Abstract
Objectives
The purpose of this systematic review is to explore the effectiveness of the National Health Inequality Strategy, which was conducted in England between 1999 and 2010.
Design
Three databases (Ovid Medline, Embase and PsycINFO) and grey literature were searched for articles published that reported on changes in inequalities in health outcomes in England over the implementation period. Articles published between January 1999 and November 2021 were included. Title and abstracts were screened according to an eligibility criteria. Data were extracted from eligible studies, and risk of bias was assessed using the Risk of Bias in Non-randomized Studies of Interventions tool.
Results
The search strategy identified 10 311 unique studies, which were screened. 42 were reviewed in full text and 11 were included in the final review. Six studies contained data on inequalities of life expectancy or mortality, four on disease-specific mortality, three on infant mortality and three on morbidities. Early government reports suggested that inequalities in life expectancy and infant mortality had increased. However, later publications using more accurate data and more appropriate measures found that absolute and relative inequalities had decreased throughout the strategy period for both measures. Three of four studies found a narrowing of inequalities in all-cause mortality. Absolute inequalities in mortality due to cancer and cardiovascular disease decreased, but relative inequalities increased. There was a lack of change, or widening of inequalities in mental health, self-reported health, health-related quality of life and long-term conditions.
Conclusions
With respect to its aims, the strategy was broadly successful. Policymakers should take courage that progress on health inequalities is achievable with long-term, multiagency, cross-government action.
Trial registration number
This study was registered in PROSPERO (CRD42021285770).
Keywords: public health, health policy, quality in health care
Strengths and limitations of this study.
This is the first study to synthesise all published studies and grey literature on the health inequalities strategy conducted in England from 1999 to 2010.
This study used a broad search strategy of peer-reviewed and grey literature.
The retrospective nature of studies and lack of counterfactual means that causal claims as to the effect of the strategy cannot easily be made. This resulted in an increased risk of bias of studies.
Introduction
The pandemic has exacerbated societal health inequalities, with higher numbers of COVID-19 related cases and deaths in areas of higher socioeconomic disadvantage and among minority ethnic groups.1 2 In England, the COVID-19 mortality rate for those under 65 was 3.7× greater in the most deprived 10% of local areas compared with the least deprived. Age-standardised COVID-19 mortality rates were more than twice as high in the most deprived 10% of areas compared with the least.2
Knowledge of the existence of health inequalities is not new. The first major UK publication describing health inequalities was the Black report in 1980, although health inequalities had been described and debated in the academic literature for decades before that. It was not until 1997, with a newly elected government, that health inequalities became a policy priority. The government commissioned a health inequalities review, subsequently published in 1998 as the Acheson report, and committed itself to implement the evidence-based policy recommendations.3 Subsequently, a wide-ranging national health inequalities strategy was implemented, with various strategies and aims updated over time. This was the first and most extensive international attempt to address health inequalities through a widespread programme of cross-government action.
Two national documents set out the health inequalities strategy. First, ‘Reducing health inequalities: an action report’ was published in 1999 in response to the Acheson report. It described a wide variety of policies designed to reduce health inequalities: both more ‘downstream’ initiatives, such as increased National Health Service (NHS) funding or the establishment of a National Institute for Clinical Excellence, and more ‘upstream’ policies, such as a national minimum wage, the new deal for employment and increased funding for schools, housing and transport.4 Second, ‘Tackling health inequalities: a Program for Action’ was published in 2003.5 It set out 82 cross-departmental commitments, along with 12 headline indicators of the key areas to be monitored. Again, these commitments included a range of ‘upstream’ and ‘downstream’ policies. Other studies have previously summarised the strategy.6–8 The strategy involved a wide range of policy actions across different sectors. These included large increases in levels of public spending on a range of social programmes (such as the introduction of the Child Tax Credit; SureStart Children’s Centres), the introduction of the national minimum wage, area-based interventions such as the Health Action Zones and Neighbourhood Renewal funds and a substantial increase in expenditure on the NHS. The latter was targeted at more deprived neighbourhoods when, after 2001, a ‘health inequalities weighting’ was added to the way in which NHS funds were geographically distributed, so that areas of higher deprivation received more funds per head to reflect higher health need.9
The programme for action included two national targets: (1) by 2010, to reduce by at least 10% the gap in infant mortality between routine and manual groups and the population as a whole and (2) by 2010, to reduce by at least 10% the gap between the fifth of areas with the lowest life expectancy at birth and the population as a whole. The ‘areas with the lowest life expectancy at birth and the population as a whole’ were defined by later documents as the ‘Spearhead areas’.10–12 These 70 local authority areas were identified as being the worst performing local authorities associated with three or more of: male and female life expectancy at birth, cancer and cardiovascular disease mortality rates for the under 75s and Index of Multiple Deprivation (IMD) 2004 scores. These targets were based on relative, rather than absolute, inequalities.12 13 This is important as debate exists as to which of these is the most appropriate measure of inequality.3 14 15 Absolute inequalities measure the numerical gap between groups, while relative inequalities measure the percentage difference between groups.
One major criticism of health inequalities research and policy is that there has been too much effort put into describing the problem, rather than finding solutions. The National Health Inequalities Strategy in England 1999–2010 provides a key international example of the latter. It is a high-profile international case study of long term multifaceted government action. Discussions to date of the effects of the strategy have been polarised, with some prominent commentators arguing that it failed,8 while others have asserted that it was effective.16 17 This is partly because early evaluations of this health inequalities strategy suggested that it had failed to reach its targets and that inequalities may have increased during this period.8 10 16 18 However, subsequent research found that this period was associated with a reduction in health inequalities.6 9 19–21 As governments around the world consider how to respond to inequalities compounded by the pandemic, here we present a systematic review of the studies assessing the effectiveness of this health inequalities strategy.
Methods
This systematic review was conducted in accordance with established methodology22 and reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.23 This systematic review was registered with PROSPERO (CRD42021285770).
Search strategy and selection criteria
Three electronic databases (Ovid Medline, Ovid Embase and Ebsco PsycINFO) were systematically searched from January 1999 to November 2021. The search terms were based in part on previous literature, which identified key search terms to identify studies investigating inequality and inequity24 and the UK.25 Online supplemental table 1 presents the search terms. After removing duplicate records, abstracts and titles were screened according to the eligibility criteria by two researchers (IH and AS) using the software Rayyan by December 2021. Discrepancies were resolved by a third researcher (JAF). Each researcher cross screened 20% of the abstracts and titles of the other to ensure accuracy. Three conflicts arose, which were resolved after discussion. A detailed grey literature search of the UK Government Web Archives, specific websites (such as the King’s Fund) and a broad search using an internet search engine (Google) was used. Relevant citations of included studies were also screened.
bmjopen-2022-063137supp001.pdf (144.9KB, pdf)
Inclusion criteria were:
Studies assessing the impact of the health inequalities strategy in England between 1999 and 2010 on inequality in health outcomes in England.
Any form of quantitative study.
Studies reporting primary research.
Studies in any language.
Exclusion criteria were:
Studies whose methodology make it impossible to draw conclusions about the impact of the strategy.
Studies that reported non-health inequalities.
Earlier editions of included reports.
The full text of all articles screened as meeting the eligibility criteria or possibly meeting the criteria were reviewed. The following information was independently extracted from each study by two authors (IH and AV): first author, year of publication, aim, design, data sources, time period of analysis, population, health inequalities measured, main findings and risk of bias. The main outcomes of interest were absolute or relative changes in socioeconomic inequalities in life expectancy and infant mortality in the population of England between 1999 and 2010 to reflect the aims of the strategy. All results compatible with each outcome domain were sought from each study. Secondary outcomes included changes to socioeconomic inequalities in mortality, comorbidities or self-reported health.
Quality assessment
Risk of bias was assessed at a study level using the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool, which assesses the risk of bias across seven domains. One author (IH) undertook the risk of bias assessment, and this was double checked by a second author (AS or AV) with disagreements resolved by a third (JAF).
Patient and public involvement
Patients were not involved in the design or execution of this study. Nor were members of the public.
Synthesis
Due to the small number of studies with a large amount of data heterogeneity, it was deemed inappropriate to perform a meta-analysis. Instead, studies were synthesised narratively.
Results
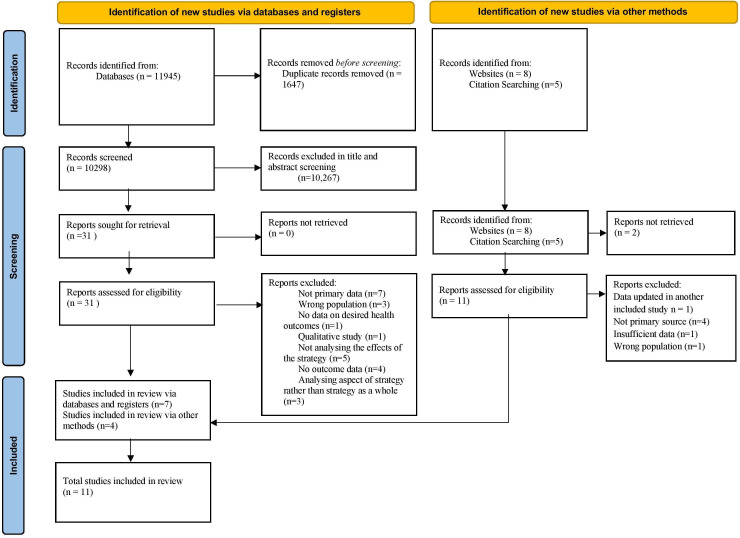
After removal of duplicates, the search identified 10 311 unique records. Forty-two were reviewed in full text, and 11 were included in the final review. A flow diagram of the screening and selection process can be found in figure 1. Six studies contained data on inequalities of life expectancy or mortality,6 7 9 10 12 19 three on disease-specific mortality,10 12 26 three on infant mortality10 13 21 and three on morbidities.7 20 27 Six studies investigated geographical health inequalities, four investigated health inequalities at an individual level and one had statistics from both measures. Measures of socioeconomic status included income, living in a spearhead area, deprivation, occupation, social class and education. Data were collected between 1983 and 2017 (table 1). Results from these papers are summarised in table 2. Table 3 shows the risk of bias of each study across seven domains.
Figure 1.
Study selection process.
Table 1.
Study characteristics
| Inequality measured at an individual or geographical level | Paper | Aim | Study design | Data sources | Time period | Population | Health inequalities measured |
| Geographical | Barr et al (2014)9 | Investigated the change in geographical inequalities in mortality amenable to healthcare and not amenable to healthcare. | Longitudinal ecological study | Mortality data obtained from NHS Information Centre indicator portal. Funds allocated to local commissioning organisations from Department of Health. Income data from indices of multiple deprivation. | 2001–2011 | 324 lower tier authorities in England. | Compared the 20% most deprived and 20% most affluent lower tier authorities. Mortality amenable to healthcare and mortality not amenable to healthcare. |
| Barr et al (2017)6 | To investigate whether the English health inequalities strategy was associated with a decline in geographical health inequalities, compared with trends before and after the strategy. | Time trend analysis | UK data archive and ONS. Income data from indices of multiple deprivation. | 1983–2015 | 324 lower tier authorities in England. | Life expectancy differences between the most deprived local authorities in England and the rest of the country and between spearhead and non-spearhead areas. Mortality rate differences between the most deprived local authorities in England and the rest of the country. Measured changes in inequalities before (1983–2003), during (2004–2012) and after (2013–2015) the times of the strategy’s effects. | |
| Buck and Maguire (2015)19 | Reports the change in the marmot curve for life expectancy between 1999–2003 and 2003–2007. | Repeated cross-sectional | Income data from indices of multiple deprivation. Life expectancy data obtained from ONS. | Compared 1999–2003 and 2003–2007 | Population of England | Life expectancy differences by an middle layer super output area’s deprivation. | |
| Department of Health (2011b)12 | Update of previously published data on inequalities of life expectancy and mortality rates to include latest available data | National report | ONS data | 1995–1997 to 2008–2010 | Population of England | Inequalities of life expectancy, all-cause mortality and death rates due to major causes of death. Inequalities between a range of groups were reported. | |
| Exarchakou et al (2018)26 | Assessed the effectiveness of national cancer policy in reducing socioeconomic inequalities in cancer survival. | Population-based cohort study | ONS national cancer registry database. Income data from index of multiple deprivation. | 1996–2013 | Individuals with a diagnosis of one of the 24 most common cancers. | Absolute difference in 1-year survival between the individuals living in fifth most and fifth least deprived lower layer super output areas. | |
| Robinson et al (2019)21 | Investigated whether the strategy was associated with a reduction in geographical inequalities in infant mortality rates. | Time trend analysis | UK Data Archive, the ONS and the Townsend index of material derivation. | 1983–2017 | All births in England between 1983 and 2017. | Compared the inequality in the infant mortality rate between the 20% most deprived local authorities and the rest of the country before, during and after the strategy. | |
| Individual | Department of Health (2011a)13 | Update of previously published data on inequalities of infant mortality rates to include the latest available 3 year average (2008–2010). | National report | ONS data | 1997–1999 to 2008–2010 | Population of England. | Inequalities of infant mortality between manual groups and the population of England as a whole. |
| Font et al (2011)20 | Estimate changes in health inequalities by calculating concentration indices. | Repeated cross sectional | Health Survey of England | 1997 and 2007 | All people who answered the health survey for England in 1997 (n=7523) and 2007 (n=5329). | Differences of self-reported health, long-standing illness and health limitations in daily activity between people living in spearhead and non-spearhead areas. | |
| Hu et al (2016)7 | Assessed whether changes in trends of self-reported health inequalities observed in England were more favourable than in other countries without such a strategy. | Difference in difference analysis | Health Survey for England. Other nationally representative surveys in Netherlands, Finland and Italy. |
1990, 2000, 2010 | All people who answered nationally representative health surveys in England (n=22 442), Finland (n=14 296), the Netherlands (n=18 353) and Italy (n=2 04 963). | Inequalities of self-assessed health, long-standing health problems and mortality. Education was used as a measure of socioeconomic status. | |
| Maheswaran et al (2015)27 | Examined trends in socioeconomic inequalities in self-reported health throughout the strategy. | Repeated cross-sectional | Health Survey of England. | 1997–2010 | All people who answered a nationally representative survey of health in England between 1997 and 2010 (n=155 311). | Inequalities of mental health (measured by General Health Questionnaire), self-assessed health and health-related quality of life. Investigated inequality based on registrar general’s social classification of occupation. Classification of social class. | |
| Both | Department of Health (2007)10 | To assess the effect of the strategy set out in the 2003 programme for action. | National report | ONS data | 1995–2006 | Population of England | The progress of a large number of inequality outcomes, headline indicators and departmental commitments were assessed. |
ONS, Office for National Statistics.
Table 2.
Study findings
| Inequality measured at an individual or geographical level | Paper | Main findings |
| Geographical | Barr et al (2014)9 |
|
| Barr et al (2017)6 |
|
|
| Buck and Maguire (2015)19 |
|
|
| Department of Health (2011b)12 |
|
|
| Exarchakou et al (2018)26 |
|
|
| Robinson et al (2019)21 |
|
|
| Individual | Department of Health (2011a)13 |
|
| Font et al (2011)20 |
|
|
| Hu et al (2016)7 |
|
|
| Maheswaran et al (2015)27 |
|
|
| Both | Department of Health (2007)10 |
|
Table 3.
Risk of bias – ROBINS-I tool
| Inequality measured at an individual or geographical level | Paper | Bias due to confounding | Bias due to selection of organisations into study | Bias in classification of interventions | Bias due to deviations from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of reported result |
| Geographical | Barr et al (2014)9 | Moderate | Low | Low | Critical | Low | Low | Low |
| Barr et al (2017)6 | Serious | Low | Serious | Critical | Low | Low | Moderate | |
| Buck & Maguire (2015)19 | Low | Low | Low | Critical | Low/ moderate | Low | Low | |
| Department of Health (2011b)12 | Moderate | Low | Low | Critical | Moderate | Low | Low | |
| Exarchakou et al (2018)26 | Low | Low | Low | Critical | NI | Low | Low | |
| Robinson et al (2019)21 | Low | Low | Moderate | Critical | Low | Low | Low | |
| Individual | Department of Health (2011a)13 | Low | Low | Low | Critical | NI | Low | Low |
| Font et al (2011)20 | Serious | Low | Moderate | Critical | Low | Low | Low | |
| Hu et al (2016)7 | Low | Low | Low | Serious | Low | Low | Moderate | |
| Maheswaran et al (2015)27 | Low | Low | Low | Critical | Low | Low | Low | |
| Both | Department of Health (2007)10 | Low | Low | Low | Critical | NI | Low | Low |
NI, No Information; ROBINS-I, Risk of Bias in Non-randomized Studies of Interventions.
Life expectancy, all-cause mortality and disease-specific mortality
Six studies reported data on life expectancy or mortality. Two earlier studies reported a widening of inequalities in life expectancy with one showing narrowing of mortality inequalities. The four more recent studies showed a narrowing of inequalities.
Two early government reports showed widening of life expectancy inequalities and mixed results for mortality inequalities. ‘Tackling Health Inequalities: 2007 Status Report on the Programme for Action’ used Office for National Statistics (ONS) data based on life estimates made using the 2006 census. It compared life expectancy in spearhead areas and the rest of the country. While life expectancy had increased for both spearhead and non-spearhead areas, absolute and relative inequalities between them had increased between 1995–1997 and 2004–2006.10 The second reported ONS data up to and including 2010.12 Compared with the 1995–1997 baseline, the absolute and relative gap in life expectancy between spearhead areas and England as a whole increased by 2008–2010.
Four later published studies found that inequalities had narrowed. The first study by Barr and colleagues9 compared individuals living in the fifth most deprived areas to those living in the fifth least deprived areas. The authors found that inequalities of healthcare amenable mortality, defined as mortality from causes that would be prevented provided appropriate access to high-quality healthcare, narrowed between 2001 and 2011. Absolute inequalities for men and women fell with 85% of the change explained by redistributive resource allocation changes between areas. The relative gap narrowed for males and females. However, the authors found that absolute or relative inequalities of mortality not amenable to healthcare failed to change noticeably between 2001 and 2011.9
The second study by Barr and colleagues6 investigated geographical inequalities between 1983 and 2015 using ONS data based on the 2011 census, rather than 2006, which informed earlier government publications. They analysed trends in the absolute difference of life expectancy and mortality in the 20% most deprived local authorities compared with the rest of England. Supplementary analysis compared life expectancy in spearhead and non-spearhead areas. The authors identified breakpoints to account for the lag between implementation and outcomes. Both socioeconomic inequalities and inequalities between spearhead and non-spearhead areas in life expectancy for men and women statistically significantly increased year-on-year before the strategy and decreased during the time of the strategy, with no evidence that this decrease continued after the strategy. Relative socioeconomic inequalities in mortality fell year-on-year throughout the strategy for both men and women and increased before and after the strategy for men. Further analysis showed that the gap in life expectancy between spearhead areas and the rest of the country did not decrease until after 2005. Relative socioeconomic inequalities in life expectancy widened before and after the strategy period and narrowed during it. The authors found that using population estimates using the 2006 census caused an artificial increase in life expectancy inequalities compared with 2011 estimates.
Hu and colleagues7 compared data from the health survey for England to similar surveys done in other European countries. They investigated trends in inequalities of all-cause mortality between those with high (tertiary) education and the rest of the country. The gap narrowed more significantly in 2000–2010 compared with 1990–2000 in England.
While aforementioned studies, analysing differences between the most and least deprived areas, are important concerning the strategies aims, they fail to describe the change in the social gradient across the whole of the population. Buck and Maguire19 examined the relationship between area-based income deprivation and life expectancy, comparing data from 1999 to 2003 to 2006–2010. The authors found improved life expectancy for all levels of deprivation but a greater improvement in more deprived areas. It was noted that both unemployment and older people’s deprivation played a particularly important role in determining differences in life expectancy between areas.
Three studies reported changes in inequalities in disease-specific mortality. Two government documents examined inequalities in mortality due to cancer between spearhead areas and England as a whole from 1995 to 1997 to 2006–2008 and 2008–2010 using ONS data. By 2006–2008, absolute inequalities fell, without a change in relative inequalities.10 By 2010, the absolute gap had fallen further, with an increase in the relative gap.12 Absolute inequalities in mortality due to circulatory disease decreased by 2006–2008, but relative inequalities widened. By 2008–2010, there was a further decrease in absolute but an increase in relative inequalities. Exarchakou and colleagues26 reported inequalities of 1-year survival rate following a diagnosis of one of the 24 most common cancers between 1996 and 2013. They investigated the absolute difference between individuals living in the fifth most and fifth least deprived areas. The gap narrowed in only 6 of 20 cancers in men and 2 of 21 cancers in women and widened for three cancers (two in women and one in men). One final study examined inequalities in road accident causality in the fifth most deprived local authority districts areas compared with England as a whole.10 The absolute gap decreased between 1998 and 2006.
Infant mortality
Three studies reported changes in the infant mortality rate. Initial reporting using ONS data from 2004 to 2006 found that inequalities had widened between routine plus manual groups and the population as a whole compared with the 1997–1999 baseline.10 A later report found that by 2008–2010, inequalities had narrowed compared with the baseline.13 Robinson and colleagues21 calculated the infant mortality rate in 323 lower tier local authorities between 1983 and 2017 to investigate changes in inequalities between the 20% most deprived areas and the rest of the country. Absolute inequality increased year on year before the strategy and decreased during it. A non-significant increase was seen after the strategy ended. Relative inequalities marginally decreased during the time of the strategy, in contrast to an increase that was seen before and after the strategy period.
Morbidities
Three studies reported on morbidities using Health Survey of England data. Specifically, these studies investigated self-assessed health, health-related quality of life, mental health and long-term health. The Health Survey of England contains data collected from a nationally representative sample of those residing at private residential addresses and has been carried out since 1991.28 Around 8000 adults and 2000 children take part in the survey each year.
Mixed results were found concerning self-reported health. Between 1996 and 2009, the probability of reporting bad or very bad health remained relatively constant for those in the highest social class but increased for those in lower social classes.27 When comparing those with high and low education, there was no significant difference in inequality trends between 2000 and 2010 compared with 1990–2000. Additionally, there was no significant difference in the change of these trends between these periods compared with three European countries.7 Costa Font and colleagues20 measured inequalities in self-reported health using concentration indices, whereby a high result indicates more inequality. Equalised household income was used to measure inequality across the whole population. In contrast to the two aforementioned studies, they reported a fall in the concentration index between 1997 and 2007, indicating a reduction in inequality.
Health-related quality of life did not change between social classes from 1996 to 2008.27 When assessed by a concentration index comparing different household incomes, inequalities of long-term health problems increased between 1997 and 2007.20 There was no significant change in the trend of inequalities of long-term health problems by education in 2000–2010 compared with 1990–2000. Nor was there a significant difference in the change in trend in England compared with three European countries.7 While mental health improved in all social classes between 1997 and 2009, it did so more for individuals in higher social classes.27
Discussion
Principle findings
There is evidence that the strategy met the infant mortality target, while the life expectancy target was reached for men but not women. Absolute health inequalities in life expectancy, mortality, infant mortality and multiple major causes of death reduced. Less evidence is available concerning relative inequalities. More recent data suggest that relative socioeconomic inequalities in life expectancy and infant mortality narrowed. Relative inequalities of mortality narrowed between the fifth most deprived areas and the country as a whole, but not between the fifth most and fifth least deprived areas. The only data available on disease-specific conditions suggest an increase in relative inequalities. This may be due to a lack of newly published studies, using more recent census data and sampling from the later years of the strategy being available as it is for life expectancy and infant mortality. The difference may also be due to the statistical relationship whereby relative inequalities may increase as a result of a fall in absolute inequalities.29 30 There was a lack of change or worsening of change for inequalities in mental health, health-related quality of life and long-term conditions. This lack of change or increased inequality for self-reported health measures may be due to multiple reasons. As all studies used the same survey, with data collected shortly after the 2008 financial crash, perceptions of economic security may have altered results. It may be that self-reported measures are more resilient to change. Alternatively, small changes in categorically assessed self-assessed measures may be less easily observed compared with life expectancy and infant mortality that are continuous measures. Health inequalities were found to have narrowed more consistently when measured between geographical areas rather than between individuals. This may be due to longer follow-up periods in many of the studies that were measured at a geographical level, extending beyond the immediate aftermath of the banking crises. Alternatively, it could have been caused by the redistributive resource allocation changes that occurred between areas.9
Strengths and limitations
This is the first study to collate and synthesise all evidence of the first international attempt at a cross-government strategy to address health inequalities. We used an extensive search strategy with robust screening, data extraction and quality assessment processes. We included peer-reviewed articles and grey literature, including documents published at the time and identified through the UK government archives.
The main limitation is that the studies included are retrospective using either time-trend or before and after methods. All of the studies have a high risk of bias due to deviations from intended interventions. This was predominantly because of the lack of a robust counterfactual that makes it difficult to unpick the impact of the strategy against the impact of other factors, such as broad economic growth before the financial crash in 2008. These limitations are common to any attempt to assess the impact of national policy; however, considering the breadth and ambition of the strategy it is disappointing that more comprehensive evaluations or data are not available. The strategy’s wide-ranging nature does however allow many of these factors to be considered a part of it rather than as a confounding factor. For example, the large decrease in poverty rates, especially in children31 and pensioners,32 may both have contributed. Additionally, not every abstract was double screened. However, 40% of abstracts were cross checked to ensure consistency, and only three discrepancies arose, none of which were included in the review.
The included articles use different measures that make direct comparisons impossible, for example, comparing the most deprived areas to either the least deprived areas or the rest of the population and using individual-level measures of socio-economic status (eg, occupation) or area-based measures (eg, IMD). Morbidity data are based on self-reported measures within a nationally representative survey, rather than chronic disease registers.
As indicated by guidance, absolute and relative inequalities were included.14 33 This aligns with existing guidance and debate both from those who argue that absolute inequalities are the more important measure for policymakers3 and others who support the idea that relative inequalities are also of significant importance.34
What this research means
A lack of progress on health inequalities, despite policy priority, can lead to a sense of fatalism and powerlessness to effect change. These findings are therefore important because they show that with sustained cross-government action, progress on health inequalities is possible. It is particularly encouraging that improvements were made in both of the areas that the strategy predominantly set out to improve: inequalities in life expectancy and infant mortality.
These results are even more encouraging when considering that they came from a strategy that was far from perfect. Critics have noted various points about the strategy, for example, that it was insufficiently based on reliable evidence,8 18 35 36 flawed in delivery,8 16 18 insufficiently focused on the wider determinants of health16 34 37 and that efforts may not have been large enough.8 34 38
Earlier findings consistently showed no improvement in life expectancy inequalities, yet later results were more positive. This may be due to a lag period between the implementation of the strategy of interventions and changes in health outcomes. Certain initiatives would take considerably longer to impact inequalities in life expectancy, such as reducing childhood poverty, compared with more downstream factors, such as blood pressure control. Alternatively, it may be due to more accurate and up-to-date data, such as the 2011 census. Importantly, this shows that sufficient time is needed between implementation and measuring outcomes.
Implications for policy and research
Governments around the world are taking steps to address health inequalities, particularly in light of the growing evidence of an unequal pandemic.39 For example, the UK government has committed to a programme of ‘levelling up’ regional inequalities and setting out new legislation to address health inequalities. This review suggests that it is possible to reduce health inequalities through long-term cross-government action, which was wide reaching both in terms of government departments and across the life course. Most encouragingly with respect to current government aims, geographical health inequalities especially narrowed. The strategy was supported by significant increases in both funding and reform of public services, of which only one has continued. Since the end of the strategy period, public services internationally, but particularly in the UK, have experienced reduced funding as a result of austerity policies from 2010 onwards. In the UK, this has particularly impacted on local authorities, social security, children’s services and, until the pandemic, to the NHS. Indeed, there is evidence that from 2010 onwards (and before the unequal impact of the pandemic) the improvements in health inequalities under the English strategy have reversed with, for example, increasing inequalities in infant mortality rates40 and falling life expectancy in the most deprived areas.41 Considerable investments in these services would be necessary to recreate a proactive attempt to tackle the social determinants of health inequalities.
The strategy used relative measures of inequality. Absolute measures are easier to change, making them appealing to policymakers as progress can be more easily proven. The goals were based on long-term changes in life expectancy and infant mortality rather than shorter term changes in measures such as blood pressure and heart rate. These were appropriate for the strategy given the wide-ranging, cross-departmental approach that aimed to target determinants of ill health. The fact that long-term, ambitious health inequalities targets require a cross-departmental approach can be of benefit to policy makers. They can provide rationale and strengthen the argument for a wide range of potentially transformative policies that may otherwise fail to be enacted due to a lack of political support. Goals were based on changes between the most and least deprived areas, rather than changes in the societal gradient in health. This again would be an easier target for policymakers to achieve. The government’s current targets, through the ‘levelling up’ programme are less ambitious than the strategy’s.42 Only an absolute narrowing in life expectancy and well-being is aimed for, rather than the 10% change targeted by the strategy. Additionally, the absolute gap in life expectancy by area is measured between the top and bottom 10% rather than 20%.
Arguably more policy priority should have been given to reducing the gap in morbidities as the data fail to show a convincing narrowing of inequalities of self-reported health, mental health, health-related quality of life and long-term conditions.
More research is needed to unpick the active ingredients and exact initiatives that were most effective during the strategy. This should start with a more detailed understanding of which diseases drove the reduction in life expectancy and a broader understanding of how the wider determinants of health such as housing, income and education may have impacted changes in infant mortality, mortality and life expectancy.
Conclusion
In summary, this review found some evidence that the 1999–2010 cross-government health inequalities strategy led to a reduction in the absolute inequalities in life expectancy, mortality, infant mortality and major causes of death. While the impact on relative inequalities is less clear, there seemed to be a narrowing of relative inequalities in at least life expectancy and infant mortality. The national targets relating to life expectancy were met for men, but not women, and were achieved for infant mortality. Policymakers should take courage that progress on health inequalities is achievable with long-term, multiagency, cross-government action. These findings are especially pertinent at present times whereby many governments are aiming to use postpandemic recovery as an opportunity to build back better.
Supplementary Material
Footnotes
Twitter: @ilk21
Contributors: JAF conceptualised the study. JAF and IH drafted the protocol, and IK and AV provided comments. IK developed the searches with the support of IH and JAF. IH and AS screened the titles and abstract and were supported by JAF. IH and JF screened the full text articles. IH, AS and AV extracted and checked the extraction. IH wrote the first draft of the manuscript. JAF, IK, CB, AS and AV redrafted. All authors approved the final version. JAF is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Bambra C, Riordan R, Ford J, et al. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;74:jech-2020-214401. 10.1136/jech-2020-214401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suleman M, Sonthalia S, Webb C. Unequal pandemic, fairer recovery: the COVID-19 impact inquiry report. The Health Foundation 2021. [Google Scholar]
- 3.Department of Health . Independent inquiry into inequalities in health (the Acheson report) 1998.
- 4.Department of Health . Reducing health inequalities: an action report 1999.
- 5.Department of Health . Tackling health inequalities: a program for action 2003.
- 6.Barr B, Higgerson J, Whitehead M. Investigating the impact of the English health inequalities strategy: time trend analysis. BMJ 2017;358:j3310. 10.1136/bmj.j3310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu Y, van Lenthe FJ, Judge K, et al. Did the English strategy reduce inequalities in health? A difference-in-difference analysis comparing England with three other European countries. BMC Public Health 2016;16:865. 10.1186/s12889-016-3505-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mackenbach JP. Has the English strategy to reduce health inequalities failed? Soc Sci Med 2010;71:1249–53. 10.1016/j.socscimed.2010.07.014 [DOI] [PubMed] [Google Scholar]
- 9.Barr B, Bambra C, Whitehead M. The impact of NHS resource allocation policy on health inequalities in England 2001-11: longitudinal ecological study. BMJ 2014;348:g3231. 10.1136/bmj.g3231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Department of Health . Tackling health inequalities: 2007 status report of the program for action 2007.
- 11.Department of Health . Tackling health inequalities: 10 years on 2009.
- 12.Department of Health . Mortality monitoring Bulletin. Life expectancy, all-age-all-cause mortality, and mortality from selected causes, overall and inequalities. Update to include data for 2010 2011.
- 13.Department of Health . Mortality monitoring Bulletin (infant mortality inequalities): update to include data for 2010 2011.
- 14.King NB, Harper S, Young ME. Use of relative and absolute effect measures in reporting health inequalities: structured review. BMJ 2012;345:e5774. 10.1136/bmj.e5774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Low A, Low A. Importance of relative measures in policy on health inequalities. BMJ 2006;332:967–9. 10.1136/bmj.332.7547.967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Department of Health . Fair society, healthy lives (the Marmot review) 2010. [DOI] [PubMed]
- 17.Marmot M. Health equity in England: the Marmot review 10 years on. BMJ 2020;368:m693. 10.1136/bmj.m693 [DOI] [PubMed] [Google Scholar]
- 18.Mackenbach JP. Can we reduce health inequalities? An analysis of the English strategy (1997-2010). J Epidemiol Community Health 2011;65:568–75. 10.1136/jech.2010.128280 [DOI] [PubMed] [Google Scholar]
- 19.Buck D, Maguire D. Inequalities in life expectancy: changes over time and implications for policy 2015;76. [Google Scholar]
- 20.Costa Font J, Hernández-Quevedo C, McGuire A. Persistence despite action? Measuring the patterns of health inequality in England (1997-2007). Health Policy 2011;103:149–59. 10.1016/j.healthpol.2011.07.002 [DOI] [PubMed] [Google Scholar]
- 21.Robinson T, Brown H, Norman PD, et al. The impact of new labour's English health inequalities strategy on geographical inequalities in infant mortality: a time-trend analysis. J Epidemiol Community Health 2019;73:564–8. 10.1136/jech-2018-211679 [DOI] [PubMed] [Google Scholar]
- 22.Higgins J, Thomas J, Chandler J. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane 2021. [Google Scholar]
- 23.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prady SL, Uphoff EP, Power M, et al. Development and validation of a search filter to identify equity-focused studies: reducing the number needed to screen. BMC Med Res Methodol 2018;18:106. 10.1186/s12874-018-0567-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ayiku L, Levay P, Hudson T, et al. The medline UK filter: development and validation of a geographic search filter to retrieve research about the UK from OVID medline. Health Info Libr J 2017;34:200–16. 10.1111/hir.12187 [DOI] [PubMed] [Google Scholar]
- 26.Exarchakou A, Rachet B, Belot A, et al. Impact of national cancer policies on cancer survival trends and socioeconomic inequalities in England, 1996-2013: population based study. BMJ 2018;360:k764. 10.1136/bmj.k764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maheswaran H, Kupek E, Petrou S. Self-reported health and socio-economic inequalities in England, 1996-2009: repeated national cross-sectional study. Soc Sci Med 2015;136-137:135–46. 10.1016/j.socscimed.2015.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mindell J, Biddulph JP, Hirani V, et al. Cohort profile: the health survey for England. Int J Epidemiol 2012;41:1585–93. 10.1093/ije/dyr199 [DOI] [PubMed] [Google Scholar]
- 29.Harper S, King NB, Meersman SC, et al. Implicit value judgments in the measurement of health inequalities. Milbank Q 2010;88:4–29. 10.1111/j.1468-0009.2010.00587.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scanlan JP. Guest editorial. Chance 2006;19:47–51. 10.1080/09332480.2006.10722787 [DOI] [Google Scholar]
- 31.Department for Work and Pensions Department for Education . Child poverty in the UK: the report on the 2010 target 2012.
- 32.Office for National Statistics . Chapter 13: inequalities and poverty in retirement. In: Pension trends: compendium, 2014. [Google Scholar]
- 33.Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med 1997;44:757–71. 10.1016/S0277-9536(96)00073-1 [DOI] [PubMed] [Google Scholar]
- 34.Law C, Parkin C, Lewis H. Policies to tackle inequalities in child health: why haven't they worked (better)? Arch Dis Child 2012;97:301–3. 10.1136/archdischild-2011-300827 [DOI] [PubMed] [Google Scholar]
- 35.Bambra C, Smith KE, Garthwaite K, et al. A labour of Sisyphus? Public policy and health inequalities research from the Black and Acheson Reports to the Marmot Review. J Epidemiol Community Health 2011;65:399–406. 10.1136/jech.2010.111195 [DOI] [PubMed] [Google Scholar]
- 36.Macintyre S, Chalmers I, Horton R, et al. Using evidence to inform health policy: case study. BMJ 2001;322:222–5. 10.1136/bmj.322.7280.222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hunter DJ, Popay J, Tannahill C, et al. Getting to grips with health inequalities at last? BMJ 2010;340:c684. 10.1136/bmj.c684 [DOI] [PubMed] [Google Scholar]
- 38.Bambra C. Health divides: where you live can kill you 2016:192–7.
- 39.Bambra C, Lynch J, Smith KE. The unequal pandemic: COVID-19 and health inequalities. Policy Press, 2021. [Google Scholar]
- 40.Taylor-Robinson D, Lai ETC, Wickham S, et al. Assessing the impact of rising child poverty on the unprecedented rise in infant mortality in England, 2000-2017: time trend analysis. BMJ Open 2019;9:e029424. 10.1136/bmjopen-2019-029424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Raleigh VS, Goldblatt P. Life expectancy in England: what’s going on? BMJ 2019. [Google Scholar]
- 42.HM Government . Levelling up the United Kingdom: missions and metrics technical Annex 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-063137supp001.pdf (144.9KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study.