Abstract
We report a 24‐year‐old female patient not infected with human immunodeficiency virus (HIV) and without other risk factors of immunosuppression, presenting with neuromeningeal cryptococcosis. Cerebrospinal fluid (CSF) analysis revealed the presence of Cryptococcus neoformans. The evolution was unfavorable and the patient died even after appropriate antifungal treatment.
Keywords: case report; Cryptococcus neoformans; immunocompetent, HIV
Testing for Cryptococcus should not be limited to immunocompromised patients. The neurologic manifestations of cryptococcosis are often less typical of meningitis. The Indian ink‐staining technique should be used routinely for all CSF examinations, regardless of the patient.
1. INTRODUCTION
Cryptococcosis is an opportunistic mycotic disease usually occurring during profound immune deficiencies, especially in subjects infected with the human immunodeficiency virus (HIV). 1 Other known risk factors are organ transplantation, kidney, and liver disease, long‐term use of corticosteroids and autoimmune diseases. 2
The most common clinical form is meningoencephalitis, which is fatal if untreated. It rarely affects immunocompetent patients. There are few reports of cryptococcal meningitis in subjects without HIV/AIDS. 2 We report a new case of neuromeningeal cryptococcosis in an HIV‐uninfected patient with no other known risk factors.
2. OBSERVATION
A 24‐year‐old woman of Malagasy nationality was admitted to the Internal Medicine Department in June 2021 for functional impotence of the right hemisphere. The disease had started 6 days before her admission with a sudden appearance of an abnormal movement of the right upper limb in the form of chorea, followed by functional impotence of the right hemisphere, a headache and aphasia. The context was apyretic and the general state was altered.
In her history, she had a cesarean delivery 5 months ago. She had no history of immunosuppression such as organ transplantation, renal or liver disease, long‐term corticosteroid use, or autoimmune disease. She was neither diabetic and not hypertensive.
Physical examination revealed right hemiparesis and aphasia. She was conscious and had no signs of intracranial hypertension or meningeal syndrome. She had white, soft, painless edema of the lower limbs, hepatojugular reflux, and liver pain on palpation.
The blood count was normal with a lymphocyte count of 1709/mm3, and the C‐reactive protein was negative. Blood ionogram, creatinine, and liver function tests were unremarkable. HIV and hepatitis serologies were negative. The Polymerase chain reaction test for SARS‐CoV‐2 was negative.
Serum protein electrophoresis revealed an albumin level of 29.48 g/L with no abnormalities in other fractions (alpha‐1 2.97 g/L, alpha‐2 6.88 g/L, beta‐1 4.35 g/L, beta‐2 2.20 g/L and gamma 9.13 g/L). The CD4 T‐cell count was 508/mm3.
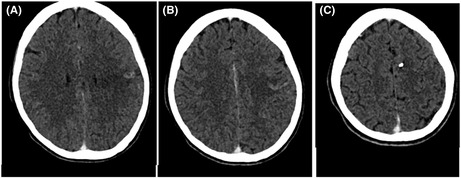
The brain scan showed left parietal hypodensity with meningeal enhancement and corticofrontal calcification (Figure 1).
FIGURE 1.
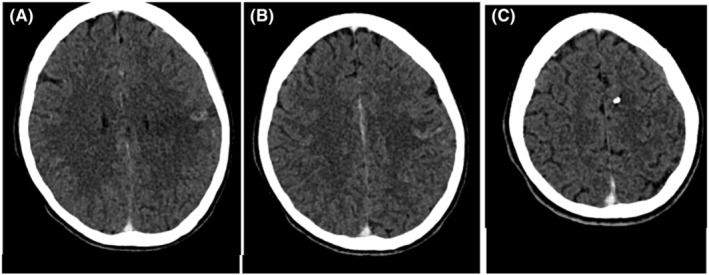
Brain CT scan without and with injection. Left parietal hypodensity, meningeal enhancement, and parasagittal corticofrontal calcification raising suspicion of meningoencephalitis
Cerebrospinal fluid (CSF) examination revealed clear fluid with high pressure, normal cellularity, normal glucose and protein levels, and sterility on routine direct examination. Cryptococcus neoformans was present on the Indian ink.
Transthoracic Doppler echocardiography showed dilatation of the left chambers with high filling pressure and global hypokinesia, suggestive of heart failure with impaired ejection fraction (38%).
The diagnosis of neuromeningeal cryptococcosis without immunosuppression was retained, associated with postpartum heart failure.
Following a multidisciplinary staff, treatment with amphotericin B injection at 1 mg/kg was started for 2 weeks followed by oral fluconazole at 400 mg daily for 6 weeks. CSF subtraction was performed regularly. The rest of the management consisted of treatment of the heart failure and monitoring.
After 3 evacuation sessions, the CSF pressure had normalized. The neurological evolution was favorable with regression of the hemiparesis and aphasia on day 7. Signs of cardiac decompensation had disappeared and hemodynamic parameters were stable.
Three months after hospitalization, the patient died at home with a condition probably related to pulmonary tuberculosis.
3. DISCUSSION
We describe cryptococcosis in an HIV‐uninfected woman. However, cryptococcosis is a condition that classifies patients as having an acquired immune deficiency status of HIV infection and is often found in patients with low CD4 counts. Neuromeningeal cryptococcosis is the most common presentation of this disease. The prevalence of cryptococcosis varies from country to country. In the United States, the annual incidence is 0.8 cases per 100,000 population. 3 In France, the prevalence is 0.2 cases per 100,000 population. 4 In African regions most affected by HIV, it is the leading cause of infectious meningitis. 5
The causative agent is an encapsulated yeast that is usually transmitted by inhalation of fungal spores. Cryptococcus neoformans is found in soil, wood, and bird droppings. Cryptococcus gattii is found mainly in tropical regions. 6 The cellular morphology and biochemical structure of the capsule are the virulence factors that facilitate its passage through the blood–brain barrier. 2
Cryptococcosis is the second most common opportunistic infection in AIDS after toxoplasmosis. According to the World Health Organization classification, it is classified as stage 4 HIV infection, affecting patients with a CD4 count below 100/mm3. 7
Cases have been reported in HIV‐uninfected patients with other types of immunosuppression, such as hematologic malignancy, cancer, diabetes, cirrhosis, systemic disease, and immunosuppressive therapy. 8 , 9 , 10 , 11 Involvement in these patients remains rare with a male predominance. 12 , 13 , 14 Our patient did not present any risk factors.
As observed in this patient, the classical signs of meningitis are often absent. The clinical manifestations are less typical of meningitis, making diagnosis difficult. 11 Headache and fever are frequently reported. Convulsion, disturbance of consciousness and neurological deficit are rarely described. The clinical polymorphism of neuromeningeal cryptococcosis may delay diagnostic and therapeutic management.
Diagnosis is based on 3 methods: direct examination with India ink to identify Cryptococcus spores, cryptococcal antigen testing, and culture on Sabouraud's medium. Biochemical analysis of CSF may show neither hypercytosis nor hyperproteinorachia.
The Indian ink staining technique should be used routinely for all CSF examinations, regardless of the patient, whether immunocompromised or not.
In patients with and without HIV infection, cryptococcosis always warrants treatment, cryptococcosis always warrants treatment. For immunocompetent hosts with the neuromeningeal form, the standard treatment is a combination of Amphotericin B and Flucytosine for 6–10 weeks. An alternative to this regimen is 2 weeks followed by Fluconazole for a minimum of 10 weeks. Consolidation therapy with Fluconazole can be continued for up to 6–12 months, depending on the clinical condition of the patient. 6 Regular CSF subtraction is recommended if the pressure is excessive. Our patient received Amphotericin for 2 weeks and Fluconazole for 6 weeks.
The occurrence of neuromeningeal cryptococcosis in an HIV‐uninfected patient is unusual. It is a serious infection, progressing to death if left untreated. The mortality rate in HIV‐uninfected subjects remains around 15% despite a well‐managed treatment. The prognosis remains guarded even in immunocompetent subjects. The rapid evolution of the symptomatology, the presence of intracranial hypertension and consciousness disorder, the low cellularity in the CSF and hypoglycorrhachia are the factors of poor prognosis.
4. CONCLUSION
Our case highlights that neuromeningeal cryptococcosis can occur even in HIV‐uninfected subjects. Similar cases have been reported, and patients often have other associated comorbidities. The prognosis remains guarded even in the absence of immunosuppression.
AUTHOR CONTRIBUTIONS
AM Andrianiaina, RMF Randrianarisoa followed up the patient, collected the clinical data, and drafted the report. LN Rakotonirina and SJN Ratsimbazafy designed and critically revised the report. HMD Vololontiana validated the report. All authors have read and accepted the final version of the article.
FUNDING INFORMATION
The authors state that they do not have a source of funding from a specific agency.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
CONSENT
The patient gave written informed consent for publication of the article. Only information necessary for scientific understanding was shared. Anonymity was respected.
ACKNOWLEDGMENTS
The authors thank the staff of the Internal Medicine Department of the Soavinandriana Hospital and the Joseph Raseta Befelatanana Hospital.
Andrianiaina AM, Randrianarisoa RMF, Ratsimbazafy SJN, Rakotonirina LN, Vololontiana HMD. Neuromeningeal cryptococcosis in a patient not infected with human immunodeficiency virus and without known risk factors: A case report. Clin Case Rep. 2022;10:e06353. doi: 10.1002/ccr3.6353
DATA AVAILABILITY STATEMENT
All data generated are included in the article.
REFERENCES
- 1. Bandadi F‐Z, Raiss C, Moustachi A, Lyagoubi M, Aoufi S. Forty cases of neuromeningeal cryptococcosis diagnosed at the mycology parasitology department of the Ibn Sina hospital in Rabat, over a 21‐year period. Pan Afr Med J. 2019;33:249. doi: 10.11604/pamj.2019.33.249.18011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Essouma M, Tangie LN, Temgoua MN, Kenfack UG, Ndam AN, Danwang C. Severe clinical immunodeficiency in a patient with human immunodeficiency virus infection and relatively high CD4 counts: a case report. J Med Case Reports. 2019;13(1):86. doi: 10.1186/s13256-019-1982-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gbané‐Koné M, Ouali B, Mègne E, et al. Neuromeningeal cryptococcosis and bone tuberculosis in an immunocompetent: a case report. Pan Afr Med J. 2015;20:109. doi: 10.11604/pamj.2015.20.109.6055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hajjeh RA, Conn LA, Stephens DS, et al. Cryptococcosis: population‐based multistate active surveillance and risk factors in human immunodeficiency virus infected persons. J Infect Dis. 1999;179(2):449‐454. doi: 10.1086/314606 [DOI] [PubMed] [Google Scholar]
- 5. Gangneux J‐P, Bougnoux M‐E, Hennequin C, et al. An estimation of burden of serious fungal infections in France. J Mycol Méd. 2016;26(4):385‐390. doi: 10.1016/j.mycmed.2016.11.001 [DOI] [PubMed] [Google Scholar]
- 6. Kambugu A, Meya DB, Rhein J, et al. Outcomes of cryptococcal meningitis in Uganda before and after the availability of highly active antiretroviral therapy. Clin Infect Dis. 2008;46(11):1694‐1701. doi: 10.1086/587667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Saag MS, Graybill RJ, Larsen RA, et al. Practice guidelines for the management of cryptococcal disease. Infectious Diseases Society of America. Clin Infect Dis. 2000;30(4):710‐718. doi: 10.1086/313757 [DOI] [PubMed] [Google Scholar]
- 8. World Health Organization . WHO Case Definitions of HIV for Surveillance and Revised Clinical Staging and Immunological Classification of HIV‐Related Disease in Adults and Children. World Health Organization; 2007. https://apps.who.int/iris/handle/10665/43699 [Google Scholar]
- 9. Revest M, Decaux O, Frouget T, et al. Cryptococcal infections in non‐HIV infected patients. Study of four cases and review of literature. Rev Med Interne. 2006;27(3):203‐208. doi: 10.1016/j.revmed.2005.11.011 [DOI] [PubMed] [Google Scholar]
- 10. Kiertiburanakul S, Wirojtananugoon S, Pracharktam R, Sungkanuparph S. Cryptococcosis in human immunodeficiency virus‐negative patients. Int J Infect Dis. 2006;10(1):72‐78. doi: 10.1016/j.ijid.2004.12.004 [DOI] [PubMed] [Google Scholar]
- 11. Mitchell TG, Perfect JR. Cryptococcosis in the era of AIDS‐100 years after the discovery of Cryptococcus neoformans. Clin Microbiol Rev. 1995;8(4):515‐548. doi: 10.1128/CMR.8.4.515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shih CC, Chen YC, Chang SC, Luh KT, Hsieh WC. Cryptococcal meningitis in nonHIV‐infected patients. Q J Med. 2000;93(4):245‐251. doi: 10.1093/qjmed/93.4.245 [DOI] [PubMed] [Google Scholar]
- 13. Chuck SL, Sande MA. Infections with cryptococcus neoformans in the acquired immunodeficiency syndrome. N Engl J Med. 1989;321(12):794‐799. doi: 10.1056/NEJM198909213211205 [DOI] [PubMed] [Google Scholar]
- 14. Pappas PG, Perfect JR, Cloud GA, et al. Cryptococcosis in human immunodeficiency virus‐negative patients in the era of effective azole therapy. Clin Infect Dis. 2001;33(5):690‐699. doi: 10.1086/322597 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated are included in the article.


