Abstract
Abstract
Musculoskeletal malignancies are a rare type of cancer. Consequently, sufficient imaging data for machine learning (ML) applications is difficult to obtain. The main purpose of this review was to investigate whether ML is already having an impact on imaging-driven diagnosis of musculoskeletal malignancies and what the respective reasons for this might be. A scoping review was conducted by a radiologist, an orthopaedic surgeon and a data scientist to identify suitable articles based on the PRISMA statement. Studies meeting the following criteria were included: primary malignant musculoskeletal tumours, machine/deep learning application, imaging data or data retrieved from images, human/preclinical, English language and original research. Initially, 480 articles were found and 38 met the eligibility criteria. Several continuous and discrete parameters related to publication, patient distribution, tumour specificities, ML methods, data and metrics were extracted from the final articles. For the synthesis, diagnosis-oriented studies were further examined by retrieving the number of patients and labels and metric scores. No significant correlations between metrics and mean number of samples were found. Several studies presented that ML could support imaging-driven diagnosis of musculoskeletal malignancies in distinct cases. However, data quality and quantity must be increased to achieve clinically relevant results. Compared to the experience of an expert radiologist, the studies used small datasets and mostly included only one type of data. Key to critical advancement of ML models for rare diseases such as musculoskeletal malignancies is a systematic, structured data collection and the establishment of (inter)national networks to obtain substantial datasets in the future.
Key Points
• Machine learning does not yet significantly impact imaging-driven diagnosis for musculoskeletal malignancies compared to other disciplines such as lung, breast or CNS cancer.
• Research in the area of musculoskeletal tumour imaging and machine learning is still very limited.
• Machine learning in musculoskeletal tumour imaging is impeded by insufficient availability of data and rarity of the disease.
Keywords: Primary musculoskeletal malignancies, Imaging-driven diagnosis, Diagnostic imaging, Machine learning, Deep learning
Introduction
Malignant tumours of the musculoskeletal system represent a group of extraordinarily rare and heterogeneous tumour entities. For example, malignant bone tumours account for only about 0.2% of all human malignancies, but they occur more frequently in children (sixth most common cancer) and adolescents (third most common cancer) [1–3]. In addition to the pronounced rarity, the mostly unspecific history or clinical presentation also complicates early diagnosis and often leads to significant delays [3]. However, undelayed diagnosis is of paramount importance in musculoskeletal tumours, as the diagnostic window also has a direct impact on resectability and patient survival prognosis [2]. Thus, prompt referral to a specialised sarcoma centre is crucial when a malignant musculoskeletal tumour is suspected. However, delays of more than 12 months sometimes occur in clinical care reality, which can be explained not least by the fact that a general medical practitioner encounters only about three malignant musculoskeletal tumours in his/her professional life [4].
Especially the morphologic heterogeneity within musculoskeletal tumours complicates imaging entity or malignancy assessment and even limits the informative value of a biopsy. In sclerotic, blastic or cartilaginous lesions, as well as in tumours with a large necrotic area, retrieving adequate material from a biopsy is extremely challenging and requires a high degree of experience [5]. The rate of biopsy-related complications that adversely affect biopsy outcome or prognosis is reported to be 15–20%, with up to 12 times higher rates in non-specialist institutions [6]. Therefore, the importance of adequate diagnostic biopsy cannot be overstated in musculoskeletal tumours, which is why biopsy is considered the “first step of therapy” by many experts.
Image interpretation as a part of precision medicine plays an increasingly important role in the future of orthopaedic oncology, and novel, more comprehensive and specific analysis tools are urgently needed, especially for outpatient clinics with limited experience and resources for detection and interpretation of rare bone and soft tissue malignancies. Machine learning (ML) and the subset deep learning (DL) represent distinct applications of artificial intelligence (AI), which evolved from pattern recognition and learning theory. ML is just in its early stages in orthopaedics, and standardised approaches are not yet established. While complex data analysis of cancerous tissue through AI and imaging data is already widely applied for research purposes in some cancers (e.g. lung, breast or CNS cancer) [7], the application of these methods in orthopaedic oncology research is still very limited [8]. The fact that globally no far-reaching structures for systematic and structured data acquisition have yet been established (to the best of our knowledge) and that sarcomas are very rare and heterogeneous makes modern AI applications, for which a sufficient and qualitative amount of data is crucial, considerably more difficult. Although various methods for dealing with limited datasets have been developed (data augmentation [9], transfer learning [10], data simulation [11]), there is no way around building up appropriate structures and networks.
The main purpose of this review was to investigate whether ML can already substantially support image interpretation of musculoskeletal (MSK) malignancies with a focus on diagnostic tasks and what the respective reasons for this might be.
Materials and methods
Eligibility criteria
A scoping review of the literature was performed to identify ML applications in imaging of musculoskeletal malignancies based on the PRISMA statement [12]. Studies meeting the following criteria were included in this review:
Primary malignant musculoskeletal tumours
Application of machine learning or deep learning
Imaging data or data retrieved from images
Human or preclinical
Written in English
Original research articles
The following focus led to the exclusion of articles for this review:
Metastases
Histological data
Secondary bone/soft tissue tumours
Lymphoma
Myeloma
Benign, intermediate
Review articles
Articles that contained benign or intermediate lesions but focused primarily on e.g. the detection of malignant lesions were included. In contrast, articles that did not contain data on malignant lesions were excluded. The focus was on malignant lesions because of their clinical relevance and difficulty in accurate assessment.
In December 2021, a thorough literature search through MEDLINE (PubMed), CENTRAL (Cochrane Library) and LISTA (EBSCO) was conducted. Grey literature was not considered. For the systematic search, the following search terms were used without any filters or limits:
((Artificial Intelligence) OR (Deep Learning) OR (Machine Learning)) AND (malignant) AND (tumour OR neoplasm OR cancer) AND (musculoskeletal OR sarcoma OR bone OR (soft tissue)) AND (imaging OR radiographic OR (computer-assisted) OR (image interpretation))
Study titles were reviewed and evaluated by an MSK radiologist, an orthopaedic surgeon and a data scientist at our institution using the above selection criteria. All discrepancies were resolved by consensus. The results were summarised, and duplicates were discarded. All articles were initially screened for relevance by title and abstract to assess the inclusion criteria. The three authors independently performed a careful reading of the studies and extracted the data. The following information was extracted from each article: title, author, year of publication, tumour entity group, number of patients, malignancy, imaging modality, algorithm, model, task, applied metric, outcome label and if or if not focused on diagnosis. For the synthesis, studies with diagnosis-oriented tasks were further examined by retrieving the scores of the most common metrics and the number of class labels to assess the number of samples per class and illustrate a potential relationship between these parameters through linear analysis and a correlation coefficient. The level of evidence is level V.
Statistical analysis
Continuous data is reported as mean with standard deviation (SD) or median with interquartile range (IQR), and the respective interval. Discrete data was reported as incidence and percentage share per entity. Due to the heterogeneous nature and the limited amount of data, a non-parametric test was chosen to calculate a correlation coefficient for metric values and number of samples per class label for the diagnosis-oriented studies.
Results
Selection and methodological characteristics
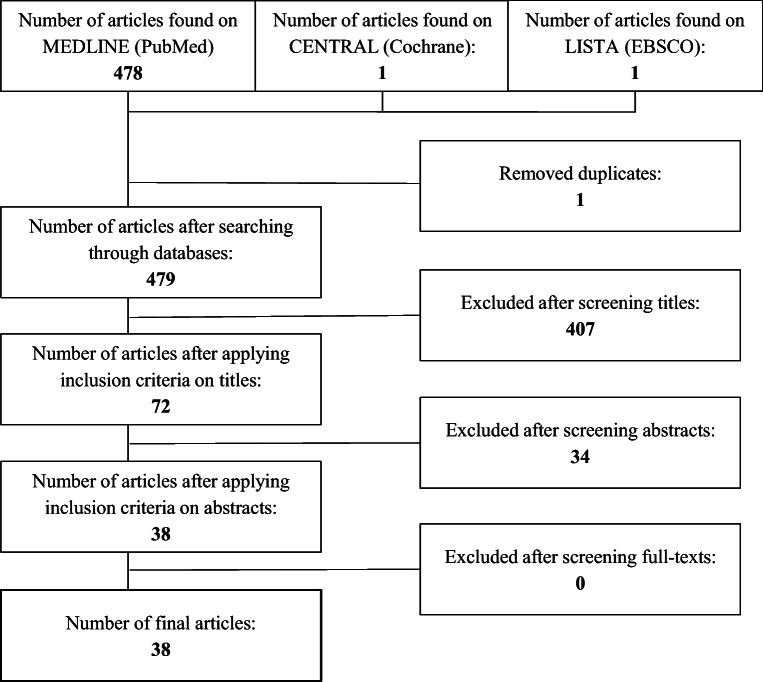
The first search resulted in 480 references in the databases mentioned above. One duplicate was discarded and 38 articles subsequently met the eligibility criteria (Fig. 1) [8, 10, 13–51]. Table 1 displays the final selection of articles with authors and continuous and discrete parameters. Final articles were published between 1994 and 2021. All 38 articles addressed an application of ML or DL with imaging data of MSK malignancies. Three review articles were found and excluded from statistical analysis [8, 14, 25]. 75.7% (28) of the studies were conducted retrospectively, 8.1% (3) were conducted prospectively and 16.2% (6) did not clearly state the study design. 60.5% (23) of the studies focused on bone, while 39.5% (15) focused on soft tissue tumours. 50.3% of the cases included were from patients with benign tumours, 3.0% were from patients with intermediate tumours, 37.4% were from patients with malignant tumours, 5.4% were from patients with metastases, 3.6% were from patients without tumours (healthy) and 0.5% did not provide any information. Further details are reported in Tables 2 and 3.
Fig. 1.
Selection process
Table 1.
Final articles with continuous and discrete parameters. Acc and AUC values as well as number of labels were further investigated for articles with diagnosis-oriented tasks
| Author | Year | Number of patients / cases | Healthy cases | Benign cases | Intermediate cases | Malignant cases | Metastases cases | Study design | Tumour entity group | Imaging modality | Radiomic data | Algorithm | Task | Model | Applied metric | Outcome label | Diagnosis-oriented | Acc | AUC | Number of labels |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bandyopadhyay et al | 2019 | 150 | 0 | 0 | 0 | 150 | 0 | Retrospective | Bone tumours | X-ray | No | Supervised | Classification | SVM, decision tree | acc, sens, Dice | Histopathological grading, staging | ✓ | 0.85 | 2 | |
| Banerjee et al | 2018 | 21 | 0 | 0 | 0 | 21 | 0 | Retrospective | Soft tissue tumours | MRI | No | Supervised | Classification | AlexNet | acc, AUC, sens, spec | Tumour entities | ✓ | 0.85 | 2 | |
| Chianca et al | 2021 | 146 | 0 | 49 | 0 | 40 | 57 | Retrospective | Bone tumours | MRI | Yes | Supervised | Classification | LogitBoost, SVM | AUC, sens, spec, acc | Malignancy | ✓ | 0.90 | 2 | |
| Do et al | 2021 | 1576 | 381 | 1061 | 0 | 134 | 0 | Retrospective | Bone tumours | X-ray | No | Supervised | Classification, segmentation | UNet | acc, IoU | Segmented tumour, tumour entities | ✓ | 0.99 | 3 | |
| Dufau et al | 2019 | 69 | 0 | 0 | 0 | 69 | 0 | Retrospective | Bone tumours | MRI | Yes | Supervised | Classification | SVM | AUC, sens, spec | Chemotherapy response assessment | × | |||
| Eweje et al | 2021 | 1060 | 0 | 582 | 0 | 478 | 0 | Retrospective | Bone tumours | MRI | No | Supervised | Classification | Efficient-Net, logistic regression | acc, sens, spec, AUC | Malignancy | ✓ | 0.79 | 2 | |
| Fields et al | 2021 | 128 | 0 | 36 | 0 | 92 | 0 | Retrospective | Soft tissue tumours | MRI | Yes | Supervised | Classification | Adaboost, random forest | AUC, sens, spec | Malignancy | ✓ | 0.77 | 2 | |
| Gao et al | 2021 | 30 | 0 | 0 | 0 | 30 | 0 | Prospective | Soft tissue tumours | MRI | No | Supervised | Classification | VGG19 | sens, spec, acc | Radiotherapy response assessment | × | |||
| Gao et al | 2020 | 30 | 0 | 0 | 0 | 30 | 0 | Prospective | Soft tissue tumours | MRI | Yes | Supervised | Classification | SVM, logistic regression | AUC | Radiotherapy response assessment | × | |||
| García-Gómez et al | 2004 | 430 | 0 | 267 | 0 | 163 | 0 | Retrospective | Soft tissue tumours | MRI | No | Supervised | Classification | K-nearest neighbour, SVM | sens, spec | Malignancy | ✓ | 0.90 | 2 | |
| Gitto et al | 2020 | 58 | 0 | 0 | 0 | 58 | 0 | Retrospective | Bone tumours | MRI | Yes | Supervised | Classification | LogitBoost | acc, AUC | Histopathological grading | ✓ | 0.75 | 0.78 | 2 |
| Glass et al | 1998 | 43 | 0 | 0 | 0 | 43 | 0 | Retrospective | Bone tumours | MRI | No | Unsupervised | Segmentation | Neural network | acc, sens, spec | Chemotherapy response assessment | × | |||
| He et al | 2020 | 1356 | 0 | 679 | 0 | 360 | 317 | Retrospective | Bone tumours | X-ray | No | Supervised | Classification | Efficient-Net | AUC, sens, spec, acc | Malignancy | ✓ | 0.73 | 2 | |
| Holbrook et al | 2020 | 79 | 0 | 0 | 0 | 79 | 0 | Unknown | Soft tissue tumours | MRI | Yes | Supervised | Segmentation | SVM, neural network | Dice, AUC | Segmented tumour | × | |||
| Hu et al | 2021 | 160 | 0 | 90 | 0 | 70 | 0 | Retrospective | Soft tissue tumours | MRI | Yes | Supervised | Classification | Least absolute shrinkage and selection operator | AUC, sens, spec, acc | Malignancy | ✓ | 0.92 | 0.96 | 2 |
| Hu et al | 2014 | 141 | 0 | 71 | 0 | 70 | 0 | Unknown | Bone tumours | X-ray | No | Supervised | Classification | SVM | acc, AUC, sens, spec | Tumour occurrence | ✓ | 0.96 | 2 | |
| Huang et al | 2020 | 12 | 0 | 0 | 0 | 12 | 0 | Prospective | Bone tumours | MRI | No | Supervised | Classification | Random forest | AUC, sens, spec, acc | Chemotherapy response assessment | × | |||
| Huang et al | 2017 | 23 | 0 | 0 | 0 | 23 | 0 | Unknown | Bone tumours | CT | No | Supervised | Segmentation | VGG16 | Dice score | Segmented tumour | × | |||
| Juntu et al | 2010 | 135 | 0 | 86 | 0 | 49 | 0 | Unknown | Soft tissue tumours | MRI | No | Supervised | Classification | SVM, neural network, decision tree | AUC, sens, spec, acc | Malignancy | ✓ | 0.93 | 2 | |
| Leporq et al | 2020 | 81 | 0 | 40 | 0 | 41 | 0 | Retrospective | Soft tissue tumours | MRI | Yes | Supervised | Classification | SVM | AUC, sens, spec, acc | Malignancy | ✓ | 0.95 | 0.96 | 2 |
| Li et al | 2019 | 210 | 0 | 154 | 0 | 56 | 0 | Retrospective | Bone tumours | MRI | Yes | Supervised | Classification | SVM | AUC, sens, spec, acc | Tumour entities | ✓ | 0.87 | 2 | |
| Liu et al | 2021 | 643 | 0 | 392 | 93 | 158 | 0 | Retrospective | Bone tumours | X-ray | No | Supervised | Classification | XGBoost, Inception V3 | AUC, sens, spec, acc | Malignancy | ✓ | 0.87 | 3 | |
| Pan et al | 2021 | 796 | 0 | 412 | 169 | 215 | 0 | Retrospective | Bone tumours | X-ray | No | Supervised | Classification | Random forest | AUC, acc | Malignancy | ✓ | 0.95 | 0.97 | 3 |
| Peeken et al | 2019 | 221 | 0 | 221 | 0 | 0 | 0 | Retrospective | Soft tissue tumours | CT | Yes | Supervised | Classification | Random forest | AUC, Dice | Histopathological grading | ✓ | 0.64 | 2 | |
| Peeken et al | 2018 | 136 | 0 | 0 | 0 | 136 | 0 | Retrospective | Soft tissue tumours | MRI, CT | No | Supervised | Classification | Random forest | AUC, sens, spec, acc | Prognosis | × | |||
| Reinus et al | 1994 | 709 | 0 | 492 | 0 | 217 | 0 | Retrospective | Bone tumours | X-ray | No | Supervised | Classification | Neural network | acc | Malignancy | ✓ | 0.85 | 2 | |
| Shen et al | 2018 | 36 | 0 | 15 | 0 | 21 | 0 | Unknown | Bone tumours | X-ray | No | Supervised | Classification | Random forest, SVM | AUC, sens, spec, acc | Malignancy | ✓ | 0.85 | 0.94 | 2 |
| Terunuma et al | 2018 | 1 | N/A | N/A | N/A | N/A | N/A | Retrospective | Bone tumours | X-ray | No | Supervised | Object detection, segmentation | SegNet | Jaccard index | Segmented tumour | × | |||
| von Schacky et al | 2021 | 934 | 0 | 623 | 0 | 311 | 0 | Retrospective | Bone tumours | X-ray | No | Supervised | Object detection, segmentation, classification | Mask-RCNN | acc, sens, spec, IoU, Dice | Malignancy | × | |||
| Vos et al | 2019 | 116 | 0 | 58 | 0 | 58 | 0 | Retrospective | Soft tissue tumours | MRI | Yes | Supervised | Classification | SVM, random forest | AUC, sens, spec | Tumour entities | ✓ | 0.89 | 2 | |
| Wang et al | 2021 | 227 | 0 | 147 | 0 | 80 | 0 | Retrospective | Bone tumours | US | No | Supervised | Classification | VGG16 | acc, sens, spec, AUC | Malignancy | ✓ | 0.79 | 0.91 | 2 |
| Wang et al | 2020 | 206 | 0 | 105 | 0 | 93 | 8 | Retrospective | Soft tissue tumours | MRI | Yes | Supervised | Classification | SVM, generalised linear models, random forest | AUC, sens, spec, acc | Malignancy | ✓ | 0.86 | 0.92 | 2 |
| Yin et al | 2019 | 120 | 0 | 0 | 30 | 54 | 36 | Retrospective | Bone tumours | MRI | Yes | Supervised | Classification | Random forest | AUC, acc | Segmented tumour, tumour entities | ✓ | 0.71 | 0.77 | 3 |
| Yin et al | 2019 | 95 | 0 | 0 | 42 | 53 | 0 | Retrospective | Bone tumours | CT | Yes | Supervised | Classification | Random forest | acc, AUC | Tumour entities | ✓ | 0.90 | 0.98 | 2 |
| Yin et al | 2021 | 795 | 0 | 215 | 0 | 399 | 181 | Retrospective | Bone tumours | CT | Yes | Supervised | Classification | Random forest | AUC, acc | Tumour entities | ✓ | 0.88 | 0.93 | 2 |
| Zhang et al | 2020 | 51 | N/A | N/A | N/A | N/A | N/A | Retrospective | Soft tissue tumours | MRI, CT | No | Supervised | Classification | Inception-v3 | acc, AUC | Histopathological grading | ✓ | 0.86 | 0.97 | 3 |
| Zhang et al | 2019 | 35 | 0 | 0 | 0 | 35 | 0 | Retrospective | Soft tissue tumours | MRI | Yes | Supervised | Classification | Random forest, SVM | AUC, sens, spec, acc | Histopathological grading | ✓ | 0.88 | 0.92 | 2 |
| Zhang et al | 2018 | 23 | 0 | 0 | 0 | 23 | 0 | Unknown | Bone tumours | CT | No | Supervised | Segmentation | ResNet-50 | Dice, sens | Segmented tumour | × |
SVM support vector machine, IoU intersection over union N/A not assessed
Table 2.
Continuous parameters with interval, median, mean IQR, and standard deviation
| Continuous parameters | |||||
|---|---|---|---|---|---|
| Parameter | Interval | Median | IQR | Mean | Std |
| Year of publication | [1994; 2021] | 2020 | 3 | 2018 | 6 |
| Number of patients/cases | [1; 1565] | 132.0 | 180.5 | 292.0 | 392.0 |
| Healthy | [0; 381] | 0.0 | 0.0 | 10.6 | 62.6 |
| Benign | [0; 1061] | 38.0 | 154.2 | 154.8 | 248.3 |
| Intermediate | [0; 169] | 0.0 | 4.6 | 9.3 | 32.0 |
| Malignant | [12; 478] | 69.5 | 79.5 | 115.1 | 113.4 |
| Metastases | [0; 317] | 0.0 | 4.3 | 17.1 | 60.4 |
IQR interquartile range, std standard deviation
Table 3.
Discrete parameters with incidence and percentage share per entity
| Discrete parameters | |||
|---|---|---|---|
| Parameter | Entity | Σ | % |
| Study design | |||
| Retrospective | 28 | 75.7% | |
| Prospective | 3 | 8.1% | |
| Unknown | 6 | 16.2% | |
| Task | |||
| Classification | 33 | 80.5% | |
| Segmentation | 6 | 14.6% | |
| Object detection | 2 | 4.9% | |
| Model | |||
| AlexNet | 1 | 1.9% | |
| LogitBoost | 2 | 3.8% | |
| Support vector machine | 14 | 26.4% | |
| U-Net | 1 | 1.9% | |
| Efficient-Net | 2 | 3.8% | |
| Logistic regression | 2 | 3.8% | |
| Adaboost | 1 | 1.9% | |
| Random forests | 12 | 22.6% | |
| VGG19 | 1 | 1.9% | |
| k-nearest neighbour | 1 | 1.9% | |
| Neural network | 4 | 7.5% | |
| LASSO | 1 | 1.9% | |
| VGG16 | 2 | 3.8% | |
| Decision tree | 2 | 3.8% | |
| XGBoost | 1 | 1.9% | |
| Inception v3 | 2 | 3.8% | |
| SegNet | 1 | 1.9% | |
| Mask RCNN | 1 | 1.9% | |
| Generalised linear model | 1 | 1.9% | |
| ResNet-50 | 1 | 1.9% | |
| Diagnosis oriented | |||
| Yes | 27 | 71.1% | |
| No | 11 | 28.9% | |
| Outcome label | |||
| Segmented tumour | 6 | 14.6% | |
| Tumour entities | 7 | 17.1% | |
| Tumour occurrence | 1 | 2.4% | |
| Histopathological grading | 5 | 12.2% | |
| Radiotherapy response | 2 | 4.9% | |
| Chemotherapy response | 3 | 7.3% | |
| Malignancy | 15 | 36.6% | |
| Staging | 1 | 2.4% | |
| Prognosis | 1 | 2.4% | |
| Tumour group | |||
| Bone tumour | 23 | 60.5% | |
| Soft tissue tumour | 15 | 39.5% | |
| Imaging modality | |||
| MRI | 22 | 55.0% | |
| CT | 7 | 17.5% | |
| X-ray | 10 | 25.0% | |
| US | 1 | 2.5% | |
| Radiomic data | |||
| Yes | 16 | 42.1% | |
| No | 22 | 57.9% | |
| Algorithm | |||
| Supervised | 37 | 97.4% | |
| Unsupervised | 1 | 2.6% | |
| Reinforcement | 0 | 0.0% | |
| Applied metric | |||
| Accuracy | 29 | 25.4% | |
| Sensitivity | 25 | 21.9% | |
| Specificity | 23 | 20.2% | |
| AUC | 28 | 24.6% | |
| Jaccard index | 1 | 0.9% | |
| Intersection over union | 2 | 1.8% | |
| Dice score | 6 | 5.3% | |
LASSO Least Absolute Shrinkage and Selection Operator
Narrative review of best studies
Several studies have presented novel and interesting implementations. However, we would like to highlight two studies that, in our opinion, provide very intriguing frameworks. Liu et al [35] demonstrated a ML-DL fusion model that integrates not only imaging but also clinical data to assess the malignancy of tumours. This approach is similar to the diagnostic procedure a radiologist would use to diagnose MSK lesions. A second noticeable study was published by von Schacky et al [42]: they presented a multi-task DL model that shows the potential of state-of-the-art DL by simultaneously detecting, segmenting and classifying image data. To classify the DL results in the context of “man vs. machine,” they were also compared with the results of radiologists of different experience levels demonstrating strengths and limitations of DL with limited data.
In-depth investigation of diagnosis-oriented tasks
Twenty-seven (71.1%) of the studies were diagnosis-oriented and mainly aimed at classification tasks [10, 13, 15, 16, 18, 19, 22, 23, 26, 28, 29, 32–37, 39, 40, 43–49, 51]. A median accuracy (Acc) of 0.88 with an interval of [0.71; 0.99] was found. For the area under the curve (AUC), the median resulted in 0.92 with a corresponding interval of [0.64; 0.98]. For the number of labels, a median of 2 with an interval of [2;3] was found. Further details are shown in Table 4.
Table 4.
Continuous parameters of diagnosis-oriented studies with interval, median, mean and standard deviation
| Continuous parameters of diagnosis-oriented parameters | |||||
|---|---|---|---|---|---|
| Parameter | Interval | Median | IQR | Mean | std |
| ACC | [0.71; 0.99] | 0.88 | 0.07 | 0.87 | 0.07 |
| AUC | [0.64; 0.98] | 0.92 | 0.14 | 0.88 | 0.09 |
| Number of labels | [2; 3] | 2 | 0 | 2.19 | 0.39 |
IQR interquartile range, std standard deviation
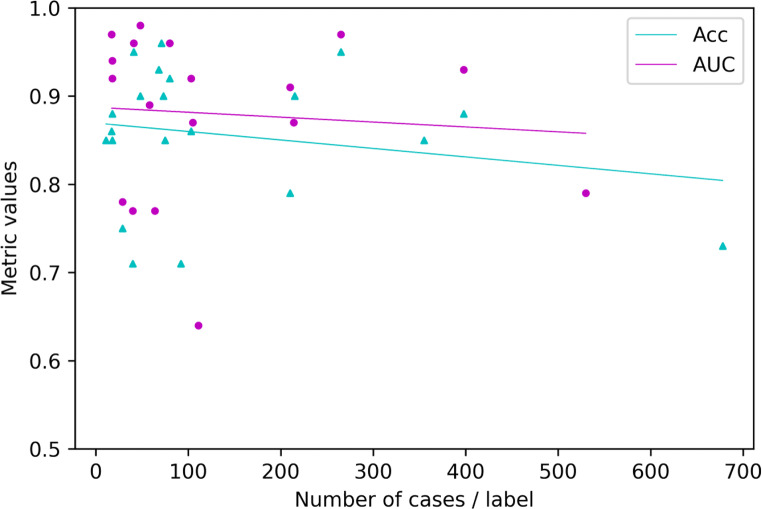
Figure 2 demonstrates the findings of a linear analysis of the metric values Acc and AUC on the vertical axis and the quotient of total number of cases and number of labels per class (= mean number of samples per class). Further, a correlation coefficient for each metric and the mean number of samples per class was calculated. The number of studies examined is limited, and the data found show considerable heterogeneity. Subsequently, a Spearman’s rank-order correlation coefficient, which is a measure for linear correlation between two datasets and does not assume that both datasets are normally distributed, was applied. We chose |ρ| > 0.5 to infer a significant direct or indirect correlation between two parameters for this study. The correlation coefficient for Acc and AUC against the mean number of samples per class resulted in ρ = − 0.204 / ρ = − 0.153, respectively. Therefore, both results represent no significant correlation coefficient.
Fig. 2.
Distribution of final metric scores against the mean number of samples per class label
Discussion
The most important finding of the presented review was that imaging-driven diagnosis for MSK malignancies does not yet experience significant impact by ML applications and this has several reasons associated with data.
The main issue might be the availability of data. In most research institutes, a systematic and structured collection of quality data does not yet seem to take place or has only recently been introduced. This can be derived from the fact that datasets in general are comparably small and dataset size is not increasing yet. Consequently, even if according patient data is existing, this does not necessarily imply data is present in a format, validity, accessibility, consistency and completeness feasible for data science. In addition, sarcomas are a very rare entity of cancer, which does not allow for fast gathering of sufficient prospective data. Terenuma et al [41] developed a technique to obtain multiple images from a single patient, which is from a data science perspective very intriguing, but does not provide enough data for a clinical application and is not generally transferable to any other study. Several mathematical techniques to cope with limited data have emerged (e.g. transfer learning [10], data augmentation [9]). However, these techniques can at this point only support an AI task, but not solve the issue of limited data. For rare diseases, building networks and databases on a national or even international basis might be a future solution. Another reason might be the considerably limited amount of research in the field of orthopaedic oncology, which can again partly be explained by insufficient data. With the respectively adapted search term, more than 1300 articles can be found for lung malignancies and even more than 2200 articles for breast malignancies, while only 480 articles were detected for MSK malignancies (initial search, each in December 2021). ML in general is still in its infancy, but more so in MSK and orthopaedic oncology.
A further finding was presented by synthesising the relationship of number of cases and number of labels per class against the metric values. In the research field of AI, it is common knowledge that the amount of data has profound impact on the model performance [10, 11, 52]. Nonetheless, Fig. 2 tells a different story. The median number of samples per class resulted in 75 and 59.3% of the diagnosis-oriented studies had less than 100 samples per class. Further, the mean metric scores of studies with fewer than 100 samples per class (Acc 0.86, AUC 0.89) were slightly higher than those of studies with more than 100 samples per class (Acc 0.85, AUC 0.86), as indicated by the linear regression lines in Fig. 2. This would suggest that less data leads to higher results. One explanation for these unexpected results could be the class imbalance: several studies developed models to classify tumour malignancy, for example [15, 18, 19, 22, 26, 28, 32, 33, 35, 36, 39, 40, 44, 45]. Benign MSK tumours occur more often than malignant MSK tumours, which results in a class imbalance in the dataset. Such an imbalance can lead to spuriously high metric values, especially for AUC. A detailed and interdisciplinary interpretation of results with regard to composition of data is crucial. Another issue associated with limited datasets and class imbalance is that specific classes of data might be sparse. Therefore, overfitting may occur, resulting in suboptimal results.
Yet another indication is that problem statements of most studies do not reflect real clinical scenarios. Most studies aim at distinguishing two to three specific tumour entities [10, 16, 34, 43, 46–48] or assessing tumour malignancy [15, 18, 19, 22, 26, 28, 32, 33, 35, 36, 39, 40, 42, 44, 45]. If one fed a third entity to a two-entity classifier, the model would try to fit the third entity into one of the first two entity classes. While confining a tumour entity from another is an imperative step in tumour assessment, nonetheless, most sarcoma diagnoses are incidental findings, and in daily practice, MSK radiologists and orthopaedic surgeons are first confronted with detecting a potential sarcoma at all [1, 4, 53]. Whereas von Schacky et al [42] aimed at differentiating various tumour entities, thus modelling a more realistic clinical scenario, the results were only moderate. More general models are needed to comply with clinical needs and difficulties. However, we hypothesise that this is again very difficult to achieve due to the very limited amount of data available and probably also closely related to the distribution of the data. Naturally, the quality and problems of AI models cannot be assessed by dataset size and data distribution alone, but data undoubtedly have major impact on the overall performance and clinical relevance.
No biopsy-focused studies
The most applied outcome labels among the 38 investigated original research articles were tumour malignancy (15, 36.6%) [15, 18, 19, 22, 26, 28, 32, 33, 35, 36, 39, 40, 42, 44, 45], tumour entities (7, 17.1%) [10, 16, 34, 43, 46–48] and segmented tumour (6, 14.6%) [16, 27, 31, 41, 46, 50]. A distinct finding of this review is that although a biopsy is a crucial step in the diagnostic process of MSK malignancies, there is no study focused on radiological images and biopsies. Retrieving relevant biopsy material—for example, via CT-guided needle biopsy—is a highly complex task and requires significant experience. From this, it could be derived that ML research in the field of MSK malignancies is currently not mainly oriented on medical needs, but models and research questions are built around available data. This underlines that ML is still in its very infancy in MSK tumour research.
MRI and radiomics
MRI is the most popular kind of imaging data for ML analysis at this point (55.0%, 22). This might be explained by the fact that MR imaging plays a fundamental role in the assessment of sarcomas due to superior soft tissue contrast and the desire to reduce unnecessary radiation dose. But also, from a data science perspective, this is comprehensible: with one patient, multiple 2D data samples (or one 3D data sample) are produced. Additionally, various image planes and weightings are possible. This suggests that less patients are necessary to acquire more data.
Likewise, radiomics appears to be on demand. 42.1% of articles (16) utilised radiomic data [15, 17, 19, 21, 23, 27, 28, 33, 34, 37, 43, 45–48, 51], while only 17.5% (7) integrated CT, 25.0% (10) X-ray and 2.5% (1) US. With radiomics, a large number of quantitative features can be extracted from imaging data. These are combined with other patient data and can be mined with modern techniques of e.g. bioinformatics and data science. In consequence, the popularity of radiomics might be associated with the capability to extract additional information from images and therefore tackle the issue of small datasets.
Limitations
This review article has several limitations. The major limitation is the early stage of the examined studies. Because ML in orthopaedic oncology is still in its infancy, most studies are also at an early stage, making it difficult to examine the impact of the studies presented and assess their quality. Most studies were not published until 2021. Further, the mean number of cases per study is 292. While a limited number of cases is related to the type of entities studied [53], the number is very small in the context of ML applications. These facts underline the early stage of the studies. Another limitation is the overall heterogeneity of the examined studies. We restricted the tumour entities and the type of data by the eligibility criteria. However, we did not impose any restrictions on ML algorithms, models, or tasks. Thus, the studies presented three distinct algorithm types, 20 different models and nine groups of outcome labels for various tasks.
Conclusion
In conclusion, for a rare disease, there are very limited amounts of data and no established large-scale networks between multiple national and international facilities yet. The impact of imaging-driven ML research in other disciplines is already present [52]. Also, several studies presented in this review demonstrated that ML can selectively support imaging-driven diagnosis for MSK malignancies. However, until statistically robust results can be achieved and clinically relevant models to cope with heterogeneous cases an orthopaedic surgeon or MSK radiologist encounters on a regular basis can be developed, data quality and quantity have to be improved. An expert radiologist from a specialised centre has seen thousands of images in his/her professional life and incorporates meta data as well as other factors into his/her decision-making process. In contrast, the presented studies only worked with 1 [41] up to 1576 [16] cases mostly focusing on one single kind of data and imaging modality.
The key to bring ML to a level where it can substantially impact clinical image interpretation in the diagnosis of MSK malignancies is data: establishing national and international networks, implementing a systematic and structural data acquisition and finally integrating multimodal data comparable to expert radiologists.
Acknowledgements
Many thanks to Fritz Seidl for his assistance with the language editing; looking forward to working with you again.
Abbreviations
- Acc
Accuracy
- AI
Artificial intelligence
- AUC
Area under the curve
- DL
Deep learning
- IoU
Intersection over union
- IQR
Interquartile range
- ML
Machine learning
- MSK
Musculoskeletal
- SD
Standard deviation
- SVM
Support vector machine
Funding
Open Access funding enabled and organised by Projekt DEAL. The authors state that this work has not received any funding.
Declarations
Guarantor
The scientific guarantor of this publication is Prof. MD Rainer Burgkart.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise (Florian Hinterwimmer).
Informed consent
Not applicable
Ethical approval
Not applicable
Methodology
• retrospective
• performed at one institution
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Grimer RJ, Briggs TW. Earlier diagnosis of bone and soft-tissue tumours. J Bone Joint Surg Br. 2010;92:1489–1492. doi: 10.1302/0301-620X.92B11.24326. [DOI] [PubMed] [Google Scholar]
- 2.Grimer RJ, Carter SR, Pynsent PB. The cost-effectiveness of limb salvage for bone tumours. J Bone Joint Surg Br. 1997;79:558–561. doi: 10.1302/0301-620x.79b4.7687. [DOI] [PubMed] [Google Scholar]
- 3.Rechl H, Kirchhoff C, Wortler K, Lenze U, Topfer A, von Eisenhart-Rothe R. Diagnosis of malignant bone and soft tissue tumors. Orthopade. 2011;40:931–941. doi: 10.1007/s00132-011-1821-7. [DOI] [PubMed] [Google Scholar]
- 4.Clark MA, Thomas JM. Delay in referral to a specialist soft-tissue sarcoma unit. Eur J Surg Oncol. 2005;31:443–448. doi: 10.1016/j.ejso.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 5.Ayala AG, Zornosa J. Primary bone tumors: percutaneous needle biopsy. Radiologic-pathologic study of 222 biopsies. Radiology. 1983;149:675–679. doi: 10.1148/radiology.149.3.6580673. [DOI] [PubMed] [Google Scholar]
- 6.Mankin HJ, Mankin CJ, Simon MA. The hazards of the biopsy, revisited. Members of the Musculoskeletal Tumor Society. J Bone Joint Surg Am. 1996;78:656–663. doi: 10.2106/00004623-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Savage N (2020) How AI is improving cancer diagnostics. Nature 579:S14+ [DOI] [PubMed]
- 8.Vogrin M, Trojner T, Kelc R. Artificial intelligence in musculoskeletal oncological radiology. Radiol Oncol. 2020;55:1–6. doi: 10.2478/raon-2020-0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zaman A, Park SH, Bang H, Park CW, Park I, Joung S. Generative approach for data augmentation for deep learning-based bone surface segmentation from ultrasound images. Int J Comput Assist Radiol Surg. 2020;15:931–941. doi: 10.1007/s11548-020-02192-1. [DOI] [PubMed] [Google Scholar]
- 10.Banerjee I, Crawley A, Bhethanabotla M, Daldrup-Link HE, Rubin DL. Transfer learning on fused multiparametric MR images for classifying histopathological subtypes of rhabdomyosarcoma. Comput Med Imaging Graph. 2018;65:167–175. doi: 10.1016/j.compmedimag.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Frangi AF, Tsaftaris SA, Prince JL. Simulation and synthesis in medical imaging. IEEE Trans Med Imaging. 2018;37:673–679. doi: 10.1109/TMI.2018.2800298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 13.Bandyopadhyay O, Biswas A, Bhattacharya BB. Bone-cancer assessment and destruction pattern analysis in long-bone X-ray image. J Digit Imaging. 2019;32:300–313. doi: 10.1007/s10278-018-0145-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chianca V, Albano D, Messina C, et al. An update in musculoskeletal tumors: from quantitative imaging to radiomics. Radiol Med. 2021;126:1095–1105. doi: 10.1007/s11547-021-01368-2. [DOI] [PubMed] [Google Scholar]
- 15.Chianca V, Cuocolo R, Gitto S, et al. Radiomic machine learning classifiers in spine bone tumors: a multi-software, multi-scanner study. Eur J Radiol. 2021;137:109586. doi: 10.1016/j.ejrad.2021.109586. [DOI] [PubMed] [Google Scholar]
- 16.Do NT, Jung ST, Yang HJ, Kim SH (2021) Multi-level seg-unet model with global and patch-based X-ray images for knee bone tumor detection. Diagnostics, 11(4):691 [DOI] [PMC free article] [PubMed]
- 17.Dufau J, Bouhamama A, Leporq B, et al. Prediction of chemotherapy response in primary osteosarcoma using the machine learning technique on radiomic data. Bull Cancer. 2019;106:983–999. doi: 10.1016/j.bulcan.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 18.Eweje FR, Bao B, Wu J, et al. Deep learning for classification of bone lesions on routine MRI. EBioMedicine. 2021;68:103402. doi: 10.1016/j.ebiom.2021.103402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fields BKK, Demirjian NL, Hwang DH, et al. Whole-tumor 3D volumetric MRI-based radiomics approach for distinguishing between benign and malignant soft tissue tumors. Eur Radiol. 2021;31:8522–8535. doi: 10.1007/s00330-021-07914-w. [DOI] [PubMed] [Google Scholar]
- 20.Gao Y, Ghodrati V, Kalbasi A, et al. Prediction of soft tissue sarcoma response to radiotherapy using longitudinal diffusion MRI and a deep neural network with generative adversarial network-based data augmentation. Med Phys. 2021;48:3262–3372. doi: 10.1002/mp.14897. [DOI] [PubMed] [Google Scholar]
- 21.Gao Y, Kalbasi A, Hsu W, et al. Treatment effect prediction for sarcoma patients treated with preoperative radiotherapy using radiomics features from longitudinal diffusion-weighted MRIs. Phys Med Biol. 2020;65:175006. doi: 10.1088/1361-6560/ab9e58. [DOI] [PubMed] [Google Scholar]
- 22.García-Gómez JM, Vidal C, Martí-Bonmatí L, et al. Benign/malignant classifier of soft tissue tumors using MR imaging. MAGMA. 2004;16:194–201. doi: 10.1007/s10334-003-0023-7. [DOI] [PubMed] [Google Scholar]
- 23.Gitto S, Cuocolo R, Albano D, et al. MRI radiomics-based machine-learning classification of bone chondrosarcoma. Eur J Radiol. 2020;128:109043. doi: 10.1016/j.ejrad.2020.109043. [DOI] [PubMed] [Google Scholar]
- 24.Glass JO, Reddick WE. Hybrid artificial neural network segmentation and classification of dynamic contrast-enhanced MR imaging (DEMRI) of osteosarcoma. Magn Reson Imaging. 1998;16:1075–1083. doi: 10.1016/s0730-725x(98)00137-4. [DOI] [PubMed] [Google Scholar]
- 25.Gorelik N, Chong J, Lin DJ. Pattern recognition in musculoskeletal imaging using artificial intelligence. Semin Musculoskelet Radiol. 2020;24:38–49. doi: 10.1055/s-0039-3400266. [DOI] [PubMed] [Google Scholar]
- 26.He Y, Pan I, Bao B, et al. Deep learning-based classification of primary bone tumors on radiographs: a preliminary study. EBioMedicine. 2020;62:103121. doi: 10.1016/j.ebiom.2020.103121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holbrook MD, Blocker SJ, Mowery YM, et al. MRI-based deep learning segmentation and radiomics of sarcoma in mice. Tomography. 2020;6:23–33. doi: 10.18383/j.tom.2019.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hu P, Chen L, Zhou Z. Machine learning in the differentiation of soft tissue neoplasms: comparison of fat-suppressed T2WI and apparent diffusion coefficient (ADC) features-based models. J Digit Imaging. 2021;34:1146–1155. doi: 10.1007/s10278-021-00513-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hu S, Xu C, Guan W, Tang Y, Liu Y. Texture feature extraction based on wavelet transform and gray-level co-occurrence matrices applied to osteosarcoma diagnosis. Biomed Mater Eng. 2014;24:129–143. doi: 10.3233/BME-130793. [DOI] [PubMed] [Google Scholar]
- 30.Huang B, Wang J, Sun M, et al. Feasibility of multi-parametric magnetic resonance imaging combined with machine learning in the assessment of necrosis of osteosarcoma after neoadjuvant chemotherapy: a preliminary study. BMC Cancer. 2020;20:322. doi: 10.1186/s12885-020-06825-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang L, Xia W, Zhang B, Qiu B, Gao X. MSFCN-multiple supervised fully convolutional networks for the osteosarcoma segmentation of CT images. Comput Methods Programs Biomed. 2017;143:67–74. doi: 10.1016/j.cmpb.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 32.Juntu J, Sijbers J, De Backer S, Rajan J, Van Dyck D. Machine learning study of several classifiers trained with texture analysis features to differentiate benign from malignant soft-tissue tumors in T1-MRI images. J Magn Reson Imaging. 2010;31:680–689. doi: 10.1002/jmri.22095. [DOI] [PubMed] [Google Scholar]
- 33.Leporq B, Bouhamama A, Pilleul F, et al. MRI-based radiomics to predict lipomatous soft tissue tumors malignancy: a pilot study. Cancer Imaging. 2020;20:78. doi: 10.1186/s40644-020-00354-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li L, Wang K, Ma X, et al. Radiomic analysis of multiparametric magnetic resonance imaging for differentiating skull base chordoma and chondrosarcoma. Eur J Radiol. 2019;118:81–87. doi: 10.1016/j.ejrad.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Liu R, Pan D, Xu Y et al (2021) A deep learning-machine learning fusion approach for the classification of benign, malignant, and intermediate bone tumors. Eur Radiol. 10.1007/s00330-021-08195-z [DOI] [PubMed]
- 36.Pan D, Liu R, Zheng B, et al. Using machine learning to unravel the value of radiographic features for the classification of bone tumors. Biomed Res Int. 2021;2021:8811056. doi: 10.1155/2021/8811056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peeken JC, Bernhofer M, Spraker MB, et al. CT-based radiomic features predict tumor grading and have prognostic value in patients with soft tissue sarcomas treated with neoadjuvant radiation therapy. Radiother Oncol. 2019;135:187–196. doi: 10.1016/j.radonc.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 38.Peeken JC, Goldberg T, Knie C, et al. Treatment-related features improve machine learning prediction of prognosis in soft tissue sarcoma patients. Strahlenther Onkol. 2018;194:824–834. doi: 10.1007/s00066-018-1294-2. [DOI] [PubMed] [Google Scholar]
- 39.Reinus WR, Wilson AJ, Kalman B, Kwasny S. Diagnosis of focal bone lesions using neural networks. Invest Radiol. 1994;29:606–611. doi: 10.1097/00004424-199406000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Shen R, Li Z, Zhang L, et al. Osteosarcoma patients classification using plain X-rays and metabolomic data. Annu Int Conf IEEE Eng Med Biol Soc. 2018;2018:690–693. doi: 10.1109/EMBC.2018.8512338. [DOI] [PubMed] [Google Scholar]
- 41.Terunuma T, Tokui A, Sakae T. Novel real-time tumor-contouring method using deep learning to prevent mistracking in X-ray fluoroscopy. Radiol Phys Technol. 2018;11:43–53. doi: 10.1007/s12194-017-0435-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.von Schacky CE, Wilhelm NJ, Schäfer VS, et al. Multitask deep learning for segmentation and classification of primary bone tumors on radiographs. Radiology. 2021;301:398–406. doi: 10.1148/radiol.2021204531. [DOI] [PubMed] [Google Scholar]
- 43.Vos M, Starmans MPA, Timbergen MJM, et al. Radiomics approach to distinguish between well differentiated liposarcomas and lipomas on MRI. Br J Surg. 2019;106:1800–1809. doi: 10.1002/bjs.11410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang B, Perronne L, Burke C, Adler RS. Artificial intelligence for classification of soft-tissue masses at US. Radiol Artif Intell. 2021;3:e200125. doi: 10.1148/ryai.2020200125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang H, Zhang J, Bao S, et al. Preoperative MRI-based radiomic machine-learning nomogram may accurately distinguish between benign and malignant soft-tissue lesions: a two-center study. J Magn Reson Imaging. 2020;52:873–882. doi: 10.1002/jmri.27111. [DOI] [PubMed] [Google Scholar]
- 46.Yin P, Mao N, Zhao C, Wu J, Chen L, Hong N. A triple-classification radiomics model for the differentiation of primary chordoma, giant cell tumor, and metastatic tumor of sacrum based on T2-weighted and contrast-enhanced T1-weighted MRI. J Magn Reson Imaging. 2019;49:752–759. doi: 10.1002/jmri.26238. [DOI] [PubMed] [Google Scholar]
- 47.Yin P, Mao N, Zhao C, et al. Comparison of radiomics machine-learning classifiers and feature selection for differentiation of sacral chordoma and sacral giant cell tumour based on 3D computed tomography features. Eur Radiol. 2019;29:1841–1847. doi: 10.1007/s00330-018-5730-6. [DOI] [PubMed] [Google Scholar]
- 48.Yin P, Zhi X, Sun C, et al. Radiomics models for the preoperative prediction of pelvic and sacral tumor types: a single-center retrospective study of 795 cases. Front Oncol. 2021;11:709659. doi: 10.3389/fonc.2021.709659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang L, Ren Z. Comparison of CT and MRI images for the prediction of soft-tissue sarcoma grading and lung metastasis via a convolutional neural networks model. Clin Radiol. 2020;75:64–69. doi: 10.1016/j.crad.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 50.Zhang R, Huang L, Xia W, Zhang B, Qiu B, Gao X. Multiple supervised residual network for osteosarcoma segmentation in CT images. Comput Med Imaging Graph. 2018;63:1–8. doi: 10.1016/j.compmedimag.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 51.Zhang Y, Zhu Y, Shi X, et al. Soft tissue sarcomas: preoperative predictive histopathological grading based on radiomics of MRI. Acad Radiol. 2019;26:1262–1268. doi: 10.1016/j.acra.2018.09.025. [DOI] [PubMed] [Google Scholar]
- 52.Rajpurkar P, Chen E, Banerjee O, Topol EJ. AI in health and medicine. Nat Med. 2022;28:31–38. doi: 10.1038/s41591-021-01614-0. [DOI] [PubMed] [Google Scholar]
- 53.Picci P, Manfrini M, Donati D et al (2020) Diagnosis of Musculoskeletal Tumors and Tumor-like Conditions: Clinical, Radiological and Histological Correlations-the Rizzoli Case Archive (pp. 3–11). Cham: Springer