Several case series have described acute myocarditis developing shortly after receiving messenger ribonucleic acid (mRNA) COVID-19 vaccines.1 Cardiac magnetic resonance (CMR) characteristics in these patients resemble those found in patients with myocarditis from other causes. However, no prior reports or studies describe the evolution of myocardial edema and late gadolinium enhancement (LGE) on serial CMR evaluation—data that may help define the natural course of the disease.
In this case series, we describe the clinical course and repeat CMR findings after 3-6 months in 9 young male patients diagnosed with acute myocarditis after receiving an mRNA-based COVID-19 vaccine. All patients developed acute myocarditis within 72 hours of receiving the second dose of COVID-19 vaccination, and they underwent initial CMR within 7 days of their hospital stay. Acute myocarditis was diagnosed based on clinical presentation (typical chest pain symptoms, electrocardiogram, and elevated cardiac biomarkers) and the presence of modified Lake Louise criteria on T1- and/or T2-weighted CMR images.2 All CMR studies were performed on 1.5-T scanners using a standard myocarditis protocol based on guidelines from the Society for Cardiovascular Magnetic Resonance. All CMR studies were analyzed off-line using CVi42 (Circle Cardiovascular Imaging) by a level III reader. Follow-up evaluation for recurrent chest pain, hospital readmission, heart failure, and arrhythmias were obtained from outpatient cardiology clinic notes after index hospitalization discharge. The study was approved by the Institutional Review Board of the Lifespan Health System.
The mean age of the cohort was 22 years. None of the patients had a history of COVID-19 infection prior to the diagnosis of acute myocarditis. Two patients received Moderna COVID-19 vaccination and 7 patients received Pfizer COVID-19 vaccination. Over a median follow-up of 146 days, none of the patients experienced recurrent myocarditis, heart failure, or arrhythmias and none were readmitted to the hospital for any cause.
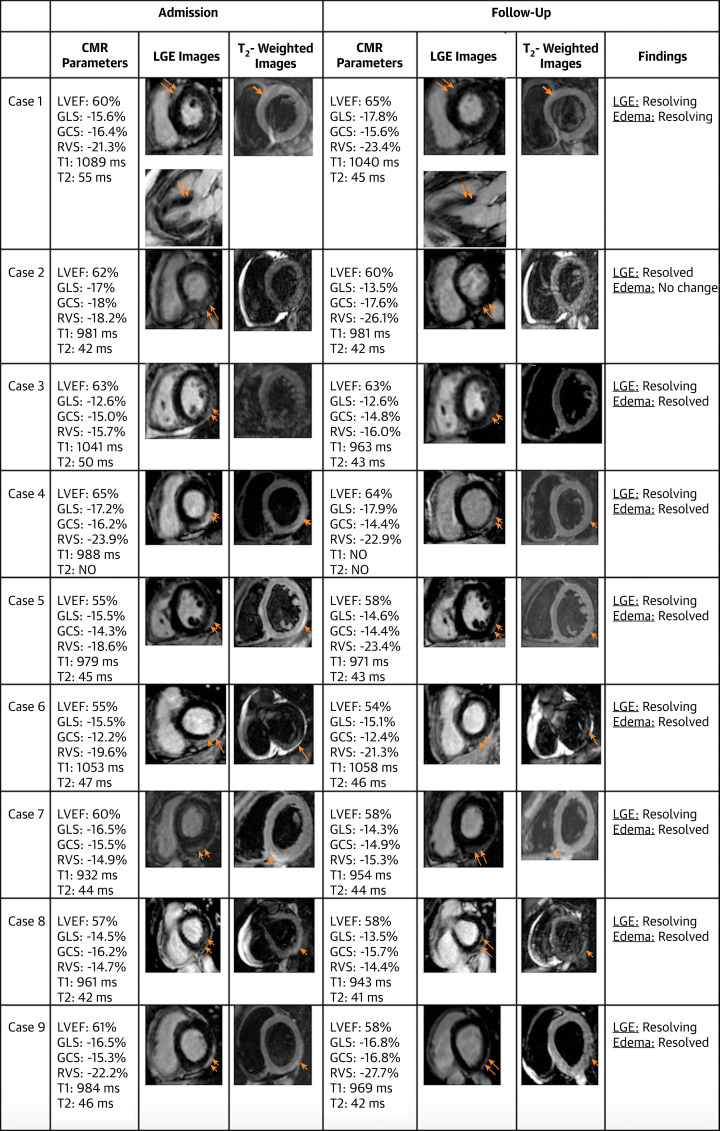
Follow-up CMR findings after a median of 94 days following initial diagnosis of acute myocarditis in these patients are shown in Figure 1 . During the index hospitalization for acute myocarditis, subclinical myocardial dysfunction (defined by left ventricular global longitudinal strain [GLS] and/or global circumferential strain [GCS] <−17%) was present in 8 of 9 patients. On follow-up, left ventricular GLS remained mildly abnormal in 7 of 8 patients and left ventricular GCS remained mildly abnormal in 8 of 9 patients. Similarly, right ventricular GLS was abnormal (<−23.9%) in all 9 patients at baseline, and although there was a numerical improvement in right ventricular GLS in all patients on the follow-up, only 2 of 9 patients had GLS value of >−23.9% on the follow-up. There was complete resolution of myocardial edema in 8 of 9 patients on T2-weighted images. LGE was present initially in all cases. On follow-up, there was resolution of LGE in 1 of 9 patients and resolving but persistent LGE in 8 of 9 patients.
Figure 1.
CMR Characteristics on Admission and on Follow-Up Among 9 Young-Adult Male Patients With Acute Myocarditis Following mRNA-Based COVID-19 Vaccination
Hyperintense signal suggestive of myocardial edema on T2-weighted fat suppression (single arrow) and late gadolinium enhancement on T1-weighted images (double arrow). All cardiac magnetic resonance (CMR) studies were performed on 1.5-T Siemens magnetic resonance imaging scanner. Global longitudinal strain (GLS) of the left ventricle was evaluated using feature tracking (CVi42) from apical long-axis views containing 4-, 3-, and 2-chamber cine views. Global circumferential strain (GCS) of the left ventricle was obtained using feature tracking on short-axis cine views. Similarly, GLS of the right ventricle was used with feature-tracking method in apical 4-chamber view. The peak strain values for GLS (negative value) and GCS (negative value) were determined from the strain curves. The reference value of left ventricular GLS and GCS was −17%, whereas the reference value of right ventricular GLS was −23.9%. T1- and T2-weighted mapping: myocardial native T1 maps were obtained on 1.5-T using a breath-hold, motion-correction, electrocardiogram-triggered, modified Look-Locker inversion recovery sequence with images acquired at end diastole before and approximately 20 minutes after contrast injection in the mid-ventricular short-axis plane. T2 mapping was performed on 1.5-T using a single-shot T2 prepared steady-state free precision in the mid-ventricular short-axis plane at end diastole during breath-hold with motion correction. LGE = late gadolinium enhancement; LVEF = left ventricular ejection fraction; mRNA = messenger ribonucleic acid; NO = not obtained; RVS = right ventricular strain.
CMR can help determine longer-term prognosis in patients with acute myocarditis.3 The ITAMY (Italian Study in Myocarditis) registry showed that the presence of any LGE without myocardial edema compared to the absence of LGE on 6-month follow-up was associated with an increased risk of adverse cardiac events including sudden cardiac death, implantable cardioverter-defibrillator shocks, and heart failure hospitalization.4 In this case series, we found that most of our patients have resolving LGE without the presence of myocardial edema on follow-up. It is likely that the persistence of LGE in the absence of myocardial edema represents myocardial fibrosis. Given that no clinical events were observed in our short-term follow-up, these tissue-related imaging findings likely portend a more favorable prognosis in the short term, but a long-term follow-up is needed to determine whether such persistence of LGE is associated with future cardiac events.
Reduced left ventricular GLS and GCS in patients with acute myocarditis have been reported to be associated with worse cardiovascular outcomes.5 In our case series, we found persistent mild abnormalities in GLS and GCS in many patients. Such findings may portend less favorable prognosis of these patients on long-term follow-up.
Limitations of this study include our relatively small patient cohort lacking any female patients. As such, our results may not be generalizable to a larger more diverse population. We did not have any Holter monitoring and exercise treadmill stress testing data on follow-up. However, the strength of this study includes robust CMR imaging techniques including T1 and T2 mapping, global ventricular strain reporting, and close follow-up of the patients.
This small case series suggests patients with acute myocarditis following mRNA-based COVID-19 vaccination have CMR evidence of myocardial recovery at 3-6 months but can have persistent mild abnormalities. These findings should be confirmed in a larger study cohort.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Truong D.T., Dionne A., Muniz J.C., et al. Clinically suspected myocarditis temporally related to COVID-19 vaccination in adolescents and young adults: suspected myocarditis after COVID-19 vaccination. Circulation. 2022;145(5):345–356. doi: 10.1161/CIRCULATIONAHA.121.056583. [DOI] [PubMed] [Google Scholar]
- 2.Ferreira V.M., Schulz-Menger J., Holmvang G., et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72(24):3158–3176. doi: 10.1016/j.jacc.2018.09.072. [DOI] [PubMed] [Google Scholar]
- 3.Aquaro G.D., Perfetti M., Camastra G., et al. Cardiac Magnetic Resonance Working Group of the Italian Society of Cardiology. Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function: ITAMY study. J Am Coll Cardiol. 2017;70(16):1977–1987. doi: 10.1016/j.jacc.2017.08.044. [DOI] [PubMed] [Google Scholar]
- 4.Aquaro G.D., Ghebru Habtemicael Y., Camastra G., et al. Prognostic value of repeating cardiac magnetic resonance in patients with acute myocarditis. J Am Coll Cardiol. 2019;74(20):2439–2448. doi: 10.1016/j.jacc.2019.08.1061. [DOI] [PubMed] [Google Scholar]
- 5.Fischer K., Obrist S.J., Erne S.A., et al. Feature tracking myocardial strain incrementally improves prognostication in myocarditis beyond traditional CMR imaging features. J Am Coll Cardiol Img. 2020;13(9):1891–1901. doi: 10.1016/j.jcmg.2020.04.025. [DOI] [PubMed] [Google Scholar]