Abstract
Background and study aims Gastric endoscopic submucosal dissection (ESD) is a highly technical procedure mainly due to the distinctive shape of the stomach and diverse locations of lesions. We developed a new gastric ESD training model (G-Master) that could accurately recreate the location of the stomach and assessed the reproducibility of located lesions in the model.
Methods The model comprises a simulated mucous membrane sheet made of konjac flour and a setting frame, which can simulate 11 locations of the stomach. We assessed the reproducibility of each location in the model by assessing the procedure speed and using a questionnaire that was distributed among experts. In the questionnaire, each location was scored on a six-point scale for similarity of locations.
Results The mean score for all locations was high with > 4 points. Regarding locations, lower anterior and posterior walls had medium scores with 3 to 4 points. The procedure speed was slower in the greater curvature of the upper and middle gastric portions, where ESD is considered more difficult than the overall procedure speed.
Conclusions The new gastric ESD training model appears to be highly reproducible for each gastric location and its application for training in assuming actual gastric ESD locations.
Introduction
Gastric endoscopic submucosal dissection (ESD) has become increasingly popular worldwide as a less invasive curative treatment for early gastric cancer. However, it requires technical proficiency mainly due to the distinctive shape of the tract and diverse locations of lesions 1 2 3 . This technique requires a strategy that includes keeping an adequate scope position, control of devices, and the amount of air in the stomach for each location.
Generally, animal (extracted) digestive tracts or live animals are used for ESD training 4 5 . However, it is difficult to simulate actual gastric ESD locations during such training, and it also raises several issues, including ethics, cost, and infection. Also, when novice operators perform ESD, they receive training on the job based on their abilities 6 and their training level, which gradually increases by transitioning from performing ESD on known, easy locations, such as the antrum, to difficult locations, such as the upper or middle portion of the greater curvature 7 8 . However, it is difficult to prepare cases based on an operator’s abilities to meet the demand.
Therefore, we developed a new gastric ESD training model that can accurately simulate the locations of the human stomach using non-animal subjects and assessed the reproducibility of each location of the training model.
Methods
Development and set-up of the new gastric ESD training model
Video 1 Setting of the location that reproduces the lesser curvature of the middle portion based on this model.
We developed a new gastric ESD training model that comprises a rectangular simulated mucous membrane sheet made of konjac flour ( Fig. 1a ) and a setting frame ( Fig. 1b ). The mucosal sheet consists of three layers of different hardness, strength, and density, which simulate the mucosal, submucosal, and muscular layers. ( Fig. 1a ). The development of this model (G-Master) was a joint research project between KOTOBUKI Medical Limited and the National Cancer Center Hospital East. The steps to set up this model are as follows: the seat was fixed at four points; the seat position was set with a two-axis gimbal structure; the position of the cardia was determined in the XYZ direction, and the angle was also determined ( Video 1 ). The mucosal tension regulator, reproducing the change in air volume in the stomach during ESD, adjusted for the tension in the model on demand. The mucosal tension regulator can tension or loosen the simulated mucosal sheet. A spatula that imitates the greater curvature of the stomach was set up because the hard part of the scope was supported by the greater curvature of the stomach in areas far from the cardia, such as parts of middle and lower portions. This model can be set up in 11 different locations by setting nine adjuster parts ( Fig. 1b ). The 11 locations consist of four circumferential locations (anterior wall, posterior wall, lesser curvature, and greater curvature) and three locations (upper, middle, and lower), except for the greater curvature of the lower portion, which was difficult to reproduce ( Fig. 2 ). Each location can be set up in about 5 minutes.
Fig. 1 a.
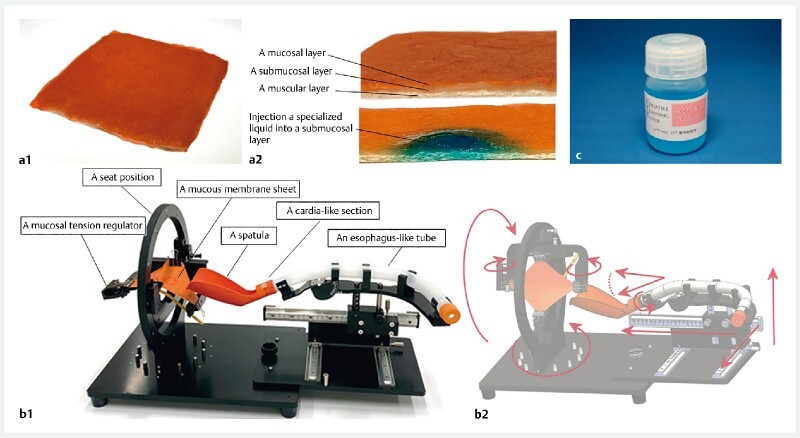
The plant-origin mucous membrane sheet was made out of konjac flour. The mucous membrane sheet is composed of three layers: the mucosal layer (thickness: 0.5–1.0 mm), the submucosal layer (thickness: 0.5–1.0 mm), and the muscular layer (thickness: 1.0–2.0 mm). The composition of the konjac flour was changed for each layer to simulate the strength and properties of the actual gastric mucosa. b The model consists of an esophagus-like tube, a seat position with a two-axis gimbal structure, a cardia-like section with adjustable position and angle in the XYZ direction, a spatula that imitates the greater curvature of the stomach, and a mucosal tension regulator that can reproduce the change in air volume in the stomach during ESD and adjust the tension on demand. The model can be set to various locations with nine adjustment parts. c A specialized liquid is injected into the submucosal layer. Its components are polysaccharide (0.1–10 %), sucrose (0.1–10 %), mineral salt (0.1–10 %), and dye (minute quantities).
Fig. 2.
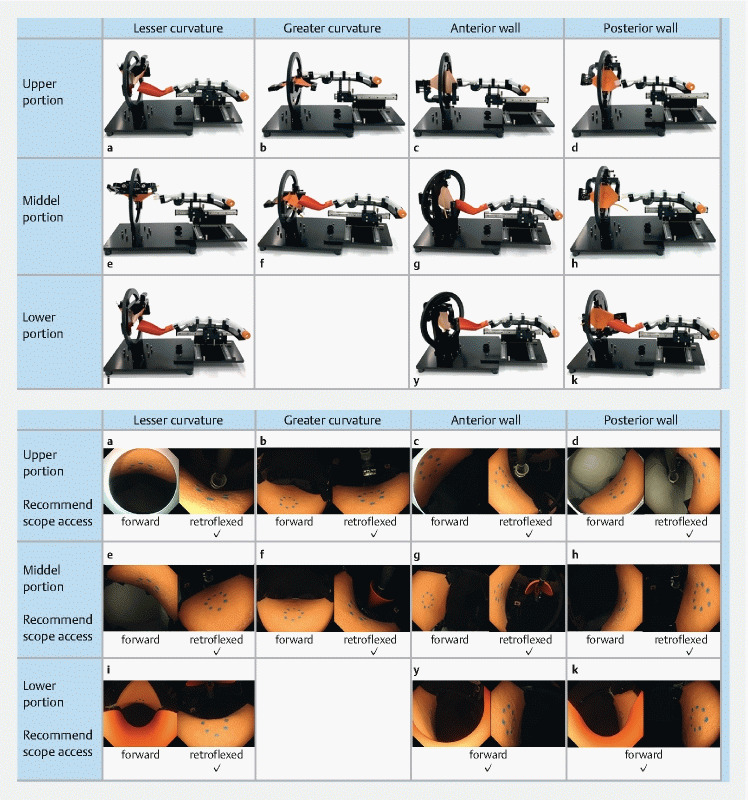
Set-up of 11 locations in G-Master. The first row is the upper portion, from left a lesser curvature, b greater curvature, c anterior wall, d posterior wall. The second row is the middle portion, from left e lesser curvature, f greater curvature, g anterior wall, h posterior wall. The third row is the lower portion, from left i lesser curvature (gastric angle), j anterior wall, and k posterior wall.
Evaluation method
Video 2 ESD was performed on the location that reproduced the gastric angle based on this model.
Eight ESD experts who were not involved in the development of this training model used the model for ESD in three to five locations per person, and each location was performed by three experts. ESD expert criteria was performing > 100 upper gastrointestinal ESD cases.
ESD was performed using a single-channel upper gastrointestinal endoscope (GIF Q260J; Olympus, Tokyo, Japan) with an electrosurgical unit (VIO-3 and VIO-300; ERBE, Tubingen, Germany) and an electrosurgical knife (Dual knife KD-650 L / IT knife-2 KD-611L; Olympus, Tokyo, Japan). IT knife-2 was the main knife used and traction devices as the clip with thread were not used. A marking of a 20-mm regular circle that mimicked the lesion on the seat was placed using an electrosurgical knife. A specialized liquid ( Fig. 1c ) (VTT-INJ; KOTOBUKI Medical, Inc.) was injected into the submucosal layer, and mucosal circumferential incision and trimming, and submucosal dissection were performed using an electrosurgical knife ( Video 2 ).
The following parameters were recorded: 1) ESD procedure time; 2) complete resection; and 3) perforation. To evaluate the technical difficulty level of each location, we calculated the ESD procedure speed. The ESD procedure speed was evaluated using the total procedure speed (from the beginning of local injection to specimen resection) and the dissection speed (from the end of the full circumferential incision to specimen resection). The ESD procedure speed (mm 2 /min) was calculated using the area of the resected specimen (mm 2 ) per unit procedure time (min). The area of the resected specimen was calculated using the following formula: major axis (mm)/2 × minor axis (mm)/2 × 3.14. Complete resection was defined as one-piece resection with no incision within the specimen. Perforation was defined as a hole in the sheet that penetrated the muscular layer. The diameter of the virtual lesion was standardized as a 20-mm regular circle. Quantitative data was expressed as median and range.
A questionnaire was distributed after each ESD. Using a six-point scale, participants subjectively scored the following: 1) similarity of locations; 2) similarity of mucosal tension changes due to adjustment of the amount of air in the stomach, and 3) similarity of simulated mucosal sheet. The similarity of locations was evaluated based on the following scoring points: 1) similarity to the actual location; and 2) feeling of the scope’s movement. The similarity of simulated mucosal sheet was evaluated for: 1) protruding after local injection; 2) feel of mucosal incision; and 3) feel of submucosal dissection. A score of < 2 points was considered a low rating, 2 to 4 points was a medium rating, and > 4 points, high rating. The rating for each location was defined as the mean of the three experts' scores.
Results
All 33 mimicked lesions were resected completely without perforations. The mucosal tension was changed at least once during all ESDs. The overall median (range) total procedure speed/dissection speed was 31 (22–45)/51 (31–79) mm 2 /min ( Table 1 ). The ESD procedure speed was slower at the following locations compared with the overall median speed: on the greater curvature side of the upper (25 (24–29)/44 (31–48) mm 2 /min) and middle (23 (22–38)/37 (34–38) mm 2 /min) portions, and on the anterior (28 (26–31)/44 (42–46) mm 2 /min) and posterior (26 (23–27)/40 (38–41) mm 2 /min) walls of the lower portion ( Table 2 ).
Table 1. Endoscopic submucosal dissection procedure data.
| Total (n = 33) | |
| ESD procedure speed, median (range), min/cm2 | |
|
31 (22–45) |
|
51 (31–79) |
| ESD procedure time, median (range), min | |
|
19 (14–31) |
|
11 (7–19) |
| Areas of resected specimen, median (range), cm2 | 589 (415–687) |
| Complete resection, n (%) | 33 (100) |
| Perforation, n (%) | 0 (0) |
| ESD endoscopic submucosal dissection | |
Table 2. ESD procedure speed for each location.
| Total procedure speed, median (range), min/cm 2 |
Dissection speed, median (range), min/cm 2 |
||
| Upper portion | Lesser curvature | 32 (25–40) | 51 (47–57) |
| Greater curvature | 25 (24–29) | 44 (31–48) | |
| Anterior wall | 32 (31–40) | 67 (57–79) | |
| Posterior wall | 33 (31–44) | 65 (55–77) | |
| Middle portion | Lesser curvature | 34 (33–36) | 66 (62–73) |
| Greater curvature | 23 (22–38) | 37 (34–38) | |
| Anterior wall | 36 (32–45) | 63 (51–79) | |
| Posterior wall | 31 (24–34) | 57 (44–68) | |
| Lower portion | Lesser curvature | 44 (27–44) | 66 (42–76) |
| Anterior wall | 28 (26–31) | 44 (42–46) | |
| Posterior wall | 26 (23–27) | 40 (38–41) |
In the questionnaire, the mean score for all locations was high, with 4 points or more in the similarity of locations and 4.5 points in the similarity of mucosal tension changes. By location, similarity of locations generally had high ratings, with > 4 points, but only the lower anterior and posterior walls had medium ratings with 3 to 4 points ( Fig. 3 ). All locations’ similarity of mucosal tension changes had high ratings, with > 4 points ( Fig. 4 ). In the similarity of simulated mucosa, the mean score for all the locations was high, with four points in all of the categories.
Fig. 3.
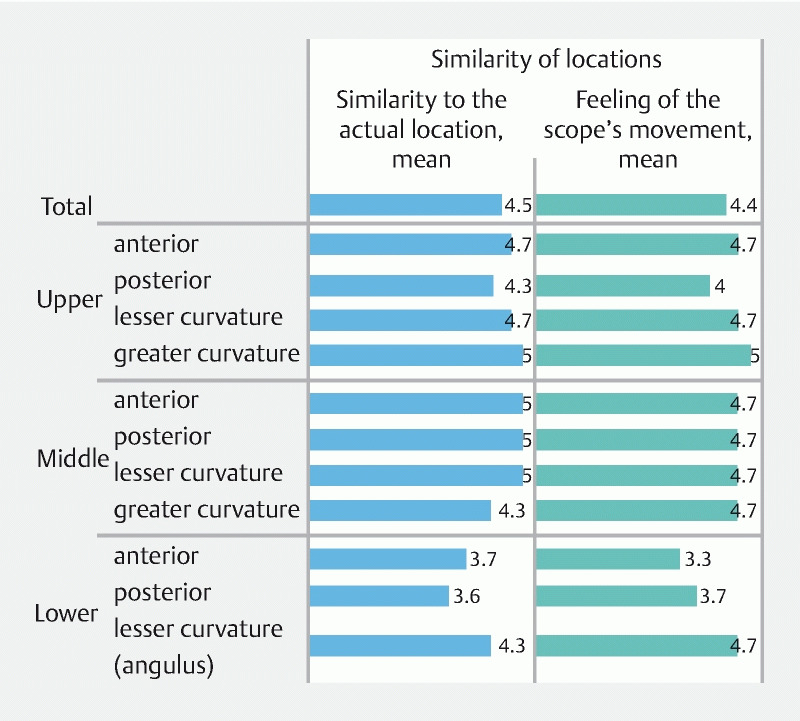
The questionnaire responses as scored on a six-point scale. The similarity of locations was evaluated based on similarity to the actual location and feeling the scope’s movement. The mean score of similarity of locations for all locations was ≥ 4. By locations, similarity of locations of lower anterior and posterior walls were 3 to 4 points, and all other locations were ≥4 points.
Fig. 4.
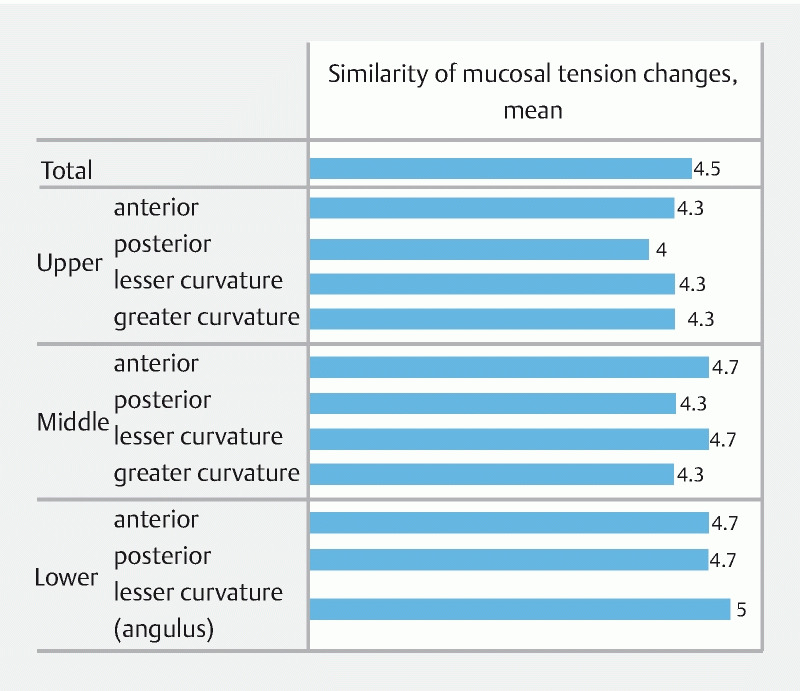
Questionnaire responses as scored on a six-point scale. The mean score of similarity of mucosal tension changes for all locations was 4.5 points. By locations, the similarity of mucosal tension changes of all locations was ≥ 4 points
Discussion
To date, there has been no training model in which ESD of various stomach locations can be reproduced. We developed a new gastric ESD training model that consists of a simulated mucous membrane sheet and a setting frame. This study showed that the new gastric ESD training model reproduced most of the real gastric ESD locations in the questionnaire, and the ESD procedure speed for each location was associated with the difficulty level in the real gastric ESD.
The simulated mucosal sheet has three layers that simulate the mucosal, submucosal, and muscular layers. The hardness, strength, and density of the three layers can vary by changing the compounding materials and manufacturing conditions. To reproduce the actual stomach wall, each layer is characterized by high density and high strength in the mucosal layer; low density and loose structure in the submucosal layer; and high hardness in the muscular layer. Separation of the layers allows for more realistic reproduction of the mucosal incision and submucosal dissection procedures. Presence of the muscle layer also allows ESD training to be performed with caution with respect to muscle layer damage and perforation during submucosal dissection. This setting frame enables ESD in various lesion sites in the stomach by adjusting the angle of the seat position, distance between the cardia and the seat, angle of the cardia, and a spatula that imitates the greater curvature of the stomach. Therefore, the feeling of the scope's movement for each location is reproduced, and this makes it possible to be used for training while considering ESD strategies for each location.
In this study, most locations were evaluated as similar to actual gastric ESD. Additionally, the dissection speed was slower in the greater curvature of the upper and middle portions than in other locations, which is in line with that of a previous report in actual gastric ESD 8 . The lesions in the greater curvature of the upper and middle gastric portions in the model is difficult to approach as well as actual gastric ESD. Also, the direction of gravity on the lesion is similar to that of actual gastric ESD, which makes it difficult for water to accumulate and getting into the submucosal layer. We considered that this is the reason for the longer ESD procedure time. Thus, we considered that this model could duplicate the actual gastric ESD in terms of the procedure speed in each location. Sato et al. and Chen et al. have reported the feasibility of ESD training models using non-animal subjects 9 10 . The model that uses non-animal subjects can be trained to be effective for ESD in any facility equipped for endoscopy, without requiring endoscopic units specialized for animal use. However, these models did not reproduce the various parts of the stomach. In our model, each location was well reproduced, and the training can be performed assuming the location with the specific strategy before the real gastric ESD.
Using the model, ESD in the anterior and posterior walls of the lower portion had low reproducibility compared to other locations. The ESD procedure speed at these two locations was slower than the overall speed. However, Konuma et al. reported that ESD in the antrum is relatively easy to perform, and the dissection speed is faster than in other locations 8 . In an isolated porcine model, Horii et al. reported that the reason for the difference in reproducibility of actual ESD in the lower portion may be related to differences in mucosal thickness and direction of gravity 11 . In line with previous reports, it was difficult to reproduce the gravity direction of the lesion and thickness of the mucosal layer to simulate the ESD in the anterior and posterior walls of the lower portion. In the future, we plan to increase the variety of thickness of the mucosal layer and submucosal layer to create simulated mucosal sheets suitable for each location.
To become an expert in ESD, it was recommended to start with gastric locations where ESD is technically easy, followed by more difficult locations 12 13 , and eventually transition to esophageal and colorectal ESD 14 15 . Despite the relatively high incidence of early-stage gastric cancer in Japan, novice endoscopists are only able to perform gastric ESD of various locations in a few institutions such as high-volume centers. In addition, gastric ESD is rare in the United States and Europe; hence, there are few opportunities of training for beginners. Therefore, endoscopists in these regions would need to perform more difficult ESD such as colorectal and Barrett's on the job. The learning curve for ESD in these regions is different from that for endoscopists in Japan, and it is considered that an endoscopist’s ESD skills will not improve without more ESD experience 16 17 . Therefore, it is considered necessary to use training models, such as animal models, for ESD training before starting ESD 18 . However, there are several issues associated with the use of animals in education. Training based on the present model, which uses simulated plant-derived mucosa and accurately reproduces the shape of the stomach, is considered to be very important. Also, to improve the technique of a special technique, it is necessary to perform it multiple times to establish muscle memory. Establishing muscle memory leads to increased efficiency, reduced costs, and improved patient safety. Since this model can reproduce the same site, repeated training is expected to acquire muscle memory 19 .
This study has some limitations. First, this was a single-center, small-group study. However, all evaluations were conducted by experts. Second, the evaluation was subjective and based on a questionnaire; therefore, we examined the ESD procedure speed of each location to obtain an objective evaluation. Third, the change of the mucosal tension in this model still only allows for changes in the longitudinal direction. Actual ESD is thought to involve changes in both the longitudinal and lateral directions. Fourth, this study focused on reproducibility and not on improving technical ESD skills. The usefulness of this ESD model in improving ESD technical skills needs to be investigated in the future.
Conclusions
In conclusion, the new gastric ESD training model appeared highly reproducible for each stomach position and may serve as a promising device for training with respect to assumed actual gastric ESD positions.
Acknowledgments
KOTOBUKI Medical Inc provided support for this study in the form of a research grant awarded to Dr. Yoda. KOTOBUKI Medical Inc played a role in the development of this model (G-Master), but no other role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Funding Statement
KOTOBUKI Medical Inc
Footnotes
Competing interests The authors have read the journal’s policy and have the following competing interests: S.T. is shareholder of KOTOBUKI Medical Inc. Y.Y. also received a research grant from KOTOBUKI Medical Inc. Additionally, KOTOBUKI Medical Limited provided the development of this model (G-Master). This does not alter our adherence to Endoscopy policies on sharing data and materials. Under the joint research agreement, T.M., Y.Y., H.S., S.T., and T.Y. jointly applied for the findings obtained from this study as a Japanese patent (2021-005642).
References
- 1.Isomoto H, Shikuwa S, Yamaguchi N et al. Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut. 2009;58:331–336. doi: 10.1136/gut.2008.165381. [DOI] [PubMed] [Google Scholar]
- 2.Lian J, Chen S, Zhang Y et al. A meta-analysis of endoscopic submucosal dissection and EMR for early gastric cancer. Gastrointest Endosc. 2012;76:763–770. doi: 10.1016/j.gie.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 3.Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T et al. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829–854. doi: 10.1055/s-0034-1392882. [DOI] [PubMed] [Google Scholar]
- 4.Vázquez-Sequeiros E, de Miquel D B, Olcina J R et al. Training model for teaching endoscopic submucosal dissection of gastric tumors. Rev Esp Enferm Dig. 2009;101:546–552. doi: 10.4321/s1130-01082009000800005. [DOI] [PubMed] [Google Scholar]
- 5.Parra-Blanco A, Arnau M R, Nicolás-Pérez D et al. Endoscopic submucosal dissection training with pig models in a Western country. World J Gastroenterol. 2010;16:2895–2900. doi: 10.3748/wjg.v16.i23.2895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teoh A Y, Chiu P W, Wong S K et al. Difficulties and outcomes in starting endoscopic submucosal dissection. Surg Endosc. 2010;24:1049–1054. doi: 10.1007/s00464-009-0724-8. [DOI] [PubMed] [Google Scholar]
- 7.Yano T, Hasuike N, Ono H et al. Factors associated with technical difficulty of endoscopic submucosal dissection for early gastric cancer that met the expanded indication criteria: post hoc analysis of a multi-institutional prospective confirmatory trial (JCOG0607) Gastric Cancer. 2020;23:168–174. doi: 10.1007/s10120-019-00991-3. [DOI] [PubMed] [Google Scholar]
- 8.Konuma H, Matsumoto K, Ueyama H et al. Procedure time for gastric endoscopic submucosal dissection according to location, considering both mucosal circumferential incision and submucosal dissection. Gastroenterol Res Pract. 2016;2016:9.183793E6. doi: 10.1155/2016/9183793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sato H, Mizuno K I, Sato Y et al. Development and use of a non-biomaterial model for hands-on training of endoscopic procedures. Ann Transl Med. 2017;5:182. doi: 10.21037/atm.2017.01.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen M J, Wang H Y, Chang C W et al. A novel artificial tissue simulator for endoscopic submucosal resection training – a pilot study. BMC Gastroenterol. 2016;16:112. doi: 10.1186/s12876-016-0529-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horii J, Goto O, Shimoda M et al. Which part of a porcine stomach is suitable as an animal training model for gastric endoscopic submucosal dissection? Endoscopy. 2016;48:188–193. doi: 10.1055/s-0034-1393047. [DOI] [PubMed] [Google Scholar]
- 12.Oda I, Odagaki T, Suzuki H et al. Learning curve for endoscopic submucosal dissection of early gastric cancer based on trainee experience. Dig Endosc. 2012;24:129–132. doi: 10.1111/j.1443-1661.2012.01265.x. [DOI] [PubMed] [Google Scholar]
- 13.Yoshida M, Kakushima N, Mori K et al. Learning curve and clinical outcome of gastric endoscopic submucosal dissection performed by trainee operators. Surg Endosc. 2017;31:3614–3622. doi: 10.1007/s00464-016-5393-9. [DOI] [PubMed] [Google Scholar]
- 14.Sakamoto T, Saito Y, Fukunaga S et al. Learning curve associated with colorectal endoscopic submucosal dissection for endoscopists experienced in gastric endoscopic submucosal dissection. Dis Colon Rectum. 2011;54:1307–1312. doi: 10.1097/DCR.0b013e3182282ab0. [DOI] [PubMed] [Google Scholar]
- 15.Hotta K, Oyama T, Shinohara T et al. Learning curve for endoscopic submucosal dissection of large colorectal tumors. Dig Endosc. 2010;22:302–306. doi: 10.1111/j.1443-1661.2010.01005.x. [DOI] [PubMed] [Google Scholar]
- 16.Zhang X, Ly E K, Nithyanand S et al. Learning curve for endoscopic submucosal dissection with an untutored, prevalence-based approach in the United States. Clin Gastroenterol Hepatol. 2020;18:580–INF. doi: 10.1016/j.cgh.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 17.Probst A, Golger D, Anthuber M et al. Endoscopic submucosal dissection in large sessile lesions of the rectosigmoid: learning curve in a European center. Endoscopy. 2012;44:660–667. doi: 10.1055/s-0032-1309403. [DOI] [PubMed] [Google Scholar]
- 18.Berr F, Ponchon T, Neureiter D et al. Experimental endoscopic submucosal dissection training in a porcine model: learning experience of skilled Western endoscopists. Dig Endosc. 2011;23:281–289. doi: 10.1111/j.1443-1661.2011.01129.x. [DOI] [PubMed] [Google Scholar]
- 19.Papanikolaou I G, Haidopoulos D, Paschopoulos M et al. Changing the way we train surgeons in the 21th century: A narrative comparative review focused on box trainers and virtual reality simulators. Eur J Obstet Gynecol Reprod Biol. 2019;235:13–18. doi: 10.1016/j.ejogrb.2019.01.016. [DOI] [PubMed] [Google Scholar]


