Abstract
Background and Purpose:
Professional online communities allow healthcare providers to exchange ideas with their colleagues about best practices for patient care. Research on this topic has focused almost exclusively on primary care physicians and specialists, to the exclusion of advanced practice providers such as nurse practitioners and physician assistants. We expand this literature by examining membership and participation on these websites among each of these provider groups.
Methods:
Participants (N = 2,008; approximately 500 per provider group) responded to an Internet-based survey in which they were asked if they use professional online communities to dialogue with colleagues and if so, what their motivation is for doing so.
Conclusions:
Nearly half of those in our sample reported utilizing professional online communities. Select differences were observed between provider groups, but overall, similar patterns emerged in their membership and participation on these websites.
Implications for Practice:
Nurse practitioners and physician assistants utilize professional online communities in similar proportion to primary care physicians and specialists. Providers should be cognizant of the impact this use may have for both themselves and their patients. Researchers are urged to take into account the various professional roles within the healthcare community when developing research on this topic.
Keywords: collaborative medicine, information sharing, online communities, social media
Social media use has grown dramatically over the past decade. Facebook, Twitter, and other platforms have acquired many millions of users around the world at dramatic speed (Kaplan & Haenlein, 2010). Likewise, social media platforms have emerged for specialized, professional groups in an effort to facilitate sharing of information. For healthcare professionals, examples include Sermo, QuantiaMD, and Clinician 1. By utilizing social media, healthcare professionals have the opportunity to exchange professional views on patient care with other healthcare professionals just as the general population might use such platforms to exchange personal information and experiences with friends and family.
Von Muhlen and Ohno-Machado (2012) reviewed 50 articles focused on clinician adoption of social media through 2011. Topics covered include healthcare professional-to-patient communication, personal use of social media websites, use of social media websites to build one’s professional network, and use of user-generated reference sites. The results of their broad review show that social media has many applications within the healthcare community. Notably missing from their review, however, is insight regarding professional online communities in which healthcare provider-to-healthcare provider communication regarding patient care takes place. This omission likely reflects the fact that very little empirical research on this topic has been conducted to date. Nevertheless, communication through these platforms has the potential to impact patient treatment approaches, particularly among those with prescribing authority.
Few empirical studies directly inform our understanding of healthcare providers’ use of professional online communities. Among these few studies, McGowan and colleagues (2012) examined communication among physicians (oncologists and primary care physicians; N = 485) using professional online communities, and found that on a weekly basis or more, 61% of their sample scanned these websites and 46% contributed to conversations on these websites. Another study conducted by Cooper and colleagues (2012) inquired about professional online community participation among a broader group of physicians (family medicine, internal medicine, pediatricians, obstetricians/gynecologists, and dermatologists; N = 1750) and found that 59.1% of their sample used such websites within the past 6 months. Although both research teams surveyed only physicians, their results reveal widespread use of professional online communities among healthcare providers. Beyond this limited empirical work, researchers and practitioners have relied on thought pieces that, for example, provide guidance about the potential impacts of professional online communities (e.g., Chauhan, George, & Coffin, 2012; Dizon, Graham, Thompson, Johnson, Johnston, Fisch, & Miller, 2012; George, Rovniak, & Kraschnewski, 2013; Ventola, 2014; Yamout, Glick, Lind, Monson, & Glick, 2011; for earlier work, see Confessore, 1997; Millen, Fontaine, & Muller, 2002).
This evolving literature further lacks insight about use of professional online communities by healthcare providers other than primary care physicians and specialists (for an exception, see Lau, 2011). Healthcare settings employ a wide variety of professionals and those with different roles may make use of online communities in different ways. Nurse practitioners and physician assistants, for example, may have different reasons for using online communities than specialized providers. Moreover, professional online communities target particular roles in the healthcare community. Sermo allows only MDs and DOs to join and participate, and uses a verification process to confirm these qualifications. Clinician 1, in contrast, is directed toward nurse practitioners and physician assistants. Opportunities for use of professional online communities vary by profession within the healthcare community; consequently, membership and participation in professional online communities may differ by profession as well.
The present research provides insight about professional online community membership and participation among four groups of healthcare providers: primary care physicians, specialists, nurse practitioners, and physician assistants. We ask how often these providers use professional online communities to dialogue with colleagues and what their motivation is for doing so. Moreover, we break our analysis down by role within the healthcare community. We seek to identify commonalities and differences between the provider groups in their membership patterns and motivations for use of professional online communities. We conclude with a call for research on this important topic and give special consideration to the importance of examining all provider groups that utilize professional online communities.
Method
Data summarized in this paper were collected as part of a larger survey about healthcare providers’ perceptions of, and attitudes toward, direct-to-consumer (DTC) advertising. Results reported here are specific to the questions about professional online communities. The study was granted an exemption by the authors’ institutional review boards.
Respondents answered the survey via the Internet in an average of 15 minutes. Prior to implementation, the full survey underwent testing via cognitive interviewing, in which participants (n = 9) were probed on how and why they responded to various questions as they did, and pretesting (n = 25), which served as a pilot of the main study on a smaller scale. Minor improvements were made to the survey based on findings from this pilot work.
Participants
Approximately 500 healthcare providers from each of four fields (primary care physicians, specialists, nurse practitioners, and physician assistants) participated in the study, for a total sample size of 2,008. Most participants were recruited by postal mail from a national panel of healthcare providers, the Physician Consulting Network (PCN), which is primarily based on the American Medical Association (AMA) Masterfile. To fulfill the purpose of the larger study, 12 specialties were considered eligible based on prominent DTC therapy areas at the time of data collection (June to August 2013): allergy/ pulmonology, psychiatry, endocrinology, dermatology, rheumatology, cardiology, otolaryngology, urology, neurology, oncology, pain management, and OB/GYN. The PCN panel includes only a limited number of nurse practitioners and physician assistants, and so we additionally conducted a custom recruit of these professionals to obtain sufficient sample size. The custom recruit (conducted through DMDConnects, an approved AMA list vendor) was designed to be a random sampling by state, specialization, and practice setting, derived from master file listings. As with the original PCN panel, the randomly sampled providers from the custom recruit were mailed invitations to join the PCN panel and then were asked to complete the survey.
Critical Measures
Participants responded to several questions regarding their professional online community membership and participation. The first question assessed membership: “Are you a member of any online sites where you dialogue with other healthcare providers (e.g., DocnDoc, Sermo)?” Participants who responded “Yes” were asked to indicate how often they used these sites to 1) post information, 2) respond to others’ posts, 3) moderate discussions, 4) read posts and information, and 5) browse the site. Responses used a 1 (Never) to 5 (Always) scale. Participants were then asked to indicate (Yes or No) whether they participate in these sites to 1) seek colleague opinions, 2) provide advice to others, 3) experience camaraderie, 4) post or read about patient issues, 5) post or read about healthcare insurance provider issues, 6) post or read about office management issues, and 7) post or read about issues with pharmaceutical representatives.
Procedure
Eligible healthcare providers were sent a prenotification letter informing them of the upcoming survey invitation. Several days later they were invited via email to participate in the survey. The invitation included a unique code that was required to access a secured website that hosted the survey. All participants provided informed consent via the secure website. A cash incentive consistent with market rates was offered for participation: specialists received $75, primary care providers received $55, and nurse practitioners and physician assistants received $50. Email reminders were periodically sent to nonresponders throughout an eight week fielding period. Telephone reminder calls were made to nonresponders starting after approximately two weeks in the field.
Results
Participant characteristics are described in Table 1. Response rates and cooperation rates were calculated based on definitions provided by the American Association for Public Opinion Research (AAPOR, 2015). AAPOR defines response rate as “the number of complete interviews with reporting units divided by the number of eligible reporting units in the sample,” and cooperation rates as “the proportion of all cases interviewed of all eligible units ever contacted.” Per these definitions, the overall response rate for the existing PCN sample members was 12.8%. The overall cooperation rate was 91.9%. For the additional recruits, the response rate was 1.4% and the cooperation rate was 100%. Weights were used to make the survey data generalizable to the national population of primary care physicians, specialists, nurse practitioners, and physician assistants by adjusting for unequal selection probabilities, unequal response rates, and for any remaining deviations between the sample and population distributions. Post-stratification weights were used to calibrate the sample distribution to the known population distribution to reduce undercoverage bias and, to some extent, nonresponse bias. Population counts for use in poststratification were obtained from the AMA Master List, the American Academy for Physician Assistants Master file and American Association for Nurse Practitioners lists for nurse practitioners. Available variables for weight calibration include age, gender, region, and graduation year.
Table 1.
Unweighted Healthcare Provider Demographics by Subgroup
| Demographics | PCPs | Specialists | NPs | PAs | Total |
|---|---|---|---|---|---|
| Total number of respondents | 507 | 500 | 500 | 501 | 2008 |
| Age | |||||
| 25–34 | 3 (.59%) | 11 (2.20%) | 34 (6.80%) | 148(29.54%) | 196 (9.76%) |
| 35–44 | 109 (21.50%) | 138 (27.60%) | 112 (22.40%) | 183(36.53%) | 542 (26.99%) |
| 45–54 | 166 (32.74%) | 170(34.00%) | 159 (31.80%) | 94(18.76%) | 589 (29.33%) |
| 55–6 | 202 (39.84%) | 138 (27.60%) | 168 (33.60%) | 62 (12.38%) | 570 (28.39%) |
| 65+ | 24 (4.73%) | 42(8.40%) | 25 (5%) | 11(2.20%) | 102 (5.08%) |
| Gender | |||||
| Male | 391 (77%) | 389 (78%) | 42 (8%) | 181 (36%) | 1,003 (50%) |
| Female | 115 (23%) | 111 (22%) | 457 (92%) | 319 (64%) | 1,002 (50%) |
| Region | |||||
| Mid-West | 106(21%) | 89(18%) | 124(25%) | 104(21%) | 423 (21%) |
| Northeast | 133(26%) | 130(26%) | 113(23%) | 117(23%) | 493 (25%) |
| South | 175(34%) | 172(34%) | 167(33%) | 169(34%) | 683 (34%) |
| West | 93(19%) | 108(22%) | 96(19%) | 111(22%) | 409 (20%) |
| Years since graduation (M, SE) | 23.4 (0.40) | 22.0 (0.40) | 15.2 (0.40) | 12.7 (0.40) | 18.3 (0.20) |
| Type of practice (multiple responses permitted) | |||||
| Family Practice | 235 (46%) | 0 | 190 (38%) | 219 (44%) | 644 (32%) |
| General Practice | 69 (14%) | 0 | 31 (6%) | 43 (9%) | 143(7%) |
| Internal Medicine | 189 (37%) | 0 | 47 (9%) | 65 (13%) | 301 (15%) |
| OB/GYN | 14 (3%) | 0 | 25 (5%) | 6 (1%) | 45 (2%) |
| Other | 0 | 500(100%) | 207(41%) | 168(34%) | 825(44%) |
| Level of prescribing authority | |||||
| Unrestricted | N/A | N/A | 295 (59%) | 285 (57%) | N/A |
| Only in conjunction with a medical doctor | N/A | N/A | 111(22%) | 198 (40%) | N/A |
| Only as part of a collaborative Drug Therapy Management agreement | N/A | N/A | 94 (19%) | 18 (4%) | N/A |
| Number of patients seen/week (M, SE) | 118 (2.6) | 108 (2.5) | 76 (1.8) | 96 (2.4) | 100 (1.2) |
| Number of prescriptions written/week (M, SE) | 195 (6.7) | 129(5.1) | 89 (4.2) | 113 (4.6) | 132 (2.8) |
Note: All data are unweighted. Total N = 2,008. PCP= primary care physician; NP = nurse practitioner; PA = physician assistant.
Of the 2,008 participants, 44% (n = 882) reported using online communities to interact with other healthcare providers. Online community membership did not differ significantly by provider group (nurse practitioners: 47%; primary care physicians: 45%; specialists: 44%; physician assistants: 39%). These findings indicate that membership on healthcare professional online community websites is relatively similar across healthcare provider positions.
As shown in Figure 1, healthcare providers who reported professional online community membership engaged in a variety of activities, the most common being browsing the sites or reading posts and information, whereas moderating discussions was uncommon. Primary care physicians (M = 2.4, SE = .08) were more likely to report “Often” or “Always” (collapsed in analyses) posting information to interact with other healthcare providers than physician assistants (M = 2.2, SE = .06), t(416) = 3.05, p = .002 (see Figure 2). Although this finding emerged as significant, it should be interpreted with the understanding that the difference between means was small. No other significant differences were identified.
Figure 1.
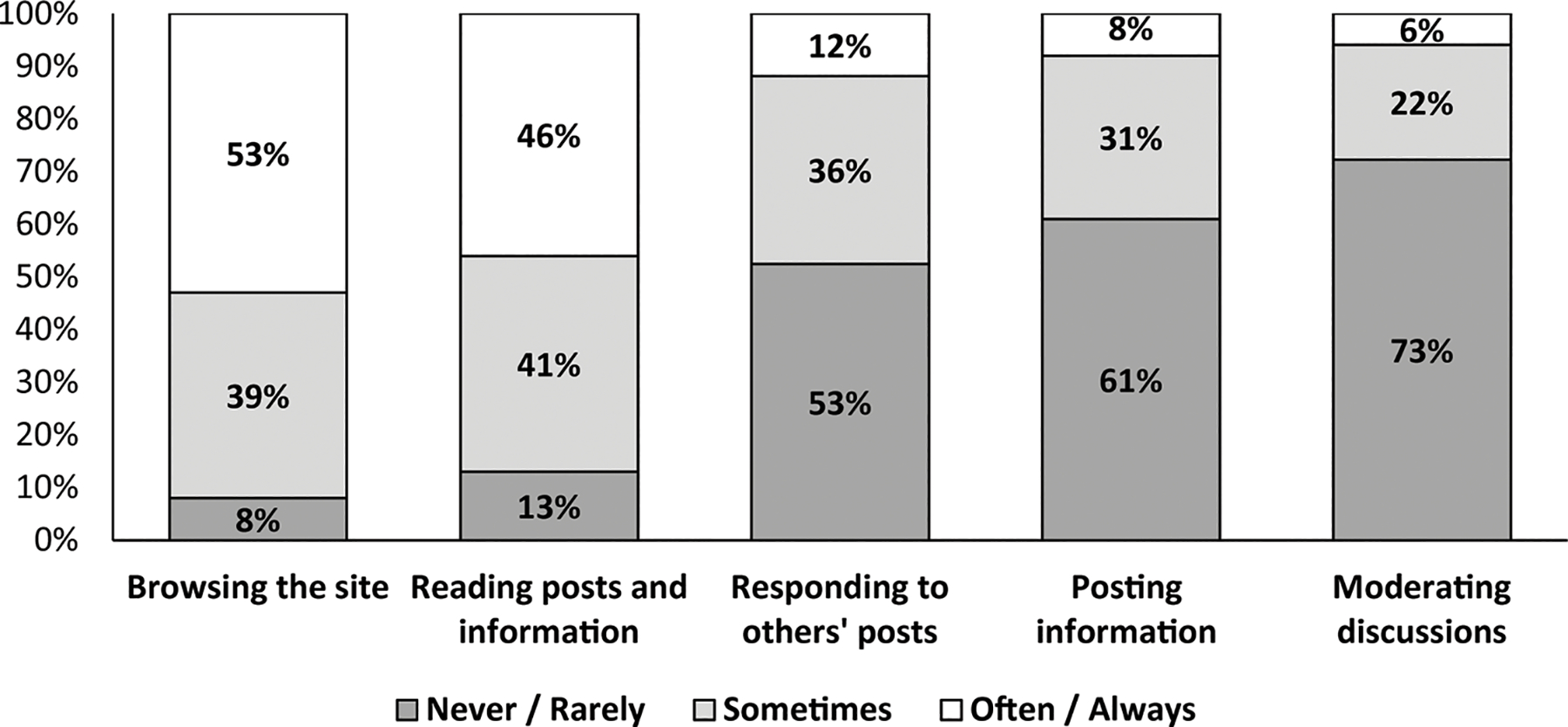
Healthcare providers’ (N = 882) frequency of professional online community activities.
Figure 2.
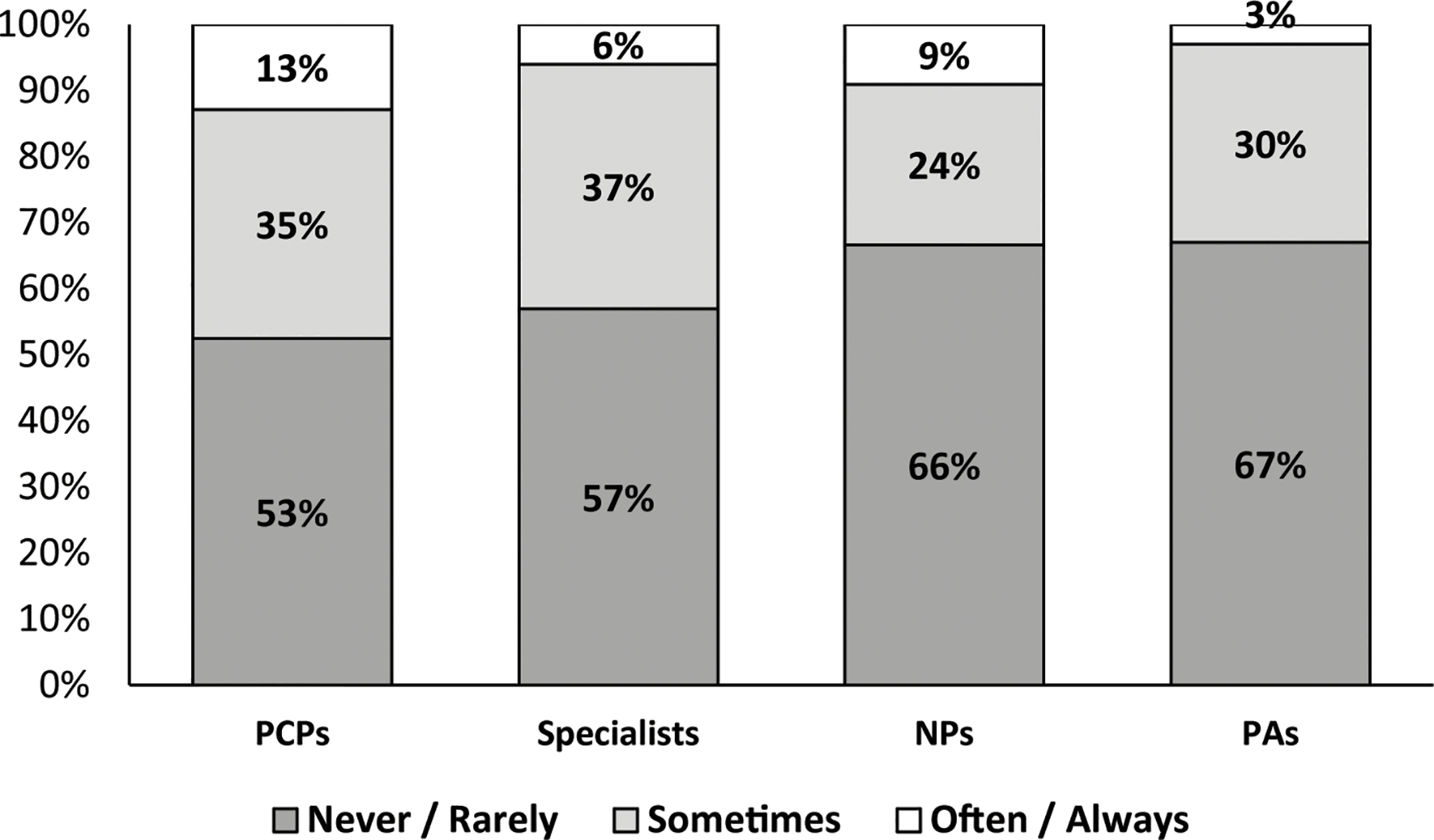
Frequency of posting information online, by healthcare provider type. N = 872. PCP = primary care physician; PA = physician assistant; NP = nurse practitioner.
When asked more specifically about their motivations for participating in these communities, healthcare providers reported a variety of reasons (see Figure 3). The most frequently cited motivations were to post or read about patient issues (86%) and seek colleague opinions (76%)—motivations that resonated across provider groups, as no significant differences were found. In contrast, only 33% of healthcare providers indicated that they participated in these communities in order to post or read about issues with pharmaceutical representatives. Of note, specialists (52%) were found to be more likely than nurse practitioners (38%) to report using online communities to provide advice to others, t(452) = 2.82, p = .005. No other significant differences between provider groups were identified.
Figure 3.
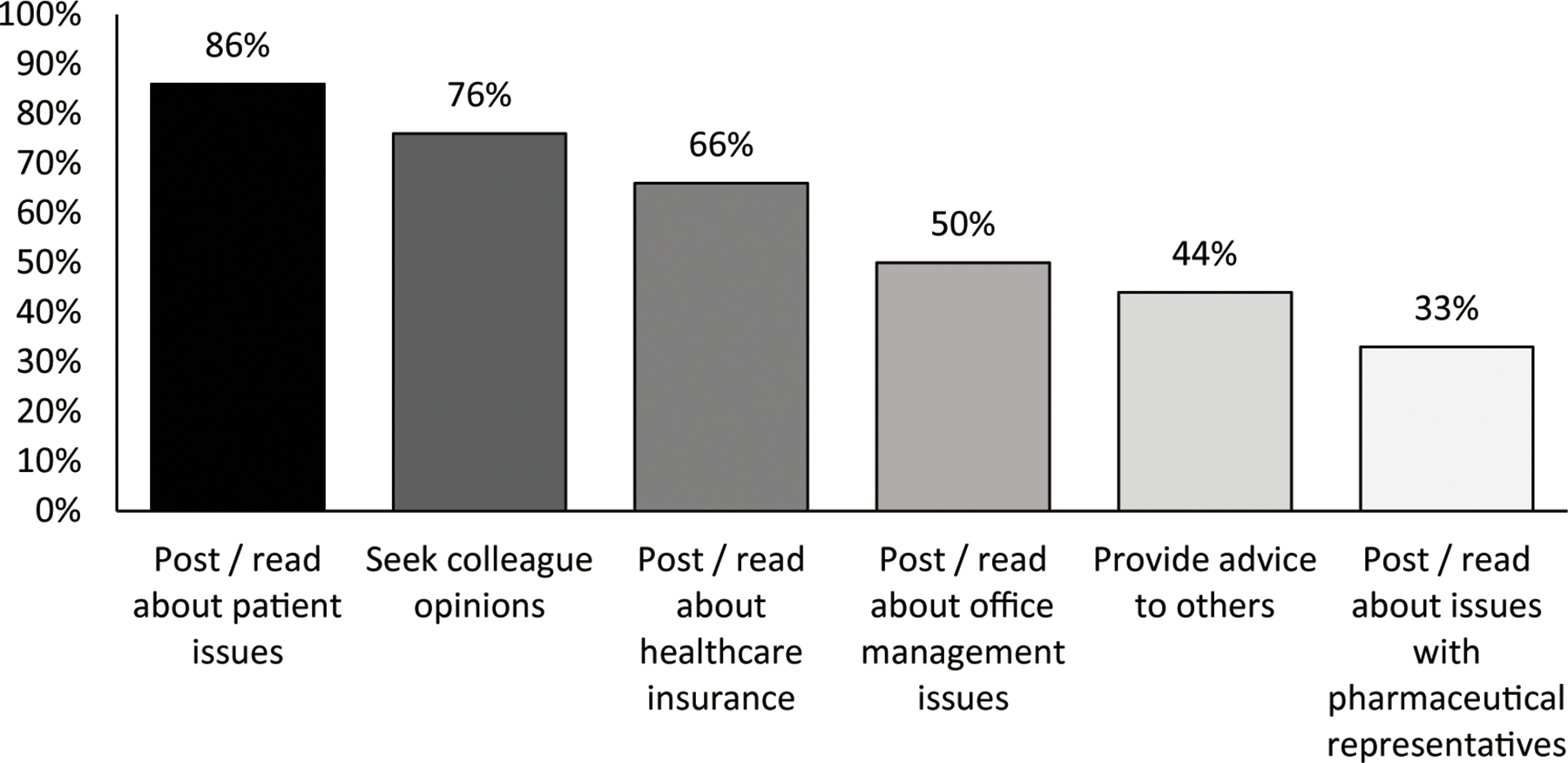
Healthcare providers’ (N = 882) motivation for participating in online communities to interact with colleagues.
Discussion
Our findings replicate outcomes from previous research concerning primary care physicians and specialists (Cooper et al., 2012; McGowan et al., 2012) and extend the literature by exploring professional online community membership and participation among nurse practitioners and physician assistants. Broadly, we found that use of these websites is widespread not only by primary care providers and specialists but also by nurse practitioners and physician assistants. Across the provider groups, use of these online communities most commonly involved relatively passive behavior such as browsing the sites rather than responding to others or posting information. Over three-quarters of providers were motivated to use these communities to seek out colleague opinions and post or read about patient issues. This motivation may reflect providers’ strategic use of these communities as a problem solving tool where they can “crowd-source” solutions with access to large numbers of other providers. Von Muhlen and Ohno-Machado (2012) found evidence that providers do use social media in this way.
We found small differences between the provider groups. Specialists were more likely than nurse practitioners to use online communities in order to provide advice to others, and primary care physicians were more likely than physician assistants to post information. The tendency for primary care physicians and specialists to share information and for physician assistants and nurse practitioners to seek information is not wholly unexpected. The responsibilities of physician assistants and nurse practitioners are continuously increasing (e.g., Moran, 2014; Naylor & Kurtzman, 2010) and so these professionals may be seeking to close knowledge gaps in efforts to meet new responsibilities. The overarching finding from this research, however, is that nurse practitioners and physician assistants are utilizing these sites at approximately the same rate and for similar purposes as primary care physicians and specialists. This is important to acknowledge because utilization of professional online communities is likely to have direct impact on patient care (e.g., see Ventola, 2014). The present research provides evidence that a large proportion of healthcare providers, regardless of role, are gathering information and obtaining and sharing advice from other healthcare providers via professional online communities.
Utilization of professional online communities is an important phenomenon in modern healthcare. Historically, healthcare providers were limited to reliance on their own knowledge, review of research literature, and perhaps consultation of colleagues within their own offices, provider networks, medical societies or associations. Professional online communities allow for access to the medical knowledge of countless healthcare professionals. Some believe that knowledge may provide certain advantages for clinicians. McGowan and colleagues (2012) reported that over half of their sample believed that these communities improved the quality of care they delivered. Nonetheless, additional research is needed to determine whether professional use of online communities actually translates to improved care rather than merely the perception of improved care.
Utilization of professional online communities may present risks as well. Access to more information does not always translate to better quality information. While providers have a frame of reference for advice they solicit from others in their practice, it may be more difficult to evaluate the quality of the advice provided on social media if they are not familiar with the source. Inappropriately trusting information communicated on these websites could result in patient harm and legal action. Healthcare professionals are expected to provide care using knowledge they accrued during their extensive training programs. How might patients respond if harm results not merely from a failure to apply this knowledge, but from misinformation that was communicated via an online forum? Grajales and colleagues (2014) and Ventola (2014) ask important questions about ethics, professionalism, privacy and confidentiality, and other issues that should be considered when healthcare professionals make use of these platforms. The present research confirms that large numbers of physician assistants and nurse practitioners are active on these websites, and consequently, it will be important for these professionals to remain cognizant of both the positive and negative aspects of participation.
The present research included a few limitations of which we are mindful. First, our results are limited to descriptive summaries of professional online community membership and participation. This ultimately limits what we can conclude about our topic. Second, our data collection method (i.e., an Internet survey) potentially biases our results in that persons willing to answer an Internet survey may be more likely to participate in online communities. Third, although consistent with response rates for online surveys involving medical practitioners (Braithwaite et al., 2003) the current study achieved a relatively low response rate. Although maintaining high response rates is always desirable, research evidence indicates that nonresponse bias may be less of a concern for physician surveys compared to surveys with the general population as most studies examining nonresponse in physician surveys have found no or only minimal amounts of response bias (Kellerman & Herold, 2001; Cull et al., 2005; Barclay et al., 2006; Menachemi et al., 2006; McFarlane et al., 2007; absent available research, nurse practitioners and physician assistants are assumed to be similar to physicians in this regard). In line with this research, we found that our sample was similarly distributed to the PCN panel across a range of demographics. A nonresponse analysis did find significant differences for gender, age, and years of practice, but these variables were used in weighting to minimize nonresponse bias. Finally, because PCN did not have sufficient numbers of physician assistants or nurse practitioners on its panel, we conducted a custom recruit. The majority (67%) of the nurse practitioner sample came from the original PCN panel; for physician assistants, the majority (67%) came from the custom recruit. Care was taken to reduce any potential bias introduced from the custom recruit and the data was weighted to reduce undercoverage bias. Both the PCN panel and DMDConnects pull from the same general pool of professionals using the same type of sources, so it’s not anticipated that there would be substantial difference in the resulting samples from each, nor would one be expected to be more or less representative than the other. Although it is unlikely, we cannot rule out that the difference in the databases may have contributed to the responses.
We conclude with a call for research regarding professional online community membership and participation among healthcare providers. Existing research on this topic is limited, and so in a broad sense, any new contributions are likely to be informative. And it is not difficult to identify potential areas for contribution. What effects do healthcare professional online community membership and participation have on diagnosis and treatment? Which aspects of these online communities promote appropriate patient care? Which aspects are potentially harmful to patient care? Even basic questions such as these have not received sufficient attention in the literature.
Beyond this general call for additional research, we especially urge researchers to take into account role within the healthcare provider community. Ideally, these investigations will involve nurse practitioners and physician assistants, but also other professional roles that involve direct patient care, such as registered nurses. These efforts will allow for not only broader representation of these professionals’ viewpoints and experiences within the research literature, but will also allow for greater precision in our understanding of the phenomena of interest. For example, why might healthcare professionals in certain positions be more likely than those in other positions to actively share advice? Are specific features of online communities more advantageous than others for particular healthcare professions (e.g., photo sharing for radiologists)? The study of healthcare professional online communities and their impact on healthcare professionals and patient care presents an important area of research, and we look forward to seeing this literature grow.
Contributor Information
Bridget J. Kelly, RTI International, Research Triangle Park, NC.
Vanessa Boudewyns, RTI International, Washington, DC
References
- American Association for Public Opinion Research (AAPOR). (2015). Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. Retrieved from http://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions2015_8theditionwithchanges_April2015_logo.pdf
- Barclay S, Todd C, Finlay I, Grande G, & Wyatt P (2006). Not another questionnaire! Maximizing the response rate, predicting non-response and assessing non-response bias in postal questionnaire studies of GPs. Family Practice, 19, 105–111. [DOI] [PubMed] [Google Scholar]
- Braithwaite D, Emery J, Lusignan S, & Sutton S (2003). Using the Internet to conduct surveys of health professionals: A valid alternative? Family Practice, 20, 545–551. [DOI] [PubMed] [Google Scholar]
- Chauhan B, George R, & Coffin J (2012). Social media and you: what every physician needs to know. Journal of Medical Practice Management, 28, 206–209. [PubMed] [Google Scholar]
- Confessore SJ (1997). Building a learning organization: Communities of practice, self-directed learning, and continuing medical education. The Journal of Continuing Education in the Health Professions, 17, 5–11. [Google Scholar]
- Cooper CP, Gelb CA, Rim SH, Hawkins NA, Rodriguez JL, & Polonec L (2012). Physicians who use social media and other internet-based communication technologies. Journal of the American Medical Informatics Association, 19, 960–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cull WL, O’Connor KG, Sharp S, & Tang SS (2005). Response rates and response bias for 50 surveys of pediatricians. Health Services Research, 40, 213–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dizon DS, Graham D, Thompson MA, Johnson LJ, Johnston C, Fisch MJ, & Johnson LJ (2012). Practical guidance: the use of social media in oncology practice. Journal of Oncology Practice, 8, e114–e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George DR, Rovniak LS, & Kraschnewski JL (2013). Dangers and opportunities for social media in medicine. Clinical Obstetrics and Gynecology, 56, 453–462. 10.1097/GRF.0b013e318297dc38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grajales FJ, Sheps S, Ho K, Novak-Lauscher H, & Eysenbach G (2014). Social media: a review and tutorial of applications in medicine and health care. Journal of Medical Internet Research, 16, e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan AM & Haenlein M (2010). Users of the world, unite! The challenges and opportunities of social media. Business Horizons, 53, 59–68. [Google Scholar]
- Kellerman SE, & Herold J (2001). Physician response to surveys: A review of the literature. American Journal of Preventative Medicine, 20, 61–67. [DOI] [PubMed] [Google Scholar]
- Lau AS (2011). Hospital-based nurses’ perceptions of the adoption of Web 2.0 tools for knowledge sharing, learning, social interaction and the production of collective intelligence. Journal of Medical Internet Research, 13, e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcfarlane EM, Olsmted MG, Murphy J, & Hill CA (2007). Nonresponse bias in a mail survey of physicians. Evaluations and the Health Professions, 30, 170–185. [DOI] [PubMed] [Google Scholar]
- McGowan BS, Wasko M, Vartabedian BS, Miller RS, Freiherr DD, & Abdolrasulnia M (2012). Understanding the factors that influence the adoption and meaningful use of social media by physicians to share medical information. Journal of Medical Internet Research, 14, e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menachemi N, Hikmet N, Stutzman M, & Brooks RG (2006). Investigating response bias in an information technology survey of physicians. Journal of Medical Systems, 30, 277–282. [DOI] [PubMed] [Google Scholar]
- Millen DR, Fontaine MA, & Muller MJ (2002). Understanding the benefit and costs of communities of practice. Communications of the ACM, 45, 69–73. [Google Scholar]
- Moran B (2014, August 1). The physician assistant will see you now. The New York Times. Retrieved from http://www.nytimes.com [Google Scholar]
- Naylor MD, & Kurtzman ET (2010). The role of nurse practitioners in reinventing primary care. Health Affairs, 29, 893–899. [DOI] [PubMed] [Google Scholar]
- Ventola CL (2014). Social media and health care professionals: Benefits, risks, and best practices. Pharmacy and Therapeutics, 39, 491–499. [PMC free article] [PubMed] [Google Scholar]
- Von Muhlen M & Ohno-Machado L (2012). Reviewing social media use by clinicians. Journal of the American Medical Informatics Association, 19, 777–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamout SZ, Glick ZA, Lind DS, Monson RA, & Glick PL (2011). Using social media to enhance surgeon and patient education and communication. Bulletin of the American College of Surgeons, 96, 7–15. [PubMed] [Google Scholar]


