Fibrolamellar hepatocellular carcinoma (FLC) is a rare form of liver cancer that usually affects children and young adults without underlying cirrhosis. Hyperammonemic encephalopathy (HAE) has been reported in patients with FLC, but the pathogenesis and optimal management of hyperammonemia (HA) in FLC are unclear. We report on two cases of HAE in patients with FLC and preserved liver function. The successful management of HA with surgical debulking of FLC tumors is described.
Case 1
A 26-year-old male with a 2-year history of FLC developed progressive somnolence and disorientation. Treatment history for FLC had included cytotoxic chemotherapy, lenvatinib, and immunotherapy. A CT scan confirmed extensive-stage FLC with numerous liver, lung, and pelvic metastasis. Laboratory results showed bilirubin 0.3 mg/dL, creatinine 0.4 mg/dL, leukocytes of 9.5 × 109/L, hemoglobin 11.2 g/dL, platelets 369 × 109/L, and ammonia 247 μmol/L (reference range, 0–32). Plasma amino acid analysis revealed relatively low citrulline (14 μmol/L), arginine (32 μmol/L), and ornithine (35 μmol/L). Urinary orotic acid excretion was markedly elevated at 149 mmol/mol creat (reference range, 0.68–3.52).
The patient was treated with i.v. sodium benzoate and sodium phenylacetate, arginine hydrochloride, and dextrose 10% (D10) 0.45% normal saline. He was transitioned to oral glycerol phenylbutyrate, but developed worsening HA over time. Approximately 6 weeks later, he underwent an extensive debulking surgery as a treatment for refractory HA in the setting of advanced FLC, including resection of the descending colon and en bloc resection of retroperitoneal nodules and pelvic masses, collectively removing ~50% of the tumor volume. The patient’s ammonia levels significantly improved (Fig. 1), and his lethargy and disorientation resolved.
FIG. 1.
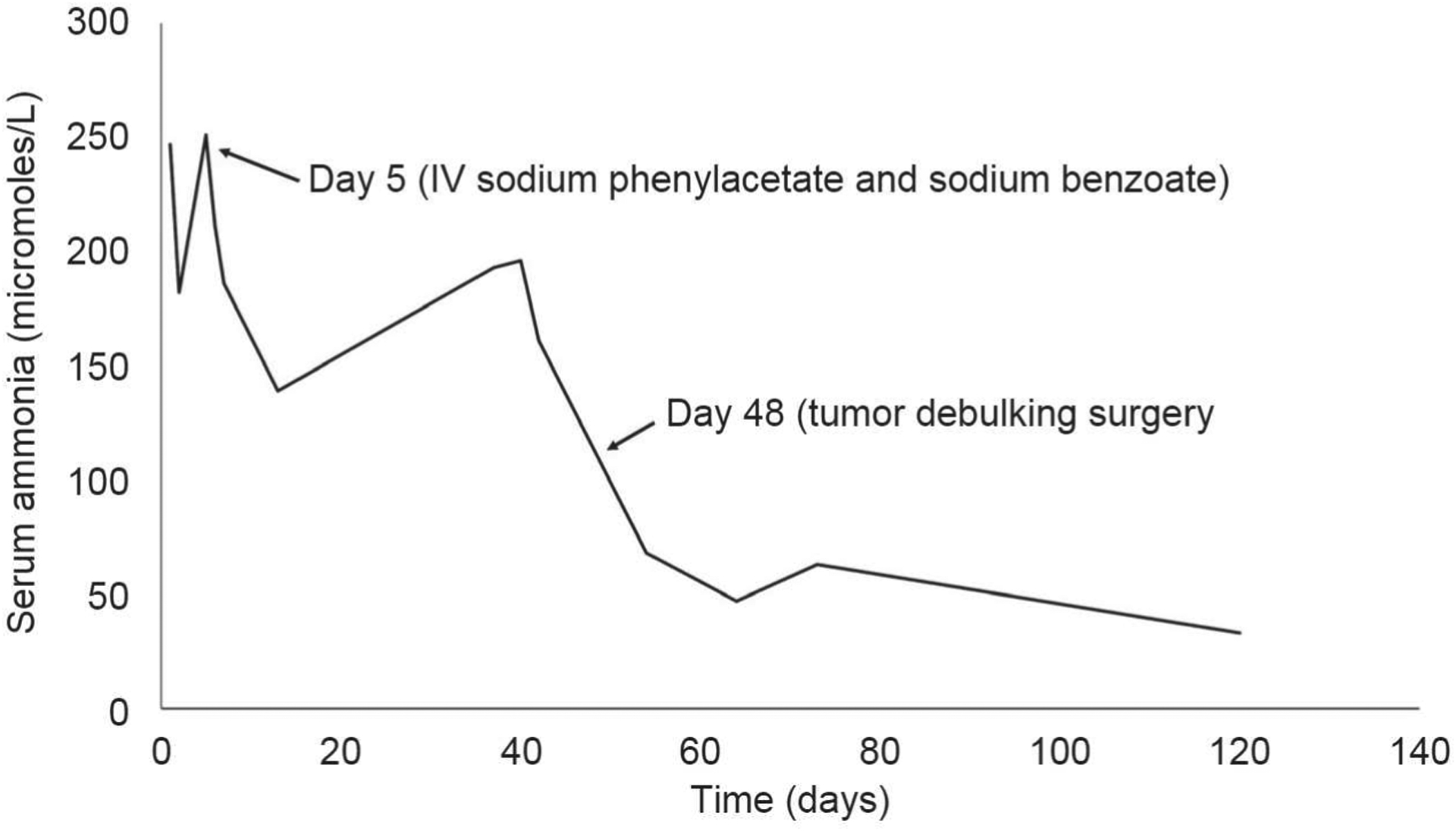
Trend in ammonia levels over time.
Case 2
A 25-year-old male with a recent diagnosis of FLC ~1 month earlier presented to the emergency room after his mother found him unarousable in bed. He was intubated upon arrival for airway protection. He had two previous hospital admissions for HAE over the preceding 3 weeks. He was receiving outpatient treatment for his FLC with gemcitabine plus oxaliplatin.
Laboratory results showed bilirubin 0.3 mg/dL, creatinine 1.17 mg/dL, leukocytes of 9.5 × 109/L, hemoglobin 11.2 g/dL, platelets 369 × 109/L, and ammonia 347 μmol/L. Plasma amino acid analysis revealed low citrulline (0 μmol/L), arginine (30 μmol/L), and ornithine (20 μmol/L). He received i.v. sodium benzoate and sodium phenylacetate, as well as arginine hydrochloride. However, his refractory HA required concurrent treatment with continuous venovenous hemofiltration (CVVH) and rebounded rapidly if either CVVH or i.v. nitrogen scavenging was discontinued. It was determined that the patient was unlikely to be safely discharged unless a more definitive solution for his HA could be established. A CT scan revealed a 9-cm lesion in the left liver and diffuse peritoneal metastatic disease. The patient was offered a palliative debulking surgery for his cancer, including left hepatectomy and omentectomy, with an estimated removal of 50% of his total tumor volume. After surgery, he was successfully transitioned to oral glycerol phenylbutyrate and l-citrulline with ammonias of 80–100 μmol/L as an outpatient.
Discussion
HAE has been reported in patients with FLC.(1) FLC generally occurs in young patients with preserved liver function, and previous cases of FLC-associated HAE have not been linked to hepatic impairment. Portosystemic shunting or anatomical compression of the liver vasculature resulting in impaired nitrogen clearance is a potential mechanism for HA(1); however, the degree of HA in these cases was out of proportion to the degree of shunting. In both cases, HA improved with surgical tumor debulking, supporting a direct link between FLC and HA. Although the threshold of tumor reduction necessary to ameliorate HA in FLC is unknown, ~50% tumor reduction was sufficient in both cases and may be a reasonable goal for surgical debulking. It has been proposed that FLC may result in HA through consumption of ornithine for polyamine synthesis, which reduces the availability of ornithine for the proximal urea cycle.(2) The striking orotic aciduria and low citrulline in our patients, and the response to surgical tumor debulking, supports this mechanism. Our proposed management of FLC-associated HA (Table 1) draws from experience in managing ornithine transcarbamylase deficiency. Pharmacological treatment of HA using nitrogen scavengers, and more definitive options focusing on decreasing the tumor volume, including tumor debulking surgery, should be considered in these patients. Further exploration into the pathophysiology and treatment of HA in FLC is necessary to refine treatment approaches.
TABLE 1.
Suggested Management of HA in FLC
| Management Options | Commonly Used Measures |
|---|---|
| Outpatient management | Oral nitrogen scavenger (e.g., sodium phenylbutyrate, glycerol phenylbutyrate) and l-citrulline |
| Emergent cases | CVVH; i.v. sodium benzoate and sodium phenylacetate, arginine hydrochloride, and D10-based fluids |
| Refractory to medical therapy | Consideration of debulking surgery to reduce FLC tumor volume, in conjunction with medical management, when feasible, and consistent with the overall goals of care |
Acknowledgments
This work was partly supported by the grant from Fibrolamellar Cancer Foundation (to Dr. Mark Yarchoan), NCI Specialized Program of Research Excellence (SPORE) in Gastrointestinal Cancers (P50 CA062924), and the NIH Center Core Grant (P30 CA006973).
Abbreviations:
- CVVH
continuous venovenous hemofiltration
- FLC
fibrolamellar cancer
- HA
hyperammonemia
- HAE
hyperammonemic encephalopathy
Footnotes
Potential conflict of interest: Nothing to report.
Informed Consent
Informed consent was obtained from the patients.
REFERENCES
- 1).Cho J, Chen JCY, Paludo J, Conboy EE, Lanpher BC, Alberts SR, et al. Hyperammonemic encephalopathy in a patient with fibrolamellar hepatocellular carcinoma: case report and literature review. J Gastrointest Oncol 2019;10:582–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Surjan RC, dos Santos ES, Basseres T, Makdissi FF, Machado MA. A proposed physiopathological pathway to hyperammonemic encephalopathy in a non-cirrhotic patient with fibrolamellar hepatocellular carcinoma without ornithine transcarbamylase (OTC) mutation. Am J Case Rep 2017;18:234–241. [DOI] [PMC free article] [PubMed] [Google Scholar]


