Abstract
The current study uses data surveyed with 2,500 respondents during August and September 2021 in Vietnam, Indonesia, the Philippines and Malaysia to examine the willingness to get vaccinated against SARS-CoV-2 virus with six COVID-19 vaccines. The willingness to get vaccinated varies according to the vaccine brands and selected influential factors. Particularly, the percentage of respondents who are willing to get vaccinated with Pfizer, Moderna and AstraZeneca dominates that of those who are willing to get vaccinated with Sinopharm, Janssen and Sputnik V vaccines. Results generated from the binary logistic regressions show that the impact of the selected influential factors on the willingness to get vaccinated varies in terms of magnitude and direction, and depending on the vaccine brands. The results indicate that additional scientific evidence on the efficacy and safety of the vaccines is essential for the respondents to decide whether to vaccinate or not. Such evidence can be made available in multiple formats and provided through appropriate channels and vaccination communication campaigns.
Keywords: Willingness to get vaccinated, COVID-19 pandemic, SARS-CoV-2 virus, Vaccine brands
Introduction
COVID-19 was declared a global pandemic in March 2020 (WHO, 2020b). However, the first case was detected on 30th December 2019 (WHO, 2020a). Eight months later (when the surveys to collect data for the current study began), the pandemic spread to all continents and negatively influenced every aspect of people’s lives worldwide. For example, the pandemic was blamed for a global GDP loss of approximately 6.7 per cent (approximately four USD trillion) in 2020 (Statista, 2021). Seriously, 211,647,672 people were infected with the SARS-CoV-2 virus and it took 4,429,460 lives during the period (Worldometer, 2021). A number of approaches have been applied to stop the pandemic and among those was vaccination. COVID-19 vaccines have been proven to help slow down the spread of the virus and ultimately stop it by creating herd immunity. Therefore, the vaccines are recommended by the World Health Organisation (WHO) and several governments (Worldometer, 2021). Although the COVID-19 vaccines are said to help stop the pandemic, numerous people hesitate to get vaccinated due to various concerns such as vaccine safety, immunity, efficacy and the waiting time between two vaccine shots. These characteristics differ from vaccine to vaccine (Amit et al., 2022; Fiolet et al., 2021). The hesitation may prevent us from reaching herd immunity to stop the pandemic. This hesitation also creates opportunities for more deathly variants such as Delta (WHO, 2021b) or Omicron (WHO, 2021a) to emerge and will be harder to deal with. Vietnam, Indonesia, the Philippines and Malaysia are among Southeast Asian countries where the cases and deaths caused by the pandemic are highest and the vaccine coverage is lowest when the Delta variant of SARS-CoV-2 virus emerged. In addition, these are the countries that do not have the initiative to source vaccines. There have been a number of studies examining the willingness to vaccinate with different vaccine origins. For example, Schwarzinger et al. (2021) found that vaccines that are manufactured in the EU had the highest acceptance while those produced in China had the lowest acceptance. Similarly, Kreps et al. (2020) found that vaccines that originated in China had the lowest acceptance, followed by those manufactured in the UK. Those that originated in the US and were recommended by CDC had the highest acceptance. Wang et al. (2021) examined the willingness among working-age people to vaccinate with BioNTech (Pfizer), AstraZeneca and Sinovac (used as reference) in Hong Kong, China. However, there are COVID-19 vaccines that have the same origin such as the US, China or Russia but have different characteristics. Therefore, the willingness to vaccinate with these vaccines should not be identical. In addition, vaccinating a group of people may not be able to create herd immunity to stop the pandemic. Also, at the time of the study, six COVID-19 vaccine brands were approved and recommended in the study countries. They are Pfizer, Moderna, AstraZeneca, Sinopharm, Janssen and Sputnik V. The current study endeavours to examine the willingness to vaccinate against the SARS-CoV-2 virus with different vaccine brands. In addition, it examines the impact of influential factors on the willingness. These analyses are believed to have not been conducted previously.
Research Design, Methodology and Models
Study Design
Selection of Study Locations
Four countries where the cases and deaths caused by the pandemic are highest and the vaccine coverage is lowest in Southeast Asia are selected. These include Vietnam, Indonesia, the Philippines and Malaysia.
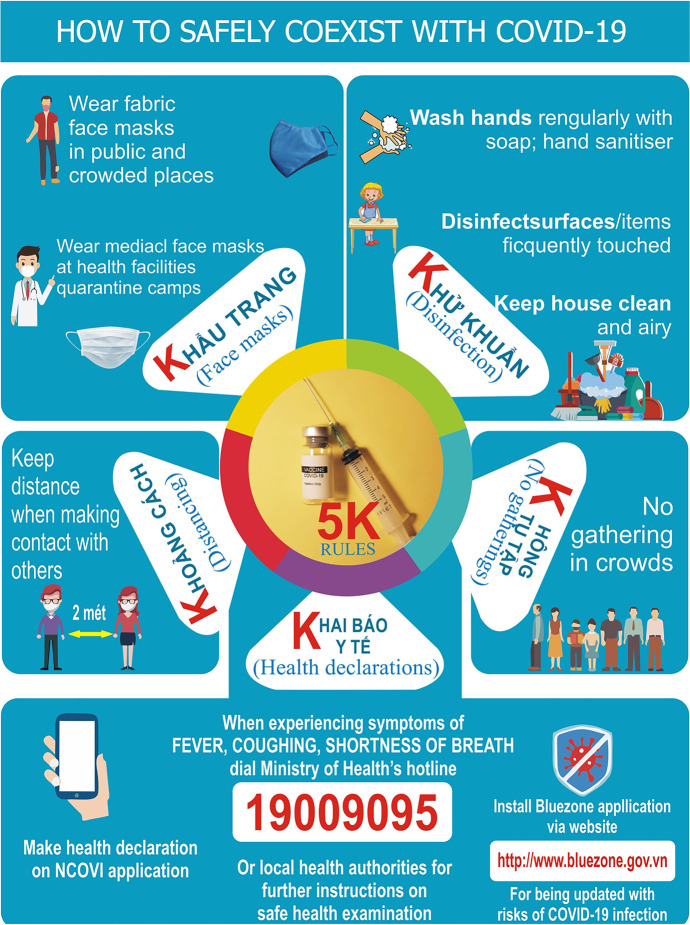
Vietnam is a good case to be selected for the study for the following reasons: it has successfully dealt with the pandemic in the first three waves by applying the 5 K (in Vietnamese) rules/practices/messages. The rules include Mask-wearing (Khau trang), Disinfection (Khu khuan), Social distancing (Khoang cach), No gathering (Khong tu tap dong nguoi) and Health declaration (Khai bao y te). It can be seen that vaccination had not been among the recommended rules or practices (MoH, 2020).
In the fourth wave of the pandemic that occurred in April 2021 with the emergence of the new variant—Delta (more contagious, more fatal and faster spread speed), the former approaches (quick track of F0, quarantine or lockdown etc.) are not sufficiently applicable and useful anymore. In the meantime, the vaccination campaigns had not started in the four countries due to some reasons such as the shortage of the vaccine supplies, responses of the governments (Hartanto & Siregar, 2021; Radjab & Fuady, 2021) and hesitancy of citizens to vaccinate with different vaccine brands (Amit et al., 2022). Consequently, the outbreak appeared to be out of control. Particularly, the number of cases and deaths caused by the pandemic in the nation between 27 April 2021 and 27 August 2021 dramatically increased while the COVID-19 vaccination coverage was modest as shown in Table 1 (Our World in Data, 2021). In addition, Arifin et al. (2021) showed that the number of deaths caused by SARS-CoV-2 of Malaysian adults who were unvaccinated significantly dominated that of those who were partially or fully vaccinated. Recognising the importance of the vaccines, vaccination has been added to the strategy to deal with the pandemic in Vietnam as illustrated in Fig. 1.
Table 1.
The total cases, deaths caused by SARS-CoV- and vaccination coverage in the study countries
| Country | Dates | Total cases | Total deaths | Total vaccinations per hundred | People vaccinated per hundred | People fully vaccinated per hundred |
|---|---|---|---|---|---|---|
| Indonesia | 27/04/21 | 1,651,794.00 | 44,939.00 | 6.93 | 4.34 | 2.60 |
| Indonesia | 27/08/21 | 4,056,354.00 | 130,781.00 | 34.21 | 21.87 | 12.35 |
| Malaysia | 27/04/21 | 398,451.00 | 1,462.00 | 4.23 | 2.60 | 1.63 |
| Malaysia | 27/08/21 | 1,662,913.00 | 15,550.00 | 104.22 | 59.74 | 44.49 |
| Philippines | 27/04/21 | 1,013,618.00 | 16,916.00 | 1.63 | 1.41 | 0.22 |
| Philippines | 27/08/21 | 1,916,461.00 | 32,841.00 | 28.31 | 16.84 | 12.04 |
| Vietnam | 27/04/21 | 2,857.00 | 35.00 | 0.32 | 0.32 | 0.01 |
| Vietnam | 27/08/21 | 410,366.00 | 10,053.00 | 19.51 | 17.14 | 2.37 |
Illustrated by the authors using Our World in Data (2021)
Fig. 1.
The 5 K Messages and Vaccination to Safely Co-exist with COVID-19. Source. The Vietnamese Ministry of Health (MoH, 2020)
Sampling
Since the dependent variables are binary, logistic regression is applied. The sample size is calculated based on the following formula (Bujang et al., 2018):
| 1 |
where
x is an integer that represents the event per variable, and i is the number of independent variables. The integer is recommended to be 50. Since the number of independent variables used in the current study is 48, the sample size is 2,500. During the study period, COVID-19 vaccines were administered to people aged between 18 and 64, then the vaccine coverage expanded to other age groups. The reason is that between the vaccine shots, there should be time to wait (for the next shot). The waiting time is different from vaccine brand to vaccine brand. To save the vaccines and time, people in other age groups (such as older and younger people) and those who were less vulnerable would be vaccinated if vaccines are available. Therefore, the sample was mainly taken from these age groups with few exceptions.
Google Forms were used to design the questionnaires. The questionnaires included questions to collect data on the willingness to vaccinate and the drivers of the willingness of the respondents. Particularly, the respondents were asked if they would be willing to vaccinate with the vaccine brands (Pfizer, Moderna, AstraZeneca, Sinopharm, Janssen and Sputnik V). Links containing information on the vaccine brands were provided in the questionnaires. The options included “Willing”, “Unwilling” and neutral options such as “I do not know” or “I am not sure”. The questionnaires were translated into local languages, which are Filipino, Indonesian, Malaysian and Vietnamese. The links to questionnaires were then distributed using email, Facebook, Twitter, Zalo, Viber and Whatsapp to survey. The data in Indonesia were collected between 28th August 2021 and 11th September 2021, those in the Philippines were collected between 27th August 2021 and 16th September 2021, those in Vietnam were collected between 16th August 2021 and 27th August 2021 and those in Malaysia were collected during 16th August 2021 and 14th September 2021.
Research Methodologies, Models and Variable Description
The respondents were asked if they would be willing to get vaccinated with different COVID-19 vaccine brands. The options include: “willing to get vaccinated”, “hesitant to get vaccinated” and “unwilling to get vaccinated”. Those who are hesitant to vaccinate tend to not vaccinate unless they perceive that the vaccines and vaccination is safe and necessary. Results generated from logistic regressions with binary outcomes (willing/unwilling) appear to be simpler to interpret for the researchers and easier to understand for the readers. Therefore, “hesitant to get vaccinated” and “unwilling to get vaccinated” responses are grouped and coded as 0. Since the dependent variables are in binary format (1 = willing to get vaccinated against SARS-CoV-2 virus with different vaccine brands, 0 = unwilling to get vaccinated), a binary regression specification is applied (Wooldridge, 2012). The independent variables are selected or modified based on previous studies, especially those reviewed in the current study. Based on previous studies, there are approximately 45 factors/independent variables that can influence the willingness of the respondents to vaccinate. The full model is briefly described in Eq. 2.
| 2 |
where
Yi is the willingness to get vaccinated (with different vaccine brands) against SARS-CoV-2 virus of the ith respondent. At the time of the current study, five COVID-19 vaccine brands, including Pfizer (Y1i, 1 = willing), Moderna (Y2i, 1 = willing), AstraZeneca (Y3i, 1 = willing), Sinopharm (Y4i, 1 = willing), Janssen (Y5i, 1 = willing) and Sputnik V (Y6i, 1 = willing) are examined in the current study. These vaccines were available and approved in the four countries by the time of the study. There are also other vaccines like Sinovac, but not included in the current study due to reasons such as unavailability or unapproved. As previously addressed, there are vaccines that have the same origin, but different characteristics. Therefore, preferences for these vaccines may not be identical and should be further examined (Al-Mistarehi et al., 2021; CDC, 2021b; Kawata & Nakabayashi, 2021).
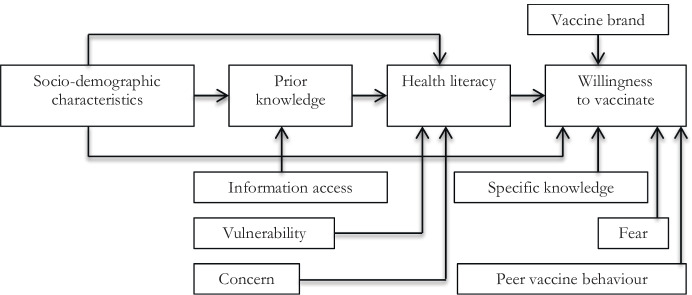
The willingness to get vaccinated against SARS-CoV-2 virus of people with different social and economic demographic characteristics may not be identical. The social and economic demographic characteristics in the current study include age, gender, residency, marital status, family main income source, savings, gold assets, the number of dependants, education and employment of the respondents. Particularly, the age is denoted as X1 and is measured in years. The gender is denoted as X2 (1 = male). The residency is denoted as X3 (1 = urban). The marital status is denoted as X4 (1 = married or cohabited). If the respondent is the main income source of the family (denoted as X5), it is coded 1 = yes, otherwise. Similarly, if the respondent has savings (demoted as X6), it is coded 1 = yes, otherwise. If the respondent has gold assets (denoted as X7, it is coded 1 = yes, otherwise. The number of dependants is coded as X8 (measured in persons). The education is denoted as X9 (1 = tertiary or above). If the respondent is employed/working (denoted as X10), it is coded 1 = employed, otherwise. Old people normally possess better knowledge, including that of the pandemic and virus, hence are expected to be more likely to vaccinate than their younger counterparts. However, they may have comorbidities that make them hesitant to vaccinate. In addition, younger people are believed to be better social media users where they can be faster updated with news on the pandemic and virus, hence are expected to be more likely to vaccinate as well. Therefore, the impact of the respondent’s age on the willingness to get vaccinated can be mixed. People with a higher education level are expected to be more likely to vaccinate than a person with a lower level of education. Urban areas are normally more crowded, hence posing more risks (such as being infected with the virus) than rural areas. In addition, urban residents are believed to have better access to information on the pandemic and vaccines than rural residents. Therefore, urban residents are expected to be more likely to get vaccinated than their counterparts residing in rural areas. A person with more family responsibilities or responsibilities at work such as a married or cohabited person or a person who earns the main income for the family or a person with a dependant to look after or an employed person is expected to be more likely to vaccinate than a person with fewer family responsibilities. The willingness to vaccinate with different vaccine brands between males and females may not be identical, but difficult to predict. Similarly, the willingness to vaccinate with different vaccine brands between people with and without savings or gold assets should not be the same, but unpredictable (Abedin et al., 2021; Al-Mistarehi et al., 2021; Chew et al., 2021; Daly & Robinson, 2021; Dodd et al., 2021; Edwards et al., 2021; Freeman et al., 2020; Kawata & Nakabayashi, 2021; Kelly et al., 2021; Kessels et al., 2021; Khubchandani et al., 2021; Kourlaba et al., 2021; Liu & Li, 2021; Neumann-Böhme et al., 2020; Schwarzinger et al., 2021; Yoda & Katsuyama, 2021). Additionally, the willingness to get vaccinated against the SARS-CoV-2 virus of people with the national health insurance (X11, 1 = national health insurance member) or private health insurance (X12, 1 = private health insurance member) and that of those without the insurance is anticipated not to be the same. Since premiums and benefits of national and private insurance are not the same, it is necessary to examine the preferences of the COVID-19 vaccines among the insurance beneficiaries (Chew et al., 2021; Dodd et al., 2021; Kelly et al., 2021). The information access (to be updated with news on the pandemic and vaccines) is believed to help people gain a better and sufficient understanding of the pandemic and vaccines, hence is expected to have an impact on the willingness to get vaccinated. Particularly, people with better information access or sufficient information are expected to be more likely to vaccinate with a better vaccine brand (safer, a higher level of immunity). In the current study, the access is represented by the number of information channels to receive news on the pandemic (X13, measured in channels) and news on the vaccines (X14, measured in channels), the frequency to receive news on the pandemic (X15, 1 = daily, 0 = otherwise) and news on the vaccines (X16, 1 = daily, 0 = otherwise), the sufficiency of news on the pandemic (X17, 1 = sufficient) and on the vaccines (X18, 1 = sufficient). Vulnerable people tend to seek protection like vaccines. In the current study, a person is considered as vulnerable if he or she belongs to the vaccine priority groups (X19, 1 = yes) (VNVC, 2021) or lives with someone who belongs to these groups (X20, 1 = yes) or has comorbidities (X21, 1 = yes) (CDC, 2021a), or has been infected with the virus (X29, 1 = yes) or has a close person such as a family member or co-worker friend who is infected with the SARS-CoV-2 virus (X30, 1 = yes). In particular, a respondent who belongs to the vaccine priority groups or lives with someone in these groups or whom has a family member/friend/co-worker infected with the virus is expected to be more likely to vaccinate. However, the willingness to vaccinate of a person with comorbidities or who has been infected with the virus is difficult to anticipate (Al-Mistarehi et al., 2021; Freeman et al., 2020; Kessels et al., 2021; Kourlaba et al., 2021; Schwarzinger et al., 2021). The willingness to get vaccinated of people with fear may not be identical to that of those without it. In the current study, it consists of the fear of being discriminated against (for example, being banned from travelling, entering crowded places such as malls or supermarkets or stadiums, or receiving government assistance) if not vaccinated (X31, 1 = fear, 0 = fearless), the fear of catching the virus (X32, 1 = fear, 0 = fearless) and the fear of needles (X33, 1 = fear, 0 = fearless). A person with the fear of being discriminated against if unvaccinated or fear of catching the virus is expected to be more likely to vaccinate. However, the willingness to vaccinate of a person with the fear of needles is difficult to predict (Kelly et al., 2021; Khubchandani et al., 2021; Neumann-Böhme et al., 2020; Yoda & Katsuyama, 2021). In contrast, people who are concerned about the vaccines and relevant matters tend to hesitate to get vaccinated. In the current study, the respondents were asked if they were concerned about the side effects (X35, 1 = concerned), safety (X38, 1 = concerned), immunity (X37, 1 = concerned) and cost (X40, 1 = concerned) of the vaccines. In addition, they were asked if concerned about the sufficiency of the official information on the vaccines (X34, 1 = concerned), the response procedure if a person faces a severe shock after being vaccinated (X36, 1 = concerned), the distance between the residency and vaccination site (X39, 1 = concerned), waiting time to vaccinate (X41, 1 = concerned), time frame to vaccinate (X42, 1 = concerned) and the safety of the vaccination waiting room (X43, 1 = concerned) (Abedin et al., 2021; Dodd et al., 2021; Kawata & Nakabayashi, 2021; Neumann-Böhme et al., 2020; Yoda & Katsuyama, 2021). Knowledge can help people gain a better and sufficient understanding of the pandemic and virus. A person with better and sufficient knowledge of the pandemic and virus is expected to be more likely to vaccinate than a person with poorer or insufficient knowledge (Dodd et al., 2021; Kelly et al., 2021; Kourlaba et al., 2021; Schwarzinger et al., 2021). In the current study, respondents were asked and tested if they have sufficient knowledge of common symptoms of people infected with the virus (X22, 1 = sufficient), on the virus transmission route (X23, 1 = sufficient), on the ways to prevent the virus (X24, 1 = sufficient), on the spread speed of the virus (X25, 1 = sufficient), on the virus fatality (X26, 1 = sufficient), on the herd immunity generated by there is at least 70 per cent of the population infected with the virus (X27, 1 = sufficient) and generated by there is at least 70 per cent of the population fully vaccinated (X28, 1 = sufficient) and on the common symptoms after getting vaccinated (X44, 1 = sufficient). Since socio-demographic characteristics of respondents, tradition and cultures, laws and regulations on vaccination and vaccine availability in the four countries are different, the willingness to vaccinate with different vaccine brands of the respondents may not be identical. A categorical variable is used to represent the nationality of the respondents in the four countries, which are Vietnamese (X45, 1 = Vietnamese), Indonesian (X45, 2 = Indonesian), Filipino (X45, 3 = Filipino) and Malaysian (X45, 4 = Malaysian). Vietnamese respondents are used as the base category, hence, regression results of this category are not shown. These factors are briefly illustrated in Fig. 2.
Fig. 2.
Conceptual framework on the willingness to get vaccinated with different COVID-19 vaccine brands. Source. Illustrated by the authors with ideas adapted from Sun et al. (2013)
Multicollinearity can cause the estimated coefficients to be biased. To inspect this issue, multicollinearity tests have been conducted and the mean variance inflation factor (VIF) is 3.0, which is remarkably lower than 10 (widely used in social science). Additionally, the correlation matrix shows no correlation coefficients greater than 5.2. These test results indicate that no serious issues of multicollinearity exist (Alin, 2010; Chong & Jun, 2005; Daoud, 2017; Farrar & Glauber, 1967; Graham, 2003; Mansfield & Helms, 1982; Schroeder et al., 1990).
Similarly, endogeneity can be another problem that makes the results of the study unreliable. Ideally, techniques such as instrumental variables (IV) or Two-stage Least Squares (2SLS) can be used to handle the endogeneity problem. However, an instrumental variable is not easy to find in reality (Bascle, 2008; Semadeni et al., 2014; Ullah et al., 2021). Similarly, the number of relevant variables that can be used to generate IVs for the 2SLS is not always sufficient (Fingleton & Le Gallo, 2010; Kelejian, 1971; Terza et al., 2008). These tasks are almost impossible in the context of the current study. To minimise the impact of this issue, the current study carefully follows previous studies to choose relevant variables.
To identify the most useful models, which use minimum factors/variables but can best explain the dependent variable/s (Box, 1976), tests on Akaike Information Criterion (AIC) were conducted using Stepwise model selection (Akaike, 1974; Anderson et al., 1998; Cavanaugh, 1997; Hurvich & Tsai, 1993; Ludden et al., 1994; Portet, 2020; Posada & Buckley, 2004; Shibata, 1976; Vrieze, 2012). Particularly, the full model with all relevant independent variables (45 variables) collected was regressed using the logistics regression. Then, the backward method was applied to eliminate irrelevant independent variables (Wang, 2000). The reduced models suggested by the AIC tests are presented after the Abbreviations.
Results and Discussion
Willingness to get Vaccinated Against SARS-CoV-2 Virus with Different Vaccine Brands
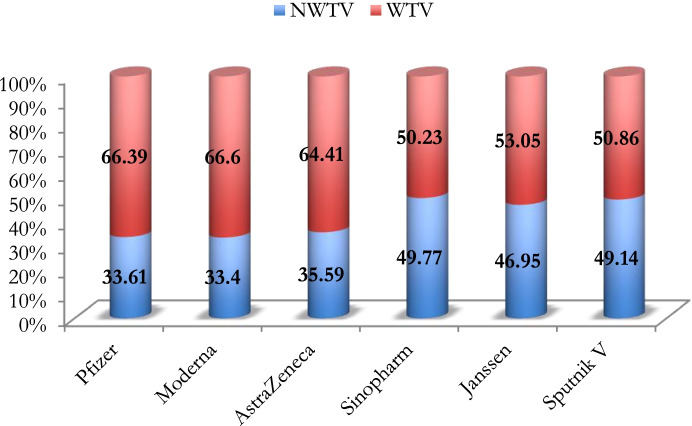
There are 450 (account for 18 per cent) neutral responses such as “I do not know” or “I am not sure” and these responses are classified as “hesitant to vaccinate” and grouped with those who are unwilling to vaccinate as previously addressed in the section of methodology. Overall, the percentage of respondents who are willing to get vaccinated with all vaccine brands dominates that of those who are not willing. In addition, Pfizer, Moderna and AstraZeneca vaccines are among the most preferred brands by the respondents (Fig. 3).
Fig. 3.
The willingness (measured in per cent) to get vaccinated with different vaccine brands. Source. Drawn by the authors using the surveyed data. Note. WTV: Willing to get vaccinated, NWTV: Not willing to get vaccinated
Details of the percentage of respondents who are willing to get vaccinated with different vaccine brands are shown in Table 2. Results in Table 2 show that Pfizer, Moderna and AstraZeneca are among the most preferred vaccines by the targeted age groups. Particularly, the percentage of respondents who are willing to get vaccinated with Pfizer, Moderna and AstraZeneca vaccines dominates that of those who are not willing.
Table 2.
Willingness to get vaccinated against SARS-CoV-2 virus with different vaccine brands
| Variable | Unit/ measures |
Total (%) |
Pfizer (%) | Moderna (%) | AstraZeneca (%) | Sinopharm (%) | Janssen (%) | Sputnik V (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NWTV 1 | WTV 2 | NWTV | WTV | NWTV | WTV | NWTV | WTV | NWTV | WTV | NWTV | WTV | |||
| X13 | 13–17 | 1.0 | 57.9 | 42.1 | 52.6 | 47.4 | 57.9 | 42.1 | 68.4 | 31.6 | 63.2 | 36.8 | 63.2 | 36.8 |
| 18–24 | 26.3 | 31.5 | 68.5 | 32.3 | 67.7 | 38.0 | 62.0 | 55.6 | 44.4 | 47.9 | 52.1 | 56.0 | 44.0 | |
| 25–34 | 26.9 | 32.3 | 67.7 | 31.1 | 68.9 | 32.1 | 67.9 | 43.5 | 56.5 | 42.7 | 57.3 | 43.9 | 56.1 | |
| 35–44 | 29.0 | 30.2 | 69.8 | 30.0 | 70.0 | 31.2 | 68.8 | 46.0 | 54.0 | 45.2 | 54.8 | 43.6 | 56.4 | |
| 45–54 | 13.0 | 42.4 | 57.6 | 42.8 | 57.2 | 42.0 | 58.0 | 54.8 | 45.2 | 52.8 | 47.2 | 53.2 | 46.8 | |
| 55–64 | 2.8 | 33.3 | 66.7 | 29.4 | 70.6 | 33.3 | 66.7 | 49.0 | 51.0 | 49.0 | 51.0 | 52.9 | 47.1 | |
| 65–81 | 1.0 | 85.0 | 15.0 | 90.0 | 10.0 | 90.0 | 10.0 | 90.0 | 10.0 | 85.0 | 15.0 | 90.0 | 10.0 | |
| X2 | 0 | 67.2 | 34.1 | 65.9 | 32.6 | 67.4 | 34.7 | 65.3 | 49.1 | 50.9 | 47.0 | 53.0 | 49.5 | 50.5 |
| 1 | 32.8 | 32.5 | 67.5 | 35.1 | 64.9 | 37.5 | 62.5 | 51.1 | 48.9 | 46.8 | 53.2 | 48.4 | 51.6 | |
| X3 | 0 | 42.7 | 26.9 | 73.1 | 27.5 | 72.5 | 32.2 | 67.8 | 50.3 | 49.7 | 45.1 | 54.9 | 50.4 | 49.6 |
| 1 | 57.3 | 38.6 | 61.4 | 37.8 | 62.2 | 38.1 | 61.9 | 49.4 | 50.6 | 48.4 | 51.6 | 48.2 | 51.8 | |
| X4 | 0 | 40.3 | 35.2 | 64.8 | 34.7 | 65.3 | 40.1 | 59.9 | 56.1 | 43.9 | 49.3 | 50.7 | 56.1 | 43.9 |
| 1 | 59.7 | 32.5 | 67.5 | 32.5 | 67.5 | 32.5 | 67.5 | 45.5 | 54.5 | 45.4 | 54.6 | 44.4 | 55.6 | |
| X5 | 0 | 45.4 | 36.7 | 63.3 | 35.7 | 64.3 | 40.4 | 59.6 | 55.5 | 44.5 | 51.8 | 48.2 | 57.1 | 42.9 |
| 1 | 54.6 | 31.0 | 69.0 | 31.5 | 68.5 | 31.6 | 68.4 | 45.0 | 55.0 | 42.9 | 57.1 | 42.6 | 57.4 | |
| X6 | 0 | 39.2 | 38.3 | 61.7 | 39.4 | 60.6 | 39.0 | 61.0 | 50.5 | 49.5 | 46.0 | 54.0 | 47.3 | 52.7 |
| 1 | 60.8 | 30.6 | 69.4 | 29.6 | 70.4 | 33.4 | 66.6 | 49.3 | 50.7 | 47.6 | 52.4 | 50.3 | 49.7 | |
| X7 | 0 | 28.6 | 30.8 | 69.2 | 30.1 | 69.9 | 36.3 | 63.7 | 49.8 | 50.2 | 50.5 | 49.5 | 54.2 | 45.8 |
| 1 | 71.4 | 34.7 | 65.3 | 34.7 | 65.3 | 35.3 | 64.7 | 49.7 | 50.3 | 45.5 | 54.5 | 47.1 | 52.9 | |
| X8 | 0 | 11.5 | 38.6 | 61.4 | 39.5 | 60.5 | 44.1 | 55.9 | 54.1 | 45.9 | 45.9 | 54.1 | 51.4 | 48.6 |
| 1 | 88.5 | 33.0 | 67.0 | 32.6 | 67.4 | 34.5 | 65.5 | 49.2 | 50.8 | 47.1 | 52.9 | 48.9 | 51.1 | |
| X9 | 0 | 20.1 | 44.7 | 55.3 | 42.9 | 57.1 | 47.5 | 52.5 | 59.0 | 41.0 | 59.0 | 41.0 | 62.3 | 37.7 |
| 1 | 79.9 | 30.8 | 69.2 | 31.0 | 69.0 | 32.6 | 67.4 | 47.5 | 52.5 | 43.9 | 56.1 | 45.8 | 54.2 | |
| X10 | 0 | 25.6 | 34.8 | 65.2 | 35.0 | 65.0 | 40.1 | 59.9 | 57.2 | 42.8 | 52.1 | 47.9 | 58.7 | 41.3 |
| 1 | 74.4 | 33.2 | 66.8 | 32.8 | 67.2 | 34.0 | 66.0 | 47.2 | 52.8 | 45.2 | 54.8 | 45.9 | 54.1 | |
| X11 | 0 | 21.6 | 35.7 | 64.3 | 65.1 | 34.9 | 40.2 | 59.8 | 46.7 | 53.3 | 55.4 | 44.6 | 64.6 | 35.4 |
| 1 | 78.4 | 33.0 | 67.0 | 45.5 | 54.5 | 31.5 | 68.5 | 32.5 | 67.5 | 44.6 | 55.4 | 44.9 | 55.1 | |
| X12 | 0 | 60.0 | 34.2 | 65.8 | 33.6 | 66.4 | 38.0 | 62.0 | 50.8 | 49.2 | 48.2 | 51.8 | 51.5 | 48.5 |
| 1 | 40.0 | 32.7 | 67.3 | 33.1 | 66.9 | 32.0 | 68.0 | 48.2 | 51.8 | 45.1 | 54.9 | 45.6 | 54.4 | |
| X13 | < 46 | 14.1 | 22.2 | 77.8 | 19.6 | 80.4 | 21.9 | 78.1 | 38.9 | 61.1 | 37.8 | 62.2 | 37.8 | 62.2 |
| > = 56 | 85.9 | 35.5 | 64.5 | 35.7 | 64.3 | 37.8 | 62.2 | 51.5 | 48.5 | 48.5 | 51.5 | 51.0 | 49.0 | |
| X14 | < 6 | 11.7 | 22.3 | 77.7 | 20.1 | 79.9 | 22.8 | 77.2 | 40.6 | 59.4 | 40.2 | 59.8 | 39.3 | 60.7 |
| > = 6 | 88.3 | 35.1 | 64.9 | 35.2 | 64.8 | 37.3 | 62.7 | 51.0 | 49.0 | 47.8 | 52.2 | 50.4 | 49.6 | |
| X15 | 0 | 7.0 | 44.8 | 55.2 | 46.3 | 53.7 | 52.2 | 47.8 | 62.7 | 37.3 | 62.7 | 37.3 | 68.7 | 31.3 |
| 1 | 93.0 | 32.8 | 67.2 | 32.4 | 67.6 | 34.3 | 65.7 | 48.8 | 51.2 | 45.8 | 54.2 | 47.7 | 52.3 | |
| X16 | 0 | 11.3 | 36.4 | 63.6 | 33.6 | 66.4 | 38.7 | 61.3 | 53.9 | 46.1 | 53.9 | 46.1 | 58.5 | 41.5 |
| 1 | 88.7 | 33.3 | 66.7 | 33.4 | 66.6 | 35.2 | 64.8 | 49.2 | 50.8 | 46.1 | 53.9 | 47.9 | 52.1 | |
| X17 | 0 | 24.8 | 53.2 | 46.8 | 55.5 | 44.5 | 58.0 | 42.0 | 71.6 | 28.4 | 63.9 | 36.1 | 68.7 | 31.3 |
| 1 | 75.2 | 27.2 | 72.8 | 26.1 | 73.9 | 28.2 | 71.8 | 42.6 | 57.4 | 41.4 | 58.6 | 42.7 | 57.3 | |
| X18 | 0 | 27.3 | 50.9 | 49.1 | 52.2 | 47.8 | 54.9 | 45.1 | 69.6 | 30.4 | 63.5 | 36.5 | 67.7 | 32.3 |
| 1 | 72.7 | 27.1 | 72.9 | 26.4 | 73.6 | 28.4 | 71.6 | 42.3 | 57.7 | 40.8 | 59.2 | 42.2 | 57.8 | |
| X19 | 0 | 32.0 | 43.8 | 56.2 | 44.8 | 55.2 | 49.0 | 51.0 | 64.5 | 35.5 | 59.3 | 40.7 | 63.5 | 36.5 |
| 1 | 68.0 | 28.8 | 71.2 | 28.0 | 72.0 | 29.3 | 70.7 | 42.8 | 57.2 | 41.1 | 58.9 | 42.4 | 57.6 | |
| X20 | 0 | 51.2 | 40.6 | 59.4 | 41.1 | 58.9 | 43.0 | 57.0 | 58.0 | 42.0 | 53.8 | 46.2 | 56.2 | 43.8 |
| 1 | 48.8 | 26.3 | 73.7 | 25.3 | 74.7 | 27.9 | 72.1 | 41.1 | 58.9 | 39.8 | 60.2 | 41.7 | 58.3 | |
| X21 | 0 | 75.7 | 32.6 | 67.4 | 32.1 | 67.9 | 34.5 | 65.5 | 48.6 | 51.4 | 45.9 | 54.1 | 48.1 | 51.9 |
| 1 | 24.3 | 36.8 | 63.2 | 37.5 | 62.5 | 39.0 | 61.0 | 53.5 | 46.5 | 50.1 | 49.9 | 52.2 | 47.8 | |
| X22 | 0 | 30.1 | 34.0 | 66.0 | 33.6 | 66.4 | 36.2 | 63.8 | 51.8 | 48.2 | 50.3 | 49.7 | 52.5 | 47.5 |
| 1 | 69.9 | 33.5 | 66.5 | 33.3 | 66.7 | 35.3 | 64.7 | 48.9 | 51.1 | 45.5 | 54.5 | 47.7 | 52.3 | |
| X23 | 0 | 16.8 | 35.3 | 64.7 | 36.5 | 63.5 | 36.8 | 63.2 | 52.6 | 47.4 | 51.1 | 48.9 | 52.3 | 47.7 |
| 1 | 83.2 | 33.3 | 66.7 | 32.8 | 67.2 | 35.3 | 64.7 | 49.2 | 50.8 | 46.1 | 53.9 | 48.5 | 51.5 | |
| X24 | 0 | 42.3 | 27.6 | 72.4 | 28.1 | 71.9 | 28.4 | 71.6 | 44.3 | 55.7 | 40.9 | 59.1 | 39.6 | 60.4 |
| 1 | 57.7 | 38.0 | 62.0 | 37.3 | 62.7 | 40.9 | 59.1 | 53.8 | 46.2 | 51.4 | 48.6 | 56.1 | 43.9 | |
| X25 | 0 | 10.7 | 47.1 | 52.9 | 46.6 | 53.4 | 51.0 | 49.0 | 66.0 | 34.0 | 62.1 | 37.9 | 67.0 | 33.0 |
| 1 | 89.3 | 32.0 | 68.0 | 31.8 | 68.2 | 33.7 | 66.3 | 47.8 | 52.2 | 45.1 | 54.9 | 47.0 | 53.0 | |
| X26 | 0 | 8.5 | 52.1 | 47.9 | 52.8 | 47.2 | 57.7 | 42.3 | 67.5 | 32.5 | 67.5 | 32.5 | 70.6 | 29.4 |
| 1 | 91.5 | 31.9 | 68.1 | 31.6 | 68.4 | 33.5 | 66.5 | 48.1 | 51.9 | 45.0 | 55.0 | 47.2 | 52.8 | |
| X27 | 0 | 37.8 | 35.9 | 64.1 | 35.3 | 64.7 | 36.7 | 63.3 | 52.1 | 47.9 | 49.8 | 50.2 | 50.5 | 49.5 |
| 1 | 62.2 | 32.2 | 67.8 | 32.2 | 67.8 | 34.9 | 65.1 | 48.3 | 51.7 | 45.2 | 54.8 | 48.3 | 51.7 | |
| X28 | 0 | 29.2 | 56.3 | 43.8 | 57.1 | 42.9 | 58.8 | 41.3 | 69.1 | 30.9 | 64.3 | 35.7 | 69.1 | 30.9 |
| 1 | 70.8 | 24.3 | 75.7 | 23.6 | 76.4 | 26.0 | 74.0 | 41.8 | 58.2 | 39.8 | 60.2 | 40.9 | 59.1 | |
| X29 | 0 | 92.7 | 33.9 | 66.1 | 34.0 | 66.0 | 35.8 | 64.2 | 50.1 | 49.9 | 47.3 | 52.7 | 49.3 | 50.7 |
| 1 | 7.3 | 30.5 | 69.5 | 25.5 | 74.5 | 32.6 | 67.4 | 46.1 | 53.9 | 42.6 | 57.4 | 46.8 | 53.2 | |
| X30 | 0 | 32.5 | 27.9 | 72.1 | 26.3 | 73.7 | 33.5 | 66.5 | 45.7 | 54.3 | 45.9 | 54.1 | 51.8 | 48.2 |
| 1 | 67.5 | 36.3 | 63.7 | 36.8 | 63.2 | 36.6 | 63.4 | 51.7 | 48.3 | 47.5 | 52.5 | 47.8 | 52.2 | |
| X31 | 0 | 47.6 | 35.6 | 64.4 | 33.3 | 66.7 | 35.9 | 64.1 | 51.5 | 48.5 | 49.7 | 50.3 | 52.0 | 48.0 |
| 1 | 52.4 | 31.8 | 68.2 | 33.5 | 66.5 | 35.3 | 64.7 | 48.2 | 51.8 | 44.5 | 55.5 | 46.6 | 53.4 | |
| X32 | 0 | 25.4 | 37.7 | 62.3 | 37.1 | 62.9 | 41.4 | 58.6 | 59.6 | 40.4 | 56.1 | 43.9 | 58.8 | 41.2 |
| 1 | 74.6 | 32.2 | 67.8 | 32.1 | 67.9 | 33.6 | 66.4 | 46.4 | 53.6 | 43.8 | 56.2 | 45.8 | 54.2 | |
| X33 | 0 | 31.8 | 42.9 | 57.1 | 42.7 | 57.3 | 42.2 | 57.8 | 60.6 | 39.4 | 56.6 | 43.4 | 59.9 | 40.1 |
| 1 | 68.2 | 29.3 | 70.7 | 29.1 | 70.9 | 32.5 | 67.5 | 44.7 | 55.3 | 42.4 | 57.6 | 44.1 | 55.9 | |
| X34 | 0 | 11.6 | 73.1 | 26.9 | 74.4 | 25.6 | 75.3 | 24.7 | 85.7 | 14.3 | 81.6 | 18.4 | 85.2 | 14.8 |
| 1 | 88.4 | 28.4 | 71.6 | 28.0 | 72.0 | 30.4 | 69.6 | 45.0 | 55.0 | 42.4 | 57.6 | 44.4 | 55.6 | |
| X35 | 0 | 11.7 | 71.4 | 28.6 | 72.3 | 27.7 | 73.7 | 26.3 | 83.0 | 17.0 | 79.5 | 20.5 | 83.0 | 17.0 |
| 1 | 88.3 | 28.6 | 71.4 | 28.3 | 71.7 | 30.6 | 69.4 | 45.4 | 54.6 | 42.7 | 57.3 | 44.7 | 55.3 | |
| X36 | 0 | 11.0 | 73.6 | 26.4 | 74.1 | 25.9 | 75.5 | 24.5 | 84.4 | 15.6 | 80.2 | 19.8 | 84.4 | 15.6 |
| 1 | 89.0 | 28.6 | 71.4 | 28.4 | 71.6 | 30.6 | 69.4 | 45.5 | 54.5 | 42.8 | 57.2 | 44.8 | 55.2 | |
| X37 | 0 | 11.0 | 77.4 | 22.6 | 75.5 | 24.5 | 77.8 | 22.2 | 86.8 | 13.2 | 84.0 | 16.0 | 87.7 | 12.3 |
| 1 | 89.0 | 27.9 | 72.1 | 28.4 | 71.6 | 30.3 | 69.7 | 45.2 | 54.8 | 42.4 | 57.6 | 44.3 | 55.7 | |
| X38 | 0 | 10.3 | 75.6 | 24.4 | 78.7 | 21.3 | 79.2 | 20.8 | 86.8 | 13.2 | 83.8 | 16.2 | 87.3 | 12.7 |
| 1 | 89.7 | 28.8 | 71.2 | 28.2 | 71.8 | 30.6 | 69.4 | 45.5 | 54.5 | 42.7 | 57.3 | 44.8 | 55.2 | |
| X39 | 0 | 20.8 | 49.8 | 50.3 | 50.5 | 49.5 | 52.3 | 47.8 | 69.5 | 30.5 | 66.3 | 33.8 | 68.0 | 32.0 |
| 1 | 79.2 | 29.4 | 70.6 | 28.9 | 71.1 | 31.2 | 68.8 | 44.6 | 55.4 | 41.9 | 58.1 | 44.2 | 55.8 | |
| X40 | 0 | 23.9 | 44.1 | 55.9 | 44.1 | 55.9 | 45.2 | 54.8 | 62.7 | 37.3 | 59.8 | 40.2 | 61.1 | 38.9 |
| 1 | 76.1 | 30.3 | 69.7 | 30.0 | 70.0 | 32.6 | 67.4 | 45.7 | 54.3 | 42.9 | 57.1 | 45.4 | 54.6 | |
| X41 | 0 | 19.2 | 51.4 | 48.6 | 53.8 | 46.2 | 53.3 | 46.7 | 69.6 | 30.4 | 65.8 | 34.2 | 68.8 | 31.3 |
| 1 | 80.8 | 29.4 | 70.6 | 28.6 | 71.4 | 31.4 | 68.6 | 45.1 | 54.9 | 42.5 | 57.5 | 44.5 | 55.5 | |
| X42 | 0 | 18.6 | 50.7 | 49.3 | 54.1 | 45.9 | 52.9 | 47.1 | 70.6 | 29.4 | 66.4 | 33.6 | 68.1 | 31.9 |
| 1 | 81.4 | 29.7 | 70.3 | 28.7 | 71.3 | 31.6 | 68.4 | 45.0 | 55.0 | 42.5 | 57.5 | 44.8 | 55.2 | |
| X43 | 0 | 12.3 | 67.8 | 32.2 | 71.2 | 28.8 | 69.5 | 30.5 | 81.8 | 18.2 | 78.8 | 21.2 | 80.1 | 19.9 |
| 1 | 87.7 | 28.8 | 71.2 | 28.1 | 71.9 | 30.8 | 69.2 | 45.3 | 54.7 | 42.5 | 57.5 | 44.8 | 55.2 | |
| X44 | 0 | 20.1 | 37.1 | 62.9 | 38.2 | 61.8 | 39.5 | 60.5 | 55.1 | 44.9 | 51.9 | 48.1 | 52.2 | 47.8 |
| 1 | 79.9 | 32.7 | 67.3 | 32.2 | 67.8 | 34.6 | 65.4 | 48.4 | 51.6 | 45.7 | 54.3 | 48.4 | 51.6 | |
| X45 = 1 | 0 | N/A6 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 1 | 26.1 | 29.6 | 70.4 | 28.4 | 71.6 | 26.6 | 73.4 | 41.6 | 58.4 | 38.4 | 61.6 | 35.4 | 64.6 | |
| X45 = 2 | 0 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 1 | 26.7 | 30.7 | 69.3 | 24.0 | 76.0 | 30.9 | 69.1 | 40.2 | 59.8 | 46.1 | 53.9 | 50.8 | 49.2 | |
| X45 = 3 | 0 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 1 | 26.1 | 45.6 | 54.4 | 52.4 | 47.6 | 56.8 | 43.2 | 76.0 | 24.0 | 63.4 | 36.6 | 72.2 | 27.8 | |
| X45 = 4 | 0 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 1 | 21.2 | 27.5 | 72.5 | 28.0 | 72.0 | 26.5 | 73.5 | 39.6 | 60.4 | 38.3 | 61.7 | 35.6 | 64.4 | |
Calculated by the authors from the surveyed data
1Not willing to get vaccinated (NWTV), 2Willing to get vaccinated (WTV), 3Please refer to the Abbreviations for details, 4Fewer than and 5Equal to or greater than and 6Neither applicable nor available
The results show that the percentage of respondents with more work or family responsibilities such as females, married or cohabited respondents, respondents who earn the main income for the family, who have a dependant or who are employed and are willing to get vaccinated with all vaccine brands dominates that of those with fewer work or family responsibilities.
As previously addressed, due to population density, urban residents face more risks of being infected with the virus than rural residents. In addition, with better information access, urban residents are believed to be better aware of the risks than their counterparts in rural areas. As expected, the percentage of urban respondents who are willing to get vaccinated with all vaccine brands moderately dominates that of rural respondents.
The percentage of respondents with protection such as having national health insurance, savings and gold assets who are willing to get vaccinated with all vaccine brands dominates that of those without any protection. However, the percentage of respondents with private health insurance who are willing to get vaccinated with all vaccine brands is slightly lower than that of those without private health insurance.
The information access and sufficiency on the pandemic and vaccines can help people understand better the danger or fatality of the virus and the advantages of the vaccines. The information access in the current study is represented by the number of channels (12), the frequency (daily or not) that respondents receive the information and the information sufficiency (sufficient or insufficient) that they perceive. As expected, the percentage of respondents with better information access (such as having more channels—more than 6 out of 12 channels to receive the news on the pandemic and vaccines, daily receiving the information and perceiving that the information received is sufficient) who are willing to get vaccinated with all vaccine brands dominates that of those with incomplete information access or insufficient information.
The results show that the percentage of vulnerable respondents who are willing to get vaccinated with all vaccine brands dominates that of those who are not or less vulnerable. There are also exceptions. Particularly, the percentage of respondents with comorbidities who are willing to get vaccinated with all vaccine brands is relatively lower than that of those without the medical conditions. Obviously, the health conditions of those with comorbidities make them hesitate to vaccinate. In addition, the percentage of respondents who have never been infected with the virus and are willing to get vaccinated with all vaccine brands dominates that of those who have been infected. Perhaps, people think that after being infected and recovered they are immunized.
Owning better or sufficient knowledge can help people fully understand the risks of being infected with the virus and the advantages of getting vaccinated. The specific knowledge in the current study is represented by the symptoms of people infected with SARS-CoV-2 virus, the virus transmission route, the ways to prevent the virus, virus spread speed, virus mortality, herd immunity, and common symptoms after getting vaccinated. As anticipated, the percentage of respondents with higher education and sufficient knowledge who are willing to vaccinate with all vaccine brands dominates that of those with a lower education level and insufficient knowledge.
Fear usually forces people to seek protection. In the current study, it comprises of the fear of being infected with the virus, being discriminated against if unvaccinated, and needles. As anticipated, the percentage of respondents with fear who are willing to get vaccinated with all vaccine brands dominates that of those who are fearless. Despite the fear of needles, the percentage of respondents with this fear who are willing to get vaccinated with all vaccine brands still dominates that of those without fear. Perhaps, the fear of being infected with the virus outweighs that of needles.
As opposed to fear, if people are concerned or worried about something, they will be reluctant to proceed. The current study asks if the respondents are concerned or worried about the information sufficiency of the vaccine brands, the side effects of the vaccines, the vaccine immunity, the vaccine safety, the distance between their residency and the vaccination site, the vaccine cost, the time to wait to vaccinate, the vaccination time frame and the safety of the vaccination waiting room. The results show that the percentage of respondents who are not concerned about the above issues and are willing to get vaccinated with all vaccine brands dominates that of those who are concerned.
The willingness to get vaccinated can be affected by nationality. The percentage of Vietnamese and Malaysian respondents who are willing to get vaccinated with all vaccine brands dominates that of those who are not. In addition, the percentage of Indonesian respondents who are willing to get vaccinated with almost all vaccine brands (except the Sputnik V vaccine) dominates that of those who are not. In contrast, the percentage of Filipino respondents who are not willing to get vaccinated with almost all of the vaccine brands (except the Pfizer vaccine) dominates that of those who are willing.
The Impact of Influential Factors on the Willingness to get Vaccinated Against SARS-CoV-2 Virus
The impact of influential factors on the willingness to get vaccinated with different vaccine brands is examined using binary regressions. The regression results are presented in Table 3.
Table 3.
The impact of influential factors on the willingness to get vaccinated against SARS-CoV-2 virus
| Variable | Pfizer | Moderna | AstraZeneca | Sinopharm | Janssen | Sputnik V | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sig.1 | OR2 | Sig | OR | Sig | OR | Sig | OR | Sig | OR | Sig | OR | |
| X31 (ln4) | 0.002 | 0.472 | 0.002 | 0.534 | 0.002 | 0.483 | 0.001 | 0.479 | 0.000 | 0.475 | 0.000 | 0.431 |
| 95% CI5 | 0.295 | 0.755 | 0.362 | 0.789 | 0.305 | 0.766 | 0.307 | 0.746 | 0.333 | 0.679 | 0.276 | 0.674 |
| X2 | 0.028 | 1.335 | N/A6 | N/A | N/A | N/A | N/A | N/A | 0.082 | 1.225 | 0.018 | 1.328 |
| 95% CI | 1.031 | 1.729 | N/A | N/A | N/A | N/A | N/A | N/A | 0.974 | 1.540 | 1.051 | 1.680 |
| X3 | 0.000 | 1.944 | 0.000 | 1.679 | 0.001 | 1.456 | 0.762 | 1.033 | 0.016 | 1.291 | N/A | N/A |
| 95% CI | 1.527 | 2.474 | 1.323 | 2.132 | 1.161 | 1.826 | 0.837 | 1.276 | 1.049 | 1.588 | N/A | N/A |
| X4 | 0.088 | 1.328 | N/A | N/A | 0.106 | 1.291 | 0.042 | 1.367 | N/A | N/A | 0.128 | 1.261 |
| 95% CI | 0.958 | 1.841 | N/A | N/A | 0.947 | 1.759 | 1.012 | 1.846 | N/A | N/A | 0.936 | 1.700 |
| X5 | 0.054 | 1.327 | 0.027 | 1.352 | 0.013 | 1.388 | 0.029 | 1.327 | 0.009 | 1.392 | 0.006 | 1.436 |
| 95% CI | 0.995 | 1.770 | 1.036 | 1.766 | 1.071 | 1.799 | 1.030 | 1.710 | 1.086 | 1.785 | 1.110 | 1.858 |
| X6 | 0.005 | 1.412 | 0.002 | 1.497 | 0.006 | 1.408 | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | 1.109 | 1.798 | 1.166 | 1.921 | 1.102 | 1.798 | N/A | N/A | N/A | N/A | N/A | N/A |
| X7 | N/A | N/A | 0.047 | 0.747 | 0.003 | 0.668 | N/A | N/A | 0.026 | 0.762 | 0.024 | 0.762 |
| 95% CI | N/A | N/A | 0.560 | 0.997 | 0.512 | 0.872 | N/A | N/A | 0.600 | 0.968 | 0.602 | 0.964 |
| X8 | N/A | N/A | N/A | N/A | N/A | N/A | 0.017 | 0.921 | N/A | N/A | 0.007 | 0.911 |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | 0.860 | 0.985 | N/A | N/A | 0.852 | 0.975 |
| X9 | 0.558 | 1.094 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | 0.811 | 1.475 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X10 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X11 | 0.001 | 0.561 | N/A | N/A | N/A | N/A | 0.049 | 1.330 | N/A | N/A | 0.134 | 1.241 |
| 95% CI | 0.397 | 0.794 | N/A | N/A | N/A | N/A | 1.001 | 1.766 | N/A | N/A | 0.936 | 1.646 |
| X12 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X13 | 0.002 | 1.090 | 0.000 | 1.127 | 0.001 | 1.092 | 0.065 | 1.044 | N/A | N/A | 0.009 | 1.064 |
| 95% CI | 1.033 | 1.150 | 1.067 | 1.191 | 1.037 | 1.151 | 0.997 | 1.093 | N/A | N/A | 1.016 | 1.115 |
| X14 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X15 | N/A | N/A | 0.007 | 2.213 | 0.010 | 2.061 | N/A | N/A | 0.049 | 1.500 | 0.061 | 1.493 |
| 95% CI | N/A | N/A | 1.237 | 3.960 | 1.191 | 3.567 | N/A | N/A | 1.002 | 2.247 | 0.982 | 2.269 |
| X16 | N/A | N/A | 0.029 | 0.575 | 0.042 | 0.620 | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | 0.350 | 0.944 | 0.390 | 0.984 | N/A | N/A | N/A | N/A | N/A | N/A |
| X17 | 0.000 | 1.700 | 0.001 | 1.568 | 0.000 | 1.672 | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | 1.275 | 2.267 | 1.194 | 2.059 | 1.283 | 2.179 | N/A | N/A | N/A | N/A | N/A | N/A |
| X18 | N/A | N/A | N/A | N/A | N/A | N/A | 0.000 | 1.694 | 0.000 | 1.566 | 0.000 | 1.599 |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | 1.320 | 2.175 | 1.224 | 2.002 | 1.243 | 2.058 |
| X19 | 0.000 | 1.608 | 0.000 | 1.685 | 0.000 | 1.754 | 0.000 | 1.737 | 0.000 | 1.624 | 0.000 | 1.672 |
| 95% CI | 1.234 | 2.095 | 1.308 | 2.169 | 1.378 | 2.233 | 1.374 | 2.197 | 1.291 | 2.043 | 1.322 | 2.114 |
| X20 | 0.001 | 1.488 | 0.000 | 1.519 | 0.002 | 1.417 | 0.000 | 1.461 | 0.002 | 1.368 | 0.003 | 1.358 |
| 95% CI | 1.184 | 1.870 | 1.210 | 1.908 | 1.138 | 1.764 | 1.190 | 1.793 | 1.117 | 1.675 | 1.106 | 1.668 |
| X21 | 0.004 | 0.679 | 0.008 | 0.706 | 0.043 | 0.774 | 0.036 | 0.778 | 0.048 | 0.788 | 0.051 | 0.787 |
| 95% CI | 0.522 | 0.883 | 0.546 | 0.912 | 0.604 | 0.992 | 0.615 | 0.983 | 0.622 | 0.998 | 0.619 | 1.001 |
| X22 | N/A | N/A | 0.066 | 1.263 | 0.095 | 1.227 | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | 0.985 | 1.619 | 0.965 | 1.560 | N/A | N/A | N/A | N/A | N/A | N/A |
| X23 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X24 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X25 | N/A | N/A | N/A | N/A | N/A | N/A | 0.131 | 1.327 | N/A | N/A | 0.110 | 1.345 |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | 0.919 | 1.915 | N/A | N/A | 0.935 | 1.934 |
| X26 | 0.180 | 1.334 | N/A | N/A | 0.113 | 1.382 | N/A | N/A | 0.054 | 1.480 | N/A | N/A |
| 95% CI | 0.875 | 2.032 | N/A | N/A | 0.926 | 2.061 | N/A | N/A | 0.994 | 2.204 | N/A | N/A |
| X27 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 0.080 | 0.830 | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 0.673 | 1.023 | N/A | N/A |
| X28 | 0.000 | 2.411 | 0.000 | 2.432 | 0.000 | 2.212 | 0.000 | 1.712 | 0.001 | 1.541 | 0.000 | 1.826 |
| 95% CI | 1.852 | 3.140 | 1.879 | 3.146 | 1.721 | 2.844 | 1.336 | 2.195 | 1.203 | 1.974 | 1.424 | 2.341 |
| X29 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 0.052 | 1.469 |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 0.997 | 2.167 |
| X30 | 0.000 | 2.415 | 0.005 | 1.479 | 0.115 | 0.841 | 0.000 | 1.766 | 0.087 | 1.240 | N/A | N/A |
| 95% CI | 1.657 | 3.521 | 1.123 | 1.948 | 0.677 | 1.043 | 1.386 | 2.251 | 0.969 | 1.586 | N/A | N/A |
| X31 | 0.003 | 0.707 | 0.061 | 0.807 | N/A | N/A | 0.001 | 0.695 | 0.001 | 0.700 | 0.001 | 0.698 |
| 95% CI | 0.563 | 0.887 | 0.644 | 1.010 | N/A | N/A | 0.566 | 0.855 | 0.571 | 0.858 | 0.569 | 0.858 |
| X32 | N/A | N/A | N/A | N/A | N/A | N/A | 0.001 | 1.492 | 0.001 | 1.488 | 0.005 | 1.423 |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | 1.171 | 1.899 | 1.169 | 1.894 | 1.114 | 1.819 |
| X33 | 0.000 | 1.679 | 0.000 | 1.708 | 0.024 | 1.299 | 0.000 | 1.667 | 0.000 | 1.603 | 0.000 | 1.616 |
| 95% CI | 1.329 | 2.122 | 1.352 | 2.158 | 1.035 | 1.631 | 1.341 | 2.074 | 1.294 | 1.986 | 1.298 | 2.012 |
| X34 | 0.054 | 2.080 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | 0.986 | 4.388 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X35 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X36 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 0.088 | 0.498 | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 0.224 | 1.108 | N/A | N/A |
| X37 | 0.018 | 2.638 | 0.000 | 3.234 | 0.006 | 3.015 | 0.000 | 2.919 | 0.001 | 4.233 | 0.000 | 4.507 |
| 95% CI | 1.179 | 5.907 | 1.764 | 5.930 | 1.366 | 6.653 | 1.734 | 4.913 | 1.848 | 9.699 | 2.645 | 7.681 |
| X38 | N/A | N/A | N/A | N/A | 0.051 | 2.287 | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | 0.998 | 5.238 | N/A | N/A | N/A | N/A | N/A | N/A |
| X39 | N/A | N/A | N/A | N/A | N/A | N/A | 0.001 | 1.806 | 0.037 | 1.462 | 0.074 | 1.377 |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | 1.271 | 2.564 | 1.024 | 2.088 | 0.969 | 1.956 |
| X40 | 0.026 | 0.637 | 0.001 | 0.532 | 0.000 | 0.504 | 0.078 | 0.750 | 0.124 | 0.776 | 0.012 | 0.662 |
| 95% CI | 0.427 | 0.948 | 0.366 | 0.772 | 0.359 | 0.709 | 0.545 | 1.032 | 0.562 | 1.072 | 0.481 | 0.912 |
| X41 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X42 | 0.135 | 0.665 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | 0.389 | 1.136 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X43 | 0.047 | 2.012 | 0.001 | 2.645 | N/A | N/A | N/A | N/A | 0.067 | 1.719 | N/A | N/A |
| 95% CI | 1.010 | 4.009 | 1.486 | 4.710 | N/A | N/A | N/A | N/A | 0.963 | 3.067 | N/A | N/A |
| X44 | 0.129 | 1.253 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | 0.937 | 1.675 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X45 = 17 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X45 = 28 | 0.502 | 0.896 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | 0.650 | 1.235 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X45 = 39 | 0.000 | 0.351 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | 0.211 | 0.583 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| X45 = 410 | 0.385 | 0.821 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 95% CI | 0.525 | 1.282 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Constant | 0.408 | 0.513 | 0.037 | 0.234 | 0.207 | 0.373 | 0.070 | 0.248 | 0.093 | 0.333 | 0.136 | 0.310 |
| 95% CI | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
Calculated by the authors from the surveyed data
1Significance, 2Odds ratio, 3Please refer to the Abbreviations for details, 4Natural log, 5Confidence interval, 6Not available/applicable, 7Vietnamese respondents (serves as the base category/nationality), 8Indonesian respondents, 9Filipino respondents and 10Malaysian respondents
The results show that the older respondents (X1) are less likely to get vaccinated with all vaccine brands. The impact is significant at the one per cent level for all vaccine brands. This finding is almost in accordance with that found by Alley et al. (2021), Al-Mistarehi et al. (2021) and Dodd et al. (2021), but different from that discovered by Edwards et al. (2021), Freeman et al. (2020) and Kessels et al. (2021). One of the reasons that makes elderly people hesitate to vaccinate is their health. Literature shows that elderly people in the study countries face more health problems and are more vulnerable than those in developed countries (Buenaventura et al., 2020; Koris et al., 2017; MoH, 2018; Momtaz et al., 2010; Wulandari et al., 2019). The male participants (X2) are more likely to get vaccinated with Pfizer, Janssen and Sputnik V vaccines. The association is significant at the five per cent level for Pfizer and Sputnik V vaccines and ten per cent level for Janssen vaccine. As anticipated, urban residents (X3) are more likely to get vaccinated than their rural counterparts. Particularly, urban respondents are more likely to get vaccinated with Pfizer, Moderna, AstraZeneca and Janssen vaccines. The impact is significant at the one per cent level for Pfizer, Moderna and AstraZeneca vaccines, and at the five per cent level for the remaining vaccine. This finding is almost similar to that found by Abedin et al. (2021) and Yoda and Katsuyama (2021) though the vaccine brands were not examined. Married or cohabited respondents (X4) are more likely to get vaccinated with Pfizer and Sinopharm vaccines. This finding is in accordance with that found by Freeman et al. (2020) and Khubchandani et al. (2021). The association is significant at the ten per cent level for Pfizer vaccine and the five per cent level for the remaining vaccine. Respondents who are the main income source of the family (X5) are more likely to get vaccinated with all vaccine brands. The association is significant at the one per cent level for Janssen and Sputnik V vaccines, at the five per cent level for Moderna, AstraZeneca and Sinopharm vaccines, and at the ten per cent level for Pfizer vaccines. Respondents who have savings (X6) are more likely to get vaccinated with Pfizer, Moderna and AstraZeneca vaccines. The impact is significant at the one per cent level for all vaccine brands. Chew et al. (2021), Edwards et al. (2021), Khubchandani et al. (2021) and Schwarzinger et al. (2021) also found that the participants with savings were more likely to get vaccinated than those without savings. Gold assets (X7) are considered and used as savings in Asian culture. However, studies that examine the impact of this factor on the willingness to vaccinate are occasional. The results show that Respondents who have gold assets (X7) are less likely to vaccinate with Moderna, AstraZeneca, Janssen and Sputnik V vaccines. The impact is significant at the one per cent level for AstraZeneca, at the five per cent level for Janssen and Sputnik V, and at the ten per cent level for the remaining vaccine. Respondents with a dependant (X8) in the family are less likely to get vaccinated with Sinopharm and Sputnik V. The impact is significant at the one per cent level for Sputnik V, and at the five per cent level for the remaining vaccine. It is undeniable that in reality, people hesitate to get vaccinated with these vaccines. This finding is almost similar to that discovered by Dodd et al. (2021) in Australia, but different from that found by Chew et al. (2021), Freeman et al. (2020), Khubchandani et al. (2021), Kourlaba et al. (2021) and Liu and Li (2021). Respondents who are covered by the national health insurance (X11) are less likely to get vaccinated with Pfizer but are more likely to get vaccinated with Sinopharm. The impact is significant at the one per cent level for Pfizer and at the ten per cent for the remaining vaccine. Dodd et al. (2021) also found in Australia that the research participants with health insurance were less likely to vaccinate. Additional conditions, like only beneficiaries who strictly follow or apply the precautionary procedures, including vaccination can be covered, may change their vaccination behaviour. Respondents who have more than six channels to receive news on the pandemic (X13) are more likely to get vaccinated with Pfizer, Moderna, AstraZeneca, Sinopharm and Sputnik V. The impact is significant at the one per cent level for Pfizer, Moderna, AstraZeneca and Sputnik V, and at the ten per cent for the remaining vaccine. This finding is almost similar to that found by Alley et al. (2021) and Yoda and Katsuyama (2021). Respondents who daily receive news on the pandemic (X15) are more likely to get vaccinated with Moderna, AstraZeneca, Janssen and Sputnik V. The impact is significant at the one per cent level for Moderna vaccine, at the five per cent for AstraZeneca and Janssen vaccines, and at the ten per cent level for the remaining vaccine. Alley et al. (2021) found a significant association between time spent on traditional media and the willingness to vaccinate among Australians. In contrast, respondents who daily receive news on the pandemic (X16) are less likely to get vaccinated with Moderna and AstraZeneca vaccines. The impact is significant at the five per cent level for both vaccines. This finding implies that the information on these two vaccines is not sufficient to gain people’s trust to vaccinate. Respondents who perceive that the information on the pandemic is sufficient (X17) are more likely to get vaccinated with Pfizer, Moderna and AstraZeneca vaccines. The impact is significant at the one per cent level for all three vaccines. Respondents who perceive that the information on the vaccines is sufficient (X18) are more likely to get vaccinated with Sinopharm, Janssen and Sputnik V The impact is significant at the one per cent level for all the three vaccines. These findings are almost similar to those discovered by Babicki et al. (2021) and Yılmaz and Sahin (2021). Respondents who belong to the vaccine priority groups (X19) are more likely to get vaccinated with all vaccine brands. The association is significant at the one per cent level for all vaccine brands. This finding is almost in accordance with that found by Freeman et al. (2020), Kessels et al. (2021) and Kourlaba et al. (2021). Similarly, Respondents who live with someone belonging to the vaccine priority groups (X20) are more likely to get vaccinated with all vaccine brands. The impact is significant at the one per cent level for all vaccine brands. Kourlaba et al. (2021) also found that respondents who lived with someone vulnerable to the pandemic were more likely to get vaccinated. As anticipated, respondents with comorbidities (X21) are less likely to get vaccinated with all of the vaccines. The impact is significant at the one per cent level for Pfizer, Moderna, at the five per cent level for AstraZeneca, Sinopharm and Janssen, and at the ten per cent level for the remaining vaccine. As previously addressed the comorbidities may make them hesitate to get vaccinated. This finding is similar to that discovered by Al-Mistarehi et al. (2021), Dodd et al. (2021) and Yoda and Katsuyama (2021) but different from that found by Abedin et al. (2021). Respondents who possess sufficient knowledge about COVID-19 infection symptoms (X22) are more likely to get vaccinated with Moderna and AstraZeneca and the impact is modest. Respondents who possess sufficient knowledge about SARS-CoV-2 virus fatality (X26) are more likely to get vaccinated with the Janssen vaccine and the impact is modest. Respondents who do not believe that her immunity is generated if at least 70 per cent of the population is infected with the virus (X27) are less likely to get vaccinated with the Janssen vaccine and the impact is modest. Kourlaba et al. (2021) also found similar vaccination behaviour in Greece. This indicates that there is room for improvement in providing more information (such as communication campaigns) on herd immunity. Respondents who believe that herd immunity occurs if at least 70 per cent of the population is fully vaccinated (X28) are more likely to get vaccinated with all vaccine brands and the impact is significant at the one per cent level for all vaccine brands. Schwarzinger et al. (2021) attempted to examine this behaviour but found an insignificant impact. People with sufficient knowledge of common symptoms after getting vaccinated (X44) are expected to be more confident to vaccinate than those with insufficient knowledge. The results show that respondents with sufficient knowledge of common symptoms after being vaccinated are more likely to get vaccinated with Pfizer, Moderna, AstraZeneca and Janssen vaccines. The impact is significant at the one per cent level for Moderna vaccine, five per cent level for Janssen vaccines, and ten per cent level for the remaining two vaccines. This finding implies that there is a relationship between the respondent’s hesitancy to vaccinate with Sinopharm and Sputnik V and symptoms after being vaccinated. Respondents who have been infected with the virus (X29) are more likely to get vaccinated with the Sputnik V vaccine and the impact is modest. This finding is almost similar to that found by Al-Mistarehi et al. (2021) Liu and Li (2021) and Schwarzinger et al. (2021). Kawata and Nakabayashi (2021) and Kessels et al. (2021) endeavoured to examine the willingness to get vaccinated of the participants who had been infected with the virus, but the impact was not significant. Respondents who have a close person (a family member, friend or co-worker) infected with the virus (X30) are more likely to get vaccinated with Pfizer, Moderna, Sinopharm and Janssen vaccines. The association is significant at the one per cent level for Pfizer, Moderna and Sinopharm, and at the ten per cent level for the remaining vaccine. Unexpectedly, respondents who are afraid of being discriminated against if unvaccinated (X31) are less likely to get vaccinated with Pfizer, Moderna, Sinopharm, Janssen and Sputnik V vaccines. The association is significant at the one per cent level for Pfizer, Sinopharm, Janssen and Sputnik V, and at the ten per cent level for the Moderna vaccine. This finding is different from that discovered by Li et al. (2021) in China. Perhaps, the discrimination in the study countries is not extremely serious. Otherwise, future studies can further inspect the impact of this factor. Respondents who are afraid of being infected with the virus (X32) are more likely to get vaccinated with Sinopharm, Janssen and Sputnik V vaccines. The impact is significant at the one per cent level for all vaccine brands. Kelly et al. (2021) and Khubchandani et al. (2021) attempted to examine this behaviour, while Kelly et al. (2021) found a significant impact, Khubchandani et al. (2021) found an insignificant impact. In spite of being afraid of needles (X33), respondents are more likely to get vaccinated with all vaccine brands. The impact is significant at the one per cent level for Pfizer, Moderna, Sinopharm, Janssen and Sputnik V, and at the five per cent level for AstraZeneca vaccine. Needle-free vaccines such as COVID-19 nasal spray or vaccines with a laser bubble gun at a reasonable price should be able to combat this fear (Armitage, 2021; World Economic Forum, 2021). In spite of being concerned about the insufficiency of the official information on the vaccines (X34), respondents are still more likely to get vaccinated with Pfizer and the impact is modest. This finding is almost in accordance with that found by Al-Mistarehi et al. (2021). Respondents who are concerned about the response procedure if severe shocks occur due to the vaccines (X36) are less likely to get vaccinated with Janssen and the impact is modest. In spite of being concerned about the immunity of the vaccines (X37), respondents are still more likely to get vaccinated with all vaccine brands. The impact is significant at the one per cent level for Moderna, AstraZeneca, Sinopharm, Janssen and Sputnik V, and at the five per cent for the remaining vaccine. This finding is different from that found by Al-Mistarehi et al. (2021). Yoda and Katsuyama (2021) attempted to examine this association, but the impact was not significant. To minimise this hesitation, test results on vaccine immunity should be made available on multiple accessible channels. In addition, the information should be translated into multiple languages, including local languages. Although being concerned and worried about the vaccine safety (X38), respondents are more likely to get vaccinated with AstraZeneca and the impact is modest. Al-Mistarehi et al. (2021) found this impact was significant, but Kawata and Nakabayashi (2021), Neumann-Böhme et al. (2020) and Yoda and Katsuyama (2021) found this impact was insignificant. Similarly, in spite of being concerned about the distance between the residency and vaccine site (X39), respondents are still more likely to get vaccinated with Sinopharm, Janssen and Sputnik V. The association is significant at the one per cent level for Sinopharm, at the five per cent level for Janssen, and at the ten per cent level for the remaining vaccine. This finding is almost in accordance with that found by Al-Mistarehi et al. (2021). Due to the vaccine supply, the facilities at the vaccination site and availability of medical staff such as nurses, the waiting time at the site ranged between 30 min to hours at the time of the current study. The longer the waiting time, the more discouraging (to vaccinate) it is. Respondents who are concerned about the vaccine cost (X40) are less likely to get vaccinated with almost all vaccine brands. The impact is significant at the one per cent level for Moderna, AstraZeneca, at the five per cent level for Pfizer and Sputnik V, and at the ten per cent level for the Sinopharm vaccine. This finding is similar to that found by Akarsu et al. (2021) and Chew et al. (2021). This finding implies that if the vaccines are not free, there may be fewer people who are willing to get vaccinated. Regardless of being concerned or worried about the safety of the vaccination waiting room (X43), respondents are still more likely to get vaccinated with Pfizer, Moderna and Janssen. The impact is significant at the one per cent level for Moderna, at the five per cent level for Pfizer and at the ten per cent level for the remaining vaccine. Compared to Vietnamese respondents (X45), Filipino respondents are less likely to get vaccinated with Pfizer vaccines and the impact is significant at the one per cent level. This finding is similar to that found by Amit et al., (2022).
The impact of the remaining variables on the willingness to get vaccinated is not significant and can be further analysed in future studies.
Conclusion
The current study utilised data surveyed with 2,500 respondents during August and September 2021 in four Southeast Asian countries to examine the willingness to get vaccinated against SARS-CoV-2 virus with different vaccine brands. It also applies the binary logistic regression model to examine the association between the willingness of the respondents to get vaccinated with the selected influential factors. The willingness to get vaccinated varies according to different vaccine brands and influential factors. Particularly, the percentage of respondents who are willing to get vaccinated with Pfizer, Moderna and AstraZeneca dominates that of those who are willing to get vaccinated with Sinopharm, Janssen and Sputnik V vaccines. The impact of selected influential factors on the willingness of the respondents to get vaccinated with different vaccine brands varies in terms of magnitude and direction, and depending on the vaccine brands. The impact of a few factors on the willingness to get vaccinated is not significant as expected and can be further analysed in future studies. Due to resource limitations, the current study cannot cover other countries or territories in Southeast Asia where the pandemic may also be severe and the willingness to vaccinate with different vaccine brands may not be identical.
Acknowledgements
The authors would like to thank the respondents who have spared their valuable time to participate in the surveys. The author would like to express their appreciation to Michelle Dela Rosa and Sherry Mariz Rafael for their valuable assistance with data collection in the Philippines. The authors would like to thank the researchers at Sebelas Maret University, Thai Nguyen University of Agriculture and Forestry and Griffith University for their valuable comments.
Abbreviations
- X1
Age (measured in years)
- X2
Gender (1 = male)
- X3
Residency (1 = urban)
- X4
Marital status (1 = married or cohabitant)
- X5
Family main income source (1 = yes)
- X6
Savings (1 = yes)
- X7
Gold assets (1 = yes)
- X8
Number of dependants (persons)
- X9
Education (1 = tertiary or above, 0 = others)
- X10
Employment (1 = employed)
- X11
National health insurance member (1 = yes)
- X12
Private health insurance member (1 = yes)
- X13
Information channels to received new on the pandemic (channels)
- X14
Information channels to received new on the vaccines (channels)
- X15
Frequency of receiving new on the pandemic (1 = daily, 0 = others)
- X16
Frequency of being updated with news on the vaccines (1 = daily, 0 = others)
- X17
Sufficiency of information on the pandemic (1 = sufficient)
- X18
Sufficiency of information on the vaccine brands (1 = sufficient)
- X19
Belongs to the vaccine priority groups (1 = yes)
- X20
Living with a person who belongs to the vaccine priority groups (1 = yes)
- X21
Having commodities (1 = yes)
- X22
Knowledge sufficiency of symptoms of COVID-19 infected people (1 = sufficient)
- X23
Knowledge sufficiency of the virus transmission route (1 = sufficient)
- X24
Knowledge sufficiency of ways to prevent the virus (1 = sufficient)
- X25
Knowledge sufficiency on SARS-CoV-2 virus spread speed (1 = sufficient)
- X26
Knowledge sufficiency of SARS-CoV-2 virus fatality (1 = sufficient)
- X27
Knowledge sufficiency on herd immunity if at least 70% of the population is infected (1 = sufficient)
- X28
Knowledge sufficiency of herd immunity if at least 70% of the population is vaccinated (1 = sufficient)
- X29
Ever been infected (1 = yes)
- X30
Having closed one infected (1 = yes)
- X31
If not vaccinated, afraid of being discriminated against (1 = yes)
- X32
Afraid of catching the virus (1 = yes)
- X33
Afraid of needles (1 = yes)
- X34
Concerned about the official and sufficiency of information on the vaccines (1 = concerned)
- X35
Concerned about the side effects of the vaccines (1 = concerned)
- X36
Concerned about the response procedure if there is a severe shock after getting vaccinated (1 = concerned)
- X37
Concerned about the vaccine immunity (1 = concerned)
- X38
Concerned about the vaccine safety (1 = concerned)
- X39
Concerned about the distance between the residency and the vaccination site (1 = concerned)
- X40
Concerned about the vaccine cost (1 = concerned)
- X41
Concerned about the waiting time to vaccinate (1 = concerned)
- X42
Concerned about the time frame to vaccinate (1 = concerned)
- X43
Concerned about the safety of the vaccination waiting room (1 = concerned)
- X44
Knowledge sufficiency of common symptoms after getting vaccinated (1 = sufficient)
- X45 = 1
Dummy variable representing Vietnamese respondents
- X45 = 2
Dummy variable representing Indonesian respondents
- X45 = 3
Dummy variable representing Filipino respondents
- X45 = 4
Dummy variable representing Malaysian respondents
Authors’ Contribution
Duong Hoai An: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing—original draft and Writing—review & editing.
Ernoiz Antriyandarti: Conceptualization, Investigation, and Supervision.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available due to the sensitive nature of the questions asked (especially those on demographic characteristics and personal perceptions). However, the datasets, test results and the R codes are available from the corresponding author on a reasonable request.
Declarations
Ethical Clearance and Informed Consent
Ethical clearance for the current study is approved and issued by the Faculty of Medicine, Universitas Sebelas Maret. No: 95/UN27.06.6.1/KEP/EC2021, Protocol/ID: 01/03/09/99. The current study was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from the survey participants and/or their parents or legal guardian(s). Particularly, the following statement was placed in the Survey Description: “You do not need to leave personal information. The information you provide will be aggregated and used for research purposes only and will not be shared with any third parties.”
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Models Suggested by the AIC Tests
Y1 (The willingness to get vaccinated with Pfizer vaccine)
~ X1 + X2 + X3 + X4 + X5 + X6 + X9 + X11 + X13 + X17 + X19 + X20 + X21 +
X26 + X28 + X30 + X31 + X33 + X34 + X37 + X40 + X42 + X43 + X44 + X45.
Residual Deviance: 1988.
AIC: 2040.
Y2 (The willingness to get vaccinated with Moderna vaccine)
~ X1 + X3 + X5 + X6 + X7 + X13 + X15 + X16 + X17 + X19 +
X20 + X21 + X22 + X28 + X30 + X31 + X33 + X37 + X40 + X43.
Residual Deviance: 1951.
AIC: 1993.
Y3 (The willingness to get vaccinated with AstraZeneca vaccine)
~ X1 + X3 + X4 + X5 + X6 + X7 + X13 + X15 + X16 + X17 +
X19 + X20 + X21 + X22 + X26 + X28 + X31 + X33 + X37 + X38 + X40.
Residual Deviance: 2068.
AIC: 2112.
Y4 (The willingness to get vaccinated with Sinopharm vaccine)
~ X1 + X2 + X4 + X5 + X8 + X11 + X13 + X18 + X19 + X20 + X21 +
X25 + X28 + X30 + X31 + X32 + X33 + X37 + X39 + X40.
Residual Deviance: 2265.
AIC: 2307.
Y5 (The willingness to get vaccinated with Janssen vaccine)
~ X1 + X2 + X3 + X5 + X7 + X15 + X18 + X19 + X20 +
X21 + X26 + X27 + X28 + X30 + X31 + X32 + X33 + X36 + X37 + X39 + X40 + X43.
Residual Deviance: 2321.
AIC: 2367.
Y6 (The willingness to get vaccinated with Sputnik V vaccine)
~ X1 + X2 + X4 + X5 + X7 + X8 + X11 + X13 + X15 + X18 + X19 + X20
+ X21 + X25 + X28 + X29 + X31 + X32 + X33 + X37 + X39 + X40.
Residual Deviance: 2256.
AIC: 2302.
The R codes for the AIC tests are available from the corresponding author on reasonable request.
Contributor Information
An Hoai Duong, Email: hoaian.duong@alumni.griffithuni.edu.au.
Ernoiz Antriyandarti, Email: ernoiz_a@staff.uns.ac.id.
References
- Abedin, M., Islam, M. A., Rahman, F. N., Reza, H. M., Hossain, M. Z., Hossain, M. A., . . ., & Hossain, A. (2021). Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLoS one, 16(4), e0250495. [DOI] [PMC free article] [PubMed]
- Akaike H. A New look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. doi: 10.1109/TAC.1974.1100705. [DOI] [Google Scholar]
- Akarsu B, Canbay Özdemir D, Ayhan Baser D, Aksoy H, Fidancı İ, Cankurtaran M. While studies on COVID-19 vaccine is ongoing, the public’s thoughts and attitudes to the future COVID-19 vaccine. International Journal of Clinical Practice. 2021;75(4):e13891. doi: 10.1111/ijcp.13891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alin A. Multicollinearity. Wiley Interdisciplinary Reviews: Computational Statistics. 2010;2(3):370–374. doi: 10.1002/wics.84. [DOI] [Google Scholar]
- Alley, S. J., Stanton, R., Browne, M., To, Q. G., Khalesi, S., Williams, S. L., . . ., & Vandelanotte, C. (2021). As the pandemic progresses, how does willingness to vaccinate against COVID-19 evolve? International Journal of Environmental Research and Public Health, 18(2), 797. [DOI] [PMC free article] [PubMed]
- Al-Mistarehi, A.-H., Kheirallah, K. A., Yassin, A., Alomari, S., Aledrisi, M. K., Ata, E. M. B., . . ., & Khassawneh, B. Y. (2021). Determinants of the willingness of the general population to get vaccinated against COVID-19 in a developing country. Clinical and Experimental Vaccine Research, 10(2), 171. [DOI] [PMC free article] [PubMed]
- Amit AML, Pepito VCF, Sumpaico-Tanchanco L, Dayrit MM. COVID-19 vaccine brand hesitancy and other challenges to vaccination in the Philippines. PLOS Global Public Health. 2022;2(1):e0000165. doi: 10.1371/journal.pgph.0000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson D, Burnham K, White G. Comparison of akaike information criterion and consistent akaike information criterion for model selection and statistical inference from capture-recapture studies. Journal of Applied Statistics. 1998;25(2):263–282. doi: 10.1080/02664769823250. [DOI] [Google Scholar]
- Arifin, W. N., Musa, K. I., Hanis, T. M., Hasani, W. S. R., Nawi, C. M. N. H. C., Khan, E. E. A., . . ., & Ab Aziz, W. A. (2021). A brief analysis of the COVID-19 death data in Malaysia. medRxiv, 1–11.
- Armitage, H. (2021). COVID-19 Nasal Spray Vaccine in The Works at Stanford Medicine. Retrieved from https://med.stanford.edu/news/all-news/2021/11/effort-to-develop-covid-vaccine-nasal-spray.html
- Babicki M, Pokorna-Kałwak D, Doniec Z, Mastalerz-Migas A. Attitudes of parents with regard to vaccination of children against COVID-19 in Poland. A nationwide online survey. Vaccines. 2021;9(10):1192. doi: 10.3390/vaccines9101192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bascle G. Controlling for endogeneity with instrumental variables in strategic management research. Strategic Organization. 2008;6(3):285–327. doi: 10.1177/1476127008094339. [DOI] [Google Scholar]
- Box GE. Science and statistics. Journal of the American Statistical Association. 1976;71(356):791–799. doi: 10.1080/01621459.1976.10480949. [DOI] [Google Scholar]
- Buenaventura RD, Ho JB, Lapid MI. COVID-19 and mental health of older adults in the Philippines: A perspective from a developing country. International Psychogeriatrics. 2020;32(10):1129–1133. doi: 10.1017/S1041610220000757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bujang MA, Sa’at N, Bakar TMITA. Sample size guidelines for logistic regression from observational studies with large population: Emphasis on The accuracy between statistics and parameters based on real life clinical data. The Malaysian Journal of Medical Sciences: MJMS. 2018;25(4):122. doi: 10.21315/mjms2018.25.4.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh JE. Unifying the derivations for the akaike and corrected akaike information criteria. Statistics & Probability Letters. 1997;33(2):201–208. doi: 10.1016/S0167-7152(96)00128-9. [DOI] [Google Scholar]
- CDC. (2021a). People with Certain Medical Conditions. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
- CDC. (2021b). Different COVID-19 Vaccines. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines.html
- Chew, N. W., Cheong, C., Kong, G., Phua, K., Ngiam, J. N., Tan, B. Y., . . ., & Han, X. (2021). An asia-pacific study on healthcare workers’ perceptions of, and willingness to receive, the COVID-19 vaccination. International Journal of Infectious Diseases, 106, 52-60. [DOI] [PMC free article] [PubMed]
- Chong I-G, Jun C-H. Performance of some variable selection methods when multicollinearity is present. Chemometrics and Intelligent Laboratory Systems. 2005;78(1–2):103–112. doi: 10.1016/j.chemolab.2004.12.011. [DOI] [Google Scholar]
- Daly M, Robinson E. Willingness to vaccinate against COVID-19 in the US: Representative longitudinal evidence from April to October 2020. American Journal of Preventive Medicine. 2021;60(6):766–773. doi: 10.1016/j.amepre.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daoud, J. I. (2017). Multicollinearity And Regression Analysis. Paper presented at the Journal of Physics: Conference Series.
- Dodd, R. H., Cvejic, E., Bonner, C., Pickles, K., McCaffery, K. J., Ayre, J., . . ., & Dakin, T. (2021). Willingness to vaccinate against COVID-19 in Australia. The Lancet Infectious Diseases, 21(3), 318-319. [DOI] [PMC free article] [PubMed]
- Edwards B, Biddle N, Gray M, Sollis K. COVID-19 vaccine hesitancy and resistance: correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE. 2021;16(3):e0248892. doi: 10.1371/journal.pone.0248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrar, D. E., & Glauber, R. R. (1967). Multicollinearity in regression analysis: The problem revisited. The Review of Economic and Statistics, 92–107.
- Fingleton, B., & Le Gallo, J. (2010). Endogeneity in A Spatial Context: Properties of Estimators Progress in Spatial Analysis (pp. 59–73): Springer.
- Fiolet, T., Kherabi, Y., MacDonald, C.-J., Ghosn, J., & Peiffer-Smadja, N. (2021). Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: A narrative review. Clinical Microbiology and Infection. [DOI] [PMC free article] [PubMed]
- Freeman, D., Loe, B. S., Chadwick, A., Vaccari, C., Waite, F., Rosebrock, L., . . ., & Vanderslott, S. (2020). COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychological Medicine, 1–15. [DOI] [PMC free article] [PubMed]
- Graham MH. Confronting multicollinearity in ecological multiple regression. Ecology. 2003;84(11):2809–2815. doi: 10.1890/02-3114. [DOI] [Google Scholar]
- Hartanto, D., & Siregar, S. M. (2021). Determinants of overall public trust in local government: meditation of government response to COVID-19 in indonesian context. Transforming Government: People, Process and Policy.
- Hurvich CM, Tsai CL. A corrected akaike information criterion for vector autoregressive model selection. Journal of Time Series Analysis. 1993;14(3):271–279. doi: 10.1111/j.1467-9892.1993.tb00144.x. [DOI] [Google Scholar]
- Kawata K, Nakabayashi M. Determinants of COVID-19 vaccine preference: A survey study in Japan. SSM-Population Health. 2021;15:100902. doi: 10.1016/j.ssmph.2021.100902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelejian HH. Two-stage least squares and econometric systems linear in parameters but nonlinear in the endogenous variables. Journal of the American Statistical Association. 1971;66(334):373–374. doi: 10.1080/01621459.1971.10482270. [DOI] [Google Scholar]
- Kelly, B. J., Southwell, B. G., McCormack, L. A., Bann, C. M., MacDonald, P. D., Frasier, A. M., . . ., & Squiers, L. B. (2021). Predictors of willingness to get A COVID-19 vaccine in the US. BMC Infectious Diseases, 21(1), 1-7. [DOI] [PMC free article] [PubMed]
- Kessels, R., Luyten, J., & Tubeuf, S. (2021). Willingness to get vaccinated against Covid-19 and attitudes towards vaccination in general. Vaccine. [DOI] [PMC free article] [PubMed]
- Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. Journal of Community Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koris, R., Nor, N. M., Haron, S. A., Ismail, N. W., Junid, S. M. A. S., Nur, A. M., . . ., & Maimaiti, N. (2017). Socio-demographic, cognitive status and comorbidity determinants of catastrophic health expenditure among elderly in Malaysia. International Journal of Economics & Management, 11.
- Kourlaba, G., Kourkouni, E., Maistreli, S., Tsopela, C.-G., Molocha, N.-M., Triantafyllou, C., . . ., & Maroudi-Manta, S. (2021). Willingness of greek general population to get a COVID-19 vaccine. Global Health Research and Policy, 6(1), 1-10. [DOI] [PMC free article] [PubMed]
- Kreps S, Prasad S, Brownstein JS, Hswen Y, Garibaldi BT, Zhang B, Kriner DL. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Network Open. 2020;3(10):e2025594–e2025594. doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Wang J, Leng A, Nicholas S, Maitland E, Liu R. Will COVID-19 vaccinations end discrimination against COVID-19 patients in China? New evidence on recovered COVID-19 patients. Vaccines. 2021;9(5):490. doi: 10.3390/vaccines9050490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R, Li GM. Hesitancy in The time of coronavirus: Temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy. SSM-Population Health. 2021;15:100896. doi: 10.1016/j.ssmph.2021.100896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludden TM, Beal SL, Sheiner LB. Comparison of the akaike information criterion, the schwarz criterion and the F test as guides to model selection. Journal of Pharmacokinetics and Biopharmaceutics. 1994;22(5):431–445. doi: 10.1007/BF02353864. [DOI] [PubMed] [Google Scholar]
- Mansfield ER, Helms BP. Detecting multicollinearity. The American Statistician. 1982;36(3a):158–160. doi: 10.1080/00031305.1982.10482818. [DOI] [Google Scholar]
- MoH. (2018). Vietnam Still Has Many Challenges in Taking Care of The Elderly's Health. Retrieved from https://moh.gov.vn/chuong-trinh-muc-tieu-quoc-gia/-/asset_publisher/7ng11fEWgASC/content/viet-nam-con-nhieu-thach-thuc-trong-cong-tac-cham-soc-suc-khoe-nguoi-cao-tuoi?inheritRedirect=false
- MoH. (2020). 5k Message and Vaccination. Retrieved from https://vncdc.gov.vn/du-co-vaccine-van-phai-luon-thuc-hien-5k-nd16013.html
- Momtaz YA, Hamid TA, Yahaya N, Ibrahim R. Effects of chronic comorbidity on psychological well-being among older persons in Northern Peninsular Malaysia. Applied Research in Quality of Life. 2010;5(2):133–146. doi: 10.1007/s11482-010-9098-2. [DOI] [Google Scholar]
- Neumann-Böhme, S., Varghese, N. E., Sabat, I., Barros, P. P., Brouwer, W., van Exel, J., . . ., & Stargardt, T. (2020). Once We Have It, Will We Use It? A European Survey on Willingness To Be Vaccinated against COVID-19 (vol. 21, pp. 977–982): Springer. [DOI] [PMC free article] [PubMed]
- Our World in Data. (2021). Daily New Confirmed COVID-19 Cases per Million People. Retrieved from https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&time=2020-04-27..2021-08-27&facet=none&pickerSort=asc&pickerMetric=location&Metric=Confirmed+cases&Interval=7-day+rolling+average&Relative+to+Population=true&Align+outbreaks=false&country=VNM~IDN~PHL~MYS
- Portet S. A primer on model selection using the akaike information criterion. Infectious Disease Modelling. 2020;5:111–128. doi: 10.1016/j.idm.2019.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posada D, Buckley TR. Model selection and model averaging in phylogenetics: Advantages of akaike information criterion and bayesian approaches over likelihood ratio tests. Systematic Biology. 2004;53(5):793–808. doi: 10.1080/10635150490522304. [DOI] [PubMed] [Google Scholar]
- Radjab S, Fuady MIN. The Indonesian government's inconsistency in handling the Covid-19 pandemic. Yuridika. 2021;36(3):745–758. doi: 10.20473/ydk.v36i3.27515. [DOI] [Google Scholar]
- Schroeder MA, Lander J, Levine-Silverman S. Diagnosing and dealing with multicollinearity. Western Journal of Nursing Research. 1990;12(2):175–187. doi: 10.1177/019394599001200204. [DOI] [PubMed] [Google Scholar]
- Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in france: A Survey experiment based on vaccine characteristics. The Lancet Public Health. 2021;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semadeni M, Withers MC, Trevis Certo S. The perils of endogeneity and instrumental variables in strategy research: Understanding through simulations. Strategic Management Journal. 2014;35(7):1070–1079. doi: 10.1002/smj.2136. [DOI] [Google Scholar]
- Shibata R. Selection of the order of an autoregressive model by akaike's information criterion. Biometrika. 1976;63(1):117–126. doi: 10.1093/biomet/63.1.117. [DOI] [Google Scholar]
- Statista. (2021). GDP loss due to COVID-19, by economy 2020. Retrieved from https://www.statista.com/statistics/1240594/gdp-loss-covid-19-economy/
- Sun, X., Shi, Y., Zeng, Q., Wang, Y., Du, W., Wei, N., . . ., & Chang, C. (2013). Determinants of health literacy and health behavior regarding infectious respiratory diseases: A pathway model. BMC Public Health, 13(1), 1-8. [DOI] [PMC free article] [PubMed]
- Terza JV, Basu A, Rathouz PJ. Two-stage residual inclusion estimation: Addressing endogeneity in health econometric modeling. Journal of Health Economics. 2008;27(3):531–543. doi: 10.1016/j.jhealeco.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullah, S., Zaefarian, G., & Ullah, F. (2021). How To Use Instrumental Variables in Addressing Endogeneity? A Step-by-step Procedure for Non-Specialists (vol. 96, pp. A1-A6): Elsevier.
- VNVC. (2021). 11 Vulnerable Groups That Are Prioritized for COVID-19 Vaccination in Vietnam Retrieved from https://vnvc.vn/doi-tuong-nao-duoc-uu-tien-tiem-vac-xin-covid-19/
- Vrieze SI. Model selection and psychological theory: A discussion of the differences between the Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC) Psychological Methods. 2012;17(2):228. doi: 10.1037/a0027127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Z. (2000). Model Selection Using The Akaike Information Criterion. STATA Technical Bulletin, 9(54).
- Wang, K., Wong, E. L.-Y., Cheung, A. W.-L., Yau, P. S.-Y., Chung, V. C.-H., Wong, C. H.-L., . . ., & Yeoh, E.-K. (2021). Influence of vaccination characteristics on COVID-19 vaccine acceptance among working-age people in Hong Kong, China: A discrete choice experiment. Frontiers in Public Health, 9. [DOI] [PMC free article] [PubMed]
- WHO. (2020a). WHO Coronavirus (COVID-19) Dashboard. Retrieved from https://covid19.who.int/
- WHO. (2020b). WHO Director-General's Opening Remarks at The Media Briefing on COVID-19 - 11 March 2020b. Retrieved from https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- WHO. (2021a). Tracking SARS-CoV-2 Variants. Retrieved from https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
- WHO. (2021b). Tracking SARS-CoV-2 Variants. Retrieved from https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
- Wooldridge J. Introductory Econometrics: A Modern Approach. Michigan State University; 2012. [Google Scholar]
- World Economic Forum. (2021). Needle-free Injections Could Become A Reality, Thanks to Lasers And The ‘Bubble Gun'. Retrieved from https://www.weforum.org/agenda/2021/10/new-technology-could-allow-you-to-have-a-needle-free-injection/
- Worldometer. (2021). COVID-19 Coronavirus Pandemic. Retrieved from https://www.worldometers.info/coronavirus/
- Wulandari RD, Qomarrudin M, Supriyanto S, Laksono AD, Qomaruddin B, Laksono A. Socioeconomic disparities in hospital utilization among elderly people in Indonesia. Indian J Public Heal Res Dev. 2019;10(11):1800–1804. [Google Scholar]
- Yılmaz M, Sahin MK. Parents’ willingness and attitudes concerning the COVID-19 vaccine: A Cross-sectional study. International Journal of Clinical Practice. 2021;75(9):e14364. doi: 10.1111/ijcp.14364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoda T, Katsuyama H. Willingness to receive COVID-19 vaccination in Japan. Vaccines. 2021;9(1):48. doi: 10.3390/vaccines9010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to the sensitive nature of the questions asked (especially those on demographic characteristics and personal perceptions). However, the datasets, test results and the R codes are available from the corresponding author on a reasonable request.