Abstract
The impact of the COVID-19 pandemic on the incidence of microbial infections and other metrics related to antimicrobial resistance (AMR) has not yet been fully described. Using data from Japan Surveillance for Infection Prevention and Healthcare Epidemiology (J-SIPHE), a national surveillance database system that routinely collects clinical and epidemiological data on microbial infections, infection control practices, antimicrobial use, and AMR emergence from participating institutions in Japan, we assessed the temporal changes in AMR-related metrics before and after the start of the COVID-19 pandemic. We found that an apparent decrease in the incidence of microbial infections in 2020 compared with 2019 may have been driven primarily by a reduction in bed occupancy, although the incidence showed a constant or even slightly increasing trend after adjusting for bed occupancy. Meanwhile, we found that the incidence of Streptococcus pneumoniae dramatically decreased from April 2020 onward, probably due to stringent non-pharmaceutical interventions against COVID-19. Antimicrobial use showed a weak increasing trend, while the use of hand sanitiser at the included medical institutions increased by about 50% in 2020 compared with 2019.
Keywords: Antimicrobial resistance, COVID-19, Surveillance
Antimicrobial resistance (AMR) is a pressing global public health threat that has been listed as a top-priority challenge by the World Health Organization (WHO) [1]. Since the adoption of the Global Action Plan on Antimicrobial Resistance in 2015 [2], member states have developed and implemented local action plans that involve monitoring and management of AMR as well as education. As part of these efforts, a national surveillance database system—Japan Surveillance for Infection Prevention and Healthcare Epidemiology (J-SIPHE)—was launched in Japan in 2017 to collect clinical and epidemiological data related to microbial infections, infection control practices, antimicrobial use, and AMR emergence from participating institutions nationwide [3].
The COVID-19 pandemic that emerged in 2020, which is still ongoing as of this writing, has had a significant impact on many aspects of healthcare. Concerns have been raised since the early days of the pandemic that the AMR situation may be exacerbated by the spread of COVID-19 due to administration of antimicrobials in COVID-19 patients, suboptimal usage due to a strained health care system, supply chain issues, disrupted vaccine programmes, and so on [4]. Meanwhile, physical distancing and personal precaution measures may limit the spread of AMR during the pandemic. Although a few studies have reported changes in antimicrobial use, AMR, and the incidence of microbial infection in various countries during the COVID-19 pandemic [[5], [6], [7]], there is still a limited body of literature on the time trend of AMR-related metrics before and after the emergence of COVID-19.
To close this gap in the literature, we performed a time-series analysis of microbial infections and related indices in Japan from January 2019 to January 2021 using the J-SIPHE database. We analysed 328 institutions (a total of 135,699 hospital beds as of January 2019) that reported their bed occupancy data throughout the study period and assessed the changes in metrics over time. We found a significant decrease in the overall incidence of infections in hospitalised patients from February to May 2020 (which coincided with the outbreak of COVID-19 outbreak in Japan and the declaration of a state of emergency) compared with the mean incidence for 2019 (Fig. 1 A). However, bed occupancy (i.e., the total number of hospitalisation days divided by the number of beds) also significantly decreased during this period and thereafter (Fig. 1B), which may reflect a change in healthcare-seeking behaviour and the cancellation of non-urgent hospitalisations. When bed occupancy was adjusted for, the incidence rate per person per hospitalisation day remained mostly constant throughout the study period, although a slight but non-significant increase was observed in June–October 2020 (Fig. 1C).
Fig. 1.
Relative change in monthly incidence of microbial infections by institution (A) Monthly incidence of all infections; (B) Monthly bed occupancy; (C) Incidence rate per bed occupancy; (D) Incidence rate per bed occupancy by selected species. Institution-level outcome variables (shown in grey lines) were summarised as a monthly mean of relative values, where the yearly average over January–December 2019 was used as a baseline (relative value of 1). Red lines in (A)–(C) and coloured lines in (D) indicate the mean and 95% confidence interval among the included institutions.
We also analysed the incidence of three selected microbial species: Staphylococcus aureus and Escherichia coli as major infectious agents in healthcare settings [8] and Streptococcus pneumoniae as the most common cause of community-acquired pneumonia [9] (Fig. 1D). The incidence of S. aureus and E. coli did not show a major temporal change after the start of the COVID-19 pandemic. Meanwhile, the slight increase in overall infections shown in Fig. 1C may be attributable to E. coli, which shows a similar pattern, rather than to S. aureus. In contrast, the incidence of S. pneumoniae dropped significantly from April 2020 onward. Significant declines in the incidence of respiratory infectious diseases were reported in 2020 and were associated with nonpharmaceutical interventions such as mask wearing, hand hygiene, and social restrictions implemented during the pandemic [10]; the observed decrease in the incidence of S. pneumoniae infections shown in Fig. 1D is consistent with those previously reported changes.
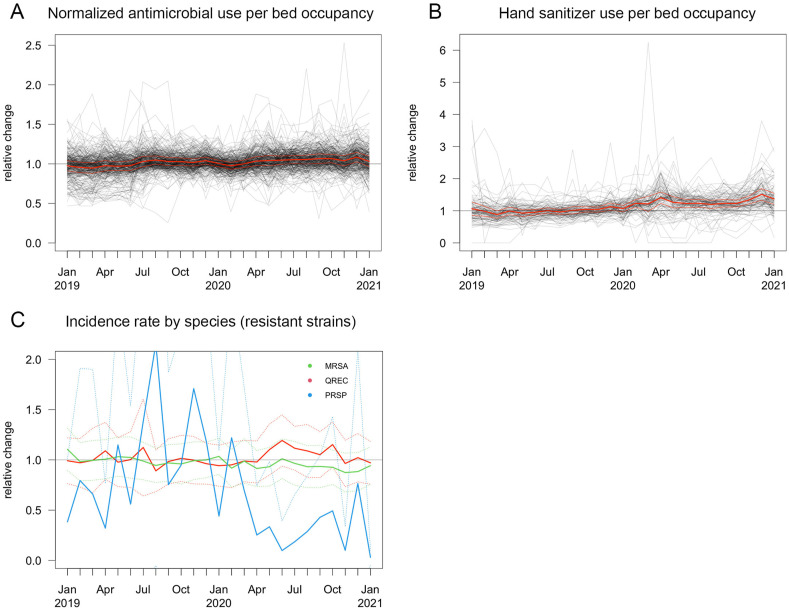
Antimicrobial use measured in antimicrobial use density (i.e., antimicrobial use per bed occupancy normalised by the defined daily dose) [11] showed a weak increasing trend in 2020 (Fig. 2 A). Institutional hand sanitiser use increased by about 50% in 2020 compared with 2019 (Fig. 2B); however, because there was also a weak increasing trend in hand sanitiser use at the end of 2019, some of the increase in 2020 may be attributable to changes not necessarily associated with the COVID-19 pandemic. The time trend in the selected antimicrobial-resistant strains, methicillin-resistant S. aureus, quinolone-resistant E. coli, and penicillin-resistant S. pneumoniae, showed similar trends to the overall incidence of each species (Fig. 2C).
Fig. 2.
Relative change in antimicrobial use, hand sanitiser use, and detection of resistance strains by institution. (A) Monthly antimicrobial use density (i.e., microbial use per bed occupancy normalised by defined daily dose); (B) Hand sanitiser use per bed occupancy; (C) Incidence rate of selected resistant strains per bed occupancy. Institution-level outcome variables (shown in grey lines) were summarised as a monthly mean of relative values, where the yearly average over January–December 2019 was used as a baseline (relative value of 1). Red lines in (A) and (B) and coloured lines in (C) indicate the mean and 95% confidence interval among the included institutions. MRSA, methicillin-resistant S. aureus; QREC, quinolone-resistant E. coli; PRSP, penicillin-resistant S. pneumoniae
Our results suggested that the apparent decrease in the incidence of microbial infections in 2020 was likely driven primarily by the decrease in bed occupancy and that the incidence of these infections was rather constant or even slightly increased after adjusting for bed occupancy. The major microbial species S. aureus and E. coli did not show a major change in incidence between 2019 and 2020, whether analysing all or only the antimicrobial-resistant strains, whereas the incidence of S. pneumoniae dramatically decreased in April 2020 onward as stringent non-pharmaceutical interventions against COVID-19 were being implemented. In sum, the impact of the COVID-19 pandemic on microbial infections may have been limited mostly to the decrease in bed occupancy and the prevalence of respiratory-associated pathogens but not necessarily to the prevalence of general pathogens. We did not find evidence of a major change in antimicrobial use per bed occupancy associated with the COVID-19 pandemic. The national antimicrobial sales data showed a 20% reduction between 2019 and 2020 [12], which may have been driven by reduced hospitalizations but not necessarily by changes in clinical practice. The use of hand sanitiser at medical facilities increased significantly, but its impact on the incidence of microbial infections was unclear.
It should be noted that our analysis was based on aggregated data at the institutional level and thus did not allow for detailed investigations of temporal changes and their possible causes that require individual-level records (e.g., age-stratification, cause of hospitalisation, underlying health conditions). This also means that some of reported organisms can be regarded as colonization then therefore there is a potential overestimation of the incidence to some extent. Because not all outcomes are necessarily reported by the included institutions, some of the results may be subject to selection bias. The majority of the detected microbial infections included in the dataset were bloodstream infections, which may not necessarily be representative of prevalence in other infection sites. Moreover, our analysis was limited to inpatient settings and may not be generalizable to outpatient settings, although similar trends (i.e., no change in S. aureus or E. coli and a decrease in S. pneumoniae) were reported in outpatient settings between 2019 and 2020 [13]. Regardless, the observed patterns of the impact of the COVID-19 pandemic on AMR-related metrics—in particular, the relatively stable per-bed incidence of microbial infections except for S. pneumoniae despite various social and epidemiological impacts associated with the pandemic—might provide potential clues for the future planning of AMR management.
Author contributions
ST and NO conceived the study. YA, TT, ME, TA, NM, and HI collected the data. AE and YA curated the data. AE analysed the data. AE, ST and YA interpreted the results. AE wrote the first draft of the manuscript and all other authors critically reviewed it. All authors approved the final version of the manuscript.
Declaration of competing interest
AE received a research grant from Taisho Pharmaceutical Co., Ltd. for research outside this study. ST received payment for supervising medical articles from Gilead Sciences, Inc. outside this study.
Acknowledgment
This study was supported by Ministry of Health, Labour and Welfare Research Grant (20HA2003), a Grant-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Science (22K17329 to AE) and a JSPS Overseas Research Fellowship (to AE).
References
- 1.Friedrich M.J. WHO's top health threats for 2019. JAMA. 2019;321:1041. doi: 10.1001/jama.2019.1934. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Global action plan on antimicrobial resistance. 2015. https://www.who.int/publications-detail-redirect/9789241509763 [DOI] [PubMed]
- 3.AMR Clinical Reference Center. National Center for Global Health and Medicine . 2019. Japan surveillance for infection prevention and healthcare Epidemiology (J-SIPHE) annual report. 2020. [Google Scholar]
- 4.Knight G.M., Glover R.E., McQuaid C.F., Olaru I.D., Gallandat K., Leclerc Q.J., et al. Antimicrobial resistance and COVID-19: intersections and implications. Elife. 2021;10 doi: 10.7554/eLife.64139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rezel-Potts E., L'Esperance V., Gulliford M.C. Antimicrobial stewardship in the UK during the COVID-19 pandemic: a population-based cohort study and interrupted time-series analysis. Br J Gen Pract. 2021;71 doi: 10.3399/BJGP.2020.1051. e331–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeon K., Jeong S., Lee N., Park M.-J., Song W., Kim H.-S., et al. Impact of COVID-19 on antimicrobial consumption and spread of multidrug-resistance in bacterial infections. Antibiotics. 2022;11:535. doi: 10.3390/antibiotics11040535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mareș C., Petca R.-C., Petca A., Popescu R.-I., Jinga V. Does the COVID pandemic modify the antibiotic resistance of uropathogens in female patients? A new storm? Antibiotics. 2022;11:376. doi: 10.3390/antibiotics11030376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poolman J.T., Anderson A.S. Escherichia coli and Staphylococcus aureus: leading bacterial pathogens of healthcare associated infections and bacteremia in older-age populations. Expert Rev Vaccines. 2018;17:607–618. doi: 10.1080/14760584.2018.1488590. [DOI] [PubMed] [Google Scholar]
- 9.Feldman C., Anderson R. The role of Streptococcus pneumoniae in community-acquired pneumonia. Semin Respir Crit Care Med. 2016;37:806–818. doi: 10.1055/s-0036-1592074. [DOI] [PubMed] [Google Scholar]
- 10.Hibiya K., Iwata H., Kinjo T., Shinzato A., Tateyama M., Ueda S., et al. Incidence of common infectious diseases in Japan during the COVID-19 pandemic. PLoS One. 2022;17 doi: 10.1371/journal.pone.0261332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoshida J., Harada Y., Kikuchi T., Asano I., Ueno T., Matsubara N. Does antimicrobial use density at the ward level influence monthly central line-associated bloodstream infection rates? Infect Drug Resist. 2014;7:331–335. doi: 10.2147/IDR.S74347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.AMR Clinical Reference Center. National Center for Global Health and Medicine hospital . 2022. National antimicrobial sales data: report of data from 2021 survey. April 22, 2022 Release. [Google Scholar]
- 13.Ministry of Health. Labour and Welfare [Japan nosocomial infections surveillance open reports] (Japanese) 2020. https://janis.mhlw.go.jp/report/kensa.html