Abstract
Purpose
Antihypertensive drugs are among the most prescribed drugs during pregnancy. Methyldopa, labetalol, and nifedipine have been perceived safe to use during pregnancy and are therefore recommended in international guidelines for treatment of hypertension. In this review, we provide a complete overview of what is known on the pharmacokinetics (PK) of the antihypertensive drugs methyldopa, labetalol, and nifedipine throughout pregnancy.
Methods
A systematic search was performed to retrieve studies on the PK of methyldopa, labetalol, and nifedipine used throughout pregnancy. The search was restricted to English and original studies. The systematic search was conducted on July 27, 2021, in Embase, Medline Ovid, Web of Science, Cochrane Library, and Google Scholar. Keywords were methyldopa, labetalol, nifedipine, pharmacokinetics, pregnancy, and placenta.
Results
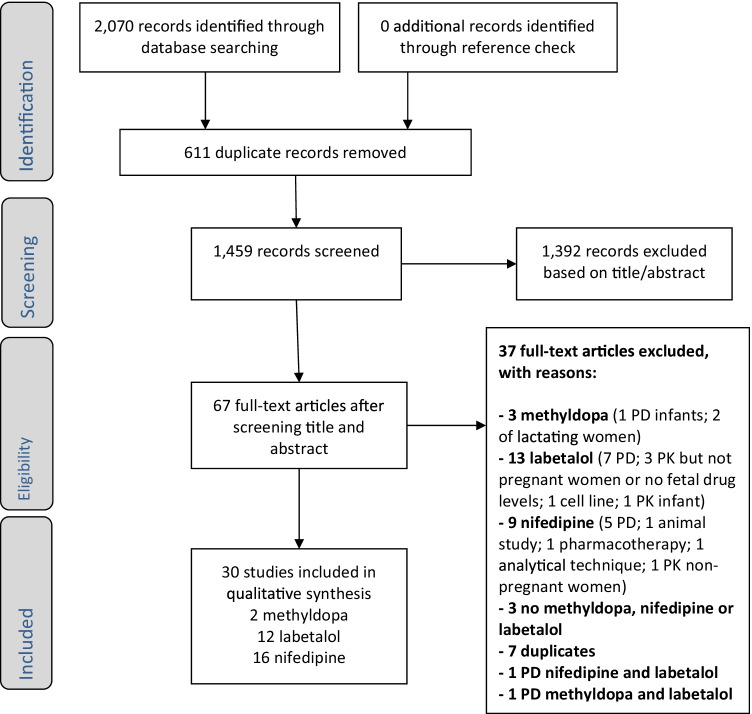
A total of 1459 unique references were identified of which title and abstract were screened. Based on this screening, 67 full-text papers were assessed, to retain 30 PK studies of which 2 described methyldopa, 12 labetalol, and 16 nifedipine. No fetal accumulation is found for any of the antihypertensive drugs studied.
Conclusion
We conclude that despite decades of prescribing methyldopa, labetalol, and nifedipine throughout pregnancy, descriptions of their PK during pregnancy are hampered by a large heterogeneity in the low number of available studies. Aiming for evidence-based and personalized dosing of antihypertensive medication in the future, further studies on the relationship of both PK and pharmacodynamics (including the optimal blood pressure targeting) during pregnancy and pregnancy-related pathology are urgently needed to prevent undertreatment, overtreatment, and side effects.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00228-022-03382-3.
Keywords: Methyldopa, Labetalol, Nifedipine, Pharmacokinetics, Pregnancy, Hypertension, Hypertensive disorders of pregnancy
Introduction
Pregnant women frequently use prescription and over-the-counter drugs: more than 80% use at least one drug throughout pregnancy including folic acid to reduce neonatal mortality and morbidity from neural tube disorders; 1.5–2% use cardiovascular drugs [1–5]. Information on optimal dosing of drugs throughout pregnancy is widely lacking, as ethical, legal, and practical reasons often prevent inclusion of pregnant women in clinical trials [6]. As a result, most drug use during pregnancy is “off-label” even when commonly used [7, 8]. Recently, the same issue occurred during the COVID-19 pandemic in which initially information on COVID-19 vaccination throughout pregnancy was lacking [9, 10]. An international call has been made to start including pregnant women in clinical trials instead of excluding them [11].
Pregnancy is associated with physiological changes, like body composition, renal clearance, protein concentration, and enzyme activity that has been shown to significantly alter the pharmacokinetics (PK) of many drugs, like amoxicillin and antipsychotics [12–14]. Due to these PK changes, simple extrapolation of normal dosages for nonpregnant women to dosages for pregnant women may lead to either subtherapeutic drug effects or supratherapeutic exposure in expecting women or toxic effects in the fetus due to placental transfer [15]. Furthermore, drug use can lead to placental dysfunction or accumulation of the drug, fetal (over)exposure, and teratogenic side effects. As an appropriate dose of a drug during pregnancy for a specific indication can be difficult to determine, most dosages have been derived empirically. In general, the aim is to dose as low as possible [16].
Hypertension is one of the most common health problems among pregnant women for which pharmacotherapy is indicated [17]. The incidence of hypertension for primigravida and multigravida is 10–15% and 2–5%, respectively [18]. Hypertensive disorders during pregnancy are classified as follows according to the International Society for the Study of Hypertension in Pregnancy (ISSHP): chronic hypertension (predating or diagnosed before 20 weeks of pregnancy), gestational hypertension (de novo after 20 weeks of gestation), (pre)eclampsia (de novo or superimposed on chronic hypertension: hypertension after 20 weeks of gestation accompanied by proteinuria and/or evidence of maternal acute kidney injury, liver dysfunction, neurological features, hemolysis or thrombocytopenia, or fetal growth restriction). Adequate and early treatment of hypertension during pregnancy is of major importance, as severe hypertension is associated with an increased risk of (pre)eclampsia and hemolysis, elevated liver enzymes, and a low platelet count (HELLP) syndrome, leading to an increased maternal and perinatal morbidity and mortality [19]. It should be noted that it has not been proven that blood pressure control lowers this risk [20]. Commonly used antihypertensive drugs in younger patients angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are contraindicated during pregnancy because of increased risk for fetal renal damage, which seems even higher after exposure to ARBs than that to ACE inhibitors [21]. Currently, methyldopa, labetalol, and nifedipine are considered safe to use during pregnancy and therefore recommended in guidelines [22] [23]. However, for example, beta-blocker use has been associated with hypoglycaemia, which, although rare, can cause severe brain injury in neonates postpartum upon exposure via placental transfer [24, 25]. Furthermore, beta-blocker exposure during pregnancy has been associated with preterm birth, newborns small for gestational age, and perinatal mortality [26, 27]. However, labetalol, a beta-blocker with also alpha blockade, has not been associated with the adverse neonatal outcomes that other beta-blockers are associated with. The mechanisms of action and metabolic routes of methyldopa, labetalol, and nifedipine in nonpregnant adults are described in Supplementary Table 1 [28–39]. Nevertheless, evidence-based PK adjusted dosages for optimizing safe and effective treatment of hypertension in pregnant women are yet lacking. Methyldopa, labetalol, and nifedipine are considered safe to use during pregnancy, and therefore, the fetal/maternal ratio of these drugs is expected < 1, which means that fetal accumulation does not occur.
The aim of this systematic review was to generate a complete overview of the evidence on the PK of the antihypertensive drugs methyldopa, labetalol, and nifedipine throughout pregnancy, after which knowledge gaps were identified. Our ultimate goal was to direct future research aiming for personalized medicine dosing of these drugs in pregnant women.
Methods
Protocol and registration
The protocol for this systematic review was registered in the International prospective register of systematic reviews (PROSPERO) and published on April 11, 2019 (registration number: CRD42019128415) [40]. To improve the reporting of this systematic review, the PRISMA checklist was used [41].
Eligibility criteria
A systematic search was performed to retrieve studies on the PK throughout pregnancy of methyldopa, labetalol, and nifedipine. Participants included pregnant women of all gestational ages (when possible) compared with nonpregnant women or women in the postpartum period. The outcome of a study should include plasma concentration–time data and/or PK parameters (e.g., elimination half-life (t1/2), clearance (CL), volume of distribution (Vd), area under the plasma drug concentration–time curve (AUC), maximum serum concentration (Cmax), and time at which the maximum serum concentration was reached (tmax)) in pregnant women. Ex vivo human placental perfusion model studies were also eligible for inclusion. Furthermore, amniotic fluid and fetal (umbilical cord) blood drug concentrations were included in this systematic review due to its relevance for describing fetal PK. Drug fractions in the amniotic fluid may have been renally cleared by the fetus to the amniotic cavity, and can be reabsorbed by swallowing the amniotic fluid. Eligible studies were randomized controlled trials, observational studies, and case reports. No publication date restrictions were applied. The search was restricted to English studies only.
Search strategy
The systematic search was conducted on August 2, 2022, in Embase, Medline Ovid, Web of Science, Cochrane Library, and Google Scholar. Keywords were methyldopa, labetalol, nifedipine, pharmacokinetics, pregnancy, and placenta. The detailed search strategy is outlined in Appendix 1. References of included studies were checked for relevant studies to be potentially included in this systematic review.
Study selection and data extraction
Titles and abstracts of the retrieved studies were screened for relevance, after which full-texts of potentially eligible studies were obtained. Studies not meeting the study aim and inclusion criteria were excluded. The study selection was performed independently by two investigators (DV, PM). In case of disagreement, a third author (JV) was consulted. Data extraction from the reports was performed independently by two investigators (DV, PM) and verified on similarity.
Results
Study selection and data extraction
A total of 2070 records were identified. After removal of duplicates, a total of 1459 references remained of which title and abstract were screened (Fig. 1). Based on this screening, full-texts were assessed for 67 studies, to retain 30 included PK studies: 2 on methyldopa, 12 on labetalol, and 16 on nifedipine. The most common reason for exclusion was that studies investigated pharmacodynamics (PD) only and PK data were not available. No additional records were found from references of included studies.
Fig. 1.
Flow diagram screened studies. Abbreviations: PD, pharmacodynamics; PK, pharmacokinetics
Study characteristics
Table 1 provides the characteristics of the 30 included PK studies. The number of subjects per study ranged from 9 to 12 for methyldopa, 1 to 57 for labetalol, and 5 to 40 for nifedipine. Three out of the 30 included studies were physiologically based pharmacokinetics (PBPK) studies, all three concerning nifedipine. One study reported data of the first trimester, three of the second trimester, twenty-two of the third trimester, and nine around delivery. The PK parameters of methyldopa, labetalol, and nifedipine derived from literature are provided in Tables 2, 3, 4, and 5, respectively. Fetal side effects were not present [42] or (in most studies) not described.
Table 1.
Study characteristics of the included studies. Studies are ordered by drug, indication/type of study, and year
| Ref | Study indicated by author (year of publication) | Drug | Country | Dose | Route of administration | Indication (or ex vivo) | Number of subjects | Samples | Gestational age (weeks) | Statistical approach |
|---|---|---|---|---|---|---|---|---|---|---|
| [43] | Jones HM et al. (1978) | Methyldopa | UK | 750–2000 mg/day | Oral | Hypertension | 12 | 30 | Unknown | Other*** |
| [44] | Jones HM et al. (1979) | Methyldopa | UK | 750–2000 mg/day | Oral | Hypertension | 9 | 28 | 33.9 (mean) | Other*** |
| [54] | Schneider H et al. (1988) | Labetalol | Switzerland | Ex vivo | Ex vivo | Ex vivo | 5 | Ex vivo 5 studysize*2 maternal and fetal*12 time points = 120 | Unknown (healthy placentas from term deliveries) | Other*** |
| [53] | Nandakumaran M et al. (1989) | Labetalol | Kuwait | Ex vivo | Ex vivo | Ex vivo | 6 | Ex vivo 6 study size*2 maternal and fetal*6 time points = 72 | Unknown (healthy placentas from term deliveries) | Other*** |
| [47] | Rubin PC et al. (1983) | Labetalol | Scotland | 50 mg single dose | Intravenous | Hypertension | 20 | 20 (subjects) * 15 (time points) = 300 | 33–38 (range) | popPK |
| [55] | Nylund L et al. (1984) | Labetalol | Sweden & Kuwait | 200 mg/6 h | Oral | Hypertension | 7 | 22 | Unknown | Other*** |
| [49] | Lunell NO et al. (1985) | Labetalol | Sweden | 600––1200 mg/day | Oral | Gestational hypertension | 8 | 32 | 34.4 ± 12.4 (mean ± SD) | Other*** |
| [48] | Rogers RC et al. (1990) | Labetalol | USA | 100 mg/8 h | Oral | Gestational hypertension | 8 | Unknown | Unknown | NCA |
| [46] | Saotome et al. (1993) | Labetalol | Japan | 150–450 mg/12 h | Oral | Hypertension | 7 | 7*7 = 49 | 34–37 (range) | NCA |
| [51] | Boulton DW et al. (1999) | Labetalol | USA | 100 mg single dose | Oral | Hypertension | 4 | 4 (subjects) * 2(maternal andumbilical) = 8 | 37–40 (range) | Other*** |
| [52] | Carvalho et al. (2009) | Labetalol | Brazil | 100 mg single dose | Oral | Hypertension | 1 | Human 13 | Unknown | popPK |
| [45] | Carvalho et al. (2011) | Labetalol | Brazil | 100 mg vs. 40 mg | Oral vs. intravenous | Hypertension in patients with diabetes | 30 | 30 (subjects * 17 (time points iv) + 30 * 16 (time points oral administration)= 990 | 28.9–40.0 (range) | popPK |
| [42] | Uematsu et al. (2013) | Labetalol | Japan | 50–100 mg/8 h | Oral | Gestational hypertension | 29 | 58 |
36.3 ± 3.5 (mean ± SD) |
popPK |
| [50] | Fischer et al. (2014) | Labetalol | USA | 50–2400 mg/day | Oral | Chronic/gestational hypertension | 57 | 649 | 20 (11–39) (mean (range)) | popPK |
| [62] | Poranen AK et al. (1998) | Nifedipine | Finland | Ex vivo | Ex vivo | Ex vivo | 5 | Ex vivo 5*16 = 80 | 40.4 (39–42) (mean (range)) | NCA |
| [57] | Pirhonen JP et al. (1990) | Nifedipine | Finland | Single dose of 20 mg | Oral | Normotensive | 10 | 10 (subjects) * 5 (time points) = 50 | 38.8 (37–39) (mean ((range) | Other*** |
| [61] | Manninen AK et al. (1991) | Nifedipine | Finland | 10 mg/8 h | Oral | Hypertension | 11 | 66 | 36 (31–39) (mean ((range) | Other*** |
| [65] | Prevost RR et al. (1992) | Nifedipine | USA | 10 mg/6 h | Oral | Gestational hypertension | 15 | approx. 15*15 = 225 | 32.1 ± 2.7 (mean ± SD) | NCA |
| [66] | Filgueira et al. (2015) | Nifedipine | Brazil | 20 mg/12 h | Oral (slow-release) | Hypertension | 12 | approx. 12*30 = 360 | 36.1 ± 1.7 (mean ± SD) | NCA |
| [39] | Filgueira et al. (2017) | Nifedipine | Brazil | 20 mg/12 h | Oral (slow-release) | Hypertension | 22 | 22*23 = 506 | Control 39.1 (38.7–39.5); case (N = 10) 36.9 (35.2–38.4) (mean ((range) | NCA |
| [63] | Ferguson IJE et al. (1989) | Nifedipine | USA | 20 mg/6 h | Oral and sublingual | Preterm labor | 13 | 9 time points at every study day per subjectt | Unknown | Other*** |
| [67] | Marin TZ et al. (2007) | Nifedipine | Switzerland | 4 × 10 mg* followed by 1 × 60 mg | Oral (capsules and continuous release) | Preterm labor | 24 | 24*1 = 24 | 22–34 (range) | Other*** |
| [58] | Papatsonis DNM et al. (2007) | Nifedipine | Netherlands | 4 × 10 mg* followed by 1 × 20 mg | Oral (capsules and slow-release tablet) | Preterm labor | 5 | 5 (subjects) * 18 (time points) = 140 | 31.3 ± 0.9 (30–33 4/7) (mean ± SD (range)) | Other*** |
| [59] | Silberschmidt AL et al. (2008) | Nifedipine | Switzerland | 30–150 mg/day | Oral | Preterm labor | 40 | 40 (subjects) * 5 (time points) = 200 | 34.7 ± 0.8 (mean ± SD) | Other*** |
| [60] | Haas DM et al. (2012) | Nifedipine | USA | 4 × 10 mg* and 2 × 20 mg | Oral (capsules and slow-release tablet) | Preterm labor | 20 | 20 (subjects) * 8 (time points) = 160 | 29.7 ± 2.7 (24–34) (mean ± SD (range)) | NCA |
| [64] | Haas et al. (2013) | Nifedipine | USA | At SS: 10–20 mg/6–8 h | Oral (immediate-release) | Preterm labor | 14 | 9 time points at every study day per patient | 32 ± 4 (24–36) (mean ± SD (range)) | NCA |
| [56] | Ter Laak et al. (2015) | Nifedipine | Netherlands | 20 mg/6 h vs. placebo | Oral (slow-release tablet) | Preterm labor | 11 | 11 (subjects) * 7 (time points) = 77 | 26–32 2/7 (range) | popPK |
| [71] | Ke AB et al. (2012) | Nifedipine | USA | 10 mg/6 h | Oral | Gestational hypertension | ** | PBPK model | Unknown | PBPK |
| [69] | Quinney et al. (2012) | Nifedipine | USA | At SS: 10–20 mg/6–8 h | Oral | Preterm labor | ** | PBPK model | Unknown | PBPK |
| [68] | Dallmann A et al. (2018) | Nifedipine | Germany | NA | Oral | Unknown | ** | PBPK model | Unknown | PBPK |
Ref reference number, UK United Kingdom, USA United States of America, h hours, SS steady state, g gram, mg milligram, vs. versus, T time, kg kilograms, PBPK physiologically based pharmacokinetics, popPK population pharmacokinetics, NCA noncompartmental analysis
*T = 0, 15, 30, 45 min; **No new patient data is generated; ***Only concentrations reported
Table 2.
Results of fetal (cord) plasma/maternal plasma and amniotic fluid/maternal plasma ratios of methyldopa
| N | Fetal (cord) plasma/maternal plasma | Amniotic fluid/maternal plasma | Dosage | Gestational age | |||||
|---|---|---|---|---|---|---|---|---|---|
| Free | Sulfate conjugated | Total | Free | Sulfate conjugated | Total | ||||
| Jones et al. [43] | 12 | 1.19 (N = 12) | 0.79 (N = 12) | 0.99 (N = 12) | 1.0 (N = 6) | 2.0 (N = 6) | 1.23 (N = 6) | 750–2000 mg/day | Unknown |
| Jones et al. [44] | 9 | 0.93 (N = 4) | 1.49 (N = 4) | 0.63 (N = 5) | 2.04 (N = 2) | 6.67 (N = 2) | 3.85 (N = 2) | 750–2000 mg/day | 33.9 (mean) |
Values are reported as mean ratios. In original articles, maternal plasma/fetal (cord) plasma and maternal plasma/amniotic fluid ratios were given; for consistency, this was converted to fetal (cord) plasma/maternal plasma and amniotic fluid/maternal plasma ratios
Jones HM et al. [43]. Total amniotic fluid concentrations ranged from 200 to 3600 ng/mL with a dose of 250 mg/8 h–500/6 h at delivery, 4–12 h after the last dose of methyldopa
Jones HM et al. [44]: Total amniotic fluid concentrations ranged from 1580 to 2520 ng/mL with a dose of 500 mg/12 h–500/6 h at delivery, 4–28 h after the last dose of methyldopa
Table 3.
Results of pharmacokinetic parameters of labetalol
| Pharmacokinetic parameter (unit) | Rogers et al. [48] | Saotome et al. [46] |
|---|---|---|
| N | 8 | 7 |
| Dosage | 100 mg/8 h | 150–450 mg/12 h |
| Elimination half-life (hours) | 1.7 ± 0.27 | 5.8 ± 0.3 (4.3–6.9*) |
| Clearance (mL/kg/min) | 21.8 ± 6.8 | 43.7 ± 5.2 (31.9–73.3*) |
| Time of maximum serum concentration (minutes) | 20 | NA |
| Tmax with food ingestion (minutes) | 60 | Approximately 60 |
Values are mean ± standard deviation
*is a range
Table 4.
Results of fetal/maternal plasma ratios of nifedipine
| Study | N | Indication | F/M ratio | A/M ratio | Dose | Gestational age |
|---|---|---|---|---|---|---|
| Poranen et al. [62] | 5 | Ex vivo (placental transfer) | 0.054 ± 0.020 | NA | Ex vivo | 40.4 (39–42) (mean (range)) |
| Pirhonen et al. [57] | 10 | Normotensive/research | 0.76 | NA | Single dose of 20 mg | 38.8 (37–39) (mean ((range) |
| Manninen et al. [61] | 11 | Hypertension | 0.8 ± 0.1 | 0.3 ± 0.1 | 10 mg/8 h | 36 (31–39) (mean ((range) |
| Prevost et al. [65] | 15 | Pregnancy-induced hypertension | 0.93 ± 0.2 | 0.56 ± 0.1 | 10 mg/6 h | 32.1 ± 2.7 (mean ± SD) |
| Filgueira et al. [66] | 12 | Hypertension | NA | 0.05 (0.03–0.06) | 20 mg/12 h | 36.1 ± 1.7 (mean ± SD) |
| Filgueira et al. [39] | 22 (12 controls vs. 10 T2DM) | Hypertension | 0.53 (T2DM 0.44) | 0.05 (T2DM 0.05) | 20 mg/12 h | control 39.1 (38.7–39.5); case (N = 10) 36.9 (35.2–38.4) (mean ((range) |
| Silberschmidt et al. [59] | 40 | Preterm labor | 0.77 | NA | 30–150 mg/day | 34.7 ± 0.8 (mean ± SD) |
Values are mean ± standard deviation
T2DM type 2 diabetes mellitus, F/M ratio umbilical serum/maternal serum ratio, A/M ratio amniotic fluid serum/maternal serum ratio, NA not applicable
Table 5.
Pharmacokinetic parameters of nifedipine as tocolytic
| Study | Ferguson et al. [63] | Marin et al. [67] | Papatsonis et al. [58] | Silberschmidt et al. [59] | Haas et al. [60] | Haas et al. [64] | Ter Laak et al. [56] |
|---|---|---|---|---|---|---|---|
| Oral dose | 10–40 mg in first hour followed by 20 mg/4–6 h (sublingual) | * followed by 60 mg continuous release nifedipine | * followed by 20 mg slow release (T = 105 min) | 30–150 mg/day tablets with sustained release | * and 1 × 20 mg (T = 105 min) | 10–20 mg/6–8 h | 20 mg/6 h vs. placebo |
| Elimination half-life (t1/2) | 81 min (49–137) | NA | NA |
maternal 17.4 h (95% CI: 13.9–21.7); fetal (umbilical cord) 20.4 h (95% CI: 15.7–26.3) |
NA | 1.68 ± 1.56 h | 2–5 h |
| Volume of distribution (Vd) | NA | NA | NA | NA | NA | NA | 6.2 ± 1.9 L/kg |
| Time of maximum serum concentration (Tmax) | NA | NA | 1.2 ± 0.1 h | `NA | 1 h | NA | NA |
| Maximum serum concentration | 96.7 ± 45.3 (23.4–197.9) ng/mL | NA | 127 ± 44 | NA | NA | NA | NA |
| Area under the plasma drug concentration–time curve (AUC) | NA | NA | NA | NA | Mean 86.1 ± 61.1 µg*h/L | AUC0-6 h: 207 ± 138 µg*h/L | NA |
| Maternal mean nifedipine concentration | 7.2 ± 5.5 ng/mL after 20 mg nifedipine orally every 6 h | 32.9 ± 25.1 ng/mL (6–101 ng/mL) | 67.4 ± 28.4 ng/mL | NA | NA | NA | 16.8 ng/mL (median concentration at SS) |
| Neonatal serum plasma concentration after delivery | 1.8–29.5 ng/mL (N = 5) | NA | NA | NA | NA | NA | NA |
Given means are reported ± SD unless stated otherwise
NA not applicable, h hours
*4 × 10 mg nifedipine (T = 0, 15, 30, 45 min)
The most important reported ex vivo (placental perfusion model) and in vivo (absorption, distribution, metabolism, excretion, and fetal (cord blood)/maternal ratio data are described below for all drugs).
Methyldopa
In vivo
Only two studies by the same group reported on the PK during pregnancy (delivery) and placental transfer of methyldopa (Table 2) [43, 44]. The first study described the free, sulfated, and total methyldopa concentration of 12 pregnant women in maternal plasma at delivery (N = 12), fetal (umbilical cord) plasma (N = 12), and amniotic fluid (N = 6) [43]. Methyldopa undergoes conjugation with sulfate to improve renal excretion of the drug. Total maternal plasma concentrations ranged between 200 and 2400 ng/mL and fetal (umbilical cord) plasma concentrations ranged between 250 and 2700 ng/mL following a dose ranging from 250 mg/8 h to 500 mg/6 h and a time of delivery of 2–16 h after the last dose of methyldopa. The fetal/maternal plasma ratio of methyldopa (N = 12) was 1.19 (free), 0.79 (sulfate conjugated), and 0.99 (total). The calculated ratios showed that both free and conjugated methyldopa concentrations were similar in maternal and fetal (cord) plasma. The amniotic fluid/maternal plasma ratio of methyldopa (N = 6) was 0.77 (free), 2.0 (conjugated), and 1.23 (total). Overall, the total methyldopa concentration in the amniotic fluid was 19% higher than the maternal plasma concentrations. The conjugated concentration in amniotic fluid was on average two times higher than the conjugated concentration in maternal plasma and in five out of six cases noticeable higher than the free form in amniotic fluid.
The second study described, similar to the previous study, the concentration of free, sulfate conjugated and total methyldopa in maternal plasma (N = 5), fetal (umbilical cord) plasma (N = 7), amniotic fluid (N = 4), and neonates (N = 7) [44]. Total maternal plasma ranged from 422 to 3543 ng/mL and fetal (umbilical cord) plasma from 154 to 1802 ng/mL with a dose range of 250 mg/6 h–500 mg/6 h and a time of delivery after the last dose of methyldopa of 4–14 h. Total fetal/maternal (cord) plasma ratio was 0.9 (free; N = 4), 0.5 (conjugated; N = 4), and 0.6 (total; N = 5). Total amniotic fluid concentrations ranged from 1580 to 2520 ng/mL with a dose of 500 mg/12 h–500 mg/6 h and a time of delivery after the last dose of methyldopa of 4–28 h. Amniotic fluid/maternal plasma ratio of methyldopa was 2.0 (free; N = 2), 6.7 (conjugated; N = 2), and 3.8 (total; N = 2). Both studies show disparities, for instance, for the maternal plasma to fetal plasma for sulfate conjugated methyldopa ratio (0.79 vs. 1.49). The authors do not give an explanation for these differences between their studies, although they speculate whether these higher conjugated drug levels are due to fetal conjugation or to placental transfer, which might also vary between fetuses.
Labetalol
Eleven studies reported on the PK of labetalol during pregnancy and its placental transfer [42, 45–55].
Ex vivo (placental transfer)
Two out of the 11 studies on labetalol were ex vivo studies using isolated human cotyledons from normal pregnancies with term deliveries to investigate the placental transfer of labetalol [53, 54]. Both studies showed placental transfer of labetalol and placental tissue binding. Schneider et al. (N = 5) reported a placental transfer at steady state of 16.6% ± 4.6% [54]. After bolus injection, placental transfer of labetalol was clearly suppressed, as a result of high placental tissue binding [54]. Different albumin levels (0.02 and 4.0 g/dl) had little effect on the labetalol transfer [54]. Nandakumaran et al. (N = 6) showed a ratio of labetalol transfer of 5% ± 0.7% and compared to antipyrine 32% ± 2.8% at steady-state perfusion conditions [53].
In vivo
The reported studies on the PK during pregnancy and placental transfer of labetalol used different outcome measures for PK, which makes a clear overview difficult. Studies assessed absorption, distribution, metabolism, and excretion in pregnant women. The largest studies are described below.
Rubin et al. investigated the PK of labetalol in ten hypertensive pregnant women before and after delivery and ten normotensive women [47]. Vd and CL were not significantly different in these three groups [47]. Nylund et al. determined labetalol plasma levels in seven pregnant women [55]. Measured plasma levels in pregnant women were generally lower compared with nonpregnant women with a similar dose in earlier studies. The fetal/maternal labetalol concentration ratio was about 0.5 in four out of five investigated patients and in the other patient about 1 [55]. A similar ratio (0.67) was found in a Japanese study in 29 patients [42]. Lunell et al. studied transfer of labetalol into the amniotic fluid [49]. In six of eight patients, the labetalol concentration in amniotic fluid was lower than that in maternal plasma.
Rogers et al. and Saotome et al. determined PK parameters of labetalol in pregnant women with different results for elimination half-life and clearance (Table 3) [46, 48]. For instance, elimination half-life ranged from 1.7 to 5.8 h; even while quite different, they are both short implicating that dosing three times daily is optimal. The umbilical cord fetal/maternal serum ratio was 0.5 ± 0.15 and amniotic fluid/maternal serum ratio 0.16 ± 0.13 in Rogers et al.; Saotome et al. mainly focused on the relation between labetalol levels and blood pressure [46, 48]. Boulten et al. and Carvalho et al. studied the transplacental distribution of labetalol stereoisomers during pregnancy and at delivery [51, 52]. The pharmacological active stereoisomers (RR and SR) had a lower plasma concentration compared to the inactive stereoisomers (SS and RS) [52]. The ratio AUC(RR)/AUC(SS) was 0.5 [52]. The inactive stereoisomer, SS, was present in the highest concentration in both maternal plasma and fetal (cord) plasma in all four subjects when labetalol was detectable [51]. The effect of gestational diabetes mellitus on the stereoselective kinetic disposition and metabolism was assessed by Carvalho et al. because diabetes mellitus can alter enantioselective PK processes potentially leading to a more outspoken blood pressure decrease in patients with diabetes [45]. Indeed, the AUC of the SS and SR isomers were higher in the diabetic women compared to the nondiabetic after oral administration [45]. The PK of labetalol was not stereoselective after intravenous administration [45]. Fischer et al. studied the influence of gestational age and body weight on the PK of labetalol in pregnancy [50]. Oral clearance (CL/F) ranged from 1.4-fold higher at 12 weeks gestational age and 1.6-fold higher at 40 weeks compared to postpartum (up to 12 weeks after delivery) CL/F; data was collected within the same patient [50]. The apparent Vd of the central compartment during pregnancy was 1.9-fold higher [50]. Plasma proteins concentrations, alpha-1 acid glycoprotein and albumin, were lower during pregnancy compared postpartum as both are decreased during pregnancy, although not significant in this cohort [50].
Nifedipine
Sixteen studies reported on nifedipine PK in pregnant women [38, 39, 56–69]. Six out of these 16 studies reported on the placental transfer investigating the fetal/maternal ratio of nifedipine plasma concentrations (Tables 4 and 5) [39, 59, 61, 62, 65, 66]
Ex vivo (placental transfer)
One out of the 16 studies on nifedipine was an ex vivo study published in 1998 by Poranen et al. using five isolated human placental cotyledons (Table 4) [62]. The mean ± SD placental CL of nifedipine at steady state was 0.54 ± 0.20 mL/min [62]. Placental transfer of nifedipine was 5.4% ± 2.0% and the CL index (the ratio between nifedipine and the internal standard antipyrine) 0.41 [62]. The recovery of the added nifedipine in the perfusion buffer was 51% ± 9.3%, although nifedipine bound to placental tissue was not measured [62].
In vivo
Normotensive
One out of the 16 studies on nifedipine investigated the PK of ten normotensive healthy pregnant women after a single oral dose of 20 mg nifedipine [57]. The mean maternal serum concentration of nifedipine before birth was 38.3 ± 26.6 ng/mL (70–90 min after intake) and at birth (on average 165 min (range 150–180 min) after intake) 17.6 ± 12.7 ng/mL [57]. The mean concentration in the umbilical vein (afferent) was 13.1 ± 14.0 ng/mL and in the umbilical artery (efferent) 10.0 ± 9.4 ng/mL [57]. Umbilical venous fetal/maternal ratio of nifedipine 2–3 h after nifedipine intake was 0.76 [57]. After one blood circulation of the drug in the fetus, approximately 25% of nifedipine had distributed in the fetal tissues [57].
Hypertension
Five out of the 16 studies on nifedipine studied the PK in hypertensive pregnant women [39, 61, 65, 66], of which one developed a PBPK model as described below [70].
Manninen et al. studied nifedipine concentrations in maternal and umbilical fetal serum, amniotic fluid, breast milk, and urine of mothers and offspring (Table 4) [61]. The mean (± SD) serum concentration in 11 third trimester pregnant women (4.3 ± 3.1 ng/mL) was lower than that in 6 different nonpregnant controls (12.0 ± 2.9 ng/mL) with the same dose of nifedipine (10 mg three times daily) [61].
The fetal/maternal serum ratio was 0.8 ± 0.1 and the amniotic fluid serum/maternal serum ratio 0.3 ± 0.1 at delivery [61].
Prevost et al. investigated the disposition of nifedipine in pregnant women using nifedipine 10 mg every 6 h (mean gestation 32.1 weeks; Table 4) [65]. At steady state, the Cmax was 38.6 ± 18 ng/mL 40 min after ingestion, t1/2 1.3 ± 0.5 h, mean CL/F 2.0 ± 0.8 L/h/kg, and the AUC 83.2 ± 42.6 ng*h/mL [65]. The umbilical cord fetal/maternal serum ratio was 0.93 ± 0.2 and the amniotic fluid/maternal serum ratio 0.56 ± 0.15 [65]. Filgueira et al. reported the following PK parameters in pregnant women using nifedipine 20 mg every 12 h: AUC0-12 250 ng*h/mL, CLt/F 89.2 L/h, Vd/F 600 L, and t1/2 5.1 h (Table 4) [66]. The amniotic fluid/plasma concentration ratio was very low: on average 0.05 ranging from 0.03 to 0.06 based on AUC0−12 [66]. In a later study, the same research group tested the effect of type 2 diabetes mellitus (T2DM) on the PK and transplacental transfer of nifedipine in hypertensive pregnant women using the same dosing regimen (Table 4) [39]. There was no effect of T2DM on the PK or placental transfer of nifedipine [39].
Tocolysis
Eight out of the 16 studies on nifedipine studied the PK of pregnant women undergoing tocolysis [56, 58–60, 63, 64, 67, 69] (Table 5) of which one developed a PBPK model as described below [69].
In a study by Ferguson et al., PK parameters of nifedipine for tocolysis were measured after sublingual administration and oral administration (Table 5) [63]. Nifedipine plasma concentrations were also measured in 11 neonates at delivery after multiple doses. In six of them, the nifedipine concentration was undetectable (below LLQ) and in the other five newborns values ranged from 1.8 to 29.5 ng/mL [63]. Results of comparable studies of Marin et al. and Papatsonis et al. can be found in Table 5 [58, 67]. For nonpregnant women, a Vd and t1/2 have been described in the literature, 1.2 ± 1.3 L/kg [58] and 6–11 h, respectively. Silberschmidt et al. determined the nifedipine concentration and other PK parameters (Table 5) in maternal and fetal blood after tocolysis with gastrointestinal therapeutic system (GITS) tablets, a modified release formulation with sustained release. The mean fetal plasma/maternal plasma ratio was 0.77 [59]. The linear regression between maternal and fetal concentrations was significant [59]. Haas et al. performed a pilot study about the impact of genotype on PK of nifedipine indicated for tocolysis; results are shown in Table 5 [60]. The nifedipine/oxidized nifedipine (nif/ox) AUC ratio was 2.83 ± 4.20 [60]. Expression of CYP3A5 (defined as at least one CYP3A5*1 allele, 5/20 subjects) did have a statistically significant effect on nifedipine exposure (expresser (exp): 139.5 ± 97.3 ng/mL/h vs. nonexpressers (non): 68.3 ± 31.8 ng/mL/h, p = 0.02) and the nif/ox ratio (exp: 6.33 ± 7.82 vs. non: 1.67 ± 0.834, p = 0.03) [60]. Four subjects (2 exp and 2 non) used CYP3A inhibiting co-medication and had significantly higher nifedipine exposure (p < 0.0001) independent of CYP3A5 genotype [60]. These results were confirmed in a later study (Table 5) [64]. The CL/F was significantly different (p = 0.007) between high and low expressers of CYP3A5 (232.0 ± 37.8 µg/mL vs. 85.6 ± 45 µg/mL, respectively) [64]. Furthermore, the average nifedipine plasma concentration, Cl/F, and Vd/F of the high and low expressers were significantly different [64]. Ter Laak et al. described the PK (t1/2, Vd, and median nifedipine concentration at steady state) of maintenance slow-release nifedipine as tocolytic (Table 5) [56].
Physiologically based pharmacokinetics (PBPK)
Three out of the 16 studies on nifedipine developed a PBPK model [38, 68, 71]. Ke et al. [71] developed a PBPK model based on third trimester data [65]. The mean CL/F of nifedipine at steady state was almost doubled during pregnancy (145.7 L/h vs. 74.4 L/h) [71], which may have implications for the pharmacodynamic effects of nifedipine in pregnant women if the same dosing is applied. The PBPK model predicted the following nonpregnant vs. third trimester pregnant data of nifedipine (observed ratio): mean steady state AUC ratio of 2.1 (2.0), Cmax 2.1 (1.8), and Cmin 2.4 (3.1) [71]. Quinney et al. performed a semi-mechanistic metabolism model of midazolam and nifedipine (based on Haas et al. CYP3A substrates, in obstetric patients) [38, 64]. Nifedipine steady-state AUC predicted by the developed model was underestimated by 11% (210 (121–299) ng*h/mL vs. 237 (224–253) ng*h/mL) and the Cmax was overestimated by 3% (178 (166–188) ng/mL vs. 184 (90–308) ng/mL) [38]. The third PBPK model was developed by Dallmann et al. to predict the PK during pregnancy of drugs metabolized via several enzymatic pathways [68]. The Cmax of both pregnant and nonpregnant women was underestimated by their model [68]. Ninety-three percent of the predicted mean plasma concentrations of nifedipine in pregnant women fell within the twofold error range and 54% within the 1.3-fold error rate.
Discussion and conclusion
This is the first systematic review that provides a complete overview of what is currently known on PK of the most commonly used antihypertensive drugs throughout pregnancy: methyldopa, labetalol, and nifedipine. Since variation of the fetal/maternal ratio of methyldopa, labetalol, and nifedipine is expected to be high, values < 0.1 (limited transfer), 0.1–1 (transfer), and > 1 (fetal accumulation) were considered concordant. All the identified ratios were between 0.1 and 1 which means that there is placental transfer of the three investigated drugs, but no fetal accumulation. Identified parameters for the same drug could vary substantially between studies. We assume that the small sample sizes and the challenges of sampling before, during, and after delivery including amniotic fluid may have led to uncertainties and discrepancies, including the fact that often point measurements instead of preferable AUC estimates were available.
Especially studies on methyldopa are scarce, while this is still considered first-line treatment of hypertension during pregnancy. For labetalol and nifedipine, the reports were highly variable in the investigated dosages, indications, patients, PK estimates, and study designs (ex vivo and in vivo). Furthermore, the studies differed in quality, methods to describe the PK, patient size, the number of samples, and the timing of sampling in relation to the dose as well as the gestational age. A few studies also described the concentration of the drug in amniotic fluid, for example, in relation to maternal plasma which might lead to prolonged exposure. The number of studies was low and data was mostly not homogeneous, often lacking ratios between maternal and fetal plasma concentrations, which made it difficult to systematically present data or perform meta-analyses. Relevant differences in PK parameters of the same drug were reported; however, it should be considered that PK parameters such as AUC and Cmax are dose dependent. Despite the frequent use of these three drugs during pregnancy according to international and national protocols, appropriate descriptions of the impact of pregnancy on the population PK are still sparse and inconsistent, while indispensable to truly assess the pharmacodynamics of these drugs during pregnancy.
Although methyldopa is first-choice drug for hypertensive disorders in pregnant women in many countries, only two studies reported on methyldopa PK in pregnant women. The free fetal/maternal ratio of methyldopa was as expected in the range of 1 [43, 44]. In amniotic fluid, the concentration of conjugated, i.e., inactive, methyldopa was higher than that of the free form. This can be explained by either less reabsorption of the conjugated form by the fetus or more renal excretion of the free form by the fetus. Both free and conjugated methyldopa were lower in arterial umbilical cord (fetal) plasma compared to venous umbilical cord (fetal) plasma which indicated that the fetus eliminates both forms and is actively involved in methyldopa disposition.
Three studies reported on in vivo placental transfer of labetalol [46, 48, 55]. Fetal/maternal serum ratios were about 0.5 with one unexplained outlier of about 1. Labetalol is a lipid-soluble drug which makes it easier to pass the placenta compared to a hydrophilic component by passive diffusion. Furthermore, there is a large unexplainable difference in the reported clearance values of labetalol [46, 48]. Studies that also addressed the ratio between active and inactive stereoisomers concluded that inactive isoforms seem to predominate both in maternal and in fetal samples.
Five studies reported on the umbilical fetal/maternal serum ratio of nifedipine [39, 57, 59, 61]. Ratios ranged from 0.53 to 0.93, meaning there is placental transfer of nifedipine but no fetal accumulation. This was confirmed in an ex vivo placental transfer study, although the ratio was even lower here (0.054). Two studies by Haas et al. showed that CYP3A5 genotype influences the nifedipine concentrations when used as tocolytic [60, 64]. Due to these PK changes during pregnancy and placental differences per trimester, it can be clinically relevant to adjust dose and dosing interval of nifedipine for the different indications during pregnancy, especially in low expressors of CYP3A5 or differences activity of CYP3A4 due to pharmacogenetic variation or interactions (not specifically studied) [61].
More detailed knowledge about the PK of methyldopa, nifedipine, and labetalol may lead to better understanding of the impact on the PD including safety consequences for the developing fetus and the offspring during the life course. A fetus is assisted by the mother to clear the drug during intrauterine exposure by placental transfer back to the mother. From birth onwards, the newborn is fully responsible for the clearance, despite its still immature drug clearance capacity. This applies even more to preterm infants, while preterm birth is commonly seen after the maternal indications for which methyldopa, labetalol, and nifedipine were prescribed. Their drug clearance capacity is even more limited.
This review serves as a good basis to identify the need for future research with the ultimate goal to reach evidence-based dosing for this vulnerable population, including the developing placenta and fetus. Currently, dosing is empirical and based on PD of the mother, since our knowledge or understanding of PD or PK is too limited to guide prescription in pregnancy. Although major adverse events for the described drugs are scarce, combining PK and PD, required drug dosages might be further minimized, hereby potentially lowering exposure of the fetus and the newborn.
As a start towards evidence-based personalized dosing in the future, further studies combining therapeutic drug monitoring (PK) studies designed with contemporary approaches to get more homogenous data and PD by ways of monitoring hemodynamics and other health parameters of pregnant women including the breastfeeding phase and their offspring are needed [72]. For example, PBPK modeling is a promising approach to evaluate different dosing regimens in pregnant women, because it can predict the influence of the physiological changes in the body [15, 73]. From these data, personalized dosing based on maternal and pregnancy characteristics, if necessary combined with therapeutic drug monitoring, can be optimized. Evidence-based personalized dosing in the future can mean that dosing will be based on trimester, weight, and/or individual characteristics (like disease, genetic polymorphism) throughout gestation.
In general, including, instead of excluding, pregnant women in clinical trials on drugs commonly required during pregnancy would give the best information. More use of standardized ex vivo placental transfer models of different gestational ages (1st, 2nd, and 3rd trimester) or “placenta-on-a-chip” before clinical trials would make this safe and helps in dose finding [74].
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank Elise Krabbendam, Biomedical Information Specialist of the Erasmus MC University Medical Center, for helping with the systematic search strategy of literature.
Author contribution
DvdV and PM did the literature search and screening, helped by JV in case of discrepancies. JV had the idea to perform this research. DvdV, PM, and JV drafted the article. All authors critically revised the work.
Funding
This review was part of a research project funded by foundation “De Merel”.
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study. All data given are available in the original articles.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Systematic review registration number
The protocol for this systematic review was registered in the International prospective register of systematic reviews (PROSPERO) and published on April 11, 2019 (registration number: CRD42019128415).
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lupattelli A, Spigset O, Twigg MJ, Zagorodnikova K, Mardby AC, Moretti ME, Drozd M, Panchaud A, Hameen-Anttila K, Rieutord A, Gjergja Juraski R, Odalovic M, Kennedy D, Rudolf G, Juch H, Passier A, Bjornsdottir I, Nordeng H. Medication use in pregnancy: a cross-sectional, multinational web-based study. BMJ Open. 2014;4:e004365. doi: 10.1136/bmjopen-2013-004365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayad M, Costantine MM. Epidemiology of medications use in pregnancy. Semin Perinatol. 2015;39:508–511. doi: 10.1053/j.semperi.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glover DD, Amonkar M, Rybeck BF, Tracy TS. Prescription, over-the-counter, and herbal medicine use in a rural, obstetric population. Am J Obstet Gynecol. 2003;188:1039–1045. doi: 10.1067/mob.2003.223. [DOI] [PubMed] [Google Scholar]
- 4.Cea Soriano L, Bateman BT, Garcia Rodriguez LA, Hernandez-Diaz S. Prescription of antihypertensive medications during pregnancy in the UK. Pharmacoepidemiol Drug Saf. 2014;23:1051–1058. doi: 10.1002/pds.3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halpern DG, Weinberg CR, Pinnelas R, Mehta-Lee S, Economy KE, Valente AM. Use of medication for cardiovascular disease during pregnancy: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73:457–476. doi: 10.1016/j.jacc.2018.10.075. [DOI] [PubMed] [Google Scholar]
- 6.De Sousa MM, Hirt D, Urien S, Valade E, Bouazza N, Foissac F, Blanche S, Treluyer JM, Benaboud S. Physiologically-based pharmacokinetic modeling of renally excreted antiretroviral drugs in pregnant women. Br J Clin Pharmacol. 2015;80:1031–1041. doi: 10.1111/bcp.12685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rayburn WF, Farmer KC. Off-label prescribing during pregnancy. Obstet Gynecol Clin North Am. 1997;24:471–478. doi: 10.1016/S0889-8545(05)70317-X. [DOI] [PubMed] [Google Scholar]
- 8.Carbonne B, Winer N (2015) [Off-label treatments in obstetrics: tocolysis with calcium channel blockers]. Traitements hors AMM en obstetrique : tocolyse par les inhibiteurs calciques. Introduction. J Gynecol Obstet Biol Reprod (Paris) 44:295–6 [DOI] [PubMed]
- 9.Rasmussen SA, Jamieson DJ. Pregnancy, postpartum care, and COVID-19 vaccination in 2021. JAMA. 2021;325:1099–1100. doi: 10.1001/jama.2021.1683. [DOI] [PubMed] [Google Scholar]
- 10.Bianchi DW, Kaeser L, Cernich AN. Involving pregnant individuals in clinical research on COVID-19 vaccines. JAMA. 2021;325:1041–1042. doi: 10.1001/jama.2021.1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kazma JM, Van Den Anker J, Ahmadzia HK (2021) Pharmacoethics and pregnancy: overcoming the therapeutic orphan stigma. Br J Clin Pharmacol [DOI] [PubMed]
- 12.Pariente G, Leibson T, Carls A, Adams-Webber T, Ito S, Koren G. Pregnancy-associated changes in pharmacokinetics: a systematic review. PLoS Med. 2016;13:e1002160. doi: 10.1371/journal.pmed.1002160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andrew MA, Easterling TR, Carr DB, Shen D, Buchanan ML, Rutherford T, Bennett R, Vicini P, Hebert MF. Amoxicillin pharmacokinetics in pregnant women: modeling and simulations of dosage strategies. Clin Pharmacol Ther. 2007;81:547–556. doi: 10.1038/sj.clpt.6100126. [DOI] [PubMed] [Google Scholar]
- 14.Westin AA, Brekke M, Molden E, Skogvoll E, Castberg I, Spigset O. Treatment With antipsychotics in pregnancy: changes in drug disposition. Clin Pharmacol Ther. 2018;103:477–484. doi: 10.1002/cpt.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dallmann A, Mian P, Van den Anker J, Allegaert K. Clinical pharmacokinetic studies in pregnant women and the relevance of pharmacometric tools. Curr Pharm Des. 2019;25:483–495. doi: 10.2174/1381612825666190320135137. [DOI] [PubMed] [Google Scholar]
- 16.Jogiraju VK, Avvari S, Gollen R, Taft DR. Application of physiologically based pharmacokinetic modeling to predict drug disposition in pregnant populations. Biopharm Drug Dispos. 2017;38:426–438. doi: 10.1002/bdd.2081. [DOI] [PubMed] [Google Scholar]
- 17.Brown CM, Garovic VD. Drug treatment of hypertension in pregnancy. Drugs. 2014;74:283–296. doi: 10.1007/s40265-014-0187-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gallery ED. Hypertension in pregnancy. Practical management recommendations Drugs. 1995;49:555–562. doi: 10.2165/00003495-199549040-00006. [DOI] [PubMed] [Google Scholar]
- 19.Mammaro A, Carrara S, Cavaliere A, Ermito S, Dinatale A, Pappalardo EM, Militello M, Pedata R. Hypertensive disorders of pregnancy. J Prenat Med. 2009;3:1–5. [PMC free article] [PubMed] [Google Scholar]
- 20.Magee LA, von Dadelszen P, Singer J, Lee T, Rey E, Ross S, Asztalos E, Murphy KE, Menzies J, Sanchez J, Gafni A, Helewa M, Hutton E, Koren G, Lee SK, Logan AG, Ganzevoort W, Welch R, Thornton JG, Moutquin JM (2016) Group* CS. The CHIPS Randomized Controlled Trial (Control of Hypertension in Pregnancy Study): is severe hypertension just an elevated blood pressure? Hypertension 68:1153–59 [DOI] [PMC free article] [PubMed]
- 21.Bullo M, Tschumi S, Bucher BS, Bianchetti MG, Simonetti GD. Pregnancy outcome following exposure to angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review. Hypertension. 2012;60:444–450. doi: 10.1161/HYPERTENSIONAHA.112.196352. [DOI] [PubMed] [Google Scholar]
- 22.Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, Hall DR, Warren CE, Adoyi G, Ishaku S (2018) International Society for the Study of Hypertension in P. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension 72:24–43 [DOI] [PubMed]
- 23.Lam MTC, Dierking E. Intensive care unit issues in eclampsia and HELLP syndrome. Int J Crit Illn Inj Sci. 2017;7:136–141. doi: 10.4103/IJCIIS.IJCIIS_33_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burns CM, Rutherford MA, Boardman JP, Cowan FM. Patterns of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics. 2008;122:65–74. doi: 10.1542/peds.2007-2822. [DOI] [PubMed] [Google Scholar]
- 25.Stomnaroska O, Petkovska E, Jancevska S, Danilovski D. Neonatal hypoglycemia: risk factors and outcomes. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2017;38:97–101. doi: 10.1515/prilozi-2017-0013. [DOI] [PubMed] [Google Scholar]
- 26.Xie RH, Guo Y, Krewski D, Mattison D, Walker MC, Nerenberg K, Wen SW. Beta-blockers increase the risk of being born small for gestational age or of being institutionalised during infancy. BJOG. 2014;121:1090–1096. doi: 10.1111/1471-0528.12678. [DOI] [PubMed] [Google Scholar]
- 27.Meidahl Petersen K, Jimenez-Solem E, Andersen JT, Petersen M, Brodbaek K, Kober L, Torp-Pedersen C, Poulsen HE (2012) beta-Blocker treatment during pregnancy and adverse pregnancy outcomes: a nationwide population-based cohort study. BMJ Open 2 [DOI] [PMC free article] [PubMed]
- 28.Pariente G, Leibson T, Carls A, Adams-Webber T (2016) Pregnancy-associated changes in pharmacokinetics: a systematic review. journals.plos.org [DOI] [PMC free article] [PubMed]
- 29.Au WY, Dring LG, Grahame-Smith DG, Isaac P, Williams RT. The metabolism of 14 C-labelled -methyldopa in normal and hypertensive human subjects. Biochem J. 1972;129:1–10. doi: 10.1042/bj1290001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MacCarthy EP, Bloomfield SS. Labetalol: a review of its pharmacology, pharmacokinetics, clinical uses and adverse effects. Pharmacotherapy. 1983;3:193–219. doi: 10.1002/j.1875-9114.1983.tb03252.x. [DOI] [PubMed] [Google Scholar]
- 31.MacCarthy EP, Bloomfield SS, Goodman RP. Labetalol: a review of its pharmacology, pharmacokinetics, clinical uses and adverse effects. Pharmacotherapy. 1983;3:193–219. doi: 10.1002/j.1875-9114.1983.tb03252.x. [DOI] [PubMed] [Google Scholar]
- 32.Flenady V, Wojcieszek AM, Papatsonis DN, Stock OM, Murray L, Jardine LA, Carbonne B (2014) Calcium channel blockers for inhibiting preterm labour and birth. Cochrane Database Syst Rev CD002255 [DOI] [PMC free article] [PubMed]
- 33.Al Khaja KA, Sequeira RP, Alkhaja AK, Damanhori AH. Drug treatment of hypertension in pregnancy: a critical review of adult guideline recommendations. J Hypertens. 2014;32:454–463. doi: 10.1097/HJH.0000000000000069. [DOI] [PubMed] [Google Scholar]
- 34.Sibai BM. Treatment of hypertension in pregnant women. N Engl J Med. 1996;335:257–265. doi: 10.1056/NEJM199607253350407. [DOI] [PubMed] [Google Scholar]
- 35.Sorkin EM, Clissold SP, Brogden RN (1985) Nifedipine. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy, in ischaemic heart disease, hypertension and related cardiovascular disorders. Drugs 30:182–274 [DOI] [PubMed]
- 36.Buhs RP, Beck JL, Speth OC, Smith JL, Trenner NR, Cannon PJ, Laragh JH. The metabolism of methyldopa in hypertensive human subjects. J Pharmacol Exp Ther. 1964;143:205–214. [PubMed] [Google Scholar]
- 37.Tønnesen HH (1996) Photostability of drugs and drug formulations. London: Taylor and Francis Ltd
- 38.Quinney SK, Mohamed AN, Hebert MF, Haas DM, Clark S, Umans JG, Caritis SN, Li L (2012) A semi-mechanistic metabolism model of CYP3A substrates in pregnancy: predicting changes in midazolam and nifedipine pharmacokinetics. CPT Pharmacometrics Syst Pharmacol 1 [DOI] [PMC free article] [PubMed]
- 39.Filgueira GCDO, Filgueira OAS, Carvalho DM, Marques MP, Moisés ECD, Duarte G, Lanchote VL, Cavalli RC. Effect of type 2 diabetes mellitus on the pharmacokinetics and transplacental transfer of nifedipine in hypertensive pregnant women. Br J Clin Pharmacol. 2017;83:1571–1579. doi: 10.1111/bcp.13226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.www.crd.york.ac.uk/prospero
- 41.prisma-statement.org
- 42.Uematsu K, kobayahi E, Katsumoto E, Sugimoto M, Kawakami T, Terijima T, Maezawa K, Kizu J (2013) Umbilical cord blood concentrations of labetalol hydrochloride administered to patients with pregnancy induced hypertension, and subsequent neonatal findings. Hypertens Res Pregnancy 1:88–92
- 43.Jones HM, Cummings AJ. A study of the transfer of alpha-methyldopa to the human foetus and newborn infant. Br J Clin Pharmacol. 1978;6:432–434. doi: 10.1111/j.1365-2125.1978.tb04609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jones HM, Cummings AJ, Setchell KD, Lawson AM. A study of the disposition of alpha-methyldopa in newborn infants following its administration to the mother for the treatment of hypertension during pregnancy. Br J Clin Pharmacol. 1979;8:433–440. doi: 10.1111/j.1365-2125.1979.tb01022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carvalho TMJP, De Carvalho CR, Cunha SP, De Baraldi CO, Marques MP, Antunes NJ, Godoy ALPC, Lanchote VL. Influence of gestational diabetes mellitus on the stereoselective kinetic disposition and metabolism of labetalol in hypertensive patients. Eur J Clin Pharmacol. 2011;67:55–61. doi: 10.1007/s00228-010-0896-0. [DOI] [PubMed] [Google Scholar]
- 46.Saotome T, Minoura S, Terashi K, Sato T, Echizen H, Ishizaki T. Labetalol in hypertension during the third trimester of pregnancy: its antihypertensive effect and pharmacokinetic-dynamic analysis. J CLIN PHARMACOL. 1993;33:979–988. doi: 10.1002/j.1552-4604.1993.tb01933.x. [DOI] [PubMed] [Google Scholar]
- 47.Rubin PC, Butters L, Kelman AW. Labetalol disposition and concentration-effect relationships during pregnancy. BR J CLIN PHARMACOL. 1983;15:465–470. doi: 10.1111/j.1365-2125.1983.tb01531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rogers RC, Sibai BM, Whybrew WD. Labetalol pharmacokinetics in pregnancy-induced hypertension. AM J OBSTET GYNECOL. 1990;162:362–366. doi: 10.1016/0002-9378(90)90386-L. [DOI] [PubMed] [Google Scholar]
- 49.Lunell NO, Kulas J, Rane A. Transfer of labetalol into amniotic fluid and breast milk in lactating women. EUR J CLIN PHARMACOL. 1985;28:597–599. doi: 10.1007/BF00544073. [DOI] [PubMed] [Google Scholar]
- 50.Fischer JH, Sarto GE, Hardman J, Endres L, Jenkins TM, Kilpatrick SJ, Jeong H, Geller S, Deyo K, Fischer PA, Rodvold KA. Influence of gestational age and body weight on the pharmacokinetics of labetalol in pregnancy. Clin Pharmacokinet. 2014;53:373–383. doi: 10.1007/s40262-013-0123-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boulton DW, Dakers JM, Fawcett JP, Fiddes TM. Transplacental distribution of labetalol stereoisomers at delivery [2] Br J Clin Pharmacol. 1999;47:573–574. [PubMed] [Google Scholar]
- 52.Carvalho TMDJP, Cavalli RC, Marques MP, da Cunha SP, Baraldi CDO, Lanchote VL (2009) Stereoselective analysis of labetalol in human plasma by LC-MS/MS: application to pharmacokinetics. Chirality 21:738–44 [DOI] [PubMed]
- 53.Nandakumaran M, Angelo-Khattar M, Ibrahim ME, Hathout H. Transfer of labetalol in the perfused human placenta: an in vitro study. MED PRINC PRACT. 1989;1:81–85. doi: 10.1159/000157287. [DOI] [Google Scholar]
- 54.Schneider H, Proegler M. Placental transfer of β-adrenergic antagonists studied in an in vitro perfusion system of human placental tissue. AM J OBSTET GYNECOL. 1988;159:42–47. doi: 10.1016/0002-9378(88)90491-7. [DOI] [PubMed] [Google Scholar]
- 55.Nylund L, Lunell NO, Lewander R (1984) Labetalol for the treatment of hypertension in pregnancy: pharmakokinetics and effects on the uteroplacental blood flow. Acta Obstetricia et [DOI] [PubMed]
- 56.Ter Laak MA, Roos C, Touw DJ, Van Hattum PRM, Kwee A, Lotgering FK, Mol BWJ, Van Pampus MG, Porath MM, Spaanderman MEA, Van Der Post JAM, Papatsonis DNM, Van TVNE. Pharmacokinetics of nifedipine slow-release tablets during sustained tocolysis. Int J Clin Pharmacol Ther. 2015;53:84–91. doi: 10.5414/CP202215. [DOI] [PubMed] [Google Scholar]
- 57.Pirhonen JP, Erkkola RU, Ekblad UU, Nyman L. Single dose of nifedipine in normotensive pregnancy: nifedipine concentrations hemodynamic responses, and uterine and fetal flow velocity waveforms. OBSTET GYNECOL. 1990;76:807–811. doi: 10.1097/00006250-199011000-00016. [DOI] [PubMed] [Google Scholar]
- 58.Papatsonis DNM, Bos JM, Van Geijn HP, Lok CAR, Dekker GA. Nifedipine pharmacokinetics and plasma levels in the management of preterm labor. Am J Ther. 2007;14:346–350. doi: 10.1097/01.mjt.0000209679.76335.df. [DOI] [PubMed] [Google Scholar]
- 59.Silberschmidt AL, Kühn-Velten WN, Juon AM, Zimmermann R, Von Mandach U. Nifedipine concentration in maternal and umbilical cord blood after nifedipine gastrointestinal therapeutic system for tocolysis. BJOG Int J Obstet Gynaecol. 2008;115:480–485. doi: 10.1111/j.1471-0528.2007.01630.x. [DOI] [PubMed] [Google Scholar]
- 60.Haas DM, Quinney SK, McCormick CL, Jones DR, Renbarger JL. A pilot study of the impact of genotype on nifedipine pharmacokinetics when used as a tocolytic. J Matern -Fetal Neonatal Med. 2012;25:419–423. doi: 10.3109/14767058.2011.583700. [DOI] [PubMed] [Google Scholar]
- 61.Manninen AK, Juhakoski A. Nifedipine concentrations in maternal and umbilical serum, amniotic fluid, breast milk and urine of mothers and offspring. INT J CLIN PHARMACOL RES. 1991;11:231–236. [PubMed] [Google Scholar]
- 62.Poranen AK, Nurmi H, Malminiemi K, Ekblad U. Vasoactive effects and placental transfer of nifedipine, celiprolol, and magnesium sulfate in the placenta perfused in vitro. Hypertens Pregnancy. 1998;17:93–102. doi: 10.3109/10641959809072241. [DOI] [Google Scholar]
- 63.Ferguson IJE, Schutz T, Pershe R, Stevenson DK, Blaschke T. Nifedipine pharmacokinetics during preterm labor tocolysis. AM J OBSTET GYNECOL. 1989;161:1485–1490. doi: 10.1016/0002-9378(89)90909-5. [DOI] [PubMed] [Google Scholar]
- 64.Haas DM, Quinney SK, Clay JM, Renbarger JL, Hebert MF, Clark S, Umans JG, Caritis SN. Nifedipine pharmacokinetics are influenced by CYP3A5 genotype when used as a preterm labor tocolytic. Am J Perinatol. 2013;30:275–282. doi: 10.1055/s-0032-1323590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Prevost RR, Akl SA, Whybrew WD, Sibai BM. Oral nifedipine pharmacokinetics in pregnancy-induced hypertension. Pharmacotherapy. 1992;12:174–177. [PubMed] [Google Scholar]
- 66.Filgueira GCDO, Filgueira OAS, Carvalho DM, Marques MP, Moisés ECD, Duarte G, Lanchote VL, Cavalli RC. Analysis of nifedipine in human plasma and amniotic fluid by liquid chromatography-tandem mass spectrometry and its application to clinical pharmacokinetics in hypertensive pregnant women. J Chromatogr B Anal Technol Biomed Life Sci. 2015;993–994:20–25. doi: 10.1016/j.jchromb.2015.04.030. [DOI] [PubMed] [Google Scholar]
- 67.Marin TZ, Meier R, Kraehenmann F, Burkhardt T, Zimmermann R. Nifedipine serum levels in pregnant women undergoing tocolysis with nifedipine. J Obstet Gynaecol. 2007;27:260–263. doi: 10.1080/01443610701195009. [DOI] [PubMed] [Google Scholar]
- 68.Dallmann A, Ince I, Coboeken K, Eissing T, Hempel G. A physiologically based pharmacokinetic model for pregnant women to predict the pharmacokinetics of drugs metabolized via several enzymatic pathways. Clin Pharmacokinet. 2018;57:749–768. doi: 10.1007/s40262-017-0594-5. [DOI] [PubMed] [Google Scholar]
- 69.Quinney SK, Mohamed AN, Hebert MF, Haas DM, Clark S, Umans JG, Caritis SN, Li L. A semi-mechanistic metabolism model of CYP3A substrates in pregnancy: predicting changes in midazolam and nifedipine pharmacokinetics. CPT Pharmacometrics Syst Pharmacol. 2012;1:e2. doi: 10.1038/psp.2012.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ke C, You X, Lin C, Chen J, Guo G, Wu W, Ye L, Huang P (2021) Development of Physiologically based pharmacokinetic model for pregabalin to predict the pharmacokinetics in pediatric patients with renal impairment and adjust dosage regimens: PBPK model of pregabalin in pediatric patients with renal impairment. J Pharm Sci [DOI] [PubMed]
- 71.Ke AB, Nallani SC, Zhao P, Rostami-Hodjegan A, Unadkat JD (2012) A PBPK model to predict disposition of CYP3A-metabolized drugs in pregnant women: verification and discerning the site of CYP3A induction. CPT Pharmacometrics Syst Pharmacol 1 [DOI] [PMC free article] [PubMed]
- 72.Chaphekar N, Caritis S, Venkataramanan R. Model-informed dose optimization in pregnancy. J Clin Pharmacol. 2020;60(Suppl 1):S63–S76. doi: 10.1002/jcph.1777. [DOI] [PubMed] [Google Scholar]
- 73.Abduljalil K, Badhan RKS. Drug dosing during pregnancy-opportunities for physiologically based pharmacokinetic models. J Pharmacokinet Pharmacodyn. 2020;47:319–340. doi: 10.1007/s10928-020-09698-w. [DOI] [PubMed] [Google Scholar]
- 74.Blundell C, Yi YS, Ma L, Tess ER, Farrell MJ, Georgescu A, Aleksunes LM, Huh D (2018) Placental drug transport-on-a-chip: a microengineered in vitro model of transporter-mediated drug efflux in the human placental barrier. Adv Healthc Mater 7 [DOI] [PMC free article] [PubMed]
- 75.Seely EW, Ecker J (2011) Clinical practice. Chronic hypertension in pregnancy. N Engl J Med 365:439–46 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study. All data given are available in the original articles.