Abstract
Pain is a complex construct that contributes to profound physical and psychological dysfunction, particularly in individuals coping with chronic pain. The current paper builds upon previous research, describes a balanced conceptual model that integrates aspects of both psychological vulnerability and resilience to pain, and reviews protective and exacerbating psychosocial factors to the process of adaptation to chronic pain, including pain catastrophizing, pain acceptance, and positive psychological resources predictive of enhanced pain coping. The current paper identifies future directions for research that will further enrich the understanding of pain adaptation and espouses an approach that will enhance the ecological validity of psychological pain coping models, including introduction of advanced statistical and conceptual models that integrate behavioral, cognitive, information processing, motivational and affective theories of pain coping.
Keywords: Chronic pain, Resilience (psychological), Coping behavior, Stress, Emotional States, Social Interactions
Pain serves a vital purpose: to signal injury or disease in the body. Acute pain serves as an indicator of the location, nature, and severity of physiological disturbance. However, a variety of causes, including intractable disease and permanent damage to the body, may cause the experience of pain to become chronic. Chronic pain loses its usefulness as an indicator of injury and becomes a toxic influence on the physical, cognitive, and emotional equilibrium of the sufferer. Chronic pain has been associated with a variety of psychological problems, including depressive illness, substance abuse, and personality disorders [1]. Greater levels of pain intensity are also predictive of lower day-to-day positive affect and greater day-to-day levels of negative affect and depressive symptoms [2]. However, adaptation to pain is a complex phenomenon, comprised of emotional and cognitive reactions to pain, automatic and conscious attempts at coping with pain, and social and physiological contributions to pain reactivity. The current paper will examine various processes relevant to pain adaptation, including the contributions of various behavioral, cognitive, affective, physiological, and social mechanisms.
Melzack and Wall [3] proposed that the experience of pain consists of 3 components: sensory, affective, and evaluative. The sensory aspect of pain refers to physical sensations associated with pain (e.g., location, temperature, intensity), the affective aspect refers to pain-related emotions (e.g., anxiety, fear), and the evaluative components of pain are cognitive in nature and refer to judgments and expectations about pain. The evaluative component of pain is subject to prior experience and the context in which pain is experienced and is influenced by the sensory and affective components of pain [4]. Pain and emotion also share common pathways linguistically [5] and neurologically [6]. The nature of pain is not purely physical and its experience is modulated significantly by psychological factors, which explains in part the lack of clarity in defining pain experience. It is thus important for newer models of pain adaptation to incorporate both physical and psychological factors and to depict them as ongoing and mutually influential phenomena. Furthermore, recent conceptualizations of psychological adaptation to stress [7] and chronic pain [8•] have indicated the need for representing the complexity of adaptation, which involves both adaptive and maladaptive processes.
Traditional definitions of adaptation have focused on factors that confer vulnerability. Resilience is sometimes contrasted with vulnerability, such that resilient functioning has been defined as the opposite: an absence of vulnerability. Recently, resilience and vulnerability have been identified as separate, albeit related, forces that act on an individual’s “developmental trajectory”, rather than as opposite sides of the same spectrum [9]. In general, resilience has been defined as sustained positive functioning in the face of significant physical or psychological challenges [10]. Researchers have also delineated 3 distinct components of individual resilience: sustained engagement in desirable and valued activities, recovery from stressful experiences by returning to equilibrium, and personal growth in response to a physical or psychological challenge [11,12]. The biopsychosocial factors that underlie these resilient outcomes differ from those typically studied to identify fragile adjustment and vulnerability [13]. For the purposes of the current paper, we will define resilience as a construct reflecting overall individual well-being despite the presence of a significant stressor, and we will refer to processes of “resilient coping” as adaptive cognitive or behavioral efforts (e.g., acceptance-based coping, seeking social support) that contribute to overall resilience.
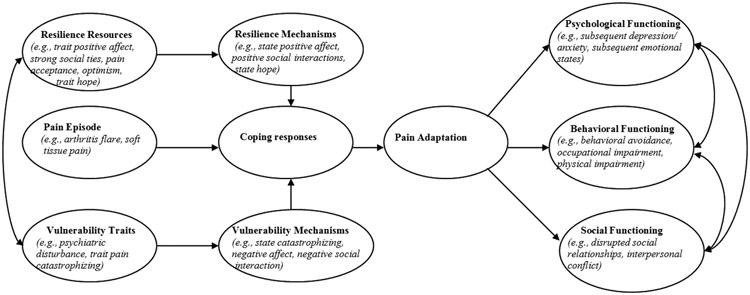
In the context of adaptation to chronic pain, resilience and vulnerability constructs are moderately correlated, yet separable [13]. A great deal of research on processes of pain adaptation has focused on individual differences and internal psychological mechanisms, both specific to pain and more broadly connected to individual well-being [8•,14]. These studies have highlighted the importance of attention to both stable and modifiable contributors to pain adaptation, and have noted that individual resilience and vulnerability may vary across domains; some individuals may show a greater vulnerability to social stressors than to physical stressors, and their subsequent coping efforts may manifest in distinct ways [14]. Additionally, there may several vulnerability and resilience factors at work simultaneously that can shape an individual’s response to an adverse or stressful event [13]. As a result, it is important to consider the independent contributions of both resilience factors and vulnerability factors in defining adaptation to pain. Figure 1 represents a previously-proposed model of pain adaptation [14], adapted to reflect contributions of stable traits (resilience resources and vulnerability traits) and time-varying mechanisms of vulnerability and resilience to pain adaptation across multiple domains.
Figure 1.
Conceptual model depicting contributions of resilience and vulnerability factors to individual pain adaptation.
Despite their conceptual relationship, the composition of the resilience and vulnerability dimensions is noticeably different; the vulnerability dimension more closely reflects emotional functioning (e.g., anxiety, depression, interpersonal sensitivity), whereas the resilience dimension largely reflects coping efforts (e.g., acceptance coping, positive reinterpretation and growth) [13]. This difference may reflect an underlying “approach/avoidance” coping difference in individuals with chronic pain, such that an individual who adopts an avoidant approach to coping with pain is also more susceptible to negative pain-related outcomes [13]. In this way, we highlight the importance of approach-focused coping in resilience to pain, whereas avoidance-based coping serves to make individuals more vulnerable to maladaptive responses to pain. The current paper will examine several factors closely associated with well-being in chronic pain: pain catastrophizing, positive affect, optimism, hope, pain acceptance, and social resilience.
Pain catastrophizing and affective vulnerability to pain
A mechanism central to the examination of pain adaptation is pain catastrophizing. Pain catastrophizing refers generally to an exaggerated cognitive and affective reaction to an expected or actual pain experience [15], and is characterized by magnification of the potential negative aspects of pain, an inability to disengage from thoughts about pain, and a feeling of helplessness in coping with pain [16]. Evidence suggests that pain catastrophizing has both stable and time-varying aspects and predicts greater daily levels of emotional distress [2], predicts greater levels of physical dysfunction and occupational interference [17], and is closely related to pain intensity and depression [18]. Pain catastrophizing predicts rates of physical disability, above and beyond the effects of concurrent depression [19]. Pain catastrophizing may also worsen the experience of pain through physiological and neural pathways by enhancing the experience of pain via differential patterns of brain activation [20] and modulating the analgesic effects of medications affecting the endogenous opioid system [21]. There is plentiful evidence that highlights pain catastrophizing as a key target of psychological intervention and that reductions in pain catastrophizing are meaningfully related to improved physical and psychological functioning [15, 17].
Individuals who catastrophize about their pain are more likely to persist in using ineffective pain coping strategies, a phenomenon that has been explained largely by a “narrowing” of focus on the potential signals and dangers of pain and contributes to a more rigid and ultimately less effective style of pain coping [22••,23••]. Similarly, individuals who engage in greater levels of pain catastrophizing appear less able to disengage from signals of pain [24]. Interestingly, recent evidence suggests that the increased vigilance to pain-related cues inherent in pain catastrophizing is also reflected in differential activation of brain regions related to arousal and expectation formation [25].
Recently, researchers have posited that pain catastrophizing is a normative, rather than aberrant, process motivated by a fear of experiencing pain [23••]. Unlike theoretical models of hypochondriasis, which suggest that catastrophizing about somatic symptoms is based on erroneous and misleading beliefs, the fear-avoidance model posits that greater levels of pain have an enhancing effect on the intensity of fear because pain is a hard-wired signal designed to increase vigilance to the body and is thus not easily ignored [23••]. The fear-avoidance model of pain is an important addition to the research and conceptual base of pain adaptation as it adds a motivational component that begins to explain why individuals catastrophize about chronic pain, despite its deleterious consequences [22••]. Whereas fear of pain may be adaptive if pain is acute and signals an actual injury, such that avoidance of pain is equivalent to avoiding future injury, it holds no such value for chronic pain, which has ceased to signal damage [22••]. It is therefore unsurprising that pain catastrophizing contributes to greater levels of sustained vigilance and fear related to pain and predicts avoidance of key daily living activities for individuals with recurrent pain [26].
Elevations in pain catastrophizing narrow an individual’s cognitive focus to threat-related cues. This cognitive and attentional narrowing results in a reduced ability to seek out and identify potential resources in the physical and social environment, fosters a rigid reliance on immediately apparent coping strategies, even obviously ineffective ones, and is likely to further exacerbate the already deleterious effects of pain on emotional functioning. It is thus possible that mechanisms that are likely to bolster well-being despite chronic pain are those that broaden an individual’s focus to the environment at large and foster a more flexible and resilient response to stress and pain, thereby reducing the narrowing effects of pain catastrophizing.
Positive affect and contributors to resilient pain coping
Among the most important psychological contributors to individual well-being and resilient stress responses is positive emotion. Positive emotion has demonstrated benefits in physical well-being, such as faster recovery from surgery [27], enhanced immune system functioning [28], and increased tolerance for physically uncomfortable stimuli [29]. Evidence suggests that positive emotions may become more accessible and aid in psychological recovery after stress [30]. Positive emotions also appear to buffer individual reactivity to pain through reductions in the occurrence of pain catastrophizing [31], and enhance individual well-being across a variety of systems of human functioning, including altered neurological and autonomic functioning, regulation of negative emotional states, and strengthening of social ties [32].The broaden-and-build theory of positive emotion suggests that positive affect may aid in physical and emotional well-being and recovery from negative emotional arousal by broadening attentional and perceptual abilities in order to identify opportunities in the environment [33]. Thus, positive affect may act to counter the cognitively narrowing effects of pain and pain catastrophizing. Given the wealth of evidence for affective dysregulation [34] and specific deficits in positive emotion [35] in individuals suffering from chronic pain, it is worthwhile to consider the role of positive psychological resources like positive emotion and positive personality traits in coping with chronic pain.
Optimism, defined broadly as a relatively stable tendency towards positive outcome expectations, has proven important in physical and emotional well-being [36]. Optimism is associated with better health behaviors and physical health [37], and may predict individual differences in responsiveness of the hypothalamic-pituitary-adrenal (HPA) axis [36]. Recent evidence suggests that optimism may be especially important for individuals low in self-efficacy, mediating the relationship between objective physical functioning and subjective physical functioning for individuals with low, but not high, self-efficacy [38]. Researchers have posited that, similar to the effects of positive emotion, optimism may bolster motivational aspects of coping and subsequent physical health by orienting individuals towards potential gains and personal advancement, rather than a pervasive focus on problem prevention [39]. Such findings highlight the potential value of an optimistic outlook for individuals with chronic pain. Maintaining positive expectancies in the face of significant pain is likely to serve as a protective factor for individual well-being, and thus may be a suitable target for intervention. Indeed, recent evidence suggests that optimism levels may respond to certain interventions. Meevissen and colleagues have indicated that individuals who are trained to imagine their “best possible selves” through imagery and writing exercises show increases in dispositional optimism that seem to be maintained across time [40].
Emerging evidence suggests that hope, defined as a mental set that promotes the belief that one can pursue and achieve desired goals [41], may function similarly to optimism [31]. Feelings of hope predict lower levels of pain intensity and pain catastrophizing, function by orienting individuals to opportunities in the environment and may more closely reflect positive, goal-related cognitions than optimism [31]. Preliminary evidence also suggests that individuals may become more hopeful if they are oriented to the benefits of hope and engage in activities specifically intended to improve hope [42]. However, the positive contributions of hope to pain coping may overlap with other psychological resources; some evidence suggests that hope does not predict psychological distress in individuals with chronic pain, above and beyond the contributions of optimism and pain acceptance [41]. It may be worthwhile for future studies to examine both state and trait components of hope to individual pain adaptation, as some researchers have found that these components may have differential contributions to pain-related distress and well-being [2].
An emerging perspective in the area of chronic pain adaptation involves the construct of acceptance. Attempts to control a chronic stressor like chronic pain are often counterproductive and can magnify the negative effects of the stressor [43]. Pain acceptance has been defined as acknowledging that one has pain, stopping attempts to control pain, and learning to live a richer life in spite of pain [44]. Individuals who adopt an accepting stance toward their pain reduce their reliance on control- or avoidance-based coping, freeing their cognitive and emotional resources for more meaningful pursuits [45]. Acceptance-based coping has been identified as a promising source of potential psychological intervention for improving coping outcomes in individuals with chronic pain [46].
Recent definitions of pain acceptance have identified 2 distinct mechanisms that impact cognitive and affective reactions to pain: willingness to experience pain and activity engagement despite the presence of pain [47]. Individuals who show a greater willingness to experience pain rather than avoiding it show less pronounced increases in negative affect in response to pain, while individuals with greater levels of activity engagement are better able to bolster their positive emotions through sustained pursuit of valued activities despite their pain [48]. It is thus unsurprising that individuals higher in pain acceptance report lower levels of anxiety related to pain and lower levels of interference because of their pain [49]. Greater levels of pain acceptance have been found to predict significantly lower levels of negative affect and greater levels of positive affect in individuals with chronic pain [50]. Additionally, pain acceptance predicts greater levels of physical functioning and physical activity and lower levels of fear of physical activity and psychological distress [41,51]. Individuals who accept their chronic pain and maintain meaningful lives in spite of pain are therefore likely to experience fewer detriments at the outset of a pain flare and to adopt more effective coping strategies that aid in a return to their typical level of functioning after the onset of pain.
Like pain catastrophizing, pain acceptance can have significant implications for cognitive, emotional, and behavioral reactions to pain. Indeed, pain acceptance levels appear to mediate the relationship between pain and anxiety, depression, and physical dysfunction [52]. Research has demonstrated that pain acceptance and catastrophizing have opposing influences on individual well-being, and this interrelation of cognitive constructs is of central importance to understanding the complex mechanics of pain adaptation. Although some studies have identified only a modest negative relationship between pain acceptance and pain catastrophizing [53], individuals who adopt a more accepting stance towards their pain appear to catastrophize less about their pain [54]. Pain acceptance may also reflect a greater level of psychological flexibility that allows for broader and more adaptive responses during times of greater pain [45]. Maintenance of this flexibility during times of greater pain is especially important, given the narrowing focus that is common during times of pain and is commonly a consequence of catastrophizing about pain [23••]. These findings may indicate the way in which pain catastrophizing and pain acceptance differ: whereas pain catastrophizing contributes to a narrower and more rigid style of coping with a painful experience, acceptance of pain appears to retain cognitive resources that can be flexibly applied to identify more effective pain coping responses. We might then expect that pain catastrophizing and pain acceptance may not simply be stable traits, but instead, may reflect both stable and time-varying processes that may wax and wane at various times. It is thus worthwhile to consider whether pain acceptance contains a state component.
Research has indicated that a variety of psychological constructs contain both trait and state components, including positive and negative affect [55], pain intensity [55] and pain catastrophizing [2,56]. Similarly, researchers have identified pain acceptance as a potentially important mechanism of change in psychological interventions for chronic pain populations [46]. Particularly for those individuals who have undergone acceptance-based interventions to improve their skills for coping with chronic pain, it is reasonable to consider whether acceptance of pain may not be stable, but instead fluctuate around an individual mean (i.e., individuals who are more accepting of their pain may still have moments of greater or less acceptance). To the authors’ knowledge, no study has examined whether a state component of pain acceptance exists. This distinction may have relevance for several reasons. First, identification of a state component of pain acceptance may add a key element in testing individual models of pain adaptation. Just as pain catastrophizing has proven to be a key mechanism of both momentary and trait affective dysregulation in individuals with chronic pain [2], momentary thoughts of pain acceptance may provide a key indicator of state resilience for those same individuals. If a state component of pain acceptance does exist, its exclusion from daily pain coping models yields at best an incomplete representation of individual pain coping efforts. State pain acceptance may also provide a valuable indicator for individuals undergoing psychological intervention targeting improvement of their pain coping efforts. One viable hypothesis might predict that mean pain acceptance scores might increase after completion of an acceptance-based intervention, but we might also expect less variability in state pain acceptance scores after intervention as well. An individual who has successfully undergone an acceptance-based intervention might exhibit a greater degree of consistency in accepting their pain, even during times of increased pain or stress.
Social resilience and chronic pain
Although a great deal of research has focused on intra-individual processes that contribute to resilient coping, individual resilience is also clearly dependent on social relations [57]. Indeed, Zautra [58] wrote, “Resilience is social, after all,” in a chapter accompanying other papers examining the factors associated with adaptation to trauma. In his chapter, meant to counterbalance the overwhelming attention to intrapsychic determinants of resilience or the lack thereof, he reminds us that the primary sources of positive emotion are beneficial social interactions. Social resilience has been observed in individuals’ utilization of social resources to recover from stress [59], and the frequency, nature, and quality of social interactions can have a significant effect on adaptation to chronic pain. Individuals with chronic pain are thus able to adapt to their condition more readily than those without those social resources [13].
In general, individuals who seek out social support exhibit greater levels of individual resilience [60] and report greater levels of life satisfaction and lower levels of depression [61]. Individuals with chronic pain report less severe pain and show less activation of the central nervous system under painful conditions when they are in the presence of their significant other [62]. However, the effects of social support are decidedly more nuanced than they might initially appear. Beyond the mere availability of friends and family who may provide support during periods of stress, the perceived quality of social support may play a significant role in the degree to which such support fosters resilient coping. In individuals with fibromyalgia, both quality and quantity of social support predict successful adaptation to pain, but the quality of social support seems to be more important in predicting indicators of individual well-being [63]. A social network that is too large or focused on aiding an individual in coping with their pain may actually reduce that individual’s self-sufficiency and lead to worse long-term pain coping [63]. In addition, intimate social relationships may influence the frequency of pain displays; individuals with chronic pain display greater frequencies of pain behaviors if their spouses catastrophize less about their pain [64].
However, individuals are not always able to successfully initiate positive social interactions, even with the people closest to them. When individuals experience a high level of pain, they may lose the ability to appreciate the complex nature of their social relationships and become prone to classifying their relationships as entirely positive or negative. Just as individuals who maintain emotional complexity are able to bolster their positive emotions during times of pain or stress, individuals who recognize social complexity are able to appreciate the positive aspects of their social relationships even during their worst moments. The failure to recognize “social complexity” may lead to an inability to seek or appreciate positive social interactions, and may endanger valued sources of support during times of interpersonal conflict [65]. During times of increased pain, individuals may be less willing or able to notice or evaluate their social interactions as positive. Given the potential biases in observational studies utilizing self-report measures, this phenomenon may be best clarified in an experimental setting. Experimental studies utilizing pain induction have indicated that under conditions of pain, individuals demonstrate an increased narrowing of focus and vigilance to pain-related cues [24], and evidence suggests that this hypervigilance may be a largely automatic reaction that occurs even at the detriment of performance in other areas [22••]. It would thus be valuable to determine if individuals under conditions of increased pain become unable to recognize or appreciate their positive relationships. Given that social support is a powerful resource in maintaining individual resilience to pain [60, 61], examining the ability to notice and appreciate social support under conditions of pain may provide valuable understanding of the effects of social support, as well as illuminate times when social support fails to bolster individual coping.
Future directions of study
There are several prospective areas of research that could further strengthen our understanding of adaptation to chronic pain. It appears that personality traits may prove important in clarifying the complexity of pain adaptation; the personality trait of extraversion, though apparently unrelated to the sensory experience of pain [66], is predictive of more adaptive attitudes toward pain coping in arthritis populations [67] and has also been identified as a contributor to resilience in arthritis populations [68]. It is thus possible that individuals with chronic pain who are more extraverted better maintain their engagement with others during times of increased pain, which may have significant implications for their momentary emotional states. Similarly, the construct of pain acceptance may relate to another stable personality construct: openness to experience. Recent evidence has connected the constructs of openness and psychological flexibility [69], and others have noted that openness reflects a flexibility to adapt to challenges and to effectively manage one’s own emotional states, which are instrumental in the maintenance of good physical health [70]. Consideration of these personality traits is therefore necessary in developing a comprehensive representation of individual pain adaptation.
Basic correlational studies, while important in preliminary phases of research, are not sufficient to yield precise and complex models of psychological adaptation and resilience. Instead, future research should be directed towards more complex and comprehensive models that reflect concurrent contributions to adaptation through the examination of multiple and competing mediators and moderators of direct relationships [71]. Another key to advancing our understanding of pain adaptation is an increased focus on experimental research to supplement existing observational studies. Use of attentional and information-processing [22••,25] and motivational theories of pain adaptation [22••] may yield hypotheses that further supplement current pain coping models. Finally, it is important to expand the scope of experimental variables relevant to pain coping. Studies that examine basic emotional responses to pain induction (e.g., changes in negative or positive affect) or simple, largely passive behaviors (pain tolerance and threshold) are valuable contributions to understanding pain reactions, but lack ecological validity and are not wholly adequate for predicting real-world pain behavior. These studies do not examine more ecologically pertinent questions: how might we define persistence in pain populations, and what keeps individuals performing their everyday tasks despite their pain? These questions are of central importance in chronic pain populations; individuals with pain may adopt a mindset focused on ignoring their pain, subsequently extend their physical activity beyond reasonable limits, and result in exacerbated physical and emotional dysfunction [22••]. Observations of pain-ignoring behavior have led to an increased call for examination of motivational factors in pain adaptation in order to clarify what factors may lead individuals with chronic pain to persist in strenuous activities, even to the point of clear physical or psychological detriment [22••]. This phenomenon may occur even when individuals hold little expectation of finding an effective solution to their pain, which may suggest that this persistence in the face of failure reflects a similar cognitive narrowing as those individuals who engage in pain catastrophizing.
One recent study utilized a novel experimental procedure and found that trait levels of pain catastrophizing in testing persistence to a painful finger-tapping task modulated the effect of a negative mood condition [72••]. This study utilized both motivational and information-processing theories to formulate and test more complex hypotheses related to pain adaptation. Furthermore, the study is noteworthy because it utilized an experimental procedure that tested not only mood states and pain tolerance, but also a more ecologically valid pain behavior. A greater focus on nuances like the immediate relationship between pain and behavior is a promising avenue by which experimental pain studies can examine task perseverance despite pain, a construct that is likely to inform conceptualization of pain-related adjustment problems, as well as interventions that may target pain-related disability and occupational dysfunction.
In summary, the psychological literature is rich in observational research and basic experimental studies that have illuminated the direct relationships between the experience of pain and a series of cognitive, affective, behavioral, and neurophysiological states. These studies have provided a valuable framework by which we can begin to construct a more advanced understanding of how individuals with chronic pain adapt and function from day to day. However, we must strive to improve the specificity and complexity of our models as pain, itself a complex physical and psychological force, demonstrates consequences that ripple across all domains of human functioning. Researchers should continue to combine our existing knowledge of pain-behavior and pain-cognition relationships and begin to ask deeper questions: why do these relationships exist? Where do catastrophic pain-related thoughts come from, what concurrent cognitive and neurological phenomena might they reflect, and what purpose might they serve? What might compel an individual to engage in avoidant or approach behaviors related to pain? It is only through the synthesis of multiple systems of analysis and concurrent examination of behavior, cognition, emotion, motivation, information processing, and neurophysiology that we might begin to achieve greater levels of descriptive and predictive precision in the examination of pain adaptation.
Table 1.
Table of Definitions
| Term | Definition |
|---|---|
| Pain Adaptation | An overall process of coping with pain, accounting for both positive and negative contributors to coping. |
| Resilience | Maintenance of positive physical and emotional functioning in spite of significant difficulty or challenge |
| Vulnerability | Factors that contribute to worsened physical and psychological functioning in response to stress |
| Well-Being | Denotes positive physical and psychological states |
| Distress | Denotes negative physical and psychological states |
| Optimism | A relatively stable tendency towards positive outcome expectations that orients attention and behavior towards opportunities in the environment |
| Hope | A mental set that promotes the belief that one can pursue and achieve desired goals |
| Pain Acceptance | A process of acknowledging that one has pain, stopping maladaptive attempts to control pain, and learning to live a richer life in spite of pain |
| Psychological Flexibility | A process of maintaining or altering behavior in response to environmental demands to maximize adaptive coping and short-term and long-term well-being |
Acknowledgments
The authors wish to thank members of the Resilience Solutions Group. The members of the Resilience Solutions Group (RSG) in addition to the authors of this article are, in alphabetical order: Leona Aiken, Felipe Castro, Mary Davis, Roger Hughes, Martha Kent, Rick Knopf, Kathy Lemery, Linda Luecken, Morris Okun, and John Reich. This work is supported in part by a grant from the National Institute on Aging (R01 AG 026006), Alex Zautra (PI), John Hall (Co-PI). In addition, the authors are grateful to St. Luke’s Charitable Trust and the Arizona State University Office of the Vice President for Research for invaluable support of the RSG.
References
- 1.Dersh J, Polatin PB, Gatchel RJ: Chronic pain and psychopathology: research findings and theoretical considerations. Psychosom Med 2002, 64: 773–786. [DOI] [PubMed] [Google Scholar]
- 2.Sturgeon JA, Zautra AJ: State and trait pain catastrophizing and emotional health in rheumatoid arthritis. Ann Behav Med 2012. DOI 10.1007/s12160-012-9408-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melzack R, Wall PD. The Challenge of Pain. New York, NY: Basic Books; 1982. [Google Scholar]
- 4.Geisser ME, Robinson ME, Keefe FJ, et al. : Catastrophizing, depression and the sensory, affective, and evaluative aspects of chronic pain. Pain 1994, 59: 79–83. [DOI] [PubMed] [Google Scholar]
- 5.Wierzbicka A Is pain a human universal? A cross-linguistic and cross-cultural perspective on pain. Emotion Review 2012, 4: 307–317. [Google Scholar]
- 6.Kross E, Berman MG, Mischel W, et al. : Social rejection shares somatosensory representations with physical pain. Proc Nat Acad Sci USA 2011, 108: 6270–6275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karatsoreos IN, McEwen BS: Psychobiological allostasis: resistance, resilience, and vulnerability. Trends Cogn Sci 2011, 15: 576–584. [DOI] [PubMed] [Google Scholar]
- 8.•. Yeung EW, Arewasikporn A, Zautra AJ: Resilience and chronic pain. J Soc Clin Psychol 2012, 31: 593–617. This recent review article offers a more comprehensive model of pain coping that integrates the traditional focus on intra-individual processes of adaptation with a consideration of the contributions of the social world on well-being for individuals with chronic pain.
- 9.Rutter M: Psychosocial resilience and protective mechanisms. Am J Orthopsychiat 1987, 57:316–331. [DOI] [PubMed] [Google Scholar]
- 10.Luthar SS, Cicchetti D, Becker B: The construct of resilience: a critical evaluation and guidelines for future work. Child Dev 2000, 71:543–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murray K, Zautra AJ. Community resilience: fostering recovery, sustainability, and growth. In: Ungar M, editor. The social ecology of resilience: A handbook of theory and practice. New York: Springer; 2011. pp. 337–346. [Google Scholar]
- 12.Zautra AJ, Arewasikporn A, Davis MC: Resilience: promoting well-being through recovery, sustainability, and growth. Res Hum Dev 2010, 7: 221–238. [Google Scholar]
- 13.Smith BW, Zautra AJ: Vulnerability and resilience in women with arthritis: test of a two-factor model. J Consult Clin Psychol 2008, 76:799–810. [DOI] [PubMed] [Google Scholar]
- 14.Sturgeon JA, Zautra AJ: Resilience: a new paradigm for adaptation to chronic pain. Curr Pain Headache Rep 2010, 14: 105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sullivan MJL, Thorn B, Haythornthwaite JA, et al. : Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 2001, 17: 52–64. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan MJL, Bishop SR, Pivik J: The Pain Catastrophizing Scale: development and validation. Psychol Assess 1995, 7:524–532. [Google Scholar]
- 17.Westman AE, Boersma K, Leppert J, et al. : Fear-avoidance beliefs, catastrophizing, and distress: a longitudinal subgroup analysis on patients with musculoskeletal pain. Clin J Pain 2011, 27: 567–577. [DOI] [PubMed] [Google Scholar]
- 18.Edwards RR, Cahalan C, Mensing G, et al. : Pain, catastrophizing, and depression in the rheumatic diseases. Nat Rev Rheumatol 2011, 7: 216–224. [DOI] [PubMed] [Google Scholar]
- 19.Arnow BA, Blasey CM, Constantino MJ, et al. : Catastrophizing, depression, and pain-related disability. Gen Hosp Psychiat 2011, 33:150–156. [DOI] [PubMed] [Google Scholar]
- 20.Rhudy JL, Martin SL, Terry EL, et al. : Pain catastrophizing is related to temporal summation of pain but not temporal summation of the nociceptive flexion reflex. Pain 2011, 152: 794–801. [DOI] [PubMed] [Google Scholar]
- 21.King CD, Goodin B, Kindler LL, et al. : Reduction of conditioned pain modulation in humans by naltrexone: an exploratory study of the effects of pain catastrophizing. J Behav Med. 2012; doi: 10.1007/s10865-012-9424-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.••. Crombez G, Eccleston C, Van Damme S, et al. : Fear-avoidance model of chronic pain: the next generation. Clin J Pain 2012;28: 475–483 This recent review article re-examines the concept of pain-related disability by detailing the fear-avoidance model of chronic pain, a theory that reconceptualizes pain catastrophizing as a normative process and offers the additional consideration of motivational factors to construction of pain adaptation models.
- 23.••. Crombez G, Viane I, Eccleston C, et al. : Attention to pain and fear of pain in patients with chronic pain. J Behav Med. 2012; doi: 10.1007/s10865-012-9433-1 This recent article utilizes an advanced method of observational analysis, Ecological Momentary Assessment, to construct a detailed examination of the relationships between attentional, emotional, and cognitive factors in day-to-day coping with chronic pain.
- 24.Van Damme S, Crombez G, Eccleston C. The anticipation of pain modulates spatial attention: evidence for pain specificity in high-pain catastrophizers. Pain 2004, 111: 392–399. [DOI] [PubMed] [Google Scholar]
- 25.Vase L, Egsgaard LL, Nikolajsen L, et al. : Pain catastrophizing and cortical responses in amputees with varying levels of phantom limb pain: a high-density EEG brain-mapping study. Exp Brain Res 2012, 218: 407–417. [DOI] [PubMed] [Google Scholar]
- 26.Westman AE, Boersma K, Leppert J, et al. : Fear-avoidance beliefs, catastrophizing, and distress: a longitudinal subgroup analysis on patients with musculoskeletal pain. Clin J Pain 2011, 27: 567–577. [DOI] [PubMed] [Google Scholar]
- 27.Seebach CL, Kirkhart M, Lating JM, et al. : Examining the role of positive and negative affect in recovery from spine surgery. Pain 2011, 153: 518–525. [DOI] [PubMed] [Google Scholar]
- 28.Pressman SD, Black LL. Positive emotions and immunity. In: Segerstrom S, editor. The Oxford Handbook of Psychoneuroimmunology. New York: Oxford University Press; 2012. pp. 92–104. [Google Scholar]
- 29.Van Laarhoven AIM, Walker AL, Wilder-Smith OH, et al. : Role of induced negative and positive emotions in sensitivity to itch and pain in women. Brit J Dermatol 2012, 167: 262–269. [DOI] [PubMed] [Google Scholar]
- 30.Dewall CM, Twenge JM, Koole SL, et al. : Automatic emotion regulation after social exclusion: Tuning to positivity. Emotion 2011, 11: 623–636. [DOI] [PubMed] [Google Scholar]
- 31.Hood A, Pulvers K, Carrillo J, et al. : Positive traits linked to less pain through lower pain catastrophizing. Pers Indiv Differ 2012, 52: 401–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tugade MM. Positive emotions and coping: Examining dual-process models of resilience. In: Folkman S, editor. The Oxford Handbook of Stress, Health, and Coping. New York: Oxford University Press; 2011. pp. 186–199. [Google Scholar]
- 33.Algoe SB, Fredrickson BL: Emotional fitness and the movement of affective science from lab to field. Am Psychol 2011, 66: 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Finucane AM, Dima A, Ferreira N, et al. : Basic emotion profiles in healthy, chronic pain, depressed and PTSD individuals. Clin Psychol Psychother 2012, 19: 14–24. [DOI] [PubMed] [Google Scholar]
- 35.Zautra AJ, Fasman R, Reich JW, et al. : Fibromyalgia: Evidence for deficits in positive affect regulation. Psychosom Med 2005, 67: 147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Endrighi R, Hamer M, Steptoe A: Associations of trait optimism with diurnal neuroendocrine activity, cortisol responses to mental stress, and subjective stress measures in healthy men and women. Psychosom Med 2012, 73: 672–678. [DOI] [PubMed] [Google Scholar]
- 37.Soliah LL: The role of optimism regarding nutrition and health behavior. Am J Lifestyle Med 2011, 5: 63–68. [Google Scholar]
- 38.Warner LM, Schwarzer R, Schuz B, et al. : Health-specific optimism mediates between objective and perceived physical functioning in older adults. J Behav Med 2012, 35: 400–406. [DOI] [PubMed] [Google Scholar]
- 39.Hazlett A, Molden DC, Sackett AM: Hoping for the best or preparing for the worst? Regulatory focus and preferences for optimism and pessimism in predicting personal outcomes. Soc Cognition 2011, 29: 74–96. [Google Scholar]
- 40.Meevissen YMC, Peters ML, Alberts HJEM: Become more optimistic by imagining a best possible self: Effects of a two week intervention. J Behav Ther & Exp Psychiat 2011, 42: 371–378. [DOI] [PubMed] [Google Scholar]
- 41.Wright MA, Wren AA, Somers TJ, et al. : Pain acceptance, hope, and optimism: Relationships to pain and adjustment in patients with chronic musculoskeletal pain. J Pain 2011, 12: 1155–1162. [DOI] [PubMed] [Google Scholar]
- 42.Duggleby WD, Degner L, Williams A, et al. : Living with hope: Initial evaluation of a psychosocial hope intervention for older palliative home care patients. J Pain Symptom Manage 2007, 33: 247–257. [DOI] [PubMed] [Google Scholar]
- 43.Notebaert L, Crombez G, Vogt J, et al. : Attempts to control pain prioritize attention towards signals of pain: An experimental study. Pain 2011, 152: 1068–1073. [DOI] [PubMed] [Google Scholar]
- 44.McCracken LM: Learning to live with the pain: acceptance of pain predicts adjustment in persons with chronic pain. Pain 1998, 74:21–27. [DOI] [PubMed] [Google Scholar]
- 45.Thompson M, McCracken LM: Acceptance and related processes in adjustment to chronic pain. Curr Pain Headache Rep 2011, 15: 144–151. [DOI] [PubMed] [Google Scholar]
- 46.Wetherell JL, Afari N, Rutledge T, et al. : A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain 2011, 152: 2098–2107. [DOI] [PubMed] [Google Scholar]
- 47.McCracken LM: Toward understanding acceptance and psychological flexibility in chronic pain. Pain 2010, 149: 420–421. [DOI] [PubMed] [Google Scholar]
- 48.Kranz D, Bollinger A, Nilges P: Chronic pain acceptance and affective well-being: A coping perspective. Eur J Pain 2010, 14: 1021–1025. [DOI] [PubMed] [Google Scholar]
- 49.Huggins JL, Bonn-Miller MO, Oser ML, et al. : Pain anxiety, acceptance, and outcomes among individuals with HIV and chronic pain: A preliminary investigation. Behav Res Ther 2011, 50: 72–78. [DOI] [PubMed] [Google Scholar]
- 50.Cho S, McCracken LM, Heiby EM, et al. : Pain acceptance-based coping in complex regional pain syndrome type I: Daily relations with pain intensity, activity, and mood. J Behav Med 2012, DOI 10.1007/s10865-012-9448-7 [DOI] [PubMed] [Google Scholar]
- 51.Gyurcsik NC, Brawley LR, Spink KS, et al. : Is level of pain acceptance differentially related to social cognitions and behavior? The case of active women with arthritis. J Health Psychol 2011, 16: 530–539. [DOI] [PubMed] [Google Scholar]
- 52.Bendayan R, Esteve R, Blanca MJ: New empirical evidence of the validity of the Chronic Pain Acceptance Questionnaire: The differential influence of activity engagement and pain willingness on adjustment to chronic pain. Brit J Health Psychol 2011, 17: 314–326. [DOI] [PubMed] [Google Scholar]
- 53.Kratz AL, Davis MC, Zautra AJ: Pain acceptance moderates the relation between pain and negative affect in osteoarthritis and fibromyalgia patients. Ann Behav Med 2007, 33:291–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vowles KE, McCracken LM, Eccleston C: Processes of change in treatment for chronic pain: The contributions of pain, acceptance, and catastrophizing. Eur J Pain 2007, 11: 779–787. [DOI] [PubMed] [Google Scholar]
- 55.Geisser ME, Robinson ME, Keefe FJ, et al. : Catastrophizing, depression and the sensory, affective, and evaluative aspects of chronic pain. Pain 1994, 59: 79–83. [DOI] [PubMed] [Google Scholar]
- 56.Turner JA, Mancl L, Aaron LA: Pain-related catastrophizing: A daily process study. Pain 2004, 110: 103–111. [DOI] [PubMed] [Google Scholar]
- 57.Arewasikporn A, Davis MC, Zautra A. Resilience: a framework for understanding the dynamic relationship between social relations and health. In Newman M, Roberts N, editors. Health and Social Relationships. Washington, DC: American Psychological Association; in press. [Google Scholar]
- 58.Zautra AJ. Resilience is social, after all. In: Kent M, Davis MC, Reich JW, editors. Handbook of Resilience Approaches to Stress and Trauma. New York: Rutledge; in press. [Google Scholar]
- 59.Friborg O, Hjemdal O, Rosenvinge JH, et al. : Resilience as a moderator of pain and stress. J Psychosom Res 2006, 61: 213–219. [DOI] [PubMed] [Google Scholar]
- 60.Connor KM, Davidson JRT: Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003, 18: 76–82. [DOI] [PubMed] [Google Scholar]
- 61.Ferreira VM, Sherman AM: The relationship of optimism, pain, and social support to well-being in older adults with osteoarthritis. Aging Ment Health 2007, 11: 89–98. [DOI] [PubMed] [Google Scholar]
- 62.Montoya P, Larbig W, Braun C, et al. : Influence of social support and emotional context on pain processing and magnetic brain responses in fibromyalgia. Arthritis Rheum 2004, 50: 4035–4044. [DOI] [PubMed] [Google Scholar]
- 63.Franks HM, Cronan TA, Oliver K: Social support in women with fibromyalgia: Is quality more important than quantity? J Community Psychol 2004, 32: 425–438. [Google Scholar]
- 64.Gauthier N, Thibault P, Sullivan MJL. Catastrophizers with chronic pain display more pain behavior when in a relationship with a low catastrophizing spouse. Pain Res Manage 2011, 16: 293–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Davis MC, Zautra AJ, Smith BW: Chronic pain, stress, and the dynamics of affective differentiation. J Pers 2004, 72: 1133–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Harkins SW, Price DD, Braith J: Effects of extraversion and neuroticism on experimental pain, clinical pain, and illness behavior. Pain 1989, 36: 209–218. [DOI] [PubMed] [Google Scholar]
- 67.Ingledew DK, Markland D, Sheppard KE: Personality and self-determination of exercise behaviour. Pers Indiv Differ 2004, 36: 1921–1932. [Google Scholar]
- 68.Wright LM, Zautra AJ, Going S: Adaptation to early knee osteoarthritis: The role of risk, resilience, and disease severity on pain and physical functioning. Ann Behav Med 2008, 36: 70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Silvia PJ, Nusbaum EC, Berg C, et al. : Openness to experience, plasticity, and creativity: Exploring lower-order, high-order, and interactive effects. J Res Pers 2009, 43: 1087–1090. [Google Scholar]
- 70.Kashdan TB: Psychological flexibility as a fundamental aspect of health. Clinical Psychol Rev 2010, 30: 865–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shahar G, Elad-Strenger J, Henrich CC: Risky resilience and resilient risk: The key role of intentionality in an emerging dialectics. J Soc Clin Psychol 2012, 31: 618–640. [Google Scholar]
- 72.••. Karsdorp PA, Ranson S, Schrooten MGS, et al. : Pain catastrophizing, threat, and the informational value of mood: Task persistence during a painful finger pressing task. Pain 2012, 153: 1410–1417. This recent experimental article offers a more ecologically valid pain coping variable, testing task persistence under a painful experimental condition. This article also provides a valuable perspective on the value of integration of cognitive and informational processing theories of pain.