- 8.Chen CWS and Fan TH (2022) Public opinion concerning governments’ response to the COVID-19 pandemic. PLoS One 17, e0260062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ritchie H et al. (2020) Coronavirus pandemic (COVID-19). Published online at OurWorldInData.org. Available at https://ourworldindata.org/coronavirus.
- 10.Khamis H (2008) Measures of association: how to choose? Journal of Diagnostic Medical Sonography 24, 155–162. [Google Scholar]
- 11.Liao Q et al. (2021) Assessing community vulnerability over 3 waves of COVID-19 pandemic, Hong Kong, China. Emerging Infectious Diseases 27, 1935–1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seong H et al. (2021) Comparison of the second and third waves of the COVID-19 pandemic in South Korea: importance of early public health intervention. International Journal of Infectious Diseases 104, 742–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Furukawa K et al. (2021) Cross-neutralizing activity against SARS-CoV-2 313 variants in COVID-19 patients: comparison of 4 waves of the pandemic in Japan. Open Forum Infectious Diseases 8, ofab430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nagao M et al. (2022) Analysis of a city-wide COVID-19 prevention strategy for aged-care facilities during third and fifth waves of COVID-19 in Kyoto City, Kyoto, Japan. Influenza and Other Respiratory Viruses 16, 690–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adam DC et al. (2020) Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kong. Nature Medicine 26, 1714–1719. [DOI] [PubMed] [Google Scholar]
- 16.Ministry of Education, Culture, Sports, Science, and Technology (2020) Temporary closure of elementary schools, junior high schools, high schools, and special needs schools, to combat COVID-19 (28 February 2020). Available at https://www.mext.go.jp/content/202002228-mxt_kouhou01-000004520_1.pdf (Accessed 19 July 2022) (in Japanese).
- 17.Yamamoto T et al. (2020) The psychological impact of ‘mild lockdown’ in Japan during the COVID-19 pandemic: a nationwide survey under a declared state of emergency. International Journal of Environmental Research and Public Health 17, 9382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shim E et al. (2020) Transmission potential and severity of COVID-19 in South Korea. International Journal of Infectious Diseases 93, 339–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taiwan Centers for Disease Control (2022) CECC raises epidemic alert level for Taipei City and New Taipei City to level 3 and strengthens national restrictions and measures, effective from May 15 to May 28, in response to increasing level of community transmission. Available at https://www.cdc.gov.tw/En/Bulletin/Detail/R1K7gSjoYa7Wojk54nW7fg?typeid=158 (Accessed 19 July 2022) (in Chinese).
- 20.Taiwan Centers for Disease Control (2022) CECC raises epidemic warning to level 3 nationwide from May 19 to May 28; strengthened measures and restrictions introduced across Taiwan to reduce community transmission. Available at https://www.cdc.gov.tw/En/Bulletin/Detail/VN_6yeoBTKhRKoSy2d0hJQ?typeid=158 (Accessed 19 July 2022) (in Chinese).
- 21.Taylor L (2022) COVID-19: Hong Kong reports world's highest death rate as zero COVID strategy fails. The BMJ 376, o707. [DOI] [PubMed] [Google Scholar]
- 22.Bian Z et al. (2021) Time lag effects of COVID-19 policies on transportation systems: a comparative study of New York City and Seattle. Transportation Research Part A: Policy and Practice 145, 269–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luo MS, Chui EWT and Li LW (2020) The longitudinal associations between physical health and mental health among older adults. Aging & Mental Health 24, 1990–1998. [DOI] [PubMed] [Google Scholar]
- 24.Kyodo News Service (2020) Available at https://www.47news.jp/4808143.html (in Japanese).
- 25.Melin M et al. (2020) The Corona Commission. Elderly care during the pandemic. Ministry of Health and Social Affairs, summary of SOU. Ministry of Health and Social Affairs: 80. Available at https://www.government.se/4af26a/contentassets/2b394e1186714875bf29991b4552b374/summary-of-sou-2020 80-elderly-care-during-the-pandemic.pdf.
- 26.Brooke J and Jackson D (2020) Older people and COVID-19: isolation, risk and ageism. Journal of Clinical Nursing 29, 2044–2046. [DOI] [PubMed] [Google Scholar]
- 27.Smith N and Lee J (2022) South Korea abandons its successful test and trace system as omicron cases surge. The Telegraph. Available at https://www.telegraph.co.uk/global-health/science-and-disease/south-korea-abandons-successful-drop-test-trace-system-omicron/.
- 28.Hsieh YH, Chen CWS and Hsu SB (2004) SARS outbreak in Taiwan: what we can learn from modeling. Emerging Infectious Diseases 10, 1515–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leung GM, Hedley AJ and Ho LM (2004) The epidemiology of severe acute respiratory syndrome in the 2003 Hong Kong epidemic: an analysis of all 1755 patients. Annals of Internal Medicine 141, 662–673. [DOI] [PubMed] [Google Scholar]
- 30.The Government of the Hong Kong Special Administrative Region. Hong Kong vaccination dashboard (2022). https://www.covidvaccine.gov.hk/en/dashboard (Accessed 3 April 2022).
- 31.Flaxman S et al. (2020) Estimating the effects of nonpharmaceutical interventions on COVID-19 in Europe. Nature 584, 257–261. [DOI] [PubMed] [Google Scholar]
- 32.So MKP, Chu AMY and Tiwari A (2022) Persistent symptoms after SARS-CoV-2 infection: long-term implications for health and quality of life. The Lancet Regional Health–Europe 17, 100373. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://doi.org/10.1017/S0950268822001388.
click here to view supplementary material
Data Availability Statement
The dataset underlying the results described in this paper can be found in the ‘Data description’ section. Details of all data sources can be found in the Supplementary material.