Abstract
Purpose
The conventional alveoloplasty approach which uses manual equipment results in more resorption of the underlying alveolar ridge that makes denture prosthesis unstable. The goal of this study was to compare results of piezosurgery alveoloplasty to those of conventional alveoloplasty.
Materials and Methods
This was an in-vivo comparative study consisting of ten edentulous individuals who needed alveoloplasty due to bilateral bony projection. On one side, a conventional alveoloplasty was performed with a bone rongeur and bone file, whereas the contralateral side was treated with a piezosurgery unit. The clinical parameters were analyzed using SPSS version 21 software including operating time, postoperative pain evaluation on day 3 and a healing on day 7.
Results
There was a statistically significant difference between the two groups in terms of outcome variables such as operating time, pain and healing. The Conventional group has a lower mean of operating time, a higher mean rank of VAS and a lower mean rank of healing index compared to the piezosurgery group.
Conclusion
Piezosurgery alveoloplasty not only lowers postoperative patient discomfort but also preserves alveolar bone integrity by not disrupting soft and hard tissue architecture thus allowing faster tissue healing and easier prosthesis replacement in the future.
Keywords: Alveoloplasty, Conventional, Piezosurgery, Bony projection
Introduction
The edentulous mandibular ridge associated with shallow vestibule and limited peri-implant keratinized mucosal width (KMW), thickness and height are frequently seen as a barrier to oral rehabilitation in patients who have lost their teeth. The lack of keratinized oral mucosa and the shallow mandibular vestibule with high muscle attachments often make it difficult to fabricate a complete or partial denture. The edentulous mandibular ridges are frequently knife-edged or uneven, making denture manufacture impossible without concurrent hard and soft tissue preparation. The purpose of alveoloplasty is to gain optimal tissue support for the proposed prosthesis while preserving as much soft and hard tissue as possible [1].
The use of manual instruments in traditional alveoloplasty results in more resorption of the underlying alveolar ridge, which is unsuitable for denture fabrication. As a result, to minimize the limitations of conventional tools, Tomaso Vercellotti in 1988 invented the first commercially accessible Mectron® piezoelectric bone surgery device to cut bone tissue [2, 3].
Piezoelectric surgery devices are typically compact portable equipment that includes a handpiece with a working tip and a foot control switch that are both connected to the main power source. The primary power unit also has holders for the handpiece and irrigation fluid, which use a peristaltic pump to create an adjustable jet of 0–60 ml/minute. Because of its cavitation action, it aids in the removal of debris from the cut surface as well as the maintenance of hemostasis. By distributing coolant liquid as an aerosol, it improves visibility, especially in difficult-to-reach anatomical zones. For effective cooling, the irrigation liquid should be kept at 4 °C. The handpiece is the most important component of this device since it houses the ceramic chips that generate micro-vibrations that are then communicated to the working tip. Ceramic chips made of Barium Titanate or a similar substance are commonly utilized in Piezoelectric surgical devices. The power supply determines the amount of deformation developed in the crystals within the handpiece and the resulting vibrations in the insert. The frequency is commonly set between 25 and 29 kHz which can produce micro-oscillations with amplitudes of 60–210 µm, giving the handpiece a power of more than 5 W. The vibrations produced in “low mode” are caused by average ultrasonic powers with no frequency overmodulation, allowing the operator to execute endodontic treatments. The “high mode” and “boosted mode” on the other hand, are characterized by vibrations with higher ultrasonic power and frequency overmodulation that is required for cutting mineralized tissues. The “boosted mode” has frequency overmodulation with an increased pace that is most efficient in osteotomy procedures, whereas the “high mode” is comparatively less effective [4, 5]
This ground-breaking tool not only preserves soft and hard tissue integrity but also preserves osteocytes which aid bone healing. In comparison to traditional rotary devices, piezosurgery allows an oral and maxillofacial surgeon to use a safer and more effective tool. It has been developed for use in neurosurgery, orthopedic surgery and otorhinolaryngology throughout the last decade, in addition to being increasingly used in OMFS.
There are few studies mentioned in the literature that have compared conventional and piezosurgery alveoloplasty but none of the studies were standardized in terms of incision placement in both groups and other clinical parameters such as assessment of operative time, pain and healing. Taking that into consideration, the current study was based on standard incisions (crestal and releasing incision) in which both techniques were compared with respect to clinical parameters such as operating time, pain and healing.
Materials and Methods
Study Design and Sample Size
After receiving approval from the college’s Ethical Committee, this study was carried out in the Department of Oral and Maxillofacial Surgery. Ten edentulous patients with bilateral sharp bony projections on the alveolar ridge who presented to our department between September 30, 2020 and September 30,2021 were included in the study. Using a simple random sampling technique, patients were assigned into study and control groups. Patients with age an range of 30–70 years with bilateral sharp bony projections and healthy patients (ASA grade 1- A normal healthy patient and ASA grade 2-Patient with mild systemic diseases such as well-controlled Diabetes mellitus and hypertension)-were included in the study. The study excluded patients with unilateral bony protrusion, bleeding disorders and uncontrolled systemic comorbidities. Maximal bony projection diameter exceeding 3 mm was excluded from the study. A consent form was signed by all of the patients who took part in the trial.
No pre and post-operative radiographs were taken for the patients and no specific hematological investigations were preformed. Patients with history of diabetes mellitus were advised for fasting blood sugar levels checked before the procedure. Patients were selected based on intraoral clinical examination and markings of bony projection made on diagnostic cast.
Methodology
This is a split-mouth study consisting of study group (piezosurgery group) and control group (conventional group). The same surgeon has performed all of the surgical procedures and postoperative examinations.
Patients were encouraged to rinse their mouths with 0.2% chlorhexidine mouthwash before surgery.
The local anesthetic containing 2% lignocaine with epinephrine 1:80,000 was administered to the site.
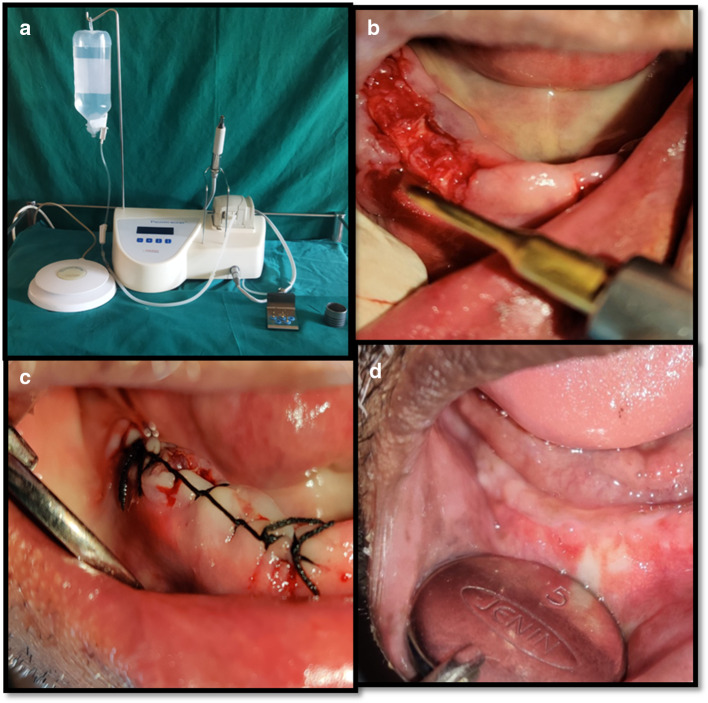
The full-thickness mucoperiosteal flap was reflected to expose the bony projection after giving crestal and releasing incisions (Fig. 1a). The triangular flap was preferred over envelope flap as it allows better visualization and access to the surgical field, avoids unanticipated tear to edges of the flap that can occur in envelope flap in areas of inadequate exposure and also triangular flap allows better mobilization of flap, ensuring tension-free closure. Also releasing incision allows inflammatory exudates, if any, to come out.
Bone rongeur (Fig. 1b) and a bone file were used to shape the bones. A non-resorbable suture material was used to approximate the flap (3–0 silk suture material) (Fig. 1c). After 7 days, patients were summoned back for piezosurgery alveoloplasty.
On the contralateral side of the arch, a crestal and releasing incisions were placed and the mucoperiosteal flap was reflected to expose the bony projection. A Piezo insert (osteotomy-OT 7) was used to accomplish bony contouring (unidirectional motion of the piezo blade) (Fig. 2b) The piezo unit (Fig. 2a) was switched on with frequency set at 26 kHz in “boosted” mode with micro-oscillations of 200 µm amplitude and the saline flow of 50 ml/min. The bony projection was shaved off carefully. The flap was approximated and secured using a non-resorbable suture (3–0 silk suture) (Fig. 2c).
The operating time was noted from the time of incision placement till the closure of incision in both the groups. Postoperative instructions were given to patients.
All the patients were advised to have a soft diet for 7 days and instructed to maintain good oral hygiene.
Postoperatively, all patients were prescribed antibiotic (capsule Amoxicillin 500 mg TID for 5 days or in case of amoxicillin allergy, erythromycin 500 mg TID for 5 days) analgesic (tab Diclofenac 50 mg TID for 3 days).
Postoperative pain was assessed by visual analog scale (VAS) in both groups (study as well as control groups) on the third postoperative day (POD). Sutures were removed on the seventh POD and the healing was assessed by Landry et al. healing index (Table 1) in both groups (figs. 1d and 2d).
Fig. 1.
a Crestal along with releasing incision b Excision of bony projections using bone rongeur c Closure done using black silk suture d Healing assessment at day 7(conventional technique)
Fig. 2.
a Piezosurgery unit b Alveoloplasty using piezo blade c Closure done using black silk suture d Healing assessment at day 7(piezosurgery technique)
Table 1.
Healing index (Landry, Turnbull and Howley)
| Group | N | Mean | Standard deviation | P-value |
|---|---|---|---|---|
| Conventional | 10 | 25.10 | 6.74 | 0.038* |
| Piezo | 10 | 32.40 | 7.74 | 0.038* |
The procured values were recorded, tabulated, and statistically evaluated.
Statistical analysis
Statistical analysis was conducted using SPSS software version. The present study consisted of a sample size of ten patients at 5% level of significance with 80% power and effect size of 0.5. Descriptive statistics have been expressed, such as mean, mean rank, and standard deviation. The independent T-test was used to assess clinical data such as operating time for study group (piezo group) and control group (conventional group) and the Mann–Whitney test was utilized for pain and healing, where P-value = 0.05 or less was regarded statistically significant.
Results
The participants consisted of 10 patients (7 men and 3 women; age range 30—70: mean age: 54.20 ± 13.34 years) diagnosed with bilateral bony projections on the edentulous alveolar ridge.
Operative time
The operative time (time of incision till the time of closure) was noted in minutes in both the groups. Using independent t test, it was found that operating time was significantly higher in study group with mean of 32.4 & standard deviation of 7.74 compared to control group with mean of 25.10 and standard deviation 6.74 with p value = 0.034 (statistically significant) as shown in Table 2
Table 2.
Operative time in the piezosurgery alveoloplasty group was significantly higher compared to the conventional group using independent –T test
| Healing index | Criteria |
|---|---|
| 1—Very Poor | (1) Tissue color: > = 50% of Gingiva red |
| (2) Response to palpation: Bleeding | |
| (3) Granulation tissue: Present | |
| (4) Incision margin: Not epithelialized, with loss of epithelium beyond incision margin | |
| (5) Suppuration: Present | |
| 2—Poor | (1) Tissue color: > = 50% of gingiva red |
| (2) Response to palpation: Bleeding | |
| (3) Granulation tissue: Present | |
| (4) Incision margin: Not epithelialized, with connective tissue exposed | |
|
3—Good : |
(1) Tissue color: > = 25% and < 50% of gingiva red |
| (2) Response to palpation: No bleeding | |
| (3) Granulation tissue: None | |
| (4) Incision margin: No connective tissue exposed | |
| 4—Very Good | (1) Tissue color: < 25% of gingiva red |
| (2) Response to palpation: No bleeding | |
| (3) Granulation tissue: None | |
| (4) Incision margin: No connective tissue exposed | |
| 5—Excellent | (1) Tissue color: All tissues pink |
| (2) Response to palpation: No bleeding | |
| (3) Granulation tissue: None |
Pain
Visual analogue scale rating from 1 to 10 was used to evaluate the pain at day 3 postoperatively in both groups. Using the Mann whitney test, it was assessed that there was a statistically significant difference between both the groups. The patients in the study group was reported significantly lower VAS score with mean rank of 6.50 compared to the control group with mean rank of 14.50 as shown in Fig. 3.
Fig. 3.
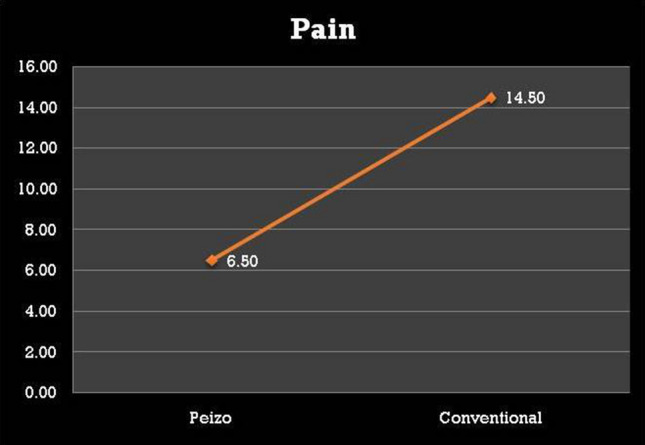
Comparison of pain between both groups based on P-values. (*Statistically significant p < 0.05) using Mann whitney test
Healing index
The healing in both groups was assessed by using the healing index by Landry [6] et al. on the 7 postoperatively. Using the Mann–Whitney test, it was assessed that there was a statistically significant difference between both the groups. The operative site in the study group showed significantly better and faster healing with mean rank of 8 compared to that in the control group with mean rank 13 with p value < 0.05 as shown in (Fig. 4).
Fig. 4.
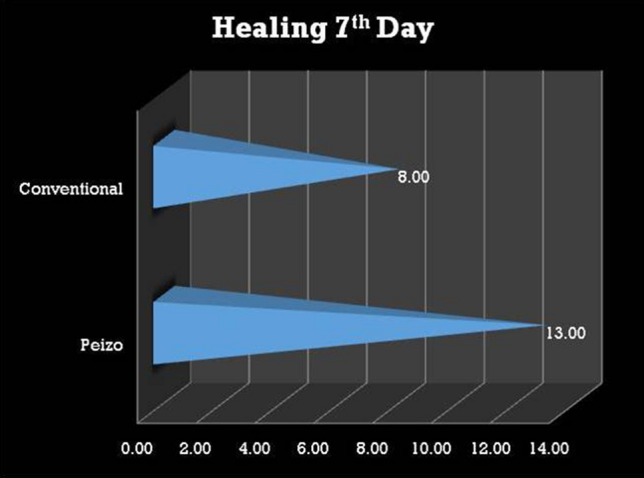
Comparison of healing between both groups based on P-values. (*Statistically significant p < 0.05) using Mann whitney test
Discussion
Pre-prosthetic surgery is the process of preparing the patient’s mouth for the insertion of a denture (or prosthesis). To achieve the highest level of comfort, some patients require minor oral surgical operations before receiving a partial or complete denture [7]. Alveolectomy or alveoloplasty is the most common pre-prosthetic surgical surgery [8].
By proposing interseptal alveoloplasty, Sir O. T Dean had changed the practice of alveoloplasty. To attain optimal alveolar ridge form, he proposed preserving the labial cortex rather than sacrificing the interradicular medullary bone [9]. Dean’s interseptal alveoloplasty was especially well-suited for immediate denture surgery. Obwegeser proposed a variant of Dean’s procedure in 1966 for cases of extensive premaxillary protrusion, in which both the palatal and labial cortices were broken and reposition [10].
One of the novel methods in ultrasonic’s is Piezosurgery. This is a relatively new alternative for bone-related procedures introduced in the field of dentistry [11].
In study done by Goyal et al. comparing the efficacy of piezosurgery and conventional rotary instruments for impacted mandibular third molar removal, the authors found that the piezosurgery group had less postoperative pain, facial swelling, and trismus while the operative time was longer than the control group [12]. Our study was also in accordance with Goyal’s study in regard to operative time.
Labanca et al. reviewed the progress in piezosurgery during the last 20 years, focusing on its applications in several surgical fields [13]. Bovi was the first to use a piezoelectric device to do inferior alveolar nerve (IAN) mobilization and implant insertion simultaneously in 2005 [14]. He claims that using a piezoelectric device to mobilize the IAN reduces the danger of irreversible injury to the nerve and allows the surgeon to create a smaller bone window which reduces overstretching of the mental nerve.
Landes et al. conducted a study on 90 patients who had used piezoelectric unit for orthognathic surgery. This study found that as compared to traditional surgery, there was less blood loss but no significant change in surgical times [15].
Kagan Degerliyurt published a paper in 2009 outlining a method known as the “bone lid technique,” which is conducted with a piezosurgery instrument when IAN is at risk of injury [16]. Because of the lack of macro-vibrations, ease of use and safe cutting, the authors concluded that piezoelectric surgery is a unique technique for safe and successful osteotomy in all of these clinical circumstances. It appears to be more effective in the early stages of bone healing, generating an earlier increase in BMPs, better regulating the inflammatory process, and encouraging bony remodeling [17].
Conclusion
Piezosurgery has proven to be a better alternative to the numerous equipments and techniques used for alveoloplasty by lowering patient discomfort and speeding up the healing process. As a result, this study supports the use of piezosurgery in all patients undergoing alveoloplasty. This research has a few limitations. The sample size is quite small. However, the results were consistent across all patients. Inadequate efficacy or cutting speed which can be compensated by better clinical results. Ultrasonic devices in future generations may improve efficiency and eventually replace all traditional cutting tools. To establish conclusion with greater statistical significance, further studies with a larger sample size are required.
Funding
None
Declarations
Conflict of interest
None
Ethical Standard
Obtained from the Yenepoya Ethics Committee-2, Yenepoya (Deemed to be University). Informed consent obtained for publication of patient data and photographs.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Adams DR, Petukhova Y, Halpern LR. The versatile “lip switch” or transitional flap vestibuloplasty combined with alveoloplasty and implant placement to treat atrophic mandibles with inadequate vestibules and attached tissue: a case series and review of the literature. Spec Care Dentist. 2021;41(1):78–84. doi: 10.1111/scd.12546. [DOI] [PubMed] [Google Scholar]
- 2.Vercellotti T, De Paoli S, Nevins M. The piezoelectric bony window osteotomy and sinus membrane elevation: introduction of a new technique for simplification of the sinus augmentation procedure. Int J Periodontics Restor Dent. 2001;21(6):561–568. [PubMed] [Google Scholar]
- 3.Vercellotti T. Technological characteristics and clinical indications of piezoelectric bone surgery. Minerva Stomatol. 2004;53(5):207–214. [PubMed] [Google Scholar]
- 4.Renapurkar S, Nagamalla S. Piezosurgery in oral and maxillofacial surgery. In: Bonanthaya K, Panneerselvam E, Manuel S, Kumar VV, Rai A, editors. Oral and Maxillofacial Surgery for the Clinician. Singapore: Springer; 2021. pp. 831–839. [Google Scholar]
- 5.Leclercq P, Zenati C, Amr S, Dohan D. Ultrasonic bone cut. Part 1: State-of-the-art technologies and common applications. J Oral Maxillofac Surg. 2008;66(1):177–182. doi: 10.1016/j.joms.2005.12.054. [DOI] [PubMed] [Google Scholar]
- 6.Landry RG, Turnbull RS, Howley T. Effectiveness of benzydamyne HCl in the treatment of periodontal post-surgical patients. Res Clin Forum. 1988;10:105. [Google Scholar]
- 7.Bhuskute MV, Shet RG. Preprosthetic surgery: an adjunct to complete denture therapy. J Int Clin Dent Res Organ. 2019;11(1):49. doi: 10.4103/jicdro.jicdro_6_19. [DOI] [Google Scholar]
- 8.Meyer I. Alveoloplasty—the oral surgeon's point of view. Oral Surg Oral Med Oral Pathol. 1966;22(4):441–455. doi: 10.1016/0030-4220(66)90422-1. [DOI] [PubMed] [Google Scholar]
- 9.Dean OT. Surgery for the denture patient. J Am Dent Assoc. 1936;23(11):2124–2128. [Google Scholar]
- 10.Obwegeser H. Surgical preparation of the maxilla for prosthesis. J Oral Surg Anesth Hosp Dent Serv. 1964;22:127–134. [PubMed] [Google Scholar]
- 11.Agarwal E, Masamatti SS, Kumar A. Escalating role of piezosurgery in dental therapeutics. J clin diagn Res. 2014;8(10):ZE08. doi: 10.7860/JCDR/2014/9161.4988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goyal M, Marya K, Jhamb A, Chawla S, Sonoo PR, Singh V, Aggarwal A. Comparative evaluation of surgical outcome after removal of impacted mandibular third molars using a Piezotome or a conventional handpiece: a prospective study. Br J Oral Maxillofac Surg. 2012;50(6):556–561. doi: 10.1016/j.bjoms.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 13.Labanca M, Azzola F, Vinci R, Rodella LF. Piezoelectric surgery: twenty years of use. Br J Oral Maxillofac Surg. 2008;46(4):265–269. doi: 10.1016/j.bjoms.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Bovi M. Mobilization of the inferior alveolar nerve with simultaneous implant insertion: a new technique case report. Int J Periodontics Restor Dent. 2005;25(4):375. [PubMed] [Google Scholar]
- 15.Landes CA, Stübinger S, Rieger J, Williger B, Ha TK, Sader R. Critical evaluation of piezoelectric osteotomy in orthognathic surgery: operative technique, blood loss, time requirement, nerve and vessel integrity. J Oral Maxillofac Surg. 2008;66(4):657–674. doi: 10.1016/j.joms.2007.06.633. [DOI] [PubMed] [Google Scholar]
- 16.Degerliyurt K, Akar V, Denizci S, Yucel E. Bone lid technique with piezosurgery to preserve inferior alveolar nerve. Oral Surg Oral Med Oral Pathol Oral Radiol and Endodontol. 2009;108(6):e1–5. doi: 10.1016/j.tripleo.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Preti G, Martinasso G, Peirone B, Navone R, Manzella C, Muzio G, Russo C, Canuto RA, Schierano G. Cytokines and growth factors involved in the osseointegration of oral titanium implants positioned using piezoelectric bone surgery versus a drill technique: a pilot study in minipigs. J Periodontol. 2007;78(4):716–722. doi: 10.1902/jop.2007.060285. [DOI] [PubMed] [Google Scholar]