Abstract
Background
No Canadian studies examined the economic impact of hepatitis B virus (HBV) using population-based, patient-level data. We determined attributable costs associated with HBV from a health care payer perspective.
Methods
We conducted an incidence-based, matched cohort, cost-of-illness study. We identified infected subjects (positive HBV surface antigen, DNA, or e-antigen) between 2004 and 2014, using health administrative data. The index date was the first positive specimen. The cohort was organized into three groups: no HBV-related complications, HBV-related complications before index date, and HBV-related complications post-index date. To evaluate costs (2017 Canadian dollars), we adopted the phase-of-care approach defining six phases. Mean attributable costs were determined by evaluating mean differences between matched pairs. Hard match variables were sex, age group, index year, rurality, neighbourhood income quintile, comorbidities, and immigrant status. Costs were combined with crude survival data to calculate 1-, 5-, and 10-year costs.
Results
We identified 41,469 infected subjects with a mean age of 44.2 years. The majority were males (54.7%), immigrants (58.4%), and residents of major urban centres (96.8%). Eight percent had HBV-related complications before index date and 11.5% had them post index date. Across groups, mean attributable costs ranged from CAD $27–$19 for pre-diagnosis, CAD $167–$1,062 for initial care, CAD $53–$407 for continuing care, CAD $1,033 for HBV-related complications, CAD $304 for continuing care for complications, and CAD $2,552–$4,281 for final care. Mean cumulative 1-, 5-, and 10-year costs ranged between CAD $253–$3,067, $3,067–$20,349, and $6,128–$38,968, respectively.
Conclusions
HBV is associated with long-term economic burden. These results support decision-making on HBV prevention and monitoring strategies.
Keywords: administrative data, cost of illness, hepatitis B virus, matched cohort, public health
Introduction
The hepatitis B virus (HBV) is a DNA virus that causes acute or chronic infection (1). The World Health Organization estimates 3.5% of the world’s population (approximately 250 million) has chronic HBV infection (68% residing in African and Western Pacific countries) (2). Although Canada has low HBV infection rates (prevalence <1%), specific groups have higher infection rates (eg, immigrants, injection drug users) (3–6). A major concern is that untreated chronic infection, can lead to serious and costly complications such as hepatocellular carcinoma (HCC) (7). Chronic infection is one of the main causes of liver cancer (8–10). Between 1997 and 2008, liver cancer prevalence increased in Canada, linked to immigration from hepatitis b (HB) and hepatitis C endemic countries (11–13).
In terms of economic burden, Canadian studies have examined HBV costs (3,5,14,15), however, only targeted specific cost components (eg, drugs, laboratory tests), were not based on patient-level data, and/or focused on particular groups (eg, immigrants, chronic infections). In order to understand the overall economic burden of HBV, there is a need for a study based on real-world data, including all relevant cost components and population groups infected by the virus. Therefore, the objective of our study was to evaluate mean attributable HBV costs from the health care payer (Ministry of Health and Ministry of Long-Term Care) perspective.
Methods
Study design, data sources, and subjects
Using a matched cohort design, we conducted an incidence-based cost-of-illness study. We established a cohort of individuals who tested positive for HBV (infected subjects) at the Public Health Ontario Laboratory (PHOL) between January 1, 2004 and December 31, 2014. These results were linked to health administrative data held at ICES, where data related to most of Ontario’s publicly funded health services (linkable via unique encoded identifiers) are available. ICES is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data, without consent, for health system evaluation and improvement. The use of the data in this study is authorized under section 45 of Ontario’s Personal Health Information Protection Act and does not require Research Ethics Board review.
We defined infected subjects as those with a positive HB surface antigen (HBsAg), HBV DNA, or HB e-antigen (HBeAg). The latter were included because not all HBsAg testing is centralized in Ontario, whereas all HBV DNA testing and most HBeAg testing is done at PHOL. Our definitions were closely aligned with HBV case definitions from the National Notifiable Diseases Surveillance System, which is supported by the Centers for Disease Control and Prevention (16). Specimen results within 90 days of each other were combined, then categorized as positive or negative. The date of the first positive specimen was the index date. Acute infection was defined as a positive result for HBsAg and positive result for IgM antibody to HB core antigen (IgM anti-HBc). Chronic infection was defined as a positive result for HBsAg, HBV DNA, or HBeAg and (if tested) a negative result for IgM anti-HBc. If a subject had acute and chronic infection within 180 days following the index date, we classified them as having chronic infection.
We divided our cohort into three groups, those with: 1) no HBV-related complications, 2) HBV-related complications prior to (or on) index date, and 3) HBV-related complications post index date. HBV-related complications included acute liver failure, complications of cirrhosis (eg, ascites, varices, encephalopathy), liver transplant, or liver cancer. These were defined using diagnostic and intervention codes outlined in Krajden et al, Janjua et al, and Thein et al (17–19). Keywords from all three studies were used to determine additional relevant outpatient codes. These included Ontario's Health Care Plan (OHIP) codes relating to portal vein thrombosis, cirrhosis of the liver, and primary malignancy of liver. Our lookback date for complications was December 31, 1988, and we looked forward to December 31, 2016.
Infected subjects were hard matched without replacement to a random sample of one million uninfected subjects in Ontario’s Registered Persons Database (RPDB). Hard match variables included: age group (five-year intervals), sex, immigrant status (defined as subject having a landing date recorded in the Immigration, Refugees and Citizenship Canada Permanent Resident Database, dates available post 1985), index year, rurality (using Rurality Index of Ontario), neighbourhood income quintile (based on 2006 and 2011 Census), comorbidities (using John Hopkins Adjusted Clinical Groups® System Version 10.0 resource utilization bands), and pregnancy. We included the latter as women are screened for HBV during pregnancy at PHOL.
We also explored the effect of HBV on costs prior to death, therefore infected subjects who died (between January 1, 2004 and December 31, 2016) were rematched without replacement to uninfected subjects who also died during that period using the same pool of subjects from the RPDB. The index date for both infected and uninfected subjects was three months prior to date of death. Hard match variables included: age group, sex, immigrant status, index year, rurality, and neighbourhood income quintile.
Outcomes
We examined costs unadjusted for survival (1-year post index date) and costs adjusted for survival (1-, 5-, 10- year post-index date) for each of the three groups.
Analysis
We conducted all analyses at ICES. We determined costs unadjusted for survival by summing costs one year post index date. Costs attributable to HBV were evaluated by determining the mean difference between matched pairs and 95% confidence intervals (CIs) were calculated using bootstrapping methods (20).
We determined costs adjusted for survival using the phase-of-care approach (17,19,21,22). The following phases were defined (Figure 1): 1) pre-diagnosis care, 2) initial care, 3) continuing care, 4) HBV-related complication, 5) continuing care for the HBV-related complication, and 6) final care. See Appendix Supplemental Table 1 for allocation of phases to each HBV group and how matching was applied to each phase. The lengths of the phases were based on clinical expertise (JF) and joinpoint analysis (23,24). Mean attributable phase-specific costs (standardized to 30 days) and 95% CIs were calculated using the same methods as the costs unadjusted for survival. We used an equation outlined by Yabroff et al (21) to combine attributable phase-specific costs with crude survival data, generated from the three groups’ matched infected subjects.
Figure 1:
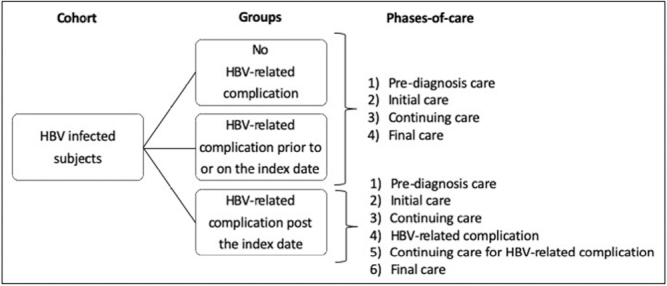
Hepatitis B virus (HBV) groups and corresponding phases-of-care
Our cost analysis was conducted from the health care payer perspective and therefore included the following cost components: inpatient hospitalizations, mental health care beds, hospital based outpatient clinic visits, same day surgeries, emergency department visits, outpatient medications, chemotherapy drugs, physician services, non-physician services, outpatient laboratory tests, rehabilitation services, complex continuing care, home care services, long-term care, dialysis clinic visits, cancer clinic visits, and assistive devices. Additional information on each of the cost components can be found in a guideline by Wodchis et al (25). We evaluated costs in 2017 Canadian dollars (CAD$). Costs beyond one year were discounted at 1.5% annually (0.0% and 3.0% were also presented) (26).
Stratified analysis
We stratified mean attributable phase-specific costs by cost component. We also stratified post 1-year costs (unadjusted for survival) and post 1-, 5-, 10-year costs (adjusted for survival) by age group, sex, and immigrant status.
Sensitivity analyses
We varied phase lengths of the initial and final care phases by ±2 months to understand the impact on costs adjusted for survival. For infected subjects that experienced HBV-related complications post index date, we rematched them on their complication date (see Appendix Supplemental Table 1).
Results
Study cohort, select characteristics, and outcomes prior to matching
Between January 1, 2004 and December 31, 2014, we identified 41,469 HBV-infected subjects (Table 1). The mean age was 44.2 years (standard deviation [SD] 14.7, median 42.7). The largest proportion of subjects were male (54.7%), moderate users of the health care system (44.8%), residents of major urban areas (96.4%), in the lowest neighbourhood income quintile (27.3%), had chronic infection (98.9%), and were immigrants (58.4%). The top three countries of birth for immigrants were China (46.6%), Vietnam (7.7%), and the Philippines (7.7%). One-year mortality was 1.8% and mean unadjusted 1-year cumulative costs were CAD $6,047 (SD $20,296, median $1,490).
Table 1:
Selected characteristics of the entire cohort and each of the three hepatitis B virus (HBV) groups
|
Entire cohort |
No HBV-related complications |
HBV-related complications prior to or on index date |
HBV-related complications post index date |
|
|---|---|---|---|---|
|
n |
41,469 |
33,349 (80.4%) |
3,334 (8.0%) |
4,786 (11.5%) |
|
Age*, mean ± SD, median |
44.2 ± 14.7, 43.0 |
42.7 ± 14.4, 41.0 |
53.8 ± 14.1, 54.0 |
48.3 ± 14.2, 48.0 |
|
Age groups |
||||
|
19 years and younger |
2.1% |
2.3% |
0.7% |
1.2% |
|
20 to 34 years |
27.2% |
30.7% |
8.1% |
16.4% |
|
35 to 49 years |
35.0% |
35.6% |
28.5% |
35.3% |
|
50 to 64 years |
26.4% |
23.8% |
40.9% |
34.2% |
|
65 years and older |
9.3% |
7.5% |
21.8% |
12.9% |
|
Females |
45.3% |
48.4% |
31.5% |
33.3% |
|
Pregnant* |
21.3% |
23.5% |
4.3% |
10.1% |
|
Index year |
||||
|
2004 |
5.0% |
4.1% |
8.0% |
9.4% |
|
2005 |
5.1% |
4.4% |
7.2% |
8.9% |
|
2006 |
5.8% |
5.1% |
7.6% |
8.9% |
|
2007 |
7.1% |
6.7% |
7.2% |
10.1% |
|
2008 |
8.8% |
8.6% |
7.0% |
11.4% |
|
2009 |
13.2% |
13.6% |
7.9% |
14.4% |
|
2010 |
13.9% |
14.9% |
7.3% |
11.5% |
|
2011 |
11.4% |
12.5% |
6.2% |
7.5% |
|
2012 |
11.8% |
11.3% |
23.6% |
7.5% |
|
2013 |
9.1% |
9.4% |
11.1% |
6.0% |
|
2014 |
8.6% |
9.4% |
6.9% |
4.5% |
|
Nearest census-based neighbourhood income quintile* |
||||
|
1 (lowest) |
27.3% |
27.6% |
25.1% |
26.6% |
|
2 |
26.0% |
26.4% |
23.2% |
25.0% |
|
3 |
19.0% |
18.9% |
18.8% |
19.9% |
|
4 |
16.3% |
16.0% |
18.6% |
16.9% |
|
5 (highest) |
11.4% |
11.1% |
14.3% |
11.6% |
|
Rurality* |
||||
|
Major urban |
96.4% |
96.8% |
92.6% |
95.9% |
|
Non-major urban |
2.9% |
2.6% |
5.5% |
3.3% |
|
Rural |
0.7% |
0.6% |
1.9% |
0.7% |
|
Resource utilization bands† |
||||
|
0-Nonuser |
4.5% |
5.1% |
3.1% |
|
|
1-Healthy users |
2.8% |
3.2% |
1.8% |
|
|
2-Low morbidity |
19.9% |
21.8% |
4.6% |
17.4% |
|
3-Moderate |
44.8% |
45.5% |
31.6% |
49.0% |
|
4-High |
21.1% |
19.9% |
36.2% |
19.5% |
|
5-Very high |
6.8% |
4.5% |
27.5% |
9.1% |
|
Immigrant‡ |
58.4% |
61.0% |
38.6% |
54.1% |
|
Top countries of birth |
China, 46.6% |
China, 48.0% |
China, 35.1% |
China, 42.0% |
|
Vietnam, 7.7% |
Philippines, 7.6% |
Vietnam, 10.0% |
Vietnam, 8.0% |
|
|
Philippines, 7.7% |
Vietnam, 7.6% |
Philippines, 8.5% |
Philippines, 7.6% |
|
|
Acute HBV§ |
1.1% |
0.6% |
5.7% |
1.1% |
|
Chronic HBV§ |
98.9% |
99.4% |
94.3% |
98.9% |
|
Mortality |
||||
|
Six months |
1.3% |
0.5% |
9.2% |
1.1% |
|
One year |
1.8% |
0.7% |
11.5% |
2.3% |
|
End of study period |
5.0% |
2.3% |
21.3% |
12.2% |
|
Unadjusted 1-year cumulative costs (CAD$) unadjusted for survival¶, mean ± SD, median |
$6,047 ± $20,296, $1,490 |
$4,569 ± $16,216, $1,262 |
$16,813 ± $39,420, $4,697 |
$8,841 ± $23,479, $2,396 |
* Measured at the index date
† Measured within two years prior to the index date
‡ Measured between January 1, 1985 and December 31, 2014
§ Acute infection was a positive result for hbv surface antigen and IgM antibody to hbv core antigen. Chronic infection was a positive result for hbv surface antigen, dna, or e-antigen with negative result for IgM antibody to hbv core antigen. If subject had acute and chronic infection within 180 days post the index date, we classified them as having chronic infection. Definitions were closely aligned with definitions from the nndss (16)
¶ Post index date
Most of our cohort did not have HBV-related complications (80.4%), while 8.0% had HBV-related complications prior to index date and 11.5% had them post index date (Table 1). Those without HBV-related complications had the largest proportion of females, immigrants, and chronic infection, along with the lowest 1-year mortality and mean unadjusted 1-year cumulative costs. Those with HBV-related complications prior to index date had the highest proportion of males, acute infection, 1-year mortality, and mean unadjusted 1-year cumulative costs.
Matching results
Across the groups, we matched 89.4%–92.9% of the infected subjects. Unmatched infected subjects had a larger proportion of high users of the health care system and immigrants compared with matched subjects (Appendix Supplemental Table 2). For our match prior to death, we were able to match nearly all the matched infected subjects that died (99.6%–99.9%; Appendix Supplemental Table 3).
Post-match outcomes
The mean attributable 1-year cumulative costs (unadjusted for survival, Table 2) were highest among infected subjects with HBV-related complications prior to index date (CAD $7,650, n = 3,098), followed by those who had HBV-related complications post index date (CAD $3,905, n = 4,408) and then infected subjects with no HBV-related complications (CAD $933, n = 29,825).
Table 2:
Mean costs by hepatitis B virus (HBV) group (CAD$)
| N matched pairs | Infected subjects | Uninfected subjects | HBV-attributable costs (95% CI) | |
|---|---|---|---|---|
| No HBV-related complications | ||||
| Mean 1-year cumulative costs unadjusted for survival* | 29,825 | $3,466 | $2,533 | $933 ($733 to $1,134) |
|
Mean costs by phase† |
||||
|
Pre-diagnosis care‡ |
29,825 |
$64 |
$91 |
–$27 (–$24 to –$31) |
|
Initial care§ |
29,717 |
$413 |
$247 |
$167 ($141 to $192) |
|
Continuing care¶ |
29,637 |
$186 |
$134 |
$53 ($42 to $65) |
|
Final care** |
685 |
$14,615 |
$10,334 |
$4,281 ($2,726 to $5,885) |
|
Mean costs adjusted for survival* |
29,825 | NA | NA | |
|
1-year cumulative costs |
$253 ($147 to $362) |
|||
|
5-year cumulative costs |
||||
|
Undiscounted |
$3,067 ($2,403 to $3,811) |
|||
|
Discounted 1.5% |
$2,890 ($2,264 to $3,591) |
|||
|
Discounted 3.0% |
$2,725 ($2,135 to $3,386) |
|||
|
10-year cumulative costs |
||||
|
Undiscounted |
$6,128 ($4,827 to $7,610) |
|||
|
Discounted 1.5% |
$5,360 ($4,222 to $6,656) |
|||
|
Discounted 3.0% |
$4,697 ($3,699 to $5,832) |
|||
| HBV-related complication prior to or on index date | ||||
| Mean 1-year cumulative costs unadjusted for survival* | 3,098 | $15,503 | $7,854 | $7,650 ($6,327 to $9,032) |
|
Mean costs by phase† |
||||
|
Pre-diagnosis care‡ |
3,098 |
$243 |
$224 |
$19 (–$2 to $41) |
|
Initial care§ |
2,869 |
$1,660 |
$599 |
$1,062 ($892 to $1,260) |
|
Continuing care¶ |
2,783 |
$760 |
$352 |
$407 ($325 to $493) |
|
Final care** |
661 |
$13,702 |
$10,669 |
$3,033 ($1,461 to $4,602) |
|
Mean costs adjusted for survival* |
3,098 | NA | NA | |
|
1-year cumulative costs |
$3,067 ($2,420 to $3,804) |
|||
|
5-year cumulative costs |
||||
|
Undiscounted |
$20,349 ($16,328 to $24,656) |
|||
|
Discounted 1.5% |
$19,173 ($15,384 to $23,230) |
|||
|
Discounted 3.0% |
$18,080 ($14,507 to $21,907) |
|||
|
10-year cumulative costs |
||||
|
Undiscounted |
$38,968 ($31,192 to $47,193) |
|||
|
Discounted 1.5% |
$34,081 ($27,280 to $41,275) |
|||
|
Discounted 3.0% |
$29,866 ($23,906 to $36,170) |
|||
| HBV-related complication post-index date | ||||
| Mean 1-year cumulative costs unadjusted for survival* | 4,408 | $7,498 | $3,593 | $3,905 ($3,233 to $4,596) |
|
Mean costs by phase† |
||||
|
Pre-diagnosis care‡ |
4,408 |
$88 |
$100 |
–$11 (–$1 to –$21) |
|
Initial care§ |
4,137 |
$708 |
$284 |
$424 ($339 to $509) |
|
Continuing care¶ |
2,893 |
$458 |
$261 |
$197 ($147 to $251) |
|
HBV-related complication†† |
4,264 |
$1,286 |
$253 |
$1,033 ($908 to $1,158) |
|
Continuing care for HBV-related complication‡‡ |
4,162 |
$501 |
$197 |
$304 ($260 to $353) |
|
Final care** |
525 |
$12,622 |
$10,069 |
$2,552 ($1,135 to $4,033) |
|
Mean costs adjusted for survival* |
4408 | NA | NA | |
|
1-year cumulative costs |
$1,339 ($990 to $1,697) |
|||
|
5-year cumulative costs |
||||
|
Undiscounted |
$16,072 ($13,277 to $19,067) |
|||
|
Discounted 1.5% |
$15,143 ($12,509 to $17,965) |
|||
|
Discounted 3.0% |
$14,280 ($11,796 to $16,941) |
|||
|
10-year cumulative costs |
||||
|
Undiscounted |
$31,921 ($26,776 to $37,516) |
|||
|
Discounted 1.5% |
$27,918 ($23,418 to $32,811) |
|||
|
Discounted 3.0% |
$24,465 ($20,522 to $28,753) |
* Post index date
† Standardized to 30 days
‡ Prior to the index date and 9 months in duration
§ Post index date and up to 6 months in duration
¶ Post index date and between 0 and 106 months in duration
** Prior to the death date and 3 months in duration
†† Post index date and up to 6 months in duration
‡‡ Post index date and between 0 and 106 months in duration
We determined the following lengths for each phase: up to nine months for pre-diagnosis care; up to six months for initial care; between 0 and 106 months for continuing care; up to six months for a HBV-related complication; between 0 and 106 months for continuing care associated with a HBV-related complication; and three months for final care (Figure 2 and Appendix Supplemental Table 1). Across the HBV groups, the mean attributable phase-specific costs ranged from CAD $27–$19 for pre-diagnosis care, CAD $167–$1,062 for initial care, CAD $53–$407 for continuing care, CAD $1,033 for HBV-related complications, CAD $304 for continuing care associated with HBV-related complications, and CAD $2,552–$4,281 for final care (Table 2). Therefore, mean attributable cumulative 1-, 5-, and 10-year costs adjusted for survival were CAD $253, $3,067, and $6,128 for those who had no HBV-related complications (n = 29,825); CAD $3,067, $20,349, and $38,968 for those who had HBV-related complications prior to index date (n = 3,098); and CAD $1,339, $16,072, and $31,921 for those who had HBV-related complications post index date (n = 4,408) (Table 2).
Figure 2:
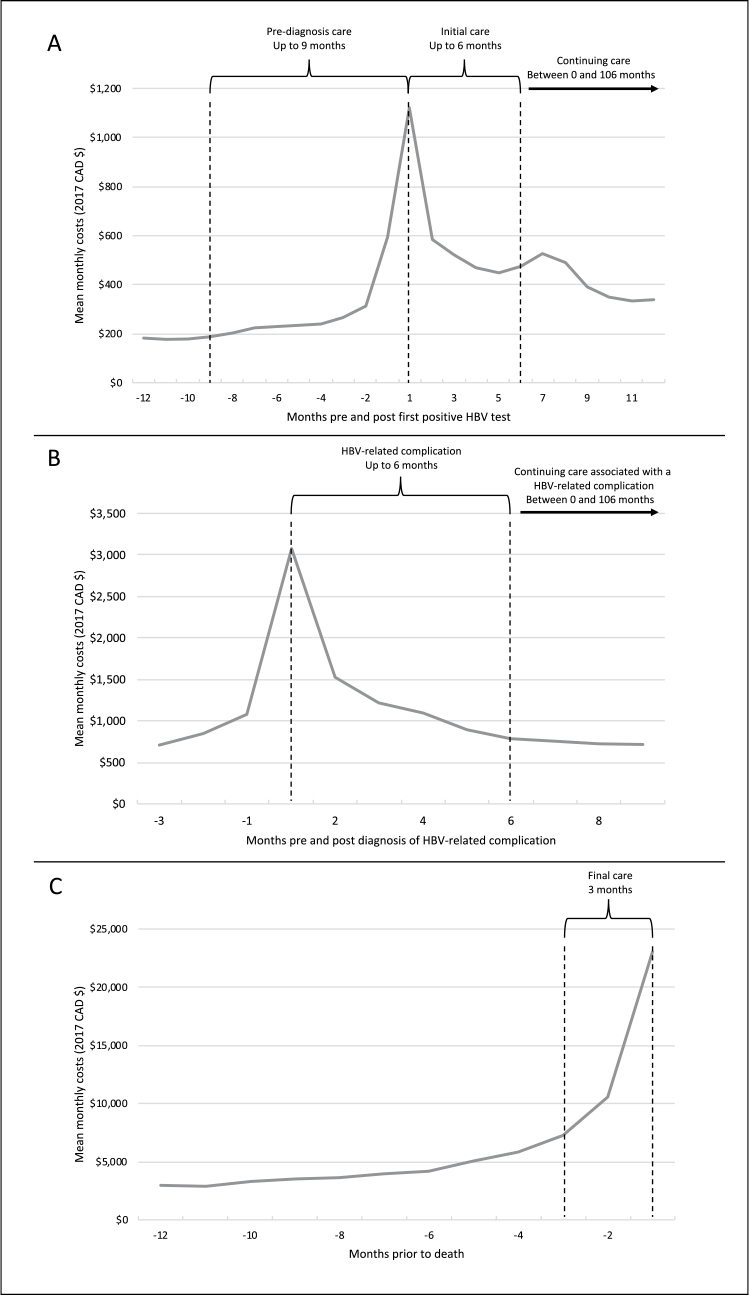
Mean monthly costs and phase-of-care durations
(A) Based on the entire cohort (n = 41,469); (B) Based on those who had a HBV-related complication post index date (n = 4,786); (C) Based on those who died by the end of the study period (n = 2,057)
Stratified analysis
Largely, the main cost components across the HBV groups were outpatient laboratory services during pre-diagnosis care; inpatient hospitalization during initial care; outpatient medication during continuing care; inpatient hospitalization during HBV-related complications; outpatient medication during continuing care for HBV-related complications; and inpatient hospitalization during final care (see Appendix Supplemental Table 4).
We found higher mean attributable costs (unadjusted and adjusted for survival) among 65 years and older, males, or long-term residents in those with no HBV complications; females or long-term residents in those with HBV-related complications prior to index date; and 19 years and younger, males, or long-term residents in those with HBV-related complications post-index date (see Appendix Supplemental Table 5).
Sensitivity analysis
Mean attributable costs adjusted for survival were sensitive to varying the phase length by ±2 months. Also, rematching at the HBV-related complication phase decreased the attributable impact three-fold 10-years post index date (CAD $31,921–$10,659) (see Appendix Supplemental Table 6).
Discussion
Our study provides a detailed cost analysis of HBV that included patient-level data, all relevant health care cost components, various population groups (eg, acute infection, children, immigrants), a comparison group, costs organized into disease-specific phases, and long-term costs up to 10-year post- index date. We found those with HBV-related complications prior to index date had higher costs than those with HBV-related complications post index date. This could be explained by how the former group may have had a more dramatic presentation of the disease prior to their HBV diagnosis. The latter group may reflect how the impact of HBV-related complications can be lessened when an HBV diagnosis is known. Our study also showed that infected subjects with no HBV-related complications still incurred costs 10-years post index date. This is most likely due to the need for continuous care such as ongoing tests to monitor disease progression (eg, serology, liver function tests, ultrasonography of the liver) and HBV-specific treatment to delay progression to complications (7,8). Our study demonstrates the importance of prevention (eg, vaccination and needle-exchange programs) and early diagnosis (eg, screening programs) (7).
Four Canadian studies examined HBV-related costs (3,5,14,15). Gagnon et al, Wong et al, and Tadrous et al focused on chronic infection only. In our cohort, approximately 99% of subjects had chronic infection. Gagnon et al calculated HBV costs based on a questionnaire to specialists and national hospitalization data (5). They found annual treatment costs for those with no HBV-related complications were $2,191 (2001 CAD$, $2,960 2017 CAD$) versus with HBV-related complications were $2,987 to $99,066 (2001 CAD$, $4,035 to $133,821 2017 CAD$) (5,27). Our mean attributable 1-year costs (unadjusted for survival) were much less, likely due to our calculations being based on patient-level data. Wong et al used an economic model to compare lifetime costs of HBV-infected immigrants to HBV-uninfected immigrants (14). In our stratified analysis, we were able do a similar comparison reaching the same conclusion as Wong et al; HBV-infected immigrants had higher long-term costs. Tadrous et al used prescription claims (held at ICES) to forecast that provincial public spending on HBV-related treatment will increase 65% between 2016 and 2020 (3). Consistent with Tadrous et al, we found outpatient medications were among the top three cost components during continuing care phases. Lastly, Lawandi et al assessed HBV testing costs at a tertiary care centre in Quebec (15). We were unable to compare our results to this study as their costs were not specifically reported for infected subjects.
Since none of these Canadian HBV costing studies used the phase-of-care approach, we compared our results to Canadian studies that adopted this method for comparable diseases. Thein et al and de Oliveira et al examined the health care costs of HCC and liver cancer, respectively, using data held at ICES (19,28). The attributable mean 5-year (undiscounted) costs were (2010) US $77,509, (2017) CAD $105,667 (2017), for HCC and between $29,933 to $35,020 (2009 CAD $, $34,116 to $39,914 2017 CAD$) for liver cancer (19,27–29). Our attributable mean 5-year (undiscounted) costs for HBV-related complications prior or post index date were lower, ranging between CAD $16,072 and CAD $20,349. This was expected since our definition for HBV-related complications included less severe conditions.
Our study had limitations. Some subjects were not diagnosed with HBV for the first time in our cohort, especially among those with HBV-related complications prior to index date. This could be due to HBV testing not being centralized in Ontario. Some may have been tested at PHOL for screening or disease monitoring purposes. We did contemplate excluding this group from our study, however felt this would understate the true burden of HBV. However, underestimation of HBV burden may have occurred, as our unmatched subjects could have included undiagnosed HBV.
We were unable to stratify costs by acute versus chronic infection. When we tried, this led to low match rates among the acute HBV cohorts. We suspect those with acute HBV may have had risk factors (eg, injection drug users, sex trade workers) which made matching more difficult (5,30).
Lastly, our phases of care did not account for acute infection transitioning into chronic infection or active versus inactive HBV infection (31). This was difficult to ascertain using administrative data and laboratory data that was noncentralized.
We found HBV has a long-term economic impact. This study will help support decision-making on HBV-related prevention and monitoring strategies. Moreover, our study showcases how the phase-of-care approach can be used to estimate the economic burden of acute and chronic illnesses.
Acknowledgements:
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). This study also received funding from a Canadian Institutes of Health Research (CIHR) operating grant (Grant number: MOP 130553, grant recipient: Beate Sander). Parts of this material are based on data and information compiled and provided by Public Health Ontario (PHO), MOH, MLTC, Canadian Institute of Health Information (CIHI), and Cancer Care Ontario (CCO, now known as Ontario Health). Parts of this material are based on data and information provided by Ontario Health (OH). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of OH. No endorsement by OH is intended or should be inferred. This research was also supported, in part, by a Canada Research Chair in Economics of Infectious Diseases held by Beate Sander (CRC-950-232429). JC Kwong is supported by a Clinician-Scientist Award from the University of Toronto Department of Family and Community Medicine. The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Parts or whole of this material are based on data and/or information compiled and provided by Immigration, Refugees and Citizenship Canada (IRCC). However, the analyses, conclusions, opinions, and statements expressed in the material are those of the author(s), and not necessarily those of IRCC.
Data-Sharing Statement:
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (eg, health care organizations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (Email: das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Ethics Approval:
N/A
Informed Consent:
N/A
Registry and the Registration No. of the Study/Trial:
N/A
Funding:
This research was supported by the Canadian Institutes of Health Research (CIHR), MOP 130553.
Disclosures:
JJ Feld has received consulting fees and grants/contracts from Gilead Sciences. The other authors have nothing to disclose.
Peer Review:
This manuscript has been peer reviewed.
Animal Studies:
N/A
Appendix
Supplemental Table 1:
Details related matching and sensitivity analyses by phase-of-care
| Phase-of-care | Included for the following group(s) | Phase length | Were covariates hard matched at the beginning of the phase? If so, the following covariates were included | Sensitivity analyses |
|---|---|---|---|---|
| Pre-diagnosis care | All | Up to 9 months | No, same match from the initial phase was used | None |
| Initial care | All | Up to 6 months | Yes, covariates included:
|
Varied the phase length ± 2 months |
| Continuing care | All | 0 to 106 months | No, same match from the initial phase was used | None |
| HBV-related complication | Cohort with HBV-related complications post index date | Up to 6 months | No, same match from the initial phase was used | Hard matched on the same covariates in the initial care match except for comorbidities and pregnancy |
| Continuing care for HBV-related complication | Cohort with HBV-related complications post index date | 0 to 106 months | No, same match from the initial phase was used | None |
| Final care | All | 3 months | Yes, covariates included:
|
Varied the phase length ±2 months |
Supplemental Table 2:
Initial care hard match results
| Pool of uninfected subjects | Matched infected subjects | Matched uninfected subjects | Unmatched infected subjects | |
|---|---|---|---|---|
| No HBV-related complication group | ||||
| n | 1,000,000 | 29,825 | 29,825 | 3,524 |
| Age groups | ||||
| 0–4 | 4.8% | 0.3% | 0.3% | NR |
| 5–9 | 5.5% | 0.2% | 0.2% | NR |
| 10–14 | 6.0% | 0.5% | 0.5% | NR |
| 15–19 | 6.8% | 1.4% | 1.4% | 1.1% |
| 20–24 | 7.2% | 5.6% | 5.6% | 8.0% |
| 25–29 | 7.2% | 10.3% | 10.3% | 21.1% |
| 30–34 | 7.2% | 12.4% | 12.4% | 21.8% |
| 35–39 | 7.4% | 12.1% | 12.1% | 14.0% |
| 40–44 | 7.9% | 11.9% | 11.9% | 8.9% |
| 45–49 | 8.0% | 12.3% | 12.3% | 7.0% |
| 50–54 | 7.3% | 11.1% | 11.1% | 6.0% |
| 55–59 | 6.2% | 8.4% | 8.4% | 3.7% |
| 60–64 | 5.1% | 5.7% | 5.7% | 2.7% |
| 65–69 | 3.9% | 3.3% | 3.3% | 2.0% |
| 70–74 | 3.1% | 2.2% | 2.2% | 1.3% |
| 75–79 | 2.5% | 1.2% | 1.2% | 1.2% |
| 80–84 | 1.9% | 0.7% | 0.7% | 0.6% |
| 85–89 | 1.2% | 0.3% | 0.3% | 0.3% |
| 90–94 | 0.5% | NR | NR | 0.2% |
| 95–99 | 0.2% | NR | NR | NR |
| 100–104 | 0.1% | NR | NR | NR |
| 105–109 | 0.0% | NR | NR | NR |
| 110–114 | 0.0% | NR | NR | NR |
| Females | 50.5% | 46.6% | 46.6% | 63.7% |
| Pregnant* | 1.6% | 14.2% | 14.2% | 81.5% |
| Index year | ||||
| 2004 | 8.9% | 3.6% | 3.6% | 8.2% |
| 2005 | 9.0% | 4.1% | 4.1% | 7.0% |
| 2006 | 9.0% | 4.9% | 4.9% | 7.2% |
| 2007 | 9.0% | 6.5% | 6.5% | 8.8% |
| 2008 | 9.0% | 8.6% | 8.6% | 8.2% |
| 2009 | 9.0% | 13.4% | 13.4% | 15.1% |
| 2010 | 9.1% | 14.8% | 14.8% | 15.9% |
| 2011 | 9.2% | 12.6% | 12.6% | 11.3% |
| 2012 | 9.3% | 11.5% | 11.5% | 9.2% |
| 2013 | 9.3% | 9.9% | 9.9% | 4.8% |
| 2014 | 9.3% | 10.0% | 10.0% | 4.2% |
| Nearest census based neighbourhood income quintile* | ||||
| 1 (lowest) | 20.6% | 27.2% | 27.2% | 31.1% |
| 2 | 19.9% | 26.1% | 26.1% | 28.7% |
| 3 | 19.6% | 19.1% | 19.1% | 17.6% |
| 4 | 20.1% | 16.2% | 16.2% | 14.2% |
| 5 (highest) | 19.8% | 11.4% | 11.4% | 8.4% |
| Rurality* | ||||
| Major urban | 74.1% | 97.2% | 97.2% | 93.7% |
| Non-major urban | 18.6% | 2.3% | 2.3% | 4.6% |
| Rural | 7.3% | 0.5% | 0.5% | 1.6% |
| Resource utilization bands† | ||||
| 0-Non user | 24.7% | 5.2% | 5.2% | 4.3% |
| 1-Healthy users | 5.5% | 3.2% | 3.2% | 3.4% |
| 2-Low morbidity | 16.7% | 21.7% | 21.7% | 22.4% |
| 3-Moderate | 38.8% | 48.3% | 48.3% | 21.8% |
| 4-High | 10.7% | 17.3% | 17.3% | 41.5% |
| 5-Very high | 3.6% | 4.2% | 4.2% | 6.7% |
| Immigrant‡ | 16.4% | 57.1% | 57.1% | 93.6% |
| HBV-related complication prior to or on index date | ||||
| n | 1,000,000 | 3,098 | 3,098 | 236 |
| Age groups | ||||
| 0–4 | 4.8% | 0.2% | 0.2% | NR |
| 5–9 | 5.5% | NR | NR | NR |
| 10–14 | 6.0% | NR | NR | NR |
| 15–19 | 6.8% | 0.3% | 0.3% | NR |
| 20–24 | 7.2% | 1.5% | 1.5% | NR |
| 25–29 | 7.2% | 2.4% | 2.4% | 3.0% |
| 30–34 | 7.2% | 3.7% | 3.7% | 11.0% |
| 35–39 | 7.4% | 6.3% | 6.3% | 11.4% |
| 40–44 | 7.9% | 9.1% | 9.1% | 8.9% |
| 45–49 | 8.0% | 12.9% | 12.9% | 10.6% |
| 50–54 | 7.3% | 15.4% | 15.4% | 16.9% |
| 55–59 | 6.2% | 13.8% | 13.8% | 11.4% |
| 60–64 | 5.1% | 12.2% | 12.2% | 5.9% |
| 65–69 | 3.9% | 7.4% | 7.4% | 4.2% |
| 70–74 | 3.1% | 6.8% | 6.8% | 6.8% |
| 75–79 | 2.5% | 4.6% | 4.6% | 3.0% |
| 80–84 | 1.9% | 2.0% | 2.0% | 3.8% |
| 85–89 | 1.2% | 0.8% | 0.8% | NR |
| 90–94 | 0.5% | 0.3% | 0.3% | NR |
| 95–99 | 0.2% | NR | NR | NR |
| 100–104 | 0.1% | NR | NR | NR |
| 105–109 | 0.0% | NR | NR | NR |
| 110–114 | 0.0% | NR | NR | NR |
| Females | 50.5% | 31.9% | 31.9% | 25.4% |
| Pregnant* | 1.6% | 2.5% | 2.5% | 33.3% |
| Index year | ||||
| 2004 | 8.9% | 8.0% | 8.0% | 8.1% |
| 2005 | 9.0% | 7.1% | 7.1% | 8.9% |
| 2006 | 9.0% | 7.8% | 7.8% | 5.5% |
| 2007 | 9.0% | 7.1% | 7.1% | 8.5% |
| 2008 | 9.0% | 7.1% | 7.1% | 5.9% |
| 2009 | 9.0% | 7.6% | 7.6% | 11.9% |
| 2010 | 9.1% | 7.0% | 7.0% | 10.6% |
| 2011 | 9.2% | 6.2% | 6.2% | 5.9% |
| 2012 | 9.3% | 23.7% | 23.7% | 22.0% |
| 2013 | 9.3% | 11.3% | 11.3% | 8.1% |
| 2014 | 9.3% | 7.1% | 7.1% | 4.7% |
| Nearest census based neighbourhood income quintile* | ||||
| 1 (lowest) | 20.6% | 25.2% | 25.2% | 23.3% |
| 2 | 19.9% | 23.0% | 23.0% | 26.3% |
| 3 | 19.6% | 18.9% | 18.9% | 17.8% |
| 4 | 20.1% | 18.5% | 18.5% | 19.5% |
| 5 (highest) | 19.8% | 14.4% | 14.4% | 13.1% |
| Rurality* | ||||
| Major urban | 74.1% | 92.7% | 92.7% | 91.5% |
| Non-major urban | 18.6% | 5.3% | 5.3% | NR |
| Rural | 7.3% | 2.0% | 2.0% | NR |
| Resource utilization bands† | ||||
| 0-Nonuser | 24.7% | NR | NR | NR |
| 1-Healthy users | 5.5% | NR | NR | NR |
| 2-Low morbidity | 16.7% | 4.7% | 4.7% | NR |
| 3-Moderate | 38.8% | 33.1% | 33.1% | 10.6% |
| 4-High | 10.7% | 35.1% | 35.1% | 48.3% |
| 5-Very high | 3.6% | 26.6% | 26.6% | 36.4% |
| Immigrant‡ | 16.4% | 34.6% | 34.6% | 91.5% |
| HBV-related complication post-index date | ||||
| n | 1,000,000 | 4,408 | 4,408 | 378 |
| Age groups | ||||
| 0–4 | 4.8% | NR | NR | NR |
| 5–9 | 5.5% | NR | NR | NR |
| 10–14 | 6.0% | 0.2% | 0.2% | NR |
| 15–19 | 6.8% | 0.8% | 0.8% | NR |
| 20–24 | 7.2% | 3.2% | 3.2% | 5.8% |
| 25–29 | 7.2% | 5.0% | 5.0% | 10.3% |
| 30–34 | 7.2% | 6.9% | 6.9% | 15.3% |
| 35–39 | 7.4% | 9.9% | 9.9% | 12.2% |
| 40–44 | 7.9% | 12.2% | 12.2% | 6.3% |
| 45–49 | 8.0% | 13.5% | 13.5% | 13.0% |
| 50–54 | 7.3% | 14.4% | 14.4% | 10.8% |
| 55–59 | 6.2% | 12.0% | 12.0% | 9.3% |
| 60–64 | 5.1% | 8.6% | 8.6% | 5.3% |
| 65–69 | 3.9% | 5.7% | 5.7% | 4.2% |
| 70–74 | 3.1% | 3.5% | 3.5% | 2.4% |
| 75–79 | 2.5% | 2.2% | 2.2% | 2.4% |
| 80–84 | 1.9% | 1.2% | 1.2% | NR |
| 85–89 | 1.2% | 0.3% | 0.3% | NR |
| 90–94 | 0.5% | NR | NR | NR |
| 95–99 | 0.2% | NR | NR | NR |
| 100–104 | 0.1% | NR | NR | NR |
| 105–109 | 0.0% | NR | NR | NR |
| 110–114 | 0.0% | NR | NR | NR |
| Females | 50.5% | 32.9% | 32.9% | 38.1% |
| Pregnant* | 1.6% | 4.8% | 4.8% | 63.2% |
| Index year | ||||
| 2004 | 8.9% | 9.6% | 9.6% | 7.7% |
| 2005 | 9.0% | 9.0% | 9.0% | 7.4% |
| 2006 | 9.0% | 8.7% | 8.7% | 10.8% |
| 2007 | 9.0% | 10.5% | 10.5% | 5.8% |
| 2008 | 9.0% | 11.7% | 11.7% | 7.9% |
| 2009 | 9.0% | 14.1% | 14.1% | 18.0% |
| 2010 | 9.1% | 11.1% | 11.1% | 15.9% |
| 2011 | 9.2% | 7.2% | 7.2% | 10.8% |
| 2012 | 9.3% | 7.4% | 7.4% | 8.5% |
| 2013 | 9.3% | 6.1% | 6.1% | 4.8% |
| 2014 | 9.3% | 4.6% | 4.6% | 2.4% |
| Nearest census based neighbourhood income quintile* | ||||
| 1 (lowest) | 20.6% | 26.7% | 26.7% | 25.4% |
| 2 | 19.9% | 24.7% | 24.7% | 28.8% |
| 3 | 19.6% | 20.1% | 20.1% | 17.5% |
| 4 | 20.1% | 16.8% | 16.8% | 18.0% |
| 5 (highest) | 19.8% | 11.7% | 11.7% | 10.3% |
| Rurality* | ||||
| Major urban | 74.1% | 96.3% | 96.3% | 92.1% |
| Non-major urban | 18.6% | 3.1% | 3.1% | 6.1% |
| Rural | 7.3% | 0.6% | 0.6% | 1.9% |
| Resource utilization bands† | ||||
| 0-Nonuser | 24.7% | 3.2% | 3.2% | 2.1% |
| 1-Healthy users | 5.5% | 1.6% | 1.6% | 4.8% |
| 2-Low morbidity | 16.7% | 16.8% | 16.8% | 24.9% |
| 3-Moderate | 38.8% | 51.7% | 51.7% | 17.5% |
| 4-High | 10.7% | 18.1% | 18.1% | 35.7% |
| 5-Very high | 3.6% | 8.6% | 8.6% | 15.1% |
| Immigrant‡ | 16.4% | 50.5% | 50.5% | 95.5% |
* Measured at the index date
† Measured within two years prior to the index date
‡ Measured between January 1, 1985 and December 31, 2014
NR = Not reported as cell was <6 observations
Supplemental Table 3:
Final care hard match results
| Infected subjects | Pool of uninfected subjects | Matched infected subjects | Matched uninfected subjects | |
|---|---|---|---|---|
| No HBV-related complication group | ||||
| n | 686 | 1,000,000 | 685 | 685 |
|
Age groups 0–4 5–9 10–14 15–19 20–24 25–29 30–34 35–39 40–44 45–49 50–54 55–59 60–64 65–69 70–74 75–79 80–84 85–89 90–94 95–99 100–104 105–109 110–114 |
NR NR NR NR NR NR 1.3% 2.3% 3.1% 6.3% 8.5% 9.3% 10.2% 10.3% 10.5% 11.8% 11.2% 10.1% 3.4% NR NR NR NR |
0.2% 0.1% 0.1% 0.3% 0.4% 0.4% 0.5% 0.7% 1.2% 2.1% 3.3% 4.6% 5.9% 7.4% 9.3% 12.4% 16.2% 16.8% 12.2% 4.9% 1.0% 0.1% 0.0% |
NR NR NR NR NR NR 1.3% 2.3% 3.1% 6.1% 8.5% 9.3% 10.2% 10.4% 10.5% 11.8% 11.2% 10.1% 3.4% NR NR NR NR |
NR NR NR NR NR NR 1.3% 2.3% 3.1% 6.1% 8.5% 9.3% 10.2% 10.4% 10.5% 11.8% 11.2% 10.1% 3.4% NR NR NR NR |
| Females | 38.3% | 50.1% | 38.2% | 38.2% |
|
Index year 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 |
NR NR 2.9% 3.1% 4.7% 6.0% 6.1% 8.5% 8.5% 9.9% 11.7% 15.9% 12.5% 8.2% |
1.9% 7.2% 7.2% 7.4% 7.4% 7.6% 7.5% 7.7% 7.6% 8.0% 7.9% 8.2% 8.2% 6.3% |
NR NR 2.9% 3.1% 4.7% 6.0% 6.1% 8.5% 8.5% 9.9% 11.7% 15.9% 12.4% 8.2% |
NR NR 2.9% 3.1% 4.7% 6.0% 6.1% 8.5% 8.5% 9.9% 11.7% 15.9% 12.4% 8.2% |
|
Nearest census based neighbourhood income quintile* 1 (lowest) 2 3 4 5 (highest) |
31.3% 23.3% 16.0% 17.3% 12.0% |
22.9% 21.0% 19.6% 18.8% 17.6% |
31.4% 23.4% 16.1% 17.2% 12.0% |
31.4% 23.4% 16.1% 17.2% 12.0% |
|
Rurality* Major urban Non-major urban Rural |
90.4% 6.4% 3.2% |
64.4% 24.7% 10.9% |
90.5% 6.4% 3.1% |
90.5% 6.4% 3.1% |
| Immigrant† | 34.0% | 5.1% | 33.9% | 33.9% |
| HBV-related complication prior to or on index date | ||||
| n | 662 | 1,000,000 | 661 | 661 |
|
Age groups 0–4 5–9 10–14 15–19 20–24 25–29 30–34 35–39 40–44 45–49 50–54 55–59 60–64 65–69 70–74 75–79 80–84 85–89 90–94 95–99 100–104 105–109 110–114 |
NR NR NR NR NR NR NR 1.8% 3.2% 6.6% 10.9% 14.8% 13.3% 11.3% 13.6% 10.7% 8.0% 3.5% 0.9% NR NR NR NR |
0.2% 0.1% 0.1% 0.3% 0.4% 0.4% 0.5% 0.7% 1.2% 2.1% 3.3% 4.6% 5.9% 7.4% 9.3% 12.4% 16.2% 16.8% 12.2% 4.9% 1.0% 0.1% 0.0% |
NR NR NR NR NR NR NR 1.8% 3.2% 6.7% 10.9% 14.8% 13.2% 11.3% 13.6% 10.7% 8.0% 3.5% 0.9% NR NR NR NR |
NR NR NR NR NR NR NR 1.8% 3.2% 6.7% 10.9% 14.8% 13.2% 11.3% 13.6% 10.7% 8.0% 3.5% 0.9% NR NR NR NR |
| Females | 23.3% | 50.1% | 23.1% | 23.1% |
|
Index year 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 |
NR NR 7.6% 5.3% 7.4% 5.1% 9.5% 9.2% 7.7% 9.4% 10.3% 11.0% 7.1% 5.3% |
1.9% 7.2% 7.2% 7.4% 7.4% 7.6% 7.5% 7.7% 7.6% 8.0% 7.9% 8.2% 8.2% 6.3% |
NR NR 7.4% 5.3% 7.4% 5.1% 9.5% 9.2% 7.7% 9.4% 10.3% 11.0% 7.1% 5.3% |
NR NR 7.4% 5.3% 7.4% 5.1% 9.5% 9.2% 7.7% 9.4% 10.3% 11.0% 7.1% 5.3% |
|
Nearest census based neighbourhood income quintile* 1 (lowest) 2 3 4 5 (highest) |
27.2% 24.8% 16.5% 16.9% 14.7% |
22.9% 21.0% 19.6% 18.8% 17.6% |
27.2% 24.7% 16.5% 16.9% 14.7% |
27.2% 24.7% 16.5% 16.9% 14.7% |
|
Rurality* Major urban Non-major urban Rural |
89.3% 7.7% 3.0% |
64.4% 24.7% 10.9% |
89.3% 7.7% 3.0% |
89.3% 7.7% 3.0% |
| Immigrant† | 23.7% | 5.1% | 23.6% | 23.6% |
| HBV-related complication post-index date | ||||
| n | 527 | 1,000,000 | 525 | 525 |
|
Age groups 0–4 5–9 10–14 15–19 20–24 25–29 30–34 35–39 40–44 45–49 50–54 55–59 60–64 65–69 70–74 75–79 80–84 85–89 90–94 95–99 100–10 105–109 110–114 |
NR NR NR NR NR NR 1.5% 1.1% 5.1% 8.0% 10.8% 13.9% 14.2% 12.9% 10.8% 6.6% 7.6% 3.0% 1.7% NR NR NR NR |
0.2% 0.1% 0.1% 0.3% 0.4% 0.4% 0.5% 0.7% 1.2% 2.1% 3.3% 4.6% 5.9% 7.4% 9.3% 12.4% 16.2% 16.8% 12.2% 4.9% 1.0% 0.1% 0.0% |
NR NR NR NR NR NR 1.5% 1.1% 5.1% 8.0% 10.7% 13.9% 14.3% 13.0% 10.9% 6.7% 7.6% 3.0% 1.7% NR NR NR NR |
NR NR NR NR NR NR 1.5% 1.1% 5.1% 8.0% 10.7% 13.9% 14.3% 13.0% 10.9% 6.7% 7.6% 3.0% 1.7% NR NR NR NR |
| Females | 25.6% | 50.1% | 25.7% | 25.7% |
|
Index year 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 |
NR NR 2.7% 5.3% 5.7% 4.9% 7.0% 8.0% 6.8% 10.6% 9.3% 12.0% 16.1% 10.1% |
1.9% 7.2% 7.2% 7.4% 7.4% 7.6% 7.5% 7.7% 7.6% 8.0% 7.9% 8.2% 8.2% 6.3% |
NR NR 2.7% 5.3% 5.7% 5.0% 6.9% 8.0% 6.9% 10.5% 9.3% 12.0% 16.2% 10.1% |
NR NR 2.7% 5.3% 5.7% 5.0% 6.9% 8.0% 6.9% 10.5% 9.3% 12.0% 16.2% 10.1% |
|
Nearest census based neighbourhood income quintile* 1 (lowest) 2 3 4 5 (highest) |
29.2% 24.1% 19.7% 15.2% 11.8% |
22.9% 21.0% 19.6% 18.8% 17.6% |
29.3% 24.2% 19.6% 15.0% 11.8% |
29.3% 24.2% 19.6% 15.0% 11.8% |
|
Rurality* Major urban Non-major urban Rural |
92.2% 5.5% 2.3% |
64.4% 24.7% 10.9% |
92.6% 5.1% 2.3% |
92.6% 5.1% 2.3% |
| Immigrant† | 33.8% | 5.1% | 33.5% | 33.5% |
* Measured at the index date
† Measured between January 1, 1985 and December 31, 2014
NR = Not reported as cell was <6 observations
Supplemental Table 4:
The top three cost components by phase-of-care and HBV group (CAD$)
| No HBV-related complication | HBV-related complication prior to or on index date | HBV-related complication post index date | |
|---|---|---|---|
| Pre-diagnosis care |
n = 29,825 |
n = 3,098 |
n = 4,408 |
|
Outpatient laboratory tests, $1 |
Outpatient medication, $17 |
Dialysis clinic visits, $3%* |
|
|
Dialysis clinic visits, $0%* |
Hospital based outpatient clinic visits, $9 |
Complex continuing care, $2%* |
|
|
Chemotherapy drugs, $0%* |
Dialysis clinic visits, $2%* |
Outpatient laboratory tests, $1 |
|
| Initial care |
n = 29,717 |
n = 2,869 |
n = 4,137 |
|
Inpatient hospitalization, $45 |
Inpatient hospitalization, $579 |
Inpatient hospitalization, $146 |
|
| Physician services, $39 | Physician services, $154 | Physician services, $90 | |
| Dialysis clinic visits, $17 | Outpatient medication, $98 | Hospital based outpatient clinic visits, $40 | |
| Continuing care | n = 29,637 | n = 2,783 | n = 2,893 |
| Outpatient medication, $12 | Inpatient hospitalization, $145 | Outpatient medication, $43 | |
| Dialysis clinic visits, $11 | Outpatient medication, $97 | Physician services, $40 | |
| Inpatient hospitalization, $9 | Physician services, $45 | Hospital based outpatient clinic visits, $28 | |
| HBV-related NA complication | NA | n = 4,264 | |
| Inpatient hospitalization, $457 | |||
| Physician services, $177 | |||
| Hospital based outpatient clinic visits, $115 | |||
| Continuing care NA for HBV-related complication | NA | NA | n = 4,162 |
| Outpatient medication, $96 | |||
| Inpatient hospitalization, $65 | |||
| Physician services, $37 | |||
| Final care | n = 685 | n = 661 | n = 525 |
| Inpatient hospitalization, $2,987 | Inpatient hospitalization, $2,747 | Inpatient hospitalization, $1,855 | |
| Dialysis clinic visits, $485 | Physician services, $410 | Physician services, $468 | |
| Physician services, $365 | Hospital based outpatient clinic visits, $126 | Dialysis clinic visits, $241 |
* 95% CI crossed zero
NA = Not applicable
Supplemental Table 5:
Stratified mean cumulative costs by HBV group (CAD$)
| n | 1-year costs unadjusted for survival | 1-year costs adjusted for survival (undiscounted) | 5-year costs adjusted for survival (undiscounted) | 10-year costs adjusted for survival (undiscounted) | |
|---|---|---|---|---|---|
| No HBV-related complication | |||||
| Mean attributable cost (undiscounted) | 29,825 | $933 | $253 | $3,067 | $6,128 |
|
Age group |
|||||
|
19 years and younger |
734 | $4,367 | $1,392 | $6,293 | $11,315 |
|
20 to 34 years |
8,432 | $186 | $26* | $1,479 | $3,137 |
|
35 to 49 years |
10,834 | $718 | $225 | $1,593 | $2,837 |
|
50 to 64 years |
7,512 | $622 | $57* | $2,590 | $5,419 |
|
65 years and older |
2,313 | $4,580 | $1,487 | $15,316 | $30,064 |
|
Sex |
|||||
|
male |
15,922 | $1,411 | $479 | $4,287 | $8,447 |
|
Female |
13,903 | $385 | $6* | $1,664 | $3,455 |
|
Immigrant status |
|||||
|
Long-term resident |
12,791 | $1,508 | $433 | $4,101 | $7,989 |
|
Immigrant |
17,034 | $501 | $118 | $2,283 | $4,709 |
| HBV-related complication prior to or on index date | |||||
| Mean attributable cost | 3098 | $7,650 | $3,067 | $20,349 | $38,968 |
|
Age group |
|||||
|
19 years and younger |
21 | $33,609* | $13,939* | $51,170* | $85,564* |
|
20 to 34 years |
235 | $3,626 | $2,507 | $12,825 | $12 |
|
35 to 49 years |
877 | $5,015 | $2,343 | $15,840 | $30,792 |
|
50 to 64 years |
1,282 | $6,844 | $2,461 | $19,895 | $38,888 |
|
65 years and older |
683 | $13,130 | $4,835 | $26,028 | $47,462 |
|
Sex |
|||||
|
Male |
2,109 | $7,790 | $3,042 | $20,166 | $38,402 |
|
Female |
989 | $7,350 | $3,128 | $20,683 | $40,031 |
|
Immigrant status |
|||||
|
Long-term resident |
2,027 | $9,134 | $3,689 | $23,906 | $45,563 |
|
Immigrant |
1,071 | $4,840 | $1,886 | $13,044 | $25,138 |
| HBV-related complication post-index date | |||||
| Mean attributable cost | 4,408 | $3,905 | $1,339 | $16,072 | $31,921 |
|
Age group |
|||||
|
19 years and younger |
54 | $12,276 | $4,429 | $43,468 | $79,544 |
|
20 to 34 years |
666 | $2,061 | $556 | $10,072 | $18,706 |
|
35 to 49 years |
1,570 | $2,607 | $897 | $12,891 | $25,336 |
|
50 to 64 years |
1,543 | $4,210 | $1,477 | $17,577 | $35,350 |
|
65 years and older |
575 | $7,981 | $2,956 | $24,369 | $47,440 |
|
Sex |
|||||
|
Male |
2,957 | $4,391 | $1,359 | $17,327 | $34,790 |
|
Female |
1,451 | $2,914 | $1,314 | $13,706 | $26,156 |
|
Immigrant status |
|||||
|
Long-term resident |
2,181 | $4,745 | $1,714 | $19,512 | $38,272 |
|
Immigrant |
2,227 | $3,082 | $983 | $12,642 | $25,319 |
* 95% CI crosses zero
Supplemental Table 6:
Sensitivity analyses by HBV group
| 1-year costs adjusted for survival (undiscounted), CAD$ | 5-year costs adjusted for survival (undiscounted), CAD$ | 10-year costs adjusted for survival (undiscounted), CAD$ | |
|---|---|---|---|
| No HBV-related complication (n = 29,825) | |||
| Mean attributable cumulative cost | $253 | $3,067 | $6,128 |
| Initial care length varied ±2 months | |||
| Up to 4 months | $337 | $3,179 | $6,524 |
| Up to 8 months | $255 | $3,040 | $5,744 |
| Final care length varied ±2 months | |||
| 1 months | $382 | $4,246 | $8,524 |
| 5 months | $179 | $2,557 | $5,139 |
| HBV-related complication prior to or on index date (n = 3,098) | |||
| Mean attributable cost (undiscounted) | $3,067 | $20,349 | $38,968 |
| Initial care length varied ±2 months | |||
| Up to 4 months | $3,486 | $20,601 | $40,222 |
| Up to 8 months | $2,819 | $20,570 | $38,794 |
| Final care length varied ±2 months | |||
| 1 months | $4,771 | $31,018 | $59,049 |
| 5 months | $2,719 | $16,914 | $32,006 |
| HBV-related complication post index date (n = 4,408) | |||
| Mean attributable cost (undiscounted) | $1,339 | $16,072 | $31,921 |
| Initial care length varied ±2 months | |||
| Up to 4 months | $1,441 | $15,697 | $31,396 |
| Up to 8 months | $1,297 | $16,027 | $31,914 |
| HBV-related complication included hard matching* | $1,242 | $8,579 | $10,659 |
| Final care length varied ±2 months | |||
| 1 months | $1,533 | $20,618 | $41,048 |
| 5 months | $1,272 | $14,073 | $27,088 |
* See Supplemental Table 7 for matching results
Supplemental Table 7:
Sensitivity analysis-hard matching at the beginning of the HBV-related complication phase
| Pool of uninfected subjects | Infected subjects | Matched infected subjects | Matched uninfected subjects | ||
|---|---|---|---|---|---|
| n | 1,000,000 | 4,402 | 3,607 | 3,607 | |
| Age groups | |||||
| 0–4 | 4.8% | NR | NR | NR | |
| 5–9 | 5.5% | NR | NR | NR | |
| 10–14 | 6.0% | NR | NR | NR | |
| 15–19 | 5.3% | 0.4% | 0.4% | 0.4% | |
| 20–24 | 8.7% | 2.4% | 2.4% | 2.4% | |
| 25–29 | 7.2% | 3.8% | 3.9% | 3.9% | |
| 30–34 | 7.2% | 5.7% | 5.6% | 5.6% | |
| 35–39 | 7.4% | 8.8% | 8.5% | 8.5% | |
| 40–44 | 7.9% | 11.6% | 12.0% | 12.0% | |
| 45–49 | 8.0% | 12.6% | 13.0% | 13.0% | |
| 50–54 | 7.3% | 13.8% | 13.8% | 13.8% | |
| 55–59 | 6.2% | 13.9% | 13.6% | 13.6% | |
| 60–64 | 5.1% | 10.7% | 10.5% | 10.5% | |
| 65–69 | 3.9% | 6.7% | 6.6% | 6.6% | |
| 70–74 | 3.1% | 4.4% | 4.5% | 4.5% | |
| 75–79 | 2.5% | 2.6% | 2.6% | 2.6% | |
| 80–84 | 1.9% | 1.7% | 1.8% | 1.8% | |
| 85–89 | 1.2% | 0.5% | 0.4% | 0.4% | |
| 90–94 | 0.5% | 0.2% | 0.2% | 0.2% | |
| 95–99 | 0.2% | NR | NR | NR | |
| 100–104 | 0.1% | NR | NR | NR | |
| 105–109 | 0.0% | NR | NR | NR | |
| 110–114 | 0.0% | NR | NR | NR | |
| Females | 50.5% | 32.9% | 32.9% | 32.9% | |
| Index year | |||||
| 2004 | 8.9% | 2.6% | 3.0% | 3.0% | |
| 2005 | 9.0% | 4.0% | 4.7% | 4.7% | |
| 2006 | 9.0% | 5.6% | 6.5% | 6.5% | |
| 2007 | 9.0% | 5.2% | 5.8% | 5.8% | |
| 2008 | 9.0% | 6.9% | 7.9% | 7.9% | |
| 2009 | 9.0% | 9.3% | 10.8% | 10.8% | |
| 2010 | 9.1% | 11.5% | 12.7% | 12.7% | |
| 2011 | 9.2% | 9.9% | 11.8% | 11.8% | |
| 2012 | 9.3% | 9.7% | 11.2% | 11.2% | |
| 2013 | 9.3% | 10.7% | 12.5% | 12.5% | |
| 2014 | 9.3% | 11.2% | 13.1% | 13.1% | |
| 2015 | 0.0% | 7.7% | 0.0% | 0.0% | |
| 2016 | 0.0% | 5.9% | 0.0% | 0.0% | |
| Nearest census based neighbourhood income quintile* | |||||
| 1 (lowest) | 20.6% | 24.8% | 25.0% | 25.0% | |
| 2 | 19.9% | 23.6% | 24.1% | 24.1% | |
| 3 | 19.6% | 20.9% | 21.1% | 21.1% | |
| 4 | 20.1% | 17.7% | 17.1% | 17.1% | |
| 5 (highest) | 19.8% | 12.9% | 12.6% | 12.6% | |
| Rurality* | |||||
| Major urban | 74.1% | 96.5% | 96.8% | 96.8% | |
| Non-major urban | 18.6% | 2.8% | 2.7% | 2.7% | |
| Rural | 7.3% | 0.7% | 0.6% | 0.6% | |
| Immigrant† | 16.4% | 50.5% | 48.1% | 48.1% |
* Measured at the index date
† Measured between January 1, 1985 and December 31, 2014
NR = Not reported as cell was <6 observations
Funding Statement
This research was supported by the Canadian Institutes of Health Research (CIHR), MOP 130553.
References
- 1.Gitlin N. Hepatitis B: Diagnosis, prevention, and treatment. Clin Chem. 1997;43(8 Pt 2): 1500–6. 10.1093/clinchem/43.8.1500. Medline: [DOI] [PubMed] [Google Scholar]
- 2.Global Hepatitis Report 2017 Geneva: World Health Organization; 2017. [Available from: https://apps.who.int/iris/bitstream/handle/10665/255016/9789241565455-eng.pdf?sequence=1. [Google Scholar]
- 3.Tadrous M, Brahmania M, Martins D, Knowles S, Janssen HLA, Mamdani MM, et al. Publicly funded oral chronic hepatitis B treatment patterns in Ontario over 16 years: An ecologic study. J Manag Care Spec Pharm. 2018;24(5):464–8. 10.18553/jmcp.2018.24.5.464. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: A systematic review of data published between 1965 and 2013. Lancet. 2015; 386(10003):1546–55. 10.1016/S0140-6736(15)61412-X [DOI] [PubMed] [Google Scholar]
- 5.Gagnon YM, Levy AR, Iloeje UH, Briggs AH. Treatment costs in Canada of health conditions resulting from chronic hepatitis B infection. J Clin Gastroenterol. 2004;38(10 Suppl 3): S179–86. 10.1097/00004836-200411003-00011. Medline: [DOI] [PubMed] [Google Scholar]
- 6.Minuk GY, Uhanova J. Chronic hepatitis B infection in Canada. Can J Infect Dis. 2001; 12(6):351–6. 10.1155/2001/650313. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kowdley KV. The cost of managing chronic hepatitis B infection: A global perspective. J Clin Gastroenterol. 2004;38(10 Suppl 3): S132–3. 10.1097/00004836-200411003-00002. Medline: [DOI] [PubMed] [Google Scholar]
- 8.Tang LSY, Covert E, Wilson E, Kottilil S. Chronic hepatitis B infection: A review. JAMA. 2018;319(17):1802–13. 10.1001/jama.2018.3795. Medline: [DOI] [PubMed] [Google Scholar]
- 9.Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006;118(12):3030–44. 10.1002/ijc.21731. Medline: [DOI] [PubMed] [Google Scholar]
- 10.Akinyemiju T, Abera S, Ahmed M, Alam N, Alemayohu MA, Allen C, et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: Results from the global burden of disease study 2015. JAMA Oncol. 2017;3(12):1683–91. 10.1001/jamaoncol.2017.3055. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hepatitis B in Canada: 2005–2011 surveillance report: Centre for Communicable Diseases and Infection Control, Infectious Disease Prevention and Control Branch. Public Health Agency of Canada; 2014. [Available from: http://publications.gc.ca/collections/collection_2015/aspc-phac/HP40-129-2014-eng.pdf. [Google Scholar]
- 12.Ellison LF, Wilkins K. Canadian trends in cancer prevalence. Health Rep. 2012;23(1):7–16. 10.1007/s10903-010-9347-3. [DOI] [PubMed] [Google Scholar]
- 13.McDermott S, DesMeules M, Lewis R, Gold J, Payne J, Lafrance B, et al. Cancer incidence among Canadian immigrants, 1980–1998: Results from a national cohort study. Journal of immigrant and minority health. 2011;13(1):15–26. 10.1007/s10903-010-9347-3. Medline: [DOI] [PubMed] [Google Scholar]
- 14.Wong WW, Woo G, Heathcote EJ, Krahn M. Disease burden of chronic hepatitis B among immigrants in Canada. Can J Gastroenterol. 2013;27(3):137–47. 10.1155/2013/924640. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawandi A, Cheng MP, Lee TC. Hepatitis B testing practices at a tertiary care centre and their associated costs: A retrospective analysis. PLoS One. 2019;14(7):e0219347. 10.1371/journal.pone.0219347. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Surveillance Case Definitions for Current and Historical Conditions: Centers for Disease Control and Prevention; 2019. [Available from: https://wwwn.cdc.gov/nndss/conditions/.
- 17.Krajden M, Kuo M, Zagorski B, Alvarez M, Yu A, Krahn M. Health care costs associated with hepatitis C: A longitudinal cohort study. Can J Gastroenterol. 2010;24(12):717– 26. 10.1155/2010/569692. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Janjua NZ, Kuo M, Yu A, Alvarez M, Wong S, Cook D, et al. The population level cascade of care for hepatitis C in British Columbia, Canada: The BC hepatitis testers cohort (BC-HTC). EBioMedicine. 2016;12:189–95. 10.1016/j.ebiom.2016.08.035. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thein H-H, Isaranuwatchai W, Campitelli MA, Feld JJ, Yoshida E, Sherman M, et al. Health care costs associated with hepatocellular carcinoma: A population-based study. Hepatology. 2013;58(4):1375–84. 10.1002/hep.26231. Medline: [DOI] [PubMed] [Google Scholar]
- 20.Austin PC, Small DS. The use of bootstrapping when using propensity-score matching without replacement: A simulation study. Stat Med. 2014;33(24):4306–19. 10.1002/sim.6276. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yabroff KR, Lamont EB, Mariotto A, Warren JL, Topor M, Meekins A, et al. Cost of care for elderly cancer patients in the United States. Journal of the National Cancer Institute. 2008;100(9):630–41. 10.1093/jnci/djn103. Medline: [DOI] [PubMed] [Google Scholar]
- 22.Brown ML, Riley GF, Potosky AL, Etzioni RD. Obtaining long-term disease specific costs of care: Application to Medicare enrollees diagnosed with colorectal cancer. Medical Care. 1999;37(12):1249–59. 10.1097/00005650-199912000-00008. Medline: [DOI] [PubMed] [Google Scholar]
- 23.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–51. . [DOI] [PubMed] [Google Scholar]
- 24.Joinpoint Trend Analysis Software: National Cancer Institute; [Available from: https://surveillance.cancer.gov/joinpoint/ [Google Scholar]
- 25.Wodchis WP, Bushmeneva K, Nikitovic M, McKillop I. Guidelines on Person-Level Costing Using Administrative Databases in Ontario. Working Paper Series. Vol 1. Toronto: Health System Performance Research Network. 2013. [Available from: https://tspace.library.utoronto.ca/bitstream/1807/87373/1/Wodchis%20et%20al_2013_Guidelines%20on%20Person-Level%20Costing.pdf [Google Scholar]
- 26.Guidelines for the Economic Evaluation of Health Technologies: Canada 4th Edition Canadian Agency for Drugs and Technologies in Health; 2017. [Available from: https://www.cadth.ca/sites/default/files/pdf/guidelines_for_the_economic_evaluation_of_health_technologies_canada_4th_ed.pdf [Google Scholar]
- 27.Inflation Calculator: Bank of Canada; [Available from: https://www.bankofcanada.ca/rates/related/inflation-calculator/ [Google Scholar]
- 28.De Oliveira C, Pataky R, Bremner KE, Rangrej J, Chan KK, Cheung WY, et al. Phase-specific and lifetime costs of cancer care in Ontario, Canada. BMC Cancer. 2016;16(1):809. 10.1186/s12885-016-2835-7. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Purchasing Power Parities for GDP and related indicators: Organisation for Economic Co-operation and Development; [Available from: https://stats.oecd.org/Index.aspx?DataSetCode=CPL. [Google Scholar]
- 30.Roy E, Haley N, Lemire N, Boivin JF, Leclerc P, Vincelette J. Hepatitis B virus infection among street youths in Montreal. CMAJ. 1999;161(6):689–93. PMID: [PMC free article] [PubMed] [Google Scholar]
- 31.Villeneuve JP. The natural history of chronic hepatitis B virus infection. J Clin Virol. 2005;34 Suppl 1:S139–42. 10.1016/S1386-6532(05)80024-1. [DOI] [PubMed] [Google Scholar]


