Abstract
In the past, the use of face masks in western countries was essentially limited to occupational health. Now, because of the COVID-19 pandemic, mask-wearing has been recommended as a public health intervention. As potential side effects and some contraindications are emerging, we reviewed the literature to assess the impact of them in daily life on patient safety and to provide appropriate guidelines and recommendations. We performed a systematic review of studies investigating physiological impact, safety, and risk of masks in predefined categories of patients, which have been published in peer-reviewed journals with no time and language restrictions. Given the heterogeneity of studies, results were analyzed thematically. We used PRISMA guidelines to report our findings. Wearing a N95 respirator is more associated with worse side effects than wearing a surgical mask with the following complications: breathing difficulties (reduced FiO2, SpO2, PaO2 increased ETCO2, PaCO2), psychiatric symptoms (panic attacks, anxiety) and skin reactions. These complications are related to the duration of use and/or disease severity. Difficulties in communication is another issue to be considered especially with young children, older person and people with hearing impairments. Even if benefits of wearing face masks exceed the discomfort, it is recommended to take an “air break” after 1–2 h consecutively of mask-wearing. However, well-designed prospective studies are needed. The COVID-19 pandemic could represent a unique opportunity for collecting large amount of real-world data.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11739-022-03083-w.
Keywords: Patient safety, Facemask, Filtering face piece, Respiratory protection, COVID-19
Introduction
The use of face masks (FMs) has become widespread as part of a multi-faceted approach to limit spread of the COVID-19 virus. In the past, use of the mask was limited to occupational health and safety settings, as well as use by individuals to combat impact of air pollution, allergies, and risk of infection in immunosuppressed people The increased use during the pandemic has highlighted problems in their use.
As of December 2021, more than 86% of the world's population lived in countries that recommended or mandated FMS in public; more than 130 countries have mandated the masks [1] The wearing of masks along with physical distancing or during exercise has been contentious [1, 2].
A well-performing FM must have the following four basic ergonomic requirements:
(1) Protect the respiratory system from the polluting or infectious agent.
(2) Allow adequate ventilation.
(3) Fit the face well.
(4) Ensure good protection and comfort during normal activities.
The demand for masks has led to new approaches to the design of face masks [3]. Different types of FMs are listed in Table 1 [3, 4].
Table 1.
The different types of face masks
| Cloth face masks can be made from a variety of fabrics although they are less effective than surgical mask or N9. CDC suggests wearing two masks (disposable mask underneath and cloth mask on top) |
| Surgical masks are fluid-resistant, disposable, and loose-fitting devices that create a physical barrier between the mouth and nose of the wearer and the immediate environment. They are for use in surgical settings and do not provide full protection from inhalation of airborne pathogens, such as viruses |
| Respirators such as N95 and Filtering Face-pieces (FFP2 and FFP3) are personal protective equipment that tightly fit the face and filter airborne particles to protect health care workers. They provide a higher level of protection against viruses and bacteria when properly fit- tested |
Rationale for the review
Reports on potential side effects of mask wearing led us to query the safety implications of wearing masks [5]. The side effects include a false sense of security, reduced compliance with other measures
and contraindications to mask wearing including young children, persons with breathing difficulties or who are unconscious, incapacitated, etc. [4].
Methods
We performed a systematic review of published studies investigating the safety of FMs categorized to different groups, i.e., children, pregnant women, patients with neurodegenerative diseases, cognitive impairment, obesity, lung/cardiac/renal diseases, psychiatric disorders, eye or upper airway diseases. We searched Medline/PubMed and EMBASE using the search strategy reported in Supplemental files, with no time and language restrictions.
The search and screening process was independently conducted by two researchers (MLR and DDS) with no time restrictions. Reports were considered potentially eligible for this review if they assessed the safety, risks and/or the respiratory impact of FMs. We included papers about the impact of FMs on communication, especially in noisy environments. Figure 1 shows the study selection process. Exclusion criteria were as follows: papers not peer reviewed, not focused on risks, safety or impact on respiratory function, no reported exposure to any type of face mask, not focused on age range or disease. From each paper we extracted the following: authors’ names, year of publication, study design, sample size, safety indicators and/or respiratory parameters, safety and/or respiratory outcomes.
Fig. 1.
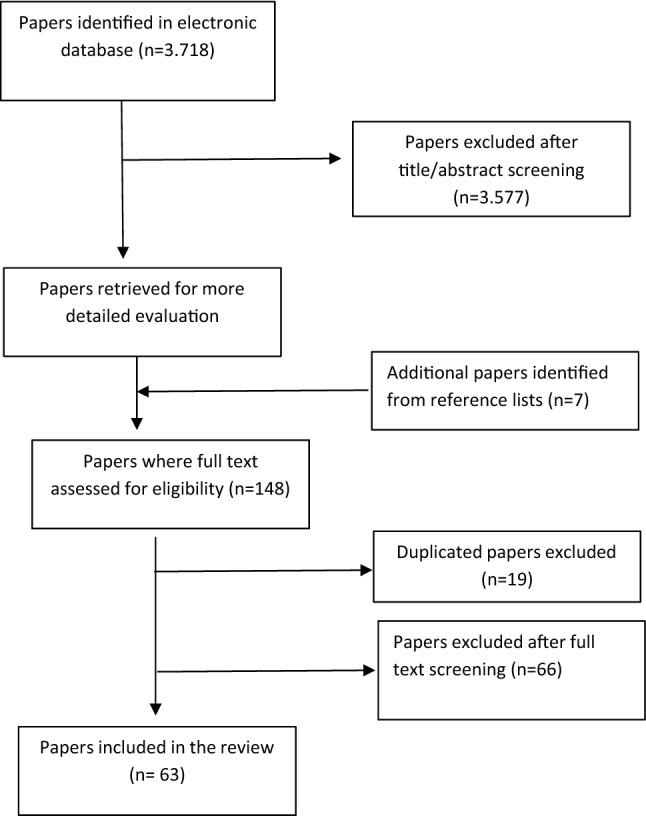
Studies‘ identification and selection
Given the heterogeneity of studies, results were analyzed thematically. We used PRISMA guidelines to report our findings.
Consensus recommendations
Following the systematic review, we arbitrary selected a panel of specialists with experience and/or interest in patient safety (1 gynecologist, 1 pediatrician, 3 internists, 1 pulmonologist, 1 ear-nose- throat specialist, 1 public health and 2 occupational medicine physician, 1 ergonomist, 1 coroner) to address specific recommendations. A Delphi consensus approach was used [6]. A detailed document with a research evidence summary, including methodological details of included papers, was sent to each panelist who reviewed the document and gave their own recommendations for any thematic area anonymously with the rationale for their proposal. All statements with the associated rationale of the proposal were sent back to the panelists to choose one option in any thematic area. We conducted three rounds to reach an acceptable level of consensus.
Results
Our research retrieved 3718 papers, of which 3577 were excluded after title/abstract screening, 66 after full test reading and 19 because of duplication; seven papers were identified from the reference list. We included 63 eligible papers, published between 1995 and January 2022. Details are provided in Table 2. We divided them into 12 thematic categories according to the investigated population/safety issues.
Table 2.
Eligible studies grouped in twelve thematic categories
| Category | Number reports | Author/year | Study design | Language | Sample (n) and measures | Results | |
|---|---|---|---|---|---|---|---|
| Children | 3 | Goh DYT et al. 2016 [7] | Two-period crossover randomized study | English |
106 children (7–14 years old) Physiological parameters: ETCO2, FICO2, RR, SpO2, HR, mask fit test, comfort assessment by visual analogue scale (VAS) without mask, with mask and with mask + microfan at rest and on mild exercise |
Mask without MF: increased the ETCO2 and FICO2 at rest and on mild exertion Mask with MF: FICO2 levels comparably closer to baseline levels without the mask for both activities Mask, with or without the MF: well fitting, comfortable and safe for use in children, at rest and on mild exertion |
|
| Lubrano R et al. 2021 [8] | Cohort study | English | 47 healthy children (aged A:4–24 months, B: 24–144 months). Parameters: ETCO2, SaO2, PR, RR, or signs of respiratory distress during two 30-min session with and without mask. In group B 12-min walking-test wearing the mask | In group A there is no significant differences with and without mask. In group B after 12-min walking-test with mask there are a significant change in PR and RR but always within normal ranges | |||
| Schwarz S et al. 2021 [9] | Survey | German |
20.353 respondents (parents, teachers, physicians) at survey of side effects of FMs worn by children and adolescents (Age: 0–17) |
67.7% of parents reported their children had side effects: headache, concentration difficulties, sleepiness, fatigue, skin worsening, nosebleed, anxiety disorders, rejection or anxiety of school, increased sweating, injuries behind ears, cracked lips, vision disorders and nightmares. Age 7–12 group, 60,4% had greater irritability, 49,3% were unhappy, 44% refused school, 25,3% developed new fears | |||
| Chronic lung diseases | 7 | Schönhofer B et al. 1995 [13] | Case control study | German | 29 cases vs 23 controls Pimax (cmH2O), P0,1 (cmH2O), P0,1/Pimax (cmH2O) | Cases: after 2 h with mask increased PaCO2, P0,1, P0,1/Pimax, HCO3 and reduced Pimax | |
| Bansal S et al. 2010 [11] | Case control study; dual cartridge half face mask vs N95 | English | 73 cases with mild respiratory disease vs 24 healthy controls; minute ventilation/high, inspiratory time, duty circle, heart rate, tidal volume / high, respiratory rate, expiratory time, time to reach, peak inspiratory/expiratory flow, mead inspiratory flow, peak inspiratory/expiratory flow | Respirator type affects physiologic measures; respiratory timing parameters are more affected that ventilator volumes; asthma has greater respirator-disease interaction than COPD and rhynopathy | |||
| Harber P et al. 2010 [12] | Case control study; dual cartridge half face mask vs N95 | English | 77 cases with mild respiratory disease vs 27 healthy controls; subjective response to respirator during tasks in a simulated work environment. Subjective response to respirator for multiple domains includes 12 specific symptoms and assessment of respirator- related duration decrement | More adverse subjective responses with half face mask than N95, especially in women. Asthma significantly increased the adverse effect of the HFM for six of the scales and showed a borderline significant effect for another. Conversely, the presence of COPD or rhinitis tended to decrease the differences between using an HFM versus an N95 device for many of the subjective rating variables | |||
| Kyung SY Kim Y et al. 2020 [10] | Observational study | English | 97 subjects with COPD; blood pressure, heart rate (HR), breathing rate (BR), SPO2, ETCO2 at baseline, during 6- minute walking test without a mask, 10 min rest with a mask and 6 mwt with the mask | BR, SPO2 and ETCO2 significantly higher after N95 use at rest; HR, BF and ETCO2 higher after 6MWT with a mask than after 6 MWT without a mask, SPO2 significantly lower after 6MWT with a mask | |||
| Ciocan C et al. 2020 [15] | Case-Series study | English | 10 participants, 3 with asthma and 3 smokers. Subject were tested three times: basal condition without mask, with mask and after 4 h of use of mask. In all times they performed Respiratory Functional Test (RFT) and Arterial Blood Gases Test (ABG). Parameters VC, FVC, FEV1, FEV1/FVC, TD, MVV, PaO2, PaCO2, SaO2 | PaCO2 showed a slight increase in well- controlled asthmatic patients, probably due to minimal increase in dead space | |||
| Samannan R. et al. 2021 [14] | Clinical observation study | English | 30 participants (15 healthy subjects; 15 with severe COPD). Parameters: ETCO2, SaO2 during 6-min walking test (6MWT) with surgical mask | Patients with severe COPD did not present any physiological changes in gas exchange measurements after 6MWT using surgical masks | |||
| Faria N. et al. 2021 [16] | Retrospective self- controlled study | English |
286 COPD patients with severe acute exacerbation (sAECOPD) They compared the incidence of sAECOPD events in 2020 with 2016, 2017, 2018 and 2019 |
Over the course of 2020 there was a statistically significant decrease of 73.4% in sAECOPD events comparing with previous years’ average | |||
| Ear-nose-throat diseases | 7 |
A. Hearing impairment Mendel LL et al 2008 [17] |
Case control study | English | 31 adults (1 talker, 15 listeners with normal hearing and 15 with hearing impairment | Surgical mask did not negatively affect speech uncerstanding. Noise has a deleterious effect on speech perception | |
| Langrish et al. 2012 [22] | Open randomized crossover trial | English | 98 patients with coronary heart disease walked on a predefined route once with and once without N95; symptoms, exercise, personal air pollution exposure, blood pressure, heart rate, and 12-lead electrocardiography were monitored throughout the 24- hr study period | Face mask well tolerated, its use was associated with decreased self-reported symptoms and reduced maximal ST segment depression (– 142 vs. – 156 μV, P = 0.046) over the 24-h period; mean ambulatory arterial blood pressure and heart rate more stable in the subjects who used masks | |||
| Atcherson SR et al. 2017 [20] | Case control study | English | 31 adults participated in this study: 1 talker, 10 listeners with normal hearing, 10 listeners with moderate sensorineural hearing loss, and 10 listeners with severe- profound hearing loss. Transparent surgical masks vs conventional paper mask | Listeners with normal hearing performed consistently well across all conditions. Both groups of listeners with hearing impairment benefitted from visual input from the transparent mask, mainly the severe-to- profound group | |||
| Trecca EMC et al. 2020 [21] | Case series | English | 59 patients with mild to profound hearing impairment referred from the Emergency Department for urgent ORL consultations; difficulties to communicate with HCWs in relation to their hearing impairment as none, mild, moderate, and severe and face mask use; causes of experienced difficulties | Eight (13.6%) subjects did not have difficulties, 15 (25.4%) presented mild difficulties, 22 (37.3%) moderate and 14 (23.7%) severe; the main cause of speech understanding about face masks was the sound attenuation for 26 (44.1%) subjects and the impossibility of lip reading for 33 (55.9%) | |||
| Chodosh J et al. 2020 [18] | Editorial | English | The challenging for people with hearing loss is reported in this study and they focused on how masks undermine speech communication for patients with hearing loss in medical care settings | They proposed solutions to overcome the difficulties with this patient: speak slowly, raise the volume voice, face masks with clear windows, low tech aids: white boards, yellow pads, app on smartphone or tablets, microphone directly connected to the headphones | |||
| Ten Hulzen RD et al. 2020 [19] | Review | English | The negative impact of universal masking and social distancing is analyzed in both health care and community settings for individuals with hearing loss | Each type of mask decreased the higher frequencies of speaker’s voice from 3 to 4 dB in medical mask, to nearly 12 dB in N95 mask. Physical distancing decreased the sound by 6–12 dB. Helpful strategies are: reduce background noise, ask how the individual prefers to communicate; speak louder | |||
| Vos TG et al. 2021 [23] | Prospective cohort study | English | 23 patients with cochlear implant (CI) for at least 6 months listened a female talker recorded sentences with: no mask, N95 mask, N95mask + face shield. They measured the speech recognition | CI Patient experienced a lower speech recognition whit N95 mask + face shield rather than only the N95 mask, because the plastic barrier attenuated the high- frequencies essential for the speech recognition | |||
| 3 |
B. Allergic and rhinopathic Dror AA et al. 2020 [24] |
Survey | English | 301 nurses with allergic rhinitis (233 with intermittent rhinitis and 68 with persistent) | Nurses who used N95 masks and surgical masks, reported a decrease of symptomatology compared with no mask. Standard surgical masks filter particles larger than 3 µm whereas N95 respirators can filter particles as small as 0.04 µm, so they can block the allergy triggers | ||
| Kishore Dayal a et al. 2020 [25] | Retrospective Observational Study | English | Patients with signs and symptoms of allergic rhinitis post pandemic (March– July2020) were compared to preceding three months (Jan 2020-March2020) | The number of patients of allergic rhinitis have shown a decreasing trend by nearly quartered as compared to immediately preceding three months | |||
| Klimek L et al. 2020 [26] | Experimental study | English | 46 healthy subjects came to the clinic for suspected new form of irritant rhinitis caused by FFP (filtering facepiece mask) | Patients referred symptoms like sneezing, itching, nasal blockage, and/or watery nasal discharge after wearing their FFP for > 2 h. Endoscopic signs of irritation and edema were found, they decreased after 3 days without mask | |||
| Heart diseases | 2 | Langrish JP et al. 2020 [22] | Open randomized crossover trial | English | 98 patients with coronary heart disease walked on a predefined route once with and once without N95; symptoms, exercise, personal air pollution exposure, blood pressure, heart rate, and 12- lead electrocardiography were monitored throughout the 24- hr study period | Face mask well tolerated, its use was associated with decreased self-reported symptoms and reduced maximal ST segment depression (– 142 vs. – 156 μV, P = 0.046) over the 24-h period; mean ambulatory arterial blood pressure and heart rate more stable in the subjects who used masks | |
| Fikenzer S et al. 2020 [27] | Prospective cross-over study | English | 12 healthy males were monitored exercising with no mask, surgical and N95/FFP2 masks. Parameters: Pmax, CO, SV, HR, VO2max VE FVC, FEV1, PEF, TIFF | FFP2/N95 marked negative impact on exercise parameters Pmax and VO2max/kg; reduced pulmonary parameters at rest and at maximum load.; they are very uncomfortable due to subjective breathing resistance | |||
| Haemodialysis | 1 | Kao TW et. al 2004 [28] | Observational study | English | 39 ESRD patients, each patient wore a new N95 mask (3 M Model 8210) during HD (4 h); vital signs, clinical symptoms and arterial blood gas measured before and at the end of HD | Wearing an N95 mask for 4 h during HD significantly reduced PaO2 and increased respiratory adverse effects in ESRD patients | |
| Eye disease | 5 | Moshifar M et al. 2020 [30] | Comment | English | People who wear FMs regularly, both patients and HCWs | They described an increased airflow that can accelerates the evaporation of the tear film and when continuous for hours or days, may result in ocular surface irritation or inflammation. Discomfort from dry eyes may also increase eye rubbing and face touching behaviours, with attendant fomite transmission | |
| El-Nimri NW et al. 2020 [33] | Case-series | English | 6 patients with the diagnosis of ocular hypertension, glaucoma suspect, or glaucoma underwent SAP while wearing surgical FM | Fogging may reduce visual field (VF) test reliability and induce artifacts that mimic glaucomatous defects | |||
| Young SL et al. 2020 [32] | Case report | English | A 32-year-old female underwent SAP while wearing a surgical FM | There was a marked reduction in sensitivity inferiorly of VF in both eyes. Patient repositioned her FM. VF were repeated and found to be normal. Poorly fitting FMs represent a new cause of VF artifact which may mimic pathologic field defects | |||
| Boccardo L. 2021 [29] | Survey | English | 3605 respondents among general people about mask- associated dry eye (MADE) | 26.9% reported exacerbation of symptoms when wearing a mask, thus 18.3% of all participants experienced MADE. The prevalence was higher in woman and in those who wore glasses and contact lens | |||
| Bayram N et al. 2021 [31] | Experimental study | English | 127 glaucoma patients: 101 wearing surgical mask; 26 cloth masks. (Age range: 34–84 years old). They underwent standard automated perimeter (SAP) | 20.5% of patients had FMs-related problems. 18.1% low SAP reliability significantly higher in cloth FMs than surgical FMs (47.8 vs. 9.9%), inferior visual field defects were present 2.4%. After taping the upper edge of masks, false- positive errors were significant improvements and after the reposition of masks, the visual field defects disappeared in the repeated SAP | |||
| Neurodegenerative disease | 2 | Gil R et al. 2020 [34] | Review | English | Challenge that patients with Alzheimer’s Disease (AD) and their caregivers have had to face during the pandemic due to amnesia and symptoms related to AD | AD patients can have sensorial deficits and perception troubles, including visual difficulties and the inability to recognize faces and emotions. FMs and physical distancing can make it more difficult to recognize emotional expressions and can provoke distress | |
| Kobayashi R et al. 2021 [35] | Observational study | English | 55 patients with AD were interviewed to examine recognition of the COVID-19 pandemic and the status of face mask wearing in patients with AD | 38.2% of AD patients knew about COVID- 19, 74.5% didn’t’ wear properly masks by themselves, 12.7% didn’t wear properly masks even with caregiver’s help | |||
| Exercise | 3 | Fikenzer S et al. 2020 [27] | Prospective cross-over study | English | 12 healthy males were monitored exercising with no mask, surgical and N95/FFP2 masks. Parameters: Pmax, CO, SV, HR, VO2max VE FVC, FEV1, PEF, TIFF | FFP2/N95 marked negative impact on exercise parameters Pmax and VO2max/kg; reduced pulmonary parameters at rest and at maximum load.; they are very uncomfortable due to subjective breathing resistance | |
| Chandrasekaran B et al. 2020 [37] | Review | English | Evidence-based hypotheses of health risk while exercising with N95 respirator | Exercising with tight face masks induces hypoxia, reduces renal functions, increases the heart rate and blood pressure | |||
| Epstein D et al. 2021 [36] | Multiple cross-over trial | English |
16 healthy male volunteers who participated in vigorous- intensity activity for 75 min or moderate-intensity activity for 150 min/week. Bbefore and after the test, were measured parameters: HR, SO2, RR, EtCO2, BP During the test was measured rate level of perceived exertion (RPE) |
Exercising with N95 mask was associated with a significant increase in end-tidal carbon dioxide (EtCO2) levels | |||
| Skin diseases and adverse reactions | 7 |
Veraldi S et al. 2020 [38] |
Letter to editor | English |
43 patients with seborrheic dermatitis (SD) using face mask for 6–10 h/day (Age range 23–48 years) |
46.5% of sample had worsening of SD. Worsening includes: increased erythema and desquamation 70% had worst itching |
|
|
Zuo Y et al. 2020 [39] |
Cross‐ sectional survey | English | 404 respondents to the questionnaire where they had to document skin, eye, and respiratory tract symptoms and suspected etiologic factors related to the use of masks | 49.0% reported mask‐related skin reactions, 85.4% facial skin problems, 17.1% respiratory tract problems, 6.2% eye symptoms. Of 129 participants, 44.2% had exacerbation, including 43.6% acne patients, 37.5% with seborrheic dermatitis, and all acne rosacea | |||
| Szepietowski JC et al. 2020 [40] | Survey | English | 2307 respondents survey about prevalence, intensity and clinical characteristics of itch related to the use of face masks | 60.4% reported using face masks during the previous week, and, of these, 19.6% reported having itch. People who reported skin had higher risk of itch development. Responders who wore masks for longer periods more frequently itch | |||
|
Han C et al. 2020 [41] |
Letter to editor | English | Two dozen of patients with diagnosis of flare of acne between April and May 2020. The most reported symptoms were itching sensation and excessive seborrhea | Higher T°C increases sebum excretion (sebum excretion increases by 10% for each 1 °C rise). Patients could be tempted to touch their face, removing of mask for itch and annoying pimples, which could increase the risk of COVID‐19 transmission | |||
|
Park S et al. 2020 [42] |
Observational study | English | 21 healthy subjects were enrolled and skin temperature, redness, hydration, elasticity sebum secretion, trans- epidermal water loss, were measured. Three measurements were taken 1) before wearing the mask, 2) after wearing the mask for 1 h, and 3) after wearing the mask for 6 h | Skin temperature, redness, hydration, and sebum secretion were changed significantly after 1 and 6 h of wearing a mask. Skin changes showed significant differences between the mask-wearing area and the non–mask-wearing area | |||
| Techasatian L et al. 2020 [44] | Prospective Survey | English | 833 respondents a survey which investigated face mask- related adverse skin reactions | Most common skin reaction were acne 39.9%, rashes 18.4% and itching 15.6%). Surgical masks were significantly more associated with skin reactions than cloth masks. Also, people who wearing masks 4- 8 h/day or ˃8 h/day had higher risk of skin reactions | |||
| Han HS et al. 2021 [43] | Cross- sectional study | English | 20 HCWs included. Skin parameters were measured: skin hydration, temperature transepidermal water loss (TEWL), erythema, sebum secretion, pH, in the mask- covered and uncovered areas of the face 4–8 h after wearing RPE and 14 h after not wearing respiratory protective equipment (RPE) | Skin hydration, temperature, TEWL, erythema, pH, increased in the RPE covered areas after wearing RPE for 4–8 h. In the RPE-uncovered areas, skin hydration decreased and TEWL, erythema, and pH showed minimal changes over time | |||
| Psychiatric disorders | 8 | Wu S et al. 2011 [49] |
Case control study; elastomeric half-face maskwith dual- cartridges (HFM)vs N95 filtering facepiece during work |
English | 12 volunteers with normal or mildly impaired respiratory conditions performed a series of simulated work tasks using the HFM and N95 on different days. The State-Trait Anxiety Inventory (STAI) measured state anxiety (SA) before and during respirator use | Work with HFM was associated with an increase in anxiety (2.92 units, p < 0.01), whereas work with the N95 had no observed effect | |
| Uvais NA, 2020 [46] | Cross- sectional study | English | 168 psychiatric patients attending the psychiatric department answered the questionnaire about the correct use of face mask. | The most common psychiatric diagnosis was depressive disorder (44%), psychotic illness (17.3%), panic disorder (12.5%), adjustment disorder (10.7%). 99.4% of the sample wore a mask, but 17.4% wore it not properly | |||
| Sivaraman M et al. 2020 [50] | Experimental study | English | 6 children with diagnosis of Autistic Spectrum Disorder (ASD) with a history of challenging behavior associated with mask wearing were recruited from different parts of the world. They had to follow 15 steps to learn to tolerate the mask | By the end of the intervention, all participants wore a face mask for a period of 10 min without exhibiting challenging behavior. Mask wearing did not affect the % of oxyhemoglobin saturation of participants | |||
| Soh KC et al. 2021 [47] | Letter to editor | English | The challenge of face mask with PTSD patients in inpatient unit in Australia | Mask-wearing hid the verbal/nonverbal communication, making difficult to establish a trusting relationship with patients. Moreover, a person, with past trauma whilst having her mouth covered, had great difficulties to cover her mouth with mask | |||
| Battista RA et al 2021 [48] | Observational study | English | 381 participants complain about side effects including psychiatric symptoms | More than 35% of respondents reported worsening of mood tone while nearly 10% complained about personal protective equipment (PPE) related panic attacks | |||
| Jung H et al. 2021 [45] | Survey | English | 261 psychiatric patients responded to a questionnaire about mask-wearing behaviour | 37.4% wore a mask in hospital and they were more aware of the recommendation to prevent COVID-19 infection than people who did not wear a mask | |||
| Halbur M et al. 2021 [51] | Experimental study | English | 12 children with ASD with a history of challenging behaviour associated with face covering (face masks and face shields) wearing. They had to follow 15 steps for each face covering | The duration of tolerance of facial coverings did not exceed 15 min | |||
| Schwarz S, et al. 2021 [9] | Survey | German |
20.353 respondents (parents, teachers, physicians) at survey of side effects of FMs worn by children and adolescents (Age: 0–17) |
67.7% of parents reported their children had side effects: headache, concentration difficulties, sleepiness, fatigue, skin worsening, nosebleed, anxiety disorders, rejection or anxiety of school, increased sweating, injuries behind ears, cracked lips, vision disorders and nightmares. Age 7–12 group, 60.4% had greater irritability, 49.3% were unhappy, 44% refused school, 25.3% developed new fears | |||
| Contraindications and side effects | 16 | Lim EC et al. 2006 [53] | Survey | English | 212 healthcare workers responded, risk factors associated with development of headaches associated to N95 (frequency, headache subtypes and duration of face- mask wear) and impact of headaches (sick days, headache frequency and use of abortive/preventive headache medications) | 37.3% reported face-mask-associated headaches: 32.9% headache frequency exceeding 6 times/month; 7.6% had taken sick leave (mean 2 days) 59.5% required abortive analgesics, 2.1% preventive medications for headaches. Pre-existing headaches and continuous use (> 4 h) were associated with development of headaches | |
| Baig AS et.al 2010 [63] | Survey | English | 559 surveys distributed, 159 respondents | Features required by respondents: comfort, less interference with breathing, diminished heat build-up, disposable, and permission of facial hair. Multivariate analyses suggest that emergency department staff had 12.3 greater odds of wanting a new respirator (P = 0.031) as compared with their referent group. Males were more likely to indicate that the N95 respirator was comfortable to wear versus females (P = 0.003) | |||
| MacIntyre CR et al. 2011 [60] | Cluster randomized trial | English | 1441 participants s aged ≥ 18 years from the emergency departments and respiratory wards of 15 hospitals wearing masks or respirators during the entire work shift for 4 weeks; clinical respiratory illness (CRI), influenza-like illness (ILI), laboratory-confirmed respiratory virus infection and influenza; Adherence to wearing the masks or respirators was monitored by these diary cards and returned to researchers on a weekly basis. Exit interviews with participants were conducted after the 4 weeks to gain further insights into adherence and other issues around the use of masks/respirators including adverse effects. A convenience no-mask/respirator group of 481 health workers from nine hospitals was compared | The rates of all outcomes were higher in the convenience no‐mask group than in the masks groups. By adjusted intention‐to‐ treat analysis, N95 respirators but not medical masks had significantly lower rates of infection compared to no masks. Among reported problems associated with using the masks or respirators N95 generates more trouble in communicating with patients than medical mask (8% vs 3%) | |||
| Thomas F. et al. 2011 [62] | Randomized controlled study | English | A flight crewmember and a layperson sitting in a Bell 407 crew compartment and a dispatcher sitting in a communication centre record 20 randomized aviation terms transmitted over the radio by a helicopter emergency medical services (HEMS) pilot wearing a surgical facemask and six different N95s with and without the aircraft engine operating | With the aircraft engine off, all terms (100% accuracy) were correctly identified, regardless of the absence or presence of the surgical facemask or N95 studied. With the aircraft engine on, the surgical facemask (3 M-1826) and two N95 respirators (3 M- 1860, Safe Life Corp-150) maintained 100% accuracy. Remaining N95 accuracy was as follows: 3 M-8511 and Kimberly- Clark PFR95 (98%), Inoyel-3212 (97%), and 3 M-1870 (93%) | |||
| Honarbakhsh M. et. al 2017 [59] | Cross sectional study | English | Problems and obstacles in using N95 respirators were identified and ranked by experts, using Fuzzy Delphi and Fuzzy Analytic Hierarchy Process (FAHP). Additionally, HCWs were asked to give their opinions about obstacles in using N95 respirators to form an opinion | 4 factors—including heat around the face, inaccessibility to respirators, difficulty breathing, and trouble in communication— achieved the highest average score according to the HCWs’ opinions | |||
| Or PP et. al 2018 [64] | Randomized study | English | 84 nursing students, divided randomly into 4 groups, with 21 in each group. Personal Respirator Sampling Test (PRST) and usability questionnaire to record their evaluations of the six perceptions of comfort of wearing N95 respirators | Respirators resulted comfortable at warm temperatures of 20–24 °C. Tightness in the respirators and discomfort on their ear lobes were the main obstacles to face masks use | |||
| Ong JJY et. al 2020 [54] | Cross sectional study | English | 158 healthcare workers completed a self-administered questionnaire | Most healthcare workers develop de novo PPE-associated headaches or exacerbation of their pre-existing headache disorders | |||
| Ramirez-Moreno JM et al. 2020 [55] | Cross- sectional study | English | 306 healthcare workers completed a self-administered questionnaire | 51.6% presented. “De novo” headache and according to the type of mask used, there were differences in headache intensity, and the impact of a headache in the subjects who used a filter mask was worse | |||
| Kalra S et al. 2020 [52] | Commentary | English | They coined new term “Mask fatigue” and proposed solution to prevent it. Mask fatigue is defined as the lack of energy that accompanies, and/or follows prolonged wearing of a mask. may be considered as a disorder if it interfered with daily life | Prevent mask fatigue: suggested: choosing right mask (size, type), drinking, and eating before wearing mask, taking voice rest and talk less, not strenuous exercises, removing mask for a few minutes at a safe place, avoiding prolonged (> 6 h) use of same mask. Washing face with soap and lukewarm water followed by cold water splashes on eye, apply an emollient if needed, relax, deep breathing exercises, respiratory muscle training, aerobic exercise of 30 min at least 5 days a week, weight management | |||
| Farronato et al. 2020 [56] | Scoping Review | English | 256 Italian dentists completed a self-administered questionnaire | Prolonged use of respirators was associated with headaches (47.5%), severe exertion and discomfort (50.8%), moderate concentration problems (54.3%), moderate breathing difficulties (63.5%), and consequently, an impaired work ability (85.5%) | |||
| Scheid JL et al. 2020 [58] | Commentary | English | Physiological effects of wearing masks for prolonged periods of time, including mask wearing among those who engaged in exercise training, and concerns for individuals with pre-existing chronic diseases |
Healthy individuals, wearing masks, even for an extended period, did not produce any clinically relevant changes in circulating O2 or CO2 concentrations, and did not seem to impact tidal volume or respiratory rate However, wearing a mask does produce a small increase in breathing resistance caused by the mask material filtering particles and aerosols in the air and any moisture that is trapped in the mask material |
|||
| Bothra A et al. 2020 [65] | Letter | English | 14 patients both healthcare workers and general population visited between 1st April- 30th April | 35.7% patients were diagnosed to have Irritant Contact Dermatitis, 28.5% patients were diagnosed with Allergic Contact Dermatitis, 21.4% patients developed sweat dermatitis, 1 patient pressure urticarial, 1 patient had exacerbation of pre-existing dermatoses. Pre-existing dermatoses were present in 50% including atopic dermatitis, seborrheic dermatitis and chronic urticaria. The most common symptoms reported were itching and dryness, whereas the most common signs seen were erythema, scaling and papules | |||
| Battista RA et al. 2021 [48] | Observational study | English | 381 participants complained about side effects including psychiatric symptoms | More than 35% of respondents reported worsening of mood tone while nearly 10% complained about Personal protective equipment (PPE) related panic attacks | |||
| Cheok GJW et al. 2021 [57] | Cross- sectional survey | English | 402 respondents of lay people completed a questionnaire | 67.2% wore disposable surgical masks. 72% felt mask-wearing was necessary to control COVID-19 transmission. 78.4% reported discomfort: dermatological issues, sweating, difficulty breathing especially panic prone individuals | |||
| Czypionka T et al. 2021 [61] | Review | English | Mask-wearing among general population were analysed in various aspects | All kind of masks caused discomforts and difficulties in communications especially with young children, older person, and people with hearing impairment, but the benefits seem to outweigh the harm | |||
| İpek S et al. 2021 [66] | Experimental study | English | 34 healthcare workers wore surgical mask one day and a N95 mask on the next day, both for 1–4 h. After removing the mask, capillary blood gases were taken, and a questionnaire was given | With N95 mask: 59% headache, 27% palpitation, 80% respiratory distress, 47% feeling of dizziness, drowsiness, 11% nausea, 53% face sweating, 59% suffocation, 50% attention deficit disorder, 62% concentration problems, 62% fatigue, 9% feeling of death. With surgical mask 15% headache, 24% respiratory distress, 6% feeling of dizziness, drowsiness, 27% face sweating, 6% suffocation, 15% attention deficit disorder, 18% concentration problems, 15% fatigue, 3% feeling of death. The symptoms were worse with N95 masks | |||
| Mask re-use | 3 | Scalvenzi M et al. 2020 [68] | Survey | English | 2562 patients of a dermatological clinic in Italy completed a questionnaire | 98.2%, regularly use masks, 1.8% not use any masks; 42.3% use mask 1–3 h/day, 23.8% use PPE 3–5 h/day, 18.3% use PPE less 1 h/day, 34.2% use of surgical mask before changing it for 3–4 h, 30.7% 1 day, 25.8% 2–5 days,6.5% 1 week, 2.8% more than 11 weeks. Use of FFP2 before changing it for about 12 h in 21.6%,1 day in 20.8%, 2–5 days in 28%, 1 week in 21.4%, more than 1 week in 8.3%. Use of FFP3 before changing it for about 12 h in 18.3%, 1 day in 18.7%, 2–5 days in 26.5%,1 week in 23%, more than 1 week in 13.5% | |
| Duong MC et al. 2021 [67] | Cross- sectional Study | English | 728 university students from Vietnam answered a self- developed questionnaire | 43% of respondents re-use the mask, 28.8% wash the mask after each use and 64.4% after every day of use, 5.5% after some days of use but less than a week, and 1.3% after every week of use | |||
| Cho Kwan R et al. 2021 [69] | Survey | English | 355 respondents an online survey about the correlation between depressive symptoms, health beliefs regarding COVID-19, and face mask use and reuse | There was a correlation between depressive symptoms and health beliefs, because depressive symptoms were more evident among older people who reused face masks, had a stronger belief in disease severity, and did not have adequate cues to preventive measures | |||
Key lessons from all the papers are that each group may experience challenges to wearing masks. In each category there are specific challenges. These include the following:
Discomfort (in all groups).
Impact on respiratory function in people with respiratory disease, children, elderly, people with heart disease.
Irritation of the skin especially for people with skin disease.
Communication problems for people with a hearing loss.
Issues with mask reuse.
Side effects with respirators [53–56] include concentration problems, reduced working capacity [56], respiratory difficulties [48, 56–58], fogging glasses, difficulty with facial recognition and psychiatric symptoms. Headache was reported after prolonged use.
Discussion
To the best of our knowledge, this is the first systematic review on FMs-related patient safety issues. We have assessed the safety, the risks and/or the respiratory physiological impact of FMs in age ranges or disease categories. We could not pool data as in a meta-analysis, nor could we cover the entire spectrum of diseases as too few papers were retrieved and they were heterogeneous in nature.
In Table 3 we summarize the recommendations based on our review to facilitate safe evidence- based use of FMs in different categories.
Table 3.
Recommendations for a safe use of respiratory protective devices during epidemic outbreaks in different categories of patient
| Category | Number and type of included studies | Sample size | Recommendations (To note that they are based on available evidence) |
|---|---|---|---|
| Pregnant women | No studies includeda | Not applicable |
Use face mask for short periods (1 h), alternating periods of use with others without (e.g., outdoor exit far from other people) Mainly use other prevention measures: avoid places crowded unless strictly necessary Women suffering from rhinitis of pregnancy, may need to change the mask more often because it can be easily moistened, breathing mainly with the mouth In case of difficult breathing or drowsiness, prefer FN95 with valve, keeping in mind the risk of spreading germs to others increases If supplementation with O2 is required, use nasal cannulas or ventimask to be covered with a surgical mask, that is less protective |
| Children |
2 observational studies 1 survey |
20.353 |
In addition to the following recommendation from CDC and American Pediatric Academy: Children over age 2 wear face masks covering over their nose and mouth in community settings where social distancing measures are difficult to maintain If children are playing outside their own homes, it is essential that they remain 6 feet from anyone who is not in their own household. Avoid gathering in groups and try to stay home Keep hands clean Face masks should not be placed: On children under 2, because of the risk of suffocation On children with cognitive impairments who may not tolerate a face mask Special precautions may be needed with these children, such as: Avoiding public areas and maintaining social distancing from others outside their home Putting a light blanket over the baby seat but giving them the ability to breathe comfortably. Make sure that the blanket cannot fall on the baby or that the baby cannot overheat. Never leave the blanket on the baby seat at any time when the baby is not in direct view Face masks with multiple layers of fabric or disposable, surgical-style masks are fine for most people to wear. For a child ensuring the right fit is important. Adult masks are usually 6 × 12 inches, and even a child-sized 5 × 10 inch mask may be too large for young children Children who are considered high-risk or severely immunocompromised are encouraged to wear an N95 mask If children are afraid of wearing a mask, parents should wear masks too, and reassure children emphasizing how they are taking steps to stay safe and to keep other people safe Children could wear a mask at home first. Decorate and personalize the mask. We recommend: Consider pediatric consultation for a tailored risk/benefit evaluation, in case of fragile children, if N95 respirators are required |
|
Chronic lung diseases |
4 experimental studies 3 observational studies |
602 |
People with chronic lung disease should discuss with their physician whether they can attend crowded places and use a respiratory protective device An accurate definition of disease status and a blood gases test at rest and after walking with a mask could be required to state a safe use Even if the face mask is allowed, they should be advised to: Use face mask for short periods (< 2 h), especially during exertion even mild (i.e., walking) Alternate periods of use with others without (e.g., outdoor exit) Practice physical distancing, avoid crowded locations, stay home, keep hands clean |
| Neurologic diseases |
1 observational study 1 review |
55 |
Epilepsy Wear the mask in crowded situations (i.e., malls, theme parks, movie theaters, etc.), with intermittent breaks away from others Remove the mask of the patient at the time of a seizure Alzheimer’s Disease: Help people with AD to wear the mask properly |
| Ear-nose-throat diseases |
4 experimental studies 3 observational studies 1 survey 1 review 1 editorial |
604 |
(a) People with hearing impairment Use speech-to-text mobile apps, available on the most popular cellular application stores, written scripts (e.g., Chalkboard) and masks with a plastic transparent panel over the mouth, which make the lip reading easier (b) Laryngectomized patients Leave the house only if necessary Do not procrastinate necessary medical consultation Constantly use HME filter on the top of tracheotomy tube; it ensures adequate filtering, heating and humidification of the inspired air (remember that it lasts 24 h) The mask should be worn above tracheotomy if patients attend places with a high risk of infection (customized masks can be used): HME filter does not guarantee protection against COVID-19 The only specific stomal device, with proven virus filtering properties available on the market, is the Micron HME. It filters thanks to an electrostatic mechanism and does not compromise patients’ quality of life in term of breathing or speaking functions (for voice prosthesis carriers) The use of nasal and facial protection (e.g., masks or scarfs) to reduce the risk of contact with oral or nasal mucosal surfaces, should not be forgotten Remind that the use of masks and micron HME filters in COVID-19 positive laryngectomized patients are necessary to prevent the spread of the virus, that is easier in this population, thanks to the anatomical conformation of their respiratory tract (c) Allergic and rhinopathic patients Face mask can become a protective factor, helping to filter the pollen grains. In fact, the size of the pollen and of the fungal spores is between 1 and 15 microns (100, 1.000 times larger than the Coronavirus, placed between 0.6 and 0.14 microns), and the mask filter can contribute to reduce the inhalable concentration of these particles leading to a reduction of allergic symptoms |
| Heart diseases | 2 experimental studies | 110 | Limited evidence suggest that N95 use for < 2 h is safe for people with coronary heart disease in a stable state |
| Hemodialysis | 1 observational study | 39 | Prolonged use of N95 in hemodialysis patients should be avoided if possible as it results in reduced pO2 after 4 h |
| Eye Disease |
2 observational study 1 experimental study 1 survey 1 comment |
3.739 | Increased airflow upward caused eye irritation and dryness: to prevent COVID-19 sanitize or wash hands before rubbing irritated eyes or itching due to mask |
| Exercise |
2 experimental studies 1 review |
28 | Low or moderate exercise intensity is recommended, because it prevent obesity, cardiovascular disease and depression, but it could intensify the dyspnea due to the higher face humidity/temperature |
| Side effects and contraindications |
7 observational studies 2 experimental studies 2 surveys 2 commentaries 1 review 1 scoping review 1 letter |
3.467 |
To avoid side effects (headache, pressure on the nose etc.), avoid prolonged face mask wearing, take a break every 2 h Contraindications: Anyone who has trouble breathing Anyone is unconscious, incapacitated, or otherwise unable to remove the mask without assistance |
| Other mask- related patient safety issues |
1 experimental study 1 review 1 observational study |
3 | To avoid communication problem due to the decrease of higher frequencies of speaker’s voice is recommended to use written orders or read-back procedure for high-risk communications, as face masks can impair speech perception in communicating with patients and with colleagues, especially in noisy environment, reduce the background noise, speak slowly and louder, |
aReported recommendations for pregnant women are from CDC (Centre for Disease Prevention and Control).
Published evidence suggests that mask-related safety issues included the following:
Increased breathing resistance with subsequent increased respiratory effort.
Decreased FiO2 and increased FiCO2.
Inconvenience in the face, head, and neck areas, increased humidity, temperature, pressure on the nose, around the ear lobes.
Psychosocial effects.
In addition, there may be inadequate protection to people who cannot tighten their face properly due to malformations or a following an operation of the skull or face.
Pregnant women have an increased risk for severe illness from COVID-19 and are at a higher risk for preterm birth and stillbirth and other pregnancy complications [72]. Interactions between FMs use and pregnancy-related rhinitis, induced airway changes (increased breathing resistance and residual volume loss) and pregnancy-related dyspnea remain to be solved [70]. Wearing FM during childbirth is not associated with any adverse outcome for mothers or newborns [73].
Most of the studies noted that the pandemic negatively affected people’s mental health. Mask- wearing is associated with mask-related panic attacks, worsening mood, depressive symptoms, anxiety and sense of suffocating [48, 49, 57]. People with mental health can have difficulties to follow the recommendations due to their disorders [45, 46]. For example, children with ASD for example, struggle to tolerate FMs for more than 15 minutes [50, 51].
Most people with Alzheimer Disease had no knowledge of the pandemic and did not wear the masks properly even with help, leading to increased risk of infection [34, 35]. We retrieved only an expert opinion paper about people with epilepsy. FMs may induce hyperventilation which can activate seizure activity [74].
People who have had a laryngectomy have an anatomical and/or surgical alteration of the upper airways that enhances susceptibility to contagion. They require multiple protection [75] in people with allergies and rhinopathology FMs have an advantage of preventing exposure to pollen grains [24, 25], but in 70% with and without chronic rhinitis the FM seemed to decrease the quality of life [76].
The literature regarding FMs and eye disease showed that not only there are mask-related symptoms: MADE (mask-associated dry eye), eye irritation and inflammation can cause increased face touching and spread of COVID-19. Artifacts could also occur in the results of the examination of the visual field [29–33].
The literature on physical exercise and FMs is limited. In general, FFP2/N95 masks are perceived as more uncomfortable than surgical mask [27]. Exercising at low or moderate intensity when wearing FM can prevent an increased risk of obesity, cardiovascular disease, and depression [36, 37].
Common SMs are responsible for a loss of hearing more than 20% while F-PPE (e.g. FFP3 masks combined with a face shield) could cause a reduction of almost 70% and significant verbal communication issues [77] to improve intelligibility without altering physical distance, the clinician had to increase the voice volume increasing the risk of loss of confidentiality [78]. Using written order and/or read-back procedure, speech-to-text mobile apps, written scripts (e.g., chalkboard) or masks with a plastic transparent panel over the mouth, make communication easier for hearing impairment patients [79].
In children N95 respirator wearing is associated with a reduced FiO2 and/or SpO2and/or PaO2 and an increased ETCO2 and/or PaCO2, proportionally to the duration of use and disease severity [7]. Recommendations for children are provided by the CDC and the American Academy of Pediatrics [70, 71].
Safety of FMs have not been yet investigated in patients with heart failure, gastroesophageal reflux, obesity, adenoid hypertrophy, and cognitive impairment.
Extended use, reuse, or decontamination of SMs and N95 respirators may result in inferior protection. Some evidence suggests that reused and makeshift mask should be used when medical- grade protection is unavailable [68]. Reuse of masks has also led to a debate given the cost and the environmental impact of discarded masks. The most frequent methods used are the decontamination with hot water and ethanol or specific cleanser because it is more suitable for people to perform at home. Information campaigns are required to promote the correct use of masks and limit the infection rate [68].
With the greater obligation to use FM, some recommendations should be made on legal medical issues. The emergency has forced governments to act based on two opposing and antithetical presumptions. In particular, the policy of mandatory mask wearing was established by assuming that the population was a potential vector of infection and that the use of FMs was free from side effects. However, not being able to go out or enter a place without a mask can be considered a restriction of individual freedoms. Similarly, a contraction of the fundamental and inalienable right to health could occur when the obligation involves individuals suffering from specific pathological conditions which could be aggravated by wearing a mask.
Nonetheless, according to current evidence, the use of FMs is complementary to other measures such as physical distance and hand hygiene. Therefore, to reconcile personal protection with public health needs, it is recommended that we recommend appropriate and safe use [80] of FMs through targeted educational campaigns and more detailed guidelines rather than solely through mandating, because the reduction of the virus and the benefits of wearing FMs outweigh the discomfort [58].
Limitations
We may have missed minor papers with our search strategy as there are no specific terms to univocally indicate protective FMs. In addition, recommendations change when new evidence is published. Finally, published papers do not provide data on major clinically relevant outcomes, such as adverse effect-related diseases or hospitalization. Evidence on respiratory impact in sick/frail subjects and mask-related patient safety issues is limited and heterogeneous; current expert-opinion recommendations need to be validated with large scale studies.
Conclusions
In general, evidence demonstrates that benefits of wearing face masks exceed discomfort; anyway an “air break” after 1–2 hours consecutively of mask-wearing can be a good practice for people with respiratory function compromised by diseases or in particular conditions (i.e. pregnancy, epilepsy, etc.). The present COVID-19 pandemic, where different public health agencies and governments have recommended universal use of FMs, represents a unique opportunity for collecting large amount of real-world data.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights statement and Informed consent
For our research any Ethical Statements/informed consent aren't avaible because is a review of orginal articles and not an experimental study involving human or animals.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Masks4All.(2021) "What Countries RequireMasks in Public or Recommend Masks?" https://masks4all.co/what-countries-require-masks-in-public/ (Last Update December 2021)
- 2.Setti L, Passarini F, De Gennaro G. Airborne transmission route of COVID-19: why 2 meters/6 feet of inter-personal distance could not be enough. Int J Environ Res Public Health. 2020;17(8):2932. doi: 10.3390/ijerph17082932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Food and Drug Administration (2021) N95 Respirators, Surgical Masks, and Face Masks https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-surgical-masks-and-face-masks (Last Update 15th September 2021)
- 4.Center for Disease Prevention and Control (2022). Types of Masks and Respirators, available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/types-of-masks.html. (Last Update 28th January 2022)
- 5.Lazzarino AI, Steptoe A, Hamer M, Michie S. COVID-19: important potential side effects of wearing face masks that we should bear in mind. BMJ. 2020 doi: 10.1136/bmj.m2003. [DOI] [PubMed] [Google Scholar]
- 6.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311:376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goh DYT, Mun MW, Lee WLJ, Teoh OH, Rajgor DD. A randomised clinical trial to evaluate the safety, fit, comfort of a novel N95 mask in children. Sci Rep. 2019;9(1):18952. doi: 10.1038/s41598-019-55451-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lubrano R, Bloise S, Testa A, Marcellino A, Dilillo A, Mallardo S, Isoldi S, Martucci V, Sanseviero M, Del Giudice E, Malvaso C, Iorfida D, Ventriglia F. Assessment of respiratory function in infants and young children wearing face masks during the COVID-19 pandemic. Jama Netw Open. 2021;4(3):e210414. doi: 10.1001/jamanetworkopen.2021.0414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwarz S, Jenetzky E, Krafft H, Maurer T, Martin D. Coronakinderstudien „Co-Ki “: erste Ergebnisse eines deutschlandweiten Registers zur Mund-Nasen-Bedeckung (Maske) bei Kindern [Corona child studies "Co-Ki": first results of a Germany-wide register on mouth and nose covering (mask) in children] Monatsschr Kinderheilkd. 2021;169(4):353–365. doi: 10.1007/s00112-021-01133-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kyung SY, Kim Y, Hwang H, Park JW, Jeong SH. Risks of N95 face mask use in subjects with COPD. Respir Care. 2020;65(5):658–664. doi: 10.4187/respcare.06713. [DOI] [PubMed] [Google Scholar]
- 11.Bansal S, Harber P, Yun D, Liu D, Liu Y, Wu S, Ng D, Santiago S. Respirator physiological effects under simulated work conditions. J Occup Environ Hyg. 2009;6(4):221–227. doi: 10.1080/15459620902729218. [DOI] [PubMed] [Google Scholar]
- 12.Harber P, Yun D, Santiago S, Bansal S, Liu Y. Respirator impact on work task performance. J Occup Environ Med. 2011;53(1):22–26. doi: 10.1097/JOM.0b013e3181febc75. [DOI] [PubMed] [Google Scholar]
- 13.Schönhofer B, Rosenblüh J, Kemper P, Voshaar T, Köhler D. Einfluss des Mundschutzes auf die Atemarbeit bei Patienten mit chronischer Belastung der Atempumpe [Effect of a face mask on work of breathing in patients with chronic obstructive respiratory disease] Pneumologie. 1995;49(Suppl 1):209–211. [PubMed] [Google Scholar]
- 14.Samannan R, Holt G, Calderon-Candelario R, Mirsaeidi M, Campos M. Effect of face masks on gas exchange in healthy persons and patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2021;18(3):541–544. doi: 10.1513/AnnalsATS.202007-812RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ciocan C, Clari M, Fabbro D, De Piano ML, Garzaro G, Godono A, Gullino A, Romano C. Impact of wearing a surgical mask on respiratory function in view of a widespread use during COVID-19 outbreak. A case – series study. Med Lav. 2020;111(5):354–364. doi: 10.23749/mdl.v111i5.9766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Faria N, Costa MI, Gomes J, Sucena M. Reduction of severe exacerbations of COPD during COVID-19 pandemic in Portugal: a protective role of face masks? COPD. J Chronic Obstr Pulm Dis. 2021 doi: 10.1080/15412555.2021.1904387. [DOI] [PubMed] [Google Scholar]
- 17.Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686–695. doi: 10.3766/jaaa.19.9.4. [DOI] [PubMed] [Google Scholar]
- 18.Chodosh J, Weinstein BE, Blustein J. Face masks can be devastating for people with hearing loss. BMJ. 2020 doi: 10.1136/bmj.m2683. [DOI] [PubMed] [Google Scholar]
- 19.Ten Hulzen RD, Fabry DA. Impact of hearing loss and universal face masking in the COVID-19 Era. Mayo Clin Proc. 2020;95(10):2069–2072. doi: 10.1016/j.mayocp.2020.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atcherson SR, Mendel LL, Baltimore WJ, Patro C, Lee S, Pousson M, Spann MJ. The effect of conventional and transparent surgical masks on speech understanding in individuals with and without hearing loss. J Am Acad Audiol. 2017;28(1):58–67. doi: 10.3766/jaaa.15151. [DOI] [PubMed] [Google Scholar]
- 21.Trecca EMC, Gelardi M, Cassano M. COVID-19 and hearing difficulties. Am J Otolaryngol. 2020;41(4):102496. doi: 10.1016/j.amjoto.2020.102496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Langrish JP, Li X, Wang S, Lee MM, Barnes GD, Miller MR, Cassee FR, Boon AN, Donaldson K, Li J, Li L, Millis LN, Newby DE, Jiang L. Reducing personal exposure to particulate air pollution improves cardiovascular health in patients with coronary heart disease. Environ Health Perspect. 2012;120(3):367–372. doi: 10.1289/ehp.1103898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vos TG, Dillon MT, Buss E, Rooth MA, Bucker AL, Dillon S, Pearson A, Quinones K, Richter ME, Roth N, Young A, Dedmon MM. Influence of protective face coverings on the speech recognition of cochlear implant patients. Laryngoscope. 2021;00:1–6. doi: 10.1002/lary.29447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dror AA, Eisenbach N, Marshak T, Layous E, Zigron A, Shivatzki S, Morozov NG, Taiber S, Alon EE, Ronen O, Zusman E, Srouji S, Sela E. Reduction of allergic rhinitis symptoms with face mask usage during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8:10. doi: 10.1016/j.jaip.2020.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kishore Dayal A, Sinha V. Trend of allergic rhinitis post COVID-19 pandemic: a retrospective observational study. Indian J Otolaryngol Head Neck Surg. 2020 doi: 10.1007/s12070-020-02223-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klimek L, Huppertz T, Alali A, Spielhaupter M, Hörmann K, Matthias C, Hagemann J. A new form of irritant rhinitis to filtering facepiece particle (FFP) masks (FFP2/N95/ KN95 respirators) during COVID- 19 pandemic. World Allergy Organ J. 2020;13:100474. doi: 10.1016/j.waojou.2020.100474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fikenzer S, Uhe T, Lavall D, Rudolph U, Falz R, Busse M, Hepp P, Laufs U. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin Res Cardiol. 2020;109(12):1522–1530. doi: 10.1007/s00392-020-01704-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kao TW, Huang KC, Huang YL, Tsai TJ, Hsieh BS, Wu MS. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc. 2004;103(8):624–628. [PubMed] [Google Scholar]
- 29.Laura B. Self-reported symptoms of mask-associated dry eye: a survey study of 3605 people. Contact Lens Anterior Eye. 2021 doi: 10.1016/j.clae.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moshirfar M, West WB, Marx DP. Face mask-associated ocular irritation and dryness. Ophthalmol Ther. 2020;9:397–400. doi: 10.1007/s40123-020-00282-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bayram N, Gundogan M, Ozsaygili C, Vural E, Cicek A. The impacts of face mask use on standard automated perimetry results in glaucoma patients. J Glaucoma. 2021;30(4):287–292. doi: 10.1097/IJG.0000000000001786. [DOI] [PubMed] [Google Scholar]
- 32.Young SL, Smith ML, Tatham AJ. Visual field artifacts from face mask use. J Glaucoma. 2020;29:989–991. doi: 10.1097/IJG.0000000000001605. [DOI] [PubMed] [Google Scholar]
- 33.El-Nimri NW, Moghimi S, Fingeret M, Weinreb RN. Visual field artifacts in glaucoma with face mask use during the COVID-19 pandemic. J Glaucoma. 2020;29:1184–1188. doi: 10.1097/IJG.0000000000001706. [DOI] [PubMed] [Google Scholar]
- 34.Gil R, Arroyo-Anllò EM. Alzheimer’s disease and face masks in times of COVID-19. J Alzheimer’s Dis. 2020 doi: 10.3233/JAD-201233. [DOI] [PubMed] [Google Scholar]
- 35.Kobayashi R, Hayashi H, Kawakatsu S, Morioka D, Aso S, Kimura M, Otani K. Recognition of the coronavirus disease 2019 pandemic and face mask wearing in patients with Alzheimer’s disease: an investigation at a medical center for dementia in Japan. Psychogeriatrics. 2021 doi: 10.1111/psyg.12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Epstein D, Korytny A, Isenberg Y, Marcusohn E, Zukermann R, Bishop B, Raz MS, S, Miller A. Return to training in the COVID-19 era: the physiological effects of face masks during exercise. Scand J Med Sci Sport. 2021;31(1):70–75. doi: 10.1111/sms.13832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chandrasekaran B, Fernandes S. Exercise with facemask; are we handling a devil's sword? – A physiological hypothesis. Med Hypotheses. 2020;144:110002. doi: 10.1016/j.mehy.2020.110002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Veraldi S, Angileri L, Barbareschi M. Seborrheic dermatitis and anti-COVID-19 masks. J Cosmet Dermatol. 2020;19(10):2464–2465. doi: 10.1111/jocd.13669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zuo Y, Hua W, Luo Y, Li L. Skin reactions of N95 masks and medial masks among health-care personnel: a self-report questionnaire survey in China. Contact Dermatitis. 2020;83(2):145–147. doi: 10.1111/cod.13555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Szepietowski JC, Matusiak L, Szepietowska M, Krajewski PK, Białynicki-Birula R. Face mask-induced itch: a self-questionnaire study of 2.315 responders during the COVID-19 pandemic. Acta Derm Venereol. 2020;100(10):adv00152. doi: 10.2340/00015555-3536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Han C, Shi J, Chen Y, Zhang Z. Increased flare of acne caused by long-time mask wearing during COVID- 19 pandemic among general population. Dermatol Ther. 2020;33(4):e13704. doi: 10.1111/dth.13704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park S, Han J, Yeon YM, Kang NY, Kim E. Effect of face mask on skin characteristics changes during the COVID-19 pandemic. Skin Res Technol. 2020 doi: 10.1111/srt.12983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Han HS, Shin SH, Park JW, Li K, Kim BJ, Yoo KH. Changes in skin characteristics after using respiratory protective equipment (medical masks and respirators) in the COVID-19 pandemic among health care workers. Contact Dermat. 2021 doi: 10.1111/cod.13855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Techasatian L, Lebsing S, Uppala R, Thaowandee W, Chaiyarit J, Supakunpinyo C, Panombualert S, Mairiang D, Saengnipanthkul S, Wichajarn K, Kiatchoosakun P, Kosalaraksa P. The effects of the face mask on the skin underneath: a prospective survey during the COVID-19 pandemic. J Prim Care Community Health. 2020;11:1–7. doi: 10.1177/2150132720966167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jung H, Park C, Kim M, Jhon M, Kim J, Ryu S, Lee J, Kim J, Park K, Jung YB, Kim S. Factors associated with mask wearing among psychiatric inpatients during the COVID-19 pandemic. Schizophr Res. 2021;228:235–236. doi: 10.1016/j.schres.2020.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Uvais NA. Use of face masks among patients with psychiatric illnesses during the COVID-19 pandemic: a hospital-based cross-sectional study. Prim Care Companion CNS Disord. 2020;22(6):20br02789. doi: 10.4088/PCC.20br02789. [DOI] [PubMed] [Google Scholar]
- 47.Soh KC, Khanna R, Parsons A, Visa B, Ejareh DM. Masks in Melbourne: an inpatient mental health unit’s COVID-19 experience. Australas Psychiatry. 2021;29(2):240–241. doi: 10.1177/1039856220968394. [DOI] [PubMed] [Google Scholar]
- 48.Battista RA, Ferraro M, Piccioni LO, Malzanni GE, Bussi M. Personal protective equipment (PPE) in COVID 19 pandemic: related symptoms and adverse reactions in healthcare workers and general population. J Occup Environ Med. 2021;63(2):e80–e85. doi: 10.1097/JOM.0000000000002100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wu S, Harber P, Yun D, Bansal S, Li Y, Santiago S. Anxiety during respirator use: comparison of two respirator types. J Occup Environ Hyg. 2011;8(3):123–128. doi: 10.1080/15459624.2011.549780. [DOI] [PubMed] [Google Scholar]
- 50.Sivaraman M, Virues-Ortega J, Roeyers H. Telehealth mask wearing training for children with autism during the COVID-19 pandemic. J Appl Behav Anal. 2020;54(1):70–86. doi: 10.1002/jaba.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Halbur M, Kodak T, McKee M, Carroll R, Preas E, Reidy J, Cordeiro MC. Tolerance of face coverings for children with autism spectrum disorder. J Appl Behav Anal. 2021;54(2):600–617. doi: 10.1002/jaba.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kalra S, Chaudhary S, Kantroo V, Ahuja J. Mask fatigue. J Pak Med Assoc. 2020;70:12. [PubMed] [Google Scholar]
- 53.Lim EC, Seet RC, Lee KH, Wilder-Smith EP, Chuah BY, Ong BK. Headaches and the N95 facemask amongst healthcare providers. Acta Neurol Scand. 2006;113(3):199–202. doi: 10.1111/j.1600-0404.2005.00560.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ong JJY, Bharatendu C, Goh Y, Tang JZY, Sooi KWX, Tan YL, Tan BYQ, Teoh HL, Ong ST, Allen DM, Sharma VK. Headaches associated with personal protective equipment - a cross-sectional study among frontline healthcare workers during COVID-19. Headache. 2020;60(5):864–877. doi: 10.1111/head.13811. [DOI] [PubMed] [Google Scholar]
- 55.Ramirez-Moreno JM, Ceberino D, Gonzalez Plata A, Rebollo B, Macias Sedas P, Hariramani R, Roa AM, Constantino AB. Mask-associated ‘de novo’ headache in healthcare workers during the COVID-19 pandemic. Occup Environ Med. 2020;78(8):548–554. doi: 10.1136/oemed-2020-106956. [DOI] [PubMed] [Google Scholar]
- 56.Farronato M, Boccalari E, Del Rosso E, Valentina Lanteri V, Mulder R, Maspero C. A scoping review of respirator literature and a survey among dental professionals. Int J Environ Res Public Health. 2020;17(16):5968. doi: 10.3390/ijerph17165968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cheok GJW, Gatot C, Sim CHS, Ng YH, Tay KXK, Howe TS, Koh JSB. Appropriate attitude promotes mask wearing in spite of a significant experience of varying discomfort. Infect Dis Health. 2021;26(2):145–151. doi: 10.1016/j.idh.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Scheid JL, Lupien SP, Ford GS, West SL. Commentary: physiological and psychological impact of face mask usage during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:6655. doi: 10.3390/ijerph17186655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Honarbakhsh M, Jahangiri M, Farhadi P. Effective factors on not using the N95 respirators among health care workers: application of Fuzzy Delphi and Fuzzy analytic hierarchy process (FAHP) J Healthc Risk Manag. 2017;37(2):36–46. doi: 10.1002/jhrm.21286. [DOI] [PubMed] [Google Scholar]
- 60.MacIntyre CR, Wang Q, Cauchemez S, Seale H, Dwyer ED, Yang P, Shi W, Gao Z, Pang X, Zhang Y, Wang X, Duan W, Rahman B, Ferguson N. A cluster randomized clinical trial comparing fit-tested and non-fit-tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers. Influenza Other Respir Viruses. 2011;5(3):170–179. doi: 10.1111/j.1750-2659.2011.00198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Czypionka T, Greenhalgh T, Bassler D, Bryant MB. Masks and face coverings for the lay public: a narrative update. Ann Intern Med. 2021;174(4):511–520. doi: 10.7326/M20-6625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thomas F, Allen C, Butts W, Rhoades C, Brandon C, Handrahan DL. Does wearing a surgical facemask or N95-respirator impair radio communication? Air Med J. 2011;30(2):97–102. doi: 10.1016/j.amj.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 63.Baig AS, Knapp C, Eagan AE, Radonovich LJ., Jr Health care workers' views about respirator use and features that should be included in the next generation of respirators. Am J Infect Control. 2010;38(1):18–25. doi: 10.1016/j.ajic.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Or PP, Chung JW, Wong TK. A study of environmental factors affecting nurses' comfort and protection in wearing N95 respirators during bedside procedures. J Clin Nurs. 2018;27(7–8):e1477–e1484. doi: 10.1111/jocn.14268. [DOI] [PubMed] [Google Scholar]
- 65.Bothra A, Das S, Singh M, Pawar M, Meheswari A. Retroauricular dermatitis with vehement use of ear loop face masks during COVID19 pandemic. J Eur Acad Dermatol Venereol. 2020;34(10):e549–e552. doi: 10.1111/jdv.16692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.İpek S, Yurttutan S, Güllü UU, Dalkıran T, Acıpayam C, Doğaner A. Is N95 face mask linked to dizziness and headache? Int Arch Occup Environ Health. 2021 doi: 10.1007/s00420-021-01665-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Duong MC, Nguyen HT, Duong BT. A cross-sectional study of knowledge, attitude, and practice towards face mask use amid the COVID-19 pandemic amongst university students in Vietnam. J Community Health. 2021;46(5):975–981. doi: 10.1007/s10900-021-00981-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Scalvenzi M, Villani A, Ruggiero A. Community knowledge about the use, reuse, disinfection and disposal of masks and filtering facepiece respirators: results of a study conducted in a dermatology clinic at the university of Naples in Italy. J Community Health. 2020;46(4):786–793. doi: 10.1007/s10900-020-00952-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cho Kwan R, Hong Lee P, Sze Ki Cheung D, Ching Lam S. Face mask wearing behaviors, depressive symptoms, and health beliefs among older people during the COVID-19 pandemic. Front Med. 2021;8:590936. doi: 10.3389/fmed.2021.590936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Centers for Disease Control and Prevention (2021) Coronavirus disease 2019 (COVID-19). Children, teens, and young adults. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/caring-for-children.html (Last Update 2nd August 2021)
- 71.American Academy of Pediatrics (2022) Masks and children during COVID-19 https://www.healthychildren.org/English/health-issues/conditions/COVID-19/Pages/Cloth-Face-Coverings-for-Children-During-COVID-19.aspx (Last Update 12th January 2022)
- 72.Center for Disease Prevention and Control (2022) Pregnant and recently pregnant people at increased risk for severe illness from COVID-19 https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html. (Last Update 24th January 2022)
- 73.Dap M, Bertholdt C, Belaisch-Allart J, Huissoud C, Morel O. Le port du masque pendant les efforts expulsifs: quel impact réel surles modalité s d’accouchement? [Wearing a mask during childbirth: what real impact on delivery issues?] Gynécologie, Obstétrique, Fertilité Sénologie. 2021;49:95–96. doi: 10.1016/j.gofs.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Asadi-Pooya AA, Cross JH. Is wearing a face mask safe for people with epilepsy? Acta Neurol Scand. 2020 doi: 10.1111/ane.13316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Parrinello G, Missale F, Sampieri C, Carobbio ALC, Peretti G. Safe management of laryngectomized patients during the COVID-19 pandemic. Oral Oncol. 2020;107:104742. doi: 10.1016/j.oraloncology.2020.104742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Primov-Fever A, Amir O, Roziner I, Maoz-Segal R, Alon EE, Yakirevitch A. How face masks influence the sinonasal quality of life during the COVID-19 pandemic. Eur Arch Oto-Rhino- Laryngol. 2021;27:1–7. doi: 10.1007/s00405-021-06752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Muzzi E, Chermaz C, Castro V, Zaninoni M, Saksida A, Orzan E. Short report on the effects of SARS-CoV-2 face protective equipment on verbal communication. Eur Arch Otorhinolaryngol. 2021;278(9):3565–3570. doi: 10.1007/s00405-020-06535-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Marler H, Ditton A. “I’m smiling back at you”: Exploring the impact of mask wearing on communication in healthcare. Int J Lang Commun Disord. 2021;56(1):205–214. doi: 10.1111/1460-6984.12578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.West JS, Franck KH, Welling DB. Providing health care to patients with hearing loss during COVID-19 and physical distancing. Laryngoscope Investig Otolaryngol. 2020;5(3):396–398. doi: 10.1002/lio2.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Greenhalgh T, Schmid MB, Czypionka T, Bassler D, Gruer L. Face masks for the public during the COVID- 19 crisis. BMJ. 2020;369:m1435. doi: 10.1136/bmj.m1435. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


