Abstract
Background
Joint arthroplasty registries traditionally report survivorship outcomes mainly on primary joint arthroplasty. The outcome of first revision procedures is less commonly reported, because large numbers of primary procedures are required to analyze a sufficient number of first revision procedures. Additionally, adequate linkage of primary procedures to revisions and mortality is required. When undertaking revision hip surgery, it is important for surgeons to understand the outcomes of these procedures to better inform patients.
Questions/purposes
Using data from a large national joint registry, we asked: (1) What is the overall rate of revision of the first aseptic revision procedure for a primary THA? (2) Does the rate of revision of the first revision vary by the diagnosis for the first revision? (3) What is the mortality after the first revision, and does it vary by the reason for first revision?
Methods
The Australian Orthopaedic Association National Joint Replacement Registry longitudinally maintains data on all primary and revision joint arthroplasties, with nearly 100% capture. The analyses for this study were performed on primary THA procedures in patients with a diagnosis of osteoarthritis up to December 31, 2020, who had undergone subsequent revision. We excluded all primary THAs involving metal-on-metal and ceramic-on-metal bearing surfaces and prostheses with exchangeable necks because these designs may have particular issues associated with revisions, such as extensive soft tissue destruction, that are not seen with conventional bearings, making a comparative analysis of the first revision involving these bearing surfaces more complicated. Metal-on-metal bearing surfaces have not been used in Australia since 2017. We identified 17,046 first revision procedures from the above study population and after exclusions, included 13,713 first revision procedures in the analyses. The mean age at the first revision was 71 ± 11 years, and 55% (7496 of 13,713) of the patients were women. The median (IQR) time from the primary procedure to the first revision was 3 years (0.3 to 7.3), ranging from 0.8 years for the diagnosis of dislocation and instability to 10 years for osteolysis. There was some variation depending on the reason for the first revision. For example, patients undergoing revision for fracture were slightly older (mean age 76 ± 11 years) and patients undergoing revision for dislocation were more likely to be women (61% [2213 of 3620]). The registry has endeavored to standardize the sequence of revisions and uses a numerical approach to describe revision procedures. The first revision is the revision of a primary procedure, the second revision is the revision of the first revision, and so on. We therefore described the outcome of the first revision as the cumulative percent second revision. The outcome measure was the cumulative percent revision, which was defined using Kaplan-Meier estimates of survivorship to describe the time to the second revision. Hazard ratios from Cox proportional hazards models, adjusting for age and gender, were performed to compare the revision rates among groups. When possible, the cumulative percent second revision at the longest follow-up timepoint was determined with the available data, and when there were insufficient numbers, we used appropriate earlier time periods.
Results
The cumulative percent second revision at 18 years was 26% (95% confidence interval [CI] 24% to 28%). When comparing the outcome of the first revision by reason, prosthesis dislocation or instability had the highest rate of second revision compared with the other reasons for first revision. Dual‐mobility prostheses had a lower rate of second revision for dislocation or instability than head sizes 32 mm or smaller and when compared to constrained prostheses after 3 months. There was no difference between dual-mobility prostheses and head sizes larger than 32 mm. There were no differences in the rate of second revision when first revisions for loosening, periprosthetic fracture, and osteolysis were compared. If cemented femoral fixation was performed at the time of the first revision, there was a higher cumulative percent second revision for loosening than cementless fixation from 6 months to 6 years, and after this time, there was no difference. The overall mortality after a first revision of primary conventional THA was 1% at 30 days, 2% at 90 days, 5% at 1 year, and 40% at 10 years. A first revision for periprosthetic fracture had the highest mortality at all timepoints compared with other reasons for the first revision.
Conclusion
Larger head sizes and dual-mobility cups may help reduce further revisions for dislocation, and the use of cementless stems for a first revision for loosening seems advantageous. Surgeons may counsel patients about the higher risk of death after first revision procedures, particularly if the first revision is performed for periprosthetic fracture.
Level of Evidence Level III, therapeutic study.
Introduction
THA is an excellent procedure for severe, symptomatic hip arthritis, and outcomes have been well documented at a national level by multiple joint replacement registries in different countries [1, 9, 16, 17, 23]. However, joint registries traditionally report survivorship outcomes mainly on primary joint arthroplasty and analyze these data by adjusting for patient, prosthesis, and process variables. The outcome of the first revision procedures is less commonly reported. There are several reasons for this. Large numbers of primary procedures are required to analyze a sufficient number of first revision procedures. Additionally, adequate linkage of primary procedures to revisions and mortality is needed. It is important to have a chronological history of revision procedures that are linked to a known primary procedure because there are differences in the outcomes of primary THA based on patient diagnosis at the time of the original procedure [1, 19]. The terminology used for the outcome of these first revision procedures can also be confusing, with presentations and publications using the term “re-revision.” With multiple revisions, the chronology again becomes difficult if the term re-revision is used for each subsequent revision. There is an increasing incidence of revision THA [21], and therefore, it is important to examine factors associated with the outcomes of these procedures to provide surgeons with appropriate information to advise patients.
Using data from the Australian Orthopaedic Association National Joint Replacement Registry, we sought to answer several questions regarding the outcome of the first revision procedure for THA: (1) What is the overall rate of revision of the first aseptic revision procedure for a primary THA? (2) Does the rate of revision of the first revision vary by the diagnosis for the first revision? (3) What is the mortality after the first revision, and does it vary by the reason for first revision?
Patients and Methods
Study Design and Setting
This was a retrospective, comparative study drawn from a large, longitudinally maintained, national registry.
The Australian Orthopaedic Association National Joint Replacement Registry began data collection on September 1, 1999, with complete nationwide data collection commencing in 2002 for almost 100% of the arthroplasty procedures performed in Australia. Registry data are validated against data provided by state and territory health departments in Australia with the use of a sequential multilevel matching process. A matching program is run monthly to search for all primary and revision arthroplasty procedures recorded in the registry that involve the same side and joint of the same patient, thus enabling each revision to be linked to the primary procedure. Data are also matched biannually with the Australian Government Department of Health National Death Index to obtain information on the date of death. The registry cannot account for revision procedures performed on Australian emigrants, but for the population likely to undergo revision THA, this number is extremely small, and we believe it is unlikely to alter our results. The registry defines revisions as reoperations of previous hip arthroplasties in which one or more of the prosthetic components is replaced or removed, or one or more components is added. The registry does not record reoperations in which a component was not added or removed. Major revisions are recorded when a component in contact with bone is exchanged, and minor revisions are defined as removal and addition of a femoral head or acetabular insert.
Study Population
The analyses were performed on primary THA procedures in patients with a diagnosis of osteoarthritis up to December 3, 2020, who had undergone subsequent revision for reasons other than infection. We identified 17,046 first revision procedures from the above study population, and after the exclusion criteria were applied, 13,713 first revision procedures were analyzed (Fig. 1).
Fig. 1.
This flowchart shows the inclusion and exclusion process for the study population.
Exclusions From Primary THA Population
We excluded all primary THA procedures involving metal-on-metal and ceramic-on-metal bearing surfaces and prostheses with exchangeable necks. These bearing surfaces may have major issues associated with revisions such as extensive soft tissue destruction that are not seen with conventional bearings, making a comparative analysis of the first revision more complicated [5, 13]. Metal-on-metal metal bearing surfaces have not been used in Australia since 2017. Prostheses with exchangeable necks are also seldom used and have an additional revision option (isolated head and neck exchange), and the reasons for revision vary from those of conventional THA [7].
Exclusions From First Revision Procedures
Because of the complexities involved in the analysis of revisions for sepsis, first revision procedures undertaken for infection were excluded from all analyses but were included in subsequent analyses of further revisions.
Demographics
The mean age at the first revision was 71 ± 11 years, and 55% (7496 of 13,713) of patients were women (Table 1). The median (IQR) time from the primary procedure to the first revision was 3 years (0.3 to 7.3), ranging from 0.8 years for dislocation or instability to 10 years for osteolysis. There was some variation depending on the reason for the first revision. For example, patients undergoing revision for fracture were slightly older (76 ± 11 years) than for other diagnoses, and patients undergoing revision for dislocation were more likely to be women (61% [2213 of 3620]) than men. There were 4018 patients who underwent revision for loosening, 3620 undergoing revision for dislocation or instability, 3675 undergoing revision for periprosthetic fracture, 364 for osteolysis, and 2036 for other reasons, which we did not analyze separately (Table 1).
Table 1.
Summary of first revisions of known total conventional hip replacement (primary diagnosis osteoarthritis)
| Parameter | Loosening (n = 4018) | Prosthesis dislocation or instability (n = 3620) | Fracture (n = 3675) | Osteolysis (n = 364) | Other (n = 2036) | Total (n = 13,713) |
| Follow-up in years, primary to first revision | 4 (1.1-8.2) | 0.8 (0.1-3.9) | 3 (0.1-7.8) | 10 (6.9-13.3) | 3 (0.9-7) | 3 (0.3-7.3) |
| Follow-up in years, first revision to second revision | 4.3 (1.8- 8) | 3.9 (1.6, 7.6) | 3 (1.1- 5.9) | 4.6 (1.8, 7.5) | 4.1 (1.6- 7.4) | 3.8 (1.5-7.2) |
| Age at first revision in years | 70 ± 11 | 71 ± 11 | 76 ± 11 | 71 ± 10 | 66 ± 11 | 71 ± 11 |
| Age at first revision in years by group | ||||||
| < 55 | 8 (320) | 8 (277) | 3 (127) | 6 (21) | 16 (320) | 8 (1065) |
| 55-64 | 19 (771) | 17 (599) | 11 (390) | 16 (57) | 27 (555) | 17 (2372) |
| 65-74 | 35 (1409) | 33 (1179) | 25 (937) | 37 (135) | 35 (704) | 32 (4364) |
| ≥ 75 | 38 (1518) | 43 (1565) | 60 (2221) | 41 (151) | 22 (457) | 43 (5912) |
| Women | 51 (2055) | 61 (2213) | 53 (1951) | 52 (190) | 53 (1087) | 55 (7496) |
| ASA class at first revisiona | ||||||
| ASA 1 | 7 (154) | 4 (89) | 3 (73) | 6 (15) | 10 (130) | 5 (461) |
| ASA 2 | 47 (1089) | 42 (847) | 27 (688) | 46 (113) | 50 (682) | 40 (3419) |
| ASA 3 | 43 (996) | 51 (1027) | 57 (1445) | 46 (111) | 37 (503) | 48 (4082) |
| ASA 4 | 4 (88) | 4 (72) | 340 (13.3) | 2 (5) | 3 (44) | 6 (549) |
| ASA 5 | 0 (1) | 7 (0.3) | 0.1 (8) | |||
| BMI in kg/m2 at first revisionb | ||||||
| Underweight: < 18.5 | 0.7 (12) | 1.2 (18) | 2 (35) | 0.8 (8) | 1 (73) | |
| Normal: 18.5-24.9 | 19 (322) | 21 (309) | 30 (459) | 23 (42) | 17 (173) | 22 (1305) |
| Pre-obese: 25.0-29.9 | 37 (636) | 37 (549) | 34 (531) | 38 (70) | 39 (405) | 37 (2191) |
| Obese class 1: 30.0-34.9 | 27 (454) | 25 (369) | 20 (312) | 28 (52) | 25 (265) | 24 (1452) |
| Obese class 2: 35.0-39.9 | 11 (186) | 11 (157) | 8 (126) | 9 (17) | 13 (138) | 11 (624) |
| Obese class 3: ≥ 40.0 | 6 (94) | 5 (80) | 5 (79) | 2 (4) | 5 (53) | 5 (310) |
| Fixation of primary procedure | ||||||
| Cemented | 16 (662) | 8 (274) | 6 (224) | 6 (22) | 3 (54) | 9 (1236) |
| Cementless | 60 (2414) | 57 (2070) | 65 (2395) | 64 (233) | 77 (1562) | 63 (8674) |
| Hybrid | 23 (942) | 35 (1276) | 29 (1056) | 30 (109) | 21 (420) | 28 (3803) |
| Femoral fixation in first revision | ||||||
| Femoral cemented | 24 (959) | 8 (290) | 22 (798) | 14 (51) | 13 (260) | 17 (2358) |
| Femoral cementless | 36 (1452) | 6 (214) | 64 (2351) | 18 (65) | 20 (404) | 33 (4486) |
| No femoral component inserted in first revision | 40 (1607) | 86 (3116) | 14 (526) | 68 (248) | 67 (1372) | 50 (6869) |
| Acetabular fixation in first revision | ||||||
| Acetabular cemented | 9 (379) | 6 (231) | 3 (123) | 8 (30) | 4 (85) | 6 (848) |
| Acetabular cementless | 39 (1570) | 34 (1246) | 8 (297) | 44 (160) | 35 (710) | 29 (3983) |
| No acetabular component inserted in first revision | 51 (2069) | 59 (2143) | 89 (3255) | 48 (174) | 61 (1241) | 65 (8882) |
| Type of acetabular prosthesis in first revisionc | ||||||
| Constrained prosthesis | 3 (136) | 28 (965) | 3 (86) | 3 (12) | 2 (39) | 9 (1238) |
| Dual mobility prosthesis | 7 (287) | 17 (592) | 6 (217) | 8 (29) | 8 (166) | 10 (1291) |
| > 32 mm | 43 (1662) | 27 (940) | 39 (1295) | 34 (120) | 46 (918) | 38 (4935) |
| 32 mm | 33 (1268) | 19 (691) | 33 (1115) | 43 (155) | 32 (645) | 30 (3874) |
| < 32 mm | 14 (544) | 9 (326) | 19 (631) | 12 (42) | 11 (222) | 13 (1765) |
| Bearing surface of primary | ||||||
| Ceramic/ceramic | 21 (849) | 15 (549) | 24 (890) | 11 (39) | 41 (827) | 23 (3154) |
| Ceramic/non-XLPE | 5 (182) | 3 (105) | 3 (103) | 13 (49) | 3 (69) | 4 (508) |
| Ceramic/XLPE | 14 (557) | 17 (614) | 17 (611) | 5 (20) | 16 (324) | 16 (2126) |
| Metal/non-XLPE | 27 (1098) | 16 (566) | 11 (413) | 51 (185) | 11 (217) | 18 (2479) |
| Metal/XLPE | 29 (1182) | 43 (1553) | 40 (1466) | 14 (50) | 24 (497) | 35 (4748) |
| Ceramicized metal/non-XLPE | 0.4 (18) | 0.2 (9) | 0.1 (2) | 3 (10) | 0.5 (11) | 0.4 (50) |
| Ceramicized metal/XLPE | 3 (130) | 6 (222) | 5 (185) | 3 (10) | 4 (89) | 5 (636) |
| Unknown | 0 (2) | 0.1 (2) | 0.1 (5) | 0.3 (1) | 0.1 (2) | 0.1 (12) |
| Bearing surface of first revisiond | ||||||
| Ceramic/ceramic | 6 (161) | 2 (76) | 5 (49) | 5 (16) | 18 (251) | 7 (553) |
| Ceramic/non-XLPE | 2 (51) | 3 (97) | 3 (28) | 2 (7) | 3 (37) | 3 (220) |
| Ceramic/XLPE | 19 (512) | 15 (454) | 17 (163) | 20 (68) | 31 (437) | 19 (1634) |
| Metal/non-XLPE | 12 (327) | 27 (842) | 13 (132) | 8 (27) | 5 (73) | 16 (1401) |
| Metal/XLPE | 54 (1431) | 45 (1386) | 57 (565) | 54 (186) | 37 (529) | 48 (4097) |
| Ceramicized metal/non XLPE | 0.2 (4) | 1 (44) | 0.5 (5) | 0.6 (2) | 0.3 (4) | 0.7 (59) |
| Ceramicized metal/XLPE | 6 (155) | 6 (178) | 4 (41) | 10 (34) | 6 (88) | 6 (496) |
| Other bearing surface | 0.9 (25) | 1 (32) | 0.2 (2) | 2 (6) | 0.7 (10) | 0.9 (75) |
Data are presented as the median (IQR), mean ± SD, or % (n). Other bearing surface of first revision includes 59 metal-on-metal, 14 ceramic-on-metal, and two ceramicized metal-on-XLPE. The % is expressed when we have all known values; thus, there are some discrepancies with the actual totals (denominator).
Excludes 5194 procedures with unknown ASA class at first revision.
Excludes 7758 procedures with unknown BMI at first revision.
Excludes 610 procedures with unknown type of acetabular prosthesis in the first revision.
Excludes 5178 procedures with unknown bearing surface of first revision; ASA = American Society of Anesthesiologists; XLPE = crosslinked polyethylene.
When an acetabular cup or femoral stem was revised at the first revision, cementless fixation was more likely to be used. The most common head size used in the first revision was larger than 32 mm (38% [4935 of 13,103]), and the most common bearing surface was metal-on-crosslinked polyethylene (48% [4097 of 8535]), followed by ceramic-on-crosslinked polyethylene (19% [1634 of 8535]). Although primary conventional THA with metal-on-metal bearing surfaces were excluded from the analysis, there were 75 procedures in which metal-on-metal or ceramic-on-metal bearings were used in the first revision.
Terminology
The registry has endeavored to standardize the sequence of revisions and uses a numerical approach to describe revision procedures (Fig. 2). The first revision is the revision of a primary procedure. The second revision is the revision of the first revision, and so on. Nonspecific terminology such as re-revision is avoided. This numerical sequence becomes increasingly important because registries have longer follow-up of known primary procedures that have multiple revisions. We therefore describe the outcome of the first revision as the cumulative percent second revision. We believe the sequential numeric terminology proposed for describing the chronology of revision procedures offers advantages over the term “re-revision” because it is unambiguous and lists, in order, the sequence of revision procedures and their subsequent outcomes. With the increasing maturity of joint registries, the pathway from the primary procedure can be clearly outlined using this terminology. We hope that the description in this article may be adopted by the international arthroplasty community for clarity and to allow comparative studies.
Fig. 2.
This flowchart shows the terminology for revision procedures.
Primary and Secondary Study Outcomes
The primary study goal was to determine the overall rate of revision of the first revision procedure, and the outcome measure for the analysis was time to the second revision, adjusted for age and gender using Kaplan-Meier estimates of survivorship.
We had two secondary study goals. The first was to determine the outcomes for each of the most common reasons for the first revision. These included prosthesis loosening, dislocation or instability, and periprosthetic fracture. The outcome measure for the analysis was time to the second revision, adjusted for age and gender using Kaplan-Meier estimates of survivorship. The reason for these analyses was to provide information on the comparative performance of the different approaches to the first revision for each of the different reasons for first revision. For first revisions for loosening, we also compared the effect of cementless femoral fixation with that of cemented fixation. For first revisions for dislocation or instability, we adjusted for the effect of femoral head size and constrained and dual-mobility prostheses used at the time of the first revision. Femoral heads smaller than 32 mm were used in 9% (326 of 3514) of procedures, 32 mm in 20% (691 of 3514), larger than 32 mm in 27% (940 of 3514), constrained liners in 27% (965 of 3514), and dual-mobility in 17% (592 of 3514) of procedures. The outcome of first revision for osteolysis is also reported; however, this is largely confined to prostheses with longer follow-up and non-crosslinked polyethylene bearing surfaces.
The second secondary study goal was to determine the mortality of the first revision and to examine whether there were differences by the reason for first revision. The outcome measure for this analysis was time to death, adjusted for age and gender. For a subanalysis on this point, we stratified the rate of revision by American Society of Anesthesiologists (ASA) class and BMI. The number of first revision procedures available for analysis was reduced to 8519 and 5955 procedures for ASA and BMI, respectively, because these data were not available for all first revision procedures.
Ethical Approval
We obtained ethical review board approval for this study.
Statistical Analysis
We used the cumulative percent revision, defined as the complement of the Kaplan-Meier estimates of survivorship, to describe the rate of revision arthroplasty. An accompanying 95% confidence interval (CI) was calculated using unadjusted pointwise Greenwood estimates. Patients were censored at the time of death, revision, or closure of the database at the end of the study period. We used hazard ratio (HRs) from Cox proportional hazards models, adjusting for age and gender, to compare the revision rates. We used standard Kaplan-Meier estimates, not competing risk, although we acknowledge this may overestimate the risk of revision when the competing risk of death is high but the overall difference is small [4].
We checked the assumption of proportional hazards analytically for each model. If the interaction between the predictor and the log of time was statistically significant in the standard Cox model, we performed estimates using a time-varying model. We iteratively chose timepoints until the assumption of proportionality was met, and then we calculated the HRs for each selected period. All tests were two-tailed at a 5% level of significance. The analysis was performed using SAS version 9.4 (SAS Institute Inc).
The cumulative percent second revision is displayed until the number at risk reaches 40 to avoid uninformative, imprecise estimates at the right tail of the distribution, where the number at risk is low. Analytical comparisons of revision rates using the proportional hazards model are based on all available data. Where possible, the cumulative percent second revision at the longest follow-up interval was determined with the available data, and when there were insufficient numbers, we used appropriate earlier time periods as stated above.
Results
Overall Rate of Revision of the First Revision Procedure
The cumulative percent second revision at 18 years was 26% (95% CI 24% to 28%) (Fig. 3). The most common reasons for second revisions were prosthesis dislocation or instability (33% [646 of 1955]), loosening (24% [476 of 1955]), infection (23% [444 of 1955]), and periprosthetic fracture (10% [190 of 1955]). A minor revision of the femoral head, insert, or acetabular component was the most common type of second revision (25% each [485 of 1955 and 482 of 1955]), followed by revision of the femoral component (21% [420 of 1955]), THA (femoral and acetabular components) (14% [271 of 1955]), and insertion of a cement spacer (7% [137 of 1955]) (Table 2).
Fig. 3.
This graph shows the cumulative percent second revision of the first revision of known primary THA for osteoarthritis.
Table 2.
Type of second revision of known primary THA (primary diagnosis osteoarthritis)
| Type of second revision | Total (n = 1955) |
| Head insert | 25 (485) |
| Acetabular component | 25 (482) |
| Femoral component | 21 (420) |
| THA (femoral and acetabular) | 14 (271) |
| Cement spacer | 7 (137) |
| Head only | 4 (73) |
| Minor components | 2 (39) |
| Insert only | 1 (24) |
| Removal of prosthesis | 1 (22) |
| Reinsertion of components | 0.1 (1) |
| Bipolar only | 0.1 (1) |
Data are presented as % (n). This excludes first revisions where no minor or major femoral or acetabular components were inserted.
Although there was no difference in the cumulative percent second revision between men and women, men and women younger than 65 years had higher rates of second revision than patients 65 years or older after 6 months (Fig. 4).
Fig. 4.
This graph shows the cumulative percent second revision of known primary THA by gender and age (primary diagnosis osteoarthritis). A color image accompanies the online version of this article.
Similar to the outcome of primary THA, patients with ASA Class 2, 3, or 4 had a higher rate of second revision than patients with ASA Class 1. Patients with a BMI obese Class 1 or 3 had higher rates of second revision than those with normal BMI, and second revision for infection increased with increasing classes of BMI.
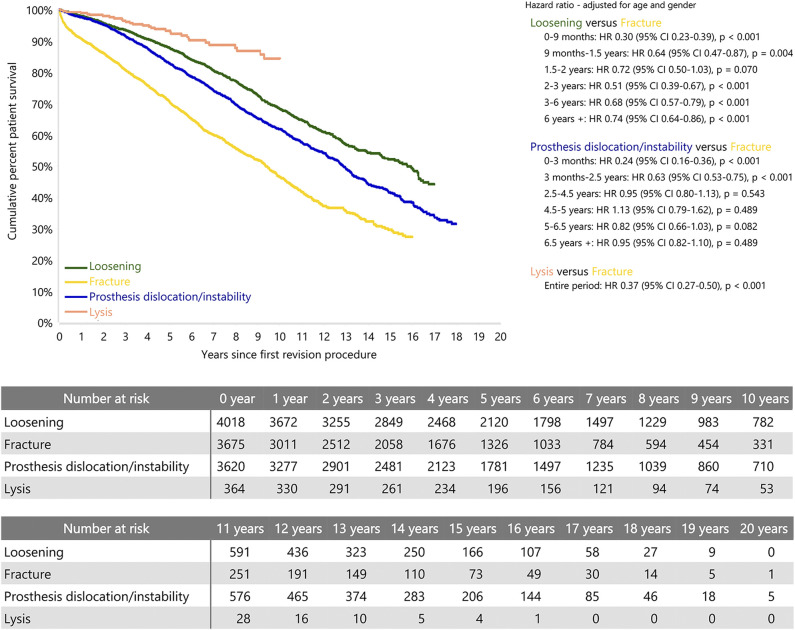
Does the Rate of Second Revision Vary by the Diagnosis of the First Revision?
First revision for prosthesis dislocation or instability had the highest rate of second revision compared with other reasons for the first revision. There were no differences in the rate of second revision when first revisions for loosening, fracture, and osteolysis were compared (Fig. 5).
Fig. 5.
This graph shows the cumulative percent second revision of known primary THA by reason for the first revision (primary diagnosis osteoarthritis). A color image accompanies the online version of this article.
Loosening
The cumulative percent second revision for the first revision for loosening at 17 years was 25% (95% CI 21% to 30%) (Table 3). The most common reason for the second revision was further loosening (34% [198 of 582]), followed by prosthesis dislocation and instability (24% [141 of 582]), infection (24% [138 of 582]), and fracture (8% [48 of 582]) (Table 4).
Table 3.
Cumulative percent second revision of known primary THA by reason for the first revision (primary diagnosis of osteoarthritis)
| Revision diagnosis | 1 year CPR (95% CI) | 2 years CPR (95% CI) | 3 years CPR (95% CI) | 4 years CPR (95% CI) | 5 years CPR (95% CI) | 6 years CPR (95% CI) | 7 years CPR (95% CI) |
| Loosening | 7 (7-8) | 10 (9-11) | 12 (11-13) | 13 (12-15) | 14 (13-15) | 15 (14-17) | 17 (15-18) |
| Fracture | 8 (7-9) | 10 (9-11) | 11 (10-12) | 11 (10-13) | 12 (11-13) | 13 (11-14) | 13 (12-15) |
| Prosthesis dislocation or instability | 10 (9-11) | 13 (12-14) | 15 (14-16) | 17 (16-18) | 18 (17-20) | 20 (18-21) | 20 (19-22) |
| Osteolysis | 7 (5-10) | 9 (7-13) | 11 (8-15) | 11 (8-16) | 11 (8-16) | 13 (10-18) | 14 (10-19) |
| Revision diagnosis | 8 years CPR (95% CI) | 9 years CPR (95% CI) | 10 years CPR (95% CI) | 11 years CPR (95% CI) | 12 years CPR (95% CI) | 13 years CPR (95% CI) |
| Loosening | 17 (16-19) | 18 (17-20) | 19 (18-21) | 20 (18-22) | 21 (19-22) | 21 (19-23) |
| Fracture | 15 (13-16) | 15 (14-17) | 16 (14-18) | 18 (15-20) | 18 (16-21) | 19 (16-22) |
| Prosthesis dislocation or instability | 21 (20-23) | 23 (21-24) | 24 (23-27) | 26 (24-29) | 28 (25-30) | 29 (27-32) |
| Osteolysis | 14 (10-19) | 14 (10-19) | 14 (10-19) |
| Revision diagnosis | 14 years CPR (95% CI) | 15 years CPR (95% CI) | 16 years CPR (95% CI) | 17 years CPR (95% CI) | 18 years CPR (95% CI) | 19 years CPR (95% CI) | 20 years CPR (95% CI) |
| Loosening | 22 (20-25) | 22 (20-25) | 24 (21-28) | 25 (21-30) | |||
| Fracture | 20 (17-23) | 21 (17-25) | |||||
| Prosthesis dislocation or instability | 30 (27-32) | 31 (28-33) | 31 (28-33) | 31 (28-35) | |||
| Osteolysis |
This excludes revisions where no minor or major femoral or acetabular components were inserted.
Table 4.
Revision diagnosis of second revision of known primary THA by reason for the first revision (primary diagnosis of osteoarthritis)
| Second revision diagnosis | Loosening (n = 582) | Prosthesis dislocation or instability (n = 670) | Fracture (n = 398) | Osteolysis (n = 43) |
| Prosthesis dislocation or instability | 24 (141) | 50 (333) | 22 (88) | 26 (11) |
| Loosening | 34 (198) | 15 (102) | 28 (112) | 26 (11) |
| Infection | 24 (138) | 20 (134) | 26 (105) | 21 (9) |
| Fracture | 8 (48) | 8 (51) | 16 (65) | 12 (5) |
| Pain | 2 (9) | 0.9 (6) | 2 (8) | 2 (1) |
| Osteolysis | 1 (7) | 0.9 (6) | 0.8 (3) | 9 (4) |
| Other | 7 (41) | 6 (38) | 5 (17) | 5 (2) |
Data are presented as % (n).
A first revision for loosening had a lower rate of second revision when both acetabular and femoral components were replaced than did other types of first revision (Fig. 6). If cemented femoral fixation was performed at the time of the first revision, there was a higher cumulative percent second revision than cementless fixation from 6 months to 6 years, and after this time, there was no difference (Fig. 7).
Fig. 6.
This graph shows the cumulative percent second revision of known primary THA by type of first revision (primary diagnosis osteoarthritis, first revision for loosening). A color image accompanies the online version of this article.
Fig. 7.
This graph shows the cumulative percent second revision of known primary THA by femoral fixation of the first revision (primary diagnosis osteoarthritis, first revision for loosening). A color image accompanies the online version of this article.
Dislocation and Instability
The cumulative percent second revision at 17 years for the first revision for dislocation or instability was 31% (95% CI 28% to 35%) (Table 3). The most common reason for the second revision was further dislocation or instability (50% [333 of 670]), followed by infection (20% [134 of 670]), loosening (15% [102 of 670]), and fracture (8% [51 of 670]) (Table 4).
Minor revisions that involved head and insert exchange were the most common type of second revision (34% [226 of 670]), followed by acetabular component only (29% [192 of 670]) and THA (13% [87 of 670]).
A minor revision involving head and insert exchange had a higher rate of second revision than acetabulum-only revision after the first month. Revision THA had a higher rate of second revision than acetabular-only revision (Fig. 8).
Fig. 8.
This graph shows the cumulative percent second revision of known primary THA by type of the first revision (primary diagnosis osteoarthritis, first revision for prosthesis dislocation or instability). A color image accompanies the online version of this article.
After adjusting for age, gender, head size, and whether a constrained or dual-mobility cup was used, we found there was no difference in the rate of overall second revision among head sizes. Constrained prostheses had a higher rate of second revision than dual-mobility prostheses after 6 months (Fig. 9). Because the most common reason for the second revision was further dislocation or instability, we examined the outcome of the first revision for dislocation or instability where the second revision diagnosis was further dislocation or instability. Dual-mobility prostheses had a lower rate of second revision for dislocation or instability than head sizes 32 mm or smaller and constrained prostheses after 3 months. There was no difference between dual-mobility prostheses and head sizes larger than 32 mm (Fig. 10).
Fig. 9.
This graph shows the cumulative percent second revision of known primary THA by prosthesis used in the first revision (primary diagnosis osteoarthritis, first revision for prosthesis dislocation or instability). A color image accompanies the online version of this article.
Fig. 10.
This graph shows the cumulative percent second revision of known primary THA by prosthesis used in the first revision (primary diagnosis osteoarthritis, first revision for prosthesis dislocation or instability, second revision for prosthesis dislocation or instability). A color image accompanies the online version of this article.
Periprosthetic Fracture
The cumulative percent second revision at 15 years for the first revision for periprosthetic fracture was 21% (95% CI 17% to 25%) (Table 3). The most common reason for the second revision was loosening (28% [112 of 398]), followed by infection (26% [105 of 398]), prosthesis dislocation or instability (22% [88 of 398]), and further fracture (16% [65 of 398]) (Table 4).
Revision of the femoral component (35% [139 of 398]) was the most common type of second revision, followed by acetabular revisions. There was no difference in the cumulative percent second revision by the type of components or method of femoral fixation used in the first revision.
Osteolysis
The cumulative percent second revision at 10 years for the first revision for osteolysis was 14% (95% CI 10% to 19%) (Table 3). The most common reason for a second revision was prosthesis dislocation or instability (26% [11 of 43]), loosening (26% [11 of 43]), infection (21% [9 of 43]), and fracture (12% [5 of 43]) (Table 4). There was no difference in the cumulative percent second revision between minor head and insert revisions and acetabular revisions. However, there was a higher rate of second revision for a femoral component only than for an acetabular component only (Fig. 11).
Fig. 11.
This graph shows the cumulative percent second revision of known primary THA by type of the first revision (primary diagnosis osteoarthritis, first revision for osteolysis). A color image accompanies the online version of this article.
Mortality
The overall mortality after a first revision of a primary conventional THA was 1% at 30 days, 2% at 90 days, 5% at 1 year, and 40% at 10 years. Compared with other reasons for revision, the first revision for periprosthetic fracture had the highest mortality at all timepoints. At 10 years, the cumulative percent survival of patients undergoing revision for periprosthetic fracture was 46% compared with 84% for osteolysis, 68% for loosening, and 62% for dislocation or instability (Fig. 12).
Fig. 12.
This graph shows the cumulative percent survival of patients with known primary THA since the first revision by reason. A color image accompanies the online version of this article.
Discussion
There is an increasing incidence of revision THA but limited evidence on the overall rate of revision of the first revision procedure. Additionally, little is known about whether the reason for this revision has an effect on the outcome of the second revision. It is therefore important to examine factors associated with the outcomes of these procedures in order to provide surgeons with appropriate information to advise patients. By defining a standard ordinal terminology to describe the sequence of revision, terms such as “re-revision” or “further revisions” can be avoided.
We determined the overall rate of all first revision procedures where the primary procedure was performed for osteoarthritis and then examined whether the cumulative percent second revision varied by the more common reasons for the first revision. This will enable surgeons to have a better understanding of the likelihood of further procedures, aid patients during the informed consent process, and may be useful with healthcare planning, especially for first revision procedures that result in a higher early second revision such as first revision for dislocation. For example, if a THA is revised for loosening or dislocation or instability, then the most common reasons for a second revision are the same as for the first revision. Surgeons might explore ways to further minimize revision for the same reason, because this procedure is often distressing for patients and surgeons. Hospital guidelines should encourage the use of larger head sizes or dual-mobility components, where possible, for the first revision procedure.
Limitations
We acknowledge that this a “broad brush” approach to the outcome of first revision procedures, and there are several limitations to this study. Patients who undergo a first revision may have poor outcomes, such as pain or infection, that do not always result in a second revision operation [3]. The cumulative percent second revision is therefore only one measure, and other data, such as patient-reported outcome measures and complications after revision THA, were not collected by the registry during the time period of this study. Patient-reported outcome measures have been introduced nationally, and we plan to report on these in the future. Complications after first revision THA that do not result in further revision surgery or death were not reported but may be determined by data-linkage studies [2]. However, despite the lack of these other outcome measures, the cumulative percent second revision is a robust and verifiable endpoint and is valuable for comparative outcome studies.
We chose to report on the most common reasons for the first revision but did not report on all of them because we excluded first revisions for infection. This is because of the complexities associated with multiple operations for sepsis and the difficulty analyzing surgeon intent for planned first-stage and second-stage revision operations. However, first revision procedures for aseptic causes carry a risk of further revision for infection. Although we did not include septic first revisions in our study population, these data are still relevant because all of the other most-common causes of first revision diagnoses were included in the analyses.
We estimated the cumulative percent second revision according to the reason for the first revision, and this may have some limitations. The reasons for the first revision are provided by the surgeon at the time the revision procedure is recorded, and an internal audit of more than 4300 revision joint replacements recorded by the registry compared with surgeon case histories demonstrated a 91% match. There may have been some aseptic loosening revisions that were later proven to have low-grade sepsis that the registry was not made aware of, although we believe that this would have had a minimal impact on the results. We have no radiographic data in the registry, nor do we have information on bone deficiency grading or femoral impaction grafting, although the latter was not commonly used during this study period. There are different reasons for component loosening, ranging from failure of initial fixation to delayed loosening because of particle wear and osteolysis. However, the median time from the primary procedure to the first revision for loosening was only 4 years, with most procedures using modern bearing surfaces. Thus, we believe it is less likely there was catastrophic osteolysis and bone loss in patients undergoing revision for loosening, and therefore, the lack of data on radiographs and bone classification system may not be as important.
We only included revisions for periprosthetic fracture when a component was removed or added. The registry may not collect all data on periprosthetic fractures when a fracture was internally fixed without revision of a component [3]. We also noted that mortality for the first revision for periprosthetic fracture was higher than for patients undergoing revision for other reasons. On average, these patients were older, and we were not able to adjust for comorbidities other than ASA class and BMI. However, if a patient undergoes revision for a periprosthetic fracture, this has substantial consequences, and the patient and their relatives can be informed of the mortality risk.
For this study, we chose to use standard Kaplan-Meier estimates, although we acknowledge this may overestimate the revision risk when the competing risk of death is high. We also performed a separate analysis using death as a competing risk. The cumulative percent second overall revision using Kaplan-Meir estimates at 10 years was 21% compared with 18% for the competing risk model.
Patients for this study were drawn from one national registry, and the information may not be generalizable to other countries, although the Australian registry records data on many different prostheses that are commonly used worldwide.
Overall Rate of Revision of the First Revision Procedure
The overall cumulative percent second revision of first revisions at 18 years was 26% and is much higher than the first revision of a primary THA at the same time (8%) [1]. This higher rate has also been reported in other joint registries, although with a smaller sample size and shorter follow-up duration. The Norwegian Arthroplasty Register reported a cumulative second revision rate of 26% at 10 years [14]; however, this was from 1987 to 2003, before modern bearing surfaces were introduced. The Dutch Arthroplasty Register reported on first revisions for patients younger than 55 years who underwent primary THA [12]. Among 1057 first revisions, 214 patients underwent a second revision, and the cumulative percent second revision at 10 years for any reason was 28%. Although our study did not directly compare the same age groups, we demonstrated a higher rate of second revision in patients younger than 65 years at the time of the first revision. In a study using Medicare data from the United States in patients older than 65 years, the 5-year cumulative percent second revision of first THA revisions was 19% [18]. In a comprehensive review of data from an integrated United States healthcare registry, Khatod et al. [11] showed a cumulative percent second revision at 5 years of 13%.
It is clear from these studies that the rate of revision of first revision procedures is much higher than that of primary procedures, and surgeons, hospitals, and healthcare systems should strive to obtain the best results from the first procedure. The United Kingdom’s initiative “Getting it Right the First Time” is a national program to identify and reduce unwarranted variation in healthcare. It was pioneered in orthopaedic surgery and has been expanded to more than 40 other branches of medicine [15]. The use of joint registries can identify techniques in primary THA, such as the use of larger heads to reduce dislocation and cementing the femoral component in older patients to reduce loosening [1], that will help reduce the first-revision burden.
Does the Rate of Second Revision Vary by the Diagnosis of the First Revision?
Our study demonstrated that the most common reason for a second revision was dislocation or instability; specifically, patients with revisions for dislocation or instability often underwent a second revision procedure for the same diagnosis. Although performing a femoral head or acetabular insert change is the most common procedure, it has a higher rate of revision than when the acetabular component is revised. Although a minor revision is easier to perform, surgeons should consider whether the cup alignment is ideal because a major component revision may be more appropriate. Dislocation or instability is the most common indication for first revision THA in the United States [25] and in several other studies of first revision procedures (Table 5). Other studies confirmed that larger head sizes protected against further revision for dislocation [10, 20] except the study from Khatod et al. [11], which did not find a difference in second revision with respect to head size.
Table 5.
Summary of first-revision THA studies
| Author | Type of study and source | Outcome measure | Number of revision procedures | Most common reason for first revision |
| Current study | Retrospective national joint registry | Cumulative risk of second revision | 13,713 | Aseptic loosening |
| Deng et al. [6] | Systematic review | Cumulative incidence of periprosthetic fracture | 882 | Only periprosthetic fracture |
| Gromov et al. [8] | Retrospective national joint registry | Cumulative risk of second revision | 2596 | Aseptic loosening or periprosthetic fracture |
| Jo et al. [10] | Retrospective hospital registry | Cumulative risk of second revision | 539 | Dislocation |
| Khatod et al. [11] | Retrospective United States healthcare joint registry | First re-revision of THA | 629 | Dislocation |
| Kuijpers et al. [12] | Retrospective national joint registry | Cumulative risk of second revision | 1037 | Dislocation |
| Lie et al. [14] | Retrospective national joint registry | Cumulative risk of second revision | 4762 | Not stated |
| Ong et al. [18] | Retrospective United States Medicare claims data | Cumulative risk of second revision | 1205 | Not stated |
| Salassa et al. [20] | Retrospective community joint registry | Frequency for re-revision for dislocation | 118 | Dislocation |
| Tyson et al. [24] | Retrospective national joint registry | Cumulative risk of second revision | 2966 | Aseptic loosening |
| Upfill-Brown et al. [25] | Retrospective national inpatient sample | Percentage of revisions for specific causes | 292,250 | Dislocation |
In the Australian registry, loosening was the most common reason for the first revision, and in patients undergoing revision for this diagnosis, it was also the most common reason for the second revision. Most first revisions were for femoral loosening, and a lower second revision rate was found from 6 months to 6 years if cementless stems were used in the first revision. This finding was confirmed by the Kaiser Permanente registry [11], the Norwegian Register [14], and the Danish Hip Register [8]; however, it differs from that of a study from the Swedish Hip Arthroplasty Register [24]. We are not sure why there are differences between the second revision rates by the type of femoral fixation in Sweden. The Swedish registry reported similar implant survival by femoral fixation up to 13 years, but the adjusted risk for cementless stems was higher only for the first year. This may have been because of better cementing techniques in a country that has a high proportion of primary cemented stems.
We reported increasing revision rates for periprosthetic fracture of primary THA [1], and 3675 first revisions were recorded for this diagnosis. Although most revisions were for femoral fractures, 5% of first revisions had an acetabular component exchange only, and 7% had both components revised. Therefore, we were unable to determine whether there were both femoral and acetabular fractures, or, more likely, whether the acetabulum was revised at the same time as the femur. The type of femoral fixation at the first revision for periprosthetic fracture had no bearing on the rate of second revision. The mean age at the time of the first revision and the time from the first revision to the second for periprosthetic fracture were similar to those reported in a systematic review of risk factors for periprosthetic fractures in revision THA [6].
We also reported on the outcomes of first revision for osteolysis (separate from loosening), although these revisions occurred much longer after the primary THA than revisions for other reasons. Minor revisions to change the head and/or acetabular liner were the most common types of revision but still had a cumulative percent second revision of 13% at 6 years. One study [22] reported on the outcomes of isolated head and liner exchange in 138 revision THAs, 57.2% of which (79) were revised for polyethylene wear or osteolysis. The authors used femoral head sizes ≥ 32 mm, and the overall cumulative rate of second revision was 5.4% at 5 years. However, the study did not report specifically on the outcome of first revision for osteolysis.
Mortality
Mortality after the first revision procedure was higher than after a primary THA and was the highest when the first revision was for periprosthetic fracture. The Swedish register reported a 90-day mortality rate of 1% for patients undergoing revision for loosening [24], compared with the rate of 0.6% in our study. Neither the Dutch nor Norwegian register studies reported on mortality after the first revision procedure [12, 14]. Considering this information, surgeons may be better prepared to discuss mortality after the first revision. Some reasons for revision are relatively urgent, such as periprosthetic fracture, and are treated with surgery, but in the surgeon-patient discussion for other reasons for revision of a primary THA, the higher rate of mortality may lead to the consideration of nonoperative management.
Conclusion
This study outlined a method for describing multiple revisions after a primary procedure that we hope will be adopted for clarity of reporting and to avoid the imprecise use of the term “re-revision.” When surgeons revise a primary THA for dislocation, larger head sizes and dual-mobility cups may help reduce further revisions for dislocation. The use of cementless stems for a first revision for loosening seems advantageous. Surgeons may counsel patients about the higher risk of death after first-revision procedures compared with primary procedures, particularly if the first revision is performed for periprosthetic fracture.
Acknowledgments
We thank the Australian Orthopaedic Association National Joint Replacement Registry and the hospitals, orthopaedic surgeons, and patients whose data made this work possible.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from the Australian Government Department of Health.
This work was performed at the Australian Orthopaedic Association National Joint Replacement Registry, based at the South Australian Health and Medical Research Institute, Adelaide, South Australia.
Contributor Information
Peter L. Lewis, Email: plewis@woc.com.au.
Ian Harris, Email: ianharris@unsw.edu.au.
Stephen E. Graves, Email: segraves@aoanjrr.org.au.
References
- 1.Australian Orthopaedic Association National Joint Replacement Registry. Hip, knee and shoulder arthroplasty: annual report 2021. Available at: https://aoanjrr.sahmri.com/annual-reports-2021. Accessed November 24, 2021.
- 2.Badarudeen S, Shu AC, Ong KL, Baykal D, Lau E, Malkani AL. Complications after revision total hip arthroplasty in the medicare population. J Arthroplasty. 2017;32:1954-1958. [DOI] [PubMed] [Google Scholar]
- 3.Constantin H, Le M, de Steiger R, Harris IA. Operation rate is more than double the revision rate for periprosthetic femur fractures. ANZ J Surg. 2019;89:1647-1651. [DOI] [PubMed] [Google Scholar]
- 4.Cuthbert AR, Graves SE, Giles LC, Glonek G, Pratt N. What is the effect of using a competing-risks estimator when predicting survivorship after joint arthroplasty: a comparison of approaches to survivorship estimation in a large registry. Clin Orthop Relat Res. 2021;479:392-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Steiger R, Peng A, Lewis P, Graves S. What is the long-term survival for primary THA with small-head metal-on-metal bearings? Clin Orthop Relat Res. 2018;476:1231-1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deng Y, Kieser D, Wyatt M, Stringer M, Frampton C, Hooper G. Risk factors for periprosthetic femoral fractures around total hip arthroplasty: a systematic review and meta-analysis. ANZ J Surg. 2020;90:441-447. [DOI] [PubMed] [Google Scholar]
- 7.Graves SE, de Steiger R, Davidson D, et al. The use of femoral stems with exchangeable necks in primary total hip arthroplasty increases the rate of revision. Bone Joint J. 2017;99:766-773. [DOI] [PubMed] [Google Scholar]
- 8.Gromov K, Pedersen AB, Overgaard S, Gebuhr P, Malchau H, Troelsen A. Do rerevision rates differ after first-time revision of primary THA with a cemented and cementless femoral component? Clin Orthop Relat Res. 2015;473:3391-3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gundersen T, Furnes O, Gjertsen J-E, et al. Norwegian Arthroplasty Register annual report 2021. Available at: https://www.researchgate.net/publication/356998659_Annual_report_2021. Accessed November 24, 2021.
- 10.Jo S, Jimenez Almonte JH, Sierra RJ. The cumulative risk of re-dislocation after revision THA performed for instability increases close to 35% at 15 years. J Arthroplasty. 2015;30:1177-1182. [DOI] [PubMed] [Google Scholar]
- 11.Khatod M, Cafri G, Inacio MC, Schepps AL, Paxton EW, Bini SA. Revision total hip arthoplasty: factors associated with re-revision surgery. J Bone Joint Surg Am. 2015;97:359-366. [DOI] [PubMed] [Google Scholar]
- 12.Kuijpers M, Hannink G, van Steenbergen L, Schreurs B. Outcome of revision hip arthroplasty in patients younger than 55 years: an analysis of 1,037 revisions in the Dutch Arthroplasty Register. Acta Orthop. 2020;91:165-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br. 2010;92:38-46. [DOI] [PubMed] [Google Scholar]
- 14.Lie SA, Havelin LI, Furnes ON, Engesaeter LB, Vollset SE. Failure rates for 4762 revision total hip arthroplasties in the Norwegian Arthroplasty Register. J Bone Joint Surg Br. 2004;86:504-509. [PubMed] [Google Scholar]
- 15.National Health Service. Getting it Right First Time (GIRFT): getting it right in orthopaedics. Available at: https://gettingitrightfirsttime.co.uk/wp-content/uploads/2020/02/GIRFT-orthopaedics-follow-up-report-February-2020.pdf. Accessed May 20, 2022.
- 16.National Joint Registry. 18th Annual Report. Available at: https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2018th%20Annual%20Report%202021.pdf. Accessed November 24, 2021. [PubMed]
- 17.New Zealand Joint Registry. The New Zealand Joint Registry: twenty-two year report. January 1999 to December 2020. Available at: https://www.nzoa.org.nz/sites/default/files/NZJR_22_Year_Report_Final.pdf. Accessed November 24, 2021.
- 18.Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res. 2010;468:3070-3076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prokopetz JJ, Losina E, Bliss RL, Wright J, Baron JA, Katz JN. Risk factors for revision of primary total hip arthroplasty: a systematic review. BMC Musculoskelet Disord. 2012;13:251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salassa T, Hoeffel D, Mehle S, Tatman P, Gioe TJ. Efficacy of revision surgery for the dislocating total hip arthroplasty: report from a large community registry. Clin Orthop Relat Res. 2014;472:962-967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwartz AM, Farley KX, Guild GN, Bradbury TL, Jr. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty. 2020;35:S79-S85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sutter EG, Akram F, Miller A, Paprosky WG, Berger RA, Gerlinger TL. Outcomes of isolated head and liner exchange using large femoral heads and modern liners in revision total hip arthroplasty. J Arthroplasty. 2020;35:1064-1068. [DOI] [PubMed] [Google Scholar]
- 23.Swedish Hip Arthroplasty Register. Annual Report 2019. Available at: https://registercentrum.blob.core.windows.net/shpr/r/VGR_Annual-report_SHAR_2019_EN_Digital-pages_FINAL-ryxaMBUWZ_.pdf. Accessed November 24, 2021.
- 24.Tyson Y, Rolfson O, Kärrholm J, Hailer NP, Mohaddes M. Uncemented or cemented revision stems? Analysis of 2,296 first-time hip revision arthroplasties performed due to aseptic loosening, reported to the Swedish Hip Arthroplasty Register. Acta Orthop. 2019;90:421-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Upfill-Brown A, Hsiue PP, Sekimura T, Patel JN, Adamson M, Stavrakis AI. Instability is the most common indication for revision hip arthroplasty in the United States: national trends from 2012 to 2018. Arthroplast Today. 2021;11:88-101. [DOI] [PMC free article] [PubMed] [Google Scholar]