Abstract
Background
In 2019, tuberculosis incidence and mortality in Brazil were 46 and 3·3 per 100 000 population, respectively, and the country has reported rising tuberculosis case rates since 2016, following an economic crisis beginning in mid-2014. We aimed to estimate the number of excess tuberculosis cases and deaths during the recession period, and assessed potential causes.
Methods
In this multi-level regression modelling study, we extracted tuberculosis case notifications from Brazil's National Notifiable Disease Information System (known as SINAN), and tuberculosis deaths from the Mortality Information System (known as SIM), for all ages. We fitted mixed-effects regression models estimating trends in these outcomes—stratified by sex, age group, and state—during the pre-recession period (Jan 1, 2010–Dec 31, 2014). We calculated excess cases and deaths between Jan 1, 2015, and Dec 31, 2019 (the recession period) as the difference between reported values and a counterfactual of continued pre-recession trends. We examined the relationship between excess cases and possible explanatory factors using ordinary least squares regression. We tested the robustness of our findings to alternative model specifications related to the pre-recession period and criteria for defining tuberculosis deaths.
Findings
We estimated 22 900 excess tuberculosis cases (95% uncertainty interval 18 100–27 500) during 2015–19. By 2019, reported cases were 12% (10–13) higher than predicted by historical trends. 54% (44–66) of excess cases occurred among 20–29-year-old men. In this group, reported cases in 2019 were 30% (25–36) higher than predicted. Excess cases were positively associated with an increasing fraction of cases among incarcerated individuals (p=0·001) and higher unemployment (p=0·04) at the state level. Estimated excess deaths for 2015–19 were not statistically significant from 0 (−600 [–2100 to 1000]). These results were robust to alternative definitions of the pre-recession period and criteria for defining tuberculosis deaths.
Interpretation
Tuberculosis cases in Brazil rose substantially in 2015–19 during the recession, largely affecting young men. This increase seems to be linked to increasing tuberculosis transmission among incarcerated populations. Rising tuberculosis case rates threaten tuberculosis control in Brazil, and highlight the threat posed by prison-based tuberculosis transmission.
Funding
US National Institutes of Health.
Translation
For the Portuguese translation of the abstract see Supplementary Materials section.
Introduction
In 2019, tuberculosis incidence and mortality in Brazil were estimated as 46 and 3·3 per 100 000 population, respectively. Both incidence and mortality have declined over the past two decades,1 linked to improvements in living conditions, stronger primary health-care systems, and more effective tuberculosis control.2, 3 However, these incidence trends have reversed, with tuberculosis notifications increasing by 7·5% between 2016 and 2019, undermining progress towards the Sustainable Development Goal targets for tuberculosis.1 Several factors might have contributed to this increase in tuberculosis cases. First, Brazil experienced an economic recession beginning in 2014,4, 5 which could have influenced tuberculosis epidemiology through several mechanisms.6, 7 Health conditions resulting from deteriorating living standards can weaken immunity, predisposing affected populations to tuberculosis infection and progression. Changes in living and working conditions can increase respiratory contact rates, and delayed health-care access can extend the duration of infectiousness for individuals with tuberculosis disease, providing additional opportunities for transmission. Second, in Brazil, the economic contraction led to reduced health-care funding—which decreased by 15% as a fraction of government spending8—and restrictions on health-care access.9 The recession also increased income inequality and unemployment,10 which have been associated with increased tuberculosis case rates.11, 12 Third, incarceration might also contribute to elevated tuberculosis case rates, with several studies documenting a growing burden of tuberculosis within prisons.13, 14 Finally, over the same time period, Brazil introduced and expanded access to a new tuberculosis diagnostic tool—Xpert MTB–RIF15—which has greater sensitivity for pulmonary tuberculosis than sputum smear microscopy. This change, coinciding with the increase in reported tuberculosis cases, raises the question of whether improvements in case detection (rather than true increases in incidence) explain the observed increase in tuberculosis case rates.
Research in context.
Evidence before this study
We searched PubMed, without language restrictions, for all records published between database inception and Sept 24, 2021, using the search terms “(TB or tuberc*)” and “(incidence or case* or notification* or burden or estimate or epidem*)” and “(economic recession or economic cris* or financial cris* or fiscal cris* or austerity or downturn)” in any field. Our search returned 74 records, of which 16 estimated the relationship between economic recession and subsequent tuberculosis outcomes using empirical data (14 studies estimated changes in recorded tuberculosis cases, seven estimated changes in recorded tuberculosis deaths). Of these studies, 11 reported a positive association between economic recession and tuberculosis cases, and four reported a positive association between economic recession and tuberculosis deaths. Three studies reported a negative association between economic recession and tuberculosis cases, and one study reported a negative association between economic recession and tuberculosis deaths. Studies were based on data from the European region (n=8 studies), region of the Americas (n=5), African region (n=1), South-East Asia region (n=1), and Western Pacific region (n=1). To our knowledge, no study has examined changes in tuberculosis cases and deaths in Brazil during the economic recession of 2015–19.
Added value of this study
Using nationally representative registry data, we estimated excess tuberculosis case notifications and tuberculosis-associated deaths in Brazil during the 2015–19 recession period. We estimated that 22 900 excess tuberculosis cases (95% uncertainty interval 18 100–27 500) occurred during this period, and that 54% (44–66) of these excess cases occurred among men aged 20–29 years old. Excess cases were positively associated with an increasing fraction of cases among incarcerated individuals, and increased unemployment. We found no significant change in tuberculosis deaths. This study adds to the evidence base describing the relationship between economic conditions and the disease burden of tuberculosis, and the specific role of incarceration in contributing to tuberculosis epidemics in Latin American countries.
Implications of all the available evidence
During the 2015–19 recession period, Brazil experienced significantly higher tuberculosis cases than expected from historical trends (2010–14). Rising tuberculosis case rates threaten tuberculosis control in Brazil, and highlight the threat posed by tuberculosis transmission among incarcerated populations. Strengthening tuberculosis control is important in situations where social and economic changes increase vulnerability.
It is important to understand the pattern of changing tuberculosis case rates over the recession period to clarify the link between changing epidemiology and potential causative factors, and to identify which population groups have been most affected. We aimed to collate granular data on tuberculosis case notifications and tuberculosis-related deaths over the recession period of 2016–19. By comparing these data to trends established during the pre-recession period (2010–14), we estimated excess tuberculosis cases and tuberculosis deaths over the recession period by age, sex, and state. Finally, we examined the association between a set of putative explanatory variables (unemployment rates, changes in incarceration, and Xpert MTB–RIF scale-up) and the excess tuberculosis case estimates to better understand the contribution of different factors to the change in tuberculosis rates in 2016–19.
Methods
Data sources
In Brazil, all diagnosed tuberculosis cases are recorded in the National Notifiable Disease Information System (SINAN).16 We extracted tuberculosis case notifications between Jan 1, 2010, and Dec 31, 2019, including all ages, and retaining variables for individual sex, age, state of residence, year of notification, incarceration status, and diagnostic methods. We excluded cases with missing data for any of these variables (2·5% of all observations). We calculated total tuberculosis cases as the sum of all individuals with new and retreatment tuberculosis, as well as individuals diagnosed post mortem (n=902 743).
To calculate the number of tuberculosis deaths, we extracted vital registration data from Brazil's Mortality Information System (SIM),16 which represents a near-complete record of all deaths in Brazil,17 coded by cause. We quantified total tuberculosis deaths, defined as all death records containing International Classification of Disease 10th edition (ICD-10) codes A15.0–A19.9, K67.3, K93.0, M49.0, N74.0–N74.1, P37.0, or B20.0 as a primary or secondary cause (n=73 358).18 As a sensitivity analysis, we calculated an alternative estimate of tuberculosis deaths using more restrictive inclusion criteria: only counting deaths with tuberculosis listed as the primary cause, using a core set of ICD-10 codes (A15.0–A19.9; n=44 856).
For each year from 2010 to 2019, we stratified data on tuberculosis cases and deaths by sex, state (26 states plus the federal district), and 10-year age group (nine groups), creating 486 analytic strata, and 4860 stratum years. We calculated annual tuberculosis notification and mortality rates, dividing case and death counts for each stratum by population estimates produced by the Brazilian Institute of Geography and Statistics.19
We collated data on possible explanatory variables. We extracted state-level data on unemployment rates over the period 2012–19 (the maximum period available) from the National Continuous Household Sample Survey.20 In these data, the unemployment rate is defined as the percentage of individuals aged 14 years and older who are currently unemployed and looking for employment. To describe the relationship between incarceration and tuberculosis, we extracted case notifications for incarcerated individuals as recorded in SINAN between 2010 and 2019. We accessed state-level population estimates for the incarcerated population from Brazil's Ministry of Justice and Public Security.21 Xpert MTB–RIF was introduced by the National TB Program of the Brazilian Ministry of Health for routine tuberculosis diagnosis beginning in 2015, as a first choice diagnostic for confirming tuberculosis. To describe the scale-up of Xpert MTB–RIF, we classified SINAN case notifications as cases diagnosed by Xpert MTB–RIF versus by other methods (eg, smear microscopy and culture). Table 1 summarises data inputs.
Table 1.
Data description and sources
| Description | Data source | |
|---|---|---|
| Tuberculosis notification cases | Tuberculosis case records, by sex, 10-year age categories, state, and year, for 2010–19 | SINAN16 |
| Tuberculosis deaths | Number of deaths with a tuberculosis-related ICD-10 code*, by sex, 10-year age categories, state, and year, for 2010–19 | SIM16 |
| General population size | Number of individuals in the population, by sex, 10-year age categories, state, and year, for 2010–19 | IBGE19 |
| Prisoner tuberculosis notification cases | Tuberculosis notification cases in the incarcerated adult population (aged ≥18 years), by sex, 10-year age categories, state, and year, for 2010–19 | SINAN16 |
| Incarcerated population size | Number of incarcerated adults (aged ≥18 years), by sex, state, and year, for 2010–19 | NPD21 |
| Tuberculosis notification cases diagnosed by Xpert MTB–RIF | Tuberculosis notification cases diagnosed by Xpert MTB–RIF, by state, for 2015–19 | SINAN16 |
| Unemployment rate | Percentage of individuals (aged ≥14 years) who are currently unemployed and looking for employment relative to employed and unemployed individuals (state-level data), for 2012–19 | IBGE20 |
ICD-10=International Classification of Disease 10th edition. SINAN=Brazil's National Notifiable Disease Information System. SIM=Brazil's Mortality Information System. IBGE=Brazilian Institute of Geography and Statistics. NPD=National Penitentiary Department.
For the main analysis, tuberculosis deaths were defined as a death with ICD-10 codes A15.0–A19.9, K67.3, K93.0, M49.0, N74.0–N74.1, P37.0, or B20.0 listed as a primary or secondary cause. In our sensitivity analyses, we recalculated results via a restrictive definition of tuberculosis-related death (deaths with ICD-10 codes A15.0–A19.9 listed as a primary cause).
Study period
According to previous economic analyses, Brazil's most recent economic recession began in mid-2014.4, 5 Since national gross domestic product (GDP) had not increased to the point of its pre-recession level by 2019,22, 23 we defined the period of Jan 1, 2015–Dec 31, 2019 as the recession period, and the period of Jan 1, 2010–Dec 31, 2014 as the pre-recession period.
Statistical analysis
Excess tuberculosis cases and deaths for the recession period
We used mixed-effects generalised linear models for SINAN tuberculosis case notifications data from the pre-recession period. This model allowed for variation in the level and time trend in tuberculosis case rates by sex, age group (introduced as a categorical variable), and state, with random-effects distributions allowing for partial pooling of results for individual strata. The relatively short (5-year) pre-recession period was chosen to reduce risks of bias due to non-linear trends in pre-recession data. In a sensitivity analysis, we tested shorter and longer pre-recession periods from 3 to 14 years:
| (1) |
| (2) |
In equation 1, Y ijsl represents the reported data (tuberculosis case counts stratified by sex i, age group j, state s, and year l), a ijsl represents the population size for each stratum, and λijsl represents the tuberculosis case notification rate. The linear equation for λijsl (equation 2), included fixed effects (β) for each individual variable (sex, age group, and state), and random effects (γ) for the intercept and slope for each analytic stratum. These fixed and random effects were specified for the intercept and for a linear time trend. As the regression uses a log-link function, explanatory variables were assumed to have a multiplicative relationship with the outcome. We fitted an equivalent regression model for the SIM tuberculosis death data, to estimate trends in tuberculosis death rates.
We used these regression models to estimate a trend for tuberculosis case and death rates within each analytic stratum over the pre-recession period. We extrapolated these trends to predict tuberculosis cases and deaths by sex, age group, and state for each year (2015–19) of the recession period, assuming continuation of the pre-recession trends. Finally, we estimated excess tuberculosis cases and deaths during the recession period—by sex, age group, state, and year—as the difference between predicted values and observed data for each of the 2430 analytical strata. To estimate uncertainty intervals, we generated 4000 values for each study outcome using the coefficients and variance–covariance matrix from the fitted regression models. We then calculated equal-tailed 95% intervals as the 2·5% and 97·5% percentiles of the distribution of values for each study outcome.
Association between excess tuberculosis cases and other variables
We estimated a series of linear models to test the strength of association between the ratio of observed:predicted tuberculosis cases and three putative explanatory variables: changes in unemployment, scale-up of Xpert MTB–RIF, and changes in incarceration.
For changes in unemployment, we used the absolute increase in the average unemployment rate from pre-recession to recession period, by state. For Xpert MTB–RIF scale-up, we used the proportion of observed tuberculosis cases diagnosed by Xpert MTB–RIF in each state over the recession period, given that Xpert MTB–RIF usage in routine settings was negligible before 2015. For changes in incarceration, we used the change in the fraction of tuberculosis case notifications among incarcerated populations between the pre-recession and recession period for each state—thus reflecting changes in prison population and changes in tuberculosis rates within prisons.
To represent changes in tuberculosis cases, we used the ratio of observed:predicted tuberculosis cases over the recession period, with a larger ratio indicating greater relative increases in case notifications during the recession period than the historical trend. All variables were estimated at state level (27 observations). We estimated the association between the excess tuberculosis variable and each individual explanatory variable using ordinary least squares regression. We also fit a model including all three explanatory variables.
Sensitivity analyses
We tested the robustness of our findings to alternative model specifications. First, we re-calculated excess tuberculosis case and death estimates using alternative lengths of the pre-recession period for determining the previous trend for these outcomes. We examined periods between 3 years (2012–14) and 14 years (2001–14) for SINAN case notification data and between 3 years (2012–14) and 13 years (2002–14) for SIM death data (the maximum period available). All years were examined as Jan 1–Dec 31. Second, we re-calculated excess tuberculosis death estimates using a more restrictive definition of tuberculosis deaths (only deaths with tuberculosis listed as a primary cause, using ICD-10 codes A15.0–A19.9). Third, we re-estimated the linear models for excess cases using increases in extreme poverty, instead of unemployment, as a predictor. Extreme poverty was operationalised as the change in the population fraction with a daily income of less than US$1·90, using 2011 purchasing power parity, between pre-recession and recession periods. The extreme poverty variable was excluded from the main analysis due to high correlation with unemployment (rank correlation 0·52), and because unemployment was posited to have a more direct relationship with recession changes.
All analyses were undertaken in R (version 3.5.2).
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Between Jan 1, 2010, and Dec 31, 2019, 902 743 cases of tuberculosis were reported in SINAN, including 81 371 cases among incarcerated adults and 138 089 among individuals diagnosed using Xpert MTB–RIF. Over the same period, there were 73 358 tuberculosis deaths recorded in SIM using the definitions adopted for the main analysis, and 44 856 tuberculosis deaths using the more restrictive definition (tuberculosis as a primary cause, ICD-10 codes A15.0–A19.9).
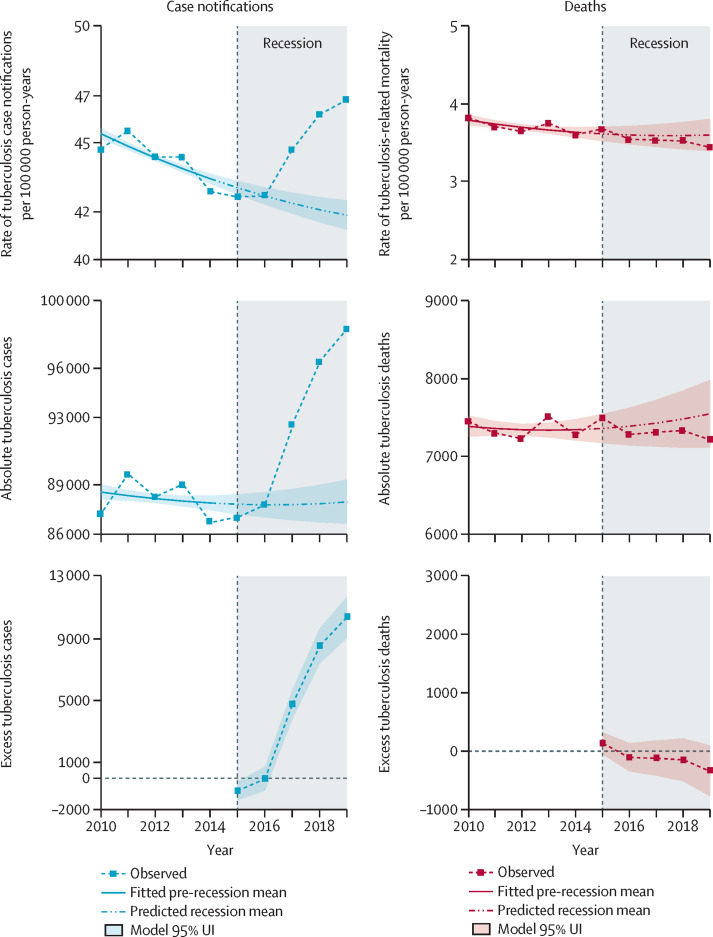
Over the pre-recession period (2010–14), the national tuberculosis case rate decreased from 45·4 (95% uncertainty interval 45·1–45·6) to 43·4 (43·2–43·7) cases per 100 000 population, with a mean annual decline of 1·09% (0·88–1·30; figure 1 ). Pre-recession tuberculosis case trends also differed by sex, age, and state (appendix 2 pp 4–7).
Figure 1.
Trends in tuberculosis case notifications and deaths during pre-recession and recession periods, and excess cases and deaths during the recession period, in the overall population in Brazil, 2010–19
Over the pre-recession period, the tuberculosis mortality rate—calculated from SIM data—declined from 3·78 (95% uncertainty interval 3·72–3·85) to 3·63 (3·56–3·70) deaths per 100 000 population, at a mean annual rate of 1·05% (0·30–1·84; figure 1). Pre-recession tuberculosis death trends by sex, age, and state are given in appendix 2 (pp 8–11).
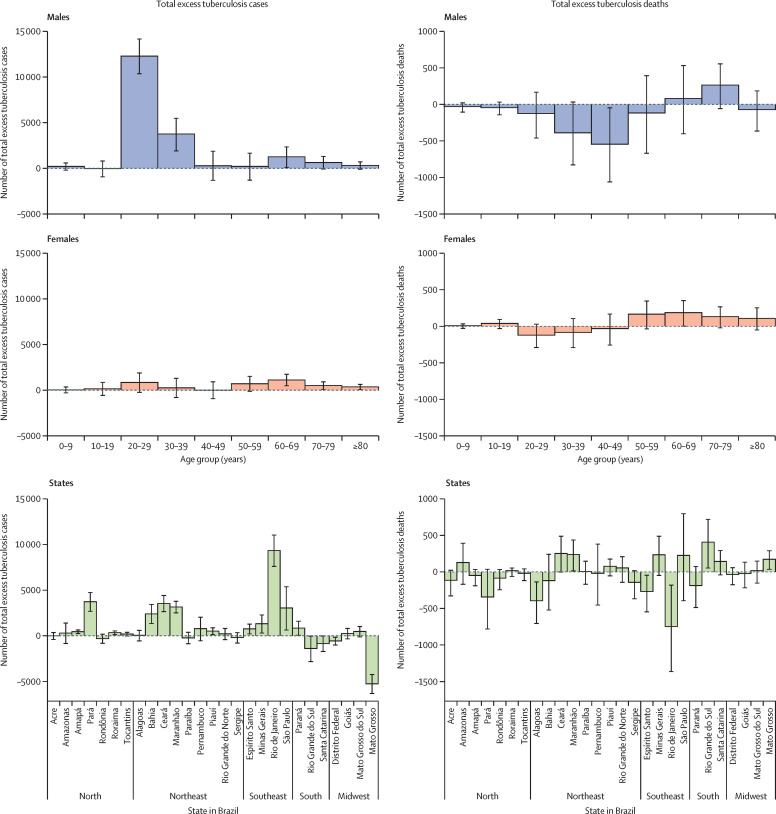
Tuberculosis cases and case rates increased during the recession period, with tuberculosis cases increasing at a mean annual rate of 3·10%, and the case rate increasing at a mean annual rate of 2·35%. Total excess cases (estimated as observed – predicted cases) were close to zero during 2015–16, but rose rapidly during 2017–19, with 10 400 (95% uncertainty interval 9000–11 700) excess cases estimated for 2019, and 22 900 (18 100–27 500) total excess cases over the full period of 2015–19 (figure 1). By 2019, reported cases were 12% (10–13) and 30% (25–36) higher than predicted by historical trends among the whole population and among 20–29-year-old men, respectively. Estimated excess cases were substantially greater in men (18 900 [14 900–22 900]) than in women (3900 [1300–6500]). Across sex and age strata, men aged 20–29 years had the highest number of excess cases (12 300 [10 400–14 100])—representing 54·1% (44·1–66·2) of total excess cases—followed by men aged 30–39 years (3800 [1900–5500]), accounting for 16·5% (8·9–23·6) of total excess cases (figure 2 ; appendix 2 p 1).
Figure 2.
Total excess cases and deaths by sex, age group, and state, during the recession period in Brazil (2015–19)
Excess cases varied greatly by state, with Rio de Janeiro having the largest number of excess cases (9300 [95% uncertainty interval 7600–11 000]), and other states having larger proportional changes (figure 2). In particular, Amapá, Roraima, and Tocantins in north Brazil and Maranhão in the northeast each had greater than 20% more cases during the recession period than predicted from the pre-recession trend (appendix 2 p 2). Time trends in excess cases by age, sex, and state are shown in appendix 2 (pp 4–7). Our sensitivity analyses for the length of the pre-recession period generally produced higher excess case estimates, although these were qualitatively similar to the main analysis (appendix 2 p 12). For example, when models were estimated with a 10-year pre-recession period (2005–14), the total estimated excess cases were 27 700 (25 200–30 300). Excess case estimates for the 20–29-year-old age group were robust to changes in the pre-recession period (appendix 2 p 12), with 11 475 (10 408–12 512) excess cases estimated using a 10-year pre-recession period.
Absolute tuberculosis deaths and the tuberculosis death rate showed little change during the recession period, with a mean annual decline of 1·0% and 1·7%, respectively. Estimates of excess tuberculosis deaths were of small magnitude (Figure 1, Figure 2). Total excess tuberculosis deaths during the recession period were estimated to be −600 (95% uncertainty interval −2100 to 1000) in the overall population, −1000 (−2300 to 400) in males, and 400 (−300 to 1100) in females. Although estimated excess deaths varied by sex, age group, and state (figure 2), these estimates were generally small compared with total tuberculosis deaths, and were not statistically significant. Appendix 2 contains further details on time trends in excess deaths by age, sex, and state (pp 8–11) and how total excess death estimates change with alternative definitions of the pre-recession period (p 12). These results were qualitatively similar to the main analysis—for example, 22 (−147 to 182) excess deaths were estimated using a 10-year pre-recession period. Although the total number of deaths with tuberculosis differed substantially depending on inclusion criteria (44 856 vs 73 358 for 2010–19), similar estimates of excess deaths were produced using the more restrictive alternative definition of tuberculosis deaths (appendix 2 p 13).
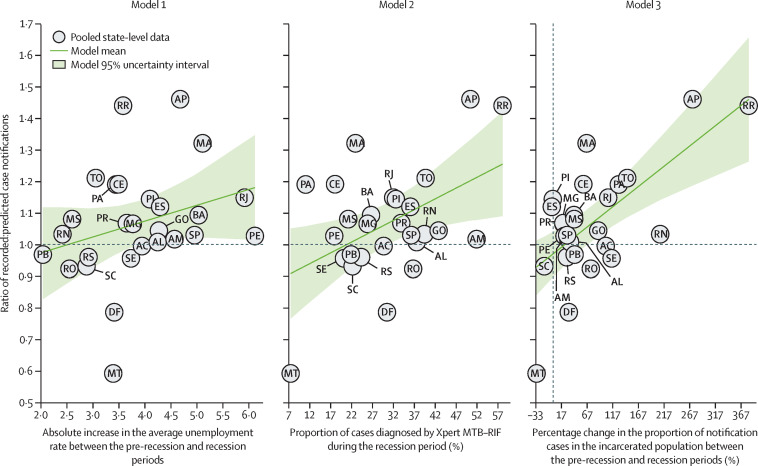
We explored the association between excess cases and three possible explanatory variables: changes in unemployment rate, Xpert MTB–RIF scale-up, and changes in incarceration. At a national level, the unemployment rate was 60·1% higher during the recession period than during the pre-recession period. Nationally, 29·3% of tuberculosis cases were diagnosed with Xpert MTB–RIF during the recession period (vs 0·7% before 2015). The proportion of cases diagnosed by Xpert MTB–RIF varied by state, from 7·4% in Mato Grosso to 58·1% in Roraima. The proportion of tuberculosis cases in the incarcerated population increased in most states during the recession, from 7·7% in 2010–14 to 9·1% in 2015–19. Only Mato Grosso, Santa Catarina, and Espírito Santo reported a reduced fraction of cases among the incarcerated population during the recession period.
Figure 3 shows the association between each explanatory variable and state-level changes in tuberculosis cases between pre-recession and recession periods. Table 2 reports regression results from univariate and multivariate models. In univariate analyses, Xpert MTB–RIF scale-up (p=0·014) and incarceration (p=0·0002) had positive associations with excess tuberculosis cases. In the multivariate analysis, incarceration (p=0·001) and unemployment (p=0·04) had positive associations with excess cases. In our sensitivity analysis of alternative specifications, tuberculosis cases during the recession did not significantly differ according to extreme poverty (p=0·078; appendix 2 p 3).
Figure 3.
Association of multiple explanatory factors with ratio of recorded to predicted case notifications across states in Brazil during the recession period (2015–19)
AC=Acre. AL=Alagoas. AM=Amazonas. AP=Amapá. BA=Bahia. CE=Ceará. DF=Distrito Federal. ES=Espírito Santo. GO=Goiás. MA=Maranhão. MG=Minas Gerais. MS=Mato Grosso do Sul. MT=Mato Grosso. PA=Pará. PB=Paraíba. PE=Pernambuco. PI=Piauí. PR=Paraná. RJ=Rio de Janeiro. RN=Rio Grande do Norte. RO=Rondônia. RR=Roraima. RS=Rio Grande do Sul. SC=Santa Catarina. SE=Sergipe. SP=São Paulo. TO=Tocantins.
Table 2.
Linear models of association of ratio of recorded:predicted cases
| Estimates | Standard error | p value | |
|---|---|---|---|
| Model 1 | |||
| Intercept | 0·875 | 0·132 | <0·0001 |
| Absolute increase in the mean unemployment rate between the pre-recession and recession periods | 0·050 | 0·033 | 0·15 |
| Model 2 | |||
| Intercept | 0·8562 | 0·0852 | <0·0001 |
| Proportion of cases diagnosed by Xpert MTB–RIF | 0·0069 | 0·0026 | 0·0139 |
| Model 3 | |||
| Intercept | 0·9706 | 0·0341 | <0·0001 |
| Percentage change in the proportion of tuberculosis notification cases in the incarcerated population between the pre-recession and recession periods | 0·0013 | 0·0003 | 0·0002 |
| Model 4* | |||
| Intercept | 0·735 | 0·1109 | <0·0001 |
| Absolute increase in the mean unemployment rate between the pre-recession and recession periods | 0·053 | 0·0249 | 0·0433 |
| Proportion of cases diagnosed by Xpert MTB–RIF | 0·0011 | 0·0025 | 0·66 |
| Percentage change in the proportion of tuberculosis notification cases in the incarcerated population between the pre-recession and recession periods | 0·0012 | 0·0003 | 0·001 |
p values are two-sided p values for differences from zero. For each model, the intercept represents the value of the outcome (ratio of observed:predicted tuberculosis cases) when all explanatory variables are equal to zero.
Model 4: all three variables, across states in Brazil. Models were estimated using pooled state-level data (27 observations).
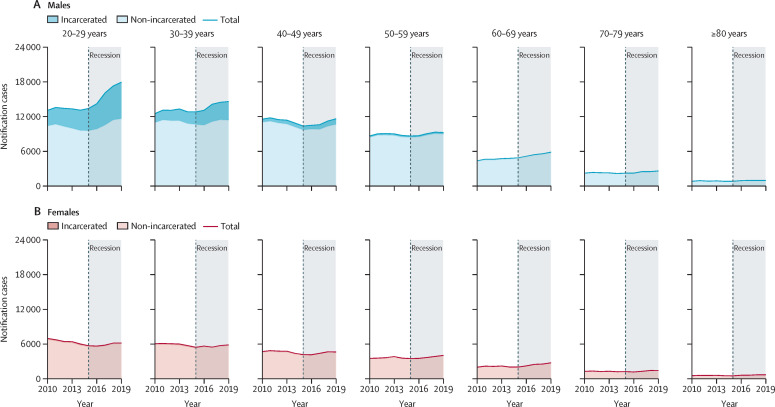
The change in tuberculosis cases among incarcerated and non-incarcerated populations differed across age groups, with the increasing burden of tuberculosis in prisons concentrated among men aged 20–29 years and 30–39 years (figure 4 ). Over the study period, tuberculosis case rates in the incarcerated population were substantially higher than in the non-incarcerated population, and increased over time (1300 vs 41 per 100 000 population in 2010; 1600 vs 40 per 100 000 in 2019). The number of incarcerated individuals also increased by 68% over the same period, from 445 700 in 2010 to 748 000 in 2019.
Figure 4.
Number of tuberculosis case notifications among incarcerated and non-incarcerated populations, by sex and age group, in adults aged ≥20 years in Brazil, 2010–19
Discussion
We estimated the excess tuberculosis cases and deaths in Brazil after a recession beginning in mid-2014. Our analyses show major increases in tuberculosis cases versus pre-recession trends, with 22 900 excess cases estimated for the recession period of 2015–19. Excess cases were concentrated among men aged 20–29 years, and secondarily among men aged 30–39 years. Taken together, 70·6% (n=16 047) of all excess tuberculosis cases occurred in men in this age group of 20–39 years, which constitutes only 16·5% of the Brazilian population. Excess cases varied widely between states, with the greatest number of excess cases estimated for Rio de Janeiro, and the greatest proportional increase seen in Amapá and Roraima. By contrast to tuberculosis cases, trends in tuberculosis deaths showed little change during the recession period, and estimates of excess tuberculosis deaths were generally small and not significant, both overall and within population subgroups. These results were robust to changes in the definition of the pre-recession period and the source of death data.
The abundance of excess tuberculosis cases among men aged 20–39 years is notable. This result is consistent with the elevated tuberculosis risks faced by men,24 and evidence from other studies that suggest the burdens of a recession might be felt most strongly for men and younger workers (aged 20–39 years).25, 26 A 2021 study found that almost one-fifth of 10–24-year-olds treated for tuberculosis in Brazil experienced unfavourable treatment outcomes (loss to follow-up, treatment failure, or death).27 This result is also consistent with our analysis of potential explanatory variables, in which increases in unemployment and the fraction of cases among incarcerated populations were closely tied to greater excess tuberculosis cases in the multivariate analysis. In these analyses, the association between tuberculosis cases and incarceration was particularly strong. Young men represent the majority of all incarcerated individuals in Brazil and the number of tuberculosis cases in this population have been increasing progressively, driven by rising tuberculosis case rates and by rapidly increasing prison populations. The increase in tuberculosis cases within prisons has been well documented for Brazil28, 29 and other South American countries.13, 14, 30 Although tuberculosis cases among incarcerated populations have risen substantially, this increase might capture only part of the impact of prison-based transmission. Given the long latent period of tuberculosis, with some cases occurring years after initial infection, a substantial proportion of individuals who acquired tuberculosis in prison might not show symptoms until after prison release. As such, these cases would not be linked to incarceration in the tuberculosis notification system. This epidemiological relationship between tuberculosis in prisons and the communities in which they are located has been confirmed by genotypic surveillance studies.24, 31 The results of our analysis suggest that the rising tuberculosis epidemic in Brazil's prisons could now be having measurable consequences beyond their surrounding communities, and could be impacting national-level disease trends.
Unlike our estimates of excess cases, the estimated number of excess deaths were small, negative, and statistically indistinguishable from zero. This outcome is consistent with a 2019 study suggesting the recession had little effect on infectious disease deaths, despite increases in cancer and cardiovascular disease deaths, and in all-cause mortality.5 However, it is surprising that estimated excess deaths were close to zero, given the large increase in cases. Allowing for case fatality of about 7%,32 the 22 900 excess cases would be expected to result in about 1600 tuberculosis deaths, which is outside the confidence interval estimated for total excess deaths. One potential explanation for this discrepancy is the lag between tuberculosis diagnosis and tuberculosis death, which can be more than a year. Given that the excess cases were concentrated in the final years of the recession period, it is possible that a proportion of the resulting deaths were not captured in our study period. Another factor that might have had a key effect on excess deaths is the age distribution of excess cases. As tuberculosis case fatality is strongly correlated with age, additional cases in the 20–29-year-old age group would be expected to produce few additional deaths. For example, a case fatality of 1% would imply 200–300 excess deaths, which is well within the reported interval. Moreover, changes in patient care, with an increasing proportion of individuals being treated in primary care facilities,33, 34 could have improved survival among treated individuals and offset increasing case rates.
An alternative interpretation of the increase in tuberculosis case notifications is that they reflect improvements in case detection, rather than a true increase in incidence. The introduction of Xpert MTB–RIF, which progressively replaced smear microscopy for tuberculosis diagnosis during the study period, could have improved case detection and led to greater tuberculosis notifications. However, there are several reasons to doubt this explanation. First, the regression analysis of possible explanatory variables had mixed results for Xpert MTB–RIF scale-up, with the multivariate analysis suggesting a relatively weak association between Xpert MTB–RIF scale-up and excess cases, after adjusting for other factors. Second, it is difficult to explain the age–sex distribution of excess cases as resulting from the scale-up of Xpert MTB–RIF, since the use of the new diagnostic tool was not differential by age or sex. Finally, evidence from trial settings has shown Xpert MTB–RIF scale-up to have little effect on total notification rates, which was linked to high rates of empirical treatment among individuals testing negative with smear or Xpert MTB–RIF.35
This study had several limitations. First, one of the main outcomes used for analyses—tuberculosis case notifications—can be affected by changes in both disease incidence and case detection, making it difficult to isolate the cause of empirical trends. Although it is implausible that Xpert MTB–RIF scale-up was solely responsible for the observed tuberculosis case trends, it is possible that Xpert MTB–RIF, or some other contemporaneous change, affected case detection during the recession period. Second, due to data gaps, we were not able to examine trends of tuberculosis case notifications and deaths across population subgroups by race or ethnicity and education. However, there is reason to suspect the additional tuberculosis cases estimated during the recession period were not distributed equally by race and education due to racial or ethnic disparities in unemployment rate, access to health care, and incarceration.5, 36 Third, the regression analyses of potential explanatory variables allow for relatively weak causal inference, and it is possible that unobserved causal factors biased the relationships that were estimated. For example, changes in employment will be highly correlated with poverty and other social changes resulting from the recession. For this reason, the relationship estimated for employment should be seen as a signal of the effects of these collective changes, rather than identifying a specific role for employment. The relationship between the economic recession and any change in tuberculosis incidence will involve a complex network of mechanisms, which is difficult to investigate with aggregate observational data.
In summary, tuberculosis case trends in Brazil rose substantially in the wake of the recession that began in 2014. Although aspects of these changes require further investigation, it is likely that increasing tuberculosis incidence is the primary cause, linked to high rates of transmission in Brazil's prisons. Although not reflected in higher tuberculosis death rates, these additional tuberculosis cases reflect a major health event for affected individuals, with the potential for lifelong disability.37 These individuals will also transmit infection to others in the community, leading to new tuberculosis cases in the future. These findings underline the importance of strengthening disease control in situations where social and economic changes increase vulnerability, and highlight the increasing threat posed by prison-based tuberculosis transmission for both incarcerated individuals and the wider community. As the SARS-CoV-2 pandemic produces fundamental social and economic disruption in Brazil, maintaining tuberculosis prevention and control will be crucial to protecting population health over the coming years.
Data sharing
All data used in this study are openly accessible and available through the sources listed in table 1.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgements
This work was supported by a grant from the National Institute of Allergy and Infectious Diseases, US National Institutes of Health (R01AI146555) to NAM.
Contributors
YL and NAM conceptualised the study. YL, RMC, DMP, LCA, PB, ELM, MS, MCC, TC, and NAM designed the study. YL, RMC, DMP, LCA, and PB curated data. YL, PB, MS, MCC, TC, and NAM contributed to methodology, formal analysis, and data validation. YL drafted the first version of the manuscript. YL, RMC, DMP, LCA, PB, ELM, MS, MCC, TC, and NAM reviewed and edited the manuscript. YL, RMC, and NAM accessed and verified the data underlying the study. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Supplementary Materials
References
- 1.World Health Organization Global tuberculosis report 2020. 2019. https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf
- 2.Pelissari DM, Rocha MS, Bartholomay P, et al. Identifying socioeconomic, epidemiological and operational scenarios for tuberculosis control in Brazil: an ecological study. BMJ Open. 2018;8:e018545. doi: 10.1136/bmjopen-2017-018545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zille AI, Werneck GL, Luiz RR, Conde MB. Social determinants of pulmonary tuberculosis in Brazil: an ecological study. BMC Pulm Med. 2019;19:87. doi: 10.1186/s12890-019-0855-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rasella D, Basu S, Hone T, Paes-Sousa R, Ocké-Reis CO, Millett C. Child morbidity and mortality associated with alternative policy responses to the economic crisis in Brazil: a nationwide microsimulation study. PLoS Med. 2018;15:e1002570. doi: 10.1371/journal.pmed.1002570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hone T, Mirelman AJ, Rasella D, et al. Effect of economic recession and impact of health and social protection expenditures on adult mortality: a longitudinal analysis of 5565 Brazilian municipalities. Lancet Glob Health. 2019;7:e1575–e1583. doi: 10.1016/S2214-109X(19)30409-7. [DOI] [PubMed] [Google Scholar]
- 6.Dye C, Lönnroth K, Jaramillo E, Williams BG, Raviglione M. Trends in tuberculosis incidence and their determinants in 134 countries. Bull World Health Organ. 2009;87:683–691. doi: 10.2471/BLT.08.058453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lönnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 2009;68:2240–2246. doi: 10.1016/j.socscimed.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 8.Brasil Constituição Emenda constitucional no 95 de 15 de dezembro de 2016. Altera o ato das disposições constitucionais transitórias, para instituir o novo regime fiscal, e dá outras providências. 1988. http://www.planalto.gov.br/ccivil_03/constituicao/emendas/emc/emc95.htm
- 9.Watts J. Brazil's health system woes worsen in economic crisis. Lancet. 2016;387:1603–1604. doi: 10.1016/S0140-6736(16)30249-5. [DOI] [PubMed] [Google Scholar]
- 10.Meyer BD, Sullivan JX. Consumption and income inequality and the Great Recession. Am Econ Rev. 2013;103:178–183. [Google Scholar]
- 11.Ploubidis GB, Palmer MJ, Blackmore C, et al. Social determinants of tuberculosis in Europe: a prospective ecological study. Eur Respir J. 2012;40:925–930. doi: 10.1183/09031936.00184011. [DOI] [PubMed] [Google Scholar]
- 12.de Castro DB, Sadahiro M, Pinto RC, de Albuquerque BC, Braga JU. Spatial distribution of tuberculosis in Manaus and its social determinants, 2008-2013. Int J Tuberc Lung Dis. 2018;22:171–178. doi: 10.5588/ijtld.17.0369. [DOI] [PubMed] [Google Scholar]
- 13.Walter KS, Martinez L, Arakaki-Sanchez D, et al. The escalating tuberculosis crisis in central and South American prisons. Lancet. 2021;397:1591–1596. doi: 10.1016/S0140-6736(20)32578-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cords O, Martinez L, Warren JL, et al. Incidence and prevalence of tuberculosis in incarcerated populations: a systematic review and meta-analysis. Lancet Public Health. 2021;6:e300–e308. doi: 10.1016/S2468-2667(21)00025-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boehme CC, Nabeta P, Hillemann D, et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 2010;363:1005–1015. doi: 10.1056/NEJMoa0907847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brasil Ministério da Saúde Departamento de Informática do Sistema Único de Saúde. Sistema de Informação de Agravos de Notificação (Sinan) https://datasus.saude.gov.br/transferencia-de-arquivos/
- 17.Queiroz BL, Freire FHMA, Gonzaga MR, Lima EEC. Estimativas do grau de cobertura e da mortalidade adulta (45q15) para as unidades da federação no Brasil entre 1980 e 2010. Rev Bras Epidemiol. 2017;20(suppl 1):21–33. doi: 10.1590/1980-5497201700050003. [DOI] [PubMed] [Google Scholar]
- 18.Chitwood MH, Pelissari DM, Drummond Marques da Silva G, et al. Bayesian evidence synthesis to estimate subnational TB incidence: an application in Brazil. Epidemics. 2021;35:100443. doi: 10.1016/j.epidem.2021.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Instituto Brasileiro de Geografia e Estatística População. https://www.ibge.gov.br/en/statistics/social/population.html
- 20.Instituto Brasileiro de Geografia e Estatística PNAD Contínua—Pesquisa Nacional por Amostra de Domicílios Contínua. https://www.ibge.gov.br/estatisticas/multidominio/condicoes-de-vida-desigualdade-e-pobreza/17270-pnad-continua.html?=&t=downloads
- 21.Ministério da Justiça e Segurança Pública. Departamento Nacional Penitenciário Levantamento Nacional de Informações Penitenciárias: INFOPEN. https://dados.mj.gov.br/dataset/infopen-levantamento-nacional-de-informacoes-penitenciarias
- 22.Instituto Brasileiro de Geografia e Estatística Produto Interno Bruto dos Municípios. https://www.ibge.gov.br/estatisticas/economicas/contas-nacionais/9088-produto-interno-bruto-dos-municipios.html?=&t=downloads
- 23.World Bank GDP per capita (constant LCU)—Brazil. https://data.worldbank.org/indicator/NY.GDP.PCAP.KN?locations=BR (accessed Feb 19, 2021).
- 24.Sacchi FPC, Praça RM, Tatara MB, et al. Prisons as reservoir for community transmission of tuberculosis, Brazil. Emerg Infect Dis. 2015;21:452–455. doi: 10.3201/eid2103.140896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Engemann KM, Wall HJ. The effects of recessions across demographic groups. https://files.stlouisfed.org/files/htdocs/publications/review/10/01/Engemann.pdf
- 26.Hoynes H, Miller DL, Schaller J. Who suffers during recessions? J Econ Perspect. 2012;26:27–48. [Google Scholar]
- 27.Chenciner L, Annerstedt KS, Pescarini JM, Wingfield T. Social and health factors associated with unfavourable treatment outcome in adolescents and young adults with tuberculosis in Brazil: a national retrospective cohort study. Lancet Glob Health. 2021;9:e1380–e1390. doi: 10.1016/S2214-109X(21)00300-4. [DOI] [PubMed] [Google Scholar]
- 28.Bourdillon PM, Gonçalves CCM, Pelissari DM, et al. Increase in tuberculosis cases among prisoners, Brazil, 2009-2014. Emerg Infect Dis. 2017;23:496–499. doi: 10.3201/eid2303.161006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mabud TS, de Lourdes Delgado Alves M, Ko AI, et al. Evaluating strategies for control of tuberculosis in prisons and prevention of spillover into communities: an observational and modeling study from Brazil. PLoS Med. 2019;16:e1002737. doi: 10.1371/journal.pmed.1002737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sequera VG, Aguirre S, Estigarribia G, et al. Increased incarceration rates drive growing tuberculosis burden in prisons and jeopardize overall tuberculosis control in Paraguay. Sci Rep. 2020;10:21247. doi: 10.1038/s41598-020-77504-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Warren JL, Grandjean L, Moore DAJ, et al. Investigating spillover of multidrug-resistant tuberculosis from a prison: a spatial and molecular epidemiological analysis. BMC Med. 2018;16:122. doi: 10.1186/s12916-018-1111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization WHO global TB database. 2020. https://www.who.int/teams/global-tuberculosis-programme/data (accessed Aug 9, 2021)
- 33.Jesus GS, Pescarini JM, Silva AF, et al. The effect of primary health care on tuberculosis in a nationwide cohort of 7·3 million Brazilian people: a quasi-experimental study. Lancet Glob Health. 2022;10:e390–e397. doi: 10.1016/S2214-109X(21)00550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Department of Chronic Diseases and Sexually Transmitted Infections Tuberculosis epidemiological bulletin. 2020. http://www.aids.gov.br/pt-br/pub/2020/boletim-epidemiologico-de-turbeculose-2020
- 35.Durovni B, Saraceni V, van den Hof S, et al. Impact of replacing smear microscopy with Xpert MTB/RIF for diagnosing tuberculosis in Brazil: a stepped-wedge cluster-randomized trial. PLoS Med. 2014;11:e1001766. doi: 10.1371/journal.pmed.1001766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hone T, Rasella D, Barreto ML, Majeed A, Millett C. Association between expansion of primary healthcare and racial inequalities in mortality amenable to primary care in Brazil: a national longitudinal analysis. PLoS Med. 2017;14:e1002306. doi: 10.1371/journal.pmed.1002306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Menzies NA, Quaife M, Allwood BW, et al. Lifetime burden of disease due to incident tuberculosis: a global reappraisal including post-tuberculosis sequelae. Lancet Glob Health. 2021;9:e1679–e1687. doi: 10.1016/S2214-109X(21)00367-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data used in this study are openly accessible and available through the sources listed in table 1.