Dear Editor,
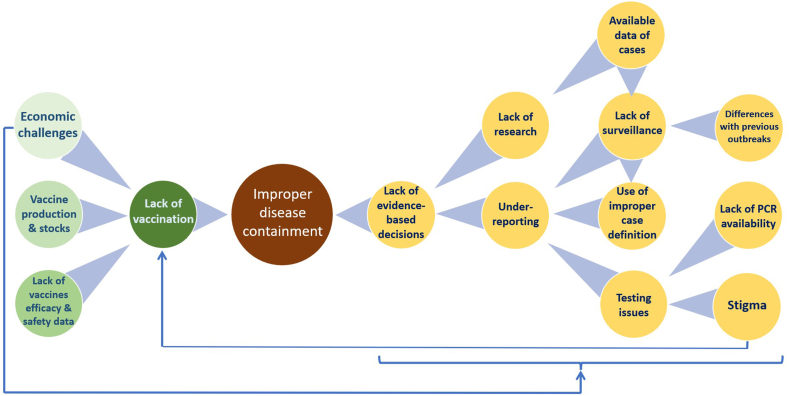
The increasing trend in monkeypox (MPX) cases raises severe concerns about the roles of healthcare authorities in preventing another pandemic when the globe did not recover yet from a close one; COVID-19. Therefore, it is essential to shedding light on the current mistakes in fighting the MPX outbreak and potential lessons learned from the COVID-19 pandemic for MPX containment (Fig. 1) [1].
Fig. 1.
Problems identified in the MPX outbreak containment.
A serious issue is the massive lack of relevant data on different aspects of the disease, discovered in 1958. The exact way of viral transmission that led to the current outbreak is not clear. It is only based on past reports regarding animal contact (outbreaks in Africa) and has a travel history to Africa (only for a few of them). A better understanding of the disease should allow the dissemination of all related data, facilitating access, relieving restrictions on data collection strategies, and strengthening active surveillance.
The actual number of MPX cases might still be underestimated. Although in many countries, the case definition is now focused on the presentation of genital ulcers and skin rash, this should be widely applied. For example, during the beginning of the COVID-19 pandemic, many cases were overlooked as they did not fit within the narrow case definition, with recent foreign travel being a must for getting tested for SARS-CoV-2. A similar scenario is seen in monkeypox with testing due to a lack of typical signs and symptoms. The underreporting of cases might be attributed to the poor contact tracing and MPX case detection, which is still limited by the underuse of MPX tests; so far, only PCR in multiple countries, especially those low- and middle-income (LMIC), is available for MPX virus in national reference centres; although efforts have been made to increase the testing [2], that is urgently needed.
It can be suggested that political and healthcare authorities collaborate to implement integrated health systems and databases that collect epidemiological data from different regions within a country and make it accessible to healthcare experts. In addition, increasing awareness about MPX and the importance of reporting and prevention is essential for healthcare workers and the general population.
Public health messages must highlight the individuals at highest risk whilst remaining free of discrimination and racism and eradicate the stigma usually caused by novel outbreaks and diseases, especially one mainly affecting men who have sex with men (MSM) [3,4].
During the COVID-19 pandemic, vaccine hesitancy was profound, and several people were left unvaccinated. A similar concern could be seen for monkeypox. Although some reports indicate that countries have sufficient stockpiles of effective smallpox vaccines and antiviral drugs, the modalities for issuing these by healthcare officials for public use are still insufficient and below demand [5]. Most LMICs do not have such vaccines available yet.
It should be noted that MPX differs from COVID-19 in many aspects. For instance, the incidence rate of COVID-19 might have been higher due to high droplet transmission. However, different ways of transmission have been reported with MPXV. Besides, MPXV is not as novel as SARS-CoV-2/COVID-19, and valuable data and tools can be found in the literature from previous outbreaks. Moreover, vaccines to prevent MPX were previously available, which required tremendous economic and scientific capabilities to facilitate vaccine development. However, MPXV needs more effective vaccine production to be further assessed in large clinical trials and real-world studies.
Both COVID-19 and Monkeypox are associated with stigma and discrimination. Such stigma has already affected the monkeypox outbreak, with several patients on the run or not giving consent for testing. Such behaviour towards a specific community or country should not be encouraged as it leads to massive underreporting of cases.
Healthcare authorities should conduct public health education campaigns and urge mass communication to reduce the stigma about getting the infection, especially among the LGBTQ + community, where most cases are reported. As a result, awareness and attitude of the public toward the disease reduced transmission increased the number of individuals with suspected infections to present for testing, and improved contact tracing should be enhanced.
MPX is preventable, and early implementation of various educational campaigns and community-oriented interventions to combat vaccine hesitancy and fight potential infodemic regarding outbreak information will play a crucial role in the battle against the Monkeypox virus.
Ethics approval and consent to participate
Not required.
Consent for publication
Not required.
Author contributions
RS developed the first draft. AR, AA, AM, AS and AJRM writing and review.
Funding
None.
Availability of data and materials
Not applicable.
Declaration of competing interest
None.
Acknowledgements
None.
Accepted: 7 September 2022
Contributor Information
Ranjit Sah, Email: ranjitsah@iom.edu.np, ranjitsah57@gmail.com.
Abdullah Reda, Email: Abdullahreda77@azhar.edu.eg.
Abdelaziz Abdelaal, Email: drabdoseliem@gmail.com.
Aroop Mohanty, Email: aroopmohanty7785@yahoo.com.
Abdelmonem Siddiq, Email: abdelmonemalsaid555@std.mans.edu.eg.
Najim Z. Alshahrani, Email: nalshahrani@uj.edu.sa.
Fatma A. Amer, Email: egyamer@yahoo.com.
Alfonso J. Rodriguez-Morales, Email: ajrodriguezmmd@gmail.com.
References
- 1.Farahat R.A., Abdelaal A., Shah J., Ghozy S., Sah R., Bonilla-Aldana D.K., et al. Monkeypox outbreaks during COVID-19 pandemic: are we looking at an independent phenomenon or an overlapping pandemic? Ann Clin Microbiol Antimicrob. 2022;21(1):26. doi: 10.1186/s12941-022-00518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aden T.A. 2022. Rapid diagnostic testing for response to the monkeypox outbreak — laboratory response network, United States, may 17–june 30, 2022. MMWR morbidity and mortality weekly report; p. 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor S., Landry C.A., Rachor G.S., Paluszek M.M., Asmundson G.J.G. Fear and avoidance of healthcare workers: an important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. 2020;75:102289. doi: 10.1016/j.janxdis.2020.102289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yufika A., Pratama R., Anwar S., Winardi W., Librianty N., Prashanti N.A.P., et al. Stigma associated with COVID-19 among health care workers in Indonesia. Disaster Med Public Health Prep. 2021:1–5. doi: 10.1017/dmp.2021.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Landman K. VOX; 2022. The smallpox vaccine stockpile isn’t the monkeypox solution we need — yet Internet.https://www.vox.com/2022/7/29/23281407/monkeypox-vaccine-acam2000-jynneos-smallpox [updated July 29, 2022. Available from: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.