Abstract
Background
Patient function after arthrodesis of the first metatarsophalangeal joint (MTPJ) relies on proper positioning of the first MTPJ. To maximize the likelihood of good postoperative function, the dorsiflexion angle, referred to as the fusion sagittal angle, should range between 20° and 30°, corresponding to 10° to 15° of dorsiflexion off the weightbearing axis. However, achieving appropriate sagittal alignment intraoperatively is challenging. The artificial floor technique (AFT) uses a rigid, flat surface to simulate the weightbearing position of the foot intraoperatively to accurately position the first MTPJ without fluoroscopy. This technique has been previously described and is commonly used but, to our knowledge, it has never been validated.
Questions/purposes
(1) Is the AFT a valid and repeatable technique for positioning the fusion sagittal angle between 20° and 30° of dorsiflexion from the first metatarsal? (2) Does the fusion sagittal angle obtained using the AFT vary with foot size?
Methods
In this retrospective study, a search was performed using Current Procedural Terminology codes for patients undergoing first MTPJ arthrodesis by one surgeon between June 2012 and June 2020. The surgical technique used during this time did not vary and consisted of the use of a rigid, flat, sterile surface. The entire foot was placed flat on the surface, simulating the weightbearing position and allowing for an evaluation of the fusion sagittal angle of the first MTPJ. The target sagittal alignment was achieved when the soft tissue of the plantar surface at the distal-most aspect of the proximal phalanx was measured (using a sterile ruler) as 1 cm off the artificial floor. The recommended fusion sagittal angle falls within a range of 20° to 30°, which allows for 1-mm to 2-mm variations in measuring the elevation of the proximal phalanx off the artificial floor. Fixation was achieved with two 2.8-mm threaded, double-pointed Steinmann pins placed through the intramedullary canal of the proximal and distal phalanges and into the first metatarsal. Once fixation was achieved, the fusion sagittal angle was confirmed with the AFT without using fluoroscopy. Postoperatively, patients were allowed to bear weight fully on their heels in a postoperative, rigid-soled shoe. During the study period, 117 patients (135 feet) underwent first MTPJ arthrodesis utilizing the AFT for either first MTPJ arthritis/hallux rigidus, hallux valgus, or inflammatory arthropathy. Of those, we considered patients with preoperative AP and lateral weightbearing radiographs and patients with AP and lateral weightbearing radiographs at 3 months postoperatively after the removal of the internal fixation construct as eligible for analysis. Based on these criteria, 84% (113 of 135) of feet were included in the final radiographic analysis. Sixteen percent (22 of 135) of the feet were excluded because postoperative radiographs demonstrating the removal of the internal fixation construct were absent from the Picture Archiving and Communication System (PACS) in these cases. The length of the whole foot, first metatarsal, and proximal phalanx were measured on preoperative weightbearing radiographs. In addition, fusion sagittal angles were measured on weightbearing radiographs after removal of internal fixation construct at a minimum of 3 months postoperatively (mean 3.5 ± 2.2 months). No patients were lost to follow-up before obtaining those radiographs. Two qualified reviewers independently evaluated each radiograph. We ascertained inter- and intraobserver reliability using intraclass correlation coefficients (ICCs). We determined whether the fusion sagittal angle obtained using the AFT varied with foot size by using a multiple linear regression model.
Results
In the entire study group, the mean fusion sagittal angle using the AFT was 27° ± 4°. The interobserver ICC of the fusion sagittal angle measurements was 0.92 (95% confidence interval [CI] 0.56 to 0.97; p < 0.001). The intraobserver ICC for reviewer 1 was 0.95 (95% CI 0.92 to 0.97; p < 0.001) and the intraobserver ICC for reviewer 2 was 0.97 (95% CI 0.88 to 0.98; p < 0.001). Ninety-one percent (103 of 113) of the study group fell within the acceptable range of 20° to 30° ± 2°. The multiple linear regression analyses demonstrated that the preoperative lengths of the whole foot (β =-0.05 [95% CI -0.12 to 0.02]; p = 0.16), proximal phalanx (β =-0.13 [95% CI -0.46 to 0.20]; p = 0.44), and first metatarsal (β = 0.13 [95% CI -0.10 to 0.35]; p = 0.27) were not independently associated with the postoperative fusion sagittal angle.
Conclusion
The AFT allows for accurate and reproducible positioning of the first MTPJ within the appropriate functional range of dorsiflexion, regardless of foot size. Additionally, this technique can be performed without fluoroscopy and so avoids radiation exposure to the patient and the surgical team.
Level of Evidence
Level III, therapeutic study.
Introduction
Arthrodesis of the first metatarsophalangeal joint (MTPJ) is commonly used to treat an array of pathologic conditions affecting this joint, including endstage Grade 4 degenerative arthritis (Fig. 1), failed cheilectomy, severe and/or recurrent hallux valgus, and inflammatory arthropathies [2, 5, 9, 25, 26]. Numerous fixation methods have been described, including dorsal plates [4, 10, 16, 17], a single intramedullary lag screw [20], crossed screwed fixation [6, 12], Steinmann pins [24], and Kirschner wires [27]. Regardless of fixation strategy, the clinical outcome and patient function after the procedure are predicated on correct positioning of the fused joint. The recommended coronal plane alignment for first MTPJ arthrodesis ranges from 10° to 15° and is relatively easy to visualize intraoperatively based on the alignment of the second toe [7, 11, 16]. Studies have shown that first metatarsophalangeal dorsiflexion alignment in the sagittal plane, which is referred to as the fusion sagittal angle, should range from 20° to 30°, which correlates with positioning the toe between 10° and 15° off the weightbearing axis [7, 8, 13, 14, 16, 17]. Bayomy et al. [2] demonstrated that a fusion sagittal angle greater than 30° is associated with increased pressure on the plantar surface of the first metatarsal head, and other authors [18] showed that a fusion sagittal angle less than 20° impairs gait. Although surgeons may vary the fusion sagittal angle based on the patient’s shoe wearing preferences, these biomechanical studies reveal the importance of maintaining the fusion sagittal angle between 20° and 30°.
Fig. 1.
A-B Preoperative weightbearing (A) AP and (B) lateral radiographs of a left foot demonstrate hallux rigidus of the first MTPJ with subchondral sclerosis, marked loss of articular cartilage, and dorsal osteophytes.
However, accurate intraoperative measurement of the fusion sagittal angle is challenging when attempting to interpret fluoroscopic imaging (Fig. 2). In addition, the radiation exposure secondary to fluoroscopy, although small, confers a risk to the surgical team and patient during orthopaedic procedures [1, 3, 22]. When obtaining fluoroscopic intraoperative images, radiation exposure to the surgeon’s hand is often required to maintain the provisional position of the great toe before fixation. It is important for the surgeon to use a reliable and replicable technique that results in proper joint alignment, regardless of foot size, to achieve an ideal fusion sagittal angle when performing first MTPJ arthrodesis. Regardless of whether the surgeon uses fluoroscopy for this procedure, it is also expeditious to accurately position the sagittal alignment before definitive fixation. At our institution, the senior author (REM) uses an intraoperative technique that accurately positions the first MTPJ in the sagittal plane. This technique uses an artificial floor consisting of a rigid flat surface (often a metal tray or box) that provides a stable reference point to position the plantar surface of the foot. Although we believe this approach has been previously used [13, 28], to our knowledge it has never been formally validated. It would be important to know whether different observers can reproducibly measure the fusion sagittal angle, and whether using this approach results in well-positioned MTPJ arthrodeses. Given that foot size may influence the measured angles in the operating room with this approach, it is also important to ascertain whether the artificial floor technique (AFT) results in accurate fusion positions across a clinically relevant range of foot sizes, such as might be represented in a series over a long span of time by a high-volume subspecialist.
Fig. 2.
A-C Intraoperative fluoroscopic sagittal images of patients undergoing first MTPJ arthrodesis illustrate the difficulty of accurately interpreting and measuring the fusion sagittal angle. In (A) and (B), exposure of the surgeon’s hand is required to maintain the position of the MTPJ arthrodesis for the fluoroscopic image. (C) This fluoroscopic image shows alignment was maintained with fixation in place.
We therefore asked: (1) Is the AFT a valid and repeatable technique for positioning the fusion sagittal angle between 20° and 30° of dorsiflexion from the first metatarsal? (2) Does the fusion sagittal angle obtained using the AFT vary with foot size?
Patients and Methods
Study Design and Setting
This was a retrospective study that drew patients from the practice of one high-volume foot and ankle subspecialist (REM) who practices in an urban setting.
Patients
We performed a search using Current Procedural Terminology codes for patients undergoing first MTPJ arthrodesis by one surgeon (REM) between June 2012 and June 2020. The surgical technique used during this time did not vary. The surgeon used the AFT to determine the position of the MTPJ during surgery for all procedures, and the surgeon did not use fluoroscopy in any of these procedures.
During the study period, 117 patients (135 feet) underwent first MTPJ arthrodesis using the AFT for either first MTPJ arthritis/hallux rigidus, hallux valgus, or inflammatory arthropathy. Of those, patients aged 18 years and older, those with preoperative AP and lateral weightbearing radiographs, and those with AP and lateral weightbearing radiographs at 3 months postoperatively after the removal of the internal fixation construct (Fig. 3) were considered eligible for analysis. Based on these criteria, 84% (113 of 135) of feet were included in the final radiographic analysis (Table 1). Sixteen percent (22 of 135) of feet were excluded because postoperative radiographs demonstrating the removal of the internal fixation construct were missing from the Picture Archiving and Communication System (PACS) in these procedures. Twenty-five percent (28 of 113) of patients were male and 75% (85 of 113) were female, with a mean age of 65 ± 8.8 years. There were 62 right feet and 51 left feet. Postoperative radiographs were performed at a mean of 3.5 ± 2.2 months after the index procedure. No patients were lost to follow-up before obtaining these postoperative radiographs.
Fig. 3.
A-B Postoperative weightbearing (A) AP and (B) lateral radiographs of the right foot of a 66-year-old woman taken 13 weeks after surgery demonstrate fusion across the first MTPJ.
Table 1.
Patient characteristics and radiographic outcomes
| Characteristic or outcome | Value |
| Number of patients (number of feet) | 100 (113) |
| Females | 75 (85) |
| Fusion sagittal angle (combined) in °a | 27 ± 4 |
| Fusion sagittal angle (reviewer 1) in °a | 26 ± 5 |
| Fusion sagittal angle (reviewer 2) in °a | 28 ± 5 |
| Difference between fusion sagittal angle measurements (reviewer 1) in ° | 0.95 ± 1 |
| Difference between fusion sagittal angle measurements (reviewer 2) in ° | 0.66 ± 2 |
| Whole foot length in mmb | 248 ± 21 |
| Proximal phalanx length in mmb | 31 ± 4 |
| First metatarsal length in mmb | 65 ± 7 |
Data presented as % (n) or mean ± SD.
Measured on postoperative lateral weightbearing radiographs.
Measured on preoperative AP and lateral weightbearing radiographs.
Measurements
The fusion sagittal angles were measured on postoperative lateral weightbearing radiographs, which were obtained after successful fusion and removal of the fixation construct. Two qualified reviewers (JTS, ASR) evaluated the radiographs; they measured the fusion sagittal angle independently and on two separate occasions, 3 weeks apart. There were four distinct measurements of the fusion sagittal angle. The method of measuring the fusion sagittal angle on postoperative radiographs was conducted using a technique described by Nawoczenski et al. [21]. Finally, to determine foot size, the lengths of the foot, proximal phalanx, and first metatarsal were obtained on preoperative AP and lateral weightbearing radiographs. The mean foot, proximal phalanx, and first metatarsal lengths were 248.1 mm, 30.6 mm, and 65 mm, respectively.
Surgical Technique
The same surgical technique was used for first MTPJ arthrodesis in all procedures. After subperiosteal exposure using a dorsomedial longitudinal incision, the surgeon removed the remaining articular surfaces with a microsagittal saw. Alignment of the first MTPJ was checked using the AFT without fluoroscopy (Fig. 4). The rigid, flat, sterile surface was brought into the operating field. The knee was placed in slight flexion to allow the entire foot to be placed flat on the artificial floor, simulating the weightbearing position and allowing for an evaluation of the fusion sagittal angle of the first MTPJ. The coronal plane’s alignment was also verified. The target sagittal alignment was achieved when the soft tissue of the plantar surface at the distal-most aspect of the proximal phalanx was measured (using a sterile ruler) as 1 cm off the artificial floor. The recommended fusion sagittal angle falls within a range of 10°, which allows for 1-mm to 2-mm variations in measuring the elevation of the proximal phalanx off the artificial floor. In these patients, fixation was achieved with two 2.8-mm threaded, double-pointed Steinmann pins placed through the intramedullary canal of the proximal and distal phalanges and into the first metatarsal. Once fixation was achieved, the fusion sagittal angle and coronal plane angle were again confirmed with the AFT without using fluoroscopy.
Fig. 4.
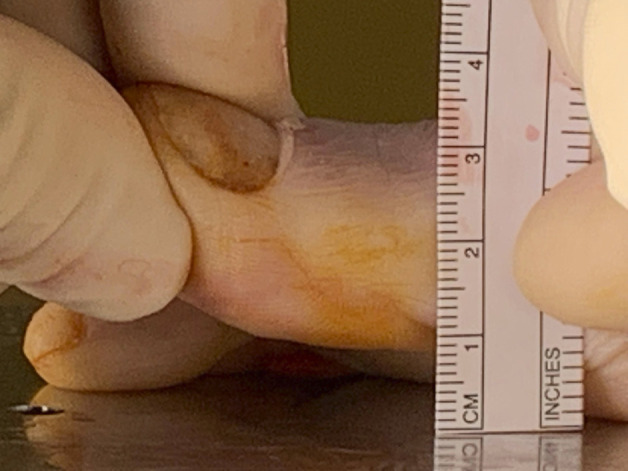
The artificial floor technique is shown in this photograph. Before fixation, the plantar surface of the foot is placed flat against the artificial floor and the first MTPJ is dorsiflexed until the plantar surface of the proximal phalanx is approximately 1 cm off the artificial floor.
Ethical Approval
Ethical approval was obtained for the current study.
Statistical Analysis
Our primary study goal evaluated whether the AFT is a valid and repeatable technique for positioning the fusion sagittal angle between 20° and 30° of dorsiflexion from the first metatarsal. To address this, two independent observers (JTS, ASR) each measured the fusion sagittal angle as previously described. The reported mean fusion sagittal angles and SDs were calculated and a pairwise comparison was performed between each reviewer’s sets of measurements. Intraobserver and interobserver reliabilities between the two reviewers were ascertained using intraclass correlation coefficients (ICCs). We chose a two-way random-effects model, where both people-effects and measures-effects are random with absolute agreement. Our secondary research goal evaluated whether the fusion sagittal angle obtained using the AFT varies with foot size. To address this, we used a multiple linear regression model to determine whether the lengths of the foot, first metatarsal, and proximal phalanx significantly affected the fusion sagittal angle. A by-sex analysis was deferred in this study because bone size, and therefore foot size, is determined by the size of the patient, not the sex of the patient [15]. For all analyses, bilateral cases were included because all procedures were performed as separate operations (that is, there are zero bilateral cases in this dataset) at least 3 months apart from each other, and the fusion sagittal angles that resulted from each procedure were measured independently of each other on two separate occasions by two separate individuals (JTS, ASR). For all tests, significance was defined as p < 0.05 (IBM SPSS, IBM Corp).
Results
Is the AFT a Valid and Repeatable Technique for Positioning the Fusion Sagittal Angle Between 20° and 30° of Dorsiflexion During First MTPJ Arthrodesis?
The AFT accurately and reproducibly positions the first MTPJ between 20° and 30°. The mean fusion sagittal angle using the AFT for the entire cohort was 27° ± 4° (Table 1). The mean fusion sagittal angle for reviewer one (JTS) was 26° ± 5° with a mean difference of 0.95° (95% confidence interval [CI] 0.70 to 1.21; p < 0.001) between the pair of measurements. The mean fusion sagittal angle for reviewer two (ASR) was 28° ± 5° with a mean difference of 0.66° (95% CI 0.28 to 1.03; p = 0.001) between the pair of measurements. The interobserver ICC of the fusion sagittal angle measurements was 0.92 (95% CI 0.56 to 0.97; p < 0.001) (Table 2). The intraobserver ICC for reviewer one (JTS) was 0.95 (95% CI 0.92 to 0.97; p < 0.001) and the intraobserver ICC for reviewer two (ASR) was 0.97 (95% CI 0.88 to 0.98; p < 0.001). Ninety-one percent (103 of 113) of the study group fell within the acceptable range of 20° to 30° ± 2°. All fusions achieved union.
Table 2.
Inter- and intraobserver reliabilities
| Outcome | Value (95% CI) | p value |
| Interobserver ICC | 0.92 (0.56-0.97) | < 0.001 |
| Intraobserver ICC, reviewer 1 | 0.95 (0.92-0.97) | < 0.001 |
| Intraobserver ICC, reviewer 2 | 0.97 (0.88-0.98) | < 0.001 |
Does Fusion Sagittal Angle Obtained Using the AFT Vary with Foot Size?
The fusion sagittal angle obtained using the AFT does not vary with foot size. Our multiple linear regression analysis (Table 3) demonstrated that the preoperative lengths of the whole foot (β = -0.05 [95% CI -0.12 to 0.02]; p = 0.16), proximal phalanx (β = -0.13 [95% CI -0.46 to 0.20]; p = 0.44), and first metatarsal (β = 0.13 [95% CI -0.10 to 0.35]; p = 0.27) were not independently associated with the postoperative fusion sagittal angle.
Table 3.
Results from a multiple regression model assessing the effect of whole foot, proximal phalanx, and first metatarsal length on the fusion sagittal angle
| Parameter | Correlation coefficient β (95% CI) | p value |
| Intercept | 35 (26 to 45) | < 0.001 |
| Whole foota | -0.05 (-0.12 to 0.02) | 0.16 |
| Proximal phalanxa | -0.13 (-0.46 to 0.20) | 0.44 |
| First metatarsala | 0.13 (-0.10 to 0.35) | 0.27 |
Lengths measured on preoperative AP and lateral weightbearing radiographs.
Discussion
Arthrodesis of the first MTPJ is a common procedure with a broad set of indications. Regardless of which surgical technique is used, it is important to obtain dorsiflexion of the first MTPJ in the sagittal plane between 20° and 30°, which corresponds to 10° to 15° of dorsiflexion off the weightbearing axis [7, 8, 13, 14, 16, 17]. An angle greater than 30° has been associated with increased pressure on the metatarsal head [2] and a fusion sagittal angle less than 20° impairs gait, causing excessive external rotation during toe-off [18]. However, achieving appropriate sagittal alignment intraoperatively is challenging. The AFT has been previously described and is commonly used, but it has never been validated in a large cohort of patients undergoing first MTPJ arthrodesis.
Limitations
There are several limitations to the current study. First, this study did not have a comparison group. The AFT was not compared with other techniques for achieving the fusion sagittal angle because we had the advantage of measuring the actual fusion sagittal angle on postoperative radiographs. Our results revealed that the fusion sagittal angles were replicable and within the ideal range of 20° to 30°. Second, the study did not attempt to correlate radiographic outcomes with clinical patient-reported outcomes. The intent was only to validate the AFT for achieving a fusion sagittal angle of between 20° and 30°, without the use of intraoperative fluoroscopy. Third, subjectivity exists when assessing the height of the proximal phalanx off the surface of the artificial floor intraoperatively. Although the soft tissue of the plantar surface at the distal-most aspect of the proximal phalanx should measure 1 cm off the artificial floor, in practice, deviations of 1-mm to 2-mm when measuring this elevation are acceptable because the recommended fusion sagittal angle falls within 10°. Fourth, the two independent physician reviewers who conducted the measurements on postoperative radiographs were not fellowship-trained foot and ankle orthopaedic surgeons. Nonetheless, the measurement of the fusion sagittal angle was conducted using established methods [21] that achieved excellent interobserver and intraobserver reliability. Fifth, a by-sex analysis was not conducted because bone size, and therefore foot size, is determined by patient size, not patient sex. An anatomical study of age- and height-matched male and female distal femora demonstrated considerable variability between male and female specimens and a high amount of overlap between sexes [15]. In addition, our regression analysis demonstrated that the size of the foot and the size of the first ray did not correlate with the fusion sagittal angle.
Discussion of Key Findings
Our study confirms that the AFT achieves sagittal plane alignment of the first MTPJ within the acceptable range of 20° to 30° without the use of costly implants or fluoroscopy. The mean fusion sagittal angle, as determined by two independent reviewers, was 27°. Further, the interobserver reliability ICC between the reviewers was 0.92 (95% CI 0.56 to 0.97]; p < 0.001) and the intraobserver ICC for each reviewer was 0.95 (95% CI 0.92 to 0.97; p < 0.001) and 0.97 (95% CI 0.88 to 0.98; p < 0.001). These indicate excellent interobserver and intraobserver reliabilities [23]. In addition, we found that 91% (103 of 113) of our patients treated using the AFT healed their fusions with sagittal angles within the range of 20° to 30° ± 2°. Finally, the fusion sagittal angle using the AFT was not affected by the size of the patient’s foot.
The results of our study are similar to other previously published studies. A technique similar to the AFT was described [13] for first MTPJ arthrodesis using a low-profile contoured titanium plate. The fusion sagittal angle in this study ranged between 20° and 25°. However, their cohort only included 12 patients. Womack and Ishikawa [28] also used a rigid surface to determine alignment in first MTPJ arthrodesis but failed to validate the results radiographically. Using radiographic measurements in 113 first MTPJ arthrodeses, our study demonstrated that the AFT is a reliable and valid technique for determining proper sagittal alignment and that it is not affected by foot size. Regardless of whether intraoperative fluoroscopy is used, it is expeditious to use a validated technique to determine the sagittal angle before fixation. The AFT is an effective method for achieving the alignment within the desired range of 20° to 30°. Additionally, this technique can be performed without fluoroscopy and so avoids radiation exposure to the patient and surgical team.
Although it uses inexpensive and readily available equipment, the AFT produces sagittal alignment results that are comparable to those of other studies using intraoperative fluoroscopy or precontoured plates [16, 19]. A retrospective study of 128 patients undergoing first MTPJ arthrodesis with either a precontoured dorsal plate or a noncontoured dorsal plate with intraoperative fluoroscopy reported a mean fusion sagittal angle of 24.2° (range 6° to 43.7°) for the noncontoured plate group [19]. The precontoured plate group had a mean fusion sagittal angle of 26° (range 14.3° to 46.1°). Goucher and Coughlin [16] conducted a prospective study of 50 patients (54 feet) undergoing first MTPJ arthrodesis using intraoperative fluoroscopy. In all 54 feet, final fixation was achieved using a dorsal titanium plate with preset valgus of 10° and dorsiflexion of 10°. The authors reported a mean fusion sagittal angle of 24°. As these results are comparable to our own, the AFT may eliminate the need for costly and bulky precontoured surgical implants and can be utilized regardless of fixation construct. Although our study validated the technique using a large cohort of patients by a single surgeon, future studies should confirm the reliability and reproducibility of the AFT when adopted by surgeons on a larger scale.
Conclusion
The AFT allows for accurate and reproducible positioning of the first MTPJ within the appropriate functional range of dorsiflexion, regardless of foot size. Additionally, this technique can be performed without fluoroscopy and so avoids radiation exposure to the patient and the surgical team.
Acknowledgment
We thank Kathleen Donahey Marcus for her editorial assistance with this manuscript.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from Case Western Reserve University Hospitals, Cleveland, OH, USA (number STUDY20190865).
Contributor Information
Alexander S. Rascoe, Email: asrascoe@gmail.com.
Randall E. Marcus, Email: randall.marcus@uhhospitals.org.
References
- 1.Baumgartner R, Libuit K, Ren D, et al. Reduction of radiation exposure from C-arm fluoroscopy during orthopaedic trauma operations with introduction of real-time dosimetry. J Orthop Trauma. 2016;30:e53-e58. [DOI] [PubMed] [Google Scholar]
- 2.Bayomy AFB, Aubin PMM, Sangeorzan BJ, Ledoux WR. Arthrodesis of the first metatarsophalangeal joint: a robotic cadaver study of the dorsiflexion angle. J Bone Joint Surg Am. 2010;92:1754-1764. [DOI] [PubMed] [Google Scholar]
- 3.Beebe MJ, Jenkins P, Rothberg DL, Kubiak EN, Higgins TF. Prospective assessment of the oncogenic risk to patients from fluoroscopy during trauma surgery. J Orthop Trauma. 2016;30:e223-e229. [DOI] [PubMed] [Google Scholar]
- 4.Bennett GL, Sabetta J. First metatarsalphalangeal joint arthrodesis: evaluation of plate and screw fixation. Foot Ankle Int. 2009;30:752-757. [DOI] [PubMed] [Google Scholar]
- 5.Coughlin M, Shurnas P. Hallux rigidus: grading and long-term results of operative treatment. J Bone Joint Surg Am . 2003;85:2072-2088. [PubMed] [Google Scholar]
- 6.Coughlin MJ. Arthrodesis of the first metatarsophalangeal joint. Orthop Rev. 1990;19:177-186. [PubMed] [Google Scholar]
- 7.Coughlin MJ. Rheumatoid forefoot reconstruction. J Bone Joint Surg Am. 2000;82:20. [PubMed] [Google Scholar]
- 8.Coughlin MJ, Grebing BR, Jones CP. Arthrodesis of the first metatarsophalangeal joint for idiopathic hallux valgus: intermediate results. Foot Ankle Int. 2005;26:783-792. [DOI] [PubMed] [Google Scholar]
- 9.Coughlin MJ, Shurnas PS. Hallux rigidus: surgical techniques (cheilectomy and arthrodesis). J Bone Joint Surg Am. 2004;86-A(suppl 1, pt 2):119-130. [DOI] [PubMed] [Google Scholar]
- 10.DeOrio JK. Technique tip: arthrodesis of the first metatarsophalangeal joint–prevention of excessive dorsiflexion. Foot Ankle Int. 2007;28:746-747. [DOI] [PubMed] [Google Scholar]
- 11.Doty J, Coughlin M, Hirose C, Kemp T. Hallux metatarsophalangeal joint arthrodesis with a hybrid locking plate and a plantar neutralization screw: a prospective study. Foot Ankle Int. 2013;34:1535-1540. [DOI] [PubMed] [Google Scholar]
- 12.Ettl V, Radke S, Gaertner M, Walther M. Arthrodesis in the treatment of hallux rigidus. Int Orthop. 2003;27:382-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flavin R, Stephens MM. Arthrodesis of the first metatarsophalangeal joint using a dorsal titanium contoured plate. Foot Ankle Int. 2004;25:783-787. [DOI] [PubMed] [Google Scholar]
- 14.Gibson JNA, Thomson CE. Arthrodesis or total replacement arthroplasty for hallux rigidus: a randomized controlled trial. Foot Ankle Int. 2005;26:680-690. [DOI] [PubMed] [Google Scholar]
- 15.Gillespie RJ, Levine A, Fitzgerald SJ, et al. Gender differences in the anatomy of the distal femur. J Bone Joint Surg Br. 2011;93:357-363. [DOI] [PubMed] [Google Scholar]
- 16.Goucher NR, Coughlin MJ. Hallux metatarsophalangeal joint arthrodesis using dome-shaped reamers and dorsal plate fixation: a prospective study. Foot Ankle Int. 2006;27:869-876. [DOI] [PubMed] [Google Scholar]
- 17.Lewis JT, Hanselman AE, Lalli TAJ, Daigre JL, Santrock RD. Effect of dorsal plate positioning on dorsiflexion angle in arthrodesis of the first metatarsophalangeal joint: a cadaveric study. Foot Ankle Int. 2014;35:802-808. [DOI] [PubMed] [Google Scholar]
- 18.Mann RA, Coughlin MJ. Biomechanics of the foot and ankle. Surgery of the Foot and Ankle. Mosby; 1993:43. [Google Scholar]
- 19.Mayer SA, Zelenski NA, DeOrio JK, Easley ME, Nunley JA. A comparison of nonlocking semitubular plates and precontoured locking plates for first metatarsophalangeal joint arthrodesis. Foot Ankle Int. 2014;35:438-444. [DOI] [PubMed] [Google Scholar]
- 20.Migues A, Calvi J, Sotelano P, Carrasco M, Slullitel G, Conti L. Endomedullary screw fixation for first metatarsophalangeal arthrodesis. Foot Ankle Int. 2013;34:1152-1157. [DOI] [PubMed] [Google Scholar]
- 21.Nawoczenski DA, Baumhauer JF, Umberger BR. Relationship between clinical measurements and motion of the first metatarsophalangeal joint during gait. J Bone Joint Surg Am . 1999;81:370-376. [DOI] [PubMed] [Google Scholar]
- 22.Patra SK, Shetty AP, Jayaramaraju D, Rajasekaran S. Radiation exposure to the surgeon, surgical assistant, and scrub nurse during closed intramedullary nailing of long bones-does it vary depending on the experience of the surgeon? J Orthop Trauma. 2019;33:e52-e57. [DOI] [PubMed] [Google Scholar]
- 23.Portney L, Watkins M. Foundations of Clinical Research: Applications To Practice. 2nd ed. Prentice Hall Health; 2000. [Google Scholar]
- 24.Rongstad KM, Miller GJ, Griend RAV, Cowin D. A biomechanical comparison of four fixation methods of first metatarsophalangeal joint arthrodesis. Foot Ankle Int. 1994;15:415-419. [DOI] [PubMed] [Google Scholar]
- 25.Sammarco GJ, Idusuyi OB. Complications after surgery of the hallux. Clin Orthop Relat Res . 2001;391:59-71. [DOI] [PubMed] [Google Scholar]
- 26.Shereff MJ, Baumhauer JF. Current concepts review - hallux rigidus and osteoarthrosis of the first metatarsophalangeal joint. J Bone Joint Surg Am. 1998;80:898-908. [DOI] [PubMed] [Google Scholar]
- 27.Smith RW, Joanis TL, Maxwell PD. Great toe metatarsophalangeal joint arthrodesis: a user-friendly technique. Foot Ankle. 1992;13:367-377. [DOI] [PubMed] [Google Scholar]
- 28.Womack JW, Ishikawa SN. First metatarsophalangeal arthrodesis. Foot Ankle Clin. 2009;14:43-50. [DOI] [PubMed] [Google Scholar]





