Abstract
Objectives
Delirium commonly occurs during hospitalisation and is associated with increased mortality, especially in elderly patients. This study aimed to determine the demographic and clinical characteristics of patients with delirium in the Japanese real-world clinical setting using a nationwide database comprising claims and discharge abstract data.
Design
This was an observational, cross-sectional, retrospective study in hospitalised patients with an incident delirium identified by a diagnosis based on International Classification of Diseases, 10th Revision codes or initiating antipsychotics recommended for delirium treatment in Japan during their hospitalisation.
Setting
Patients from the Medical Data Vision database including more than 400 acute care hospitals in Japan were evaluated from admission to discharge.
Participants
Of the 32 910 227 patients who were included in the database between April 2012 and September 2020, a total of 145 219 patients met the criteria for delirium.
Primary and secondary outcome measures
Demographic and baseline characteristics, comorbidities, clinical profiles and pharmacological treatments were evaluated in patients with delirium.
Results
The mean (SD) patient age was 76.5 (13.8) years. More than half of the patients (n=82 159; 56.6%) were male. The most frequent comorbidities were circulatory system diseases, observed in 81 954 (56.4%) patients. Potentially inappropriate medications (PIMs) with risk of delirium including benzodiazepines and opioids were prescribed to 76 798 (52.9%) patients. Approximately three-fourths of these patients (56 949; 74.2%) were prescribed ≥4 PIMs. The most prescribed treatment for delirium was injectable haloperidol (n=82 490; 56.8%). Mean (SD) length of hospitalisation was 16.0 (12.1) days.
Conclusions
The study results provide comprehensive details of the clinical characteristics of patients with delirium and treatment patterns with antipsychotics in the Japanese acute care setting. In this patient population, the prescription rate of injectable haloperidol and PIMs was high, suggesting the need for improved understanding among healthcare providers about the appropriate management of delirium, which may benefit patients.
Keywords: delirium & cognitive disorders, psychiatry, epidemiology
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This was the first nationwide study that comprehensively assessed the clinical characteristics of patients with delirium in the real-world setting of acute care hospitals in Japan.
Analysis of the nationwide claims and discharge abstract database, using an algorithm adapted to the Japanese clinical setting, enabled identification of a large sample of patients with delirium in acute care hospitals in Japan.
As data were identified from the Medical Data Vision database, which is designed to capture claims and discharge abstracts in Japan and is not for research use, misclassification of the International Classification of Diseases, 10th Revision codes may occur, given that no quality check is performed.
Introduction
Delirium is an acute condition characterised by fluctuating disturbances in attention, awareness and cognition.1 It frequently occurs in hospitalised elderly patients in an acute care setting, especially those in intensive care units (ICUs), and in postoperative care settings.2 3 The prevalence of delirium is reported as 10%–31% among hospitalised patients within 24 hours of admission.4 Among elderly patients, the prevalence is reported as 15%–53% after surgery5 6 and 80% in those admitted to the ICU.5 Previous studies have shown that delirium is associated with prolonged hospital stay and institutionalisation2 7 and increased mortality in non-surgical and surgical patients in general wards, emergency departments and ICUs.7 8 Furthermore, long-term cognitive and functional decline is associated with delirium, often lasting up to a year following hospital discharge.7 9 Consequently, delirium increases economic burden by raising healthcare expenditure and imposing costs related to loss of well-being.3
Despite its high prevalence and poor prognosis, delirium remains unrecognised in a substantial proportion of old patients. In a prospective clinical epidemiological study, even nursing personnel were unable to recognise delirium in up to two-thirds of the hospitalised elderly patients.10 Recent evidence suggests that antipsychotics and multicomponent interventions can notably reduce the incidence of delirium and improve clinical outcomes,11–13 emphasising the need for early intervention and prevention in the hospitalised or postoperative elderly population that is at risk of delirium.14
Antipsychotics are widely used for the treatment of delirium, although no standard clinical pathway for the management of delirium has been established. The Japanese Ministry of Health, Labour and Welfare issued a notification in 2011, permitting the reimbursement of off-label oral and injectable haloperidol, oral perospirone, quetiapine and risperidone for the treatment of delirium, psychomotor agitation and irritability associated with organic diseases.15 In addition, the Japanese Society of General Hospital Psychiatry recommended the use of several antipsychotics in a pharmacotherapy algorithm for delirium.16 However, few studies have quantitatively investigated the use of antipsychotics for the treatment of patients with delirium in real-world clinical practice in Japan.17 18
A limited number of studies have examined the characteristics of patients experiencing delirium based on a medical database.17–25 This is because identification of delirium through a medical database is quite challenging, given the inconsistent and poor documentation of records.26 Moreover, the identification of delirium requires bedside cognitive assessments and application of validated diagnostic tools such as the Confusion Assessment Method27 or the Diagnostic and Statistical Manual of Mental Disorders criteria.1 Therefore, delirium is not routinely evaluated in acute care hospitals,26 28 and the information on delirium diagnosis rarely gets recorded in healthcare utilisation databases (eg, claims data or hospital clinical data repository).
Although several medical database studies in the USA19 and Japan24 have used International Classification of Diseases, 9th Revision (ICD-9) or ICD, 10th Revision (ICD-10) codes to identify patients with a diagnosis of delirium, only around 2% of patients with delirium (postoperative in Japan) could be identified. On the other hand, several medical database studies have employed antipsychotic use to identify patients with delirium.21 23 25 However, either of these criteria, when used exclusively, may be inadequate in obtaining a comprehensive and true picture of patients with delirium in the real-world clinical setting in Japan.
To date, few studies have investigated the overall profile of patients with delirium in the real-world clinical setting in Japan. The present study aimed to assess the demographic characteristics, comorbidities, clinical profiles and treatments in patients with delirium during hospitalisation from a nationwide administrative database of acute care hospitals in Japan, the Medical Data Vision (MDV) database. In this study, delirium was defined using the algorithms that were recommended in the recently published claims-based database studies with slight modifications.22 24
Methods
Study design
This was a retrospective, cross-sectional, observational study using a nationwide administrative database (MDV Co, Tokyo, Japan), with data collected from 1 April 2012 to 30 September 2020. The MDV database contains anonymised administrative data of more than 30 million patients from over 400 hospitals, which cover approximately 24% of all acute care hospitals in Japan. The MDV database includes claims data and discharge abstract data collected from inpatient and outpatient visits.
Patient selection
In this study, patients admitted to general wards and ICUs were included. Patients meeting the prespecified delirium identification algorithm criteria who were hospitalised for surgery or an emergency and those who were discharged, transferred to other hospitals or died after hospitalisation during the study period were included in the analysed data set.
The delirium identification algorithm in this study was based on that recently reported by Kim et al.22 Kim et al proposed an algorithm that defines delirium based on ICD diagnosis codes or antipsychotic use and has a modestly better profile (30% sensitivity; 97% specificity) than existing algorithms such as either ICD diagnosis codes alone or antipsychotic use alone. In this study, patients were identified and included as the study participants based on the following criteria: a confirmed diagnosis of delirium during hospitalisation, coded as F05 per ICD-10 (criterion 1), or prescription of at least one antipsychotic agent (haloperidol, olanzapine, perospirone, quetiapine or risperidone) between the index date (admission date) and the next 7 days (criterion 2). The algorithm was modified to adjust with the clinical setting in Japan. Patients with a minimum stay of 3 days, including at least two antipsychotic-free days, were included in the study.23 This ‘two day washout’ period after hospitalisation allowed the exclusion of patients who already had a prescription of the selected antipsychotic because of pre-existing conditions. Patients who were hospitalised for less than 3 days; who had schizophrenia spectrum disorder (F20–29 codes per ICD-10), bipolar disorder (F30–31 codes per ICD-10) or delirium (F05 code per ICD-10) as ‘admission-precipitating diagnosis’ or ‘comorbidities present on admission’; who were prescribed antipsychotics on the hospitalisation date or the next day; and who were prescribed olanzapine in combination with cisplatin for nausea within 1 week from the index date were excluded from the analyses.
Patients hospitalised multiple times were evaluated only at the first hospitalisation when the inclusion criteria were met. Repeated episodes of delirium in the same patient were not tracked or included in the analysis. The observation period was from the index date (date of hospitalisation) to the end of hospitalisation, defined as discharge, hospital transfer or death of the patient.
Outcomes
The following demographic and baseline characteristics, clinical profiles and comorbidities of patients with delirium were assessed from the MDV database: patients’ baseline characteristics (sex, age, activities of daily living [ADL] score calculated using the Barthel Index,29 cognitive impairment [assessed as ‘present’ if the patient was previously diagnosed with dementia or prescribed antidementia medications or had a low degree of independence]), inpatient departments, comorbidities, type of clinical practice (delirium-associated PIM use [identified based on the Beers Criteria,30 the Guidelines for Medical Treatment and its Safety in the Elderly from the Japan Geriatrics Society Working Group31 and the report from Noshiro et al32], type of surgery [sites or duration of anaesthesia], duration of hospitalisation and ICU stay), hospitalisation information (type of hospitalisation [surgery or emergency hospitalisation], number of beds), prescription pattern for each antipsychotic and patient outcomes (transfer to other hospitals/nursing homes, death). Among the outcomes, age, ADL, cognitive impairment and comorbidities were assessed as the risk (predisposing) factors of delirium. Surgery information, hospitalisation information (surgery or emergency) and PIM use were assessed as triggers (precipitating factors) of delirium.8
Statistical analysis
The aim of this study was descriptive; therefore, no sample size calculations were performed. Data were summarised as mean (SD) or number and frequency (%). All statistical analyses were performed using SAS V.9.4 (SAS Institute).
Sensitivity analysis
As many assumptions were made while creating the delirium identification algorithm, two sensitivity analyses (SAs) were conducted for patients selected in the main analyses to confirm how different assumptions on the analysed populations might have influenced the outcomes. As some patients could have undergone surgery several days after their admission and the criteria used to identify patients to be included in the main analysis do not allow their inclusion, patients who had a prescription of any of the ‘selected’ antipsychotics between the third day of hospitalisation and the day of discharge (or transfer or death) were included in SA1. Furthermore, as some patients may undergo surgery immediately after the emergency admission and have delirium on the next day and the criteria set for the main analysis do not allow their inclusion, patients who had a prescription of the specified antipsychotics between the second and the eighth day of hospitalisation were included in SA2.
Patient and public involvement
Patients were not involved in any phase of this retrospective study, and data were collected from deidentified administrative claims database.
Results
Identification of patients with delirium
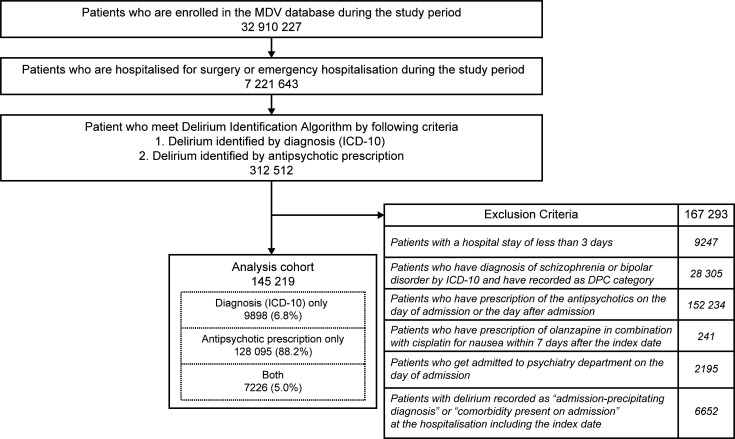
Of the 32 910 227 patients who were included in the MDV database during the study period, 145 219 were identified as having delirium (figure 1). Among patients who were hospitalised for surgery or an emergency (n=7 221 643), 2.0% were identified as having delirium. Overall, 9898 (6.8%) patients who met the delirium identification algorithm criteria were diagnosed with delirium based on ICD-10 codes and did not receive any of the selected antipsychotic treatments during their hospitalisation; 128 095 (88.2%) patients were identified because they had been prescribed any of the selected antipsychotics, and 7226 (5.0%) patients who met the delirium identification algorithm criteria had both a diagnosis of delirium and an antipsychotic prescription (figure 1). Most (n=14 801; 86.4%) of the 17 124 patients with an ICD-10-coded diagnosis had ‘delirium’ (code F05.9), followed by ‘nocturnal delirium’ (code F05.9), ‘delirium superimposed on dementia’ (code F05.1) and ‘delirium not superimposed on dementia’ (code F05.0; online supplemental table 1).
Figure 1.
Patient selection flow chart. DPC, diagnosis procedure combination; ICD-10, International Classification of Diseases, 10th Revision; MDV, Medical Data Vision.
bmjopen-2021-060630supp001.pdf (377.9KB, pdf)
Patient demographics and baseline characteristics
Mean (SD) patient age was 76.5 (13.8) years, and approximately 65% of patients were ≥75 years of age; more than 50% (n=82 159) of patients were male. Approximately half (n=76 422; 52.6%) of the patients with delirium were categorised as ‘dependent (need someone’s help)’ based on the Barthel Index score (table 1). Cognitive impairment was noted in 40 376 (27.8%) patients (table 1; online supplemental table 2). Circulatory system diseases were the most common comorbidity, observed in 81 954 (56.4%) patients, followed by endocrine, nutritional and metabolic diseases (n=59 955; 41.3%) and digestive system diseases (n=59 691; 41.1%; table 1; online supplemental table 3). These outcomes were assessed as the risk (predisposing) factors of delirium.
Table 1.
Patient demographic and baseline characteristics
| Patients, n (%) | ||
| Patients (n) | 145 219 | |
| Age (years) | Mean (SD) | 76.5 (13.8) |
| ≤64 | 22 168 (15.3) | |
| 65–74 | 28 371 (19.5) | |
| 75–84 | 49 739 (34.3) | |
| ≥85 | 44 941 (30.9) | |
| Sex | Male | 82 159 (56.6) |
| Female | 63 060 (43.4) | |
| ADL score (points)* | Dependent group (0–59) | 76 422 (52.6) |
| Independent group (60–100) | 66 381 (45.7) | |
| Unknown | 2416 (1.7) | |
| Cognitive impairment† | Yes | 40 376 (27.8) |
| No | 104 843 (72.2) | |
| Inpatient department | Surgery | 28 656 (19.7) |
| Internal medicine | 28 232 (19.4) | |
| Gastroenterology | 15 445 (10.6) | |
| Cardiology | 12 337 (8.5) | |
| Orthopaedics | 11 302 (7.8) | |
| Neurosurgery | 8144 (5.6) | |
| Urology | 7031 (4.8) | |
| Cardiovascular surgery | 6042 (4.2) | |
| Respiratory medicine | 5506 (3.8) | |
| Gastrointestinal surgery | 4093 (2.8) | |
| Emergency medicine | 3414 (2.4) | |
| Neurology | 3008 (2.1) | |
| Others | 11 573 (8.0) | |
| Comorbidities (ICD-10 major category)‡ |
Circulatory system diseases (I00–I99) | 81 954 (56.4) |
| Endocrine, nutritional and metabolic diseases (E00–E90) | 59 955 (41.3) | |
| Digestive system diseases (K00–K93) | 59 691 (41.1) | |
| Malignant neoplasms (C00–C97) | 41 710 (28.7) | |
| Respiratory system diseases (J00–J99) | 36 958 (25.4) | |
*Barthel Index was used for evaluation.
†Cognitive impairment was assessed as ‘present’ if the patient was previously diagnosed with dementia or prescribed antidementia drugs or had a low degree of independence.
‡Top 5 major ICD-10 categories are presented.
ADL, activities of daily living; ICD-10, International Classification of Diseases, 10th Revision.
Clinical practice
Around half (n=85 492; 58.9%) of the patients with delirium underwent any surgery, of whom approximately one-third (n=28 557) were anaesthetised for more than 2 hours (table 2). There was a wide distribution of surgical sites, with the abdomen being the most common site (n=38 898; 26.8%; online supplemental table 4). Mean (SD) duration of hospitalisation was 16.0 (12.1) days; 55 709 (38.4%) patients were hospitalised for 1–2 weeks (table 2). Overall, 33 718 (23.2%) patients were admitted to the ICU for a mean (SD) of 3.4 (3.1) days, of whom 4379 (3.0%) spent at least 7 days in the ICU (table 2). PIMs were prescribed to 76 798 (52.9%) patients, including benzodiazepines in 31 324 (21.6%) patients and opioids in 29 268 (20.2%) patients. Approximately three-fourths (n=56 949; 74.2%) of these patients were prescribed ≥4 PIMs. Multiple classes of PIMs were used by 38.6% of patients to whom PIMs were prescribed (table 2). These factors were assessed as triggers (precipitating factors) of delirium.
Table 2.
Clinical practice
| Patients, n (%) | ||
| Patients (n) | 145 219 | |
| Prescription of PIM | Yes (any type of PIM) | 76 798 (52.9) |
| Antidepressants | 299 (0.2) | |
| Anticholinergic drugs | 163 (0.1) | |
| Benzodiazepines | 31 324 (21.6) | |
| Non-benzodiazepines | 10 582 (7.3) | |
| Corticosteroids | 16 879 (11.6) | |
| H1 receptor antagonists | 10 283 (7.1) | |
| H2 receptor antagonists | 17 360 (12.0) | |
| Opioids | 29 268 (20.2) | |
| Number of PIMs (drugs) | 76 798 (100.0) | |
| 1 | 5268 (6.9) | |
| 2 | 7232 (9.4) | |
| 3 | 7349 (9.6) | |
| ≥4 | 56 949 (74.2) | |
| Number of PIMs (classes) | 76 798 (100.0) | |
| 1 | 47 128 (61.4) | |
| 2 | 21 637 (28.2) | |
| 3 | 6561 (8.5) | |
| ≥4 | 1472 (1.9) | |
| Surgery | Yes | 85 492 (58.9) |
| Anaesthesia type/duration | 85 492 (100.0) | |
| Surgery+no anaesthesia/local anaesthesia/light general anaesthesia | 35 048 (41.0) | |
| Surgery+general anaesthesia (<2 hours) | 21 887 (25.6) | |
| Surgery+general anaesthesia (≥2 hours) | 28 557 (33.4) | |
| Duration of hospitalisation (days) | Mean (SD) | 16.0 (12.1) |
| ≤1 week | 22 542 (15.5) | |
| >1 to ≤2 weeks | 55 709 (38.4) | |
| >2 to ≤3 weeks | 38 342 (26.4) | |
| >3 to ≤4 weeks | 17 004 (11.7) | |
| >4 to ≤12 weeks | 11 046 (7.6) | |
| >12 weeks | 576 (0.4) | |
| Use of ICU | Yes | 33 718 (23.2) |
| Duration of ICU (days) | Mean (SD) | 3.4 (3.1) |
| 1 day | 12 218 (8.4) | |
| 2 days | 5970 (4.1) | |
| 3 days | 4247 (2.9) | |
| 4 days | 3104 (2.1) | |
| 5 days | 2192 (1.5) | |
| 6 days | 1608 (1.1) | |
| ≥7 days | 4379 (3.0) | |
ICU, intensive care unit; PIM, potentially inappropriate medication.
Treatment for delirium
Injectable haloperidol was the most prescribed antipsychotic (n=82 490; 56.8%) for the treatment of delirium, followed by risperidone solution (n=34 282; 23.6%), quetiapine tablet (n=19 830; 13.7%), risperidone orodispersible tablet (n=7645; 5.3%) and risperidone tablet (n=4958; 3.4%; table 3). The mean (SD) duration of these antipsychotic prescriptions was 5.4 (8.1) days (table 3).
Table 3.
Antipsychotics used for treating delirium
| Patients, n (%) | |||
| Patients (n) | 145 219 | ||
| Antipsychotics used for delirium | Yes | 135 321 (93.2) | |
| Type of drug formulation | Haloperidol | INJ | 82 490 (56.8) |
| TAB | 1913 (1.3) | ||
| FGR | 192 (0.1) | ||
| SOL | 13 (0.0) | ||
| Risperidone | SOL | 34 282 (23.6) | |
| ODT | 7645 (5.3) | ||
| TAB | 4958 (3.4) | ||
| FGR | 257 (0.2) | ||
| INJ | 6 (0.0) | ||
| Quetiapine | TAB | 19 830 (13.7) | |
| FGR | 652 (0.4) | ||
| SRT | 20 (0.0) | ||
| Olanzapine | TAB | 2262 (1.6) | |
| ODT | 915 (0.6) | ||
| FGR | 156 (0.1) | ||
| INJ | 11 (0.0) | ||
| Perospirone | TAB | 2210 (1.5) | |
| Duration of prescription (days) | Mean (SD) | 5.4 (8.1) | |
FGR, fine granule; INJ, injectable; ODT, orodispersible tablet; SOL, solution; SRT, sustained release tablet; TAB, tablet.
Hospitalisations and patient outcome
Assessment of patients with delirium by hospital department showed that the departments where at least 5% of patients experienced delirium were surgery (n=28 656; 19.7%), internal medicine (n=28 232; 19.4%), gastroenterology (n=15 445; 10.6%), cardiology (n=12 337; 8.5%), orthopaedics (n=11 302; 7.8%) and neurosurgery (n=8144; 5.6%; table 1; online supplemental table 4). In general, 52 766 (36.3%) patients with delirium were hospitalised for planned elective surgery, whereas 59 727 (41.1%) patients were hospitalised due to an emergency (without subsequent surgery) and 32 726 (22.5%) patients were hospitalised due to an emergency and underwent surgery (online supplemental table 4). A total of 15 556 (10.7%) patients died while in hospital, and 22 081 (15.2%) were transferred to other hospitals or clinics (table 4).
Table 4.
Patient outcome—transfer to other hospitals/nursing homes and death
| Patients, n (%) | ||
| Patients (n) | 145 219 | |
| Transfer to other hospitals/nursing homes | Yes | 32 651 (22.5) |
| Transfer to other hospitals or clinics | 22 081 (15.2) | |
| Admission to social welfare facilities or fee-based homes for the elderly, etc | 5070 (3.5) | |
| Admission to facilities covered by public aid providing long-term care to the elderly | 3017 (2.1) | |
| Admission to long-term care health facilities | 2472 (1.7) | |
| Nursing home | 11 (0.0) | |
| Death | Yes | 15 556 (10.7) |
| No | 129 637 (89.3) | |
Sensitivity analysis
The results of the SAs identified 184 817 patients with delirium in SA1 and 213 844 in SA2 (online supplemental figure 1). Patients’ mean (SD) age was 76.1 (13.8) years in SA1 and 76.3 (14.1) years in SA2. A total of 96 591 (52.3%) patients in SA1 and 113 005 (52.8%) patients in SA2 were classified as dependent (online supplemental table 5).
The proportion of patients prescribed one or more antipsychotics to treat their delirium was 95.5% in SA1 and 95.4% in SA2. The proportion of injectable haloperidol prescriptions was 58.1% in SA1 and 60.1% in SA2, while the proportion of prescriptions for risperidone solution was 24.8% in SA1 and 23.5% in SA2 and that for risperidone tablets was 4.0% in SA1 and 3.5% in SA2 (online supplemental table 5).
Discussion
The present study was the first nationwide database study that assessed the clinical characteristics of patients with delirium in acute care hospitals in Japan. To identify patients with delirium from the hospital database, the study used the delirium identification algorithm which consists of diagnoses based on ICD-10 codes and prescriptions of antipsychotics frequently used in the treatment of delirium.22 The prevalence of delirium obtained in our study was 2.0% among patients who were hospitalised for surgery or an emergency, which was lower than the incidence of new delirium per admission (3%–29%) reported in a systematic review of the literature.4 The low prevalence of delirium might be due to the sensitivity of the algorithm used in our study. A potential explanation is that physicians are not aware of delirium, thereby leading to its inappropriate management. Another possible explanation is that physicians do not proactively record a diagnosis of delirium in claims because there is no approved drug for delirium treatment or prevention in Japan, except for tiapride that is approved for the management of delirium after stroke.
In our study, about half of the patients (n=85 492; 58.9%) underwent surgery during their hospital stay, and delirium was also identified among non-surgical patients in general medical wards such as internal medicine, gastroenterology and cardiology. A systematic literature review reported the prevalence of delirium among patients admitted to general medical and geriatric wards as 18%–35%.8 Our findings revealed the occurrence of delirium in broad clinical departments in Japanese acute care hospitals, suggesting the need for physicians and nurses in these departments to understand the diagnosis and management of patients with delirium.
Drug classes such as benzodiazepines, opioids and H2 blockers were selected as PIMs, which are reported to be associated with the onset of delirium in guidelines30 31 and several studies.32–36 In our study, more than half (52.9%) of the patients were prescribed a PIM of any type; approximately one-fifth of the patients were prescribed either benzodiazepines or opioids (21.6% and 20.2%, respectively). Benzodiazepines and opioids are associated with an increased risk of delirium in medical and surgical patients.34 In a single-centre study in Canada, the risk was more than doubled within 28 days of hospitalisation in patients with cancer who were receiving benzodiazepines (>2 mg/day) and opioids (>90 mg/day).37 It should be noted that Japan is one of the countries with a high rate of consumption of benzodiazepine-type sedative hypnotics.38 In addition, opioids are necessary to control severe pain, and pain is also known to be associated with a risk of delirium,16 suggesting the importance of delirium control in combination with pain control. PIMs also include several drugs with anticholinergic activities, such as antihistamines and antidepressants.30 Use of anticholinergic drugs is associated with an increased risk of delirium.39 40 Thus, physicians should avoid unnecessarily prescribing drugs with anticholinergic effects considering the risk of delirium onset. Furthermore, at least four PIMs were prescribed in 74.2% of patients with delirium in the present study. Polypharmacy with ≥3 drugs is reported to increase the risk of delirium by 2.9 times in elderly patients during hospitalisation.41 As drug interactions are a concern regarding PIMs in patients with polypharmacy, potential drug interactions in addition to the number of PIMs used should be carefully considered especially in patients with polypharmacy. The frequent use of PIMs that increase the risk of delirium in the real world, particularly in elderly patients, reaffirms the need for a better understanding of the benefit-risk profile of such medications.
In our study, injectable haloperidol was the most frequently prescribed (56.8%) antipsychotic, followed by risperidone solution (23.6%) and quetiapine tablets (13.7%) in patients with delirium. The outcomes are similar to those from a recent database study in Japan, where haloperidol infusion was the most frequently used treatment in postoperative patients with delirium.17 These results are also consistent with those of a questionnaire-based cross-sectional study in which more than two-thirds of Japanese experts recommended intravenous haloperidol as the initial drug (if an intravenous line was placed during hospitalisation) and atypical oral antipsychotics such as risperidone or quetiapine as initial oral drugs for hyperactive delirium.42 Risperidone solution and olanzapine orodispersible tablets could be useful for patients who have difficulties in taking medicines.16 In our study, a relatively high proportion of patients were prescribed risperidone solution (23.6%); however, only 0.6% were prescribed olanzapine orodispersible tablets. The low proportion of olanzapine prescription could be due to the long half-life of olanzapine and its contraindication in patients with diabetes in Japan.16 Overall, our findings suggest that injectable haloperidol is the major treatment modality for delirium in an acute care setting likely because it can be used as needed for the treatment of delirium in such a setting. Unlike psychiatrists, the majority of physicians who treat patients with delirium are likely to be unfamiliar with use of atypical antipsychotics. However, in a broader clinical context, the risk of death in the elderly was reported to be 2.26-fold higher with haloperidol versus olanzapine,43 and the likelihood of overall survival was 1.73-fold higher with placebo in a randomised controlled trial.44 Moreover, the incidence of adverse events, particularly extrapyramidal symptoms, is reportedly higher with haloperidol versus risperidone, although their efficacy is reportedly similar.45 46 While antipsychotics are frequently used for treating delirium in real-world clinical settings, physicians should note that non-pharmacological treatment is the first-line therapy for delirium and that antipsychotic use should be considered only if the non-pharmacological treatment is ineffective and patients are at risk of injuring themselves and others. For example, the National Institute for Health and Care Excellence delirium guidelines state that short-term haloperidol may be given when an individual with delirium is distressed or considered to be at risk to themselves or others and if verbal and non-verbal de-escalation methods have not shown effect.47 The Beers Criteria by the American Geriatrics Society recommend that PIMs including antipsychotics be avoided in older adults at high risk of delirium owing to the risk of inducing or worsening the condition.30 Moreover, olanzapine has anticholinergic effects, and its use in managing delirium is controversial because some case reports have shown that its use may be associated with delirium onset.48 49 Therefore, it is important for healthcare providers to understand the appropriate non-pharmacological management of delirium.
The greatest strength of this study is the large size of the MDV database, which enabled the identification of a large number of patients with delirium. The use of our algorithm optimised for the Japanese clinical setting led to an increased number of patients being retrieved from hospital databases, thus highlighting the utility of this algorithm in real-world scenarios. More importantly, outcomes of the SAs, which considered different treatment time frames in determining index, were consistent with those of the main analysis, reinforcing the robustness of our study results. The prevalence of delirium obtained by identifying patients using an ICD-coded diagnosis was only 0.2% among patients who were hospitalised for surgery or an emergency in our study, which is similar to that reported in previous studies in Japan.18 24 However, this low prevalence may not be a true reflection of the occurrence of delirium in the real world, as observed in a prospective study that compared the sensitivity and specificity of various delirium identification algorithms.22 According to Sakakibara et al, delirium is recorded on the claims receipt only for patients with severe delirium requiring more medical resources, but not for those with mild-to-moderate delirium.24 Our results confirm that the majority of Japanese patients with delirium can be identified from a Japanese claims database based on prescription of an antipsychotic during their hospital stay; 88.2% of patients with delirium were identified based on an antipsychotic prescription. A recent study employing a Japanese national inpatient database used the daily nursing necessity score (dangerous behaviour or misunderstanding of nursing instructions) as the criterion of delirium, but reported a prevalence of delirium of approximately 1% (n=21 182) among 2 070 000 postoperative patients.17 The results of the present study show the feasibility of using administrative databases for identifying patients with delirium in an acute care hospital setting in Japan.
This study has several limitations. First, the data were extracted from the MDV database, which is designed primarily for insurance purposes and not for research; therefore, no quality checks for data are performed and there is a likelihood of misclassification of ICD-10 coding. Second, as the data of patients transferred to other hospitals were not registered in this database, patients who were moved to or hospitalised in a different hospital after the index hospitalisation could not be identified. This could have led to multiple hospitalisations of the same high-risk patients, with multiple episodes of delirium at different times being identified as separate events and possibly increasing the number of identified cases. Third, the number of prescribed antipsychotics may be inflated because some patients with psychotic disorders may have been included from the database during analysis although the present study excluded patients with schizophrenia or bipolar disease. Lastly, the sensitivity and specificity of the modified delirium identification algorithm used in this study have not yet been validated in Japan. The recent addition of a medical fee for the care of high-risk patients with delirium in the medical reimbursement revision of 2020 in Japan may increase the accuracy of identification of patients with delirium from the medical database. For future research, the delirium identification algorithm used in our study needs to be validated.
In conclusion, the results of the present study provide comprehensive details of the clinical characteristics of patients with delirium and treatment patterns with antipsychotics in the Japanese acute care setting. The results reinforce the need to consider the risk of delirium in hospitals, especially in high-risk patients, and provide useful information for healthcare professionals to understand the clinical profile of patients who are likely to experience delirium when hospitalised. The study reveals two important findings in this patient population: (1) the high prescription rate of injectable haloperidol and (2) the frequent use of PIMs in patients with delirium. Thus, there is a need for improved understanding among healthcare providers about appropriate management of delirium in an acute care setting, which may benefit patients.
Supplementary Material
Acknowledgments
The authors thank Andrea Rossi and Deepali Garg of Cactus Life Sciences (part of Cactus Communications) for medical writing of the manuscript and editorial assistance, which was funded by MSD KK, Tokyo, Japan, and Shinya Miura, Hideaki Ogawa and Shinichiro Suzuki of CMIC Co, Ltd, for medical writing of the protocol and data analysis under the guidance and approval of MSD KK, Tokyo, Japan.
Footnotes
Contributors: SO, HS, KT, ZPQ, ST, AO and YO conceptualised the study. NU, MI, KO and SO conducted the study designing and data analysis planning. HS, KT, ZPQ and ST contributed to the study designing. KT, AO and YO provided advice on study design and contributed to the interpretation of the findings from the viewpoint of the clinical scientist, the physician and the epidemiologist, respectively. All authors contributed to interpretation of data and approved the final version of the manuscript. NU and SO are guarantors and accept full responsibility for the work.
Funding: This work was supported by MSD KK, Tokyo, Japan. The funder of the study was involved in the development of the study design, data analysis, data interpretation, writing of the manuscript, and the decision to submit the manuscript for publication. All authors had full access to the study results.
Competing interests: NU, MI, KO, HS, KT, ST and SO are employees of MSD KK, Tokyo, Japan, a subsidiary of Merck & Co Inc, Rahway, New Jersey, USA, and may own stock and/or hold stock options in Merck & Co Inc, Rahway, New Jersey, USA. ZPQ is an employee of Merck Sharp & Dohme Corp, a subsidiary of Merck & Co Inc, Kenilworth, New Jersey, USA, and may own stock and/or hold stock options in Merck & Co Inc, Kenilworth, New Jersey, USA. AO and YO have received funding from MSD KK, Tokyo, Japan for research consulting.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. The Medical Data Vision database analysed in this study is not publicly accessible, and the data cannot be shared with external researchers according to the contract with Medical Data Vision.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study used deidentified data from the MDV database and ethics approval was not required, in line with the Ethical Guidelines for Epidemiological Research from the MHLW, Japan. Therefore, no ethics or institution review board approval was obtained.
References
- 1.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Fifth Edition. Washington, DC: American Psychiatric Association Publishing, 2013: 596–7. [Google Scholar]
- 2.Oh ES, Fong TG, Hshieh TT, et al. Delirium in older persons: advances in diagnosis and treatment. JAMA 2017;318:1161–74. 10.1001/jama.2017.12067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pezzullo L, Streatfeild J, Hickson J, et al. Economic impact of delirium in Australia: a cost of illness study. BMJ Open 2019;9:e027514. 10.1136/bmjopen-2018-027514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing 2006;35:350–64. 10.1093/ageing/afl005 [DOI] [PubMed] [Google Scholar]
- 5.Fricchione GL, Nejad SH, Esses JA, et al. Postoperative delirium. Am J Psychiatry 2008;165:803–12. 10.1176/appi.ajp.2008.08020181 [DOI] [PubMed] [Google Scholar]
- 6.Marcantonio ER. Postoperative delirium: a 76-year-old woman with delirium following surgery. JAMA 2012;308:73–81. 10.1001/jama.2012.6857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hshieh TT, Inouye SK, Oh ES. Delirium in the elderly. Clin Geriatr Med 2020;36:183–99. 10.1016/j.cger.2019.11.001 [DOI] [PubMed] [Google Scholar]
- 8.Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet 2014;383:911–22. 10.1016/S0140-6736(13)60688-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldberg TE, Chen C, Wang Y, et al. Association of delirium with long-term cognitive decline: a meta-analysis. JAMA Neurol 2020;77:1373–81. 10.1001/jamaneurol.2020.2273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inouye SK, Foreman MD, Mion LC, et al. Nurses' recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med 2001;161:2467–73. 10.1001/archinte.161.20.2467 [DOI] [PubMed] [Google Scholar]
- 11.Chen CC-H, Li H-C, Liang J-T, et al. Effect of a modified Hospital Elder Life Program on delirium and length of hospital stay in patients undergoing abdominal surgery: a cluster randomized clinical trial. JAMA Surg 2017;152:827–34. 10.1001/jamasurg.2017.1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Janssen TL, Alberts AR, Hooft L, et al. Prevention of postoperative delirium in elderly patients planned for elective surgery: systematic review and meta-analysis. Clin Interv Aging 2019;14:1095–117. 10.2147/CIA.S201323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogawa A, Okumura Y, Fujisawa D, et al. Quality of care in hospitalized cancer patients before and after implementation of a systematic prevention program for delirium: the DELTA exploratory trial. Support Care Cancer 2019;27:557–65. 10.1007/s00520-018-4341-8 [DOI] [PubMed] [Google Scholar]
- 14.Whalin MK, Kreuzer M, Halenda KM, et al. Missed opportunities for intervention in a patient with prolonged postoperative delirium. Clin Ther 2015;37:2706–10. 10.1016/j.clinthera.2015.09.012 [DOI] [PubMed] [Google Scholar]
- 15.About insurance medical treatment related to off-label use of pharmaceutical products, 2011. Available: https://www.hospital.or.jp/pdf/14_20110928_01.pdf [Accessed 06 Jun 2022].
- 16.Clinical guideline for the treatment of delirium . Japanese Society of General Hospital psychiatry practice guidelines 1. 2nd edition. Tokyo, Japan: Seiwa Shoten Publishers. PP: 1-32 & PP85-111. [Google Scholar]
- 17.Noda Y, Tarasawa K, Fushimi K, et al. Drug treatment for patients with postoperative delirium and consultation-liaison psychiatry in Japan: a retrospective observational study of a nationwide Hospital claims database. ACE 2021;3:116–26. 10.37737/ace.3.4_116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ota K, Nakamura M, Makiuchi T, et al. Surveillance of antipsychotic drugs use in elderly patients with postoperative delirium (Japanese). Proceedings of the The Annual Meeting of the Pharmaceutical Society of Japan. Annual meeting of the Pharmaceutical Society of Japan, 2011. [Google Scholar]
- 19.McCoy TH, Snapper L, Stern TA, et al. Underreporting of delirium in statewide claims data: implications for clinical care and predictive modeling. Psychosomatics 2016;57:480–8. 10.1016/j.psym.2016.06.001 [DOI] [PubMed] [Google Scholar]
- 20.Pal N, Abernathy JH 3rd, Taylor MA, et al. Dexmedetomidine, delirium, and adverse outcomes: analysis of The Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann Thorac Surg 2021;112:1886–92. 10.1016/j.athoracsur.2021.03.098 [DOI] [PubMed] [Google Scholar]
- 21.Ahn EJ, Kim HJ, Kim KW, et al. Comparison of general anaesthesia and regional anaesthesia in terms of mortality and complications in elderly patients with hip fracture: a nationwide population-based study. BMJ Open 2019;9:e029245. 10.1136/bmjopen-2019-029245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim DH, Lee J, Kim CA, et al. Evaluation of algorithms to identify delirium in administrative claims and drug utilization database. Pharmacoepidemiol Drug Saf 2017;26:945–53. 10.1002/pds.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park Y, Bateman BT, Kim DH, et al. Use of haloperidol versus atypical antipsychotics and risk of in-hospital death in patients with acute myocardial infarction: cohort study. BMJ 2018;360:k1218. 10.1136/bmj.k1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sakakibara Y, Ochibe T, Amari S, et al. Study on the risk factors for postoperative delirium using the National Health Insurance Claims Database in Japan. Iryo Yakugaku 2019;45:195–207. 10.5649/jjphcs.45.195 [DOI] [Google Scholar]
- 25.Zimmerman KM, Paquin AM, Rudolph JL. Antipsychotic prescription to identify delirium: results from two cohorts. Clin Pharmacol 2017;9:113–7. 10.2147/CPAA.S138441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hope C, Estrada N, Weir C, et al. Documentation of delirium in the Va electronic health record. BMC Res Notes 2014;7:208. 10.1186/1756-0500-7-208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990;113:941–8. 10.7326/0003-4819-113-12-941 [DOI] [PubMed] [Google Scholar]
- 28.Johnson JC, Kerse NM, Gottlieb G, et al. Prospective versus retrospective methods of identifying patients with delirium. J Am Geriatr Soc 1992;40:316–9. 10.1111/j.1532-5415.1992.tb02128.x [DOI] [PubMed] [Google Scholar]
- 29.Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J 1965;14:61–5. [PubMed] [Google Scholar]
- 30.By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel . American Geriatrics Society 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2019;67:674–94. 10.1111/jgs.15767 [DOI] [PubMed] [Google Scholar]
- 31.Kojima T, Mizukami K, Tomita N, et al. Screening Tool for Older Persons' Appropriate Prescriptions for Japanese: Report of the Japan Geriatrics Society Working Group on "Guidelines for medical treatment and its safety in the elderly". Geriatr Gerontol Int 2016;16:983–1001. 10.1111/ggi.12890 [DOI] [PubMed] [Google Scholar]
- 32.Noshiro Y, Imai T, Sakai M, et al. Relationship between the onset of delirium during hospitalization and the use of high-risk drugs for delirium. Med J Matsue City Hosp 2018;1. [Google Scholar]
- 33.Ahmed S, Leurent B, Sampson EL. Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Ageing 2014;43:326–33. 10.1093/ageing/afu022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Inouye SK. Delirium in older persons. N Engl J Med 2006;354:1157–65. 10.1056/NEJMra052321 [DOI] [PubMed] [Google Scholar]
- 35.Fujii S, Tanimukai H, Kashiwagi Y. Comparison and analysis of delirium induced by histamine h(2) receptor antagonists and proton pump inhibitors in cancer patients. Case Rep Oncol 2012;5:409–12. 10.1159/000341873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing 2011;40:23–9. 10.1093/ageing/afq140 [DOI] [PubMed] [Google Scholar]
- 37.Gaudreau J-D, Gagnon P, Harel F, et al. Psychoactive medications and risk of delirium in hospitalized cancer patients. J Clin Oncol 2005;23:6712–8. 10.1200/JCO.2005.05.140 [DOI] [PubMed] [Google Scholar]
- 38.International Narcotics Control Board, Vienna International Centre, Vienna, Austria . International Narcotics Control Board. Availability of internationally controlled drugs: ensuring adequate access for medical and scientific purposes, 2015. Available: https://www.incb.org/documents/Publications/AnnualReports/AR2015/English/Supplement-AR15_availability_English.pdf [Accessed 06 Jun 2022].
- 39.Rudolph JL, Salow MJ, Angelini MC, et al. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med 2008;168:508–13. 10.1001/archinternmed.2007.106 [DOI] [PubMed] [Google Scholar]
- 40.Egberts A, Moreno-Gonzalez R, Alan H, et al. Anticholinergic drug burden and delirium: a systematic review. J Am Med Dir Assoc 2021;22:65–73. 10.1016/j.jamda.2020.04.019 [DOI] [PubMed] [Google Scholar]
- 41.Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. predictive model and interrelationship with baseline vulnerability. JAMA 1996;275:852–7. [PubMed] [Google Scholar]
- 42.Okumura Y, Hatta K, Wada K, et al. Expert opinions on the first-line pharmacological treatment for delirium in Japan: a conjoint analysis. Int Psychogeriatr 2016;28:1041–50. 10.1017/S1041610215002446 [DOI] [PubMed] [Google Scholar]
- 43.Hollis J, Grayson D, Forrester L, et al. Antipsychotic medication dispensing and risk of death in veterans and war widows 65 years and older. Am J Geriatr Psychiatry 2007;15:932–41. 10.1097/JGP.0b013e31813547ca [DOI] [PubMed] [Google Scholar]
- 44.Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med 2017;177:34–42. 10.1001/jamainternmed.2016.7491 [DOI] [PubMed] [Google Scholar]
- 45.Boettger S, Jenewein J, Breitbart W. Haloperidol, risperidone, olanzapine and aripiprazole in the management of delirium: a comparison of efficacy, safety, and side effects. Palliat Support Care 2015;13:1079–85. 10.1017/S1478951514001059 [DOI] [PubMed] [Google Scholar]
- 46.Miyaji S, Yamamoto K, Hoshino S, et al. Comparison of the risk of adverse events between risperidone and haloperidol in delirium patients. Psychiatry Clin Neurosci 2007;61:275–82. 10.1111/j.1440-1819.2007.01655.x [DOI] [PubMed] [Google Scholar]
- 47.The National Institute for Health and Care Excellence (NICE) . Delirium: prevention, diagnosis and management. London, 2019. [Google Scholar]
- 48.Muench J, Hamer AM. Adverse effects of antipsychotic medications. Am Fam Physician 2010;81:617–22. [PubMed] [Google Scholar]
- 49.Lim CJ, Trevino C, Tampi RR. Can olanzapine cause delirium in the elderly? Ann Pharmacother 2006;40:135–8. ‒. 10.1345/aph.1G318 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-060630supp001.pdf (377.9KB, pdf)
Data Availability Statement
No data are available. The Medical Data Vision database analysed in this study is not publicly accessible, and the data cannot be shared with external researchers according to the contract with Medical Data Vision.