Abstract
Objective
To get a feedback from students participating in a skill enhancement course where a combination of a 3D-printed mandible with a natural tooth in place of the impacted tooth for surgical training is used and to compare it to an animal jaw model used for the same purpose.
Methods
41 participants were enrolled for the study, and extraction procedure was performed on both the bovine jaw and the 3D-printed mandible. Participants evaluated both models using a validated questionnaire to assess the anatomical and operative simulation and to compare its cost effectiveness.
Results
Overall significant differences between the two models were found in the student assessment. Whilst the animal jaw models achieved better results in the haptic feedback of the soft tissue, the 3D-printed models were regarded significantly more realistic with regard to the anatomical correctness, the degree of freedom of movement and the operative simulation.
Conclusion
The 3D-printed models presented a realistic alternative to cadaveric jaw models in the training of operational skills of dental surgeons. Whilst the 3D-printed models received positive feedback from students in a hands-on course, some aspects of the model leave room for improvement.
Keywords: 3D printing, 3D rapid prototyping, Dentoalveolar surgery, Impacted teeth, Simulation training, Cadaveric jaw training
Introduction
A significant part of dental training includes acquisition of clinical and surgical skills. Various treatment procedures carried out in the dental clinic require an understanding of the precise anatomy and careful handling of the tissues in that region. This skill acquisition as a part of dental training is done before directly performing the procedure on a patient to be able to practice repeatedly and finally perform the procedure confidently.
Surgical proficiency is acquired through a long and meticulous process either in the form of learning by cadaver dissection, practice on prefabricated models or apprenticeship under senior surgeons till the surgeon feels comfortable to be able to perform independently. Traditionally, biological specimens (bovine or porcine) jaw models have been used in the pre-clinical setting to develop surgical competency during dental procedure training [1, 2]. These animal models come with the advantage of having hard and soft tissues similar to the oral environment. Various procedures such as soft tissue incisions, grafting techniques, sinus lift and other surgical procedures are demonstrated and performed on animal jaws by students as it simulates the soft tissue close to the natural tissues [1, 2]. These animal models, however, have problems related to biosafety factors and become expensive as it includes the cost of safe transportation and storage. There is a need to design and fabricate realistic anatomical phantoms which can be both economical and reproduceable to be feasible for use in the pre-clinical setting. The challenge is to be able to reproduce the soft tissue and simulated bony tissue with an anatomically realistic density to be used for osteotomy. This improves the surgical tactile simulation which enhances the quality of the surgical training.
Additive manufacturing enables us to fabricate more realistic 3D models using different materials simulating anatomical properties of different tissues. High fidelity anatomical models developed using 3D printing have now proved to benefit young surgeons who are gradually ascending the learning curve as they can repeatedly use these models for training until they are confident of the procedure. This is not possible using animal biological specimens due to their limited availability. Advances in technology have now made 3D-printed models a newer alternative for the training of dental students and clinicians in skill enhancement. The cost can be minimized with the use of models printed using FDM technology with simple desktop printers [3]. The models have the advantage of being able to simulate the patient’s jaw anatomically and can be custom-printed to simulate bone density by altering the fill capacity [4]. The use of natural extracted teeth in different pre-clinical dental training programs is well known [5, 6]. It gives the participant a perfect resemblance to the natural tooth in terms of density and texture. This is especially true in case of simulated procedures for removal of impacted teeth.
The student needs to feel the resemblance to the soft tissue, the bone surrounding the tooth, the tooth structure and texture and the periodontal tissues. A combination of a 3D-printed mandible with a natural tooth in place of the impacted tooth can give the student a more realistic approach to the surgical removal of impacted tooth in the model. This model was used in a skill enhancement program teaching the participants the surgical removal of impacted teeth.
The purpose of this study was to get a feedback from students participating in this skill enhancement course regarding this novel educational model used for surgical training and to compare it to an animal jaw model used for the same purpose.
Materials and Methods
Participants
Dental interns and practitioners who were interested in improving their surgical skill attended a skill enhancement course teaching them the skill of removing an impacted third molar. They were asked to volunteer for this study by answering a questionnaire at the end of the hands-on session. After a detailed orientation, the surgical procedure was demonstrated on the models by experienced surgeons in a hands-on session. This procedure was then replicated under supervision by the participants for the surgical removal of impacted teeth first using fresh goat jaws and subsequently on 3D-printed mandibles with a sterilized extracted tooth fixed in the third molar region in a mesio-angular impacted position.
Design and Fabrication of the 3D Model
A patient with bilateral mesio-angular impacted third molars was selected, and a CBCT was taken for the surgical removal of the same. The mandible was scanned using a high-resolution CBCT (Hyperion X9Pro MyRay®) with the following parameters 16-bit dynamic range, image voxel size 75 µm and FOV 10 × 8 set in the standard mode to get the maximum bone threshold.
The Digital Imaging and Communications in Medicine (DICOM) data of the two-dimensional image slices from CBCT scan were imported into a medical imaging and computer-aided design (CAD) software. Following this, optimal bone thresholding values were applied, and a 3D virtual volumetric reconstruction of the patient's mandible anatomy was generated (Fig. 1).
Fig. 1.
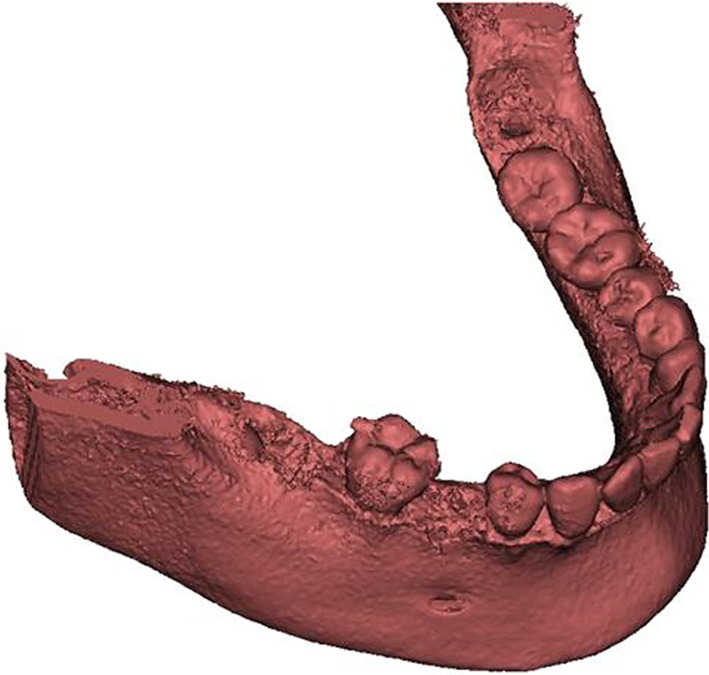
3D virtual volumetric reconstruction of the patient's mandible anatomy
Bilateral impacted mandibular third molars were virtually removed leaving behind an empty socket in the same angulation as the impacted tooth. The models were printed using a MakerBot® FDM 3D printer using PLA material with the density of bone set to 40% of the fill capacity (In fill of 3D model). This gave a texture to the cortical and medullary bone simulating the natural bone texture.
A previously extracted mandibular molar was cleaned to remove debris first under running water and then using an ultrasonic bath. The tooth was then soaked in 10% formalin for a week and autoclaved at 121 degrees centigrade at 15 psi pressure for about 40 min using a steam autoclave.
This sterilized extracted tooth was inserted into the empty third molar socket in the 3D-printed mandible model. To simulate the periodontal tissues around the tooth, hot silicon glue was placed into the empty socket followed by insertion of the tooth firmly into a mesio-angular position. This hot silicon glue not only kept the tooth in place but also formed a thin resilient layer around the roots of the extracted tooth representing the periodontal tissue.
Silicone rubber was then used to form a simulated soft tissue layer around the buccal and lingual aspects of the jaw. This was also extended in the interdental regions resembling gingival tissue.
Animal Jaw Model
Fresh goat jaws were obtained from the local slaughterhouse with the teeth and gingival tissue intact. One jaw was given to each participant (Fig. 2).
Fig. 2.

Fresh goat jaw
Hands on Procedure
Participants in the surgical skill enhancement program voluntarily enrolled for this study. 41 participants from both genders with almost similar clinical experience were enrolled for the study. The hands-on procedure was first demonstrated by experienced oral and maxillofacial surgeons on both the animal jaw and the 3D-printed mandible. The procedure started with examination of the tooth and surrounding structures, a mucoperiosteal incision, exposure of the tooth, bony osteotomy and splitting the tooth vertically to remove interference to the path of removal (Figs. 3, and 4). The distal part of the tooth was elevated first using a Coupland’s elevator. This was followed by the elevation of the mesial portion of the tooth.
Fig. 3.

Mucoperiosteal incision placed on the simulated soft tissue flap of 3D model to expose the impacted tooth
Fig. 4.

Splitting the tooth vertically to remove interference to the path of removal
The participants were divided into groups to perform the surgical procedure first on the animal jaw and then on the 3D-printed mandible with the extracted tooth in the third molar region. Operative simulation was maintained similar to the surgical environment with the use of appropriate instruments. The presence of the silicon glue around the impacted tooth created a resilience on elevation simulating periodontal tissues. After removing the tooth, the simulated soft tissue flap was repositioned and sutured carefully (Figs. 5 and 6).
Fig. 5.

Removal of impacted third molar
Fig. 6.

The simulated soft tissue flap being repositioned and sutured carefully
The participants were then given a questionnaire to assess the anatomical and operative simulation and to compare the cost effectiveness of both the models.
Statistical Analysis
The data were entered and analysed on SPSS version 22. P value was set significant equal to or less than 5% (0.05).
Results
A total of 41 candidates participated in the study. 23 were male and 18 were female participants. The age varied from 22 to 28 years, and the clinical experience ranged from 1 to 5 years with maximum participants being in the range of 2–4 years of experience.
Considering the sample simulation to a real human jaw, most participants scored positively on 3D-printed mandible being realistic and bearing simulation in the hard tissue component which was statistically significant. The simulation of impacted tooth and its root pattern to that of a natural tooth was significantly higher in 3D-printed model when compared to that of cadaveric model. The 3D-printed models were also rated significantly higher in feedback of the simulation of the periodontal tissue in the model to that of the natural periodontal tissue. The haptic feedback of the soft tissue component was rated better in the cadaveric jaws as also the mucoperiosteal incision which was considered more realistic by the participants when compared to the silicon rubber soft tissue component in the 3D-printed model.
The osteotomy on the 3D-printed mandible for surgical removal of the natural tooth simulated natural bone more than the cadaveric jaw. The most significant difference was noted in the haptic feedback of the tooth sectioning being closest to the natural tooth in the 3D-printed mandible as compared to the cadaveric jaw. The elevation of sectioned tooth fragments simulated a resistance which closely resembled the natural periodontal tissue in 3D-printed models. Removal of fractured root from a 3D-printed model closely simulated natural tooth removal over a cadaveric jaw tooth.
In the free text commentary section, participants commented on the fragility of the silicon rubber simulated gingiva on the 3D model making it tear during reflection and suturing. Comments were also noted on the realistic simulation of the natural tooth during tooth sectioning. The students particularly appreciated the use of dental elevators to remove individual sectioned tooth fragments with the resilience of the periodontal tissue created by the silicone glue. Suggestions for improvement included use of better soft tissue materials and fabrication of models with different impacted teeth positions for better exposure to different clinical situations. (Table 1).
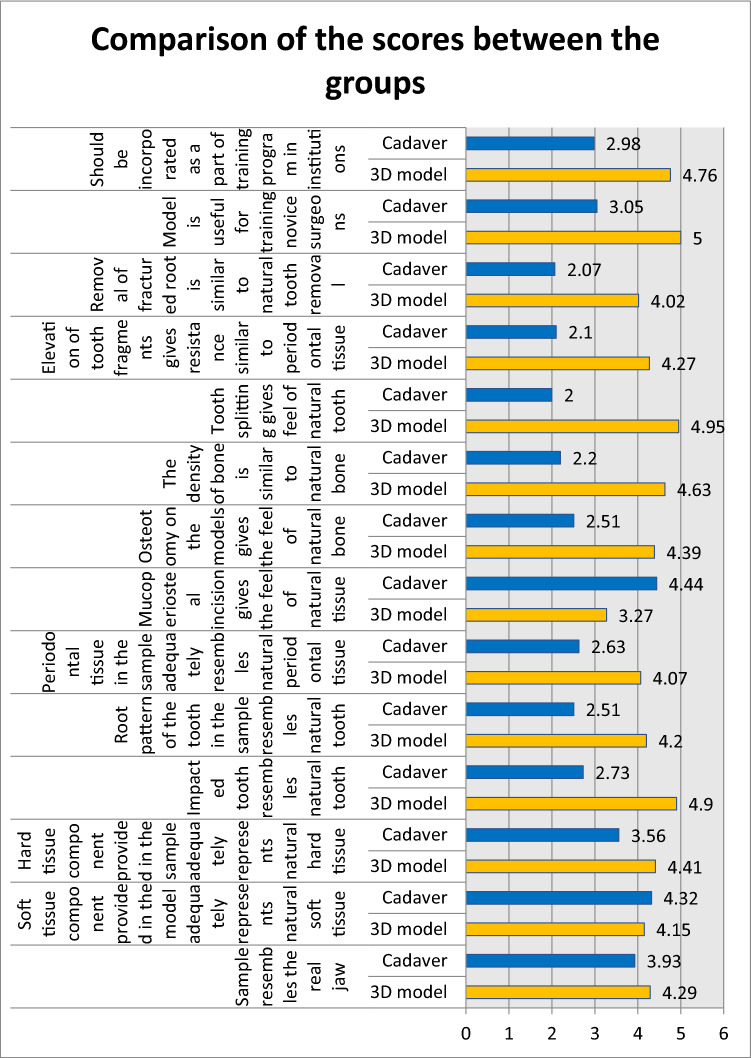
Table 1.
Comparison of the groups using independent sample t test
| Min | Max | Mean | S.D | Mean diff | P value | ||
|---|---|---|---|---|---|---|---|
| Sample resembles the real jaw | 3D model | 4 | 5 | 4.29 | .461 | 0.36 | 0.00* |
| Cadaver | 3 | 5 | 3.93 | .346 | |||
| Soft tissue component provided in the model adequately represents natural soft tissue | 3D model | 4 | 5 | 4.15 | .358 | – 0.17 | 0.068 |
| Cadaver | 4 | 5 | 4.32 | .471 | |||
| Hard tissue component provided in the sample adequately represents natural hard tissue | 3D model | 4 | 5 | 4.41 | .499 | 0.85 | 0.00* |
| Cadaver | 2 | 4 | 3.56 | .634 | |||
| Impacted tooth resembles natural tooth | 3D model | 4 | 5 | 4.90 | .300 | 2.17 | 0.00* |
| Cadaver | 1 | 4 | 2.73 | .708 | |||
| Root pattern of the tooth in the sample resembles natural tooth | 3D model | 3 | 5 | 4.20 | .511 | 1.68 | 0.00* |
| Cadaver | 1 | 4 | 2.51 | .711 | |||
| Periodontal tissue in the sample adequately resembles natural periodontal tissue | 3D model | 3 | 5 | 4.07 | .519 | 1.43 | 0.00* |
| Cadaver | 1 | 4 | 2.63 | .767 | |||
| Mucoperiosteal incision gives the feel of natural tissue | 3D model | 2 | 5 | 3.27 | .775 | – 1.17 | 0.00* |
| Cadaver | 2 | 5 | 4.44 | .634 | |||
| Osteotomy on the models gives the feel of natural bone | 3D model | 3 | 5 | 4.39 | .542 | 1.87 | 0.00* |
| Cadaver | 1 | 4 | 2.51 | .840 | |||
| The density of bone is similar to natural bone | 3D model | 4 | 5 | 4.63 | .488 | 2.43 | 0.00* |
| Cadaver | 1 | 4 | 2.20 | .782 | |||
| Tooth splitting gives feel of natural tooth | 3D model | 4 | 5 | 4.95 | .218 | 2.95 | 0.00* |
| Cadaver | 1 | 4 | 2.00 | .632 | |||
| Elevation of tooth fragments gives resistance similar to periodontal tissue | 3D model | 3 | 5 | 4.27 | .501 | 2.17 | 0.00* |
| Cadaver | 1 | 4 | 2.10 | .583 | |||
| Removal of fractured root is similar to natural tooth removal | 3D model | 3 | 5 | 4.02 | .524 | 1.95 | 0.00* |
| Cadaver | 1 | 3 | 2.07 | .519 | |||
| Model is useful for training novice surgeons | 3D model | 5 | 5 | 5.00 | .000 | 1.95 | 0.00* |
| Cadaver | 2 | 4 | 3.05 | .384 | |||
| Should be incorporated as a part of training program in institutions | 3D model | 4 | 5 | 4.76 | .435 | 1.78 | 0.00* |
| Cadaver | 2 | 4 | 2.98 | .273 |
*significant
The fabrication of 20 3D models using PLA filament and coating it with silicone rubber approximated to a total of 10,000 rupees (around 500 rupees for a complete model). The cost of 20 cadaveric goat jaws amounted to 16,000 rupees (approximately 800 rupees for a single jaw). An additional 2000 rupees was spent on the safe disposal of the jaws after use.
In our study, the 3D-printed models were rated significantly more realistic than the cadaveric models making it useful for training of novice surgeons and considering it to be incorporated as a part of training program in institutions. (Fig. 7).
Fig. 7.
Graph 1: Comparison of scores between both groups
Discussion
Traditional methods for surgical skill acquisition involve the use of cadaveric specimen in a pre-clinical environment. However, there are certain limitations to the use of biological specimens such as biosafety, ethical/religious issues, storage, transportation and disposal of the specimen. The biological specimen may not completely represent the human anatomy in most cases discouraging its use in the pre-clinical setting. Shah and Ahmed [7] have pointed out the preferences of students to use a more multimodal kinesthetic or tactile way of learning. High fidelity phantoms enable trainees to get a superior understanding of the anatomy with these graspable models. There is an increasing need to develop realistic and high-fidelity simulations representing the clinical environment for surgical training of dental students. The materials used to fabricate the models should have physical, visual, and tactile characteristics to simulate the human tissues sufficiently [7]. Fabrication of such high-fidelity models make them a viable educational tool in the pre-clinical setting for improvement of psychomotor skills in a more realistic environment.
The present study was conducted to analyse the benefits of using 3D-printed jaw models with a natural extracted tooth inserted in it for surgical skill enhancement of dental professionals in comparison with routinely used animal jaws. The comparison was done on 41 enrolled course participants using a questionnaire given to them at the end of the hands-on session.
The anatomical similarity of the hard and soft tissues was assessed in both the models, and it was noted that the animal jaws noted better scores with respect to the soft tissue simulation not only in appearance but also during the mucoperiosteal incision. Similar results were obtained by Mariana S. Ragghianti Zangrando’s study [1] with regard to soft tissue simulation and mucoperiosteal incisions. On the contrary, Lukas B. Seifert [2] in their comparative study found superior scores for intra-oral incisions and hard tissue anatomy precision in 3D-printed models compared to cadaveric models. It was noted that the 3D-printed models received a better score in terms of a more anatomical realism, the density of the model being closer to bone density during osteotomy. Similar results were obtained by various authors like Juhno Lee [8], Michael Bohl [9] and Meir Max Barak[10]. The natural tooth placed in the impacted tooth region received maximum scores for not only the anatomical simulation but also for the operative simulation, especially during the tooth split and elevation.
An important step in designing a model as an educational tool is to first define the learning objectives of that model. By understanding this objective, we can select the appropriate material based on its properties and fabricate the surrounding structures accordingly. Anatomical phantoms have been fabricated using PLA or ABS as the material using an FDM printer [2]. Not only is it the most accessible and cost-effective technology, but it also represents and simulates the hard tissue of the mandible adequately [8, 9]. By altering the infill capacity to (10 to 40 percent), it can create a high-fidelity model with adequate haptic feedback. The soft tissue surrounding the mandible was fabricated using silicone rubber. Although many of the participants were satisfied with the soft tissue simulation, some of them commented that in comparison with the cadaveric model, this was too fragile, especially during suturing.
The natural tooth was placed in a socket created in the model and stabilized using a layer of hot silicone glue. This helped in the retention of the tooth in the model and provided a small flexible layer around the tooth which simulated the periodontal ligament tissue as seen around a natural tooth. The procedure during the course was to place an incision and reflect a flap, osteotomy around the tooth using rotary instruments with adequate cooling techniques to simulate the clinical procedure. The tooth was then split, and using an elevator, it was luxated and elevated from the socket. The presence of the silicone glue layer helped to simulate the clinical situation satisfactorily by simulating periodontal ligament.
A combination of different materials to represent different tissues and use of a hybrid approach where a natural tooth is placed in the 3D-printed model made this surgical model unique when compared to the cadaveric model. Further improvement can be done to make this model more representative. PLA 3D-printed models can be custom-printed according to the use. It can be used as an educational model. Use of natural extracted teeth for training purposes is not a new concept. It has been used for various aspects of dental training. In a study by D.I.Al Sudani et al. [5], it was seen that the extracted teeth were sterilized to make it safe for use and disposed after using standard protocols for natural teeth disposal.
The realism, usefulness and cost effectiveness of both the models were analysed using independent E T test. Combining the usefulness of a natural tooth with a 3D-printed jaw is a novel concept adopted in this course. This gave us the benefit of the natural jaw appearance, near natural density of the model for osteotomy and the natural feel whilst splitting the tooth. The use of silicon glue to stabilize the tooth gave a thin soft film around the tooth giving it the simulation of periodontal tissue during elevation of the tooth or root fragments.
Conclusion
Through this study, we intended to describe a method to fabricate patient specific models based on real patient simulation using 3D printing technology and compared them to cadaveric jaw models. Overall, the 3D-printed models presented a realistic alternative to cadaveric models in the training of operational skills of dental practitioners. Whilst the 3D-printed models received positive feedback from students in a hands-on course, some aspects of the model leave room for improvement.
Acknowledgements
Not applicable.
Funding
No funds, Grants or other support was received.
Declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zangrando M, Sant’Ana A, Greghi S, De Rezende M, Damante C. Pig mandible as a valuable tool to improve periodontal surgery techniques. Int Educ Stud. 2014;7(10):82–88. doi: 10.5539/ies.v7n10p82. [DOI] [Google Scholar]
- 2.Seifert L, Schnurr B, Herrera-Vizcaino C, et al. 3D-printed patient individualised models vs cadaveric models in an undergraduate oral and maxillofacial surgery curriculum: comparison of student's perceptions. Eur J Dent Educ. 2020;24(4):799–806. doi: 10.1111/eje.12522. [DOI] [PubMed] [Google Scholar]
- 3.Yap Y, Tan Y, Tan H, et al. 3D printed bio-models for medical applications. Rapid Prototyp J. 2017;23(2):227–235. doi: 10.1108/RPJ-08-2015-0102. [DOI] [Google Scholar]
- 4.Garcia J, Yang Z, Mongrain R, Leask R, Lachapelle K. 3D printing materials and their use in medical education: a review of current technology and trends for the future. BMJ STEL. 2017;4(1):27–40. doi: 10.1136/bmjstel-2017-000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Sudani D, Basudan S. Students’ perceptions of pre-clinical endodontic training with artificial teeth compared to extracted human teeth. Eur J Dent Educ. 2016;21(4):e72–e75. doi: 10.1111/eje.12223. [DOI] [PubMed] [Google Scholar]
- 6.Decurcio D, Lim E, Nagendrababu V, Estrela C, Rossi-Fedele G. Difficulty levels of extracted human teeth used for pre-clinical training in endodontics in an Australian dental school. Aust Endod J. 2019;46(1):47–51. doi: 10.1111/aej.12355. [DOI] [PubMed] [Google Scholar]
- 7.Shah K, Ahmed J, Shenoy N, Srikant N. How different are students and their learning styles? Int J Res Med Sci. 2013;1(3):1. doi: 10.5455/2320-6012.ijrms20130808. [DOI] [Google Scholar]
- 8.Lee J, Choi K, Choi J. Developing customized phantom for korean bone density using 3D printing. J Radiol Sci Technol. 2019;42(3):223–229. doi: 10.17946/JRST.2019.42.3.223. [DOI] [Google Scholar]
- 9.Bohl M, Morgan C, Mooney M, et al. Biomechanical testing of a 3D-printed L5 vertebral body model. Cureus. 2019;11(1):e3893. doi: 10.7759/cureus.3893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barak M, Black M. A novel use of 3D printing model demonstrates the effects of deteriorated trabecular bone structure on bone stiffness and strength. J Mech Behav Biomed Mater. 2018;78:455–464. doi: 10.1016/j.jmbbm.2017.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]