Abstract
Background
The advent of immune checkpoint inhibitors (ICIs) have led to a paradigm change in the management of metastatic renal cell carcinoma (mRCC), nevertheless, the benefit of treatment is confined to a limited proportion of patients. Therefore, the identification of predictive biomarkers for response to ICIs represents an unmet clinical need. Here, we performed a large-scale plasma proteomic profile of patients with mRCC, treated with nivolumab, to identify soluble molecules potentially associated with clinical benefit.
Methods
We analyzed the levels of 507 soluble molecules in the pretreatment plasma of 16 patients with mRCC (discovery set) who received nivolumab therapy as a single agent. The ELISA assay was performed to confirm the protein level of candidate biomarkers associated to clinical benefit in 15 patients with mRCC (validation set). Survival curves of complete cohort were estimated by the Kaplan-Meier method and compared with the log-rank test.
Results
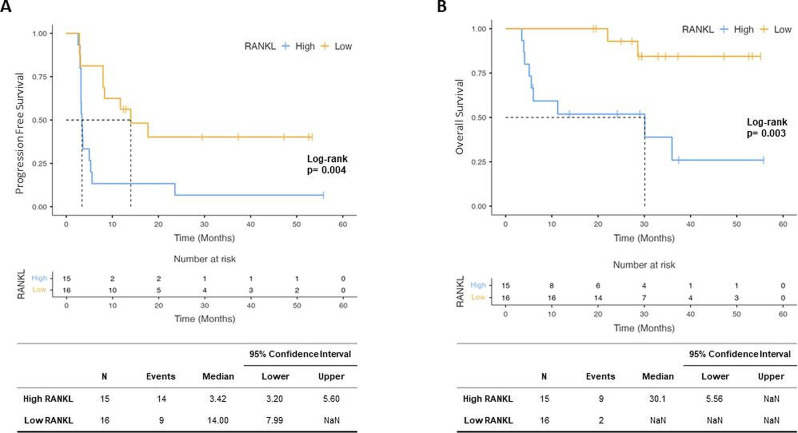
Out of 507 screened molecules, 135 factors were selected as expressed above background and 12 of them were significantly overexpressed in patients who did not benefit from treatment (non-responders (NR)) compared with responders (R) group. After multiplicity adjustment, receptor activator of nuclear factor kappa-Β ligand (RANKL) was the only molecule that retained the statistical significance (false discovery rate: 0.023). RANKL overexpression in NR patients was confirmed both in discovery (median NR: 528 pg/mL vs median R: 288 pg/mL, p=0.011) and validation set (median NR: 440 pg/mL vs median R: 253 pg/mL, p<0.001). Considering the complete cohort of patients (discovery+validation set), significantly higher RANKL levels were found in patients who primarily progressed from treatment compared with those who had a partial response (p=0.003) or stable disease (p=0.006). Moreover, patients with low RANKL levels had significant improvements in progression-free survival (median 14.0 months vs 3.4 months, p=0.004) and overall survival (median not reached vs 30.1 months, p=0.003).
Conclusions
Our exploratory study suggests RANKL as a novel independent biomarker of response and survival in patients with mRCC treated with nivolumab.
Keywords: Immunotherapy, Kidney Neoplasms
Key messages.
The clinical benefit of immune checkpoint inhibitors is still limited to a minority of patients reflecting the need to identify novel non-invasive biomarkers to improve patient selection. Currently available markers such as programmed death ligand-1 expression and tumor mutational burden have shown important limitations in metastatic renal cell carcinoma (mRCC) setting.
Our extensive proteomic analysis identified receptor activator of nuclear factor kappa-Β ligand (RANKL) as potential biomarker associated to response and survival in patients with nivolumab-treated mRCC.
The findings presented here, if confirmed in a larger prospective trial, could validate the predictive role of RANKL and translate this biomarker in clinical practice.
Introduction
The development of immune checkpoint inhibitors (ICIs) revolutionized the armamentarium for the treatment of metastatic renal cell carcinoma (mRCC) leading to a remarkable improvement in patients’ outcome and quality of life.1–7 In particular, immunotherapy entered the mRCC clinical scenario after the publication of the Phase 3 CheckMate-025 trial results.1 2 This study demonstrated superior efficacy for the anti-programmed cell death protein- 1 (PD-1) nivolumab compared with the standard-of-care everolimus in patients who had received a prior line with antiangiogenic agents. More recently, ICIs have been investigated in the first-line setting alone or associated with other agents (ipilimumab or antivascular drugs), showing significant survival benefit over antivascular tyrosine kinase inhibitor (TKI) monotherapy.3–7 Unfortunately, only a limited proportion of patients with mRCC achieved a significant and durable disease control from ICIs treatment. Therefore, the identification of predictive biomarkers of ICI clinical benefit represents the major clinical need in mRCC in order to increase the number of patients who may benefit from these treatments and reduce the exposition to potentially inactive, but nevertheless toxic, agents. In mRCC, programmed death ligand-1 (PD-L1) assessment demonstrated to be more prognostic8–10 than predictive and, therefore, it cannot be used in daily clinical practice. Indeed, in CheckMate-0251 and CheckMate-2143 trials, patients benefit from ICIs treatment regardless of the PD-L1 expression levels. Similarly, in the KEYNOTE-426 study, the efficacy of pembrolizumab plus axitinib was observed both in patients with high and low PD-L1 expression.6 In addition, several technical issues related to immunohistochemistry tests and thresholds have contributed to the inconclusive results achieved. Similarly, in mRCC setting, data supporting tumor mutational burden (TMB) as potential predictive biomarker to ICIs response are limited and conflicting.11 In this regard, RCC is considered a ‘cold’ tumor with a low TMB compared with the ‘hot tumor’ such as melanoma and non-small cell lung cancer.12 13 Tumor microenvironment including tumor infiltrating immune cells and microbiome14–16 are other interesting fields of investigation, but these are far to be reproducibility as biomarkers.
Here, we focused on the identification of circulating biomarkers potentially associated with ICIs response in plasma of patients with mRCC. In particular, an extensive panel of 507 soluble molecules including cytokines, chemokines, adipokines, growth factors, angiogenic factors, proteases, soluble receptors and soluble adhesion molecules was evaluated in patients with mRCC before starting nivolumab and correlated with clinical benefit associated with ICI therapy.
Material and methods
Study design and patient characteristics
A consecutive series of 31 patients with mRCC was administered with nivolumab from 2017 to 2020 and followed-up until December 2021 at Fondazione Policlinico Universitario Campus Bio-Medico. The study has been designed to provide an adequate discovery set (16 patients) and validation cohort (15 patients) (see Sample size section below). The study was conducted in accordance with the principles of the Helsinki declaration.
The inclusion criteria were patients who were at least 18 years old, with a performance status of 0–1, with good or intermediate risk by IDMC criteria, no signs of active autoimmune disease and treated with nivolumab as monotherapy as second line or third line of treatment for advanced disease. Plasma samples were collected at the day of the first cycle of treatment before the infusion. The patients’ disease had to be measurable per Response Evaluation Criteria in Solid Tumors (RECIST) V.1.1 at baseline and had to be evaluated for response to treatment by radiological evaluation (CT scan) every 12 weeks. We considered two groups: responder (R) and non-responder (NR). Briefly, R were defined as patients who showed either an objective response and/or a stable disease (SD) lasting at least 6 months and NR were patients who showed progressive disease (PD) at first radiological evaluation according to RECIST V.1.1 criteria. Progression-free survival (PFS) was defined as the time from the first infusion of nivolumab to the first documented tumor progression and overall survival (OS) was defined as the time from the first infusion of nivolumab to death or last news.
Sample size
Sample size estimation for discovery (discovery) set was calculated to identify circulating molecules significantly associated, after false discovery rate (FDR) correction, to a better prognosis during treatment with nivolumab. The following parameters were used: G0 (estimating a number of detected circulating molecules)=150; E(R0) (mean number of false positives)=1; expected differential expression between R and NR of |μ1|=2.5 on a log2 scale; anticipated experimental error SD (σ)=0.70 on a log2 scale.17 For these specifications, eight samples for each group were needed. Sample size for validation set has been calculated based on an estimated effect size of d=1.47 (detected on discovery set). Considering a one tail t-test statistics with an alpha error probability of 0.05, a power of 0.8 and an allocation ratio of 1 a total of 14 patients was required.
Proteomic assay
A panel of 507 human target proteins was analyzed using the human antibody Array Membrane Kit (RayBiotech) according to the manufacture instructions. In brief, the primary amines of samples were biotinylated and added on the membrane array. After overnight incubation, the Horseradish Peroxidase (HRP)-conjugated streptavidin was added and then the signals were visualized by chemiluminiscence. Band signal was detected by ChemiDoc MTP Imaging System (Bio-Rad) and their intensity was quantified using ImageLab Software (Bio-Rad). The signals were normalized using the positive membrane internal controls (anti-HRP and anti-streptavidin control signals).
Plasma RANKL assessment
Receptor activator of nuclear factor kappa-Β ligand (RANKL) concentrations were determined in plasma samples using Human TRANCE-RANKL/TNFSF11 kit (R&D Systems) according to the manufacturer instructions. A stop solution was added to the ELISA plates at the end of the assay resulting in a change of color (from blue to yellow). Optical density was calculated at 450 nanometers using a microplate reader (Tecan Infinite M200Pro) and a standard curve was created. Data were expressed in picograms per milliliter (pg/mL).
Statistical analysis
T-test statistics was used to identify circulating molecules that can discriminate between R and NR. FDR correction for multiple hypothesis testing was applied. Survival curves were estimated by the Kaplan-Meier method and compared with the log-rank test (univariate analysis). Univariate HRs were calculated using log-rank method. Variables found to be statistically significant at the p<0.05 level.
Results
Clinicopathological findings of the patient population
From 2017 to 2020, a consecutive series of 31 patients with advanced RCC (discovery+validation set) treated with anti-PD-1 therapy nivolumab was prospectively enrolled. The median follow-up was 29.5 months (95% CI 28.8 to 52.6). The median PFS and OS were 5.9 months (95% CI 3.2 to 19.6) and not reached (95% CI 28.6 to not reached), respectively. The clinicopathological features of the discovery and validation set were similar and are summarized in table 1.
Table 1.
Clinicopathological variables of study population
| Discovery set (N=16) | Validation set (N=15) |
|
| Sex | ||
| Female | 5 (31%) | 4 (27%) |
| Male | 11 (69%) | 11 (73%) |
| Age | ||
| ≥66 | 9 (56%) | 7 (47%) |
| <66 | 7 (44%) | 8 (53%) |
| Therapy line | ||
| Second | 13 (81%) | 12 (75%) |
| Third | 3 (19%) | 3 (25%) |
| First-line TKI | ||
| Sunitinib | 11 (69%) | 8 (53%) |
| Pazopanib | 5 (31%) | 7 (47%) |
| IMDC score | ||
| Good risk | 5 (31%) | 5 (33%) |
| Intermediate risk | 11 (69%) | 10 (67%) |
IMDC, International Metastatic RCC Database Consortium; TKI, tyrosine kinase inhibitor.
RANKL is overexpressed in ‘non-responders’ patients
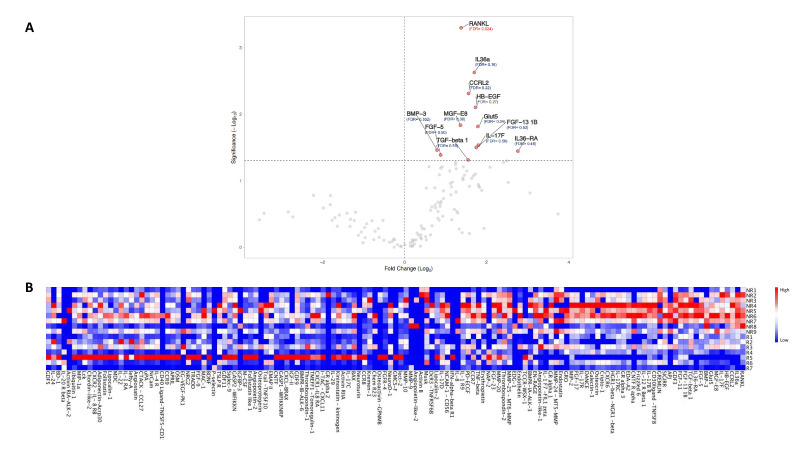
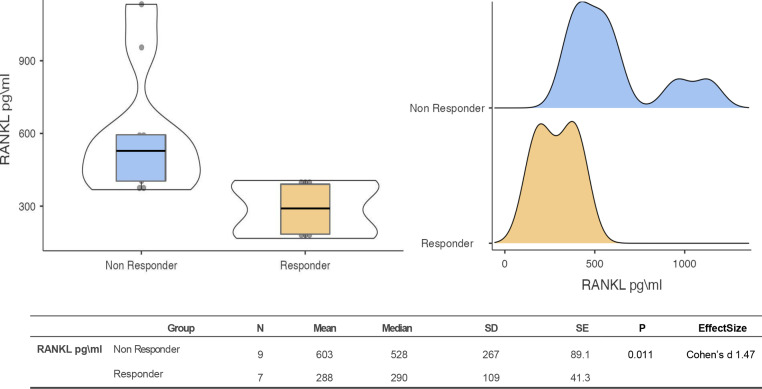
The analysis of soluble proteomic profile was performed on a discovery set of 16 patients (7 R and 9 NR patients). Out of 507 screened molecules, 135 factors were detected in plasma samples and 12 of them were significantly increased in NR (p<0.05) compared with R patients before FDR correction. After FDR correction, RANKL was found to be the only significant overexpressed factor (FDR: 0.023) (figure 1). ELISA assay confirmed in the discovery set that RANKL levels were significant higher in NR group (median 528 pg/mL) compared with patients who benefit from treatment (median 288 pg/mL) (p=0.011) (figure 2).
Figure 1.
(A) Volcano plot for differential soluble molecules expression in patients with R and NR metastatic renal cell carcinoma (molecules significantly overexpressed are on the right). (B) Heat map of relative intensity signal (expression) of 135 soluble factors detected. FDR, false discovery rate; NR, non-responder; R, responder; RANKL, receptor activator of nuclear factor kappa-Β ligand.
Figure 2.
Box/violin plot and density plot representing RANKL levels in responder and non-responder patients of discovery set. RANKL, receptor activator of nuclear factor kappa-Β ligand.
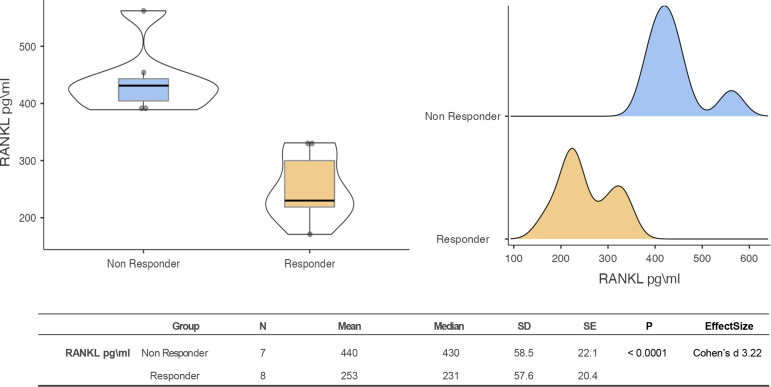
To confirm the predictive value of RANKL for response to nivolumab treatment, we analyzed RANKL soluble levels in a validation set of 15 patients (8 R and 7 NR patients). Data showed a significant overexpression of RANKL in plasma of NR patients compared with R patients (median 440 pg/mL vs 253 pg/mL, p<0.001) (figure 3).
Figure 3.
Box/violin plot and density plot representing RANKL levels in responder and non-responder patients of validation set. RANKL, receptor activator of nuclear factor kappa-Β ligand.
RANKL is associated to response and survival in patients with mRCC treated with nivolumab
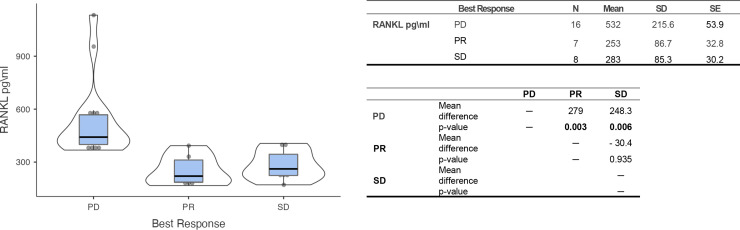
First, the association between RANKL and response to nivolumab treatment was evaluated in our complete cohort (31 patients) by ELISA test. Notably, higher RANKL levels were found in patients who progressed from treatment compared with those had a partial response (PR) (p=0.003) or SD (p=0.006). No differences were observed in R group (PR vs SD patients) (figure 4).
Figure 4.
Box/violin plot representing RANKL levels in the three classes of patients (PD, PR and SD). PD, progressive disease; PR, partial response; RANKL, receptor activator of nuclear factor kappa-Β ligand; SD, stable disease.
Next, PFS and OS were evaluated dichotomizing patients in ‘High’ and ‘Low’ RANKL according to the median RANKL expression value. Data showed that Low RANKL patients had significant improvements in both PFS and OS. In particular, the median PFS in the RANKL Low and High class were, respectively, 14.0 months (95% CI 7.99 to not reached) and 3.4 (95% CI 3.2 to 5.6) (p=0.004) (figure 5A). Similarly, the median OS in the RANKL Low and High group were, respectively, not reached (95% CI not reached to not reached) and 30.1 (95% CI 5.56 to not reached) (p=0.003) (figure 5B). Univariate analyses for PFS and OS with all clinicopathological variables were conducted (online supplemental table 1). Clinically relevant variables such as sex, age, International Metastatic RCC Database Consortium score, line of treatment and TKI used as first line were not associated with survival parameters.
Figure 5.
Kaplan-Meier curves reporting the progression-free survival (A) and overall survival (B) in Low and High RANKL patient stratified according to RANKL median value. RANKL, receptor activator of nuclear factor kappa-Β ligand.
jitc-2022-005136supp001.pdf (94.2KB, pdf)
Discussion
Our extensive proteomic analysis identified pre-treatment levels of RANKL as a specific biomarker associated to response and survival in patients with nivolumab-treated mRCC. Although the sample size is limited, our study provides the first evidence of correlation between RANK–RANKL axis and response to anti-PD-1 agent in patients with metastatic renal cancer. Previous studies investigating the possibility of repurposing the RANKL inhibitor, denosumab, from an antiresorptive agent to cancer immunotherapy in combination with ICIs.18 19 In this regard, two case reports showed that denosumab in combination with ipilimumab (anti-cytotoxic T-lymphocytes-associated protein 4 (CTLA-4) therapy) induced dramatic responses in patients with metastatic melanoma.20 21 In addition, two retrospective analyses in patients who had bone metastasis with melanoma or non-small cell lung cancer revealed that RANKL inhibition may enhance the antitumor effects of ICIs.22 In accordance with these results, preclinical data demonstrated synergistic effects of RANK/RANKL inhibitors and anti-CTLA-4 agents in immune-mediated tumor rejection.19 23 However, mechanisms underlying the synergistic action of anti-RANKL and ICIs remain unclear. Several evidences showed that RANKL/RANK is involved not only in bone homeostasis, but also in various physiological immune processes. Interestingly, RANK–RANKL pathway is required for the development of the autoimmune regulator (AIRE)-expressing medullary thymic epithelial cells, crucial in the induction of central T-cell tolerance. In vivo RANKL blockade selectively and transiently depleted central tolerance mechanisms allowing the increased generation of antitumor T cells.24 Moreover, it has been widely demonstrated that RANK is expressed in a variety of immune cells including macrophages, dendritic cells, natural killers (NKs), T cells, and myeloid-derived suppressor cells (MDSCs). In tumor microenvironment, RANKL signaling play a key role in modulating the immunological niche inducing T cell and NK suppression and promoting regulatory T cells or MDSCs activation.25–27 Taken together, these evidences partially explain how RANKL could affects antitumor responses of the immune system supporting our findings.
As previously mentioned, our exploratory study included a small number of patients, but it was adequately powered to screen the potential prognostic/predictive role of soluble molecules (discovery set) and to confirm the magnitude of differences observed in RANKL levels (validation set). However, sample size was designed taking into account binary endpoint (R vs NR) and not survival endpoints (differences in PFS or OS) that would have required a larger number of patients. Moreover, the study was at least in part limited by immortal time biases since patients who died before first CT scan restaging were excluded. In addition, RANKL levels were only evaluated at the baseline and there is no longitudinal assessment of its dynamics during treatment and on progression. Finally, although we observed a clear association between RANKL levels and poor clinical outcomes, its predictive role cannot be definitively stated in absence of control group not treated with ICIs.
Overall, this hypothesis-generating result suggests that RANKL might represent a novel biomarker to stratify patients affected by RCC treated with nivolumab. However, the establishment of a cut-off for RANKL expression, which could be specified prospectively in future studies, would be needed for validation of the biomarker. Moreover, the association with clinical benefit and the biological role of RANKL to immune-related processes suggest its potential predictive role related to modulation of tumor-associated immunity. Confirmatory results in larger prospective studies, including a control group of patients who do not receive ICI treatment, are warranted also to validate its predictive value.
Acknowledgments
We acknowledge the Italian Network for Research in Urologic-Oncology (MEET-URO)
Footnotes
DS and FP contributed equally.
Contributors: Conception and design: FP and DS. Development of methodology: SS, MI, and MS. Analysis and interpretation of data: FP, MI, and SS. Writing, review, and/or revision of the manuscript: MI, MS, SC, DS, and FP. Study supervision: GT and BV. All authors read and approved the final manuscript. MS is the guarantor.
Funding: The study was supported by Bristol Myers Squibb.
Competing interests: No, there are no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
The study was approved by the Internal Review and Ethics Boards of the Fondazione Policlinico Universitario Campus Bio-Medico (Prot. N. 48.17OSS). Participants gave informed consent to participate in the study before taking part.
References
- 1.Motzer RJ, Escudier B, McDermott DF, et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med 2015;373:1803–13. 10.1056/NEJMoa1510665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Escudier B, Sharma P, McDermott DF, et al. CheckMate 025 randomized phase 3 study: outcomes by key baseline factors and prior therapy for nivolumab versus everolimus in advanced renal cell carcinoma. Eur Urol 2017;72:962–71. 10.1016/j.eururo.2017.02.010 [DOI] [PubMed] [Google Scholar]
- 3.Motzer RJ, Rini BI, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in first-line treatment for advanced renal cell carcinoma: extended follow-up of efficacy and safety results from a randomised, controlled, phase 3 trial. Lancet Oncol 2019;20:1370–85. 10.1016/S1470-2045(19)30413-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Motzer RJ, Tannir NM, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med 2018;378:1277–90. 10.1056/NEJMoa1712126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Motzer RJ, Penkov K, Haanen J, et al. Avelumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med 2019;380:1103–15. 10.1056/NEJMoa1816047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rini BI, Plimack ER, Stus V, et al. Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med 2019;380:1116–27. 10.1056/NEJMoa1816714 [DOI] [PubMed] [Google Scholar]
- 7.Rini BI, Powles T, Atkins MB, et al. Atezolizumab plus bevacizumab versus sunitinib in patients with previously untreated metastatic renal cell carcinoma (IMmotion151): a multicentre, open-label, phase 3, randomised controlled trial. Lancet 2019;393:2404–15. 10.1016/S0140-6736(19)30723-8 [DOI] [PubMed] [Google Scholar]
- 8.Ueda K, Suekane S, Kurose H, et al. Prognostic value of PD-1 and PD-L1 expression in patients with metastatic clear cell renal cell carcinoma. Urol Oncol 2018;36:499.e9–499.e16. 10.1016/j.urolonc.2018.07.003 [DOI] [PubMed] [Google Scholar]
- 9.Kahlmeyer A, Stöhr CG, Hartmann A, et al. Expression of PD-1 and CTLA-4 are negative prognostic markers in renal cell carcinoma. J Clin Med 2019;8:743. 10.3390/jcm8050743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iacovelli R, Nolè F, Verri E, et al. Prognostic role of PD-L1 expression in renal cell carcinoma. A systematic review and meta-analysis. Target Oncol 2016;11:143–8. 10.1007/s11523-015-0392-7 [DOI] [PubMed] [Google Scholar]
- 11.Maia MC, Almeida L, Bergerot PG, et al. Relationship of tumor mutational burden (TMB) to immunotherapy response in metastatic renal cell carcinoma (mRCC). JCO 2018;36:662. 10.1200/JCO.2018.36.6_suppl.662 [DOI] [Google Scholar]
- 12.de Velasco G, Miao D, Voss MH, et al. Tumor mutational load and immune parameters across metastatic renal cell carcinoma risk groups. Cancer Immunol Res 2016;4:820–2. 10.1158/2326-6066.CIR-16-0110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alexandrov LB, Nik-Zainal S, Wedge DC, et al. Signatures of mutational processes in human cancer. Nature 2013;500:415–21. 10.1038/nature12477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodriguez-Vida A, Strijbos M, Hutson T. Predictive and prognostic biomarkers of targeted agents and modern immunotherapy in renal cell carcinoma. ESMO Open 2016;1:e000013. 10.1136/esmoopen-2015-000013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seeber A, Klinglmair G, Fritz J, et al. High IDO-1 expression in tumor endothelial cells is associated with response to immunotherapy in metastatic renal cell carcinoma. Cancer Sci 2018;109:1583–91. 10.1111/cas.13560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Derosa L, Hellmann MD, Spaziano M, et al. Negative association of antibiotics on clinical activity of immune checkpoint inhibitors in patients with advanced renal cell and non-small-cell lung cancer. Ann Oncol 2018;29:1437–44. 10.1093/annonc/mdy103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee M-LT, Whitmore GA. Power and sample size for DNA microarray studies. Stat Med 2002;21:3543–70. 10.1002/sim.1335 [DOI] [PubMed] [Google Scholar]
- 18.Dougall WC, Roman Aguilera A, Smyth MJ. Dual targeting of RANKL and PD-1 with a bispecific antibody improves anti-tumor immunity. Clin Transl Immunology 2019;8:e01081. 10.1002/cti2.1081 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.Ahern E, Harjunpää H, O'Donnell JS, et al. Rankl blockade improves efficacy of PD1-PD-L1 blockade or dual PD1-PD-L1 and CTLA4 blockade in mouse models of cancer. Oncoimmunology 2018;7:e1431088. 10.1080/2162402X.2018.1431088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smyth MJ, Yagita H, McArthur GA. Combination anti-CTLA-4 and anti-RANKL in metastatic melanoma. J Clin Oncol 2016;34:e104–6. 10.1200/JCO.2013.51.3572 [DOI] [PubMed] [Google Scholar]
- 21.Bostwick AD, Salama AK, Hanks BA. Rapid complete response of metastatic melanoma in a patient undergoing ipilimumab immunotherapy in the setting of active ulcerative colitis. J Immunother Cancer 2015;3:19. 10.1186/s40425-015-0064-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liede A, Hernandez RK, Wade SW, et al. An observational study of concomitant immunotherapies and denosumab in patients with advanced melanoma or lung cancer. Oncoimmunology 2018;7:e1480301. 10.1080/2162402X.2018.1480301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahern E, Harjunpää H, Barkauskas D, et al. Co-administration of RANKL and CTLA4 antibodies enhances lymphocyte-mediated antitumor immunity in mice. Clin Cancer Res 2017;23:5789–801. 10.1158/1078-0432.CCR-17-0606 [DOI] [PubMed] [Google Scholar]
- 24.Khan IS, Mouchess ML, Zhu M-L, et al. Enhancement of an anti-tumor immune response by transient blockade of central T cell tolerance. J Exp Med 2014;211:761–8. 10.1084/jem.20131889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ming J, Cronin SJF, Penninger JM. Targeting the RANKL/RANK/OPG axis for cancer therapy. Front Oncol 2020;10:1283. 10.3389/fonc.2020.01283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li B, Wang P, Jiao J, et al. Roles of the RANKL-RANK axis in Immunity-Implications for pathogenesis and treatment of bone metastasis. Front Immunol 2022;13:824117. 10.3389/fimmu.2022.824117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pantano F, Rossi E, Iuliani M, et al. Dynamic changes of receptor activator of nuclear factor-κB expression in circulating tumor cells during denosumab predict treatment effectiveness in metastatic breast cancer. Sci Rep 2020;10:1288. 10.1038/s41598-020-58339-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2022-005136supp001.pdf (94.2KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.