Abstract
Purpose of Review
This is a review of recent literature on the role of indirect calorimetry in surgical nutrition.
Recent Findings
All critical care societal guidelines recommend the use of indirect calorimetry as the standard of care to determine energy needs. Recent studies confirm discrepancy between measured and equation-predicted energy expenditure and further demonstrate improved outcomes with indirect calorimetry-guided nutrition. Patients that undergo ECMO, CRRT and those with COVID-19 would benefit from the use of indirect calorimetry.
Summary
Indirect calorimetry-guided nutrition is the standard of care in mechanically ventilated surgical patients.
Introduction
Nutrition remains a critical mainstay of surgical patients. Overfeeding and underfeeding have clinically significant consequences including prolonged intubation, hyperglycemia, organ failure, other morbidity and increased mortality [1–3]. Direct measurement of energy expenditure is the most accurate method to determine energy needs and indirect calorimetry (IC) enables data-driven and individualized care specific to the patient’s unique requirements. The Society of Critical Care Medicine (SCCM), the American Society for Parenteral and Enteral Nutrition (ASPEN), and the European Society for Clinical Nutrition and Metabolism (ESPEN) all recommend indirect calorimetry to determine energy needs in critical illness, which frequently includes the surgical patient [4, 5]. It is well known that energy prediction equations are inaccurate and this was recently confirmed in the COVID-19 population [6]. Previously indirect calorimetry was expensive and cumbersome to obtain, but with recent advances in technology, measurements are now easier to obtain, more portable, and affordable. Furthermore, changes in the physiologic condition of a patient may require repeat indirect calorimetry measures for accuracy and to optimize care. The aim of this review is to describe how indirect calorimetry is performed, summarize the recent literature, and define the role of indirect calorimetry in surgical patients (Table 1).
Table 1.
Society recommendations regarding energy requirement determination in critically ill patients
| Author | Society | Year | Recommendation |
|---|---|---|---|
| Taylor et al | ASPEN/SCCM | 2016 | We suggest that indirect calorimetry (IC) be used to determine energy requirements, when available and in the absence of variables that affect the accuracy of measurement |
| McClave et al | ESPEN | 2019 | In critically ill mechanically ventilated patients, EE should be determined by using indirect calorimetry |
How Does Indirect Calorimetry Work?
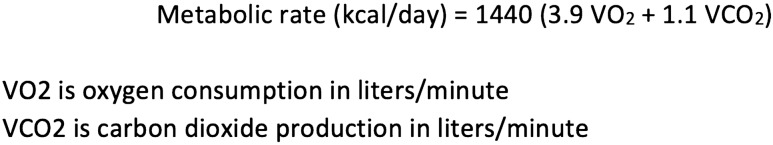
Indirect calorimetry measures carbon dioxide production and oxygen consumption to derive the energy expenditure (EE) of a body [7]. Since heat production corresponds to O2 consumption (VO2) and CO2 production (VCO2), one can use VO2(L/min) and VCO2(L/min) to calculate EE (kcal/day) using the Weir equation [8]. In the spontaneously breathing subject, an artificial chamber using a ventilated hood or face mask is used to collect the inspired and expired gases. In the mechanically ventilated patient, the gases are sampled from the circuit connecting the endotracheal tube to the ventilator. There are two techniques used in mechanically ventilated patients, one uses a breath-by-breath technology and the other uses a mixing chamber. The breath-by-breath machines generate rapid readings (e.g., 3–5 min) and do not require the mixing chamber. Potential benefits of this method include a smaller size and the ability to rapidly detect a change in requirements such as in exercise physiology experiments. The mixing chamber technology requires more space (e.g., 3–5 L) and takes longer to provide results but provides more stable measurements since the mixing chamber physically “averages” the gases prior to analysis, thereby generating more accurate analysis [9]. Older generation calorimetry machines were physically large, required complex and frequent calibration, required a long warm up duration, and were challenging to maintain [10]. In the early 2010s, several academic organizations, including ESPEN and the European Society for Intensive Care Medicine, initiated the development and validation of a new generation of metabolic cart technology with improved accuracy and ease of use compared to prior generations. These calorimeters are applicable to a variety of intensive care unit (ICU) patients beyond the adult critically ill population where indirect calorimetry is recommended.
Gold Standard in ICU Care
Limitations of Predictive Equations
A recent systematic review and meta-analysis showed that indirect calorimetry-guided energy delivery significantly reduced short-term mortality in critically ill patients [11••]. This is thought to be secondary to improved accuracy of assessing nutritional requirements of ICU patients. It is well established that predictive equations for energy consumption are inaccurate [12–15]. These equations to predict resting energy expenditure (REE) were developed in primarily healthy individuals and have been found to be particularly inaccurate in critical illness and organ failure [16, 17]. Some of the equations commonly used in the critically ill patients include Harris–Benedict, Mifflin, Ireton-Jones and Penn State. Predicted REE by the Harris–Benedict equation was well below measured REE during the acute phase in a study of mechanically ventilated septic shock patients [13•]. Similarly, in a study of intracerebral hemorrhage and subarachnoid hemorrhage patients, the predictive equations were inadequate [14]. The largest study to compare measured REE to predictive formulas (Faisy, Fusco, Joliet, Harris–Benedict, Ireton-Jones, Mifflin-St Jeor, Penn State) evaluated 1565 patients with IC measurements and found that predictive equations have low correlation and agreement with IC [18]. In one systematic review, the authors reported that of 160 variations of 13 predictive equations reviewed, 50% either over- or under-estimated the REE by more than 10% at the group level and large discrepancies existed between the predictive equation estimates and IC estimates at both the individual and group level [19].
One multicenter randomized trial reported reduced nosocomial infections when using IC-guided supplemental parenteral nutrition [20]. Berger et al. demonstrated decreased systemic inflammation, increased immunity (decreased serum IL-6, IL-1β, IL-10, and TNF-α by peripheral blood mononuclear cells consistent with decrease infection) and a trend toward decreased muscle mass loss with IC-guided nutrition [21]. In a systematic review and meta-analysis including eight randomized control trials, the authors reported reduced short-term mortality in the IC-guided group and that IC-guidance did not prolong duration of mechanical ventilation, length of stay in the ICU, or hospital length of stay compared to a predictive equations strategy [11••]. This was in contrast to an earlier meta-analysis including only four studies by Tatuca-Babet that showed no between-groups difference in mortality or length of stay, but increased mechanical ventilation days [22]. Likely, the addition of four trials had increased power to detect the effect. The 2016 SCCM/ASPEN and 2018 ESPEN guideline recommends use of IC to determine energy requirements in critically ill, mechanically ventilated patients [5, 23].
Trauma Surgery
Similar to other patient populations, predictive equations are limited in estimating REE of mechanically ventilated surgical-trauma critically ill patients [24]. One study of critically injured trauma patients concluded that continuous IC resulted in better individualized treatment to account for dynamic metabolic changes over time [25] compared to Harris–Benedict which had previously been identified as the most accurate of the predictive equations [24] in trauma patients. In a Canadian study examining the traumatic brain injured (TBI) population, the Penn State equation was particularly inadequate in predicting severe TBI patients, and the authors concluded that TBI, particularly those with severe TBI should be routinely evaluated using IC [26]. One study examined the post-traumatic metabolic response in the trauma intensive care unit and identified four nutrition phenotypes using group-based trajectory modeling (GBTM), with two hyperconsumptive phenotypes at increased risk of malnutrition at discharge [27]. These were only identified using IC.
Liver Transplant Surgery
Patients with end-stage liver disease frequently present with malnutrition. A Korean study reported inaccuracy of predictive equations in liver transplant patients and recommended using IC to avoid over- and underfeeding [28]. Measured REE was significantly associated with age, sex, Model for End-Stage Liver Disease score before liver transplant, surgery time, and graft cold ischemia time on a multiple regression analysis in a cohort of liver transplant patients on postoperative day six [29]. Given these associations along with directly observed inaccuracy using the Harris–Benedict formula, the authors concluded that fixed factors should not be used to determine energy expenditure and that IC should be used for liver transplant patients. One plausible explanation is that hypermetabolism results from increased REE which then decreases after liver transplantation. There is no consensus regarding the metabolic state pre-liver transplant and post-liver transplant and therefore IC is a helpful and essential tool in high-quality nutrition management [30].
Extracorporeal Life Support (ECLS)
ECLS including venovenous (VV) and venoarterial extracorporeal membrane (ECMO) and ventricular assist devices (VAD) provide mechanical pulmonary and cardiovascular support in patients with pulmonary and/or cardiac failure. However, a significant proportion of CO2 is removed across the extracorporeal membrane and thus cannot be identified by the calorimeter as exhaled gas [31]. In a pilot study by Wollersheim et al., conventional IC measurement of the native lung was performed and combined with pre-membrane and post-membrane oxygenator blood gas analysis to calculate total O2 uptake and CO2 elimination to then use the Weir formula to determine total EE, called the Measuring Energy Expenditure in ECLS Patients (MEEP) protocol. They showed 20 patients requiring VV-ECMO for ARDS did not differ significantly in energy expenditure compared to those with ARDS not requiring VV-ECMO and that none of the estimating equations matched the measured energy expenditure [32]. These early results are encouraging but more studies are required before IC can be routinely recommended in the setting of ECLS (Fig. 1).
Fig. 1.
Weir formula relates metabolic rate to oxygen consumption and carbon dioxide production
Continuous Renal Replacement Therapy (CRRT)
In the Metabolic consequences of continuous venovenous hemofiltration on indirect calorimetry (MECCIAS) trial, the authors found that no correction factor of REE was necessary during CRRT [33••]. Carbon dioxide production measured with IC was adapted by adding the CO2 flow of the effluent and deducing CO2 in post-dilution fluid and true REE was calculated using the Weir equation. Since CO2 from the bicarbonate containing dialysate can pass through the filter in various forms, an unknown quantity may be removed in the effluent. There is also the theoretical heat loss during CRRT that would increase metabolism and REE. Finally, dialysate compositions may contribute to caloric uptake [34]. However, despite these considerations, the study found that CRRT led to a minimal change (~ 3%) of measured EE. After careful consideration of theoretical contributing carbon dioxide alterations due to CVVH, the authors found that these are of no clinical importance. Therefore, no correction factor of REE during CVVH is needed and IC should be used during CVVH since CVVH alters metabolism. Of relevance, IC is preferably performed 24 h after the end of a hemodialysis session, as it may take up to 24 h after for the body to restore balance to the pre-dialysis state.
Utilization During COVID-19
During the COVID-19 pandemic, the need for longitudinal IC measurements was apparent to guide nutrition care in a novel disease phenotype. The LEEP-COVID study team demonstrated that this could be performed routinely and safely [35••]. Furthermore, they showed that mREE was between 15 and 20 kcal/kg (for actual body weight in BMI < 30 and adjusted body weight in obese patients) in this population for the first week. Hypermetabolism persisted into the second and third week, contrary to some other ICU populations [36]. Unsurprisingly, predictive equations were found to be inaccurate in the COVID-19 population and frequently overpredicted mREE following the first post-intubation ICU week in the COVID-19 cohort compared to other ICU populations. Similar to other populations, neuromuscular blockade does not appear to affect mREE. The COVID-19 infected mechanically ventilated patients has proven to exhibit a metabolic trajectory poorly predicted by standard predictive equations and therefore IC remains crucial in guiding nutrition in these critically ill patients.
Current Issues and Limitations Using IC in Surgical Patients
While IC is well validated in critically ill patients, it is worth mentioning some of the technical limitations and threats to validity unique to the surgical patient population. IC requires a completely closed respiratory circuit, and therefore patients with an air leak on chest tube pleuro-vacuum device cannot be studied using IC [37]. Unfortunately, mechanically ventilated patients with ARDS and non-compliant lungs may be more prone to this limitation [38]. Furthermore, involuntary movements secondary to seizures or profound agitation may result in inaccurate EE. In a 2013 study, 61% of patients were ineligible for IC secondary to renal replacement therapy (a contra-indication at the time), high PEEP or oxygen requirements, chest tube/drainage system, non-invasive ventilation, hypothermia, agitation, and high-frequency ventilation [10]. Other clinical considerations that could lead to inaccurate results include the use of anesthetic gases in the postoperative period along with sedatives and analgesia administered. Plausible causes of lack of steady state would include increasing or decreasing FiO2 applied along with variable energy delivery via enteral or parenteral nutrition. These are some of the reasons that multiple measurements may be necessary throughout the day to account for these changes in energy expenditure. As mentioned previously, renal replacement therapy may affect the oxygen dynamics and accuracy of IC. In the outpatient setting, measurements must be conducted with strict restrictions including no recent exercise (at least 4 h), no recent meal (5 h of fasting), no recent caffeine or stimulatory nutrition supplements such as ephedra-containing (at least 4 h), no recent nicotine (at least 1 h) and it should be performed in a quiet environment after 10–15 min of rest prior to each measurement [39].
Conclusion
Indirect calorimetry is universally recommended for use in critically ill patients in the ICU by all professional society nutritional and critical care guidelines and remains the gold standard to measure energy expenditure. Predictive equations have repeatedly shown to be inaccurate and can lead to over- and underfeeding with clinically significant consequences. Repeated measures of indirect calorimetry are necessary to account for physiologic changes of the critically ill surgical patient.
Compliance with Ethical Guidelines
Conflict of interest
DDY: Fresnius Kabi—consulting fees to participate on scientific advisory board; Eli Lilly: consulting fees to participate on scientific advisory board; Baxter—consulting fees to participate on scientific advisory board; Takeda Pharmaceuticals—educational grant to fund a fellowship training position, consulting fees to moderate and participate on scientific advisory boards.
Footnotes
This article is part of the Topical collection on Nutrition, Metabolism, and Surgery.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Saskya E. Byerly, Email: sbyerly1@uthsc.edu
D. Dante Yeh, Email: daniel.yeh@dhha.org.
References
Recently published papers of particular interest have been highlighted as: • Of importance •• Of major importance
- 1.Preiser J-C, van Zanten ARH, Berger MM, Biolo G, Casaer MP, Doig GS, et al. Metabolic and nutritional support of critically ill patients: consensus and controversies. Crit Care BioMed Central. 2015;19:1–11. doi: 10.1186/s13054-015-0737-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weijs PJM, Looijaard WGPM, Beishuizen A, Girbes ARJ, Oudemans-van Straaten HM. Early high protein intake is associated with low mortality and energy overfeeding with high mortality in non-septic mechanically ventilated critically ill patients. Crit Care. 2014;18:1–10. doi: 10.1186/s13054-014-0701-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ndahimana D, Kim E-K. Energy requirements in critically ill patients. Clin Nutr Res. Korean Society of Clinical Nutrition; 2018;7:81–90. [DOI] [PMC free article] [PubMed]
- 4.McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, et al. ASPEN Board of Directors; American College of Critical Care Medicine; Society of Critical Care Medicine. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM). JPEN J Parenter Enter Nutr. 2009;33:277–316. [DOI] [PubMed]
- 5.Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38:48–79. doi: 10.1016/j.clnu.2018.08.037. [DOI] [PubMed] [Google Scholar]
- 6.Lakenman PLM, Van der Hoven B, Schuijs JM, Eveleens RD, van Bommel J, Olieman JF, et al. Energy expenditure and feeding practices and tolerance during the acute and late phase of critically ill COVID-19 patients. Clin Nutr ESPEN. 2021;43:383–389. doi: 10.1016/j.clnesp.2021.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frayn KN. Calculation of substrate oxidation rates in vivo from gaseous exchange. J Appl Physiol. 1983;55:628–634. doi: 10.1152/jappl.1983.55.2.628. [DOI] [PubMed] [Google Scholar]
- 8.Weir JBV. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1. doi: 10.1113/jphysiol.1949.sp004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oshima T, Berger MM, De Waele E, Guttormsen AB, Heidegger C-P, Hiesmayr M, et al. Indirect calorimetry in nutritional therapy. A position paper by the ICALIC study group. Clin Nutr. 2017;36:651–662. doi: 10.1016/j.clnu.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 10.De Waele E, Spapen H, Honoré PM, Mattens S, Van Gorp V, Diltoer M, et al. Introducing a new generation indirect calorimeter for estimating energy requirements in adult intensive care unit patients: feasibility, practical considerations, and comparison with a mathematical equation. J Crit Care. 2013;28:884–e1. doi: 10.1016/j.jcrc.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 11.Duan J-Y, Zheng W-H, Zhou H, Xu Y, Huang H-B. Energy delivery guided by indirect calorimetry in critically ill patients: a systematic review and meta-analysis. Crit Care 2021;25:1–10. This recent meta-analysis of eight RCTS compares energy delivery guided by indirect calorimetry vs predictive equations in critically ill patients. They demonstrated indirect calorimetry guided nutrition reduces short-term ICU mortality with no difference in duration of mechanical ventilation, ICU length of stay or hospital length of stay. [DOI] [PMC free article] [PubMed]
- 12.Guttormsen AB, Pichard C. Determining energy requirements in the ICU. Curr Opin Clin Nutr Metab Care. 2014;17:171–6. doi: 10.1097/MCO.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 13.Israfilov E, Kir S. Comparison of energy expenditure in mechanically ventilated septic shock patients in acute and recovery periods via indirect calorimetry. J Parenter Enter Nutr. 2021;45:1523–31. This retrospective study shows increased measured resting energy expenditure (mREE) in septic shock patients. The mREE and equation predicted REE (pREE) were significantly different and did not correlate with mREE higher in the acute phase and pREE was consistently below mREE during the ICU stay. [DOI] [PubMed]
- 14.Smetana KS, Hannawi Y, May CC. Indirect calorimetry measurements compared with guideline weight-based energy calculations in critically ill stroke patients. J Parenter Enter Nutr. 2021;45:1484–90. doi: 10.1002/jpen.2035. [DOI] [PubMed] [Google Scholar]
- 15.Fraipont V, Preiser J-C. Energy estimation and measurement in critically ill patients. JPEN J Parenter Enteral Nutr. 2013;37:705–13. doi: 10.1177/0148607113505868. [DOI] [PubMed] [Google Scholar]
- 16.Ahmad A, Duerksen DR, Munroe S, Bistrian BR. An evaluation of resting energy expenditure in hospitalized, severely underweight patients. Nutrition. 1999;15:384–8. doi: 10.1016/S0899-9007(99)00068-4. [DOI] [PubMed] [Google Scholar]
- 17.Frankenfield DC, Coleman A, Alam S, Cooney RN. Analysis of estimation methods for resting metabolic rate in critically ill adults. J Parenter Enter Nutr. 2009;33:27–36. doi: 10.1177/0148607108322399. [DOI] [PubMed] [Google Scholar]
- 18.Zusman O, Kagan I, Bendavid I, Theilla M, Cohen J, Singer P. Predictive equations versus measured energy expenditure by indirect calorimetry: a retrospective validation. Clin Nutr. 2019;38:1206–10. doi: 10.1016/j.clnu.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 19.Tatucu-Babet OA, Ridley EJ, Tierney AC. Prevalence of underprescription or overprescription of energy needs in critically ill mechanically ventilated adults as determined by indirect calorimetry: a systematic literature review. J Parenter Enter Nutr. 2016;40:212–25. doi: 10.1177/0148607114567898. [DOI] [PubMed] [Google Scholar]
- 20.Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, et al. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet (London, England) 2013;381:385–93. doi: 10.1016/S0140-6736(12)61351-8. [DOI] [PubMed] [Google Scholar]
- 21.Berger MM, Pantet O, Jacquelin-Ravel N, Charrière M, Schmidt S, Becce F, et al. Supplemental parenteral nutrition improves immunity with unchanged carbohydrate and protein metabolism in critically ill patients: the SPN2 randomized tracer study. Clin Nutr. 2019;38:2408–16. doi: 10.1016/j.clnu.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 22.Tatucu-Babet OA, Fetterplace K, Lambell K, Miller E, Deane AM, Ridley EJ. Is energy delivery guided by indirect calorimetry associated with improved clinical outcomes in critically ill patients? A systematic review and meta-analysis. Nutr Metab Insights. 2020;13:1178638820903295. doi: 10.1177/1178638820903295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN) J Parenter Enteral Nutr. (JPEN) 2016;40:159–211. doi: 10.1177/0148607115621863. [DOI] [PubMed] [Google Scholar]
- 24.Kamel AY, Robayo L, Liang D, Rosenthal MD, Croft CA, Gabriela G, et al. Estimated versus measured energy expenditure in ventilated surgical-trauma critically Ill patients. J Parenter Enter Nutr. 2021;46(6):1431–1440. doi: 10.1002/jpen.2314. [DOI] [PubMed] [Google Scholar]
- 25.Vasileiou G, Mulder MB, Qian S, Iyengar R, Gass LM, Parks J, et al. Continuous Indirect Calorimetry in Critically Injured Patients Reveals Significant Daily Variability and Delayed, Sustained Hypermetabolism. JPEN J Parenter Enteral Nutr. 2020;44:889–94. doi: 10.1002/jpen.1713. [DOI] [PubMed] [Google Scholar]
- 26.Wu S, Iqbal S, Giroux M, Alam N, Campisi J, Razek T, et al. Penn State equation versus indirect calorimetry for nutritional assessment in patients with traumatic brain injury. Can J Surg. 2022;65:E320–5. doi: 10.1503/cjs.022420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Byerly S, Vasileiou G, Qian S, Mantero A, Lee EE, Parks J, et al. Early hypermetabolism is uncommon in trauma intensive care unit patients. J Parenter Enter Nutr. 2020 doi: 10.1002/jpen.1945. [DOI] [PubMed] [Google Scholar]
- 28.Lee SJ, Lee H-J, Jung Y-J, Han M, Lee S-G, Hong S-K. Comparison of measured energy expenditure using indirect calorimetry vs predictive equations for liver transplant recipients. JPEN J Parenter Enteral Nutr. 2021;45:761–7. doi: 10.1002/jpen.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lindqvist C, Nordstedt P, Nowak G, Slinde F, Majeed A, Bottai M, et al. Energy expenditure early after liver transplantation: better measured than predicted. Nutrition. 2020;79–80:110817. doi: 10.1016/j.nut.2020.110817. [DOI] [PubMed] [Google Scholar]
- 30.Santos BC, Correia MITD, Anastácio LR. Energy expenditure and liver transplantation: what we know and where we are. JPEN J Parenter Enteral Nutr. 2021;45:456–64. doi: 10.1002/jpen.1985. [DOI] [PubMed] [Google Scholar]
- 31.Stoppe C, Nesterova E, Elke G. Nutritional support in patients with extracorporeal life support and ventricular assist devices. Curr Opin Crit Care LWW. 2018;24:269–76. doi: 10.1097/MCC.0000000000000512. [DOI] [PubMed] [Google Scholar]
- 32.Wollersheim T, Frank S, Müller MC, Skrypnikov V, Carbon NM, Pickerodt PA, et al. Measuring Energy Expenditure in extracorporeal lung support Patients (MEEP)–Protocol, feasibility and pilot trial. Clin Nutr. 2018;37:301–7. doi: 10.1016/j.clnu.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 33.Jonckheer J, Demol J, Lanckmans K, Malbrain MLNG, Spapen H, De Waele E. MECCIAS trial: Metabolic consequences of continuous veno-venous hemofiltration on indirect calorimetry. Clin Nutr. England; 2020;39:3797–803. Prior to the MECCIAS study, continueous renal replacement therapy precluded the use of indirect calorimetry. This study demonstrated that carbon dioxide alterations secondary to CRRT are insignificant therefore no correction factor of REE is needed. Since CVVH alters metabolism, indirect calorimetry should be performed during CVVH. [DOI] [PubMed]
- 34.Ostermann M, Lumlertgul N, Mehta R. Nutritional assessment and support during continuous renal replacement therapy. Semin Dial. 2021;34(6):449–56. doi: 10.1111/sdi.12973. [DOI] [PubMed] [Google Scholar]
- 35.Whittle J, Molinger J, MacLeod D, Haines K, Wischmeyer PE. Persistent hypermetabolism and longitudinal energy expenditure in critically ill patients with COVID-19. Crit Care. 2020;24:581. This study is the first to show a unique metabolic response in COVID-19 mechanically ventilated patients with normometabolism in the first week and hypermetabolism in the 2nd and 3rd week of the ICU admission. This study demonstrates the importance of indirect calorimetry as predictive equations are inaccurate in this population. [DOI] [PMC free article] [PubMed]
- 36.Uehara M, Plank LD, Hill GL. Components of energy expenditure in patients with severe sepsis and major trauma: a basis for clinical care. Crit Care Med. 1999;27:1295–302. doi: 10.1097/00003246-199907000-00015. [DOI] [PubMed] [Google Scholar]
- 37.AARC Clinical Practice guideline. Metabolic measurement using indirect calorimetry during mechanical ventilation—2004 revision & update. Respir Care. 2004;49:1073–9. [PubMed]
- 38.El-Orbany M, Salem MR. Endotracheal tube cuff leaks: causes, consequences, and management. Anesth Analg LWW. 2013;117:428–34. doi: 10.1213/ANE.0b013e318292ee21. [DOI] [PubMed] [Google Scholar]
- 39.Haugen HA, Chan L, Li F. Indirect calorimetry: a practical guide for clinicians. Nutr Clin Pract. 2007;22:377–88. doi: 10.1177/0115426507022004377. [DOI] [PubMed] [Google Scholar]