Abstract
Individuals who introduce illicit substances such as opioids and amphetamines into the gastrointestinal tract by swallowing or inserting them into the rectum are known as body packers. We describe a prisoner who developed severe poisoning symptoms after swallowing amphetamine packets and was promptly removed by laparotomy.
Keywords: amphetamine, body packer, laparotomy, poisoning, prisoner
Short abstract
In body packers and body stuffers, if these packages are opened in the gastrointestinal tract, it can be associated with severe poisoning and high mortality, which requires surgical intervention.
1. INTRODUCTION
Methamphetamine (MAP), often known as “ice,” “crack,” “glass,” and “speed,” is a simple chemical that can be made with only basic laboratory equipment and starting materials. MAP is less expensive, more readily available, and lasts longer than cocaine. These characteristics have facilitated the spread of its popularity throughout time. 1
Methamphetamine is readily absorbed in several ways, such as oral, injection, and inhalation, all of which can lead to severe poisoning. In other words, individuals who try to sneak illicit substances into their bodies by swallowing them or inserting them into the rectum or vagina are known as “body packers” or “mules.” Illicit substances are commonly packaged in condoms, balloons, or plastic film in such scenarios, while body stuffers are those who swallow or insert illicit substances into the body to avoid imminent apprehension by authorities, which can lead to acute life‐threatening toxicity and death Therefore, these two groups of people should be distinguished from each other. 2 , 3
With the expanding drug industry and sales, body packing is becoming more of an issue. Body packers conceal illegal substances in their bodies for a variety of reasons. They conceal small amounts of the drug in order to cross borders between countries and in order to hide them when apprehended by police; the latter are known as “mini packers” because they pack small amounts of the drug. 4
Other reported substances include amphetamine (AP) and, on rare occasions, cannabis, as well as a combination of drugs in several cases. The substance's type is determined by the area's drug market and crosses countries. 5 The number of packages in different cases varies and can reach 50–60 packages. 6 Different packaging substances are utilized depending on whether the packaging was done manually or by sophisticated equipment. 7
There have been reports of latex, condoms, foil, wax paper, and bottle vials being packed with illegal substances. 3 Special techniques are used by machine packing to produce packs that are both safe and difficult to identify. 8 Body packers use various cavities in the body to hide illegal packets and organs such as the stomach, rectum, vagina, and ear, all of which have been documented. 8 , 9 A rare example of concealing a drug package behind the foreskin of the penis was also described. 10
Simple tests for suspected conditions include urine and blood analysis. However, they could potentially be signs of drug usage rather than a leaking package. The second phase of suspicion includes radiological studies, which can include abdominal X‐rays and ultrasounds. These studies look for specific indicators, including parallelism, rosette patterns, and tic‐tac patterns. 6 Packers create false negatives by moving, drinking fluids to mask density, or taking constipating medications to collect stool around the packages. 8 , 11 The most useful diagnostic method is a computed tomography scan (CT scan), but it has the disadvantage of exposing the patient to high radiation. In a CT scan, different drugs have varied densities, with cocaine being less dense than fat, cannabis having the same bone density as bone, and heroin having a density somewhere between fat and air. 11 We describe a male prisoner who swallowed two packets of AP (body packer) that lead to severe MAP toxicity when one of them is opened and the other pack is removed by laparotomy.
2. CASE PRESENTATION
On December 2, 2021, a 47‐year‐old man suffered from abdominal pain, restlessness, agitation, and hyperexcitability for 6 h after being transferred to a prison in northern Iran. The prisoner was immediately referred to the hospital due to the severity of his pain and restlessness, as well as his lack of cooperation. An ampoule of diazepam and haloperidol was administered to the patient after they had been brought to the emergency room with agitation and seizure‐like movements in order to manage them. The blood pressure (BP) was 150/95 mm Hg, the heart rate (HR) was 110/min, the respiratory rate (RR) was 26/min, the temperature was 37.8°C, and oxygen saturation (SO2) was 96% during the examination. His pupils were dilated, and he guarded his abdomen. The laboratory findings are shown in the Table 1.
TABLE 1.
Results of initial tests and comparison with measured values 5 days after treatment.
| Parameter | Initial blood sample | Blood sample 5 days after treatment | Normal range |
|---|---|---|---|
| CPK | 6754 | 693 | 39–308 U/L |
| Cr | 1 | 0.8 | 0.74–1.35 mg/dl |
| BUN | 13 | 11 | 6–24 mg/dl |
| K | 3.8 | 4.1 | 3.5–5.0 mEq/L |
| Na | 138 | 140 | 135–145 mEq/L |
| Ca | 8.5 | 9 | 8.5–10.5 mg/dl |
| pH | 7.60 | 7.44 | 7.35–7.45 |
| PCO2 | 22.9 | 38.8 | 35–45 mm Hg |
| HCO3 | 22.5 | 26.1 | 22–28 mEq/L |
| WBC | 12.3 × 103 | 7.1 × 103 | 4000–1000/mm3 |
| AST | 33 | 21 | 50–40 IU/L |
| ALT | 102 | 38 | <45 U/L |
| BS | 155 | 102 | <200 mg/dl |
| Mg | 1.9 | 2.1 | 1.8–2.6 mg/dl |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; BS, blood sugar; BUN, blood urea nitrogen; Ca, calcium; CPK, creatine phosphokinase; Cr, creatinine; HCO3, bicarbonate; K, potassium; Mg, magnesium; Na, sodium; PCO2, partial pressure of carbon dioxide; PH, potential of hydrogen; WBC, white blood cells.
In addition, at the time, gas chromatography and mass spectrometry of the urine revealed the presence of MAP and AP metabolites; co‐intoxicants were ruled out based on a full urine drug test utilizing gas chromatography–mass spectrometry (GC–MS). MAP and AP serum levels were quantified to be 1200 and 80 ng/ml, respectively. For him, an abdominal and pelvic CT scan without contrast was requested, which revealed foreign bodies in his stomach (Figure 1A,B), but the CT scan of the brain was normal. An electrocardiogram showed sinus tachycardia with a ventricular rate of 110 beats per minute.
FIGURE 1.
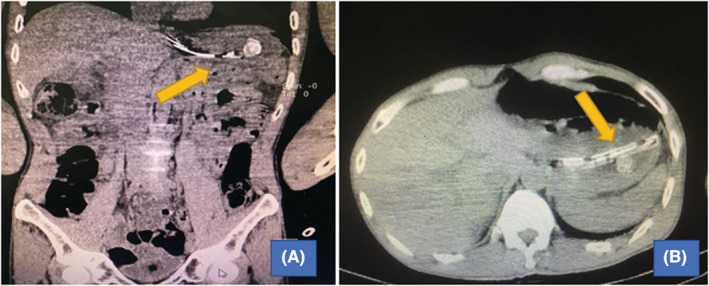
(A, B) Pelvic and abdominal CT scan shown revealed foreign bodies in his stomach, ruptured plastic, and a complete package.
Finally, with the diagnosis of ruptured AP packages, surgical consultation is requested. The patient was transferred to the operating room immediately and underwent a laparotomy, as well as having an opened plastic bag and a complete package removed (see Videos S1 and S2). After surgery, the patient was transferred to the intensive care unit (ICU), but he was still agitated, so he was given an intravenous infusion of midazolam at a dose of 1 mg/h. In addition, pantoprazole 40 mg twice a day (BID), ceftriaxone (1 g BID), and metronidazole 500 mg three times a day (TDS) ampoules were prescribed.
The patient's agitation improved, and his level of consciousness increased after 48 h of sedation, and he stated that he had ingested two packets of AP. For the next 5 days, the patient was transferred to the surgical ward, and after a week, he was discharged from the hospital in good general condition and tolerating nutrition. Written informed consent was obtained from the patient for publication of this case report. This study was conducted according to the Declaration of Helsinki Principles. Also, CARE guidelines and methodology were followed in this study.
3. DISCUSSION
Methamphetamine (MAP) has an effect on the brain by increasing dopamine release from vesicular storage and increasing extracellular dopamine levels via reverse transport. MAP also affects serotonergic, glutamatergic, and nor‐adrenergic neurotransmission via interactions with 5‐HT transporters, N‐Methyl‐D‐aspartate transporters, and monoamine transporters. 2 The cardiovascular and neurological systems are most affected by MAP poisoning.
Our patient had gastrointestinal discomfort and restlessness after swallowing two packs of AP compounds in plastic bags, 6 h after entering prison. Agitation and tachycardia were present at the time of admission, indicating that the package had been opened. A CT scan revealed the presence of an unopened package and a broad foreign object. Our patient had seizure‐like movements, high blood pressure, altered mental status, and tachycardia, all of which were symptoms of MAP poisoning. Overdose with MAP can also cause dysrhythmias, myocardial ischemia, hyperthermia, agitation, and intracerebral hemorrhage.
Kashani et al. reported a young woman who had an AP package intravaginal body stuffing without providing a history, which caused severe MAP poisoning after opening. This showed that MAP was absorbed via the mucosa as a result of body stuffing. As a result, in these individuals, a thorough examination of uncommon body locations, including the vagina, appears to be necessary. 9
A study in New York City discovered 50 cases with five deaths, while another in the United Kingdom reported 180 cases with no fatalities. 7 When rapidly swallowing the packages in mini packers, death occurs due to drug leakage, intestinal obstruction, 12 peritonitis, 13 perforation, or even obstruction of the airways. Death can occur for reasons unrelated to the body packing, such as drug overdose or other causes of death, with packages discovered in the body by accident during an autopsy.
According to Abedzadeh et al., 11 who reported a tragic case, the victim in this case utilized the most common method of hiding the drugs: swallowing, which resulted in death after the pills opened in the gastrointestinal tract. On the contrary, Klein et al. 14 described how body packers are frequently found by police not only at airports but also in places such as prisons and mental health facilities. In the past, surgery was the first‐line management of body packers. Surgical intervention will be used mainly in cases with symptoms of leakage or intestinal obstruction, and it will be more conservatively managed with purgation or close monitoring until discharged naturally. 15 , 16
In our study, the prisoner was transported to the hospital after experiencing abdominal pain and restlessness in the prison, which suggested that the AP package had been opened; fortunately, he was saved from death by timely surgery. AP and MAP were found in toxicological tests of the blood. Furthermore, his addiction and dependence on AP chemicals may have been the cause of his tolerable clinical symptoms in this case. Takekawa et al. 17 showed that the level of MAP in the central blood from the heart and peripheral blood was greater in the central blood in 20 postmortem cases, and it was recommended to avoid interpreting the cause of death based on the central blood sample.
4. CONCLUSION
In prisons and mental health facilities, body packing syndrome should be suspected, and steps should be taken to save the body packer's life while also preventing drug smuggling. Officials may obtain information from such cases, such as insights into the drug industry, developments in packaging methods, and drug‐hiding strategies in the area. Therefore, it is recommended that in all prisoners who are referred to the emergency department with symptoms of poisoning and have abdominal symptoms on examination, in such cases, clinicians should consider performing an abdomen and pelvis CT scan for a definitive diagnosis.
AUTHOR CONTRIBUTIONS
ZZ and RR involved in interpretation and collecting of data. AM and ESB involved in writing and editing the manuscript. ZZ and MS involved in editing and preparing the final version of manuscript. All authors reviewed the paper and approved the final version of the manuscript.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ETHICAL APPROVAL
The study was approved by our local ethics committee.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor‐in‐Chief of this journal.
Supporting information
Video S1
Video S2
ACKNOWLEDGMENTS
None declared.
Rouhani R, Zakariaei Z, Malakian A, Banimostafavi ES, Soleymani M. Methamphetamine poisoning due to body packer swallowing in a prisoner. Clin Case Rep. 2022;10:e06358. doi: 10.1002/ccr3.6358
DATA AVAILABILITY STATEMENT
The data are available with the correspondence author and can be achieved on request.
REFERENCES
- 1. Sribanditmongkol P, Chokjamsai M, Thampitak S. Methamphetmaine overdose and fatality: 2 cases report. J Med Assoc Thai. 2000;83(9):1120‐1123. [PubMed] [Google Scholar]
- 2. Fineschi V, Centini F, Monciotti F, Turillazzi E. The cocaine “body stuffer” syndrome: a fatal case. Forensic Sci Int. 2002;126(1):7‐10. [DOI] [PubMed] [Google Scholar]
- 3. Koehler SA, Ladham S, Rozin L, et al. The risk of body packing: a case of a fatal cocaine overdose. Forensic Sci Int. 2005;151:81‐84. doi: 10.1016/j.forsciint.2004.07.005 [DOI] [PubMed] [Google Scholar]
- 4. Introna F Jr, Smialek JE. The “mini‐packer” syndrome. Fatal ingestion of drug containers in Baltimore, Maryland. Am J Forensic Med Pathol. 1989;10(1):21‐24. [PubMed] [Google Scholar]
- 5. Gill JR, Graham SM. Ten years of “body packers” in new York City: 50 deaths. J Forensic Sci. 2002;47(4):1‐4. [PubMed] [Google Scholar]
- 6. Pinto A, Reginelli A, Pinto F, et al. Radiological and practical aspects of body packing. The British journal ofradiology. 2014;87(1036):20130500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bulstrode N, Banks F, Shrotria S. The outcome of drug smuggling by ‘body packers’–the British experience. Ann R Coll Surg Engl. 2002;84(1):35‐38. [PMC free article] [PubMed] [Google Scholar]
- 8. Cappelletti S, Piacentino D, Ciallella C. Systematic review of drug packaging methods in body packing and pushing: a need for a new classification. Am J Forensic Med Pathol. 2019;40(1):27‐42. [DOI] [PubMed] [Google Scholar]
- 9. Kashani J, Ruha AM. Methamphetamine toxicity secondary to intravaginal body stuffing. J Toxicol Clin Toxicol. 2004;42(7):987‐989. [DOI] [PubMed] [Google Scholar]
- 10. Wilcher G. Drug‐related deaths with evidence of intracorporeal drug concealment at autopsy: five case reports. Am J Forensic Med Pathol. 2011;32(4):314‐318. [DOI] [PubMed] [Google Scholar]
- 11. Abedzadeh AA, Iqbal SS, Al Bastaki U, Pierre‐Jerome C. New packaging methods of body packers: role of advanced imaging in their detection. A case study. Radiol Case Rep. 2019;14(5):627‐633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hutchins KD, Pierre‐Louis PJ, Zaretski L, Williams AW, Lin RL, Natarajan GA. Heroin body packing: three fatal cases of intestinal perforation. J Forensic Sci. 2000;45(1):42‐47. [PubMed] [Google Scholar]
- 13. Wetli CV, Rao A, Rao VJ. Fatal heroin body packing. Am J Forensic Med Pathol. 1997;18(3):312‐318. [DOI] [PubMed] [Google Scholar]
- 14. Klein C, Balash Y, Pollak L, Hiss J, Rabey MJ. Body packer: cocaine intoxication, causing death, masked by concomitant administration of major tranquilizers. Eur J Neurol. 2000;7(5):555‐558. [DOI] [PubMed] [Google Scholar]
- 15. Beckley I, Ansari NA, Khwaja HA, Mohsen Y. Clinical management of cocaine body packers: the Hillingdon experience. Can J Surg. 2009;52(5):417. [PMC free article] [PubMed] [Google Scholar]
- 16. Benko MJ, Abdulla SG, Cuoco JA, et al. Short‐and long‐term geriatric mortality after acute traumatic subdural hemorrhage. World Neurosurg. 2019;130:e350‐e355. [DOI] [PubMed] [Google Scholar]
- 17. Takekawa K, Ohmori T, Kido A, Oya M. Methamphetamine body packer: acute poisoning death due to massive leaking of methamphetamine. J Forensic Sci. 2007;52(5):1219‐1222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1
Video S2
Data Availability Statement
The data are available with the correspondence author and can be achieved on request.


