Abstract
Background
In the wake of the coronavirus disease 2019 (COVID-19) pandemic, demand for deep cleaning and environmental services workers grew exponentially. Although there is extant literature examining the impact of the COVID-19 pandemic on healthcare workers, less emphasis has been placed on environmental services workers, who play an equally important front-line role.
Aim
To examine the impact of the COVID-19 pandemic on environmental services workers employed in healthcare settings.
Methods
Scoping review methodology. A search strategy was developed, in consultation with a medical information specialist, employing various combinations of the keywords [(environmental services worker OR health attendant OR housekeeping) AND (COVID OR coronavirus OR pandemic OR epidemic)]. Four bibliographical databases were searched from inception to 5th July 2022: OVID Medline, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and Cochrane Database.
Results
In total, 24 studies were included in this review. The studies were generally cross-sectional in design. Seroprevalence studies highlighted significantly higher rates of COVID-19 among environmental services workers (housekeeping, cleaning and janitorial staff) compared with other clinical and non-clinical staff in the same institutions. In addition, based on qualitative interviews, environmental services workers experienced greater psychological stress working during the pandemic.
Conclusions
Environmental services workers were particularly vulnerable to increased work stress and COVID-19 during the pandemic. Health systems need to do more to support these workers. Further research could investigate specific policy and procedural changes to benefit this under-recognized group in the greater healthcare workforce.
Keywords: Environmental services workers, Cleaners, Healthcare, COVID-19, Scoping review
Introduction
It is well recognized that regular disinfection, housekeeping and cleaning are essential for the daily operations of any healthcare facility. Environmental services workers are the unsung heroes who perform these arduous tasks, despite often long hours and limited renumeration [1].
During the coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), demand for deep cleaning and environmental services workers grew exponentially [2]. At the time of writing, there have been more than 555 million cases of COVID-19 and 6.3 million COVID-related deaths worldwide [3]. Besides vaccines, the importance of hygiene and personal protective measures (e.g. mask wearing and disinfecting) in stemming the transmission of SARS-CoV-2 is critical, but adds to the burden of these workers [4]. Preliminary evidence showed that the virus could survive on surfaces for up to 3 days, although surface transmission is now thought to be a minor mode of transmission [5].
Although there is extant literature examining the impact of the COVID-19 pandemic on healthcare workers [6,7], less emphasis has been placed on environmental services workers, who play an equally – if not more – important role, in the modus operandi of a well-functioning hospital. As such, this scoping review aimed to map the literature in this area and identify gaps for future research.
Methods
The protocol of this scoping review was guided by recommendations from Arksey and O'Malley's framework and the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [8,9]. A search strategy was developed, in consultation with a medical information specialist, employing various combinations of the keywords [(environmental services worker OR health attendant OR housekeeping) AND (COVID OR coronavirus OR pandemic OR epidemic)]. Four bibliographical databases were searched from inception to 5th July 2022: OVID Medline, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and Cochrane Database. The full search strategy for the individual databases is available in Supplementary Material 1. Grey literature was not searched.
The key research question was: what is the impact of the COVID-19 pandemic on environmental services workers in healthcare settings?
All study designs (case series, randomized controlled trials and observational cohort studies) were included in the initial search for this scoping review. Studies needed to have data specifically pertaining to environmental services workers, housekeeping staff or sanitary workers etc. Overlapping data studies, reviews, commentaries, and letters without original data were excluded to improve the quality of the included literature. The full text was obtained for all articles of interest, and their reference lists were hand-searched to identify additional relevant papers. Conflicts were resolved by discussion and consensus amongst four study investigators (QXN, CYLY, CEY and YLL).
Relevant quantitative and qualitative data were extracted by three study investigators (CYLY, CEY and YLL) and cross-checked by a fourth investigator (QXN) for accuracy.
Results
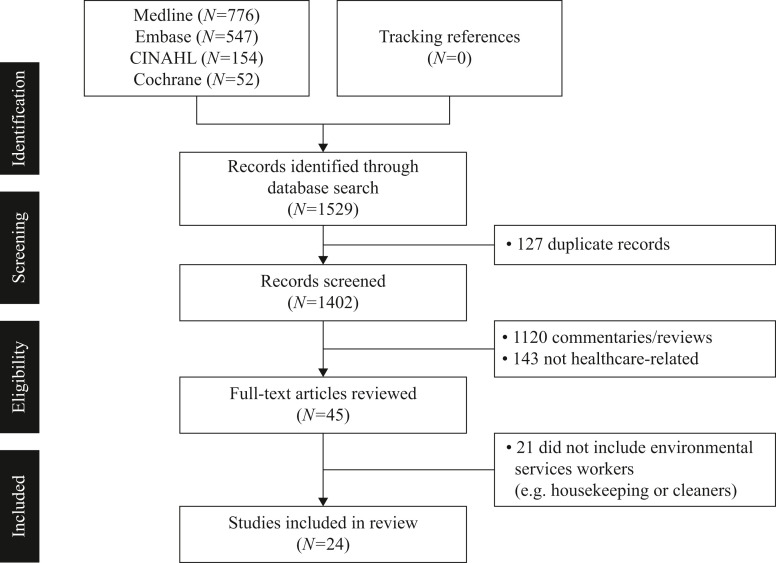
The study selection and abstraction processes are illustrated in Figure 1 . The database search identified 1529 records, from which 127 duplicates were removed. A further 1357 articles were removed after title and abstract screening, and 21 articles were removed after full-text review. Finally, 24 articles were included in the scoping review [[10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33]]. The characteristics and salient findings of the included studies are summarized in Table I, Table II, Table III , grouped broadly as SARS-CoV-2 seropositivity studies, outbreak investigations and studies on mental health.
Figure 1.
PRISMA flowchart illustrating the study selection process.
Table I.
Characteristics of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) seropositivity studies included in this scoping review (arranged alphabetically)
| Author, year | Country | Study design | Study population and sample size (N) | Key findings |
|---|---|---|---|---|
| Akinbami, 2021 [10] | USA | Cross-sectional study | Environmental services workers, N=114 (hospital) and N=69 (nursing home) | Environmental services workers in the hospital and nursing home were at elevated risk of SARS-CoV-2 seropositivity, with 2.6% (95% CI 0.6–7.5%) and 13.0% (95% CI 6.1–23.3%) seropositive, respectively. |
| Al-Kuwari, 2021 [11] | Qatar | Cross-sectional study | Housekeeping staff, N=530 | Non-clinical staff including housekeeping staff had a higher attack rate (46.8%) and higher prevalence of RT-PCR positivity (47.1%, 248/526) than clinical staff (P<0.001). |
| Baker, 2021 [12] | USA | Cross-sectional study | Environmental services workers, N=35 | Environmental services workers had a slightly higher likelihood of SARS-CoV-2 seropositivity, although with a wide CI (crude OR 1.6, 95% CI 0.4–4.6). |
| Barry, 2021 [13] | Saudi Arabia | Retrospective analysis | Housekeeping staff, N=146 | Housekeeping staff had the highest infection rate (17.1%, 25/146) compared with other healthcare workers. Most infections appeared to have been acquired in the community. |
| Cruz-Arenas, 2021 [14] | Mexico | Cross-sectional study | Janitorial staff, N=11 | Security staff (62.5%, 5/8) and janitorial staff (45.4%, 5/11) had the highest IgG seroprevalence amongst all healthcare professionals working at a ‘non-COVID’ hospital. |
| Darvishian, 2022 [15] | Iran | Cross-sectional study | Janitors and building superintendents, N=349 | Janitors and building superintendents had the lowest prevalence of SARS-CoV-2-specific IgG or IgM antibodies (9.5%, 33/349). |
| Das, 2022 [16] | India | Cross-sectional study | Ward boys and cleaners, N=97 | IgG seroprevalence was higher amongst ward boys and cleaners (29.9%, 29/97) compared with other healthcare workers in the hospital. |
| Eyre, 2020 [17] | UK | Prospective cohort study | Porters and cleaners, N=323 | Over a 3-month period, porters and cleaners had higher seroprevalence (18.6%, 60/323) and greater risk of COVID-19 compared with other healthcare professionals (adjusted OR 2.06, 95% CI 1.34–3.15; P=0.001). |
| Goenka, 2020 [18] | India | Cross-sectional study | Housekeeping staff, N=226 | Housekeeping staff had the highest SARS-CoV-2-specific IgG seroprevalence (26.1%, 59/226) and highest OR of seropositivity (adjusted OR 4.90, 95% CI 2.04–11.74; P<0.001). |
| Jacob, 2021 [19] | USA | Cross-sectional study | Environmental services workers, N=122 | Environmental services workers had slightly higher likelihood of seropositivity compared with other healthcare professionals (adjusted OR 1.5, 95% CI 0.8–3.1). |
| Mishra, 2021 [20] | India | Cross-sectional study | Housekeeping and sanitation staff, N=186 | Housekeeping and sanitation staff had higher seroprevalence (6.99%, 13/186) compared with other healthcare workers. |
| Musa, 2021 [21] | Egypt | Prospective cohort study | Patient transporters and cleaners, N=37 | Patient transporters and cleaners had higher seroprevalence (45.9%, 17/37) and higher likelihood of SARS-CoV-2 infection compared with other healthcare professionals (OR 5.94, 95% CI 2.08–16.96). |
| Oliveira, 2021 [22] | Brazil | Cross-sectional study | Cleaners, N=93 | Among healthcare professionals working in a dedicated COVID-19 facility, cleaners were most likely to be infected with COVID-19 (crude OR 2.44, 95% CI 1.26–4.73; P=0.006) based on positive SARS-CoV-2 serology. |
| Pınarlık, 2021 [23] | Turkey | Retrospective analysis | Janitorial staff, N=66 | On multi-variate analysis, being a janitorial staff worker was independently associated with increased risk of SARS-CoV-2 infection (adjusted OR 2.24, 95% CI 1.21–4.14; P=0.011). Most infections were likely acquired in the community. |
| Rosser, 2021 [24] | USA | Retrospective analysis | Environmental services, food service, patient transport staff, N=335 | On multi-variable regression analysis, environmental services, food service and patient transport staff had significantly higher likelihood of seropositivity (OR 2.64, 95% CI 1.33–4.80; P<0.001). This was not observed for other occupations in the academic medical health system. |
| Shepard, 2021 [25] | USA | Retrospective analysis | Environmental services workers (56.12% females, average age 43.18 years), N=335 | At an academic medical centre, there was significantly higher prevalence of COVID-19 R T-PCR positivity among environmental services workers (5.96%) compared with clinicians (1.93%; P<0.0001) and nurses (1.46%; P<0.0001). |
| Shields, 2020 [26] | UK | Cross-sectional study | Housekeeping staff, N=29 | In a large hospital trust, the seroprevalence of SARS-CoV-2 antibodies was higher among housekeeping staff (34.5%, 10/29 tested positive) compared with other asymptomatic healthcare workers. |
| Wattal, 2021 [27] | India | Cross-sectional study | Sanitary workers, N=203 | At a tertiary medical hospital, sanitary workers were at significantly higher risk of SARS-CoV-2 IgG seropositivity (OR 3.946; P<0.001) than other asymptomatic healthcare workers. |
| Zuñiga, 2022 [28] | Chile | Cross-sectional study | Janitorial staff, N=8606 | In regions with low and medium SARS-CoV-2 seroprevalence, doctors, nurses, allied health professionals, and janitorial and other support staff were at increased risk of infection. The likelihood of seropositivity for janitorial staff in low and medium seroprevalence regions was OR 1.12 (95% CI 0.68–1.85) and OR 1.37 (95% CI 1.07–1.74), respectively. |
CI, confidence interval; COVID-19, coronavirus disease 2019; OR, odds ratio; PPE, personal protective equipment; RT-PCR, reverse transcription polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2.
Table II.
Characteristics of outbreak investigations included in this scoping review (arranged alphabetically)
| Author, year | Country | Study design | Study population and sample size (N) | Key findings |
|---|---|---|---|---|
| Barani, 2021 [29] | India | Outbreak investigation | Housekeeping staff, N=120 | In the wake of a COVID-19 cluster in a tertiary care cancer hospital, 2.5% of the housekeeping staff tested RT-PCR positive (3/120), and they showed the highest secondary attack rate (3.3 per 100 persons) among all healthcare workers. |
| Girgis, 2022 [30] | Egypt | Outbreak investigation | Housekeeping staff, N=118 | In the wake of a hospital COVID-19 outbreak, 7.6% of the housekeeping staff were infected (9/118), and they had the highest risk of RT-PCR positivity (risk ratio 5.08, 95% CI 1.4–1.84) compared with other hospital staff. |
CI, confidence interval; COVID-19, coronavirus disease 2019; RT-PCR, reverse transcription polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2.
Table III.
Characteristics of studies on mental health of environmental services workers (arranged alphabetically)
| Author, year | Country | Study design | Study population and sample size (N) | Key findings |
|---|---|---|---|---|
| Jordan, 2022 [31] | USA | Qualitative study; semi-structured telephone interviews | Environmental services workers (69% females; average age 51 years), N=16 | The COVID-19 pandemic worsened the existing stressors facing environmental services workers, and there is a need for more support (training, education and adequate PPE) and recognition for these front-line workers. |
| Latha, 2022 [32] | India | Cross-sectional study | Housekeeping staff, N=64 | Based on self-reported DASS-21 and IES-R scores, hospital housekeeping staff had high levels of depressive, anxiety and stress symptoms during and after lockdown. Housekeeping staff had the highest levels of anxiety, and this worsened after lockdown. |
| Tamene, 2022 [33] | Ethiopia | Qualitative study; key informant interviews and one-on-one in-depth interviews | Environmental services workers, N=19 | There were concerns regarding a lack of sufficient and appropriately-sized PPE in the workplace; poor renumeration; increased work fatigue; and lack of experience and training dealing with potential hazards. |
DASS-21, Depression, Anxiety and Stress Scale 21; IES-R, Impact of Event Scale-revised; PPE, personal protective equipment.
There were six studies from the USA [10,12,19,24,25,31], six studies from India [16,18,20,27,29,32], two studies from the UK [17,26], two studies from Egypt [21,30], and one study from each of Brazil [22], Chile [28], Ethiopia [33], Iran [15], Mexico [14], Qatar [11], Saudi Arabia [13] and Turkey [23].
The seroprevalence studies, with the exception of a single study from Iran [15], consistently reported that environmental services workers (housekeeping, cleaners and janitorial staff) were significantly more likely to have contracted COVID-19 compared with other healthcare workers in the same institutions [[10], [11], [12], [13], [14],[16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28]]. The quality of these cross-sectional studies was assessed using the Joanna Briggs Institute critical appraisal checklist for analytical cross-sectional study [34] by consensus among three study investigators (QXN, CYLY and CEY). The studies had generally low-to-moderate risk of bias, with shortcomings in response rate reporting and sample size (further details in Supplementary Material 2).
One cross-sectional, quantitative study looked at the levels of anxiety, depression and stress experienced by healthcare workers, including housekeeping staff, during and after a lockdown situation [32]. Two qualitative studies conducted individual interviews with environmental services workers, and examined their thoughts, feelings and concerns during the pandemic [31,33]. All of these studies found high levels of stress and anxiety among environmental services workers during the pandemic. Of note, compared with doctors and nurses, the prevalence of anxiety during and after lockdown was significantly higher among non-clinical workers (e.g. housekeeping and security staff), and this remained significant after adjustment for possible confounders [32]. Based on self-reported Depression, Anxiety and Stress Scale 21 scores, the mean score for anxiety among housekeeping staff was 4.8 during lockdown and 7.2 after lockdown. In contrast, doctors had a lower mean anxiety score of 4.22 during lockdown and 5.6 after lockdown, and nurses had a lower mean anxiety score of 4.0 during lockdown and 7.0 after lockdown [32]. These studies collectively highlighted a clear need for more support and recognition for these frontline workers [[31], [32], [33]]. Areas of deficit include psychological support, staff training, infection control education and adequate supplies of personal protective equipment (PPE).
Discussion
COVID-19 has been an unprecedented global pandemic of unparalleled scale, and has caused a serious strain for health systems and greatly increased the demands on healthcare workers. Based on the available studies, environmental services workers appeared to be particularly vulnerable to increased work stress and COVID-19 during the pandemic.
Seroprevalence studies highlighted higher rates of COVID-19 among environmental services workers (housekeeping, cleaning and janitorial staff) compared with other clinical and non-clinical staff. In a prospective cohort study conducted in a teaching hospital in the UK over a 3-month period, porters and cleaners were found to have higher seroprevalence (18.6%, 60/323) and higher risk of COVID-19 compared with other healthcare professionals [adjusted odds ratio 2.06, 95% confidence interval (CI) 1.34–3.15, P=0.001] [17]. Similarly, in a study conducted in the wake of a COVID-19 outbreak in a university cardiothoracic hospital in Cairo, Egypt, housekeeping staff were the most affected out of all hospital staff, with 7.6% (9/118) contracting COVID-19; these workers had the highest risk of reverse transcription polymerase chain reaction positivity (risk ratio 5.08, 95% CI 1.4–1.84) [30].
This difference could be due to a combination of knowledge, training and socio-economic factors. Although the studies did not control directly for income or education attainments, occupation is a surrogate for socio-economic status. As COVID-19 could be acquired in both healthcare (albeit less likely [13,23]) and community settings, environmental services workers could have poorer knowledge and compliance with PPE use, and they tend to gather frequently during mealtimes, as highlighted by a number of studies [11,24,30]. Environmental services workers could also live in more crowded housing conditions that might expose them to SARS-CoV-2 [13]. Several international studies have found that COVID-19 further exacerbated income and socio-economic inequalities [[35], [36], [37]], and this could have adversely impacted the housing and living conditions of these employees. These have been identified as risk factors for SARS-CoV-2 transmission in other contexts. Workers living in dormitories and close quarters were particularly predisposed to COVID-19 outbreaks [38].
Environmental services workers are a vital part of the wider public health workforce as they positively impact the health and wellbeing of staff and patients through their work. Hence, due consideration and appreciation should be given to this population. Due to possibly increased staff turnover during the pandemic, infection control training should be provided (and reiterated) for these staff members. They should also be educated and receive reminders on potential sources of nosocomial and fomite transmission. In addition, across hospital systems, cost-cutting to hospital environmental services has been associated with an increased risk of nosocomial infections for these employees [39]. As mentioned above, the majority of the infections were thought to have been acquired in the community, suggesting potential social inequalities which need to be addressed.
For workers who have been infected and are returning to work, psychoneuroimmunity prevention measures (e.g. good ventilation in the workplace and availability of PPE) may also help with possible psychiatric symptoms and facilitate a smooth return to work [40].
Apart from these physical needs and issues, the qualitative studies also indicated that environmental services workers experienced greater psychological stress working during the pandemic due to increased demands, fear of contagion of the virus and staff shortages [31]. Health systems can consider additional measures to support these workers, who are at times underappreciated and underprivileged [41]. They should be entitled to paid sick leave benefits to stay home if feeling unwell. Their work and stories could be elevated and recognized, and technology and innovation should be considered to complement their work and ease their burden.
In conclusion, environmental services workers had increased work stress and heightened risk of COVID-19 during the pandemic compared with other healthcare staff. There is a paucity of studies focusing specifically on these employees, and addressing the impact of the COVID-19 pandemic on their lived experiences. Further research is needed to investigate policy and procedural changes to benefit this under-recognized group in the greater healthcare workforce.
Author contributions
QXN and JT conceived the original idea. QXN, CEY, CYLY and YLL carried out the study, investigation, and the relevant data analysis and interpretation. XX, KYF and JT contributed to the data analysis and interpretation. KYF and JT supervised the study. All authors contributed to the writing and proofreading of the final manuscript. The final manuscript was approved by all authors.
Conflict of interest statement
None declared.
Funding sources
This research did not receive any specific grant funding from agencies in the public, commercial or not-for-profit sectors.
Ethical approval
Not required.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhin.2022.09.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Siganporia P., Astrakianakis G., Alamgir H., Ostry A., Nicol A.M., Koehoorn M. Hospital support services and the impacts of outsourcing on occupational health and safety. Int J Occup Environ Health. 2016;22:274–282. doi: 10.1080/10773525.2016.1227035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tyan K., Cohen P.A. Investing in our first line of defense: environmental services workers. Ann Intern Med. 2020;173:306–307. doi: 10.7326/M20-2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johns Hopkins Coronavirus Resource Center . Johns Hopkins Coronavirus Resource Center; Baltimore, MD: 2022. COVID-19 map.https://coronavirus.jhu.edu/map.html Available at: [last accessed July 2022] [Google Scholar]
- 4.Girum T., Lentiro K., Geremew M., Migora B., Shewamare S., Shimbre M.S. Optimal strategies for COVID-19 prevention from global evidence achieved through social distancing, stay at home, travel restriction and lockdown: a systematic review. Arch Public Health. 2021;79:150. doi: 10.1186/s13690-021-00663-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katona P., Kullar R., Zhang K. Bringing transmission of SARS-CoV-2 to the surface: is there a role for fomites? Clin Infect Dis. 2022;75:910–916. doi: 10.1093/cid/ciac157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tan B.Y., Chew N.W., Lee G.K., Jing M., Goh Y., Yeo L.L., et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173:317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chew N.W., Lee G.K., Tan B.Y., Jing M., Goh Y., Ngiam N.J., et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arksey H., O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 9.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 10.Akinbami L.J., Chan P.A., Vuong N., Sami S., Lewis D., Sheridan P.E., et al. Severe acute respiratory syndrome coronavirus 2 seropositivity among healthcare personnel in hospitals and nursing homes, Rhode Island, USA. Emerg Infect Dis. 2021;27:823–834. doi: 10.3201/eid2703.204508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Kuwari M.G., AbdulMalik M.A., Al-Nuaimi A.A., Abdulmajeed J., Al-Romaihi H.E., Semaan S., et al. Epidemiology characteristics of COVID-19 infection amongst primary health care workers in Qatar: March–October 2020. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.679254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baker J.M., Nelson K.N., Overton E., Lopman B.A., Lash T.L., Photakis M., et al. Quantification of occupational and community risk factors for SARS-CoV-2 seropositivity among health care workers in a large US health care system. Ann Intern Med. 2021;174:649–654. doi: 10.7326/M20-7145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barani S., Jahan N., Karuppiah M., Chaudhuri S., Raju M., Ponnaiah M., et al. Epidemiology of hospital-based COVID- 19 cluster in a tertiary care cancer hospital, Chennai, India 2020. Clin Epidemiol Glob Health. 2021;12 doi: 10.1016/j.cegh.2021.100889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barry M., Robert A.A., Temsah M.H., Abdul Bari S., Akhtar M.Y., Al Nahdi F., et al. COVID-19 community transmission among healthcare workers at a tertiary care cardiac center. Med Sci. 2021;9:49. doi: 10.3390/medsci9030049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cruz-Arenas E., Cabrera-Ruiz E., Laguna-Barcenas S., Colin-Castro C.A., Chavez T., Franco-Cendejas R., et al. Serological prevalence of SARS-CoV-2 infection and associated factors in healthcare workers in a "non-COVID" hospital in Mexico City. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Darvishian M., Sharafkhah M., Mohammadi Z., Sadeghniiat-Haghighi K., Abdollahi A., Jafary M., et al. SARS-CoV-2 seroprevalence among health care workers in major private and public hospitals with COVID-19 patient's referral in Tehran, Iran. Front Public Health. 2022;10 doi: 10.3389/fpubh.2022.832003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Das D., Basu K., Biswas L., Bhattacharya S., Sarkar P., Pant N., et al. Asymptomatic COVID-19 infection among healthcare workers in dedicated tertiary care facility of Kolkata, India. J Clin Diagn Res. 2022;16:OC28–31. [Google Scholar]
- 18.Eyre D.W., Lumley S.F., O'Donnell D., Campbell M., Sims E., Lawson E., et al. Differential occupational risks to healthcare workers from SARS-CoV-2 observed during a prospective observational study. Elife. 2020;9 doi: 10.7554/eLife.60675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Girgis S.A., Halim M., Habil I.S., Hussein W.M., Mossad I.M., Abdel-Aziz A., et al. Investigation of a COVID-19 outbreak in a university cardio-thoracic hospital in Cairo: exploration of the risk to healthcare workers and patients. J Prev Med Hyg. 2022;62:E802–E807. doi: 10.15167/2421-4248/jpmh2021.62.4.2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goenka M., Afzalpurkar S., Goenka U., Das S.S., Mukherjee M., Jajodia S., et al. Seroprevalence of COVID-19 amongst health care workers in a tertiary care hospital of a metropolitan city from India. J Assoc Physicians India. 2020;68:14–19. [PubMed] [Google Scholar]
- 21.Jacob J.T., Baker J.M., Fridkin S.K., Lopman B.A., Steinberg J.P., Christenson R.H., et al. Risk factors associated with SARS-CoV-2 seropositivity among us health care personnel. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jordan S.R., Daddato A.E., Patel H.P., Jones C.D. Forgotten frontline workers: environmental health service employees' perspectives on working during the COVID-19 pandemic. J Hosp Med. 2022;17:158–168. doi: 10.1002/jhm.12781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Latha S.L., Priscilla T., Sudha Ty S., Saritha C., Alimchandani A., Thangaraju P. Estimation of prevalence and comparing the levels of stress, anxiety, depression, and psychological impact before and after COVID-19 lockdown among front line health care workers. J Patient Exp. 2022;9 doi: 10.1177/23743735211069805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mishra B., Behera B., Singh A.K., Mohapatra P.R., Patro B.K., Panigrahi M.K., et al. Seroprevalence of SARS-CoV-2 antibodies among healthcare workers in a teaching hospital in Eastern India. J Family Med Prim Care. 2021;10:2974–2979. doi: 10.4103/jfmpc.jfmpc_2486_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Musa S., Abdel Alem S., Amer K., Elnagdy T., Hassan W.A., Ali M.A., et al. Prevalence of SARS-CoV-2 infection and dynamics of antibodies response among previously undiagnosed healthcare workers in a university hospital: a prospective cohort study. J Infect Public Health. 2021;14:1466–1473. doi: 10.1016/j.jiph.2021.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oliveira M.S., Lobo R.D., Detta F.P., Vieira-Junior J.M., Castro T.L.S., Zambelli D.B., et al. SARS-CoV-2 seroprevalence and risk factors among health care workers: estimating the risk of COVID-19 dedicated units. Am J Infect Control. 2021;4:1197–1199. doi: 10.1016/j.ajic.2021.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pınarlık F., Genç Z., Kapmaz M., Tekin S., Ergönül Ö. Risk groups for SARS-CoV-2 infection among healthcare workers: community versus hospital transmission. Infect Dis Rep. 2021;13:724–729. doi: 10.3390/idr13030067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosser J.I., Röltgen K., Dymock M., Shepard J., Martin A., Hogan C.A., et al. Stanford Healthcare COVID-19 Workforce Response Group Severe acute respiratory coronavirus virus 2 (SARS-CoV-2) seroprevalence in healthcare personnel in northern California early in the coronavirus disease 2019 (COVID-19) pandemic. Infect Control Hosp Epidemiol. 2021;42:1053–1059. doi: 10.1017/ice.2020.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shepard J., Kling S.M., Lee G., Wong F., Frederick J., Skhiri M., et al. The prevalence of COVID-19 in healthcare personnel in an adult and pediatric academic medical center. Am J Infect Control. 2021;49:542–546. doi: 10.1016/j.ajic.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shields A., Faustini S.E., Perez-Toledo M., Jossi S., Aldera E., Allen J.D., et al. SARS-CoV-2 seroprevalence and asymptomatic viral carriage in healthcare workers: a cross-sectional study. Thorax. 2020;75:1089–1094. doi: 10.1136/thoraxjnl-2020-215414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tamene A., Habte A., Endale F., Gizachew A. A qualitative study of factors influencing unsafe work behaviors among environmental service workers: perspectives of workers, and safety managers: the case of government hospitals in Addis Ababa, Ethiopia. Environ Health Insights. 2022;16 doi: 10.1177/11786302221109357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wattal C., Oberoi J.K., Goel N., Datta S., Raveendran R., Rao B.K., et al. A cross-sectional study of SARS-CoV-2 seroprevalence among asymptomatic healthcare workers in a tertiary healthcare centre: assessing the impact of PPE guidelines. Ind J Med Microbiol. 2021;39:528–533. doi: 10.1016/j.ijmmb.2021.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zuñiga M., Lagomarcino A.J., Muñoz S., Alonso A.P., Rodriguez M.A., O'Ryan M.L. A cross sectional study found differential risks for COVID-19 seropositivity amongst health care professionals in Chile. J Clin Epidemiol. 2022;144:72–83. doi: 10.1016/j.jclinepi.2021.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Joanna Briggs Institute . JBI; Adelaide: 2020. Checklist for analytical cross sectional studies.https://jbi.global/sites/default/files/2021-10/Checklist_for_Analytical_Cross_Sectional_Studies.docx Available at: [last accessed September 2022] [Google Scholar]
- 35.Silva J., Ribeiro-Alves M. Social inequalities and the pandemic of COVID-19: the case of Rio de Janeiro. J Epidemiol Community Health. 2021;75:975–979. doi: 10.1136/jech-2020-214724. [DOI] [PubMed] [Google Scholar]
- 36.Marí-Dell'Olmo M., Gotsens M., Pasarín M.I., Rodríguez-Sanz M., Artazcoz L., Garcia de Olalla P., et al. Socioeconomic inequalities in COVID-19 in a European urban area: two waves, two patterns. Int J Environ Res Public Health. 2021;18:1256. doi: 10.3390/ijerph18031256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laajaj R., Webb D., Aristizabal D., Behrentz E., Bernal R., Buitrago G., et al. Understanding how socioeconomic inequalities drive inequalities in COVID-19 infections. Sci Rep. 2022;12:8269. doi: 10.1038/s41598-022-11706-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Deyn M.L., Ng Q.X., Loke W., Yeo W.S. A tale of two cities: a comparison of Hong Kong and Singapore's early strategies for the coronavirus disease 2019 (COVID-19) J Infect. 2020;81:e51–e52. doi: 10.1016/j.jinf.2020.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Litwin A.S., Avgar A.C., Becker E.R. Superbugs versus outsourced cleaners: employment arrangements and the spread of health care-associated infections. ILR Rev. 2017;70:610–641. [Google Scholar]
- 40.Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L., et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92. doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rocha M.R.A., Marin M.J.S., Macias-Seda J. Living, working conditions and mental health: a study with Brazilian and Spanish workers who work in hospital cleaning services. Cien Saude Colet. 2020;25:3821–3832. doi: 10.1590/1413-812320202510.35912018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.