Abstract
Objectives
To define the population prevalence of rotator cuff tears and test their association with pain and function loss; determine if severity symptom correlates with tear stage severity, and quantify the impact of symptomatic rotator cuff tears on primary healthcare services in a general population cohort of women.
Design
Cross-sectional observational study.
Participants
Individuals were part of the Chingford 1000 Women cohort, a 20-year-old longitudinal population study comprising 1003 women aged between 64 and 87, and representative of the population of the UK.
Main outcome measures
Rotator cuff pathology prevalence on ultrasound, shoulder symptoms using the Oxford Shoulder Score and resultant number of general practitioner (GP) consultations.
Results
The population prevalence of full-thickness tears was 22.2%, which increased with age (p=0.004) and whether it was the dominant arm (Relative Risk 1.64, OR 1.58, 95% CI 1.07 to 2.33, p=0.021).
Although 48.4% of full-thickness tears were asymptomatic, there was an association between rotator cuff tears and patient-reported symptoms. Individuals with at least one full-thickness tear were 1.97 times more likely than those with bilateral normal tendons (OR 3.53, 95% CI 2.00 to 5.61, p<0.001) to have symptoms. Severity of symptoms was not related to the severity of the pathology until tears are >2.5 cm (p=0.009).
In the cohort, 8.9% had seen their GP with shoulder pain and a full-thickness rotator cuff tear, 18.8% with shoulder pain and an abnormality and 29.3% with shoulder pain.
Conclusion
Rotator cuff tears are common, and primary care services are heavily impacted. As 50% of tears remain asymptomatic, future research may investigate the cause of pain and whether different treatment modalities, aside from addressing the pathology, need further investigation.
Keywords: Shoulder, Ultrasonography, Musculoskeletal disorders, Diagnostic radiology
Strengths and limitations of this study.
Pain on the Oxford Shoulder Score is associated with the presence of rotator cuff tendon pain but not the extent of structural pathology identified on ultrasound imaging.
Rotator cuff pathology and associated symptoms pose a large burden on the healthcare system with 28.8% of people seeking general practitioner consultation for their shoulder pain.
This epidemiological study demonstrates association but not causality and leaves unanswered questions as to what additional factors contribute to shoulder pain.
Introduction
Musculoskeletal pain is one of the most common sources of disability in the Western world.1 The shoulder is the third most common site of musculoskeletal disease,2 with an estimated 20% of the population reporting pain at any given time.3 Pain related to rotator cuff tears are estimated to account for 30%–40% of these shoulder complaints,4 causing high levels of disability and associated healthcare costs.5–7 High-definition ultrasound is the current gold standard for the detection of full-thickness tears and is a valid tool to detect an abnormal tendon enthesis,8 but has poorer accuracy to detect partial-thickness tears.8–14 Full thickness tears are recognised to be common and associated with increasing age15–18; however, prevalence in symptomatic and asymptomatic shoulders varies widely across cadaveric,19 radiological19 and retrospective cohort studies.16–18 20–28 Furthermore, the presence of selection bias in studies undertaken in rotator cuff tendon tears16–28 has meant population-based studies available are not representative of Western demographics. Thus, research in this area may lead to a better understanding of the natural history of rotator cuff tears.
Clinical manifestations of rotator cuff tears are varied,15 17 22 26 28 and detection of pathology and its relationship to clinical symptoms is not well established. Many tears are asymptomatic but are thought to be a risk of developing symptoms with time.26 Although larger tears are more likely to be painful, there is also no evidence to suggest that they have a greater severity of symptoms than smaller tears.29 One population cohort from a mountainous region has suggested that only a third of full-thickness tears were painful, of which symptoms were more prevalent in the dominant arm.30 However, all studies investigating symptom association have looked at isolated shoulders and have not considered that the individual has two shoulders. It is therefore plausible that there may be the presence of other physical or psychological factors unique to the individual, rather than the specific shoulder, that may have an influence on symptom presentation, rather than solely the underlying pathology. To date, no study has explored the association between rotator cuff tears, pain and functional loss in a general population cohort, or how these impact on a health service.
Objectives
This study aims to (1) describe the population prevalence of different stages of rotator cuff tear in a general population cohort of women; (2) determine what proportion of rotator cuff tears are symptomatic and whether the severity of symptoms correlates with tear stage severity; (3) identify individual influences on the likelihood of symptoms and (4) quantify the impact of symptomatic rotator cuff tears on primary healthcare services.
Methods
Study design, setting and participants (including study size)
Participants in this cross-sectional observational study were involved in the larger Chingford 1000 Women study. This is an ethically approved, well-described prospective population-based longitudinal study of osteoarthritis and osteoporosis comprising 1003 white Caucasian women, derived from the register of a large general practice in Chingford, North London.31 32 33 31–33 The cohort was recruited in 1989 where the women were aged 44–67. They have been characterised as representative of women in the UK general population with respect to weight, height and smoking characteristics. The cohort has been subsequently listed by the National Institute for Health Research as an important epidemiological recourse. This study took place at the Chingford 20-year follow-up visit where 516 of the original 1003 cohorts attended (158 women had died; 111 were unable to attend; 218 had moved away or had been lost to follow-up). A musculoskeletal assessment, including the Oxford Shoulder Score (OSS) and shoulder ultrasound examination, was performed on both shoulders (left and right) in 463 women (out of the 515, 52 attended but did not have a shoulder assessment due to lack of assessor, and one did not complete an OSS).
Variables and data sources
Participant characteristics of age, height, weight, hand dominance and a self-reported musculoskeletal questionnaire filled out a priori (including the OSS,34 35 body chart and questions regarding previous pain, treatments and whether medical advice has been sought) were all collected at baseline. A musculoskeletal ultrasound assessment on bilateral shoulders was then undertaken using a fixed standard operating procedure protocol).
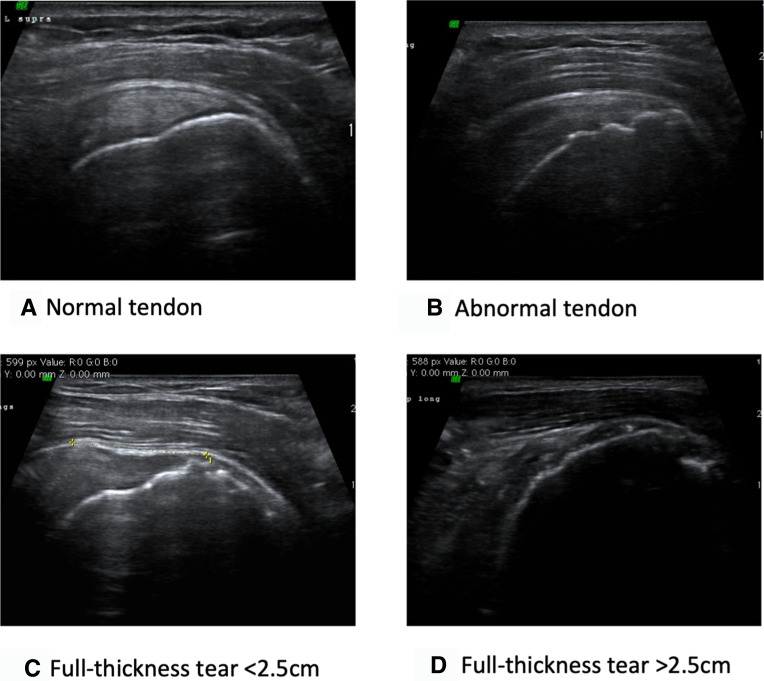
The ultrasound examination of the 464 women was completed by two orthopaedic assessors and performed using a GE Voluson i portable ultrasound machine with a 10–16 MHz linear probe. Ultrasound training and appropriate validation studies36 were completed as recommended by the BESS focus group; 343 individuals were scanned by assessor 1 and 121 individuals by assessor 2. Appropriate inter-rater and intra-rater reliability studies were performed and showed high reproducibility (weighted kappa 0.92, p<0.001) and no difference in reporting trends (p=0.08). The ultrasound protocol was derived according to the recommendations of the Nuffield Orthopaedic Centre musculoskeletal radiology department. Tendons were classified into one of four working groups based on ultrasound measurements as validated by Hinsley et al8: normal tendon, abnormal tendon and partial thickness tear, single-tendon full-thickness tear (0–2.5 cm) and multitendon full-thickness tear (>2.5 cm) (figure 1).
Figure 1.
Tendon classification on ultrasound. (A) Normal tendon: normal homogenous appearance throughout with no abnormality at the enthesis; (B) abnormal tendon: loss of homogenous appearance and abnormal ragged enthesis±enlarged fluid-filled bursa or partial thickness tear; (C) full thickness tear (0–2.5 cm): lucent patch through the full thickness of the tendon with tear size defined as its width in the sagittal plane; (D) full-thickness tears (>2.5 cm): evidence of large defect or no evidence of tendon tissue present.
Quantitative variables and statistical methods
All statistics were performed using IBM SPSS Statistics V.22.
Age, body mass index (BMI), hand dominance and symptom presence were compared across the four different tendon pathology groups. Wilcoxon rank-sum test, one-way analysis of variance (ANOVA) and χ2 tests were used for non-normal, normal and categorical data, respectively.
Population prevalence of full-thickness tears was defined as having at least one unilateral full-thickness tear. Population prevalence of tendon abnormalities was defined as having at least a unilateral tendon abnormality ranging from abnormal enthesis to a full-thickness tear. This was calculated by summing the percentage with unilateral tears and the percentage with bilateral tears for each age group.
Symptoms were defined using the OSS.34 35 This was chosen for what the authors believed represented the best content and construct validity as applicable to the study as it covers a range of symptoms (both relating to pain and function) over a 4-week time period and also allows discriminate ability. Binary symptoms were defined by dichotomising the OSS,34 35 where any non-perfect score (≤47/48) was classified as symptomatic. The cut-off at 47 was used to determine symptoms as we were not looking for significant changes, rather the ability to detect any individual who was unable to perform an activity to the full or who has pain at any given time. We validated this by running a Pearson correlation subanalysis between the OSS pain subset with the Numerical Rating Scale (NRS) (R=0.816, p<0.001, 95% CI 0.793 to 0.836) and a simple binary question (R=0.812, p<0.001, 95% CI 0.789 to 0.833), and the full OSS with a binary pain question (R=0.759, p<0.001, 95% CI 0.730 to 0.785). Furthermore, we reran the analysis using a 3-point difference to reflect a clinically significant difference between groups, and the results were not significantly different. Where questions are pain specific, the four pain specific questions of the OSS were used as a subscale. In symptomatic participants, the full OSS scale, scored on a 0–48 point scale, was used to define symptom severity. A χ2 test was used to determine any difference between tendon pathology groups. Multivariate binary logistic regression was used to adjust for the potential confounders age, BMI and hand dominance determined a priori. To account for a high positive skew of the OSS data when determining symptom severity, all asymptomatic shoulders were removed, and a logarithmic transformation of the inverse OSS was used to create a normal distribution. Symptom severity in symptomatic shoulders was compared across tendon pathology groups using one-way ANOVA. Multivariate linear regression was used to adjust for potential confounders age and hand dominance determined a priori.
Results
Participants and descriptive data
A total of 464 individuals (928 shoulders) were included in the study (table 1). The distribution of age across each tendon pathology group was significantly different (p<0.001), with age increasing in accordance with tear severity. There was a statistical difference in the proportion of dominant and non-dominant arms in each tendon pathology group (p=0.033), with there being significantly more non-dominant arms in the normal tendon group (p=0.010) and significantly more dominant arms in those with full-thickness tears (p=0.026). There were no between-group differences in BMI (p=0.080).
Table 1.
Demographics of all the shoulders included in the study
| Frequency | % | Median age | Mean BMI | Dominant arm (%) | |
| Normal | 510 | 55.0 | 70 | 27.5 | 46.1 |
| Abnormal/partial tear | 294 | 31.7 | 73 | 28.0 | 52.7 |
| Full-thickness tear, 0–2.5 cm | 85 | 9.2 | 74 | 27.9 | 58.8 |
| Full-thickness tear, >2.5 cm | 39 | 4.2 | 74 | 29.6 | 61.5 |
| All | 928 | 100 | 71 | 27.8 | 50 |
BMI, body mass index.
Outcome data and main results
Prevalence of rotator cuff tendon pathology
The population prevalence of having at least one full-thickness tear was 22.2% (4.5% bilateral). For age groups 60–69, 70–79 and 80–89, these were 14.9%, 25.9% and 29%, respectively, and bilateral tears were 2.3%, 5.9% and 5.8%, respectively. The difference in prevalence between age groups was statistically different (p<0.001).
The population prevalence of having at least a unilateral tendon pathology or tear was 59.5% (30.6% bilateral). For age groups 60–69, 70–79 and 80–89, these were 51.5%, 61.8% and 72.5%, respectively, and bilateral tears were 24.6%, 32.3% and 40.6%, respectively. The difference in population prevalence between age groups was statistically significant (p<0.001).
Table 2 shows the prevalence of rotator cuff tendinopathy in the dominant and non-dominant arms in age deciles. The distribution of tendinopathy differed between age groups (dominant arm, p=0.002; non-dominant arm, p=0.037) with more pathology found in older age groups and in the dominant compared with non-dominant arms (p=0.004). There was no difference in prevalence according to the BMI group. The relative risk of full-thickness tear was 1.64 (OR 1.580, 95% CI 1.073 to 2.326, p=0.021) in the dominant arm compared with non-dominant arm. For those aged 70–79, it was 2.072 (OR 2.026, 95% CI 1.286 to 3.190, p=0.002), and those aged 80–89 was 2.293 (OR 2.256, 95% CI 1.264 to 4.027, p=0.006) compared with those aged 60–69.
Table 2.
Prevalence of rotator cuff tendon pathology according to age decile and arm dominance
| Age group (years) | ||||||||
| 60–69 (n=175) | 70–79 (n=220) | 80–89 (n=69) | Total (N=464) | |||||
| Count | % | Count | % | Count | % | Count | % | |
| Dominant arm | ||||||||
| Normal tendon | 102 | 58.30 | 111 | 50.50 | 22 | 31.90 | 235 | 50.60 |
| Abnormal tendon/partial thickness tear | 54 | 30.90 | 67 | 30.50 | 34 | 49.30 | 155 | 33.40 |
| Full-thickness tear, 0–2.5 cm | 14 | 8.00 | 27 | 12.30 | 9 | 13.00 | 50 | 10.80 |
| Full-thickness tear, >2.5 cm | 5 | 2.90 | 15 | 6.80 | 4 | 5.80 | 24 | 5.20 |
| Non-dominant arm | ||||||||
| Normal tendon | 115 | 65.70 | 122 | 55.50 | 38 | 55.10 | 275 | 59.30 |
| Abnormal tendon/partial thickness tear | 49 | 28.00 | 70 | 31.80 | 20 | 29.00 | 139 | 30.00 |
| Full-thickness tear, 0–2.5 cm | 10 | 5.70 | 18 | 8.20 | 7 | 10.10 | 35 | 7.50 |
| Full-thickness tear, >2.5 cm | 1 | 0.60 | 10 | 4.50 | 4 | 5.80 | 15 | 3.20 |
Association of symptoms (all shoulders)
An analysis of symptom association was completed in 926 shoulders (463/464 participants due to loss of one questionnaire). There were 289 (31.2%) symptomatic shoulders according to a dichotomised OSS. The presence of symptoms was statistically significant between tendon groups (p<0.001); 51.6% of all full-thickness tears were symptomatic. There was no difference in age, BMI or arm dominance between symptomatic or asymptomatic shoulders. The relative risks of having symptoms compared with those with a reported normal tendon were as follows: abnormal/partial tears 1.969 (OR 1.991, 95% CI 1.454 to 2.727); full-thickness tears 0–2.5 cm 2.203 (OR 2.366, 95% CI 1.465 to 3.891); and full-thickness tears >2.5 cm 4.718 (OR 9.800, 95% CI 4.638 to 20.705). All were significant (p<0.001) with the model correctly predicting 71% of symptom outcomes correctly. The distribution of symptoms across each tendon group is shown in figure 2.
Figure 2.
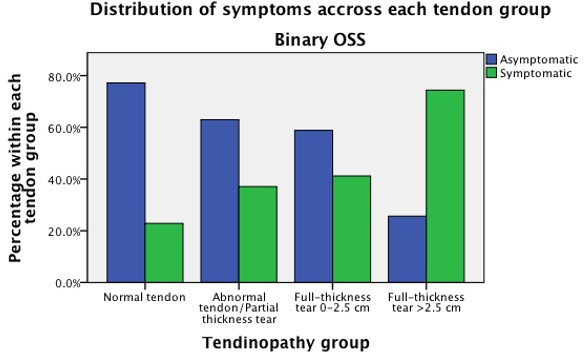
Distribution of symptoms across each tendon group. OSS, Oxford Shoulder Score.
When the same analysis was performed using a 3-point change in the OSS to define symptoms, the results were not statistically different and compared with normal tendons were as follows: abnormal/partial tears 1.793 (OR 1.936, 95% CI 1.374 to 2.726); full-thickness tears 0–2.5 cm 2.098 (OR 2.506, 95% CI 1.513 to 4.150); and full-thickness tears >2.5 cm 3.924 (OR 9.678, 95% CI 4.784 to 19.580). All were significant (p<0.001).
Symptom severity
For the 289 symptomatic shoulders, the full OSS was reported (table 3). Median age was significantly different between groups (p=0.047), with age increasing with tear stage severity. No statistically significant between-group differences in BMI were identified, nor any within-group differences for arm dominance.
Table 3.
Demographics of the 289 symptomatic shoulders
| N | Median age | Mean BMI | Dominant arm (%) | |
| Normal | 116 | 70 | 28.3 | 46.6 |
| Abnormal/partial tear | 109 | 73 | 28.4 | 54.1 |
| Full-thickness tear, 0–2.5 cm | 35 | 72 | 28.1 | 62.9 |
| Full-thickness tear, >2.5 cm | 29 | 73 | 30.3 | 58.6 |
| All | 289 | 71 | 28.5 | 50 |
The mean OSS for symptomatic shoulders was 41.8. For normal tendons, this was 42.5, abnormal tendons, 42.1; full-thickness tears (0–2.5 cm), 40.2; and full-thickness tears (>2.5 cm), 38.4. There was a statistical difference between the groups (one-way ANOVA, p=0.030). Linear regression analysis after adjustment for age, BMI and hand dominance (no interactions identified) showed that the only significant difference in OSSs was between normal tendons (mean OSS 42.5) and large full-thickness tears (OSS 38.3, p=0.009, power 0.75; overall model p=0.007, power 0.892).
Association of symptoms (individuals)
Table 4 shows the relationship between the individual, presence of full-thickness rotator cuff tear and the likelihood of symptoms. A clustering effect of bilateral symptoms or lack thereof is present, irrespective of the underlying pathology. After adjustment for age and BMI, compared with those with bilaterally normal shoulders, the relative risk of having at least one symptomatic shoulder in the presence of a full thickness rotator cuff tear is 1.49 (OR 1.867, 95% CI 1.200 to 2.904) and that in the presence of at least a unilateral abnormality or cuff tear is 1.97 (OR 3.352, 95% CI 2.003 to 5.609).
Table 4.
Distribution of individual shoulder symptoms according to the presence of full-thickness tears or tendon abnormalities
| No symptoms | Unilateral symptoms | Bilateral symptoms | Total | |
| Bilateral no Full Thickness Tear (FTT) | 226 | 71 | 63 | 360 |
| Unilateral FTT | 33 | 25 | 24 | 82 |
| Bilateral FTT | 10 | 3 | 8 | 21 |
| Bilateral normal | 131 | 28 | 28 | 187 |
| Unilateral abnormality | 72 | 34 | 28 | 134 |
| Bilateral abnormality | 66 | 37 | 39 | 142 |
| Total | 269 | 99 | 95 | 463 |
Shoulder pain and use of primary care health services
Table 5 shows the proportion of individuals with shoulder pain, past or present, seeking medical advice. The likelihood of seeking medical attention for shoulder pain was statistically different between each pathology group (χ2 test, p=0.005), reflecting the increasing likelihood of pain. However, of those with pain, the likelihood of seeking medical attention was not statistically different between groups (χ2 test p=0.179). Overall, 28.3% (131/463) of all individuals had at some stage seen their general practitioner (GP) for shoulder pain. In this cohort, 8.9% (41/463) had seen their GP with shoulder pain and a full-thickness tendon tear, and 18.8% (87/463) had seen their GP with an abnormal tendon or full thickness tear.
Table 5.
Proportion of individuals seeking medical advice
| Present symptoms (either shoulder) |
Past or present symptoms (either shoulder) |
All individuals | |||
| % | % seen GP | % | % seen GP | % seen GP | |
| All individuals (n=463) |
41.9 (n=194) |
44.8 (n=87) |
55.7 (n=258) |
50.8 (n=131) |
28.3 (n=131) |
| Bilaterally normal tendons (n=187) |
29.9 (n=56) |
41.1 (n=23) |
48.1 (n=90) |
48.9 (n=44) |
23.5 (n=44) |
| At least one abnormality (no tear) (n=173) |
45.1 (n=78) |
41.0 (n=32) |
57.2 (n=99) |
46.5 (n=46) |
26.6 (n=46) |
| At least one full-thickness tear (n=103) |
58.3 (n=60) |
53.3 (n=32) |
67.0 (n=69) |
59.4 (n=41) |
39.8 (n=41) |
GP, general practitioner.
A multivariable regression model using all individuals was used to predict the likelihood of attending a GP for shoulder pain. The presence of at least one full-thickness tear had a relative risk of 1.63 (OR 2.179, 95% CI 1.282 to 3.703) compared with those with normal tendons of attending the GP. There was no statistical difference in relative risk of those with any tendon abnormality compared with those with bilaterally normal shoulders.
Discussion
Key results
Using a large general population cohort of women aged 65–84 years, this study has reported on the prevalence of rotator cuff pathology, the association of pathology to symptoms and uniquely the consequential impact on health services.
The prevalence of rotator cuff pathology has been well reported in the literature, and this general population study supports previous findings. Prevalence was found to increase with every decile of age, and the relative risk of having a full thickness tear increased more than twofold between the 65–69 and >80 age groups, suggesting age-related change.18 Overall, the prevalence of at least a unilateral full thickness tear was 22%. The dominant arm was 1.64 times likely to be affected, inferring that the presence of pathology may exist in shoulders with higher cumulative loading.
The relative risk of having symptomatic pathology (worsening OSSs) increased with tear stage severity, though the severity of symptoms did not increase accordingly. Although larger tear size increased the likelihood of symptom presence, 48.4% of full-thickness rotator cuff tears remained asymptomatic.
The burden of musculoskeletal shoulder pain on health services is large, with 28.3% of individuals in this general population cohort having at some point sought medical advice for shoulder symptoms. This is the first study to look at the impact of rotator cuff pathology on the impact on the health services. Although on average only 50% of individuals with symptomatic rotator cuff tendon pathology (tendinopathy) will seek medical advice, the impact remains significant. Overall, almost 10% of individuals in the general population have sought medical advice for shoulder symptoms in the presence of a full-thickness tear, and almost 20% of the population for any tendon abnormality.
The major strength of this study is that it uses a large population-based cohort and is therefore not subject to selection bias. The cohort was originally investigated with the primary focus of osteoporosis, and not shoulder symptoms, thus any continued participation is not driven by shoulder symptoms.
Limitations (including bias)
The cohort can only comment on associations in women aged between 65 and 84, but as previous studies have found no relationship between symptoms and age or sex,23 30 this will not bias the results. Potential survival bias is introduced by the cohort being in its 20th year. If a greater proportion of individuals with pathology were lost to follow-up, this may cause us to underestimate any association; however, no known associations exist in the literature between rotator cuff tears and other medical comorbidities. Furthermore, as the prime goal of the cohort was not to investigate shoulder symptoms, this had no impact on continued study participation. Furthermore, only 463/516 individuals that attended the year 20 study underwent a shoulder examination due to lack of an examiner being present at these follow-up appointments. However, the age and BMI of the groups was not statistically different to the full cohort.
Bias arising from having two examiners was ameliorated by two interobserver reproducibility studies that demonstrated minimal effect of interobserver analytic bias. Furthermore, to demonstrate ultrasound-scanning accuracy, a learning curve study was undertaken a priori by both examiners, which demonstrated scanning accuracies comparable to those quoted in the literature. Interobserver studies also demonstrated good reproducibility reducing analytical bias. Potential risk of over-reporting pathology in symptomatic presentations is acknowledged as the assessor (ultrasonographer) was unblinded to the OSS result as for pragmatic reasons due to lack of assessors, both assessments were carried out by the same individual. To overcome this, a small intraobserver study was completed, and an additional ultrasound scan was performed on 18 willing participants. The examiner was blind to all previous results and shoulder scores. Overall agreement gave a weighted kappa score of 0.915 (p<0.001).
The effect of tear size on symptom severity may have been underestimated in this study. The inability to transform the complete data set due to the skew of the OSS data meant all asymptomatic shoulders had to be removed. Pain severity in the presence of a tear was then compared with a pain severity in a normal (no tendon pathology) shoulder. We recognise that there may be many causes of shoulder pain (eg, rheumatological causes), and therefore referencing against all causes of painful shoulder may represent the contribution of rotator cuff tear to the symptoms.
The definition of symptoms in previous studies varies widely with no consensus. The decision to use the OSS was based on its content, construct validity in relation to our research question, and validation of use against other pain scores. Furthermore, dichotomisation of the scale at perfect versus non-perfect scores is not validated and may make results too sensitive. However, we ran a comparison with 3-point change, as validated as clinically significant by the makers of the OSS, and there was no statistical difference.
Relationship to other studies
This study has demonstrated similar prevalence figures to previous studies, but it is the first to use a general population cohort that has been extensively characterised as representative of the Western world population.
Further studies have shown that the clinical presentation of rotator cuff tears varies and may or may not be associated with symptoms.17 22 23 This general population cohort supports this with 48.4% of full-thickness rotator cuff tears being asymptomatic. Prior to this, the only other population-based study looking at symptom association with full-thickness tears was that of Yamamoto et al30 that investigated symptom association with full-thickness tears using a mountain cohort in Japan. They reported 34% of full-thickness tears to be symptomatic. However, unlike the current study, it was not a general population cohort representative of western society. Furthermore, it was subject to selection bias by removing any individuals with restricted shoulder movement or previous treatments.
Further studies have suggested that tear size affects the likelihood of symptoms. The current study supports this with larger tears having a greater than twofold increase in relative risk of symptoms than small tears.17 22 23 A previous study in the Washington series investigated by Yamaguchi et al,26 reported development of symptoms in previously asymptomatic tendons in the context of a contralateral symptomatic tear. However, this study was subject to selection bias as recruitment occurred in a cohort actively being treated for contralateral symptomatic rotator cuff tears, which may have strengthened associations.
This is the first study that has looked at individuals as entities, rather than shoulders, and has highlighted the effect the individual has on symptom presentation, which could include physical and psychological factors unique to that individual, not solely the presence of tendon pathology on imaging. It is also the first study to look at the impact on health services.
Interpretation
This study has shown that, although patient reported pain on the OSS is associated with rotator cuff tendon pathology, it is not related to the severity of structural pathology identified on ultrasound imaging. The likelihood of pain also appears to be strongly dependent on the individual rather than simply the pathology. Consequently, clinicians should rely less on imaging findings to explain the cause and severity of shoulder pain presentations. Furthermore, other drivers of shoulder pain should be considered (eg, pain sensitisation), and treatment be targeted on symptom management rather than solely interventions to improve tendon pathology.
Investigation into the impact of musculoskeletal shoulder pain on the healthcare system revealed that 28.8% of people in this general population cohort sought consultation with their GP for shoulder pain, a third of whom had a full thickness tear, and a third with at least one abnormality (no tear). This study highlights the huge burden of shoulder pain on the healthcare system. However, neither does it demonstrate causality of pain as shown by the lack of symptoms in nearly half of cases and the lack of correlation with the severity of pain and pathology nor does it show how the individual affects pain presentation.
Generalisability
This epidemiological study that is generalisable to the UK population demonstrates association but not causality and leaves unanswered questions as to what additional factors contribute to shoulder pain. Particularly interesting is how individuals may or may not have painful shoulders irrespective of the pathology. Further research into this could provide alternative targets to treatment methods and potentially reduce the cost of imaging modalities and surgical interventions.
Conclusion
In conclusion, this population-based study has demonstrated that full-thickness rotator cuff tears affect 22.1% of women over the age of 60 and tendon abnormalities affect 59.4%. Despite 41.7% of individuals with a full-thickness tear (48.4% of all full-thickness tears) being asymptomatic, tendon abnormalities and tears are associated with pain. The likelihood, but not severity of symptoms, increases with greater structural damage.
This high prevalence and association of symptoms results in a significant impact on primary care health services, with 28.3% of this population having presented to a GP with shoulder pain. Of these, a third had a full-thickness tear and a third had an abnormal but non-torn tendon. Overall, 8.9% of this cohort had seen their GP with shoulder pain and a full-thickness tear, and 18.8% had seen their GP with an abnormal or torn tendon.
Supplementary Material
Acknowledgments
We would like to thank all the participants of the Chingford 1000 Women study for their time; Mrs Maxine Daniels and Dr Alan Hakim for their time and dedication; both Mr Alex Nichols and Mr Michael Daines for their assistance with data collection; and Dr Gemma Wallis for her assistance with data analysis.
Footnotes
Contributors: HH, NKA and AJC were responsible for planning, conducting, and reporting the work described in the article, had access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. HH and CG drafted the manuscript. All authors approved the final version of the article. HH is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. All authors fully acknowledge the contribution of the patients that participated in this study. No authors are employees of the National Institutes of Health.
Disclaimer: Arthritis Research United Kingdom awarded the project £190,361.00 to cover costs to completion. Researchers were independent from the funding body. All authors, external and internal, had full access to all the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. For information about the Chingford 1000 Women study, email chingford@ndorms.ox.ac.uk.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the local ethics committee (Outer North East London Research Ethics Committee (formerly Barking and Havering and Waltham Forest RECs), LREC (R&WF) reference ID = 96). The participants gave informed consent to participate in the study before taking part.
References
- 1. VosT, AbajobirAA, AbateKH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet 2017;390:1211–59. 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998;57:649–55. 10.1136/ard.57.11.649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pope DP, Croft PR, Pritchard CM, et al. Prevalence of shoulder pain in the community: the influence of case definition. Ann Rheum Dis 1997;56:308–12. 10.1136/ard.56.5.308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bunker T. Rotator cuff disease. Curr Orthop 2002;16:223–33. 10.1054/cuor.2002.0257 [DOI] [Google Scholar]
- 5.Meislin RJ, Sperling JW, Stitik TP. Persistent shoulder pain: epidemiology, pathophysiology, and diagnosis. Am J Orthop 2005;34:5–9. [PubMed] [Google Scholar]
- 6.Roquelaure Y, Ha C, Leclerc A, et al. Epidemiologic surveillance of upper-extremity musculoskeletal disorders in the working population. Arthritis Rheum 2006;55:765–78. 10.1002/art.22222 [DOI] [PubMed] [Google Scholar]
- 7.Ng Man Sun S, Gillott E, Bhamra J, et al. Implant use for primary hip and knee arthroplasty: are we getting it right first time? J Arthroplasty 2013;28:908–12. 10.1016/j.arth.2012.11.012 [DOI] [PubMed] [Google Scholar]
- 8.Hinsley H, Nicholls A, Daines M, et al. Classification of rotator cuff tendinopathy using high definition ultrasound. Muscles Ligaments Tendons J 2014;4:391–7. 10.32098/mltj.03.2014.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teefey SA, Rubin DA, Middleton WD, et al. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am 2004;86:708–16. [PubMed] [Google Scholar]
- 10.de Jesus JO, Parker L, Frangos AJ, et al. Accuracy of MRI, Mr arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol 2009;192:1701–7. 10.2214/AJR.08.1241 [DOI] [PubMed] [Google Scholar]
- 11.Naqvi GA, Jadaan M, Harrington P. Accuracy of ultrasonography and magnetic resonance imaging for detection of full thickness rotator cuff tears. Int J Shoulder Surg 2009;3:94–7. 10.4103/0973-6042.63218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith TO, Back T, Toms AP, et al. Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol 2011;66:1036–48. 10.1016/j.crad.2011.05.007 [DOI] [PubMed] [Google Scholar]
- 13.Dinnes J, Loveman E, McIntyre L, et al. The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review. Health Technol Assess 2003;7:1–166. :iii. 10.3310/hta7290 [DOI] [PubMed] [Google Scholar]
- 14.Ottenheijm RP, Jansen MJ, Staal JB, et al. Accuracy of diagnostic ultrasound in patients with suspected subacromial disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil 2010;91:1616–25. 10.1016/j.apmr.2010.07.017 [DOI] [PubMed] [Google Scholar]
- 15.Fehringer EV, Sun J, VanOeveren LS, et al. Full-Thickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elbow Surg 2008;17:881–5. 10.1016/j.jse.2008.05.039 [DOI] [PubMed] [Google Scholar]
- 16.Milgrom C, Schaffler M, Gilbert S, et al. Rotator-Cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br 1995;77:296–8. 10.1302/0301-620X.77B2.7706351 [DOI] [PubMed] [Google Scholar]
- 17.Moosmayer S, Smith H-J, Tariq R, et al. Prevalence and characteristics of asymptomatic tears of the rotator cuff: an ultrasonographic and clinical study. J Bone Joint Surg Br 2009;91:196–200. 10.1302/0301-620X.91B2.21069 [DOI] [PubMed] [Google Scholar]
- 18.Tempelhof S, Rupp S, Seil R. Age-Related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg 1999;8:296–9. 10.1016/S1058-2746(99)90148-9 [DOI] [PubMed] [Google Scholar]
- 19.Reilly P, Macleod I, Macfarlane R, et al. Dead men and radiologists don't lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Ann R Coll Surg Engl 2006;88:116–21. 10.1308/003588406X94968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116–20. 10.1016/j.jse.2009.04.006 [DOI] [PubMed] [Google Scholar]
- 21.Schibany N, Zehetgruber H, Kainberger F, et al. Rotator cuff tears in asymptomatic individuals: a clinical and ultrasonographic screening study. Eur J Radiol 2004;51:263–8. 10.1016/S0720-048X(03)00159-1 [DOI] [PubMed] [Google Scholar]
- 22.Yamaguchi K, Ditsios K, Middleton WD, et al. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am 2006;88:1699–704. 10.2106/JBJS.E.00835 [DOI] [PubMed] [Google Scholar]
- 23.Mall NA, Kim HM, Keener JD, et al. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am 2010;92:2623–33. 10.2106/JBJS.I.00506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Needell SD, Zlatkin MB, Sher JS, et al. Mr imaging of the rotator cuff: peritendinous and bone abnormalities in an asymptomatic population. AJR Am J Roentgenol 1996;166:863–7. 10.2214/ajr.166.4.8610564 [DOI] [PubMed] [Google Scholar]
- 25.Sher JS, Uribe JW, Posada A, et al. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 1995;77:10–15. 10.2106/00004623-199501000-00002 [DOI] [PubMed] [Google Scholar]
- 26.Yamaguchi K, Tetro AM, Blam O, et al. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg 2001;10:199–203. 10.1067/mse.2001.113086 [DOI] [PubMed] [Google Scholar]
- 27.Chandnani V, Ho C, Gerharter J, et al. Mr findings in asymptomatic shoulders: a blind analysis using symptomatic shoulders as controls. Clin Imaging 1992;16:25–30. 10.1016/0899-7071(92)90085-N [DOI] [PubMed] [Google Scholar]
- 28.Minagawa H, Yamamoto N, Abe H, et al. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: from mass-screening in one village. J Orthop 2013;10:8–12. 10.1016/j.jor.2013.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris JD, Pedroza A, Jones GL, et al. Predictors of pain and function in patients with symptomatic, atraumatic full-thickness rotator cuff tears: a time-zero analysis of a prospective patient cohort enrolled in a structured physical therapy program. Am J Sports Med 2012;40:359–66. 10.1177/0363546511426003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yamamoto A, Takagishi K, Kobayashi T, et al. Factors involved in the presence of symptoms associated with rotator cuff tears: a comparison of asymptomatic and symptomatic rotator cuff tears in the general population. J Shoulder Elbow Surg 2011;20:1133–7. 10.1016/j.jse.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 31.Hart DJ, Spector TD. The relationship of obesity, fat distribution and osteoarthritis in women in the general population: the Chingford study. J Rheumatol 1993;20:331–5. [PubMed] [Google Scholar]
- 32.Hart DJ, Mootoosamy I, Doyle DV, et al. The relationship between osteoarthritis and osteoporosis in the general population: the Chingford study. Ann Rheum Dis 1994;53:158–62. 10.1136/ard.53.3.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arden NK, Griffiths GO, Hart DJ, et al. The association between osteoarthritis and osteoporotic fracture: the Chingford study. Br J Rheumatol 1996;35:1299–304. 10.1093/rheumatology/35.12.1299 [DOI] [PubMed] [Google Scholar]
- 34.Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 1996;78:593–600. 10.1302/0301-620X.78B4.0780593 [DOI] [PubMed] [Google Scholar]
- 35.Dawson J, Rogers K, Fitzpatrick R, et al. The Oxford shoulder score revisited. Arch Orthop Trauma Surg 2009;129:119–23. 10.1007/s00402-007-0549-7 [DOI] [PubMed] [Google Scholar]
- 36.Murphy RJ, Daines MT, Carr AJ, et al. An independent learning method for orthopaedic surgeons performing shoulder ultrasound to identify full-thickness tears of the rotator cuff. J Bone Joint Surg Am 2013;95:266–72. 10.2106/JBJS.K.00706 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. For information about the Chingford 1000 Women study, email chingford@ndorms.ox.ac.uk.