Abstract
Background
Covid-19 pandemic greatly impacted on the healthcare systems worldwide with negative consequences on several aspects of clinical populations. For neurological chronic conditions such as Multiple Sclerosis (MS), rehabilitation activities have been suspended or postponed during the pandemic. Rehabilitation is crucial for people with MS (PwMS) because it promotes recovery from relapses and maximizes opportunities for social participation. To better understand the impact of Covid-19 emergency on rehabilitation services for MS, the European network for rehabilitation in MS (RIMS) disseminated a survey to healthcare professionals (HPs) and representatives of the MS rehabilitation services (RSs), to explore the two different perspectives on the delivery of rehabilitation in usual circumstances and during the Covid-19 emergency.
Methods
The online survey was distributed from July 9th to September 20th, 2020. Besides general information on the responders (e.g. location of center, and memebership to RIMS), information was collected on usual service delivery (e.g. settings, specialities, and types of treatment), the impact of Covid-19 circumstances (e.g. restrictions, use of personal protective equipment, and impact on work), and the use of technologiesin rehabilitation.
Results
Twenty-two representatives of MS rehabilitation services (RSs)and 143 health care professionals (HPs) responded. Most of RSs and HPs worked in services specialized for MS including a mixture of all usual rehabilitation settings (i.e. inpatient, outpatient and community setting). The majority of services adopted a multidisciplinary framework, including physical therapy, occupational therapy, social service, speech and language therapy, psychological support, dietary interventions, medical management, vocational rehabilitation and cognitive rehabilitaton. Overall, most of responders indicated they did not use technologies in their practice (e.g. for treatment or assessment). However, depending on the type of technology a low-to-medium percentage of responders declared to use some technologies before Covid-19 crisis (5-55% for RSs and 12-53% for HPs) and a low percentage planned the use after pandemic (0-14% for RSs and 1-10% for HPs). Moreover, for the responders the most feasible interventions deliverable through tele-rehabilitation were psychological support and dietary interventions, with psychological support considered the most necessary intervention to be remotely implemented. Moderate feasibility (30-60%) was reported for hands-off interventions (e.g. aerobic exercise and cognitive rehabilitation) whereas low feasibility (<30%) was reported for hands-on interventions. Feasibility was especially low when tools were used that are not adaptable at-home (e.g. hyperbaric oxygen therapy).
Conclusion
The Covid-19 pandemic has stimulated the MS healthcare professionals to find new solutions to deliver alternative interventions to PwMS. In this context, the role of telemedicine is crucial to continue rehabilitation services at home, and limit exposure to infection. However, most of healthcare professionals have not incorporated the use of technologies. Therefore, the implementation of digital health solutions in the clinical practice needs more attention towards education on the potentials of technologies for rehabilitation and simplification of the national healthcare system reimbursement procedures for the rehabilitation technologies use.
Keywords: Multiple sclerosis, Rehabilitation, COVID-19 pandemic, Digital health, International network, Technology
1. Introduction
Rehabilitation is a key strategy for achieving population health and well-being as it promotes recovery from illness, improves human functioning, and maximizes opportunities for social participation (World Health Organization, 2017).
Multiple Sclerosis (MS) has physical and psychosocial consequences (Giovannoni et al., 2016), which usually have enormous long-term impacts on almost every aspect of the lives of people with MS (PwMS) and their families. Rehabilitation is required in many different kinds of MS impairments and disabilities, especially decreased mobility and dexterity, bladder and bowel dysfunction, communication and swallowing disorders, and cognitive impairment. Since 1991, the European network for rehabilitation in MS (RIMS) (www.eurims.org) recommends the MS services and healthcare professionals towards the best rehabilitation practice and research through always new challenges (www.ectrims.eu).
As already highlighted by several authors since the early months into the Covid-19 pandemic (Chaler et al., 2020; De Biase et al., 2020; Leocani et al., 2020), the healthcare systems worldwide have been greatly impacted with negative consequences on several domains and patients populations. For neurological chronic conditions such as MS rehabilitation many activities have been suspended or postponed (Leocani et al., 2020). During the tsunami of the Covid-19 breakdown in March 2020, this solution together with population lockdowns was an unavoidable measure to reduce infection risks; proactive strategies towards the restoration of adequate levels of rehabilitation care have been adopted afterwards to prevent or reverse already established consequences of prolonged restriction of motor, cognitive, leisure and social activities (Hubbard et al., 2015; Wilski et al., 2019).
To better understand the impact of Covid-19 emergency on rehabilitation services for MS, RIMS sent a global survey to healthcare professionals (HPs) and representatives of the MS rehabilitation services (RSs), with the aim to explore the two different perspectives on the delivery of rehabilitation in usual circumstances and the strategies adopted during the Covid-19 pandemic emergency. This survey is a relevant complement of a survey study recently published by the Special Interest Group for Mobility (SIG Mobility) of RIMS showing that Covid-19 pandemic has affected MS physical therapy services internationally in terms of content, frequency of use and format (Kahraman et al., 2022). In our study, we explore the feasibility of tele-rehabilitation as perceived by rehabilitation practitioners and managers, to investigate the level of adoption of low-cost technological tools for rehabilitation in usual and Covid-19 pandemic circumstances. Moreover, we investigated whether responses differences depended on the role the therapists had in their rehabilitation center of reference.
2. Material and methods
From July 9th to September 20th, 2020 an online survey devoted to outline a view of the consequences and effects of Covid-19 emergency on MS rehabilitation services was disseminated by email through RIMS and ECTRIMS newsletters, reaching healthcare professionals in contact with both organizations (www.eurims.org, www.ectrims.eu).
The study was carried out in accordance with the Declaration of Helsinki (1964). All information related to study purposes, target population, data collection, storage and privacy were described at the beginning of the survey and based on this information the participants gave their online consent to participate.
2.1. Online survey
After providing consent and indicating their role (i.e. RS or HP) and in the case of HPs also reporting age and discipline, the survey started. Depending on the responder role some specific questions were delivered (Supplemental File 1 and Supplemental File 2). The first part collected information on the European region and current membership to RIMS. Both surveys consisted of other two parts, for usual and Covid-19 pandemic circumstances.
Usual circumstances part collected information on settings, specialities and types of treatment of the rehabilitation services in which the responder worked; the responders were also asked to rate telerehabilitation feasibility in their centre and the need for its implementation. Only in RS survey, the number of working healthcare professionals and treated patients were required and information on disease course and disability level of patients had to be indicated.
The third part was devoted to collect information related to Covid-19 pandemic circumstances; specifically, on current emergency, impact on the delivered activities, types of adopted personal protective equipment (PPE) and PPE guidelines; specific questions on the use of e-Health technology for rehabilitation before, during and after the pandemic were present. Only in HP survey the responders were asked to rate their perception of the pandemic impact on their work.
2.2. Statistics
Statistical analysis was performed using STATISTICA 7.1. Data are expressed as absolute scores and percentage distribution based on the total responses.
3. Results
3.1. Participants
The newsletters was sent to 1621 healthcare professionals. In total, the responders were 165 with a response rate of 10%; 22 answered as RS and 143 as HP (mean age = 42,4 ± 11,1 years). Although the list of dissemination was balanced per European regions, most of the 165 responders were from South Europe (Table 1 ). Among HPs, 68 (47,5%) were physical therapists, 14 (9,8%) physiatrist, 12 (8,4%) neurologists, 11 (7,7%) speech and language therapists, 11 (7,7%) nurses, 8 (5,6%) occupational therapists, 8 (5,6%) psychologists, 4 (2,8%) neuropsychologists, 4 (2,8%) nutritionists, 1 (0,7%) audiologist, 1 (0,7%) general practitioner and 1 (0,7%) counsellor.
Table 1.
Features of the Rehabilitation Services
| RSs | HPs | |
|---|---|---|
| n (%) | n (%) | |
| Location | ||
|
1 (4,6%) | 17 (11,9%) |
|
1 (4,6%) | 4 (2,8%) |
|
3 (13,6%) | 22 (15,4%) |
|
17 (77,2%) | 90 (62,9%) |
|
0 (0%) | 10 (7,0%) |
| Membership to RIMS | ||
|
18 (81,8%) | 65 (45,4%) |
|
4 (18,2%) | 78 (54,6%) |
| Setting | ||
|
2 (9,1%) | 14 (9,8%) |
|
3 (13,6%) | 42 (29,4%) |
|
5 (22,7%) | 27 (18,9%) |
|
12 (54,6%) | 60 (41,9%) |
| Speciality | ||
|
2 (9,1%) | 29 (20,3%) |
|
10 (45,5%) | 47 (32,9%) |
|
18 (81,8%) | 103 (72,0%) |
| Number of healthcare professionals | ||
|
3 (13,6%) | - |
|
0 (0%) | - |
|
19 (86,4%) | - |
| Patients treated in a year | ||
|
40-2000 | - |
|
56,5 ± 35,8% | - |
| Disease course | ||
|
31,5 ± 28,5% | - |
|
52,5 ± 33,2% | - |
|
16,0 ± 18,3% | - |
| EDSS | ||
|
23,9 ± 18,3% | - |
|
31,1 ± 14,5% | - |
|
44,6 ± 29,5% | - |
3.2. Usual circumstances
3.2.1. Settings
Most of RSs reported that their service included a mixture of all usual rehabilitation settings (i.e. inpatient, outpatient and community setting) (Table 1). Similarly, HPs declared that the rehabilitation services in which they worked mostly included a mix of settings.
For both RSs and HPs the rehabilitation services could deliver more than one type of rehabilitation speciality. Eighteen RSs (81,8%) delivered MS rehabilitation and among those 11 exclusively MS rehabilitation (61,1%i.e. 50% of the total) and seven (38,9%, i.e. 31,8% of the total sample) also rehabilitation for other neurological diseases (Table 1).
Most of services, in which HPs worked, were specialized in MS (n=103, 72,0%); 76 of those (73,8%, i.e. 53,1% of the total) delivered exclusively MS rehabilitation, 18 (17,5%, i.e. 12,6% of the total) also rehabilitation for other neurological diseases, 2 (1,9%, i.e. 1,4% of the total) also general rehabilitation and 7 (6,8%, i.e. 4,9% of the total) also both neurological and general rehabilitation (Table 1).
RSs reported that the size of the rehabilitation services was prevalently large as shown by the number of services with more than 30 healthcare professionals and by the number of patients treated each year that in about 70% of cases was higher than 400 (range 40-2000). The percentage of treated PwMS (56,5%) seems to reflect the overview on the rehabilitation specialities of the RSs; indeed, half of the RSs was specialized in MS rehabilitation alone. Most of the RSs followed PwMS at more advanced disease stages, mainly with a progressive course (more than 68%) and a moderate-to-severe level of disability (about 76%) (Table 1).
3.2.2. Treatments
Overall, the responders declared that the most adopted organizational framework was multidisciplinary rehabilitation (Table 2 ).
Table 2.
Rehabilitation service delivery and tele-rehabilitation in usual circumstances
| RSs | HPs | |||||
|---|---|---|---|---|---|---|
| Type | Feasibility | Need | Type | Feasibility | Need | |
| Organizational Framework | ||||||
|
68,2% | 44,1±36,2% | 63,6% | 82,8% | 49,6±31,0% | 47,3% |
| Treatments | ||||||
|
||||||
|
77,3% | 46,4±33,3% | 50,0% | 45,2% | 50,9±28,7% | 33,0% |
|
72,7% | 37,7±34,2% | 27,3% | 53,8% | 46,0±30,9% | 33,0% |
|
77,3% | 31,2±24,0% | 18,2% | 46,2% | 35,0±30,4% | 19,8% |
|
4,5% | 6,8±17,8% | 0% | 2,2% | 13,4±24,4% | 2,2% |
|
13,6% | 10,0±19,5% | 0% | 8,6% | 14,6±24,5% | 2,2% |
|
31,8% | 13,2±26,6% | 0% | 17,5% | 15,9±27,2% | 5,5% |
|
63,6% | 44,5±33,3% | 54,5% | 41,9% | 51,3±30,7% | 35,2% |
|
||||||
|
50,0% | 39,1±35,4% | 27,3% | 29,0% | 48,1±30,6% | 19,8% |
|
36,4% | 47,3±34,1% | 40,9% | 25,8% | 59,8±31,3% | 39,6% |
|
40,9% | 53,2±38,7% | 36,4% | 16,1% | 53,6±32,5% | 26,4% |
|
27,3% | 45,5±39,4% | 31,8% | 9,7% | 44,8±33,2% | 18,7% |
|
63,6% | 53,6±33,0% | 45,5% | 39,8% | 55,0±29,0% | 37,4% |
|
63,6% | 63,2±34,4% | 50,0% | 41,9% | 64,7±30,0% | 48,4% |
|
50,0% | 56,8±33,1% | 40,9% | 16,1% | 46,7±28,8% | 28,6% |
|
54,5% | 57,7±34,9% | 31,8% | 30,1% | 61,0±30,8% | 41,8% |
|
54,5% | 53,6±36,8% | 36,4% | 31,2% | 53,8±29,4% | 40,7% |
|
59,1% | 47,3±35,6% | 31,8% | 34,4% | 51,5±31,1% | 27,5% |
RSs reported their center provided mainly physical therapy (gait, balance, mobility, spasticity management and aerobic training) (about 75%), occupational therapy (64%), speech and language therapy (64%) and psychological support (64%). Postural re-education, fall prevention, Tai Chi Chuan, Ch'i Kung, robotic rehabilitation (e.g. exoskeleton, balance platforms), specific speech and language therapy training for respiration, communication and swallowing and podiatrist interventions were reported (Table 2).
Similarly, the interventions for gait, balance, mobility, spasticity management and aerobic training were the most reported (range 45-50%) by HPs, followed by occupational therapy, speech and language therapy and psychological support (range 35-45%). Also nursing care, psychosexual rehabilitation, gardening, hippo-therapy, music-therapy, bladder and bowel rehabilitation, self-management support, health education and prevention interventions, coaching for healthcare professionals were reported (Table 2).
Percentage of response related to the type of organizational framework and treatments in the rehabilitative centers of RSs and HPs. Moreover, the percentages of feasibility and need of implementation in Tele-rehabilitation for the multidisciplinary organizational framework and the several treatments are reported.
3.2.3. Feasibility of Tele-rehabilitation
Overall, both RSs and HPs declared that the most feasible interventions deliverable in usual circumstances through tele-rehabilitation were psychological support and dietary interventions, with psychological support considered the most necessary intervention to be remotely implemented (Table 2).
A medium score of feasibility (30-60%) was reported for other disciplines that do not involve “hands-on” interventions, such as aerobic exercise, cognitive rehabilitation, speech and language therapy, vocational rehabilitation, and social service. Although the therapist-patient body contact is usually present, also the implementation through tele-rehabilitation of disciplines such as gait, balance and mobility training, spasticity treatment, occupational therapy and medical management, was considered feasible (Table 2).
A low score of feasibility for telerehabilitation (<30%) was reported for techniques using tools that are not adaptable to a home setting, such as hyperbaric oxygen therapy, whole-body vibration and aquatic therapy. Obviously, very low need of implementation through tele-rehabilitation (<6%) was reported for these types of treatment (Table 2).
Interestingly, in general, HPs reported higher percentages of feasibility with respect to RSs in implementing traditional treatments through tele-rehabilitation; however, HPs seemed to be less confident (i.e. lower percentages) than RSs on the actual necessity to implement treatments in a remote digital way.
3.3. Covid-19 pandemic circumstances
3.3.1. Restrictions
Most of responders (about 70%) reported they were still under emergency at the time of the survey. Almost all the responders (98,9%) declared to have already fully or partially restarted their rehabilitation activities.
Almost 75% of the RSs and 85% of HPs declared they did not interrupt activities (e.g. reduced, changed or shifted to Covid-19 patients). Wide differences among responders for both RSs (range: 10-88%) and HPs (range: 10-90%) were found for the percentage of activities reduction.
On average, the impact of Covid-19 crisis on the rehabilitation work of HPs has been medium to high. Table 3 lists the positive and negative effects of pandemic reported by HPs.
Table 3.
Impact of Covid-19 pandemic on HPs practice
| POSITIVE impact on the rehabilitation work due to Covid-19 pandemic |
|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| NEGATIVE impact on the rehabilitation work due to Covid-19 pandemic |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3.3.2. Personal Protective Equipment
As expected, all the responders in both RSs and HPs reported the adoption of PPE prevalently following national/regional governmental guidelines (86,4% and 62,9% respectively) (Table 4 ). Some RSs adopted more than one guideline: 2 (9,2%) adopted all of them, 6 (27,3%) the national/regional governmental guidelines and one of the others, and 1 (4,5%) all except the WHO guidelines. Also some HPs declared to use more than one guideline: 2 (1,4%) all of them, 30 (20,9%) the national/regional governmental guidelines and one of the others, and 9 (6,3%) all except the WHO guidelines. Unexpectedly, 2 responders reported to not follow guidelines and 3 to not know which type of guidelines they used.
Table 4.
Effects of Covid-19
| RSs | HPs | |
|---|---|---|
| n (%) | n (%) | |
| Impact of Covid-19 on activities | ||
|
6 (27,3%) | 22 (15,4%) |
|
12 (54,5%) | 94 (65,7%) |
|
1 (4,5%) | 14 (9,8%) |
|
2 (9,2%) | 2 (1,4%) |
|
1 (4,5%) | 11 (7,7%) |
| Guidelines for PPE usage | ||
|
0 (0%) | 2 (1,4%) |
|
7 (31,8%) | 49 (34,3%) |
|
19 (86.4%) | 90 (62.9%) |
|
6 (27,3%) | 31 (21,7%) |
|
3 (13,6%) | 25 (17,5%) |
|
0 (0%) | 3 (2,1%) |
HPs reported that surgical and FFP2/K95 masks were the main used PPE (67,8% and 62,2% respectively); few responders (4,9%) reported also FFP3. Who used another type of PPE (21,7%) specified in a dedicated free-text field to use masks made of cloth, gloves, sterile gown and apron, overshoes, glasses and goggles, face shield and alcoholic solution.
3.3.3. Adoption of technology
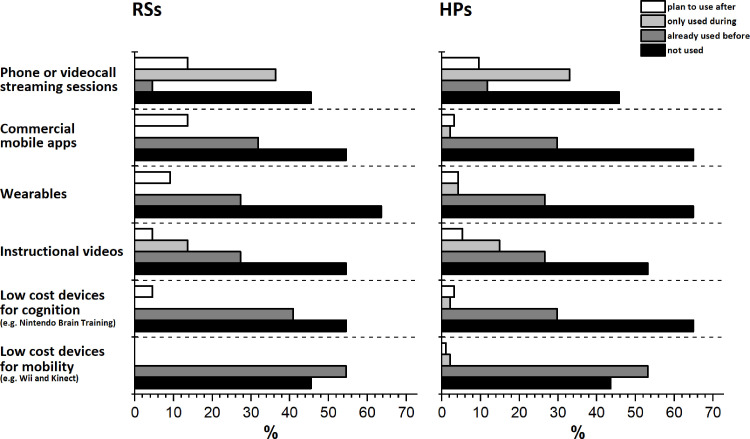
Overall, most of responders indicated they did not use technologies in their practice (e.g. for treatment or assessment) (Fig. 1 ). However, depending on the type of technology a low-to-medium percentage of responders declared to use some technologies before Covid-19 crisis (5-55% for RSs and 12-53% for HPs). During the pandemic, RSs and HPs did not frequently use technologies except for instructional video and phone- and video-calls, the latter strongly stimulated to be adopted with respect to the pre-pandemic.
Fig. 1.
Use of technologies. Percentages of the use of technologies before and during Covid-19 crisis and planned to use after. The technologies were selected among those prevalently used in the MS rehabilitation context. RSs = Representatives of the MS rehabilitation services; HPs = healthcare professionals.
Only few responders planned to use technologies after pandemic (0-14% for RSs and 1-10% for HPs). Interestingly, except for low-cost devices for mobility (e.g. Nintendo Wii and Microsoft Kinect) the percentage of RSs planning to use the proposed technologies after pandemic was always higher than the percentage of HPs.
HPs listed other technologies (open-ended question) they used before and planned to be used after the Covid-19 crisis. Because these devices required supervision (e.g. balance robotic platforms, gait trainers, recumbent cross trainers, virtual reality treadmill, augmentative and alternative communication tools, cognitive trainers, functional electrical stimulation) their use during pandemic was not feasible.
Interestingly, some HPs reported in this open-ended question the need to simplify the national healthcare system reimbursement procedures for the rehabilitation technologies use.
4. Discussion
This survey study explored the impact of the Covid-19 pandemic and related restrictions on the MS rehabilitation service delivery in Europe from the perspective of representatives of the MS rehabilitation services and health care professionals. The survey was designed, developed and distributed during the third phase of the first wave when the virus seemed almost defeated, all new infections were identified and isolated and, despite an unstable epidemiological situation, governments started to lift restrictive measures and allowed a resurrection of social life (Plümper and Neumayer, 2020). The dynamics of the first wave Covid-19 pandemic involved a first phase of unawareness (risk essentially ignored, social behaviour not yet adjusted, infections spread at an exponential rate) and a second phase of lockdown (clear virus-associated risks, preventive measures, changes in behaviours, social distancing) (Plümper and Neumayer, 2020).
In usual circumstances, the rehabilitation services mostly adopted a mixed model based on at least two of inpatient service, outpatient service and community setting; it would reflect the high number of PwMS treated by most of the rehabilitation services and the consequent need to reach them through different rehabilitation settings. In addition, a high number of PwMS with progressive course and moderate-severe level of disability, as reported by RSs, would strongly increase the heterogeneity of MS needs to be managed (Ponzio et al., 2019). A mixed model could be a necessary response to these needs and would advantage the provision of the best healthcare solutions to PwMS at all stages of their journey.
In addition, most of responders declared that the services were exclusively dedicated or had a unit dedicated to MS rehabilitation and adopted an organizational framework based on the multidisciplinary team, by suggesting the presence of the high professional and management competences necessary to take care of all the rehabilitation needs of PwMS.
Current evidence suggests that having MS does not increase the risk of Covid-19 infection or worsen clinical outcomes compared to people without MS (Evangelou et al., 2021; Parrotta et al., 2020). Nevertheless, up to 81% of rehabilitation services reduced their activity or were closed at time of distributing the survey. The several levels of stringency of the lockdown policies, from a soft recommendation to stay at home, to a moderate directive stay at home or a much harder order not to leave home (Plümper and Neumayer, 2020), could reduce or not permit the access to MS rehabilitation services. As consequence, the clinical management, especially treatment, fundamental to preserve the physical, cognitive and psychological status of PwMS (Kalron et al., 2021; Mantovani et al., 2020; Motolese et al., 2020), was limited and social interaction was prohibited.
In this respect, although all the participants were from countries that had applied restrictions and many of them were still under lockdown policies (soft, moderate or hard) at the time of the survey, most of them reported the working activities were maintained. Indeed, the adoption of a plethora of PPE and multiple types of guidelines would have made feasible and safer face-to-face interventions essential and not deliverable remotely (Landi et al., 2020; Robinson et al., 2021).
These findings are in line with the SIG Mobility survey results (Kahraman et al., 2022) showing a reduction of activities in the rehabilitation services during the pandemic. Overall the entity of the reduction reported by Kahraman et al. (2022) was lower than in the current survey. Indeed, there the respondents were required to refer to the entire 2020 and probably they reported percentages of activities reduction taking into account the different periods of restrictions and relaxation. On the contrary, our survey referred to the specific period immediately subsequent to the the first wave of pandemic when some services restarted most of activities and other still experienced a lot of restrictions. Currently, the availability of vaccines and the consequent progressive gradual relaxation of restrictive measures allowed restoring the delivery of rehabilitative treatments as before Covid-19 pandemic. Moreover, new ways of thinking the significant changes the pandemic has made are nowadays under discussion and could represent an opportunity towards a post-pandemic “new normal” of the National Healthcare Systems (NHS) encompassing concepts of solidarity, care, and reciprocal responsibility (Redhead et al., 2022).
Technologies would make feasible remote assessment, monitoring and treatment. However, most of MS professionals, independently from their role (i.e. RSs and HPs) reported to not have incorporated the use of technologies in their clinical practice. Indeed, although a consistent part of responders declared that before pandemic they used low-cost devices for cognition and mobility and at a lower extent apps, wearables and instructional videos, most of them reported that in their rehabilitation services these common technological solutions were not used at all. Low percentages of responders declared to use technologies during pandemic or they would have used after the crisis. Phone- or video-call streaming sessions was the most considered technology during and after pandemic.
These results, similar for both RSs and HPs, would highlight two contrasting tendencies in using technologies among MS healthcare professionals. On one side, they would need a better education and training on the technologies benefits such as reliability, utility to support outcomes in rehabilitation, equity of access to health care and costs reduction (Corea et al., 2021; McGinley et al., 2021, 2020; Sun et al., 2020; Wesson and Kupperschmidt, 2013). In fact, they could not use technologies because of a lack of knowledge on the best existing opportunities, limited reimbursement policies from the National Healthcare Systems (e.g. individually sustained costs of devices), absence or lack of scientific validation of technologies and, of relevance, a defined regulatory framework of healthcare professional’ liability and data privacy management (Ferorelli et al., 2020). These considerations could be extended also to operators not specialized in MS.
On the other side, a minor but consistent part of responders reported to use technologies already before Covid-19 pandemic. Besides ascertaining the relevance in improving their working activities (Bove et al., 2019), they could have met the strong enthusiasm shown by PwMS towards internet-based patient reports (Bove et al., 2013), mobile devices (Bove et al., 2015), and wearables to assess clinical outcomes (Block et al., 2017).
Interestingly, despite the use of technologies during and after pandemic was reduced for both RSs and HPs, with respect to RSs, HPs were more confident on the feasibility to deliver traditional treatments through tele-rehabilitation and considered less necessary their implementation in a remote digital mode. We can speculate that, because RSs are more involved in the practical implementation of their rehabilitation service, they would know less how some technologies could make a treatment feasible through tele-rehabilitation devices whereas they would glimpse the possibility to meet through the digital solutions use unmet needs such as promoting continuity of care for PwMS and delivering rehabilitation to patients living away from the center (Nicholas et al., 2021). After all, during the Covid-19 health emergency, the use of technologies was an essential asset through which the NHS strengthened their response during the most critical phases (The Organisation for Economic Co-operation and Development (OECD) 2020).
According to the post-pandemic economic reform plans of many countries (e.g. Italy, Germany and France) (European Union), telemedicine will not be limited to a tool for responding to an emergency condition but it will become a structural resource contributing to the reorganization of the NHS, allowing the shift of health care to the home-based settings through innovative citizen centered care models, and facilitating access to healthcare services, rehabilitative services included. Currently, telemedicine is a great resource that makes possible new approaches to care and new ways of continuity of care between hospital and home-based care (De Micco et al., 2022).
Despite this relevance, scientific evidences have shown that healthcare delivered through telemedicine can be burdened by numerous ethical and legal issues that represent some of the most relevant challenges for the onoging reorganization process of the NHS (De Micco et al., 2022).
4.1. Limitations
We are aware that the present study is not free from limitations. One limitation is a low response rate. Though response rates for surveys can vary considerably (Ward et al., 2022), online surveys typically have a response rate of 20%–30% (Safdar et al., 2016). With such a low response rate, there is potential for nonresponse bias and poor representation. However, it is not surprising that the response rate was low. Indeed, for long time following the first pandemic wave (including the dissemination period of our survey), everywhere healthcare professionals received frequent requests of online surveys on the impact of Covid-19 pandemic on their activities by giving up on answering. Nevertheless, we felt that the responses that we did receive were very valuable, also considering that part of responses were reported from representative of MS rehabilitation centers, and provided interesting insights on the impact of Covid-19 emergency on MS rehabilitation services.
Moreover, there may have been an overrepresentation of responders from South Europe which could be attributed to a high number of Covid-19 cumulative cases (Naqvi, 2021). Furthermore, we did not ask the participants the country of provenience and, for this reason, we can not present the data according to each country.
In addition, it would have been beneficial to utilize widespread, standardized, and validated scales. However, no such scales existed at the beginning of the study and the time frame was too short for a comprehensive development process of questionnaires.
5. Conclusions
The Covid-19 pandemic has stimulated the MS healthcare professionals to find new solutions to deliver interventions to PwMS. In this context, the role of tele-rehabilitation is crucial to continue rehabilitation service delivery and limit exposure to infection. As a consequence, digital health and telemedicine seem to transform rehabilitation and could pave the way to digital/standard mixed rehabilitation personalized approaches. The reported reluctance of implementing technology in rehabilitation, demands more consideration towards education on the potentialities of technologies for rehabilitation and simplification of the National Healthcare Systems reimbursement procedures for the rehabilitation technologies use.
6. Study Group
Anders Skjerbaek, PT, MSc, Ry and Haslev, Denmark, Roshan das Nair, Psy., Nottingham, United Kingdom, Piet Eelen, RN, MSc, Melsbroek, Belgium, Jana Pöttgen, Psy., Hamburg, Germany, Lars Hvid, PT, Aarhus, Denmark, Daiana Bezzini, Siena Italy, Ludovico Pedullà, Genoa, Italy, Jessica Podda, Genoa, Italy, Margherita Monti Bragadin, Genoa, Italy, Alice Bellosta, Genoa, Italy
CRediT authorship contribution statement
Giampaolo Brichetto: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft. Andrea Tacchino: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Supervision, Writing – original draft. Letizia Leocani: Writing – review & editing. Daphne Kos: Conceptualization, Validation, Supervision, Writing – review & editing.
Declaration of competing interest
None.
Acknowledgments
Funding
No funding was received for this study
Acknowledgement
The authors want to thank Davide Cafiero and HELAGLOBE SRL for the support in implementing and disseminating the survey. The authors also thank the respondents for sharing their valuable information. This work was presented on the 5th December 2020 at the RIMS conference.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.msard.2022.104179.
Appendix. Supplementary materials
References
- Block V.J., Lizée A., Crabtree-Hartman E., Bevan C.J., Graves J.S., Bove R., Green A.J., Nourbakhsh B., Tremblay M., Gourraud P.-A., Ng M.Y., Pletcher M.J., Olgin J.E., Marcus G.M., Allen D.D., Cree B.A.C., Gelfand J.M. Continuous daily assessment of multiple sclerosis disability using remote step count monitoring. J. Neurol. 2017;264:316–326. doi: 10.1007/s00415-016-8334-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bove R., Bevan C., Crabtree E., Zhao C., Gomez R., Garcha P., Morrissey J., Dierkhising J., Green A.J., Hauser S.L., Cree B.A., Wallin M.T., Gelfand J.M. Toward a low-cost, in-home, telemedicine-enabled assessment of disability in multiple sclerosis. Multiple Sclerosis J. 2019;25:1526–1534. doi: 10.1177/1352458518793527. [DOI] [PubMed] [Google Scholar]
- Bove R., Secor E., Healy B.C., Musallam A., Vaughan T., Glanz B.I., Greeke E., Weiner H.L., Chitnis T., Wicks P., De Jager P.L. Evaluation of an online platform for multiple sclerosis research: patient description, validation of severity scale, and exploration of BMI effects on disease course. PLoS One. 2013;8:e59707. doi: 10.1371/journal.pone.0059707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bove R., White C.C., Giovannoni G., Glanz B., Golubchikov V., Hujol J., Jennings C., Langdon D., Lee M., Legedza A., Paskavitz J., Prasad S., Richert J., Robbins A., Roberts S., Weiner H., Ramachandran R., Botfield M., De Jager P.L. Evaluating more naturalistic outcome measures. Neurol. - Neuroimmunol. Neuroinflammat. 2015;2:e162. doi: 10.1212/NXI.0000000000000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaler J., Gil Fraguas L., Gómez García A., Laxe S., Luna Cabrera F., Llavona R., Miangolarra Page J.C., del Pino Algarrada R., Salaverría Izaguirre N., Sánchez Tarifa P., Santandr Eu M.E., Garreta Figuera R. Impact of Coronavirus disease 2019 outbreak on rehabilitation services and physical rehabilitation medicine and rehabilitation physicians’ activities: perspectives from the Spanish experience. Eur. J. Phys. Rehabilit. Med. 2020;56 doi: 10.23736/S1973-9087.20.06304-2. [DOI] [PubMed] [Google Scholar]
- Corea F., Ciotti S., Cometa A., De Carlo C., Martini G., Baratta S., Zampolini M. Telemedicine during the Coronavirus Disease (COVID-19) pandemic: a multiple sclerosis (MS) outpatients service perspective. Neurol. Int. 2021;13:25–31. doi: 10.3390/neurolint13010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Biase S., Cook L., Skelton D.A., Witham M., ten Hove R. The COVID-19 rehabilitation pandemic1. Age Ageing. 2020;49:696–700. doi: 10.1093/ageing/afaa118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Micco F., Fineschi V., Banfi G., Frati P., Oliva A., Travaini G.V., Picozzi M., Curcio G., Pecchia L., Petitti T., Alloni R., Rosati E., De Benedictis A., Tambone V. From COVID-19 pandemic to patient safety: a new “Spring” for telemedicine or a boomerang effect? Front. Med. 2022;9 doi: 10.3389/fmed.2022.901788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Union, Regulation (EU) 2021/522 of the European Parliament and of the Council of 24 March 2021 Establishing a Programme for the Union's Action in the Field of Health (‘EU4Health Programme’) for the Period 2021-2027, and Repealing Regulation (EU) No 282/2014. (20 [WWW Document]. URL https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=uriserv:OJ.%0AL_.2021.107.01.0001.01.ENG. (accessed 9.7.22).
- Evangelou N., Garjani A., DasNair R., Hunter R., Tuite-Dalton K.A., Craig E.M., Rodgers W.J., Coles A., Dobson R., Duddy M., Ford D.V., Hughes S., Pearson O., Middleton L.A., Rog D., Tallantyre E.C., Friede T., Middleton R.M., Nicholas R. Self-diagnosed COVID-19 in people with multiple sclerosis: a community-based cohort of the UK MS Register. J. Neurol. Neurosurg. Psychiatry. 2021;92:107–109. doi: 10.1136/jnnp-2020-324449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferorelli D., Nardelli L., Spagnolo L., Corradi S., Silvestre M., Misceo F., Marrone M., Zotti F., Mandarelli G., Solarino B., Dell'Erba A. Medical legal aspects of telemedicine in italy: application fields, professional liability and focus on care services during the COVID-19 health emergency. J. Primary Care Commun. Health. 2020;11 doi: 10.1177/2150132720985055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovannoni G., Butzkueven H., Dhib-Jalbut S., Hobart J., Kobelt G., Pepper G., Sormani M.P., Thalheim C., Traboulsee A., Vollmer T. Brain health: time matters in multiple sclerosis. Multiple Scleros. Rel. Disord. 2016;9:S5–S48. doi: 10.1016/j.msard.2016.07.003. [DOI] [PubMed] [Google Scholar]
- Hubbard E.A., Motl R.W., Manns P.J. The descriptive epidemiology of daily sitting time as a sedentary behavior in multiple sclerosis. Disab. Health J. 2015;8:594–601. doi: 10.1016/j.dhjo.2015.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahraman T., Rasova K., Jonsdottir J., Medina C.S., Kos D., Coote S., Tacchino A., Smedal T., Arntzen E.C., Quinn G., Learmonth Y., Pedulla L., Moumdjian L., Kalron A. The impact of the COVID-19 pandemic on physical therapy practice for people with multiple sclerosis: a multicenter survey study of the RIMS network. Multiple Scleros. Rel. Disord. 2022;62 doi: 10.1016/j.msard.2022.103799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalron A., Dolev M., Greenberg-Abrahami M., Menascu S., Frid L., Avrech-Shezifi S., Harari G., Magalashvili D., Achiron A. Physical activity behavior in people with multiple sclerosis during the COVID-19 pandemic in Israel: Results of an online survey. Multiple Scleros. Rel. Disord. 2021;47 doi: 10.1016/j.msard.2020.102603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landi D., Ponzano M., Nicoletti C.G., Cecchi G., Cola G., Mataluni G., Mercuri N.B., Sormani M.P., Marfia G.A. Adherence to social distancing and use of personal protective equipment and the risk of SARS-CoV-2 infection in a cohort of patients with multiple sclerosis. Multiple Scleros. Rel. Disord. 2020;45 doi: 10.1016/j.msard.2020.102359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leocani L., Diserens K., Moccia M., Caltagirone C. Disability through COVID-19 pandemic: neurorehabilitation cannot wait. Eur. J. Neurol. 2020;27 doi: 10.1111/ene.14320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantovani E., Zucchella C., Bottiroli S., Federico A., Giugno R., Sandrini G., Chiamulera C., Tamburin S. Telemedicine and virtual reality for cognitive rehabilitation: a roadmap for the COVID-19 Pandemic. Front. Neurol. 2020;11 doi: 10.3389/fneur.2020.00926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinley M.P., Gales S., Rowles W., Wang Z., Hsu W.-Y., Amezcua L., Bove R. Expanded access to multiple sclerosis teleneurology care following the COVID-19 pandemic. Multiple Scleros. J. - Exp. Transl. Clin. 2021;7 doi: 10.1177/2055217321997467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinley M.P., Ontaneda D., Wang Z., Weber M., Shook S., Stanton M., Bermel R. Teleneurology as a solution for outpatient care during the COVID-19 pandemic. Telemed. e-Health. 2020;26:1537–1539. doi: 10.1089/tmj.2020.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motolese F., Rossi M., Albergo G., Stelitano D., Villanova M., Di Lazzaro V., Capone F. The psychological impact of COVID-19 pandemic on people with multiple sclerosis. Front. Neurol. 2020;11 doi: 10.3389/fneur.2020.580507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naqvi A. COVID-19 European regional tracker. Sci. Data. 2021;8:181. doi: 10.1038/s41597-021-00950-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholas J.A., Shin R.K., Alvarez E., Hendin B., Nair K.V., Lublin F.D. Pandemic forward: Lessons learned and expert perspectives on multiple sclerosis care in the COVID-19 era. Multiple Scleros. Rel. Disord. 2021;49 doi: 10.1016/j.msard.2020.102715. https://www.eurims.org [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrotta E., Kister I., Charvet L., Sammarco C., Saha V., Charlson R.E., Howard J., Gutman J.M., Gottesman M., Abou-Fayssal N., Wolintz R., Keilson M., Fernandez-Carbonell C., Krupp L.B., Zhovtis Ryerson L. COVID-19 outcomes in MS. Neurol. - Neuroimmunol. Neuroinflammat. 2020;7:e835. doi: 10.1212/NXI.0000000000000835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plümper T., Neumayer E. Lockdown policies and the dynamics of the first wave of the Sars-CoV-2 pandemic in Europe. J. Eur. Publ. Policy. 2020:1–21. doi: 10.1080/13501763.2020.1847170. [DOI] [Google Scholar]
- Ponzio M., Tacchino A., Vaccaro C., Brichetto G., Battaglia M.A., Messmer Uccelli M. Disparity between perceived needs and service provision: a cross-sectional study of Italians with multiple sclerosis. Neurolog. Sci. 2019;40 doi: 10.1007/s10072-019-03780-z. [DOI] [PubMed] [Google Scholar]
- Redhead C.A.B., Fovargue S., Frith L., Chiumento A., Draper H., Baines P.B. Relationships, Rights, and Responsibilities: (Re)viewing the NHS Constitution for the post-pandemic ‘new normal’. Med. Law Rev. 2022 doi: 10.1093/medlaw/fwac028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson M.R., Koverman B., Becker C., Ciancio K.E., Fisher G., Saake S. Lessons learned from the COVID-19 pandemic: occupational therapy on the front line. Am. J. Occup. Ther. 2021;75 doi: 10.5014/ajot.2021.047654. p1. [DOI] [PubMed] [Google Scholar]
- Safdar N., Abbo L.M., Knobloch M.J., Seo S.K. Research methods in healthcare epidemiology: survey and qualitative research. Infect. Control Hospital Epidemiol. 2016;37:1272–1277. doi: 10.1017/ice.2016.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S., Folarin A.A., Ranjan Y., Rashid Z., Conde P., Stewart C., Cummins N., Matcham F., Dalla Costa G., Simblett S., Leocani L., Lamers F., Sørensen P.S., Buron M., Zabalza A., Guerrero Pérez A.I., Penninx B.W., Siddi S., Haro J.M., Myin-Germeys I., Rintala A., Wykes T., Narayan V.A., Comi G., Hotopf M., Dobson R.J. Using smartphones and wearable devices to monitor behavioral changes during COVID-19. J. Med. Internet Res. 2020;22:e19992. doi: 10.2196/19992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Organisation for Economic Co-operation and Development (OECD), Beyond Containment: health systems responses to COVID-19 in the OECD. (2020) [WWW Document]. URL https://www.oecd.org/coronavirus/%0Apolicy-responses/beyond-containment-health-systems-responses-tocovid-%0A19-in-the-oecd-6ab740c0/#blocknotes-d7e786. (accessed 9.7.22).
- Ward C., Banfield J., Brousseau P. A survey of Canadian respiratory therapists working in the COVID-19 pandemic: the RRT perspective. Canad. J. Respirat. Therapy. 2022;58:57–63. doi: 10.29390/cjrt-2020-065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesson J.B., Kupperschmidt B. Rural trauma telemedicine. J. Trauma Nurs. 2013;20:199–202. doi: 10.1097/JTN.0000000000000012. [DOI] [PubMed] [Google Scholar]
- Wilski M., Gabryelski J., Brola W., Tomasz T. Health-related quality of life in multiple sclerosis: links to acceptance, coping strategies and disease severity. Disab. Health J. 2019;12:608–614. doi: 10.1016/j.dhjo.2019.06.003. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2017. Rehabilitation: key for health in the 21st century.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.