Abstract
The length of stay in the hospital for COVID-19 can aid in understanding the disease's prognosis. Thus, the goal of this study was to collectively estimate the hospital length of stay (LoS) in COVID-19 hospitalized individuals. To locate related studies, international databases (including Google Scholar, Science Direct, PubMed, and Scopus) were searched. The I2 index, the Cochran Q test, and T2 were used to analyze study heterogeneity. The mean LoS in COVID- 19 hospitalized patients was estimated using a random-effects model. COVID-19's total pooled estimated hospital LoS was 15.35, 95%CI:13.47-17.23; p<0.001, I2 = 80.0). South America had the highest pooled estimated hospital LoS of COVID-19 among the continents, at 20.85 (95%CI: 14.80-26.91; p<0.001, I2 = 0.01), whereas Africa had the lowest at 8.56 8 (95%CI: 1.00-22.76). The >60 age group had the highest pooled estimated COVID-19 hospital LoS of 16.60 (95%CI: 12.94-20.25; p<0.001, I2 = 82.6), while the 40 age group had the lowest hospital LoS of 10.15 (95% CI: 4.90-15.39, p<0.001, I2 = 22.1). The metanalysis revealed that COVID-19's hospital LoS was more than 10 days. However, it appears that this duration varies depending on a number of factors, including the patient's age and the availability of resources.
Key words: COVID-19, length of stay, hospital
Introduction
In late 2019, in Wuhan, China, a novel coronavirus of severe acute respiratory syndrome (coronavirus 2; SARS-CoV-2) caused a disease called COVID [1]. On January 30, 2020, the World Health Organization announced this situation as a public health emergency. At the date of December 1, 2020, more than 1.45 million deaths had occurred worldwide [2]. This disease creates serious challenges to the health system. The demand for hospital beds, intensive care beds, and mechanical ventilators is one of the challenges facing the health system [3-6].
The rapid spread of COVID-19 led to severe shortages of hospital beds. To plan a response, hospital and public health officials need to understand how many people in their area are likely to require hospitalization for COVID-19 [7]. The COVID-19 pandemic overburdens the intensive care units with the influx of critically ill patients and challenges the health systems’ capacity to respond to the need [8]. In Winnipeg, Manitoba, critical care was severely challenged during the initial peak of the influenza A (H1N1) virus pandemic in June 2009, as intensive care units (ICUs) were at full capacity [9]. Since the shortage of ICU beds may engender a trade-off between saving the life of one patient over another, the ability to timely forecast the impact of the epidemic on ICU bed capacity usage is a critical component of adequate outbreak management [10].
The study by Jamshidi et al. compared the length of hospital stay during the COVID-19 pandemic in the USA, Italy, and Germany, the length of hospitalization for the fatal cases in the USA, Italy, and Germany are 2-10, 1-6, and 5-19 days, respectively. Overall, this length in the USA is 2 days more than that in Italy and 5 days less than in Germany [11].
Understanding how long COVID-19 patients require healthcare in hospitals is important for predicting bed demand and planning resource allocation, particularly in resource constraint settings [12]. Because of the pathogen COVID-19, the characteristics of the disease vary at different times and places [13,14]. Therefore, following these changes, it is essential to update our findings to better manage this disease. Thus, this study was aimed to estimate the hospital length of stay of COVID-19 patients.
Methods
Search strategy
We performed this study according to PRISMA guidelines. To identify all studies that reported hospital length of stay in COVID-19 hospitalized patients, a comprehensive search of several electronic databases, including PubMed, Scopus, and Web of Science, was performed on January 29, 2021. The search term comprised the following keywords: “length of stay”,” Stay Length”,” Hospital Stay”, “Admission duration”, “Admission length”,” COVID 19”, “COVID-19”, “2019-ncov”, “2019 ncov”, “sars cov 2”, “sars-cov 2”, “Coronavirus”, “hospital”.
The following inclusion criteria were selected for meta-analysis: the study subjects were adults (≥18 years old) infected with COVID-19 and hospitalized, the primary outcome was mean or median hospital length of stay or ICU length of stay, and finally, studies were included in which the study population was not limited to a specific group of chronic patients. Furthermore, the exclusion criteria were articles that include a letter to the editor, case reports and case series, review, and meta-analysis.
Study selection and data extraction
Titles and abstracts of all studies were screened to identify those that met the inclusion criteria. We send all of the related articles to Endnote X8 software. Afterward, we removed the duplicate articles. The remaining articles were reviewed in three steps. In the first step, we reviewed the title of the article and then the abstract, and finally, the article’s full texts were evaluated. Full-texts were assessed for studies that were difficult to screen with titles and abstracts only. Two authors screened the final full texts, and each study was decided after reading the full texts of all potentially eligible articles. In cases of disagreement, a third review author was consulted.
The extracted data included: the first author’s last name, publication year, country, sample size, mean age or age range, gender, mean or median hospital length of stay, IQRs, mean or median ICU length of stay (LoS), and standard deviations. Data extraction was done by the same two review authors who conducted the study selection independently.
The assessment of methodological quality and risk of bias
The Newcastle-Ottawa Scale was applied to evaluate the quality of selected studies [15]. The NOS consists of three domains. These domains include the selection of study groups, comparability of groups, and description of exposure and outcome. This scale, including eight items and star scores, assesses the quality of each study in each domain. The total score of each of the articles was calculated. Study quality was rated on a scale from one star, very poor, to 10 stars, high quality. Studies are rated as high (7-10), medium (5-6), or low quality (<4). Two review authors completed quality assessments independently. A third review author was involved in cases of disagreement.
Statistical analysis
Cochran’s Q test assessed heterogeneity in the CRF of COVID-19 between different studies with a significance level of p<0.1 and I2 statistic with values >75% [13]. The random-effects meta-analysis model was used to estimate pooled CFR because of high heterogeneity (I2 =99.7% and Cochran’s Q (p<0.001). The univariate meta-regression model was used to assess the effect of sample size on the heterogeneity of pooled CFR. Publication bias was assessed by Beggs and Eggers tests. Data were analyzed by STATA v 11 (StataCorp, College Station, TX, USA).
Results
Description of included studies
In the current systematic review and meta-analysis, 126 records with 428,977 cases estimated hospital length of stay, were included. These studies were from different continents.
A total of 4,745 records were retrieved through an electronic databases search, and 3,425 possibly relevant articles were identified after removing 1,320 articles due to duplication and irrelevance for the review purpose. In the second step, 2,655 articles were excluded after the title and abstract screeded for the inclusion and exclusion criteria. The remaining 644 articles were excluded due to lack of relevant information, or they were not original articles. Finally, 126 articles that reported hospital length of stay of COVID-19 were included in the final analysis (Figure 1; Table 1).
The mean (SD) of hospital LoS among all records was 14.49 (7.92); also, the median and interquartile range (IQR) of reported hospital LoS were 13.00 (17.8-9). The minimum and maximum reported hospital LOS was 3.5 and 53.8, respectively. The overall pooled estimated hospital LoS of COVID-19 was 15.35, 95% CI:13.47-17.23; p<0.001, I2 = 80.0). The highest pooled estimated Hospital LOS of COVID-19 among the different continents was estimated in South America at 20.85 (95%CI: 14.80-26.91; p<0.001, I2 = 0.01), while in hospitalized patients in Africa was 8.56 (95% CI: 1.00-22.76).
Table 1.
Description of included studies in the current meta-analysis.
| First author | Year | Country | Study design | Sample size | Age group* | Sex | Mean hospital LoS | LCL | UCL | Se | Continent° | NOS score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Al Sulaiman et al. [16] | 2021 | Saudi Arabia | Cohort | 560 | 1 | Both genders | 17/00 | -6/19 | 40/19 | 11/83 | 5 | 7 |
| 2 | Rosenthal et al. [17] | 2021 | China | Cohort | 721 | 3 | Both genders | 9/89 | -16/42 | 36/20 | 13/43 | 5 | 7 |
| 3 | Anudeep et al. [18] | 2020 | India | Cohort | 50 | 2 | Both genders | 6/00 | -0/93 | 12/93 | 3/54 | 5 | 6 |
| 4 | Zarzosa et al. [19] | 2021 | Spain | Cohort | 67 | 1 | Both genders | 14/10 | 6/08 | 22/12 | 4/09 | 2 | 7 |
| 5 | Cai et al. [20] | 2020 | China | Cohort | 149 | 3 | Both genders | 16/80 | 4/84 | 28/76 | 6/10 | 1 | 7 |
| 6 | Chen et al. [21] | 2020 | China | Case cohort | 114 | 1 | Both genders | 19/56 | 9/10 | 30/02 | 5/34 | 1 | 6 |
| 7 | Creel-Bulos et al. [22] | 2020 | Georgia | Cohort | 115 | 1 | Females | 19/00 | 8/49 | 29/51 | 5/36 | 3 | 8 |
| 8 | Daher et al. [23] | 2021 | Germany | Cohort | 18 | 1 | Females | 44/00 | 39/84 | 48/16 | 2/12 | 2 | 8 |
| 9 | Davoudi et al. [24] | 2021 | Iran | Cross-sectional | 153 | 4 | Both genders | 6/30 | -5/82 | 18/42 | 6/18 | 5 | 6 |
| 10 | Deeb et al. [25] | 2021 | UAE | Cohort | 1075 | 2 | Both genders | 6/20 | -25/93 | 38/33 | 16/39 | 5 | 5 |
| 11 | Demir et al. [26] | 2021 | Turkey | Retrospective cohort | 227 | 3 | Both genders | 3/88 | -10/89 | 18/65 | 7/53 | 5 | 7 |
| 12 | Diaz De Teran et al. [27] | 2021 | Spain/Italy | Cohort | 162 | 1 | Males | 17/00 | 4/53 | 29/47 | 6/36 | 2 | 7 |
| 13 | Seon et al. [28] | 2021 | Korea | Cohort | 7969 | Both genders | 26/70 | -60/78 | 114/18 | 44/63 | 1 | 6 | |
| 14 | Xiaofang et al. [29] | 2021 | China | Cohort | 75 | Both genders | 16/10 | 7/61 | 24/59 | 4/33 | 1 | 7 | |
| 15 | Fei et al. [30] | 2021 | USA | Cohort | 50 | 1 | Both genders | 11/64 | 4/71 | 18/57 | 3/54 | 3 | 8 |
| 16 | Xie et al. [31] | 2020 | USA | Cohort | 3641 | 1 | Both genders | 10/00 | -49/13 | 69/13 | 30/17 | 3 | 7 |
| 17 | Abbasi et al. [32] | 2021 | Iran | Cross-sectional | 37 | 2 | Both genders | 22/37 | 16/41 | 28/33 | 3/04 | 5 | 8 |
| 18 | Alshukry et al. [33] | 2020 | Kuwait | Cohort | 417 | 3 | Both genders | 20/69 | 0/68 | 40/70 | 10/21 | 5 | 5 |
| 19 | Cabanillas et al. [34] | 2020 | Spain | Cohort | 329 | 2 | Both genders | 7/85 | -9/93 | 25/63 | 9/07 | 2 | 6 |
| 20 | Capuzzi et al. [35] | 2021 | Italy | Cross-sectional | 151 | 1 | Both genders | 16/10 | 4/06 | 28/14 | 6/14 | 2 | 6 |
| 21 | Conlon et al. [36] | 2021 | USA | Cohort | 27201 | 3 | Both genders | 10/00 | 151/63 | 171/63 | 82/46 | 3 | 7 |
| 22 | Ersöz et al. [37] | 2021 | Turkey | Cohort | 310 | 2 | Both genders | 15/87 | -1/38 | 33/12 | 8/80 | 5 | 8 |
| 23 | Gharebaghi et al. [38] | 2021 | Iran | Cross-sectional | 215 | 2 | Both genders | 4/91 | -9/46 | 19/28 | 7/33 | 5 | 6 |
| 24 | Ipekci et al. [39] | 2020 | Turkey | Cohort | 51 | 2 | Both genders | 10/49 | 3/49 | 17/49 | 3/57 | 5 | 7 |
| 25 | Lenka et al. [40] | 2020 | USA | Cohort | 32 | 1 | Both genders | 14/80 | 9/26 | 20/34 | 2/83 | 3 | 6 |
| 26 | Liu et al. [41] | 2021 | China | Cohort | 178 | 3 | Both genders | 32/40 | 19/33 | 45/47 | 6/67 | 1 | 7 |
| 27 | Lu et al. [42] | 2020 | China | Cohort | 28 | 2 | Both genders | 14/96 | 9/77 | 20/15 | 2/65 | 1 | 7 |
| 28 | Li et al. [43] | 2020 | China | Cohort | 54 | 1 | Both genders | 21/40 | 14/20 | 28/60 | 3/67 | 1 | 7 |
| 28.1 | Li et al. [43] | 2020 | China | Cohort | 54 | 1 | Both genders | 29/30 | 22/10 | 36/50 | 3/67 | 1 | 7 |
| 29 | Li et al. [44] | 2021 | China | Cohort | 57 | 2 | Both genders | 11/20 | 3/80 | 18/60 | 3/77 | 1 | 8 |
| 30 | Omrani-Nava et al. [45] | 2020 | Iran | Case-Control | 279 | 2 | Both genders | 6/00 | 10/37 | 22/37 | 8/35 | 5 | 7 |
| 31 | Payandemehr et al. [46] | 2020 | Iran | RCT | 20 | 2 | Both genders | 6/75 | 2/37 | 11/13 | 2/24 | 5 | 8 |
| 32 | Saying et al. [47] | 2021 | Turkey | Cohort | 349 | 2 | Both genders | 9/70 | -8/61 | 28/01 | 9/34 | 5 | 8 |
| 33 | Velayos et al. [48] | 2020 | Spain | Cohort | 66 | 4 | Both genders | 5/60 | -2/36 | 13/56 | 4/06 | 2 | 7 |
| 34 | Wu et al. [49] | 2020 | China | Cohort | 6055 | 1 | Both genders | 3/90 | 72/36 | 80/16 | 38/91 | 1 | 7 |
| 35 | Yasin et al. [50] | 2021 | Egypt | Cohort | 210 | 3 | Both genders | 8/56 | -5/64 | 22/76 | 7/25 | 6 | 7 |
| 36 | Yuan, et al. [51] | 2020 | China | Cohort | 94 | 3 | Both genders | 14/28 | 4/78 | 23/78 | 4/85 | 1 | 6 |
| 37 | Zhan, et al. [52] | 2021 | China | Cohort | 476 | 1 | Both genders | 27/76 | 6/38 | 49/14 | 10/91 | 1 | 6 |
| 38 | Tan et al. [53] | 2021 | China | Cohort | 227 | 2 | Both genders | 22/40 | 4/52 | 40/28 | 9/12 | 1 | 6 |
| 38.1 | Tan et al. [53] | 2021 | China | Cohort | 15 | 2 | Both genders | 27/33 | 24/49 | 30/17 | 1/45 | 1 | 7 |
| 38.2 | Tan et al. [53] | 2021 | China | Cohort | 8 | 2 | Both genders | 14/50 | 7/18 | 21/82 | 3/74 | 1 | 6 |
| 38.3 | Tan et al. [53] | 2021 | China | Cohort | 14 | 2 | Both genders | 22/29 | 18/47 | 26/11 | 1/95 | 1 | 7 |
| 38.4 | Tan et al. [53] | 2021 | China | Cohort | 19 | 2 | Both genders | 13/42 | 11/54 | 15/30 | 0/96 | 1 | 8 |
| 39 | Jiang et al. [54] | 2020 | China | Cohort | 131 | 2 | Both genders | 16/60 | 5/38 | 27/82 | 5/72 | 1 | 7 |
| 40 | M et al. [55] | 2020 | China | Cohort | 72 | 1 | Both genders | 19/50 | 11/18 | 27/82 | 4/24 | 1 | 8 |
| 41 | Mallow et al. [56] | 2020 | USA | Cohort | 21,676 | 1 | Both genders | 8/90 | 135/38 | 153/18 | 73/61 | 3 | 7 |
| 42 | de Moura et al. [57] | 2020 | Brazil | Cohort | 400 | 2 | Both genders | 14/15 | -5/45 | 33/75 | 10 | 4 | 7 |
| 43 | Gupta et al. [58] | 2020 | India | Cohort | 200 | 3 | Both genders | 11/17 | -2/69 | 25/03 | 7/07 | 5 | 7 |
| 44 | Özyılmaz et al. [59] | 2020 | Turkey | Cohort | 105 | 3 | Both genders | 11/12 | 1/08 | 21/16 | 5/12 | 5 | 7 |
| 45 | Parry et al. [60] | 2020 | India | Cohort | 61 | 3 | Both genders | 18/46 | 10/81 | 26/11 | 3/91 | 5 | 8 |
| 46 | Rahim et al. [61] | 2020 | Pakistan | Cross-sectional | 204 | 2 | Both genders | 6/20 | -7/80 | 20/20 | 7/14 | 5 | 8 |
| 47 | Rosenthal et al. [62] | 2020 | USA | Cohort | 35,302 | 1 | Both genders | 7/74 | -176/39 | 191/87 | 93/94 | 3 | 6 |
| 48 | Sardiña-González et al. [63] | 2020 | Spain | Cohort | 18 | 1 | Both genders | 9/40 | 5/24 | 13/56 | 2/12 | 2 | 6 |
| 49 | Shi et al. [64] | 2020 | China | Cohort | 184 | 3 | Both genders | 17/30 | 4/01 | 30/59 | 6/78 | 1 | 6 |
| 50 | Sun et al. [65] | 2020 | China | Cohort | 217 | 3 | Both genders | 17/90 | 3/46 | 32/34 | 7/37 | 1 | 7 |
| 51 | Teich et al. [66] | 2020 | Brazil | Cohort | 510 | 4 | Both genders | 9/00 | -13/13 | 31/13 | 11/29 | 4 | 7 |
| 52 | Turcotte et al. [67] | 2020 | USA | Cohort | 117 | 1 | Both genders | 11/80 | 1/20 | 22/40 | 5/41 | 3 | 6 |
| 53 | UlHaq et al. [68] | 2020 | Pakistan | Cohort | 179 | 3 | Both genders | 8/20 | -4/91 | 21/31 | 6/69 | 5 | 7 |
| 54 | Abi Fadel et al. 69] | 2020 | USA | Cross-sectional | 495 | 1 | Both genders | 13/90 | -7/90 | 35/70 | 11/12 | 3 | 6 |
| 55 | Erturk et al. [70] | 2020 | Turkey | Cohort | 262 | 2 | Both genders | 8/34 | -7/52 | 24/20 | 8/09 | 5 | 7 |
| 56 | Vernaz-Hegi et al. [71] | 2020 | Switzerland | Cohort | 840 | 1 | Both genders | 10/38 | -18/02 | 38/78 | 14/49 | 2 | 6 |
| 57 | Wagner et al. [72] | 2020 | USA | Cohort | 99 | 2 | Both genders | 32/61 | 22/86 | 42/36 | 4/97 | 3 | 6 |
| 58 | Wu et al. [73] | 2020 | China | Cross-sectional | 80 | 3 | Both genders | 8/00 | -0/77 | 16/77 | 4/47 | 1 | 7 |
| 59 | Wu et al. [8] | 2020 | China | Cohort | 58 | 2 | Both genders | 10/30 | 2/84 | 17/76 | 3/81 | 1 | 7 |
| 60 | Xie et al. [74] | 2020 | China | Case-control | 25 | 2 | Both genders | 21/20 | 16/30 | 26/10 | 2/50 | 1 | 7 |
| 61 | Yuan et al. [75] | 2020 | Switzerland | Cohort | 94 | 3 | Both genders | 14/28 | 4/78 | 23/78 | 4/85 | 2 | 7 |
| 62 | Zhang et al. [76] | 2020 | china | Cohort | 420 | 2 | Both genders | 17/80 | -2/28 | 37/88 | 10/25 | 1 | 8 |
| 63 | Egol et al. [77] | 2020 | USA | Cohort | 17 | 1 | Both genders | 9/80 | 5/76 | 13/84 | 2/06 | 3 | 7 |
| 64 | Del Giorno et al. [78] | 2020 | Switzerland | Cohort | 90 | 1 | Both genders | 16/40 | 7/10 | 25/70 | 4/74 | 2 | 8 |
| 65 | Cengiz et al. [79] | 2020 | Turkey | Cohort | 30 | 2 | Both genders | 10/40 | 5/03 | 15/77 | 2/74 | 5 | 8 |
| 66 | Ayaz et al. [80] | 2020 | Pakistan | Cohort | 66 | 2 | Both genders | 8/30 | 0/34 | 16/26 | 4/06 | 5 | 8 |
| 67 | Battaglini et al. [81] | 2020 | Italy | Cohort | 94 | 1 | Both genders | 28/10 | 18/60 | 37/60 | 4/85 | 2 | 7 |
| 68 | Ar Bhuyan et al. [82] | 2020 | Bangladesh | Cohort | 33 | 4 | Both genders | 14/50 | 8/87 | 20/13 | 2/87 | 5 | 6 |
| 69 | Agrupis et al. [83] | 2021 | Philippines | Cohort | 500 | 3 | Both genders | 12/00 | -9/91 | 33/91 | 11/18 | 1 | 6 |
| 70 | Almas et al. [84] | 2021 | Pakistan | Cohort | 699 | 2 | Both genders | 7/26 | -18/65 | 33/17 | 13/22 | 5 | 8 |
| 71 | Arslan et al. [85] | 2021 | Turkey | Cohort | 413 | 2 | Both genders | 9/30 | -10/62 | 29/22 | 10/16 | 5 | 7 |
| 72 | Banwait et al. [86] | 2021 | USA | Cohort | 2726 | 1 | Both genders | 9/53 | -41/64 | 60/70 | 26/11 | 3 | 9 |
| 73 | Beatty et al. [87] | 2021 | Ireland | Cohort | 575 | Both genders | 17/70 | -5/80 | 41/20 | 11/99 | 2 | 7 | |
| 74 | Dagher et al. [88] | 2021 | USA | Cohort | 310 | 1 | Both genders | 6/14 | -11/11 | 23/39 | 8/80 | 3 | 7 |
| 75 | Ersöz et al. [89] | 2021 | Turkey | Cross-sectional | 310 | 2 | Both genders | 15/87 | -1/38 | 33/12 | 8/80 | 5 | 7 |
| 76 | Zhan et al. [90] | 2021 | China | Cohort | 180 | Both genders | 18/60 | 5/45 | 31/75 | 6/71 | 1 | 8 | |
| 77 | Yoon et al. [91] | 2021 | USA | Cohort | 13 | 2 | Both genders | 9/00 | 5/47 | 12/53 | 1/80 | 3 | 6 |
| 78 | Yesilkaya et al. [92] | 2021 | Turkey | Cohort | 10 | 1 | Both genders | 14/50 | 11/40 | 17/60 | 1/58 | 5 | 6 |
| 79 | Yeates et al. [93] | 2021 | USA | Cross-sectional | 110,223 | Both genders | 12/10 | -313/26 | 337/46 | 166/00 | 3 | 7 | |
| 80 | Xiong et al. [94] | 2021 | China | Cohort | 75 | 2 | Both genders | 21/05 | 12/56 | 29/54 | 4/33 | 1 | 5 |
| 81 | Vranis et al. [95] | 2021 | USA | Cohort | 39 | 2 | Both genders | 20/90 | 14/78 | 27/02 | 3/12 | 3 | 7 |
| 82 | Villamañán et al. [96] | 2021 | Spain | Cross-sectional | 327 | 1 | Both genders | 13/20 | -4/52 | 30/92 | 9/04 | 2 | 7 |
| 83 | Varela Rodríguez et al. [97] | 2021 | Spain | Cohort | 188 | 1 | Both genders | 5/00 | -8/44 | 18/44 | 6/86 | 2 | 7 |
| 84 | Ferry et al. [98] | 2021 | Australia | Cohort | 223 | 3 | Both genders | 3/50 | -11/13 | 18/13 | 7/47 | 1 | 7 |
| 85 | Valverde-López et al. [99] | 2021 | Spain | Cohort | 178 | 1 | Both genders | 8/10 | -4/97 | 21/17 | 6/67 | 2 | 7 |
| 86 | Spoldi et al. [100] | 2021 | Italy | Cross-sectional | 63 | 1 | Both genders | 12/00 | 4/22 | 19/78 | 3/97 | 2 | 8 |
| 87 | Soares et al. [101] | 2021 | Brazil | Cross-sectional | 46 | 2 | Both genders | 22/70 | 16/05 | 29/35 | 3/39 | 4 | 7 |
| 88 | Sikkema et al. [102] | 2021 | Netherlands | Cohort | 382 | 1 | Both genders | 22/50 | 3/35 | 41/65 | 9/77 | 2 | 7 |
| 89 | Rubio-Gracia et al. [103] | 2021 | Spain | Cohort | 130 | 2 | Both genders | 8/00 | -3/17 | 19/17 | 5/70 | 2 | 6 |
| 90 | Di Fusco et al. [104] | 2021 | USA | Cohort | 173,942 | 1 | Both genders | 8/30 | -400/42 | 417/02 | 208/53 | 3 | 6 |
| 91 | Ronan et al. [105] | 2021 | Ireland | Case-control | 19 | Both genders | 6/08 | 1/81 | 10/35 | 2/18 | 2 | 5 | |
| 92 | Rojas-Marte et al. [106] | 2021 | USA | Cohort | 398 | 1 | Both genders | 19/10 | -0/45 | 38/65 | 9/97 | 3 | 6 |
| 93 | Ramos et al. [107] | 2021 | Spain | Cohort | 936 | 1 | Both genders | 17/30 | -12/68 | 47/28 | 15/30 | 2 | 7 |
| 94 | Aghajani et al. [108] | 2021 | Iran | Cohort | 991 | 1 | Both genders | 6/00 | -24/85 | 36/85 | 15/74 | 5 | 6 |
| 95 | Groah et al. [109] | 2021 | USA | Cohort | 82 | 2 | Both genders | 16/40 | 7/53 | 25/27 | 4/53 | 3 | 7 |
| 96 | Oliveira et al. [110] | 2021 | USA | Cohort | 98 | 1 | Both genders | 8/30 | -1/40 | 18/00 | 4/95 | 3 | 7 |
| 97 | Martínez-Urbistondoet al.[111] | 2021 | Spain | Cohort | 165 | 1 | Both genders | 14/00 | 1/41 | 26/59 | 6/42 | 2 | 7 |
| 98 | Marmarchi et al. [112] | 2021 | USA | Cohort | 288 | 1 | Both genders | 18/00 | 1/37 | 34/63 | 8/49 | 3 | 7 |
| 99 | He et al. [113] | 2021 | China | Cross-sectional | 2702 | 2 | Both genders | 17/88 | -33/06 | 68/82 | 25/99 | 1 | 8 |
| 100 | Yousef et al. [114] | 2021 | India | Cohort | 57 | 1 | Both genders | 10/54 | 3/14 | 17/94 | 3/77 | 5 | 7 |
| 101 | Majeed et al. [115] | 2021 | Pakistan | Cohort | 75 | 2 | Both genders | 11/40 | 2/91 | 19/89 | 4/33 | 5 | 7 |
| 102 | Mader et al. [116] | 2021 | Germany | Cohort | 50 | 2 | Both genders | 17/22 | 10/29 | 24/15 | 3/54 | 2 | 8 |
| 103 | Ahlström et al. [117] | 2021 | Sweden | Cohort | 9905 | 1 | Both genders | 10/50 | -87/03 | 108/03 | 49/76 | 2 | 8 |
| 104 | Al Sulaiman et al. [16] | 2021 | Saudi Arabia | Cohort | 560 | 1 | Both genders | 10/00 | -13/19 | 33/19 | 11/83 | 5 | 7 |
| 105 | Alamdari et al. [118] | 2020 | Iran | Cohort | 83 | 1 | Both genders | 11/00 | 2/07 | 19/93 | 4/56 | 5 | 8 |
| 106 | Aldhaeefi et al. [119] | 2021 | USA | Cohort | 315 | 1 | Both genders | 12/00 | -5/39 | 29/39 | 8/87 | 3 | 6 |
| 107 | Andrade et al. [120] | 2021 | USA | Case control | 189 | 1 | Male | 7/00 | -6/47 | 20/47 | 6/87 | 3 | 7 |
| 108 | Bonnet et al. [121] | 2021 | France | Case-control | 138 | 2 | Both genders | 12/50 | 0/99 | 24/01 | 5/87 | 2 | 8 |
| 109 | Bozan et al. [122] | 2021 | Turkey | Cohort | 263 | 1 | Both genders | 12/60 | -3/29 | 28/49 | 8/11 | 5 | 7 |
| 110 | Breik et al. [123] | 2020 | USA | Cohort | 164 | 2 | Both genders | 12/00 | -0/55 | 24/55 | 6/40 | 3 | 7 |
| 111 | Cai et al. [124] | 2020 | China | Cohort | 149 | 1 | Both genders | 16/18 | 4/22 | 28/14 | 6/10 | 1 | 7 |
| 112 | Creel-Bulo et al. [22] | 2020 | Georgia | Cohort | 115 | 2 | Both genders | 19/00 | 8/49 | 29/51 | 5/36 | 2 | 7 |
| 113 | Jaiswal et al. [125] | 2021 | United Arab Emirates | Cohort | 14 | 2 | Both genders | 35/64 | 31/97 | 39/31 | 1/87 | 5 | 7 |
| 114 | Zhang et al. [126] | 2021 | China | Cohort | 420 | 2 | Both genders | 17/80 | -2/28 | 37/88 | 10/25 | 1 | 6 |
| 115 | Charoenngam et al. [127] | 2021 | USA | Cohort | 1427 | 1 | Both genders | 8/10 | -28/92 | 45/12 | 18/89 | 3 | 8 |
| 116 | Xu et al. [128] | 2020 | New York | Cohort | 101 | 2 | Both genders | 13/00 | 3/15 | 22/85 | 5/02 | 3 | 7 |
| 117 | Sarpong et al. [129] | 2021 | USA | Cohort | 405 | 2 | Both genders | 8/90 | -10/82 | 28/62 | 10/06 | 3 | 7 |
| 118 | Özçelik Korkmaz et al. [130] | 2021 | Turkey | Cohort | 116 | 1 | Both genders | 14/36 | 0/01 | 28/00 | 5/39 | 5 | 9 |
| 119 | Hittesdorf et al. [131] | 2021 | USA | Cohort | 116 | 1 | Both genders | 53/80 | 43/25 | 64/35 | 5/39 | 3 | 7 |
| 120 | Diez-Quevedo et al. [132] | 2021 | Spain | Cohort | 2150 | 2 | Both genders | 14/00 | -31/44 | 59/44 | 23/18 | 2 | 9 |
| 121 | Forsblom et al. [133] | 2021 | Finland | Cohort | 585 | Both genders | 10/00 | -13/70 | 33/70 | 12/09 | 2 | 9 |
*Age group: 1 = <40, 2= 40-50, 3 = 50-60, 4 = >60; °Continent: 1 = East Asia, 2= Europe, 3 = North America, 4 = South America, 5 = West Asia, 6 = Africa.
In the comparison of different age groups, the highest pooled estimated LOS in COVID-19 was seen in the >60 years old 16.60 (95%CI: 12.94-20.25; p<0.001, I2 = 82.6), and the lowest hospital LOS was seen in the <40 age groups 10.15 (95% CI: 4.90-15.39, p<0.001, I2 = 22.1). then 200 cases) was higher than the studies with more than 200 understudies cases (16.28 vs 11.94 days) (Table2).
Meta-regression
To identify the cause of different factors on heterogeneity among studies, the variables like sample size, the mean age of participants, study year, and the continent was assessed. The effect of the year of study (p=0.21), age of participants (p=0.13), and sample size (p=0.71), on heterogeneity among studies was not statistically significant; but the continent had a significant effect on heterogeneity among studies (p=0.001) (Table3).
Figure 1.
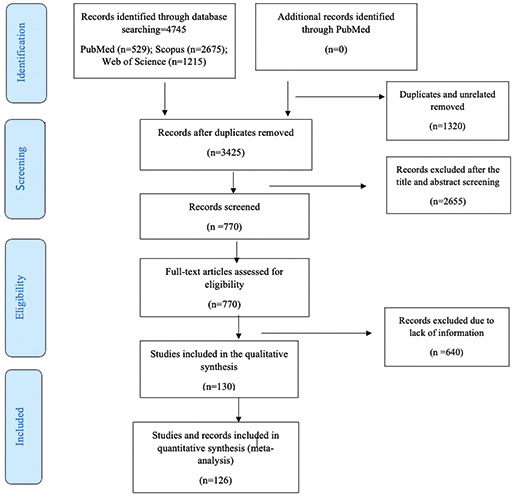
PRISMA flow diagram for included studies in the current meta-analysis.
Publication bias
According to the results of Begg’s and Egger’s test, there was no evidence of publication bias (0.31, 0.51) about the understudied subject (Figure 2).
Discussion
Understanding the influence of COVID-19 on hospital capacity requires precise estimation of total LoS, which may then be used to predict bed demand. Given the complexity and partiality of numerous data sources, as well as the quickly evolving nature of the COVID-19 pandemic, multiple analysis approaches on many datasets, such as meta-analysis studies, are most suited [134].
In this meta-analysis study, the mean hospital LoS among all records was 14.49, and the median of reported hospital LoS was 13. The study’s principal findings include that the majority of research on hospital length of stay among COVID-19 patients were conducted in West Asia. The African area recorded the fewest studies. Our findings demonstrated a considerable effect of study heterogeneity. South America had the highest pooled hospital LoS of COVID-19, whereas hospitalized patients in Africa had the lowest one. This could be due to excellent hospital quality data in America and little or no hospitalization data in Africa. Furthermore, because COVID-19 death rates are higher in Africa, most hospitalized patients die earlier and have a shorter hospital stay. Those over the age of 60 had the highest pooled estimated hospital LoS of COVID-19. It should come as no surprise that elderly patients had a longer hospital stay. As a result, our study backs up prior findings in the literature [135,136]. This could also be attributed to their weakened immune systems and behavioral reactions to the measures implemented. Simultaneously, diabetes or other chronic illnesses in older individuals complicate infection management and lengthen hospital stay [137].
The first formal review on LoS for COVID-19 was conducted on 52 research, 46 of which were from China. The researches showed that the median hospital LoS in China was 14 days, compared to 5 days outside of China. Because only five research recorded LoS outside of China, this comparison is fairly ambigu ous. Patients with COVID-19 appeared to be hospitalized for longer in China than elsewhere. This could be explained by changes in admission and discharge criteria among nations, as well as disparities in pandemic timing [138]. The majority of the surveys included in this evaluation focused on the small number of subjects hospitalized during the first month of the outbreak and did not take censoring into account [139]. Our research was more extensive, with publications from East Asia, Europe, North America, South America, and West Asia included. As a result, our estimate is more accurate because we included all publications from various countries in our research.
Figure 2.
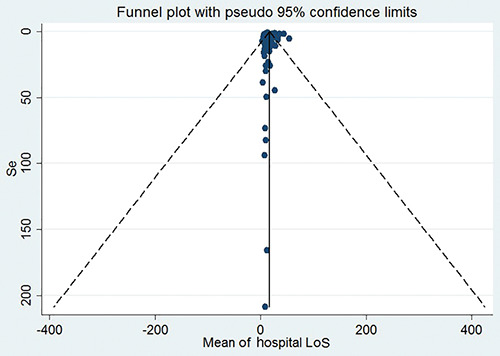
The funnel plot to assess the presence of publication bias.
Table 2.
Pooled estimation of the hospital length of stay for coronavirus disease 2019 according to different variables
| Group | Number of records | Pooled estimation (%) | 95% CI | Q | I2 (%) |
|---|---|---|---|---|---|
| Continent | |||||
| East Asia | 33 | 18.41 | 15.70-21.12 | p<0.001 | 71.4 |
| Europe | 24 | 15.31 | 9.03 – 21.59 | p<0.001 | 89.4 |
| North America | 27 | 15.78 | 11.45 – 20.11 | p<0.001 | 71.3 |
| South America | 3 | 20.85 | 14.80-26.91 | p<0.001 | 0.01 |
| West Asia | 34 | 11.93 | 8.26-15.60 | p<0.001 | 80.8 |
| Africa | 1 | 8.56 | 1.00-22.76 | - | - |
| Unknown | 4 | 13.67 | 5.96-21.38 | p<0.001 | 43.8 |
| Age group | |||||
| >60 | 50 | 16.60 | 12.94-20.25 | p<0.001 | 82.6 |
| 50-60 | 19 | 15.12 | 12.30-17.94 | p<0.001 | 27.9 |
| 40-50 | 46 | 14.67 | 11.15-18.18 | p<0.001 | 84.0 |
| <40 | 4 | 10.15 | 4.90-15.39 | p<0.001 | 22.1 |
| Unknown | 7 | 12.38 | 6.86-17.91 | p<0.001 | 28.7 |
| Sample size | |||||
| Less than 200 | 73 | 16.28 | 14.03-18.52 | p<0.001 | 88.0 |
| More than 200 | 53 | 11.94 | 9.01-14.88 | p<0.001 | 0.0 |
| Overall | 126 | 15.35 | 13.47-17.23 | p<0.001 | 80.0 |
Table 3.
The meta-regression results to identify the cause of different factors on heterogeneity among studies.
| Variable | Coefficient | SE | p |
|---|---|---|---|
| Sample size | -0.02 | 0.007 | 0.71 |
| Study year | 2.16 | 1.74 | 0.21 |
| Age | -1.68 | 1.10 | 0.13 |
| Continent | -1.46 | 1.77 | 0.001 |
In Oksuz et al.’s cohort study in Turkey on 1,056 patients, 55% were men, and 45% were women. The mean age was 56.6 years. The mean length of stay was 9.1 days. The mean length of stay was 8.0 days for patients hospitalized inwards versus 14.8 days for patients hospitalized in the ICU. During the first months of the COVID-19 pandemic, physicians tended to hospitalize the patients for close monitoring regardless of severity. However, that practice changed over time, and later only patients with higher disease severity, lower oxygen saturation, comorbid conditions, and evidence of chest CT were hospitalized. Therefore, this change in treatment approach may have resulted in a lower number of inpatients in the months following the first peak and higher hospital costs among hospitalized patients [140]. In the study by Fadel et al., 495 patients were admitted for severe COVID-19 infection. The mean age was 67.3 years. Most patients (54.9%) were Caucasian, and 192 (38.3%) were African American. Mean ICU and hospital LoS values were 7.4 and 13.9 days, respectively [69].
Contrary to our study, one study in France has shown that fewer older patients were admitted to the ICU. They found that the length of stay in the hospital was highly variable, depending on age and wards (ICU or not). ICU stays were longer in the young patients compared to other pulmonary diseases requiring intensive care [139]. Probably the reason for the shorter hospital stay in old age is the higher mortality at these ages. In addition, their study had little censoring (5%).
Remdesivir is a 5-day treatment and can only be administered during an inpatient stay. Hospital stays that would otherwise be 5– 8 days could be shortened with remdesivir therapy but by fewer than 4 days. Patients who would otherwise be discharged in fewer than 5 days could not experience any reduction in LoS and might have their hospital stay prolonged to complete their treatment course. A peak in discharge rates upon completion of therapy suggests that physicians delayed discharge to complete treatment [141]. In a case series, 174 confirmed COVID-19 adult patients hospitalized were included. The median age was 45.5 years, and 91 patients (52.3%) were male. The median duration of hospitalization was 4 days (0-28 days) [134]. The difference between the results of this study and other studies is because of the higher number of men in the study population. In Chiam et al.’s study, six hundred and eighty-seven patients with a mean age of 60.94 were included in the investigation. Analysis showed that patients’ age, sex, ethnicity, number of Exhauster comorbidities, and number of weeks since the pandemic were significantly associated with LoS. The median LoS was 12.34 days and 5.72 days for ICU and non- ICU patients, respectively. This study, like ours, shows an association between older age with longer hospital LoS [142].
Limitations
The current study has some limitations, including the continents’ difference. Different factors, such as disease prognosis, comorbidities, resource availability, available beds, and so on, can complicate hospital LoS. However, we lack the necessary data in this review to adjust the influence of the aforementioned parameters. In addition, the hospital LoS was reported based on discharge status; those who died had a shorter hospital stay than those who were discharged alive. Furthermore, COVID-19 hospital stays are affected by county-specific factors such as admission criteria and the date of the pandemic. Patients with COVID-19 disease who have comorbidities like hypertension or diabetes are more prone to acquire a more severe course and progression of the disease.
Furthermore, elderly patients, particularly those 65 and older with comorbidities and infections, have a higher rate of admission to the critical care unit (ICU). The most common comorbidities among COVID-19 patients were hypertension, diabetes, and cardiopathy, and they were hospitalized for a longer period of time. Comorbidity is one of the key causes for the varying lengths of hospitalization in different studies, and the average length of hospital stay is reported to be longer depending on the number of patients studied.
Additionally, willingness to pay may influence hospital duration of stay in different countries or continents based on resource availability. Willingness to pay is associated with mortality/morbidity risk reductions by incorporating several highly relevant aspects during an epidemic, namely, healthcare capacity constraints, dynamic aspects of prevention (i.e., interventions aimed at flattening the epidemic curve), and distributional issues due to high heterogeneity in the underlying risks. In countries with abundant resources, patients are more eager to pay for hospital treatments, therefore hospital equipment is sufficient to keep patients in the hospital until they are fully recovered, and hospital lengths of stay are indeed longer. While in low-resource countries, in an epidemic situation where the number of patients is increasing, hospitals may be forced to discharge patients earlier than usual due to a lack of equipment such as ventilators, intensive care equipment, and adequate hospital beds, and thus the average hospital length of stay may be reduced.
These are the most important factors influencing the hospital length of stay of COVID-19 patients in various nations, and they should be considered in the results and interpretations.
Conclusions
The mean hospital LoS across all records was 14.49 days, with 13 days as the median recorded hospital LoS. In our analysis, the continent had a substantial effect on study heterogeneity. South America had the highest pooled hospital LoS of COVID-19, whereas hospitalized patients in Africa had the lowest one. It should be noted that hospital LoS of COVID-19 patients can be influenced by other factors such as disease prognosis, comorbidities, availability, and accessibility to health services, so this disparity between continents can be muddled by various factors such as major comorbidities, different treatment protocols, different care protocols, availability of resources, available beds, and so on.
Acknowledgments
We would like to thank the authors of the studies included in this meta-analysis; we are also deeply grateful to all the authors who kindly provided the additional information for our meta-analysis.
References
- 1.World Health Organization. Origin of SARS-CoV-2. 2020. Available from: https://apps.who.int/iris/bitstream/handle/10665/332197/WHO-2019-nCoV-FAQVirus_origin-2020.1-eng.pdf [Google Scholar]
- 2.Bramer CA, Kimmins LM, Swanson R, Kuo J, Vranesich P, Jacques-Carroll LA, et al. Decline in child vaccination coverage during the COVID-19 pandemic - Michigan Care Improvement Registry, May 2016-May 2020. Am J Transplant 2020;20:1930-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emanuel JE, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020;382:2049-55. [DOI] [PubMed] [Google Scholar]
- 4.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020;323:1545-6. [DOI] [PubMed] [Google Scholar]
- 5.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet 2020;395:1225-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Truog RD, Mitchell C, Daley GQ. The toughest triage—allocating ventilators in a pandemic. N Engl J Med 2020;382: 1973-5. [DOI] [PubMed] [Google Scholar]
- 7.Ferstad JO, Gu A, Lee RY, Thapa I, Shin AY, Salomon JA, et al. A model to forecast regional demand for COVID-19 related hospital beds. medRxiv 2020.03.26.20044842. [Google Scholar]
- 8.Wu S, Xue L, Legido-Quigley H, Khan M, Wu H, Peng X, et al. Understanding factors influencing the length of hospital stay among non-severe COVID-19 patients: A retrospective cohort study in a Fangcang shelter hospital. PloS One 2020;15:e0240959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shoukat A, Wells CR, Langley JM, Singer BH, Galvani AP, Moghadas SM. Projecting demand for critical care beds during COVID-19 outbreaks in Canada. CMAJ 2020;192:E489-E96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gitto S, Di Mauro C, Ancarani A, Mancuso P. Forecasting national and regional level intensive care unit bed demand during COVID-19: The case of Italy. PloS One 2021;16: e0247726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jamshidi B, Jamshidi Zargaran S, Bekrizadeh H, Rezaei M, Najafi F. Comparing length of hospital stay during COVID- 19 pandemic in the USA, Italy and Germany. Int J Qual Health Care 2021;33:mzab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang X, Wu C, Li X, Song Y, Yao X, Wu X, et al. On the origin and continuing evolution of SARS-CoV-2. Nat Sci Rev 2020;7:1012-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu XW, Wu XX, Jiang XG, Xu KJ, Ying LJ, Ma CL, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ 2020;368:m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2011. Available from: https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp [Google Scholar]
- 16.Al Sulaiman KA, Aljuhani O, Eljaaly K, Alharbi AA, Al Shabasy AM, Alsaeedi AS, et al. Clinical features and outcomes of critically ill patients with coronavirus disease 2019 (COVID-19): A multicenter cohort study. Int J Infec Dis 2021;105:180-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenthal JA, Awan SF, Fintzi J, Keswani A, Ein D. Asthma is associated with increased risk of intubation but not hospitalization or death in coronavirus disease 2019. Ann Allergy Asthma Immunol 2021;126:93-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anudeep A, Somu C, Kumar JS. Clinical profile and outcomes of critically ill covid-19 patients admitted in a tertiary care hospital. Ann Trop Med Public Health 2020;23. [Google Scholar]
- 19.Zarzosa SG, Lucas JH, Llorente B, Trascasa M, Molina R, Serrano C, et al. Acute renal failure in COVID-19 patients on mechanical ventilation. Rev Chil Anest 2021;49:867-73. [Google Scholar]
- 20.Cai Y, Liu J, Yang H, Wang M, Guo Q, Huang D, et al. Association between incubation period and clinical characteristics of patients with COVID-19. J Int Med Res 2020;48:300060520956834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen Q, Kong H, Qi X, Ding W, Ji N, Wu C, et al. Carcinoembryonic antigen: A potential biomarker to evaluate the severity and prognosis of COVID-19. Front Med (Lausanne) 2020; 7:579543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Creel-Bulos C, Liu M, Auld SC, Gaddh M, Kempton CL, Sharifpour M, et al. Trends and diagnostic value of D-dimer levels in patients hospitalized with coronavirus disease 2019. Medicine (Baltimore) 2020;99:e23186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daher A, Cornelissen C, Hartmann NU, Balfanz P, Müller A, Bergs I, et al. Six months follow-up of patients with invasive mechanical ventilation due to COVID-19 related ARDS. Int J Environ Res Public Health 2021;18:5861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davoudi A, Najafi N, Aarabi M, Tayebi A, Nikaeen R, Izadyar H, et al. Lack of association between vitamin D insufficiency and clinical outcomes of patients with COVID- 19 infection. BMC Infect Dis 2021;21:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deeb A, Khawaja K, Sakrani N, Alakhras A, Al Mesabi A, Trehan R, et al. Impact of ethnicity and underlying comorbidity on COVID-19 inhospital mortality: An observational study in Abu Dhabi, UAE. Biomed Res Int 2021;2021:6695707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Demir M, Demir F, Aygun H. Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease. J MedVirol 2021;93:2992-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Diaz De Teran T, Gonzales Martinez M, Banfi P, Garuti G, Ferraioli G, Russo G, et al. management of patients with severe acute respiratory failure due to SARS-CoV-2 pneumonia with noninvasive ventilatory support outside Intensive Care Unit. Minerva Medica 2021;112:329-37. [DOI] [PubMed] [Google Scholar]
- 28.Seon JY, Jeon WH, Bae SC, Eun BL, Choung JT, Oh IH. Characteristics in pediatric patients with coronavirus disease 2019 in Korea. J Korean Med Sci 2021;36:e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xiaofang G, Chunxia M, Yujie M, Xiaoqi W, Jianhua W, Tao F, et al. [Clinical efficacy and safety of different antiviral regimens in patients with coronavirus disease 2019].[Article in Chinese]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2021;32:1423-7. [DOI] [PubMed] [Google Scholar]
- 30.Fei F, Smith JA, Cao L. Clinical laboratory characteristics in patients with suspected COVID-19: One single-institution experience. J MedVirol 2021;93:1665-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xie Y, Bowe B, Maddukuri G, Al-Aly Z. Comparative evaluation of clinical manifestations and risk of death in patients admitted to hospital with covid-19 and seasonal influenza: cohort study. BMJ 2020;371:m4677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abbasi S, Naderi Z, Amra B, Atapour A, Dadkhahi SA, Eslami MJ, et al. Hemoperfusion in patients with severe COVID-19 respiratory failure, lifesaving or not? J Res Med Sci 2021;26:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alshukry A, Ali H, Ali Y, Al-Taweel T, Abu-Farha M, AbuBaker J, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) patients in Kuwait. PloS One 2020;15:e0242768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cabanillas R, Terrones-Huaman CI, Soto-Caceres VA, Diaz- Velez C. Characteristics of clinic discharge patients with SARS-Cov-2 hospitalized at EsSalud in the Lambayeque Region. Rev Cuerpo Med Hosp Nac Almanzor Aguinaga Asenjo 2020;13:395-402. [Google Scholar]
- 35.Capuzzi E, Caldiroli A, Leo S, Buoli M, Clerici M. Initiation of psychotropic medication in hospitalized patients with COVID-19: Association with clinical and biological characteristics. Hum Psychopharmacol 2021;36:e2789.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Conlon A, Ashur C, Washer L, Eagle KA, Bowman MAH. Impact of the influenza vaccine on COVID-19 infection rates and severity. Am J Infect Control 2021;49:694-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ersöz A, Yılmaz TE. The association between micronutrient and hemogram values and prognostic factors in COVID-19 patients: A single-center experience from Turkey. Int J Clin Pract 2021;75:e14078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gharebaghi N, Farshid S, Boroofeh B, Nejadrahim R, Mousavi J, Dindarian S, et al. Evaluation of epidemiology, clinical features, prognosis, diagnosis and treatment outcomes of patients with COVID-19 in West Azerbaijan Province. Int J Clin Pract 2021;75:e14108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ipekci A, Akdeniz YS, Tutar O, Sirolu S, Simsek O, Ozkan S. The clinical and computed tomography findings of patients with COVID-19. Signa Vitae 2020;16:173-8. [Google Scholar]
- 40.Lenka J, Chhabria MS, Sharma N, Tan BEX Boppana LKT, Venugopal S, et al. Clinical characteristics and outcomes of critically ill patients with COVID-19 in a tertiary community hospital in upstate New York. J Community Hosp Intern Med Perspect 2020;10:491-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu S, Yuan HC, Zhang B, Li W, You JJ, Liu J, et al. Comparison of clinical features and CT temporal changes between familial clusters and non-familial patients with COVID-19 pneumonia. Front Med (Lausanne) 2021;8: 630802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lu RF, Qin JR, Wu Y, Wang J, Huang SY, Tian LJ, et al. Epidemiological and clinical characteristics of COVID-19 patients in Nantong, China. J Infect Dev Ctries 2020;14:440-6. [DOI] [PubMed] [Google Scholar]
- 43.Li YL, Hu YB, Yu JY, Ma TG. Retrospective analysis of laboratory testing in 54 patients with severe- or critical-type 2019 novel coronavirus pneumonia. Lab Investig 2020;100:794-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li BB, Bao CM. Disparity in clinical characteristics between 2019 novel coronavirus pneumonia and leptospirosis. Open Med (Wars) 2021;16:494-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Omrani-Nava V, Maleki I, Ahmadi A, Moosazadeh M, Hedayatizadeh-Omran A, Roozbeh F, et al. Evaluation of hepatic enzymes changes and association with prognosis in COVID-19 patients. Hepat Mon 2020;20:e103179. [Google Scholar]
- 46.Payandemehr P, Azhdarzadeh M, Bahrami-Motlagh H, Hadadi A, Najmeddin F, Shahmirzaei S, et al. Interferon beta- 1a as a candidate for COVID-19 treatment; An open label single-arm clinical trial. Front Emerg Med 2020;4:e51. [Google Scholar]
- 47.Sayiner A, Tasbakan MS, Ergan B, Kilinc O, Sayiner A, Sertoz R, et al. Clinical outcome of PCR-negative COVID- 19 patients: A retrospective study. Turk Thorac J 2021;22:247-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Velayos M, Munoz-Serrano AJ, Estefania-Fernandez K, Caldas MCS, Lapena LM, [Lopez-Santamaria M, et al. Influence of the coronavirus 2 (SARS-Cov-2) pandemic on acute appendicitis].[Article in Spanish with English abstract]. Anal Pediatria 2020;93:118-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wu N, Kuznik A, Wang DG, Moretz C, Xi A, Kumar S, et al. Incremental costs associated with length of hospitalization due to viral pneumonia: Impact of intensive care and economic implications of reducing the length of stay in the era of COVID-19. Clinicoecon Outcomes Res 2020;12:723-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yasin R, Gomaa AAK, Ghazy T, Hassanein SA, Ibrahem RAL, Khalifa MH. Predicting lung fibrosis in post-COVID- 19 patients after discharge with follow-up chest CT findings. Egypt J Radiol Nucl Med 2021;52:118. [Google Scholar]
- 51.Yuan J, Zou RR, Zeng LJ, Kou SL, Lan JF, Li XH, et al. The correlation between viral clearance and biochemical outcomes of 94 COVID-19 infected discharged patients. Inflamm Res 2020;69:599-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhan N, Guo YY, Tian S, Huang BL, Tian XL, Zou JJ, et al. Clinical characteristics of COVID-19 complicated with pleural effusion. BMC Infect Dis 2021;21:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tan JH, Yuan Y, Xu C, Song CY, Liu D, Ma D, et al. A retrospective comparison of drugs against COVID-19. Virus Res 2021;294;198262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jiang S, Wang R, Li L, Hong D, Ru R, Rao Y, et al. Liver injury in critically ill and non-critically ill COVID-19 patients: a multicenter, retrospective, observational study. Front Med (Lausanne) 2020;7:347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma Q, Zhang M, Ali S, Kirikkaleli D, Khan Z. Natural resources commodity prices volatility and economic performance: Evidence from China pre and post COVID-19. Resour Policy 2021;74:102338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mallow PJ, Belk KW, Topmiller M, Hooker EA. Outcomes of hospitalized COVID-19 patients by risk factors: results from a United States hospital claims J Health Econ Outcomes Res 2020;7:165-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moura DTHd, Proença IM, McCarty TR, Sagae VMT, Ribeiro IB, Oliveira GHPd, et al. Gastrointestinal manifestations and associated health outcomes of COVID-19: a Brazilian experience from the largest South American public hospital. Clinics (Sao Paulo) 2020;75:e2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gupta N, Agrawal S, Ish P, Mishra S, Gaind R, Usha G, et al. Clinical and epidemiologic profile of the initial COVID-19 patients at a tertiary care centre in India. Monaldi Arch Chest Dis 2020;90:1294. [DOI] [PubMed] [Google Scholar]
- 59.Özyılmaz S, Ergün Alış E, Ermiş E, Allahverdiyev S, Uçar H. Assessment of the relationship between mortality and troponin I levels in hospitalized patients with the novel coronavirus (COVID-19). Medicina (Kaunas) 2020;56:693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Parry AH, Wani AH, Yaseen M, Shah NN, Dar KA. Clinicoradiological course in coronavirus disease-19 (COVID-19) patients who are asymptomatic at admission. BJR| Open 2020;2:20200033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rahim F, Amin S, Noor M, Bahadur S, Gul H, Mahmood A, et al. mortality of patients with severe COVID-19 in the intensive care unit: an observational study from a major COVID-19 receiving hospital. Cureus 2020;12:e10906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Netw Open 2020;3:e2029058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sardina-González C, López-Reboiro ML, Suárez-Fuentetaja R, Castro-Conde BA, Álvarez-Asensio E, López-Castro J. COVID 19 comprehensive management in a regional hospital of Northwestern Spain. Gac Med Mex 2020;156:294-7. [DOI] [PubMed] [Google Scholar]
- 64.Shi X, Lu Y, Li R, Tang Y, Shi N, Song F, et al. Evaluation of antiviral therapies for coronavirus disease 2019 pneumonia in Shanghai, China. J Med Virol 2020;92:1922-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sun J, Deng X, Chen X, Huang J, Huang S, Li Y, et al. Incidence of adverse drug reactions in COVID-19 patients in China: an active monitoring study by hospital pharmacovigilance system. Clin Pharmacol Ther 2020;108:791-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Teich VD, Klajner S, Almeida FASd, Dantas ACB, Laselva CR, Torritesi MG, et al. Epidemiologic and clinical features of patients with COVID-19 in Brazil. Einstein (Sao Paulo) 2020;18:eAO6022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Turcotte JJ, Meisenberg BR, MacDonald JH, Menon N, Fowler MB, West M, et al. Risk factors for severe illness in hospitalized Covid-19 patients at a regional hospital. PLoS One 2020;15:e0237558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.UlHaq Z, Shahzad M, Khattak MI, Fazid S, Ullah N, Shireen A, et al. Clinical Characteristics, Mortality and Associated risk factors in COVID-19 patients reported in ten major hospitals of Khyber Pakhtunkhwa, Pakistan. J Ayub Medi Coll. 2020;32:S633-S9. [PubMed] [Google Scholar]
- 69.Abi Fadel F, Al-Jaghbeer M, Kumar S, Griffiths L, Wang X, Han X, et al. Clinical characteristics and outcomes of critically Ill patients with COVID-19 in Northeast Ohio: low mortality and length of stay. Acute Crit Care 2020;35:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Erturk SM, Durak G, Ayyildiz H, Comert RG, Medetalibeyoglu A, Senkal N, et al. Covid-19: correlation of early chest computed tomography findings with the course of disease. J Comput Assist Tomogr 2020;44:633-9. [DOI] [PubMed] [Google Scholar]
- 71.Vernaz-Hegi N, Agoritsas T, Calmy A, Gayet-Ageron A, Gold G, Perrier A, et al. Early experimental COVID-19 therapies: associations with length of hospital stay, mortality and related costs. Swiss Med Wkly 2020;150:w20446. [DOI] [PubMed] [Google Scholar]
- 72.Wagner J, Garcia-Rodriguez V, Yu A, Dutra B, Bhatt A, Larson S, et al. The model for end-stage liver disease-sodium score at admission is prognostic of Covid-19 disease severity. SN Compr Clin Med 2020;2:1978-1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wu J, Li W, Shi X, Chen Z, Jiang B, Liu J, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Inter Med 2020;288:128-38. [DOI] [PubMed] [Google Scholar]
- 74.Xie Q, Fan F, Fan XP, Wang XJ, Chen MJ, Zhong BL, et al. COVID-19 patients managed in psychiatric inpatient settings due to first-episode mental disorders in Wuhan, China: clinical characteristics, treatments, outcomes, and our experiences. Transl Psychiatry 2020;10:337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yuan J, Zou R, Zeng L, Kou S, Lan J, Li X, et al. The correlation between viral clearance and biochemical outcomes of 94 COVID-19 infected discharged patients. Inflamm Res 2020;69:599-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhang Y, Du M, Johnston JM, Andres EB, Suo J, Yao H, et al. Estimating length of stay and inpatient charges attributable to hospital-acquired bloodstream infections. Antimicrob Resist Infect Control 2020;9:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Egol KA, Konda SR, Bird ML, Dedhia N, Landes EK, Ranson RA, et al. Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a New York City perspective. J Orthop Trauma 2020;34:395-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Del Giorno R, Quarenghi M, Stefanelli K, Rigamonti A, Stanglini C, De Vecchi V, et al. Phase angle is associated with length of hospital stay, readmissions, mortality, and falls in patients hospitalized in internal-medicine wards: A retrospective cohort study. Nutrition 2021;85:111068. [DOI] [PubMed] [Google Scholar]
- 79.Cengiz M, Uysal BB, Ikitimur H, Ozcan E, Islamoğlu MS, Aktepe E, et al. Effect of oral L-glutamine supplementation on Covid-19 treatment. Clin Nutr Exp 2020;33:24-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ayaz A, Arshad A, Hajra Malik HA, Hussain E, Jamil B. Risk factors for intensive care unit admission and mortality in hospitalized COVID-19 patients. Acute Crit Care 2020;35:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Battaglini D, Santori G, Chandraptham K, Iannuzzi F, Bastianello M, Tarantino F, et al. Neurological complications and noninvasive multimodal neuromonitoring in critically ill mechanically ventilated COVID-19 patients. Front Neurol 2020;11:602114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ar Bhuyan M, Al Mahtab M, Ashab E, Haque MJ, Hoque SMM, Huq AF, et al. Treatment of COVID-19 patients at a medical college hospital in Bangladesh. Euroasian J Hepatogastroenterol 2020;10:27-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Agrupis KA, Smith C, Suzuki S, Villanueva AM, Ariyoshi K, Solante R, et al. Epidemiological and clinical characteristics of the first 500 confirmed COVID-19 inpatients in a tertiary infectious disease referral hospital in Manila, Philippines. Trop Med Health 2021;49:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Almas A, Mushtaq Z, Moller J. Acuity level of care as a predictor of case fatality and prolonged hospital stay in patients with COVID-19: a hospital-based observational follow-up study from Pakistan. BMJ Open 2021;11:e045414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Arslan Y, Dogan D, Ocal N, Koc A, Ayaz T, Ozkan R, et al. The boundaries between survival and non-survival at COVID-19: Experience of tertiary care pandemic hospital. Int J Clin Pract 2021;75:e14461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Banwait R, Singh D, Blanco A, Rastogi V, Abusaada K. Renin-angiotensin-aldosterone system blockers prior to hospitalization and their association with clinical outcomes in coronavirus disease 2019 (COVID-19). Cureus 2021;13:e13429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Beatty K, Hamilton V, Kavanagh PM. Just a bad flu? Tackling the “infodemic” in Ireland through a comparative analysis of hospitalised cases of COVID-19 and influenza. Public health 2021;194:19-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dagher L, Wanna B, Mikdadi G, Young M, Sohns C, Marrouche NF. High-degree atrioventricular block in COVID-19 hospitalized patients. Europace 2021;23:451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ersöz A, Yılmaz TE. The association between micronutrient and hemogram values and prognostic factors in COVID-19 patients: A single-center experience from Turkey. Int J Clin Pract 2021;75:e14078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhan X, Chen Z, Hu H, Yang Y, Wu K, Cheng Z, et al. Dandelion and focal crazy paving signs: the lung CT based predictors for evaluation of the severity of coronavirus disease. Curr Med Res Opin 2021;37:219-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yoon DH, Koller S, Duldulao PMN, Ault GT, Lee SW, Cologne KG. COVID-19 impact on colorectal daily practice - How long will it take to catch up? J Gastrointest Surg 2021;25:260-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yesilkaya N, Tellioglu TM, Unay FC, İner H, Besir Y, Gokalp O, et al. Histopathologic evaluation of COVID-19 patients with peripheral arterial thromboembolism: Does clot composition make any sense? Ann Vascul Surg 2021;74:80-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yeates EO, Nahmias J, Chinn J, Sullivan B, Stopenski S, Amin AN, et al. Improved outcomes over time for adult COVID-19 patients with acute respiratory distress syndrome or acute respiratory failure. PloS One 2021;16:e0253767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Xiong B, He LM, Qin YY, Du H, Zhan Z, Zhou YH, et al. Effectiveness of adjunctive corticosteroid therapy in patients with severe COVID-19: A retrospective cohort study. World J Clin Cases 2021;9:3546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Vranis NM, Bekisz JM, Daar DA, Chiu ES, Wilson SC. Clinical outcomes of 2019 COVID-19 positive patients who underwent surgery: A New York City experience. J Surg Res 2021;261:113-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Villamanán E, Sobrino C, Carpio C, Moreno M, Arancón A, Lara C, et al. Inhaled bronchodilators use and clinical course of adult inpatients with Covid-19 pneumonia in Spain: A retrospective cohort study. Pulm Pharmacol Ther 2021;69:102007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Varela Rodríguez C, Arias Horcajadas F, Martín-Arriscado Arroba C, Combarro Ripoll C, Juanes Gonzalez A, Esperesate Pajares M, et al. COVID-19-related neuropsychiatric symptoms in patients with alcohol abuse conditions during the SARS-CoV-2 pandemic: A retrospective cohort study using real world data from electronic health records of a tertiary hospital. Front Neurol 2021;12:630566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ferry OR, Moloney EC, Spratt OT, Whiting GF, Bennett CJ. A virtual ward model of care for patients with COVID-19: retrospective single-center clinical study. J Med Internet Res 2021;23:e25518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Valverde-López F, Tendero-Peinado C, Lecuona-Munoz M, Heredia-Carrasco C, Abellán-Alfocea P, Ortega-Suazo EJ, et al. A gastroenterologist’ clinical experience in COVID 19 and in-hospital mortality and length of stay analysis. Postgrad Med 2021;133:592-8. [DOI] [PubMed] [Google Scholar]
- 100.Spoldi C, Castellani L, Pipolo C, Maccari A, Lozza P, Scotti A, et al. Isolated olfactory cleft involvement in SARS-CoV-2 infection: prevalence and clinical correlates. Eur Arch Otorhinolaryngol 2021;278:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Soares FHC, Kubota GT, Fernandes AM, Hojo B, Couras C, Costa BV, et al. Prevalence and characteristics of new-onset pain in COVID-19 survivours, a controlled study. Eur J Pain 2021;25:1342-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sikkema B, Sint Nicolaas J, van Wijngaarden P. No association between COVID-19 related liver injury and the course of disease: a retrospective study. Scand J Gastroenterol 2021;56:68-71 [DOI] [PubMed] [Google Scholar]
- 103.Rubio-Gracia J, Giménez-López I, Garcés-Horna V, López-Delgado D, Sierra-Monzón JL, Martínez-Lostao L, et al. Point-of-care lung ultrasound assessment for risk stratification and therapy guiding in COVID-19 patients. A prospective non-interventional study. Eur Respir J 2021;58:2004283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Di Fusco M, Vaghela S, Moran MM, Lin J, Atwell JE, Malhotra D, et al. COVID-19-associated hospitalizations among children less than 12 years of age in the United States. J Med Econ 2022;25:334-46. [DOI] [PubMed] [Google Scholar]
- 105.Ronan G, Kumar L, Davey M, O′ Leary C, McAleer S, Lynch J, et al. Factors associated with SARS‐CoV‐2 infection in patients attending an acute hospital ambulatory assessment unit. J Med Virol 2021;9:4488-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rojas-Marte G, Hashmi AT, Khalid M, Chukwuka N, Fogel J, Munoz-Martinez A, et al. Outcomes in patients with COVID-19 disease and high oxygen requirements. J Clin Mede Res 2021;13:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ramos A, Joaquin C, Ros M, Martin M, Cachero M, Sospedra M, et al. Impact of COVID-19 on nutritional status during the first wave of the pandemic. Clin Nutr 2021; S0261-5614(21)00238-7. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Aghajani MH, Sistanizad M, Toloui A, Neishaboori AM, Pourhoseingholi A, Maher A, et al. COVID-19 related hospitalization costs; assessment of influencing factors. Front Emerg Med 2022;6:e3-e. [Google Scholar]
- 109.Groah SL, Pham CT, Rounds AK, Semel JJ. Outcomes of COVID‐19 patients after inpatient rehabilitation. PM R 2021;14:202-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Oliveira MR, Back GD, da Luz Goulart C, Domingos BC, Arena R, Borghi-Silva A. Endothelial function provides early prognostic information in patients with COVID-19: A cohort study. Resp Med 2021;185:106469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Martínez-Urbistondo M, Moreno-Torres V, Mora-Vargas A, Expósito-Palomo E, Castejón-Díaz R, Daimiel L, et al. Interaction of ACEI antihypertensive agent's administration with the inflammatory status at admission concerning COVID-19 clinical stay outcomes. Vascul Pharmacol 2022;143:106955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Marmarchi F, Liu M, Rangaraju S, Auld SC, Creel-Bulos MC, Kempton CL, et al. Clinical outcomes of critically iii patients with COVID-19 by race. J Racial Ethn Health Disparities 2022;9:385-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.He M, Li X, Tan Q, Chen Y, Kong Y, You J, et al. Disease burden from COVID-19 symptoms among inpatients at the temporary military hospitals in Wuhan: a retrospective multicentre cross-sectional study. BMJ Open 2021;11:e048822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yousef M, Showe LC, Shlomo IB. Clinical presentation of COVID-19–a model derived by a machine learning algorithm. J Integr Bioinform 2021;18:3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Majeed AI, Raza F, Riaz SK, Kanwal J. The essential role of conventional radiography in Covid-19; Perspective of a developing country. J Ayub Med Coll 2021;33:267-73. [PubMed] [Google Scholar]
- 116.Mader C, Bernatz S, Michalik S, Koch V, Martin SS, Mahmoudi S, et al. Quantification of COVID-19 opacities on chest CT - Evaluation of a fully automatic AI-approach to noninvasively differentiate critical versus noncritical patients. Acad Radiol 2021;28:1048-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ahlström B. The epidemiology of risk factors and short and long-term outcome in the Swedish intensive care cohort. PhD Thesis, University of Uppsala; 2021. [Google Scholar]
- 118.Alamdari NM, Shams F, Abbasi M, Nadian MAA, Fathi M, Besharat S. COVID-19-related spontaneous pneumomediastinum: An atypical manifestation. J Cell Mol Anesth 2021;6:188-91. [Google Scholar]
- 119.Aldhaeefi M, Dube K, Kovacevic M, Szumita P, Lupi K, DeGrado J. 299: Evaluation of rocuronium in critically ill patients during the COVID-19 pandemic. Crit Care Med 2021;49:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Andrade JA, Muzykovsky K, Truong J. Risk factors for mortality in COVID‐19 patients in a community teaching hospital. J Med Virol 2021;93:3184-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Bonnet N, Martin O, Boubaya M, Levy V, Ebstein N, Karoubi P, et al. High flow nasal oxygen therapy to avoid invasive mechanical ventilation in SARS-CoV-2 pneumonia: a retrospective study. Ann Intensive Care 2021;11:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bozan Ö, Atiş ŞE, Cekmen B, Kocer MT, Koca Y, Karaaslan EB, et al. Clinical findings and prognosis of hospitalized elderly COVID-19 patients. Turk J Geriatrics 2021;24:194. [Google Scholar]
- 123.Breik O, Nankivell P, Sharma N, Bangash MN, Dawson C, Idle M, et al. Safety and 30-day outcomes of tracheostomy for COVID-19: a prospective observational cohort study. Br J Anaesth 2020;125:872-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Cai Y, Huang T, Liu X, Xu G. The effects of "Fangcang, Huoshenshan, and Leishenshan" makeshift hospitals and temperature on the mortality of COVID-19. Peer J 2020. Jul 21;8:e9578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jaiswal V, Nasa P, Raouf M, Gupta M, Dewedar H, Mohammad H, et al. Therapeutic plasma exchange followed by convalescent plasma transfusion in critical COVID-19— An exploratory study. Int J Infect Dis 2021;102:332-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Zhang M, Zhou J, Dirlikov B, Cage T, Lee M, Singh H. Impact on neurosurgical management in Level 1 trauma centers during COVID-19 shelter-in-place restrictions: The Santa Clara County experience. J Clini Neurosci. 2021;88:128-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Charoenngam N, Shirvani A, Reddy N, Vodopivec DM, Apovian CM, Holick MF. Association of vitamin D status with hospital morbidity and mortality in adult hospitalized patients with COVID-19. Endocr Pract 2021;27:271-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Xu H, Martin A, Singh A, Narasimhan M, Lau J, Weinberg M, et al. Pulmonary embolism in patients hospitalized with COVID-19 (from a New York health system). Am J Cardiol 2020;133:148-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sarpong K, Dowlati E, Withington C, Chesney K, Mualem W, Hay K, et al. Perioperative coronavirus disease 2019 (COVID-19) incidence and outcomes in neurosurgical patients at two tertiary care centers in Washington, DC, during a pandemic: A 6-month follow-up. World Neurosurg 2021;146:e1191-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Korkmaz MÖ, Eğilmez OK, Özçelik MA, Güven M. Otolaryngological manifestations of hospitalised patients with confirmed COVID-19 infection. Eur Arch Otorhinolaryngol 2021;278:1675-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hittesdorf E, Panzer O, Wang D, Stevens JS, Hastie J, Jordan DA, et al. mortality and renal outcomes of patients with severe COVID-19 treated in a provisional intensive care unit. J Crit Care 2021;62:172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Diez‐Quevedo C, Iglesias‐González M, Giralt‐López M, Rangil T, Sanagustin D, Moreira M, et al. Mental disorders, psychopharmacological treatments, and mortality in 2150 COVID‐19 Spanish inpatients. Acta Psychiatr Scand 2021;143:526-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Forsblom E, Silén S, Kortela E, Ahava M, Kreivi H-R, Holmberg V, et al. Male predominance in disease severity and mortality in a low Covid-19 epidemic and low case-fatality area–a population-based registry study. Infect Dis (Lond) 2021;53:789-99. [DOI] [PubMed] [Google Scholar]
- 134.Vekaria B, Overton C, Wiśniowski A, Ahmad S, Aparicio-Castro A, Curran-Sebastian J, et al. Hospital length of stay for COVID-19 patients: Data-driven methods for forward planning. BMC Infect Dis 2021;21:700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wei C, Liu Y, Liu Y, Zhang K, Su D, Zhong M, et al. Clinical characteristics and manifestations in older patients with COVID-19. BMC Geriatr 2020;20:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Alwafi H, Naser AY, Qanash S, Brinji AS, Ghazawi MA, Alotaibi B, et al. Predictors of length of hospital stay, mortality, and outcomes among hospitalised COVID-19 patients in Saudi Arabia: a cross-sectional study. J Multidiscip Healthc 2021;14:839-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Liu K, Chen Y, Lin R, Han K. Clinical features of COVID- 19 in elderly patients: A comparison with young and middleaged patients. J Infect 2020;80:e14-e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rees EM, Nightingale ES, Jafari Y, Waterlow NR, Clifford S, Pearson CA, et al. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med 2020;18:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Boëlle P-Y, Delory T, Maynadier X, Janssen C, Piarroux R, Pichenot M, et al. Trajectories of hospitalization in COVID- 19 patients: an observational study in France. J Clin Med 2020;9:3148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Oksuz E, Malhan S, Gonen MS, Kutlubay Z, Keskindemirci Y, Tabak F. COVID-19 healthcare cost and length of hospital stay in Turkey: retrospective analysis from the first peak of the pandemic. Health Econ Rev 2021;11:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Spinner CD, Gottlieb RL, Criner GJ, López JRA, Cattelan AM, Viladomiu AS, et al. effect of remdesivir vs standard care on clinical status at 11 days in patients with moderate COVID-19: a randomized clinical trial. JAMA 2020;324:1048-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Chiam T, Subedi K, Chen D, Best E, Bianco FB, Dobler G, et al. Hospital length of stay among COVID-19-positive patients. J Clin Transl Res 2021;7:377-85. [PMC free article] [PubMed] [Google Scholar]


