Abstract
Alzheimer’s disease (AD) is a progressive neurodegenerative disease with phenotypic changes closely associated with both genetic variants and imaging pathology. Brain imaging biomarker genomics has been developed in recent years to reveal potential AD pathological mechanisms and provide early diagnoses. This technique integrates multimodal imaging phenotypes with genetic data in a noninvasive and high-throughput manner. In this review, we summarize the basic analytical framework of brain imaging biomarker genomics and elucidate two main implementation scenarios of this technique in AD studies: (1) exploring novel biomarkers and seeking mutual interpretability and (2) providing a diagnosis and prognosis for AD with combined use of machine learning methods and brain imaging biomarker genomics. Importantly, we highlight the necessity of brain imaging biomarker genomics, discuss the strengths and limitations of current methods, and propose directions for development of this research field.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40035-022-00315-z.
Keywords: Imaging biomarker genomics, Alzheimer’s disease, Evolving technologies, Implementation
Background
Alzheimer’s disease (AD), as the most common form of dementia, is an irreversible neurodegenerative disease. Epidemiological investigations have reported that about 55 million people worldwide live with AD and other types of dementia today [1]. The number is expected to reach 78 million by 2030 (World Alzheimer Report 2021, www.alz.co.uk). The primary clinical manifestations of AD include progressive impairments in memory and other cognitive functions, accompanied by several pathophysiological changes, such as amyloid deposition and neurofibrillary tangle formation. However, the aetiology and pathogenesis leading to heterogeneity in these manifestations among AD patients remain unclear. In addition, no effective therapeutic strategies are available for AD [2]. High-throughput imaging and genomics studies can provide valid information on AD pathology, and gain insights into the early detection and treatment of AD patients, and thus have attracted much attention recently.
Genomic studies have been developed over three decades [3–5]. In 1984, Glenner et al. [6] first isolated amyloid-β (Aβ) peptide from plaques in AD patients, and this peptide was shown to be generated from the amyloid precursor protein (APP) through its sequential cleavage by two enzymes: β-secretase and γ-secretase [3]. This finding was later confirmed by genetic mutations in APP in 1991 [7] and presenilins (PSEN1 and PSEN2) in 1995 [8, 9]. The above genomic studies support an evident molecular mechanism underlying AD, resulting in the amyloid hypothesis. Additionally, the apolipoprotein E (APOE) ɛ4 allele has been reported to be associated with AD risk [10]. APOE can bind to Aβ, which influences the clearance of soluble Aβ and Aβ aggregation [11, 12], and regulates Aβ metabolism [13]. Notably, APOE ɛ4 binds more rapidly than APOE ɛ3, resulting in accelerated formation of fibrils [14]. Furthermore, with the development of high-throughput sequencing technology, genome-wide association studies (GWAS) have identified thousands of risk variants related to complex diseases and traits, including AD [15–34]. These studies have improved the understanding of genetic complexity and provided insights into the molecular pathways of AD pathogenesis. However, significant results are not only dependent on sufficiently large sample sizes but also require further analysis of gene-to-disease specificity.
Alternatively, neuroimaging technologies [35, 36] such as structural magnetic resonance imaging (sMRI), functional MRI (fMRI), diffusion tensor imaging (DTI), and positron emission tomography (PET), enable noninvasive detection of brain degeneration from the perspective of brain structure and function. SMRI can provide accurate in vivo quantification of specific regions with cortical and subcortical grey matter (GM) atrophy and white matter (WM) lesions associated with AD pathology, even at the mild cognitive impairment (MCI) stage [37, 38]. DTI is another MRI technique that is sensitive to translational motion of water molecules throughout the brain, providing quantification of WM tissue microstructure and visualization of WM tract abnormalities in AD patients. FMRI can measure brain activity by detecting associated changes in blood flow when no task is being performed, and task fMRI focuses on activity activation. Moreover, PET scans can demonstrate characteristic patterns of amyloid load, tau burden and glucose metabolism in AD patients by using specific molecular imaging tracers. The advanced imaging technologies have played important roles in quantitative assessment of biomarkers and understanding processes underlying AD. The National Institute on Aging−Alzheimer’s Association (NIA−AA) outlined in 2018 an unbiased descriptive AD biomarker classification scheme, called the ATN (amyloid, tau, neurodegeneration) diagnosis framework [39]. However, due to the complex heterogeneity of AD, the interactions among accessible, objective imaging markers and the complete pathological loop that is formed remain unknown. The emerging field of imaging biomarker genomics that combines multimodal imaging and high-throughput sequencing technologies, is committed to analysing associations between imaging phenotypes and genomics data and using imaging phenotypes as intermediate phenotypes between genetic variants and clinical diagnosis to investigate the pathogenesis of AD. Hence, the imaging biomarker genomics approach can overcome the shortcomings of separate genomics or imaging analysis, in that it can confirm gene-to-disease specificity, promote the biological interpretability of pathological biomarkers, and contribute to the diagnosis, treatment and prevention of AD with multiscale imaging and genetic features.
When combined with clinical information, the imaging biomarker genomics approach may even facilitate precision medicine (Fig. 1). In this review, we provide a comprehensive summary of the brain imaging biomarker genomics approach, including (1) the basic analytical framework of brain imaging biomarker genomics studies and (2) implementation of this approach in AD based on the ATN framework, for exploring and validating AD biomarkers/variants and performing AD diagnosis and prognosis analysis. In particular, we introduce some key considerations relevant to studies using the brain imaging biomarker genomics approach and provide perspectives on the integration of neuroimaging and multiomics data and further methodological possibilities.
Fig. 1.
Landscape of advances of the AD imaging biomarker genomics field. This field covers genomics, imaging, and clinical information, ultimately pointing towards integrated diagnosis and precision medicine. CSF cerebrospinal fluid, CT computed tomography, MMSE mini-mental state examination, MoCA montreal cognitive assessment, AVLT auditory-verbal learning test, AFT animal fluency test, BNT boston naming test, MES memory and executive screening scale
In particular, this study focuses on neuroimaging markers based on the ATN framework. Other biomarkers, such as various cerebrospinal fluid (CSF) biomarkers, electroencephalography (EEG) or magnetoencephalography (MEG) markers, are excluded. In addition, other risk factors for AD (e.g. sex, education, cognitive tests, etc.) will not be discussed in this paper.
Methods
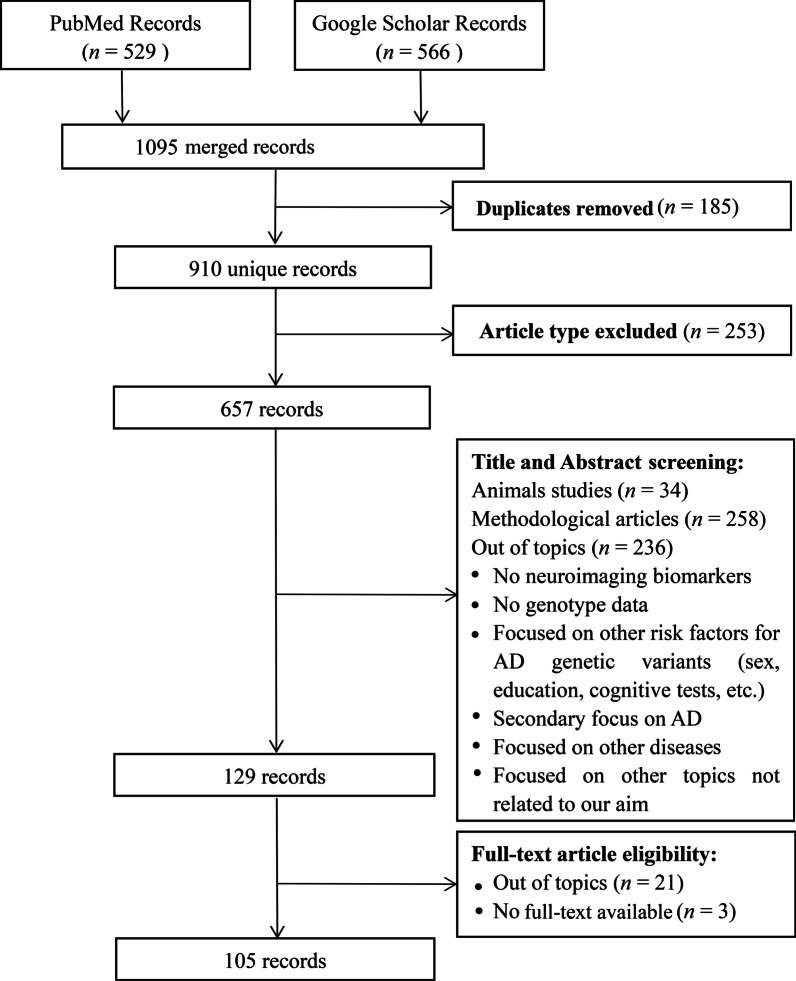
Literature was searched in Google Scholar and PubMed databases. Only human studies in English language, published from January 1991 (the publication year of earliest gene cloning of APP mutations) to December 2021 were reviewed. A total of 1095 records were yielded, of which 910 records were left after duplicate removal. A thorough description of the search strategy is provided in Additional file 1.
The inclusion criteria were as follows: (1) studies that identified AD candidate variants in large GWAS and meta-analyses, or described imaging biomarker genomics associations based on the ATN framework, such as genome-wide associations, polygenic scores analyses, AD classification diagnosis and prognosis, etc.; (2) studies focused on quantitative analysis of neuroimaging markers by using amyloid PET, tau PET, fluorodeoxyglucose (FDG) PET, anatomic MRI, or other MRI techniques including fMRI and DTI; (3) studies focused on single nucleotide polymorphism (SNP) genotype analysis. Articles were excluded if they were: (1) case reports, reviews, study-design protocols, books and documents, thesis, editorials, communications, opinion (methodological perspective) articles, and letters to the editors; (2) animal studies; (3) focused on methodological proposal and comparison, (4) not related to neuroimaging markers based on the ATN framework (e.g., various CSF biomarkers or EEG recording), or focused on other risk factors for AD (e.g., sex, education, cognitive tests). Finally, 105 records were included in this review. The detailed process of literature search and screening is presented in Fig. 2.
Fig. 2.
A flowchart of the search and screening process for articles included in this review
Evolving technologies of brain imaging biomarker genomics
The research field of brain imaging biomarker genomics has been developing for two decades. Initially, twin-based and family-based genetic designs were used to calculate the heritability of measures derived from neuroimaging, such as brain volume [40–42], functional connectivity [43], and WM structure [44]. These studies have confirmed that the brain imaging measures have a moderate to strong genetic effect in AD [45], suggesting the potential value of brain imaging biomarker genomics studies in AD. In this section, we will introduce the evolving technologies in this field and describe the technical frameworks used in AD research from both genetic and imaging perspectives.
Analytical procedures for AD imaging
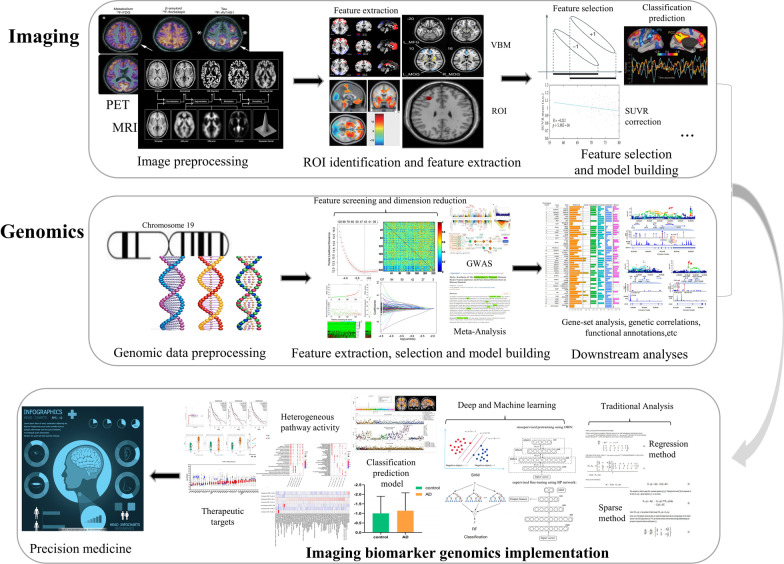
The systematic framework of brain imaging biomarker genomics for AD is composed of three panels: imaging, genomics and imaging biomarker genomics (Fig. 3).
Fig. 3.
Systematic computational framework for studies in the field of AD brain imaging biomarker genomics. The top panel indicates the analytical steps involved in imaging: image preprocessing, identification of regions of interest, feature extraction, feature selection, and model building and evaluation. The middle panel represents genomics procedures: genetic preprocessing, feature extraction and dimension reduction, model building, and statistical analysis. The bottom panel indicates integrated analysis methods in studies of imaging biomarker genomics, including association analysis, classification and prediction
Based on the ATN framework, the commonly used imaging techniques for AD are MRI and PET. MRI mainly includes sMRI, fMRI and DTI. PET imaging includes [18F] FDG PET, [18F] AV45 or [11C] Pittsburgh compound B ([11C] PiB) amyloid PET, and [18F] AV1451 tau-PET. Advances in imaging technologies have led to noninvasive or minimally invasive imaging of biomarkers, which may help capture all aspects of the disease process, including amyloid deposition [46], tau pathology [47], functional decline [48] and neuronal loss [49]. Below are the calculation frameworks for imaging analysis.
Step 1 Image preprocessing
High-resolution sMRI preprocessing includes realignment, segmentation, spatial normalization and smoothing. PET image processing includes realignment, coregistration, partial-volume correction, spatial normalization and smoothing. Resting-state fMRI preprocessing includes removal of unstable time points, slice timing corrections, head-motion corrections, baseline drift removal, spatial normalization and spatial smoothing. DTI data preprocessing includes skull stripping, background region filtering, and head-motion and eddy-current corrections. Several toolboxes can be used for this purpose, such as FSL (FMRIB’s Software Library) that processes MRI images (task or resting-state fMRI, sMRI, DTI, etc.) [50], Freesurfer that provides a series of algorithms to quantify brain functional and structural markers [51], and statistical parametric mapping (SPM) that is used for PET image preprocessing [52, 53]. More specifically, Data Processing & Analysis for Brain Imaging (DPABI) provides a complete resting-state fMRI analysis pipeline [54]. Other toolkits, such as DPARSF (Data Processing Assistant for Resting-State fMRI) and REST (Resting-State fMRI Data Analysis Toolkit) are also useful for fMRI analysis.
Step 2 Identification of regions of interest (ROIs) and feature extraction
This step includes precise identification of ROIs and extraction of imaging features [55, 56]. There are two common approaches to locating ROIs in brain imaging analyses: the voxel-based morphometry (VBM)-based method and the atlas-based method. VBM can achieve quantitative detection of differences in voxel-level imaging characteristics between groups. The atlas-based method projects the partitioning information from the standard brain atlas onto the images to identify specific brain regions. The identification of ROIs is followed by manual/automatic extraction of imaging features. The detailed characterization and calculation of imaging features are elaborated in Table 1. Feature extraction can usually be carried out by using FSL, Freesurfer, DPABI, SPM, the radiomics tool developed by Vallieres et al. (https://github.com/mvallieres/radiomics), and the Brain Connectivity Toolbox for graph theory-based brain network analyses [57].
Table 1.
Summary of imaging radiomics features and calculation formulas
| Feature name | Calculation formula | |
|---|---|---|
| First-order features | SUVR | |
| FA | ||
| Skewness | ||
| Kurtosis | ||
| Variance | ||
| Other First-order features: cortical thickness; grey matter volume (sMRI features); ALFF, fALFF, ReHo, FC (fMRI signals); MD, radD, axD (DTI diffusion parameters); clustering coefficient, characteristic path length, small-worldness, global efficiency, transitivity, assortativity coefficient, modularity (various network parameters); and so on | ||
| High-dimensional features | Energy | |
| Strength | ||
| Entropy | ||
| GLN | ||
| LRHGE | ||
| GLV | ||
| Other High-dimensional features are based on other analytical methods | ||
ALFF amplitude of low-frequency fluctuations, axD axial diffusivity, FA fractional anisotropy, fALFF fractional ALFF, FC functional connectivity, GLN/GLV grey-level non-uniformity/variance, LRHGE long run high grey-level emphasis, MD mean diffusivity, radD radial diffusivity, ReHo regional homogeneity, SUVR standard update value ratios. Where is the average intensity of the brain regions, is the average intensity of the reference region, means the DTI eigenvalues, denotes the number of grey levels, is the maximum distance of run lengths, denotes the number of pixels with grey level in the normalized grey histogram, and denotes the mean value
Step 3 Feature selection and model building
The aims of feature selection are to reduce feature redundancy and remove irrelevant features. Common feature selection methods include consistent stability analysis, statistical tests (two-sample t-test and rank-sum test), correlation analysis, sparse-group lasso, etc. There are two types of model construction: classification/prediction models and other statistical analysis models, such as regression analysis, correlation analysis, and survival analysis. Finally, model generalization capabilities are evaluated in terms of accuracy, sensitivity, specificity, correlation coefficient, and regression coefficient.
The above processes could also be carried out using deep learning (DL) algorithms, which can automatically extract quantitative and high-throughput features from medical images by end-to-end deep neural networks, which avoids complex hand-coding and does not need prior knowledge [58–61].
Analytical procedures for AD genomics
Early studies of brain genomics mainly focused on linkage and association analyses [62], in which candidate genetic markers were selected typically based on a hypothesis that implicates certain genes in AD pathogenesis. Advances in large-scale genotyping technologies enable comprehensive, unbiased GWAS, which can simultaneously test thousands of genetic markers. Nevertheless, GWAS might not avoid statistical artefacts that arise from the large number of tests. Systematic meta-analysis can alleviate this situation because this approach can quantitatively synthesize published genotype data for each polymorphism and produce a summary risk estimate (called the odds ratio) that contributes to the overall interpretation of association studies independent of positive or negative outcomes. Moreover, with the increase of sample sizes in GWAS analyses, ploygenic scores (PGS) are emerging as a novel statistical index that associates the collective individual SNP genotypes with specific diseases [63, 64]. In summary, AD genomics studies are mainly concentrated on traditional linkage and association analyses, large-scale case–control GWAS, systematic GWAS meta-analyses and recent PGS analyses, which facilitate identification of novel AD susceptibility genes as well as early diagnosis and prevention. The calculation frameworks for genomic analysis are mainly as follows.
Step 1 Genomic data preprocessing
As the first step, genomic data preprocessing includes quality control and imputation of genotyping data. Standard genotyping data quality control at the sample and variant level can be performed following a previously published pipeline [65, 66]. Genotyping data imputation is performed based on the Haplotype Reference Consortium (full panel) and the 1000 Genomes reference panel (for indels only).
Step 2 Feature extraction, selection and model building
This step aims at data mining and statistical analysis. Data mining focuses on feature extraction and dimensionality reduction, and constructs classification/prediction and statistical models with consideration of the complex nature of large genomics data. Statistical analysis mainly refers to construction of threshold-based association analysis models, including GWAS and meta-analysis. Subsequently, replication studies are always conducted to validate the results.
Step 3 Downstream analyses
Downstream analyses include conditional analysis, statistical fine-mapping analysis, colocalization with expression quantitative trait loci and metabolism quantitative trait loci, functional annotation, network analysis, gene-based analysis, gene set or tissue enrichment analysis, linkage disequilibrium analysis, PGS analysis, gene pleiotropy, heritability, genetic correlation calculation, etc.
Analytical procedures for AD imaging biomarker genomics
In general, the research field of AD imaging biomarker genomics is mainly focused on univariate or multivariate association analyses using imaging phenotypes as an intermediate. For example, Kim et al. [67] investigated genetic variants that influence cortical atrophy in 919 participants from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database. They analyzed correlations between 3,041,429 SNPs selected based on GWAS and cortical thickness in the whole brain. This study included three steps: (1) imaging/genomic data preprocessing; (2) calculation of cortical thickness as an imaging feature; and (3) statistical analysis. The results of the study identified that rs10109716 in ST18 and rs661526 in NFIA are significantly associated with the mean cortical thicknesses of the left inferior frontal gyrus and left parahippocampal gyrus, respectively. In addition, Ning et al. [68] employed a neural network (NN) framework that combined both brain atrophic measurements and SNP genotype data to distinguish AD patients from healthy controls (HC). In this study, volumes of 16 ROIs selected based on prior knowledge on brain regions affected by AD were used as the imaging feature, and genotypes of APOE ɛ4 risk allele and 19 SNPs were used as the genetic features. The results showed that the NN model with both imaging and genetic features had an area under the receiver operating characteristic curve (AUC) of 0.99 in classifying AD and HC subjects.
Implementation of AD imaging biomarker genomics studies
Findings from studies on candidate genetic variants for AD
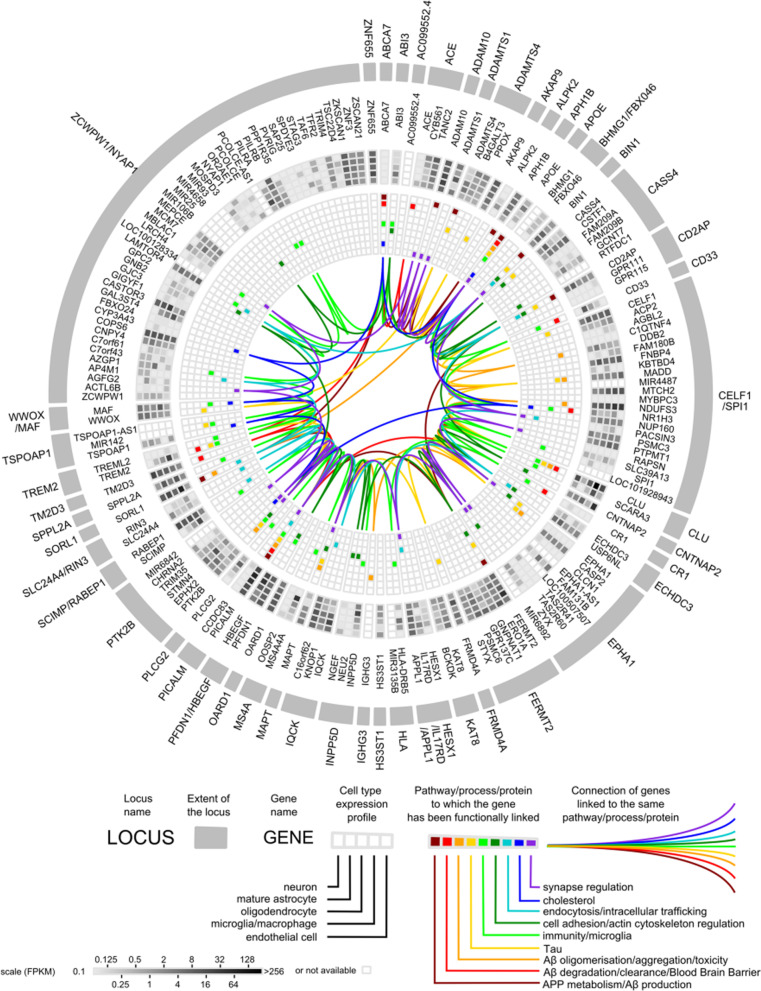
Since imaging biomarker genomics studies rely in part on prior knowledge of candidate genetic variants, we summarize the candidate variants in accordance with the timeline of identification in large GWAS and meta-analyses. Initially, mutations of APP, PSEN1 and PSEN2 genes were found in molecular studies in 1993 and in 1995, which caused rare, Mendelian forms of the disease, usually resulting in early-onset AD. APOE was recognized as the strongest susceptibility gene for late-onset AD (LOAD) in 1995. In studies to confirm new risk loci related to LOAD, GWAS and meta-analyses further identified a series of loci relevant to LOAD. The first GWAS study was conducted in 2007. Later, GWAS studies were separately performed in four LOAD genetic consortia (Genetic and Environmental Risk in Alzheimer’s Disease, European Alzheimer’s Disease Initiative, Cohorts for Heart and Aging Research in Genomic Epidemiology, and Alzheimer’s Disease Genetic Consortium), which identified a total of 11 loci, namely, CLU, PICALM, CR1, BIN1, CD2AP, CD33, EPHA1, MS4A4A, ABCA7, MS4A6A, and MS4A4E [16, 27–30]. Under the support from the International Genomics of Alzheimer’s Project (IGAP), a meta-analysis including 74,046 individuals of European ancestry further identified 11 new susceptibility loci for AD, which were HLA-DRB5, SORL1, PTK2B, SLC24A4-RIN3, ZCWPW1, NME8, FERMT2, CELF1, INPP5D, MEF2C and CASS4 [31]. A case–control study of 85,133 subjects from the IGAP identified 3 rare coding variants in PLCG2, ABI3, and TREM2, which are highly expressed in microglia, highlighting the contribution of microglial-mediated innate immunity to the development of AD [32]. Given the difficulty of AD case confirmation, a case–control genome-wide association study by proxy (GWAX) was conducted with the UK Biobank dataset using family history of disease (14,482 proxy cases, i.e., relatives of affected individuals and 10,0082 proxy controls, i.e., relatives of unaffected individuals). Meta-analysis of the previously published IGAP GWAS results combining with the above-highlighted GWAX summary statistics identified 4 new risk loci associated with AD (HBEGF, ECHDC3, SPPL2A, and SCIMP) [33]. In the following year, a second meta-analysis of IGAP data and parental history of AD in an expanded UK Biobank dataset (n = 314,278) based on the previous proxy-phenotype AD study by Liu et al. identified 3 new loci (ADAM10, KAT8, and ACE) [34]. A larger meta-analysis with clinically diagnosed AD and AD-by-proxy (71,888 cases, 383,378 controls), using cohorts collected by the Psychiatric Genomics Consortium Alzheimer, the IGAP, the Alzheimer’s Disease Sequencing Project and AD-by-proxy from UK Biobank, yielded 8 loci (ADAMTS4, HESX1, CLNK, CNTAP2, APH1B, ABI3, ALPK2, and ACO74212.3) [21]. An expanded IGAP analysis (n = 94,437) confirmed 20 previous LOAD risk loci and identified 5 new loci (IQCK, ACE, ADAM10, ADAMTS1 and WWOX) [20], two of which (ACE and ADAM10) had been recently identified in the study of Marioni et al. [34]. Following the meta-analysis of Lambert et al. and Marioni et al., an updated meta-analysis of GWAX in the UK Biobank with the latest GWAS for AD diagnosis was performed and identified 37 risk loci and 4 new associations (CCDC6, TSPAN14, NCK2 and SPRED2) [24]. Finally, the most recent GWAS with 1,126,563 individuals, which expanded on the basis of Jansen’s work and contained the largest sample size thus far, identified 38 loci, including 7 loci (AGRN, TNIP1, TMEM106B, GRN, HAVCR2, NTN5 and LILRB2) that had not been reported previously [25]. A detailed summary of the representative AD candidate genes is shown in Table 2. Figure 4 depicts a circular diagram of AD genetic risk factors according to several postgenomics analyses based on animal and cellular models, although the AD genetic background remains largely unidentified.
Table 2.
Summary of candidate genes used in AD pathology
| Year | Author | Dataset | Methods | Novel genes |
|---|---|---|---|---|
|
1991 [7] |
Goate et al. | Gene Cloning | Molecular studies | APP gene |
|
1993 [10] |
Corder et al. | Gene Cloning | Molecular studies | APOE gene |
|
1995 |
Sherrington et al. | Gene Cloning | Molecular studies |
2 genes (PSEN1 and PSEN2) |
|
2009–2011 |
Lambert et al. |
GERAD EADI CHARGE ADGC |
Meta-analysis |
11 genes (CLU, PICALM, CR1, BIN1, CD2AP, CD33, EPHA1, MS4A4A, ABCA7, MS4A6A, and MS4A4E) |
|
2013 [31] |
Lambert et al. |
IGAP (n = 74,046) |
Meta-analysis |
11 genes (HLA-DRB5, SORL1, PTK2B, SLC24A4-RIN3, ZCWPW1, NME8, FERMT2, CELF1, INPP5D, MEF2C, and CASS4) |
|
2017 [32] |
Sims et al. |
IGAP (n = 85,133) |
Meta-analysis |
3 genes (PLCG2, ABI3, and TREM2) |
|
2017 [33] |
Liu et al. |
UK Biobank (n = 116,196) |
Meta-analysis |
4 genes (HBEGF, ECHDC3, SPPL2A, and SCIMP) |
|
2018 [34] |
Marioni et al. |
UK Biobank (n = 314,278) |
Meta-analysis |
3 genes (ADAM10, KAT8, and ACE) |
|
2019 [21] |
Jansen et al. |
PGC-ALZ IGAP ADSP (n = 455,266) |
Meta-analysis |
8 genes (ADAMTS4, HESX1, CLNK, CNTAP2, APH1B, ABI3, ALPK2, and ACO74212.3) |
|
2019 [20] |
Kunkle et al. |
IGAP (n = 94,437) |
Meta-analysis |
5 genes (IQCK, ACE, ADAM10, ADAMTS1, and WWOX) |
|
2020 [24] |
Schwartzentruber et al. |
UK Biobank (n = 408,942) |
Meta-analysis |
4 genes (CCDC6, TSPAN14, NCK2, and SPRED2) |
|
2021 [25] |
Wightman et al. | 1,126,563 individuals | Meta-analysis |
7 genes (AGRN, TNIP1, TMEM106B, GRN, HAVCR2, NTN5, and LILRB2) |
Fig. 4.
Circular diagram of AD genetic risk factors. From outside to inside: (1) genomic loci in alphabetical order; (2) genes therein; (3) expression profiles of these genes in different cell types of the brain (greyscale); and (4) pathways/processes/proteins to which these genes have been functionally linked (colour lines).
Adapted from Dourlen P et al. Acta Neuropathologica. 2019 Aug; 138 (2):221–236. Reprinted with permission from Springer Nature
Findings from studies on AD candidate imaging biomarkers
In earlier studies, pairwise univariate analysis was performed to identify associations between genetic markers and imaging phenotypes. To accommodate more flexible associations involving multiple genetic markers and multiple imaging phenotypes, multiple regression and multivariate models have been used in recent studies in combination with machine learning (ML) methods [69]. In the following, we will review candidate-gene, genome-wide and polygenic associations with imaging-derived traits, according to the ATN framework for AD biomarkers proposed by NIA-AA in 2018 (Table 3) [39].
Table 3.
Summary of AD-relevant effects based on candidate imaging biomarkers and association studies
| Author | Dataset | Genes included | Model | Methods | Imaging phenotypes | Neural location | Results |
|---|---|---|---|---|---|---|---|
| Pathophysiological pathway: Brain Aβ accumulation (Aβ PET) | |||||||
|
2009 Drzezga et al. [70] |
32 AD | APOE | Univariate imaging—Univariate genetic | Candidate-based association | Aβ plaque deposition | Bilateral temporoparietal, frontal cortex | The ɛ4-positive patients with AD had higher levels of Aβ plaque deposition compared to age-matched ɛ4-negative patients with similar levels of cognitive impairment and brain atrophy |
|
2009 Reiman et al. [71] |
28 AD | APOE | Univariate imaging—Univariate genetic | Candidate-based association |
PiB DVR fibrillar Aβ burden |
Frontal, temporal, parietal, posterior cingulate-precuneus,basal ganglia ROIs | Fibrillar Aβ burden in cognitively normal older people was associated with APOE ɛ4 gene dose |
|
2011 Chibnik et al. [72] |
n = 1666 |
CR1, CLU, PICALM |
Univariate imaging—Multivariate genetic | Candidate-based association | Pathology score of neuritic plaques | Whole brain cortex | Common variation at the CR1 locus had a broad impact on cognition and this effect was mediated by an individual’s amyloid plaque burden |
|
2012 Thambisetty et al. [73] |
57 HC | CR1, APOE | Univariate imaging—Multivariate genetic | Candidate-based association | PIB DVR |
Orbitofrontal, prefrontal, superior frontal, posterior cingulate, lateral temporal, occipital cortices |
There was a greater variability in brain amyloid deposition in the CLU rs3818361 noncarrier group relative to risk carriers, an effect explained partly by APOE genotype |
|
2012 Swaminathan et al. [74] |
ADNI (22 HC, 25 AD, 56 MCI) |
15 amyloid candidate genes (DNCR24, NCSTN, SOAT1, BCHE, etc.) |
Multivariate imaging—Multivariate genetic | Candidate-based association | Normalized PiB uptake value | Anterior cingulate, frontal cortex, parietal cortex, precuneus | The minor allele of an intronic SNP within DHCR24 was identified and associated with a lower average PiB uptake, and non-carriers of the minor allele had higher PiB uptake in frontal regions compared to carriers |
|
2013 Shulman et al. [75] |
Multiple cohorts (n = 725/ 56/58) |
ABCA7, MS4A6A/MS4A4E, EPHA1, CD3, CR1, CD2AP, CLU, BIN1, PICALM |
Univariate imaging—Multivariate genetic | Candidate-based association | Pathology score of neuritic plaques | Midfrontal, middle temporal, inferior parietal, entorhinal, hippocampal cortex | Besides the previously reported APOE and CR1 loci, ABCA7 (rs3764650) and CD2AP (rs9349407) were associated with neuritic plaque burden |
|
2013 Shulman et al. [75] |
Multiple cohorts (n = 725/ 56/58) |
Genome-wide genotyping | Univariate imaging—Multivariate genetic | GWAS | Pathology score of neuritic plaques | Midfrontal, middle temporal, inferior parietal, entorhinal, hippocampal cortex | The finding discovered a novel variant near the amyloid precursor protein gene (APP, rs2829887) that is associated with neuritic plaques |
|
2013 Hohman et al. [76] |
ADNI (174 HC, 64 AD, 292 MCI) |
PICALM, BIN1, CR1, CLU, MS4A6A, EPHA1, CD33, ABCA7, CD2AP |
Multivariate imaging—Univariate genetic | Candidate-based association | Aβ PET SUVR | Cingulate, frontal, temporal, lateral parietal cortices | Two SNP-SNP interactions (BIN1 (rs7561528, rs744373) × PICALM (rs7851179)) reached significance when correcting for multiple comparisons |
|
2014 Lehmann et al. [77] |
52 AD | APOE | Multivariate imaging—Univariate genetic | Candidate-based association |
PIB DVR, FDG SUVR |
Frontal, lateral parietal/temporal, occipital cortices, precuneus, posterior cingulate gyrus, hippocampus | APOE ε4+ AD patients showed lower global amyloid burden and greater medial temporal hypometabolism compared with matched APOE ε4- patients |
|
2014 Ramanan et al. [78] |
ADNI (n = 555) |
Genome-wide genotyping | Univariate imaging—Multivariate genetic | GWAS | Aβ PET brain amyloid burden | Frontal, parietal, temporal, limbic, occipital lobes | A novel association with higher rates of amyloid load independent from APOE ε4 status was identified in IL1RAP (rs12053868-G) |
|
2018 Apostolova et al. [17] |
ADNI (322 HC, 159 AD, 496 MCI) |
The top 20 AD risk variants (ABCA7,CLU, SORL1, DSG2, etc.) | Univariate imaging—Multivariate genetic | Candidate-based association | Florbetapir mean SUVR | Frontal, anterior–posterior cingulate, lateral-parietal, lateral-temporal cortices | ABCA7 gene had the strongest association with amyloid deposition, after APOE ε4. FERMT2 gene had a stage-dependent association with brain amyloidosis |
|
2018 Scelsi et al. [79] |
ADNI (226 HC, 125 AD, 92 SMC, 501 MCI) |
Genome-wide genotyping | Multivariate imaging—Multivariate genetic | PGS-based association | Aβ PET SUVR, HV | Hippocampus | The finding identified a genome-wide significant locus implicating LCORL rs6850306. The possession of a minor allele at rs6850306 was protective against conversion from MCI to AD |
|
2019 Li et al. [80] |
ADNI (155 HC, 125 AD, 72 SMC, 422 MCI) |
Genome-wide genotyping | Univariate imaging—Multivariate genetic | GWAS | Florbetapir composite SUVR |
Frontal, anterior/ posterior cingulate, lateral parietal/ temporal regions |
The study identified 24 consensus modules enriched by robust genetic signals in a genome wide association analysis, including a few novel genes (ABL1, ABLIM2) |
|
2021 Kim et al [81] |
Korean cohort (n = 1474) |
Genome- wide genotyping |
Univariate imaging—multivariate genetic | GWAS | Aβ PET SUVR | Whole brain | In addition to APOE, nine SNPs of FGL2 gene on chromosome 7 were identified, which were associated with a decreased risk of Aβ positivity at a genome-wide suggestive level |
|
2021 Liu et al. [82] |
Multiple cohorts (n = 767/ 1373) |
Summary statistics | Multivariate imaging—Multivariate genetic | PGS-based association |
Aβ PET SUVR, HV, entorhinal, middle temporal gyrus volumes |
Whole brain cortex, Hippocampus, entorhinal cortex |
PGS was associated with the increased cortical amyloid burdens (PiB-PET and AV45-PET), but decreased hippocampus and entorhinal cortex volumes |
| Pathophysiological pathway: Tau hyperphosphorylation (Tau PET) | |||||||
|
2016 Smith et al. [83] |
4 HC, 3 AD |
MAPT | Univariate imaging—Univariate genetic | Candidate-based association |
Tau PET SUVR, GM volume |
Global AD pathology | 18F-AV1451 tau PET imaging correlated with tau pathology in MAPT mutation carriers |
|
2018 Mattsson et al. [84] |
65 Aβ + patients | APOE | Univariate imaging—Univariate genetic | Candidate-based association |
Tau PET SUVR, GM volume |
Parietal, entorhinal cortex | APOE ε4-negative patients had greater tau load and reduced cortical thickness, with the most pronounced effects for both in the parietal cortex |
|
2019 Shen et al. [85] |
ADNI (90 HC) |
MAPT rs242557 | Univariate imaging—Univariate genetic | Candidate-based association | Tau PET SUVR | Hippocampus | The finding confirmed the significant correlation of MAPT rs242557 risk variant with increased hippocampus tau burden in non-demented elders |
|
2019 Therriaultet al. [86] |
Multiple cohorts (281 HC, 75 AD, 133 MCI) |
APOE | Univariate imaging—Univariate genetic | Candidate-based association | Tau PET SUVR | Entorhinal cortex, hippocampus | The elevated risk of developing dementia conferred by APOE ε4 genotype involved mechanisms associated with both Aβ and tau aggregation |
|
2019 Franzmeier et al. [87] |
ADNI (49 HC, 40 MCI) |
BIN1 rs744373 | Univariate imaging—Univariate genetic | Candidate-based association |
Global/stage- specific Tau PET SUVR |
Brain Braak stage II–VI |
BIN1 rs744373 SNP was associated with increased tau but not Aβ pathology, that is alterations in BIN1 may contribute to memory deficits via increased tau pathology |
|
2020 Yan et al. [88] |
ADNI (57 AD) |
APOE | Multivariate imaging—Univariate genetic | Candidate-based association |
Tau PET SUVR, GM volume |
Temporal, parietal, posterior cingulate, entorhinal cortex, amygdala, parahippocampal gyrus, etc |
Among elderly individuals with AD, sex modified the effects of the APOE ε4 allele on region-specific tau deposition and GM volume |
|
2020 Neitzel et al. [89] |
Multiple cohorts (n = 493) |
APOE | Univariate imaging—Univariate genetic | Candidate-based association |
Baseline Tau PET SUVR, annual change rates |
MTL (entorhinal cortex, parahippocampus) |
There was an amyloid-independent association between APOE ε4 and elevated tau PET specifically in medial temporal regions |
|
2021 Franzmeier et al. [90] |
Multiple cohorts (n = 216) |
BIN1 rs744373 | Univariate imaging—Univariate genetic | Candidate-based association |
ROI Tau PET SUVR, annual change rates |
Whole brain | BIN1-associated AD risk was potentially driven by accelerated tau accumulation in the face of Aβ |
|
2021 Neitzel et al. [91] |
ADNI (347 HC, 48 AD, 156 MCI) |
Klotho-VShet | Multivariate imaging—Univariate genetic | Candidate-based association | Global/ROI tau/Aβ PET SUVR | Whole brain; bilateral inferior temporal gyri | Findings proved a protective role of KL-VShet against amyloid-related tau pathology and tau-related memory impairments in elderly humans at risk of AD dementia |
|
2021 Sun et al. [92] |
ADNI (n = 158) |
Summary statistics | Multivariate imaging—Multivariate genetic | PGS-based association | Global tau SUVR for Braak stage ROIs | Whole brain | The association between PGS and tau pathology was significant when APOE was excluded, even among females |
| Pathophysiological pathway: Neurodegeneration (sMRI) | |||||||
|
2007 Lunetta et al. [93] |
449 HC, 366 AD |
APOE | Univariate imaging—Univariate genetic | Candidate-based association | Cerebral atrophy, MTA, WMH, CVR | Cerebral atrophy, MTA, WMH | A substantial proportion of the additive genetic variation in MRI traits was explained by other genes, and MRI traits were heritable |
|
2009 Potkin et al. [94] |
ADNI (n = 381) |
Genome-wide genotyping | Univariate imaging—Multivariate genetic | GWAS | GM voxels of hippocampal regions | The right and left hippocampal regions | The study identified candidate risk genes (EFNA5, CAND1, MAGI2, ARSB, and PRUNE2) for sporadic AD, involved in the regulation of protein degradation, apoptosis, neuronal loss and neurodevelopment |
|
2010 Wolk et al. [95] |
ADNI (91 AD) |
APOE | Univariate imaging—Univariate genetic | Candidate-based association |
Cortical thickness, HV |
Hippocampus, superior frontal gyrus,angular gyrus, MTL, precentral gyrus | The presence or absence of the APOE ε4 allele influenced the cognitive and anatomic phenotypic expression of AD in a dissociable manner |
|
2010 Biffi et al. [96] |
Multiple cohorts (215 HC, 168 AD, 357 MCI) |
GWAS-validated and GWAS-promising novel AD loci | Univariate imaging—Multivariate genetic | Candidate-based association |
HV, amygdala volume, WM lesion volume, parahippocampal, entorhinal, temporal pole cortex thickness |
Hippocampal, parahippocampal gyrus, amygdala, entorhinal, temporal pole cortex |
Loci associated with AD influenced neuroimaging correlates of this disease. And neuroimaging analysis identified 2 additional loci (BIN1 and CNTN5) of high interest for further study |
|
2013 Meda et al. [97] |
ADNI (156 HC, 140 AD, 281 MCI) |
151 million SNPs within 212 KEGG pathways | Univariate imaging—Multivariate genetic | Candidate-based association | 12-month regional structural atrophy rates | Hippocampus, entorhinal cortex | A total of 109 SNP-SNP interactions were associated with right hippocampus atrophy, and 125 were associated with right entorhinal cortex atrophy |
|
2013 Jahanshad et al. [98] |
366 HC | SPON1 gene | multivariate imaging—multivariate genetic | Candidate-based association | Heritable brain connections | Maps of the brain’s structural connectome | Rs2618516 was shown to affect brain structure in an elderly population with varying degrees of dementia |
|
2014 Morgen et al. [99] |
165 AD | PICALM, APOE | Univariate imaging—Multivariate genetic | Candidate-based association | GM volume | Prefrontal cortex | There was a synergistic adverse effect of homozygosity for the PICALM risk allele G in rs3851179 and APOE ε4 on prefrontal volume and performance on the Trail Making Test A, which is sensitive to processing speed and working memory function |
|
2014 Hohman et al. [100] |
ADNI (388 HC, 228 AD, 764 MCI) |
Genome-wide genotyping | Univariate imaging—multivariate genetic | GWAS | Baseline ICV | Whole brain | One intergenic SNP rs4866650 and one SNP rs7849530 within the SPTLC1 gene modified the association between amyloid positivity and neurodegeneration |
|
2015 Chauhan et al. [101] |
8175– 11,550 HC |
24 AD candidate loci (APOE, BIN1,HLA-DRB1,CR33,CR1,CLU, ABCA7, SORL1, etc.) |
Multivariate imaging—Multivariate genetic | Meta- analysis |
ICV, TBV, HV, WMH |
Hippocampus | APOE rs2075650 was associated with smaller HV and CD33 rs3865444 with smaller ICV. There was associations of HLA-DRB1 with TBV and BIN1 with HV. A weighted AD genetic risk score was associated with smaller HV, even after excluding APOE locus |
|
2015 Desikan et al. [102] |
9386 HC, 6409 AD |
Summary statistics | Univariate imaging—Multivariate genetic | PGS-based association |
Longitudinal volume loss in MTL, entorhinal cortex, hippocampus |
MTL, hippocampus, entorhinal cortex |
Polygenic hazard scores predicted in vivo markers (volume loss in MTL, hippocampus, entorhinal cortex) |
|
2016 Yang et al. [103] |
ADNI (194 HC, 168 AD, 337 MCI) |
PICALM, CLU | Univariate imaging—Multivariate genetic | Candidate-based association |
HV, hippocampal shape |
Hippocampus | Common LOAD risk loci in CLU and PICALM exhibited significant interaction effects on hippocampal morphology in both young healthy adults and elderly individuals |
|
2016 Ramirez et al. [104] |
50 HC, 98 MCI |
the top 10 AD non-APOE genes | Univariate imaging—Multivariate genetic | Candidate-based association | Cortical thickness, hippocampal radial distance | Hippocampus | MS4A6A rs610932 and ABCA7 rs3764650 demonstrated significant associations with cortical and hippocampal atrophy |
|
2016 Habes et al. [105] |
n = 1472 | APOE | Univariate imaging—Univariate genetic | Candidate-based association |
AD-related GM volume |
Lateral frontal, lateral temporal, medial frontal cortex, hippocampus | Measurable APOE-related brain atrophy did not occur in early adulthood and midlife and such atrophy may only occur more proximal to the onset of clinical symptoms of dementia |
|
2016 Foley et al. [106] |
n = 272 |
APOE, summary statistics |
Multivariate imaging—Multivariat genetic |
PGS-based association |
HV | Hippocampus | A significant association was found between AD PGS and left HV, with higher risk associated with lower left HV, although excluding the APOE gene |
|
2016 Harrison et al. [107] |
n = 66 | Summary statistics | Univariate imaging—Multivariate genetic | PGS-based association | Thickness in hippocampal subregions | Hippocampus, entorhinal cortex | Polygenic AD risk scores may be especially sensitive to structural change over time in regions affected early in AD, like the hippocampus and adjacent entorhinal cortex |
|
2017 Wang et al. [108] |
ADNI (281 HC, 48 AD, 483 MCI) |
12 SNPs in HLA |
Univariate imaging—Multivariate genetic | Candidate-based association | Structural volumes |
Hippocampus, parahippocampus, posterior cingulate, middle temporal, etc |
TNF-α SNPs at rs2534672, rs2395488, HFE rs1800562 and RAGE rs2070600 were correlated with various structures on MRI |
|
2017 Wang et al. [109] |
ADNI (281 HC, 48 AD, 483 MCI) |
HLA-A2 | Univariate imaging—Univariate genetic | Candidate-based association |
Hippocampal/ parahippocampal/ amygdala/ middle temporal/ posterior cingulate volume, entorhinal cortex thickness |
Hippocampus, parahippocampus, posterior cingulate, precuneus, middle temporal, entorhinal cortex, amygdala | HLA-A2 in Caucasians contributed to the risk of AD by modulating the alteration of HV and HLA-A gene variants appeared to play a role in altering AD-related brain structures on MRI |
|
2017 Xiao et al. [110] |
n = 231 | APOE, summary statistics | Univariate imaging—Multivariate genetic | PGS-based association | Activation in hippocampus ROI | Hippocampus | There was a cumulative deleterious effect of LOAD risk genes on hippocampal function even in healthy volunteers |
|
2018 Axelrud et al. [111] |
Multiple cohorts | Summary statistics | Univariate imaging—Multivariate genetic | PGS-based association | HV | Left and right hippocampus | Genetic risk for AD may affect early-life cognition and HV |
|
2018 Li et al. [112] |
Multiple cohorts (n = 683) |
Summary statistics | Univariate imaging—Multivariate genetic | PGS-based association | GM volume | Precuneal cortex | An elevated AD PGR was associated with a smaller precuneal volume, and the effect remained after excluding the APOE genotype |
|
2019 Lancaster et al. [113] |
Multiple cohorts | AD SNPs within a microglia-mediated immunity network | Univariate imaging—Multivariate genetic | PGS-based association | HV | Hippocampus | The observations suggested that the relationship between AD and HV was partially explained by genes within an AD-linked microglia-mediated immunity network |
|
2020 Lyall et al. [114] |
UK Biobank (n = 8539) |
APOE | Multivariate imaging—Univariate genetic | Candidate-based association | FA, MD, left/right HV, total GM, total WM and log WMHV |
Left or right Hippocampus, total GM and WM |
There was association between APOE ε4 and WMHV, but not TBV or WM integrity |
|
2020 Cong et al. [115] |
ADNI (41 HC, 26 AD, 67 MCI) |
Genome- wide genotyping |
Univariate imaging—Multivariate genetic | GWAS | 14 MTL substructures | MTL | A novel association with right Brodmann area 36 volume was discovered in an ERC1 SNP rs2968869. And rs2968869 was associated with GM density and glucose metabolism in the right hippocampus and disease status |
|
2020 De Marco et al. [116] |
ADNI (317 HC, 562 MCI) |
Summary statistics | Univariate imaging—Multivariate genetic | PGS-based association | GM and WM volumes | Whole brain | PGS predicted volume in sensorimotor regions in ε3ε3 Aβ + participants. The link between polygenic hazard and neurocognitive variables varies depending on APOE ε4 allele status |
|
2020 van der Meer et al. [117] |
Multiple cohorts (n = 21,297) |
Genome-wide genotyping | Univariate imaging—multivariate genetic | GWAS | Hippocampal and subfield volumes | Hippocampus | GWAS of whole HV identified eight whole-genome significant loci, including three novel loci, namely, TFDP2 SNP rs7630893, FAM175B rs2303611, and PARP11 rs1419859 |
|
2021 Foo et al. [118] |
UK Biobank (n = 17,161) |
Summary statistics | Univariate imaging—Multivariate genetic | PGS-based association |
Volumes in hippocampal subregions |
Multiple hippocampal regions | PGSAD had differential effects on the hippocampal subfield volumes |
|
2021 Tank et al. [119] |
UK Biobank (n = 32,790) |
APOE, summary statistics | Univariate imaging—Multivariate genetic | PGS-based association | Volumes of total GM, WM, WMH, whole brain, left/ right hippocampus | Left hippocampus |
LOAD-PGR was associated with smaller HV and aspects of cognitive ability in healthy adults and could supplement APOE status in risk stratification of cognitive impairment/LOAD |
| Pathophysiological pathway: Neurodegeneration (FDG PET) | |||||||
|
2010 Corneveaux et al. [120] |
Multiple cohort (n = 1728) |
KIBRA rs17070145 | Univariate imaging—Univariate genetic | Candidate-based association | Glucose metabolism | Entorhinal cortex, hippocampus, middle temporal gyrus, posterior cingulate cortex, superior frontal gyrus, primary visual cortex | Non-carriers of the KIBRA rs17070145-T had increased risk of LOAD in an association study of 702 neuropathologically verified expired subjects and in a combined analysis of 1026 additional living and expired subjects |
|
2014 Lehmann et al. [77] |
52 AD | APOE | Multivariate imaging—Univariate genetic | Candidate-based association |
PIB DVR, FDG SUVR |
Lateral temporoparietal cortex, precuneus, posterior cingulate cortex, middle frontal gyrus, etc | APOE ε4+ AD patients showed lower global amyloid burden and greater medial temporal hypometabolism compared with matched APOE ε4- patients |
|
2018 Miller et al. [121] |
ADNI (n = 695) |
EXOC3L4 | Univariate imaging—Multivariate genetic | WGS | Global cortical glucose metabolism | Whole brain cortex | EXOC3L4 gene, was identified as significantly associated with global cortical glucose metabolism. Three loci that may affect splicing within EXOC3L4 helped to the association |
|
2018 Kong et al. [122] |
ADNI (37 HC, 59 AD, 126 MCI) |
Genome-wide genotyping | Univariate imaging—Univariate genetic | GWAS | ROI glucose metabolic uptake | Left and right angular, temporal gyri, bilateral posterior cingulate | A genome-wide significant SNP rs12444565 in the RBFOX1, four suggestive loci (rs235141, rs79037, rs12526331 and rs12529764) were associated with 18F-FDG |
|
2020 Seo et al. [123] |
KBASE (336 HC, 84 AD, 136 MCI) |
132 AD candidate genes | Multivariate imaging—Multivariate genetic | Candidate-based association |
Aβ deposition, region cerebral glucose metabolism/ cortical thickness, HV |
AD-signature cortical, hippocampus | Several novel loci for common variants were associated with AD pathology (PIWIL1, NME8 and PSEN2, PSEN1, CASS4). Cases carrying rare variants in LPL, FERMT2, NFAT5, DSG2, and ITPR1 displayed associations with the neuroimaging features |
|
2021 Wang et al. [124] |
ADNI (n = 586) |
Genome- wide genotyping |
Univariate imaging—Multivariate genetic | GWAS | Glucose metabolic uptake in ROIs | Left angular gyri, bilateral posterior cingulate gyrus, right /left middle/inferior temporal gyrus | Two genome-wide significant SNPs (rs4819351, rs13387360) in AGPAT3 and LOC101928196 served as protective sites to regulate the decline of glucose metabolism |
|
2019 Li et al. [80] |
ADNI (37 HC, 86 AD, 188 MCI) |
Genome-wide genotyping | Univariate imaging—Multivariate genetic | GWAS | Glucose metabolic uptake in ROIs | Frontal, lateral parietal, lateral temporal regions, anterior/posterior cingulate regions | Indirect genetic effects on certain chemical compound or protein translocation were reflected in the PET scans and may be associated with AD |
| Pathophysiological pathway: Neurodegeneration (fMRI) | |||||||
|
2000 Bookheimer et al. [125] |
30 HC | APOE | Univariate imaging—Univariate genetic | Candidate-based association | Patterns of brain activation |
Left hippocampal, parietal, prefrontal cortices |
Both the magnitude and the extent of brain activation during memory-activation tasks in regions of the left hippocampal, parietal, and prefrontal regions, were greater among the carriers of the APOE ε4 allele than among the carriers of the APOE ɛ3 allele |
|
2011 Erk et al. [126] |
109 HC | CLU rs11136000 | Univariate imaging—Univariate genetic | Candidate-based association | FC | Hippocampus, prefrontal cortex | Healthy carriers of the variant exhibited altered coupling between hippocampus and prefrontal cortex during memory processing |
|
2011 Lancaster et al. [127] |
43 HC | CLU rs11136000 | Univariate imaging—Univariate genetic | Candidate-based association | Working memory values based on brain activity |
Frontal, posterior cingulate cortex, hippocampus |
Participants with the CLU risk genotype had higher activity than participants with the protective allele in frontal and posterior cingulate cortex and hippocampus |
|
2014 Green et al. [128] |
131 HC | APOE, CLU | Univariate imaging—Multivariate genetic | Candidate-based association | ROI BOLD signal change |
Hippocampus, MTL |
APOE ε4 and CLU-C had an additive effect on brain activity, that is, increased combined genetic risk was associated with decreased brain activity during executive attention, including in the MTL |
|
2014 Guerini et al. [129] |
n = 1680 | SNAP-25 SNP | Univariate imaging—Univariate genetic | Candidate-based association | FMRI task accuracy |
Cingulate cortex, frontal, temporoparietal cortices |
FMRI analyses indicated that SNAP-25 genotypes correlated with a significantly decreased brain activity in the cingulate cortex and in the frontal (middle, superior gyri) and the temporo-parietal (angular gyrus) area |
|
2014 Liu et al. [130] |
Han Chinese (21 HC, 46 MCI) |
TOMM40 rs157581 | Univariate imaging—Univariate genetic | Candidate-based association | ALFF | Bilateral superior frontal gyrus, bilateral lingual gyrus, right calcarine sulcus, left cerebellar | TOMM40 rs157581 polymorphism may modulate regional spontaneous brain activity and relate to the progression of aMCI |
|
2015 Lancaster et al. [131] |
85 HC | CLU rs11136000 | Multivariate imaging—Univariate genetic | Candidate-based association | Working memory task accuracy, GM density |
Hippocampus, prefrontal, limbic areas |
Young individuals with the CLU rs11136000-C had higher activation levels in prefrontal and limbic areas during a working memory task. And there were subtle reductions in GM in the right hippocampal formation in carriers of the risk variant |
|
2015 Zhang et al. [132] |
360 HC | BIN1 rs744373 | Multivariate imaging—Univariate genetic | Candidate-based association |
Working memory, GM volume, FC |
Whole brain |
Healthy homozygous carriers of the rs744373 risk allele exhibited worse high-load working memory performance, larger HV and lower FC between the bilateral hippocampus and right dorsolateral prefrontal cortex |
|
2017 Sun et al. [133] |
32 HC, 32 MCI |
PICALM rs3851179 | Univariate imaging—Univariate genetic | Candidate-based association | FC | DMN | The PICALM rs3851179 polymorphism significantly affected the DMN network in MCI |
|
2017 Xiao et al. [110] |
n = 231 | APOE, summary statistics | Univariate imaging—Multivariate genetic | PGS-based association | Activation in hippocampus ROI | Hippocampus | There was a cumulative deleterious effect of LOAD risk genes on hippocampal function even in healthy volunteers |
|
2017 Su et al. [134] |
131 HC, 87 MCI |
APOE, summary statistics | Univariate imaging—Multivariate genetic | PGS-based association | FC in ROIs of DMN | Temporal cortex |
The pMCIs exhibited tremendous decrements in DMN connections that were partially determined by the AD-related risk alleles |
|
2018 Korthauer et al. [135] |
76 HC | APOE | Multivariate imaging—Univariate genetic | Candidate-based association | Graph analysis of network efficiency | Whole brain functional-structural network | ε4 carriers had significantly lower global and local efficiency of the integrated resting-state structural connectome compared to non-carriers |
|
2021 Franzmeier et al. [136] |
Multiple cohort (n = 378) |
BDNFVal66Met SNP | Univariate imaging—Univariate genetic | Candidate-based association | FC | DMN, DAN, SAL, CON | BDNFVal66Met was associated with a higher vulnerability of hippocampus-frontal connectivity to primary AD pathology |
|
2019 Chandler et al. [137] |
n = 75 |
APOE, summary statistics |
Univariate imaging—Multivariate genetic | PGS-based association | Whole-brain gmCBF | Frontal cortex | The results found a reduction in gmCBF in APOE ε4 carriers, a negative relationship between AD-PGS and gmCBF, and regional reductions in gmCBF in individuals with higher AD-PGS across the frontal cortex |
|
2019 Axelrud et al. [138] |
Multiple cohorts (n = 636) |
APOE, summary statistics |
Univariate imaging—Multivariate genetic | PGS-based association | FC among main nodes for 10 tau pathology networks |
Precuneus, superior temporal gyrus |
The PGS was associated with the connectivity between the right precuneus and the right superior temporal gyrus |
|
2020 Chandler et al. [139] |
n = 608 |
APOE, summary statistics |
Univariate imaging—Multivariate genetic | PGS-based association | Bilateral hippocampus bold parameters | Hippocampus | AD-PGS, not APOE, selectively influenced activity within the HC in response to scenes, while other perceptual nodes remained intact |
| Pathophysiological pathway: Neurodegeneration (DTI) | |||||||
|
2010 Smith et al. [140] |
23 HC, 42 AD |
APOE | Univariate imaging—Univariate genetic | Candidate-based association | FA |
Inferior temporal lobe, amygdala/ hippocampal head region |
Reduced FA was observed in the fronto-occipital and inferior temporal fasciculi (particularly posteriorly), the splenium of the corpus callosum, subcallosal white matter and the cingulum bundle |
|
2005 Nierenberg et al. [141] |
29 HC | APOE | Univariate imaging—Univariate genetic | Candidate-based association |
FA, axD, radD |
Parahippocampal region | The APOE ε4 carriers showed significantly lower fractional anisotropy and higher radial diffusivity in the parahippocampal WM 15 mm below the anterior commissure-posterior commissure plane than noncarriers |
|
2014 Warstadt et al. [142] |
n = 481 | Genome-wide genotyping | multivariate imaging—multivariate genetic | GWAS | Diffusion tensor, FA | Corpus callosum, fornix, internal capsule, inferior fronto-occipital fasciculus | A follow-up analysis detected WM associations with rs5882 in the opposite direction |
|
2015 Liang et al. [143] |
126 HC | SORL1 rs2070045 | Univariate imaging—Univariate genetic | Candidate-based association |
FA, MD, axD, radD |
Bilateral cingulum, cingulum hippocampal area | Sex moderated the effects of the SOR1 gene rs2070045 polymorphism on cognitive impairment and disruption of the cingulum hippocampal integrity in healthy elderly |
|
2016 Foley et al. [106] |
n = 197 |
APOE, summary statistics |
Multivariate imaging—Multivariat genetic |
PGS-based association |
FA | Right cingulum | Fractional anisotropy of the right cingulum was inversely correlated with AD polygenic risk scores |
|
2017 Cavedo et al. [144] |
74 HC | APOE | Univariate imaging—Univariate genetic | Candidate-based association |
FA, MD, radD, axD |
Cingulum, corpus callosum, inferior fronto-occipital, inferior longitudinal fasciculi, internal, external capsule | These findings indicated a modulatory role of APOE ε4 on WM microstructure in elderly individuals at risk for AD suggesting early vulnerability and/or reduced resilience of WM tracts involved in AD |
|
2018 Rutten-Jacobs et al. [145] |
UK Biobank (n = 8448) |
Genome-wide genotyping | Univariate imaging—Multivariate genetic | GWAS | FA, MD, WMHV | White matter hyperintensity | A novel genome-wide significant locus VCAN rs13164785 on chr5q14 was identified, which may work in the mechanisms underlying microstructural integrity of the WM measured as FA and MD |
|
2019 Gu et al. [146] |
GWAS Summary Statistics | PSEN1 | Multivariate imaging—Univariate genetic |
Meta- analysis |
WM integrity, cerebral amyloid deposition and brain metabolism | Whole brain | PSEN1 mutation associated with WM changes and amyloid deposition occurred in AD. Increased MD was observed and showed significant increase with amyloid deposition |
|
2020 Yan et al. [147] |
ADNI (34 HC, 36 AD, 49 MCI) |
34 GWAS AD risk SNPs | Univariate imaging—Multivariate genetic | Candidate-based association | Fibre anisotropy, fibre length and density | 278 brain ROIs | Rs10498633 in SLC24A4 was found to be significantly associated with anisotropy, total number and length of fibres. APOE rs429358 showed nominal significance of association with the density of fibres between subcortical and cerebellum regions |
|
2020 Horgusluoglu-Moloch et al. [148] |
ADNI (34 HC, 15 AD, 56 MCI) |
23 AD genes | Univariate imaging—Multivariate genetic | Candidate-based association | FA, MD, radD, axD, LIN, SPH, PLA, MOD |
Hippocampus, cingulum, parahippocampal gyrus right, sagittal stratum, etc |
A SNP rs2203712 in CELF1 was most significantly associated with several DTI-derived features in the hippocampus, the top ranked brain region |
ALFF amplitude of low-frequency fluctuations, axD axial diffusivity, CVR rating of cerebrovascular disease, DAN dual attention network, DMN default mode network, DVR distribution volume ratios, FA fractional anisotropy, FC functional connectivity, FN frontoparietal network, HV hippocampal volume, ICV intracranial volume, gmCBF grey-matter cerebral blood flow, KBASE Korean brain aging study for early diagnosis and prediction of Alzheimer’s disease, KL-VShet KL-VS heterozygosity, LIN linearity of the tensor, MD mean diffusivity, MOD mode of the tensor, MTA medial temporal atrophy, MTL medial temporal lobe, PLA planarity of the tensor, pMCI progressive MCI, radD radial diffusivity, SMC significant memory concern, SN salience network, SPH sphericity of the tensor, SUVR standard update value ratios, TBV total brain volume, WMH white matter hyperintensity
Imaging genomics analysis of “A” biomarker
Of the ATN framework, “A” refers to the Aβ plaque biomarker, including cortical amyloid PET ligand binding and CSF Aβ42 level. The deposition of amyloid plaques in the brain is one of the two main pathological signs of AD. As a reliable imaging phenotype of AD, amyloid PET can selectively detect Aβ deposition in the brain. A number of studies using amyloid PET have investigated how various genetic variants influence Aβ burden.
At the candidate-gene level, Drzezga et al. [70] examined the effect of APOE genotype on the levels of [11C] PiB PET Aβ plaques in AD patients using the VBM-based method and regression analysis. The results showed higher levels of Aβ plaque deposition in ε4-positive patients in bilateral temporoparietal and frontal cortical areas. Apostolova et al. [17] investigated the associations of the top 20 AD risk variants with brain amyloidosis using ADNI datasets by multivariable linear regression analysis. The results showed that the ABCA7 gene has the strongest association with amyloid deposition, while the APOE ε4 and FERMT2 genes show stage-dependent associations with amyloid deposition, especially in the MCI stage.
At the genome-wide level, Yan et al. [149] conducted a GWAS meta-analysis using [11C] PiB PET imaging from the ADNI datasets, and found that the APOE region showed the most significant association with brain Aβ burden. Ramanan et al. [150] performed the first GWAS of cortical Aβ burden in humans using data from ADNI-2 and ADNI-Grand Opportunity and reported that APOE and BCHE (BUCHE) are independent regulators of amyloid deposition in the brain, accounting for nearly 15% of the variance in cross-sectional amyloid load. At the polygenic level, Tan et al. [151] observed a strong association between polygenic hazard scores and Aβ uptake. A detailed summary of these findings is shown in Table 3.
Imaging genomics analysis of “T” biomarker
“T” refers to the tau biomarker, including CSF phosphorylated tau and cortical tau PET. The twisted strands of the protein tau (tangles) inside neurons are the other pathological marker of AD. Although tau pathology serves as a primary brain pathology associated with cognitive impairment in AD, most previous studies have focused on CSF tau levels, which reflect tau production rather than the amount of pathological tau deposition in the brain. The recent advent of AV1451 tau-PET imaging has allowed the assessment of fibrillary tangles in the living brain.
At the candidate-gene level, Smith et al. [83] reported that the [18F] AV1451 tau-PET imaging is strongly correlated with tau neuropathology in MAPT (microtubule-associated protein tau) mutation carriers. After that, Yan et al. [88] explored the association of sex and APOE ε4 with brain tau deposition and atrophy in older adults with AD, and found that female APOE ε4 carriers (FACs) have elevated tau-PET SUVR in comparison to non-FACs. Therriault et al. [86] and Neitzel et al. [89] independently evaluated different datasets and reported that APOE ε4 is associated with higher tau accumulation and that this association is independent of amyloid burden. Regarding other AD candidate genes, Franzmeier et al. [87, 90] and Neitzel et al. [91] suggested that the BIN1 rs744373 SNP and Klotho-VS heterozygosity are associated with higher and lower pathologic tau levels, respectively, by analyses of variance and multiple linear regression.
At the genome-wide level, Ramanan et al. [152] conducted the first neuroimaging GWAS of tau pathology in 754 individuals. The findings not only confirmed the association of MAPT with tau burden, but also identified the NTNG2-rs75546066 locus as having a novel protective effect against tau pathology.
At the polygenic level, Sun et al. [92] assessed PGS values as a predictor of tau pathology in non-demented individuals. The results showed that higher PGS values were correlated with elevated tau-PET uptake values, and the significance remained when APOE was regressed.
Imaging genomics analysis of “N” biomarker
“N” refers to neurodegeneration or neuronal injury, including CSF total tau level, [18F]FDG PET hypometabolism, and atrophy on sMRI. Among them, sMRI is the most widely used technology in imaging biomarker genomics studies to extract targeted imaging phenotypes, with increased discriminative power and improved biological interpretability. [18F]FDG PET can detect brain glucose metabolism and provide important pathological staging information. Several studies have also investigated how various genetic variants influence brain glucose metabolism.
At the candidate-gene level, the associations of APOE with MRI genotypes have been investigated, especially between ε4 carriers and noncarriers. For example, Wolk et al. [95] found that the APOE genotype affects cognitive and anatomic phenotypic expression of AD, in that the ɛ4 carriers with mild AD show greater impairment on measures of memory retention and greater MTL atrophy compared to noncarriers who are more impaired in working memory and show greater frontoparietal atrophy. Risacher et al. [153] found that the annual percent change rate of MRI atrophy is influenced by the APOE genotype. Morgen et al. [99] found that the genetic interaction between PICALM and APOE is associated with brain atrophy and cognitive impairment using univariate analysis of variance. Moreover, Biffi et al. [96] investigated the impact of multiple GWAS-validated and GWAS-promising candidate loci on hippocampal volume, amygdala volume, WM lesion volume, entorhinal cortical thickness, parahippocampal gyrus thickness and temporal pole cortical thickness. The study indicated that genetic variants that modulate AD risk as revealed in previous GWASs may influence neuroimaging measures. In addition, BIN1 and CNTN5 were identified as two novel loci that show associations with multiple MRI characteristics, which are of interest for further studies. Regarding brain glucose metabolism biomarkers, Lehmann et al. [77] assessed the relationships between glucose metabolism and APOE genotype in clinical AD patients, with one-way analysis of variance and Tukey’s post-hoc test, and found a greater degree of medial temporal hypometabolism in APOE ε4 carriers. Miller et al. [121] explored and confirmed the associations between rare variants in splicing regulatory element loci of EXOC3L4 and global cortical glucose metabolism in the ADNI cohort. Notably, Seo et al. [123] analyzed the effects of 132 selected susceptibility genes previously identified to be associated with LOAD, on neurodegenerative brain features by using neuroimaging data from the KBASE (Korean Brain Aging Study for Early Diagnosis and Prediction of Alzheimer’s disease) cohort, including [11C]PiB PET, [18F]FDG PET, and MRI. In contrast to previous studies, this study utilized five in vivo AD pathologies and associated them with both common and rare genetic variants by performing targeted sequencing of 132 candidate genes.
At the genome-wide level, Kong et al. [122] performed the first GWAS examining brain FDG metabolism in 222 subjects from the ADNI cohort in 2018, and identified RBFOX1 (RNA-binding Fox1) SNP rs12444565 to have a strong association with brain glucose metabolism. Wang et al. [124] identified two genome-wide significant SNPs, rs4819351 in AGPAT3 (1-acylglycerol-3-phosphate O-acyltransferase 3) and rs13387360 in LOC101928196, that had strong protective effects against the longitudinal metabolic decline in the right temporal gyrus and the left angular gyrus, respectively. At the polygenic level, Desikan et al. [102] reported that the polygenic hazard score was associated with longitudinal MRI-derived volume loss in the entorhinal cortex and hippocampus.
In addition to the above “N” biomarker, many other advanced MRI technologies have also been applied to study the influence of genetic variation on functional or WM alterations. Based on the DTI technology, WM alterations have been found in AD and MCI, and APOE may play a role in modulating these alterations [140, 141, 143, 144, 146–148]. Some researchers have reported differences in WM integrity between healthy APOE ɛ4 carriers and noncarriers by using diffusion parameters, including fractional anisotropy, mean diffusivity, and radial diffusivity. In addition, Gu et al. [146] performed a meta-analysis of associations of the PSEN1 genotype with WM integrity and brain metabolism, and indicated that PSEN1 is associated with mean diffusivity increase in DTI markers and decreased brain metabolism. Foley et al. [106] analyzed associations between AD polygenic risk scores and diffusion-weighted parameters in young adults, and revealed that the fractional anisotropy of the right cingulum is correlated with AD polygenic risk score. Regarding fMRI, both resting-state fMRI and task-fMRI were conducted to evaluate associations of brain activity with APOE and other AD risk genes [129, 130, 133, 136]. Many of these studies were performed in healthy older adults [125–128, 131, 132, 135] to investigate potential risk-allele influences on functional brain activity. It is worth noting that Jahanshad et al. [98] explored the heritability of various brain connections based on genome-wide associations and discovered the SPON1 (F-spondin) rs2618516 variant to affect dementia severity. Besides, Su et al. [134] investigated the associations between AD PGS and functional connectivity in the default mode network, and found significant correlations in the temporal cortex.
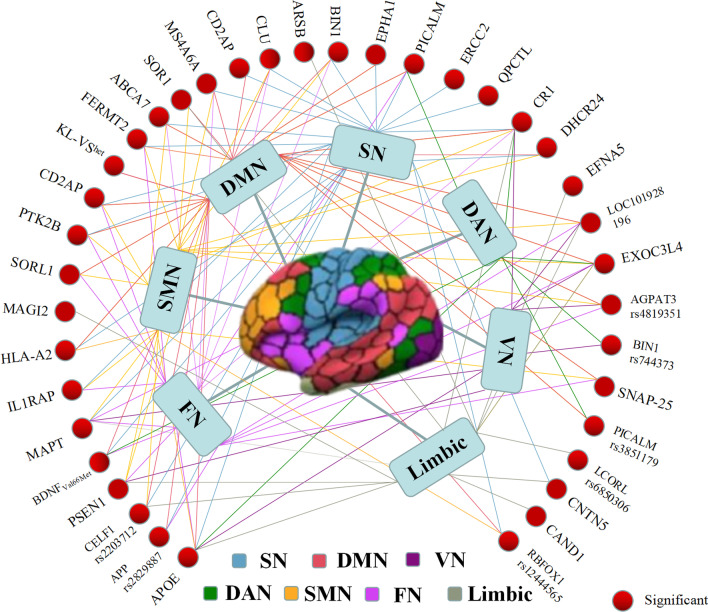
Figure 5 illustrates the mapping of associations between genomic data and brain functional networks, which are classified into 7 brain networks according to Yeo’s template, including visual network, somatomotor network, dual attention network, salience network, limbic network, frontoparietal network, and default mode network. In summary, associative studies of AD brain imaging biomarker genomics can provide new insights into the pathological and genetic mechanisms underlying AD. In addition, the number of genome-wide studies is relatively small compared with candidate-gene association studies, which may be caused by the scarcity of neuroimaging data. However, studies only focused on selected candidate genes may ignore potential interactions among multiple significant genetic variants, which emphasizes the necessity of genome-wide interaction and PGS analyses with improvement in multimodal imaging databases.
Fig. 5.
The relationship between genomic data and 7 specific brain networks from Yeo’s template. These associations are respectively marked in colors consistent with the corresponding brain networks. DAN dual attention network, DMN default mode network, FN frontoparietal network, SMN somatomotor network, SN salience network, VN visual network
AD diagnosis and prognosis based on brain imaging biomarker genomics
Recent advances of artificial intelligence (AI) techniques enable automatic combination of multimodal neuroimaging and genomics data to provide complementary and comprehensive information for AD diagnosis and prognosis. Specifically, ML methods have been widely implemented in computer-aided diagnosis of AD, including traditional ML models and advanced DL algorithms. The traditional classification models include support vector machine (SVM), random forest (RF), linear discriminant analysis (LDA) and regression models (RL). De Velasco et al. [154] compared performances of ML models least absolute shrinkage and selection operator (LASSO), k-nearest neighbour (KNN), and SVM in predicting LOAD from genetic variation data, with SVM showing the best performance (AUC = 0.72). In addition, APOE genotype is the most commonly utilized genomic data. For example, Gray et al. [155] performed multi-modality classification based on joint embedding of sMRI, FDG PET, CSF biomarkers, and APOE genotype data, using a multimodal RF model and a fourfold cross validation (CV) to predict AD, and achieved an accuracy of 89% in classifying AD from healthy controls. Similarly, by combining sMRI, FDG PET, CSF biomarkers, APOE genotype, age, sex and body mass index, Kohannim et al. [156] selected a SVM model and performed leave-one-out CV for AD and MCI classification and prediction of future cognitive decline within 1 year, and achieved a maximum of 90% accuracy for AD vs healthy controls. To distinguish between stable and progressive MCI, Dukart et al. [157] used a plain Bayesian (naive Bayesian, NB) algorithm based on APOE genotype, neuropsychological assessment, sMRI, and FDG PET, achieving an accuracy of approximately 87%. Moreover, Bi et al. [158] combined fMRI and SNP data and used the multimodal RF algorithm to distinguish AD from normal control, and finally obtained AD prediction accuracy of 87%. Varol et al. [159] proposed the heterogeneity through discriminative analysis (HYDRA) algorithm to predict AD based on combined sMRI and SNP data, with the highest AUC value being 0.942.
On the other hand, in the context of DL method, Liu et al. [160] integrated DTI and SNP data with deep convolutional neural networks for prediction of AD, and obtained AUC values of 0.8571, 0.8291, 0.8583, and 0.7756 at baseline, 6 months, 12 months and 24 months, respectively. Similarly, combining sMRI and SNP data, Ning et al. [68] used a neural network to predict AD and achieved an AUC value of 0.992. Moreover, based on sMRI, demographics, neuropsychological assessment and APOE genotype data, Spasov et al. [161] used the convolutional neural network model to distinguish MCI patients who would develop AD within 3 years from patients with stable MCI, with an AUC value of 0.925. By combining sMRI, FDG PET and SNP data, Zhou et al. [162] conducted three-stage deep feature learning and fusion to simultaneously predict HC, MCI and AD, with an accuracy of 65%, which was higher than that of other ML classification methods. In addition to the joint use of imaging and clinical information, combination with multiomics information is also an emerging trend in AD research. Shigemizu et al. [163] integrated genomic data and microRNA expression profiles to construct a proportional hazards model-based prognostic model to identify MCI individuals at high risk of AD. A consistency index of 0.702 was obtained on an independent test set. A detailed list of machine learning-based studies of imaging biomarker genomics is provided in Table 4.
Table 4.
Application of machine learning based on imaging biomarker genomics in AD diagnosis and prognosis
| Method | Year | Modality | Model | Dataset | CV | Neural location | Results |
|---|---|---|---|---|---|---|---|
| Machine learning | 2010 [156] | sMRI, FDG PET, CSF, APOE genotype, age, sex, body mass index | SVM |
HC: 213 AD: 158 MCI: 264 |
LOOCV |
Hippocampal, ventricular, temporal lobe |
A maximum up to 90% accuracy for AD |
| 2013 [155] | sMRI, FDG PET, CSF, APOE genotype | MRF |
HC: 35 AD: 37 MCI: 75 |
Fourfold CV | Whole brain | An accuracy of 89% for AD | |
| 2014 [164] |
sMRI, FDG PET, CSF, SNP |
SVM |
HC: 47 AD: 49 MCI: 93 |
Tenfold CV |
Whole brain | An accuracy of 71% among HC, MCI and AD | |
| 2016 [157] | APOE genotype, neuropsychological assessment, sMRI, FDG PET | NB |
HC: 112 AD: 144 sMCI: 265 pMCI: 177 |
independent test set | Whole brain | An accuracy of 87% in identifying pMCI from sMCI | |
| 2017 [159] | sMRI, SNP | HYDRA |
HC: 139 AD: 103 |
– |
Hippocampus, entorhinal cortex frontal lobe |
The highest AUC value of 0.942 for AD | |
| 2017 [165] | sMRI, SNP | SVM |
HC: 204 AD: 171 MCI: 362 |
Tenfold CV |
Whole brain | An accuracy of 80.8% identifying pMCI from sMCI | |
| 2019 [158] | fMRI, SNP | MRF |
HC: 35 AD: 37 |
– | Olfactory cortex, insula, posterior cingulate gyrus and lingual gyrus | An accuracy of 87% AD prediction | |
| 2019 [154] | SNP |
LASSO, KNN, SVM |
HC: 371 AD: 267 |
CV | – | The highest reached 0.72 of the AUC | |
| 2019 [166] | APOE, PET, PGS | LR |
HC: 224 AD: 174 MCI: 344 |
– | Whole brain | An AUC value of 0.69 using PGS and APOE to predict amyloid state | |
| 2020 [167] | sMRI, FDG PET, AV45 PET, DTI, resting-state fMRI, APOE genotype | MKL |
HC: 35 AD: 33 sMCI: 30 pMCI: 31 |
LOOCV | Whole brain | An accuracy of 96.9% in identifying pMCI from sMCI | |
| Deep learning | 2017 [162] |
SNP, sMRI FDG PET |
DFFF |
HC: 226 AD: 190 MCI: 389 |
Twentyfold CV | Whole brain | An accuracy of 0.65 among HC, MCI and AD |
| 2018 [68] | sMRI, SNP | NN |
HC: 225 AD: 138 MCI: 358 |
Fivefold CV | 16 ROIs (hippocampus, entorhinal cortex, parahippocampal gyrus, amygdala, precuneus, etc.) | An AUC value of 0.992 using combined features | |
| 2019 [161] | sMRI, demographic, neuropsychological assessment, APOE genotype data | CNN |
HC: 184 AD: 192 sMCI: 228 pMCI: 181 |
Tenfold CV | Whole brain | An AUC value of 0.925 for pMCI prediction | |
| 2019 [160] | DTI, SNP | DCNN |
HC: 100 AD: 51 |
Fivefold CV | Temporal lobes (including the hippocampus) and the ventricular system | The highest AUC value of 0.858 | |
| 2021 [61] | MRI, SNP, electronic health records | CNN | ADNI | independent test set | Whole brain | A maximum up to 87% accuracy |
CNN convolutional neural network, CV cross validation, DCNN deep CNN, DFFF deep feature learning and fusion framework, HYDRA heterogeneity through discriminative analysis, LOOCV leave-one-out CV, MKL multiple kernel learning, MRF multimodal random forest, NN neural network, pMCI progressive MCI, sMCI stable MCI
In summary, the above-mentioned studies show that ML methods with multimodal data such as imaging, clinical and multiomics data as input measures, are valuable tools for prognosis and risk stratification of AD with improved accuracy.
Key considerations and perspectives regarding AD imaging biomarker genomics
As a novel approach, the brain imaging biomarker genomics technique still needs further optimization, mainly in the following aspects.
Variable control in calculations
Calculations in AD imaging biomarker genomics can be influenced by various factors. Differences in physiological, demographic, and environmental factors can affect heritability estimates and measurements of brain-related features, which may obscure the disease-related effects and limit the utility of brain-related features as endophenotypes. Some recent studies have investigated associations of APOE ε4 status and sex with cognitive memory [88, 95, 168–170]. Therefore, these potential confounding factors should be included as covariates to improve comparability and reliability of findings. In particular, sex, education and APOE ε4 status are always used as covariates in large imaging–genomics GWAS and meta-analyses. Another way to avoid these potential influences is to carry out studies in healthy individuals or in a single ethnic or sex group. Ethnicity is another critical factor. Independent replication and meta-analyses remain the most reliable methods for reducing false-positive findings [171]. Comprehensive and ethnicity-homogeneous databases are needed to verify the generalizability and robustness of significant results. Compared to candidate-gene analyses which could not account for epistatic effects between genes, genome-wide analysis is more unbiased, thus underscoring again the significance of large samples in the future.
Use of prior knowledge on calculations
Interpretation of results is a focus of brain imaging biomarker genomics for AD. The use of prior knowledge, such as the Allen Human Brain atlas (AHBA), can facilitate calculations in brain imaging biomarker genomics and correlate spatial variations at the molecular scale with macroscopic neuroimaging phenotypes. For example, Franzmeier et al. [90] and Neitzel et al. [91] have used the AHBA to explore associations of BIN1 rs744373 and KL-VS heterozygosity with tau accumulation, respectively. Moreover, Sepulcre et al. [172] have developed a novel graph theory approach named directional graph theory regression (DGTR) to investigate the intersection of tau/Aβ pathological changes in the brain and the genetic transcriptome of AHBA. This approach can potentially be applied to explore more phenotype-genotype associations. Taken together, increasing the sensitivity and power of genetic effects, adequately utilizing ROIs, reliably stimulating responses, and highlighting differences among individuals are extremely necessary. For example, identifying differential masks first, as ROIs on a unique dataset, will lead to higher sensitivity.
Generalization of multivariate approaches beyond GWAS
Currently, biomarkers derived from GWASs were usually identified based on clinical outcomes. This approach has both advantages and disadvantages. Compared with imaging phenotypes limited by the scarcity of neuroimaging data, it is easier and more feasible to obtain a large number of clinical phenotypes, thus better meeting the prerequisites of large-scale GWAS and reducing greatly false-positive results. However, the accuracy of this approach is influenced by the sample size and statistical methods. In contrast, combining neuroimaging markers with GWAS genetic phenotypes can explain potential biological mechanisms in relatively small sample sizes.
Therefore, imaging biomarker genomics studies are gaining novel insights in comparison to traditional GWAS analyses. For example, data-driven multivariate approaches are emerging to explain more imaging-genetic variants, such as sparse canonical correlation analysis and parallel independent component analysis [69]. These multivariate approaches have provided increased detection power and put forward new technical challenges, including data dimensionality reduction and feature selection strategies. Besides, the GWAS analysis pipelines are also expected to be further optimized to process complex and high-dimension genetic data automatically.
Combination of AI and brain imaging biomarker genomics
Currently, ML methods have been widely used for AD diagnosis and prognosis. On the one hand, traditional ML and advanced DL algorithms are relatively mature computational methods in AD imaging studies and include model building, feature processing and model evaluation. On the other hand, combination of genomics calculations with ML algorithms has not been widely performed. Applications of deep neural networks in genetic studies are still scarce, although seminal studies have demonstrated the accessibility of deep neural networks to DNA sequencing data, resulting in generation of DeepBind, DeepSEA and Basset networks [173–176]. Therefore, more efforts should be focused on the development of solutions for technical challenges especially for DL algorithms, such as how to reduce dimensionality of multimodal data, how to integrate imaging and genomics data, and how to interpret the effectiveness of DL features.
Integration of multiomics data
AD imaging biomarker genomics research has identified numerous novel genetic variants and gained insights into disease mechanisms. However, the pathological mechanisms underlying AD are still far from well understood. Apart from the development of methods, the integration of multimodal imaging data and genomics, microRNAomics, metabolomics, proteomics, and transcriptomics will continue to be an important research direction. Genomics is now the most mature omic technology with development of high-throughput genotyping arrays and sequencing strategies. Other omic technologies have also been incorporated into research domains. For example, mass spectrometry-based proteomics has driven deep profiling of the proteome in AD. The AD proteomic review by Bai et al. [177] indicated that proteomics-driven systems biology would be a promising frontier to link genotype, proteotype, and phenotype and accelerate improvement in AD models and treatment strategies. Besides, neuroimaging markers are not limited to MRI and PET markers. During the last few decades, EEG and MEG techniques have also been commonly applied in AD studies. For instance, alterations of brain rhythms and functional connectivity have been revealed in EEG and MEG studies [178–180]. Relationships between various AD genetic risk factors and EEG phenotypes have also been reported [181–184]. Hence, compared with a single omics category, integration of multiomics information allows systemic exploration at multiscale layers to better understand the comprehensive biological information flow that underlies the disease and to pave the way for precision medicine.
Conclusions
The field of brain imaging biomarker genomics has made tremendous progress in the last decade to capture novel genetic variants and explore potential disease pathophysiology mechanisms. Future studies in this field are anticipated to move forward to precise medicine, to identify significant findings that can be used in clinical practice, and to achieve computer-aided AD diagnosis and prognosis. Therefore, further development of current research methods and integration of information will continue to be an important research direction. There is no doubt that unbiased genome-wide approaches remain critical, and replication studies are necessary. Advances in next-generation sequencing approaches coupled with more refined brain mapping (such as AHBA that maps genetic variants to brain tissues) are increasingly promoting the interpretability of findings from imaging biomarker gemonics. In addition, DL algorithms allow for integration of multiple preprocessing steps into a single model to improve AD diagnosis and prognosis. In summary, current studies in the AD imaging biomarker genomics field have profiled the brain mechanisms at an unprecedented scale, raising new hypotheses for subsequent validation.
Supplementary Information
Additional file 1. Search strategy for literature.
Acknowledgements
Not applicable.
Abbreviations
- AD
Alzheimer’s disease
- ADNI
Alzheimer’s disease neuroimaging initiative
- AHBA
Allen human brain atlas
- AI
Artificial intelligence
- APOE
Apolipoprotein E
- APP
Amyloid precursor protein
- AUC
Area under curve
- Aβ
Amyloid β
- CSF
Cerebrospinal fluid
- CV
Cross validation
- DGTR
Directional graph theory regression
- DL
Deep learning
- DPABI
Data processing and analysis for brain imaging
- DPARSF
Data processing assistant for resting-state fMRI
- DTI
Diffusion tensor imaging
- EEG
Electroencephalography
- FAC
Female APOE ɛ4 carriers
- FDG
Fluorodeoxyglucose
- fMRI
Functional MRI
- FSL
FMRIB’s Software Library
- GM
Grey matter
- GWAS
Genome-wide association analysis
- GWAX
Genome-wide association study by proxy
- HC
Healthy controls
- HYDRA
Heterogeneity through discriminative analysis
- IGAP
International genomics of Alzheimer’s project
- KBASE
Korean brain aging study for early diagnosis and prediction of Alzheimer’s disease
- KNN
K-nearest neighbour
- LASSO
Least absolute shrinkage and selection operator
- LDA
Linear discriminant analysis
- LOAD
Late-onset AD
- MCI
Mild cognitive impairment
- MEG
Magnetoencephalography
- ML
Machine learning
- NB
Naive Bayesian
- NIA−AA
National Institute on Aging−Alzheimer’s Association
- NN
Neural network
- PET
Positron emission tomography
- PGS
Polygenic scores
- PSEN
Presenilins
- REST
Resting-state fMRI data analysis toolkit
- RF
Random forest
- RL
Regression models
- ROI
Regions of interest
- sMCI
Stable MCI
- sMRI
Structural magnetic resonance imaging
- SNP
Single nucleotide polymorphism
- SPM
Statistical parametric mapping
- SVM
Support vector machines
- VBM
Voxel-based morphometry
- WM
White matter
Author contributions
JJ and YH conceived and designed the manuscript. LL and XY had equal contributions in searching literature, tabulating the results and writing the manuscript. CS, XJ, QZ revised and provided critical input to the manuscript. JJ and YH revised and finalized the review. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (82020108013) and Science and Technology Innovation 2030 Major Projects (2022ZD0211600).
Availability of data and materials
Not applicable.
Declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Lanlan Li and Xianfeng Yu contribute equally to this work
Contributor Information
Ying Han, Email: hanying@xwh.ccmu.edu.cn.
Jiehui Jiang, Email: jiangjiehui@shu.edu.cn.
References
- 1.2021 Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2021;17:327-406. [DOI] [PubMed]
- 2.Cummings J. New approaches to symptomatic treatments for Alzheimer’s disease. Mol Neurodegener. 2021;16(1):2. doi: 10.1186/s13024-021-00424-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karch CM, Cruchaga C, Goate AM. Alzheimer’s disease genetics: from the bench to the clinic. Neuron. 2014;83(1):11–26. doi: 10.1016/j.neuron.2014.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Cauwenberghe C, Van Broeckhoven C, Sleegers K. The genetic landscape of Alzheimer disease: clinical implications and perspectives. Genet Med. 2016;18(5):421–430. doi: 10.1038/gim.2015.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.König T, Stögmann E. Genetics of Alzheimer’s disease. Wien Med Wochenschr. 2021;171:249–256. doi: 10.1007/s10354-021-00819-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glenner GG, Wong CW. Alzheimer’s disease: Initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun. 1984;120:885–890. doi: 10.1016/S0006-291X(84)80190-4. [DOI] [PubMed] [Google Scholar]
- 7.Goate A, Chartier-Harlin MC, Mullan M, Brown J, Crawford F, Fidani L, et al. Segregation of a missense mutation in the amyloid precursor protein gene with familial Alzheimer’s disease. Nature. 1991;349:704–706. doi: 10.1038/349704a0. [DOI] [PubMed] [Google Scholar]
- 8.Sherrington R, Rogaev EI, Liang Y, Rogaeva EA, Levesque G, et al. Cloning of a gene bearing missense mutations in early-onset familial Alzheimer’s disease. Nature. 1995;375(6534):754–760. doi: 10.1038/375754a0. [DOI] [PubMed] [Google Scholar]
- 9.Sherrington R, Froelich S, Sorbi S, Campion D, Chi H, et al. Alzheimer’s disease associated with mutations in presenilin 2 is rare and variably penetrant. Hum Mol Genet. 1996;5(7):985–988. doi: 10.1093/hmg/5.7.985. [DOI] [PubMed] [Google Scholar]
- 10.Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993;261:921–923. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- 11.Kim J, Basak JM, Holtzman DM. The role of apolipoprotein E in Alzheimer’s disease. Neuron. 2009;63:287–303. doi: 10.1016/j.neuron.2009.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castellano JM, Kim J, Stewart FR, Jiang H, DeMattos RB, Patterson BW, et al. Human apoE isoforms differentially regulate brain amyloid-β peptide clearance. Sci Transl Med. 2011;3:89ra57. doi: 10.1126/scitranslmed.3002156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verghese PB, Castellano JM, Garai K, Wang Y, Jiang H, Shah A, et al. ApoE influences amyloid-β (Aβ) clearance despite minimal apoE/Aβ association in physiological conditions. Proc Natl Acad Sci U S A. 2013;110:E1807–E1816. doi: 10.1073/pnas.1220484110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanan DA, Weisgraber KH, Russell SJ, Mahley RW, Huang D, Saunders A, et al. Apolipoprotein E associates with beta amyloid peptide of Alzheimer’s disease to form novel monofibrils. Isoform apoE4 associates more efficiently than apoE3. J Clin Invest. 1994;94(2):860–9. doi: 10.1172/JCI117407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grupe A, Abraham R, Li Y, Rowland C, Hollingworth P, Morgan A, et al. Evidence for novel susceptibility genes for late-onset Alzheimer’s disease from a genome-wide association study of putative functional variants. Hum Mol Genet. 2007;16:865–873. doi: 10.1093/hmg/ddm031. [DOI] [PubMed] [Google Scholar]
- 16.Lambert JC, Heath S, Even G, Campion D, Sleegers K, Hiltunen M, et al. Genome-wide association study identifies variants at CLU and CR1 associated with Alzheimer’s disease. Nat Genet. 2009;41:1094–1099. doi: 10.1038/ng.439. [DOI] [PubMed] [Google Scholar]
- 17.Apostolova LG, Risacher SL, Duran T, Stage EC, Goukasian N, West JD, et al. Associations of the top 20 Alzheimer disease risk variants with brain amyloidosis. JAMA Neurol. 2018;75:328–341. doi: 10.1001/jamaneurol.2017.4198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee JJ, Wedow R, Okbay A, Kong E, Maghzian O, Zacher M, et al. Gene discovery and polygenic prediction from a genome-wide association study of educational attainment in 1.1 million individuals. Nat Genet. 2018;50:1112–21. doi: 10.1038/s41588-018-0147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andrews SJ, McFall GP, Booth A, Dixon RA, Anstey KJ. Association of Alzheimer’s disease genetic risk loci with cognitive performance and decline: a systematic review. J Alzheimer’s Dis. 2019;69(4):1109–1136. doi: 10.3233/JAD-190342. [DOI] [PubMed] [Google Scholar]
- 20.Kunkle BW, Grenier-Boley B, Sims R, Bis JC, Damotte V, Naj AC, et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat Genet. 2019;51:414–430. doi: 10.1038/s41588-019-0358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jansen IE, Savage JE, Watanabe K, Bryois J, Williams DM, Steinberg S, et al. Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Nat Genet. 2019;51:404–413. doi: 10.1038/s41588-018-0311-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dehghan A. Genome-wide association studies. Methods Mol Biol. 2018;1793:37–49. doi: 10.1007/978-1-4939-7868-7_4. [DOI] [PubMed] [Google Scholar]
- 23.Yeung CHC, Lau KWD, Au Yeung SL, Schooling CM. Amyloid, tau and risk of Alzheimer’s disease: a Mendelian randomization study. Eur J Epidemiol. 2021;36:81–88. doi: 10.1007/s10654-020-00683-8. [DOI] [PubMed] [Google Scholar]
- 24.Schwartzentruber J, Cooper S, Liu JZ, Barrio-Hernandez I, Bello E, Kumasaka N, et al. Genome-wide meta-analysis, fine-mapping and integrative prioritization implicate new Alzheimer’s disease risk genes. Nat Genet. 2021;53:392–402. doi: 10.1038/s41588-020-00776-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wightman DP, Jansen IE, Savage JE, Shadrin AA, Bahrami S, Holland D, et al. A genome-wide association study with 1,126,563 individuals identifies new risk loci for Alzheimer’s disease. Nat Genet. 2021;53:1276–1282. doi: 10.1038/s41588-021-00921-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kunkle BW, Schmidt M, Klein HU, Naj AC, Hamilton-Nelson KL, Larson EB, et al. Novel Alzheimer disease risk loci and pathways in African American individuals using the African genome resources panel: a meta-analysis. JAMA Neurol. 2021;78:102–113. doi: 10.1001/jamaneurol.2020.3536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harold D, Abraham R, Hollingworth P, Sims R, Gerrish A, Hamshere ML, et al. Genome-wide association study identifies variants at CLU and PICALM associated with Alzheimer’s disease. Nat Genet. 2009;41:1088–1093. doi: 10.1038/ng.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seshadri S, Fitzpatrick AL, Ikram MA, DeStefano AL, Gudnason V, Boada M, et al. Genome-wide analysis of genetic loci associated with Alzheimer disease. JAMA. 2010;303(18):1832–1840. doi: 10.1001/jama.2010.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naj AC, Jun G, Beecham GW, Wang LS, Vardarajan BN, Buros J, et al. Common variants at MS4A4/MS4A6E, CD2AP, CD33 and EPHA1 are associated with late-onset Alzheimer’s disease. Nat Genet. 2011;43:436–441. doi: 10.1038/ng.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hollingworth P, Harold D, Sims R, Gerrish A, Lambert JC, Carrasquillo MM, et al. Common variants at ABCA7, MS4A6A/MS4A4E, EPHA1, CD33 and CD2AP are associated with Alzheimer’s disease. Nat Genet. 2011;43:429–435. doi: 10.1038/ng.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lambert JC, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C, et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat Genet. 2013;45:1452–1458. doi: 10.1038/ng.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sims R, Van Der Lee SJ, Naj AC, Bellenguez C, Badarinarayan N, Jakobsdottir J, et al. Rare coding variants in PLCG2, ABI3, and TREM2 implicate microglial-mediated innate immunity in Alzheimer’s disease. Nat Genet. 2017;49:1373–1384. doi: 10.1038/ng.3916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu JZ, Erlich Y, Pickrell JK. Case-control association mapping by proxy using family history of disease. Nat Genet. 2017;49:325–331. doi: 10.1038/ng.3766. [DOI] [PubMed] [Google Scholar]
- 34.Marioni RE, Harris SE, Zhang Q, McRae AF, Hagenaars SP, Hill WD, et al. GWAS on family history of Alzheimer’s disease. Transl Psychiatry. 2018;8(1):99. doi: 10.1038/s41398-018-0150-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rathore S, Habes M, Iftikhar MA, Shacklett A, Davatzikos C. A review on neuroimaging-based classification studies and associated feature extraction methods for Alzheimer’s disease and its prodromal stages. Neuroimage. 2017;155:530–548. doi: 10.1016/j.neuroimage.2017.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gao F. Integrated positron emission tomography/magnetic resonance imaging in clinical diagnosis of Alzheimer’s disease. Eur J Radiol. 2021;145:110017. doi: 10.1016/j.ejrad.2021.110017. [DOI] [PubMed] [Google Scholar]
- 37.Braak H, Braak E. Development of Alzheimer-related neurofibrillary changes in the neocortex inversely recapitulates cortical myelogenesis. Acta Neuropathol. 1996;92:197–201. doi: 10.1007/s004010050508. [DOI] [PubMed] [Google Scholar]
- 38.Delacourte A, David JP, Sergeant N, Buée L, Wattez A, Vermersch P, et al. The biochemical pathway of neurofibrillary degeneration in aging and Alzheimer’s disease. Neurology. 1999;52:1158–1165. doi: 10.1212/WNL.52.6.1158. [DOI] [PubMed] [Google Scholar]
- 39.Jack CR, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA research framework: toward a biological definition of alzheimer’s disease. Alzheimer’s Dement. 2018;14:535–562. doi: 10.1016/j.jalz.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thompson PM, Cannon TD, Narr KL, van Erp T, Poutanen VP, Huttunen M, et al. Genetic influences on brain structure. Nat Neurosci. 2001;4:1253–1258. doi: 10.1038/nn758. [DOI] [PubMed] [Google Scholar]
- 41.Ge T, Reuter M, Winkler AM, Holmes AJ, Lee PH, Tirrell LS, et al. Multidimensional heritability analysis of neuroanatomical shape. Nat Commun. 2016;7:13291. doi: 10.1038/ncomms13291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roshchupkin GV, Gutman BA, Vernooij MW, Jahanshad N, Martin NG, Hofman A, et al. Heritability of the shape of subcortical brain structures in the general population. Nat Commun. 2016;7:13738. doi: 10.1038/ncomms13738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Glahn DC, Winkler AM, Kochunov P, Almasy L, Duggirala R, Carless MA, et al. Genetic control over the resting brain. Proc Natl Acad Sci U S A. 2010;107:1223–1228. doi: 10.1073/pnas.0909969107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Peper JS, Brouwer RM, Boomsma DI, Kahn RS, Hulshoff Pol HE. Genetic influences on human brain structure: a review of brain imaging studies in twins. Hum Brain Mapp. 2007;28(6):464–473. doi: 10.1002/hbm.20398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jansen AG, Mous SE, White T, Posthuma D, Polderman TJC. What twin studies tell us about the heritability of brain development, morphology, and function: a review. Neuropsychol Rev. 2015;25:27–46. doi: 10.1007/s11065-015-9278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rabinovici GD, Jagust WJ. Amyloid imaging in aging and dementia: testing the amyloid hypothesis in vivo. Behav Neurol. 2009;21:117–128. doi: 10.1155/2009/609839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Villemagne VL, Okamura N. In vivo tau imaging: obstacles and progress. Alzheimers Dement. 2014;10:S254–S264. doi: 10.1016/j.jalz.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 48.Shen L, Thompson PM, Potkin SG, Bertram L, Farrer LA, Foroud TM, et al. Genetic analysis of quantitative phenotypes in AD and MCI: imaging, cognition and biomarkers. Brain Imaging Behav. 2014;8:183–207. doi: 10.1007/s11682-013-9262-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Frisoni GB, Fox NC, Jack CR, Scheltens P, Thompson PM. The clinical use of structural MRI in Alzheimer disease. Nat Rev Neurol. 2010;6:67–77. doi: 10.1038/nrneurol.2009.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jenkinson M, Beckmann CF, Behrens TE, Woolrich MW. Smith SM. FSL Neuroimage. 2012;62:782–90. doi: 10.1016/j.neuroimage.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 51.Fischl B. FreeSurfer. Neuroimage. 2012;62:774–781. doi: 10.1016/j.neuroimage.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ding C, Du W, Zhang Q, Wang L, Han Y, Jiang J. Coupling relationship between glucose and oxygen metabolisms to differentiate preclinical Alzheimer’s disease and normal individuals. Hum Brain Mapp. 2021;42:5051–5062. doi: 10.1002/hbm.25599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dong QY, Li TR, Jiang XY, Wang XN, Han Y, Jiang JH. Glucose metabolism in the right middle temporal gyrus could be a potential biomarker for subjective cognitive decline: a study of a Han population. Alzheimer’s Res Ther. 2021;13:74. doi: 10.1186/s13195-021-00811-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yan CG, Wang XD, Zuo XN, Zang YF. DPABI: data Processing & Analysis for (Resting-State) Brain Imaging. Neuroinformatics. 2016;14(3):339–351. doi: 10.1007/s12021-016-9299-4. [DOI] [PubMed] [Google Scholar]
- 55.Zhou H, Jiang J, Lu J, Wang M, Zhang H, Zuo C. Dual-model radiomic biomarkers predict development of mild cognitive impairment progression to Alzheimer’s disease. Front Neurosci. 2019;13:1045. doi: 10.3389/fnins.2018.01045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu Y, Jiang J-H, Chen L, Lu J-Y, Ge J-J, Liu F-T, et al. Use of radiomic features and support vector machine to distinguish Parkinson’s disease cases from normal controls. Ann Transl Med. 2019;7:773. doi: 10.21037/atm.2019.11.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bullmore E, Sporns O. Complex brain networks: graph theoretical analysis of structural and functional systems. Nat Rev Neurosci. 2009;10:186–198. doi: 10.1038/nrn2575. [DOI] [PubMed] [Google Scholar]
- 58.Jo T, Nho K, Saykin AJ. Deep learning in Alzheimer’s disease: diagnostic classification and prognostic prediction using neuroimaging data. Front Aging Neurosci. 2019;11:220. doi: 10.3389/fnagi.2019.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ding Y, Sohn JH, Kawczynski MG, Trivedi H, Harnish R, Jenkins NW, et al. A deep learning model to predict a diagnosis of Alzheimer disease by using 18 F-FDG PET of the brain. Radiology. 2019;290:456–464. doi: 10.1148/radiol.2018180958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu M, Li F, Yan H, Wang K, Ma Y, Shen L, et al. A multi-model deep convolutional neural network for automatic hippocampus segmentation and classification in Alzheimer’s disease. Neuroimage. 2020;208:116459. doi: 10.1016/j.neuroimage.2019.116459. [DOI] [PubMed] [Google Scholar]
- 61.Venugopalan J, Tong L, Hassanzadeh HR, Wang MD. Multimodal deep learning models for early detection of Alzheimer’s disease stage. Sci Rep. 2021;11:3254. doi: 10.1038/s41598-020-74399-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Clark RF, Goate AM. Molecular genetics of Alzheimer’s disease. Arch Neurol. 1993;50:1164–1172. doi: 10.1001/archneur.1993.00540110044004. [DOI] [PubMed] [Google Scholar]
- 63.Torkamani A, Wineinger NE, Topol EJ. The personal and clinical utility of polygenic risk scores. Nat Rev Genet. 2018;19:581–590. doi: 10.1038/s41576-018-0018-x. [DOI] [PubMed] [Google Scholar]
- 64.Leonenko G, Sims R, Shoai M, Frizzati A, Bossù P, Spalletta G, et al. Polygenic risk and hazard scores for Alzheimer’s disease prediction. Ann Clin Transl Neurol. 2019;6:456–465. doi: 10.1002/acn3.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.de Rojas I, Moreno-Grau S, Tesi N, Grenier-Boley B, Andrade V, Jansen IE, et al. Common variants in Alzheimer’s disease and risk stratification by polygenic risk scores. Nat Commun. 2021;12(1):3417. doi: 10.1038/s41467-021-22491-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.DeMichele-Sweet MAA, Klei L, Creese B, Harwood JC, Weamer EA, McClain L, et al. Genome-wide association identifies the first risk loci for psychosis in Alzheimer disease. Mol Psychiatry. 2021;26:5797–5811. doi: 10.1038/s41380-021-01152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim BH, Nho K, Lee JM. Genome-wide association study identifies susceptibility loci of brain atrophy to NFIA and ST18 in Alzheimer’s disease. Neurobiol Aging. 2021;102:200.e1–200.e11. doi: 10.1016/j.neurobiolaging.2021.01.021. [DOI] [PubMed] [Google Scholar]
- 68.Ning K, Chen B, Sun F, Hobel Z, Zhao L, Matloff W, et al. Classifying Alzheimer’s disease with brain imaging and genetic data using a neural network framework. Neurobiol Aging. 2018;68:151–158. doi: 10.1016/j.neurobiolaging.2018.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sheng J, Wang L, Cheng H, Zhang Q, Zhou R, Shi Y. Strategies for multivariate analyses of imaging genetics study in Alzheimer’s disease. Neurosci Lett. 2021;762:136147. doi: 10.1016/j.neulet.2021.136147. [DOI] [PubMed] [Google Scholar]
- 70.Drzezga A, Grimmer T, Henriksen G, Mühlau M, Perneczky R, Miederer I, et al. Effect of APOE genotype on amyloid plaque load and gray matter volume in Alzheimer disease. Neurology. 2009;72(17):1487–1494. doi: 10.1212/WNL.0b013e3181a2e8d0. [DOI] [PubMed] [Google Scholar]
- 71.Reiman EM, Chen K, Liu X, Bandy D, Yu M, Lee W, et al. Fibrillar amyloid-burden in cognitively normal people at 3 levels of genetic risk for Alzheimer’s disease. Proc Natl Acad Sci U S A. 2009;106(16):6820–6825. doi: 10.1073/pnas.0900345106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chibnik LB, Shulman JM, Leurgans SE, Schneider JA, Wilson RS, Tran D, et al. CR1 is associated with amyloid plaque burden and age-related cognitive decline. Ann Neurol. 2011;69:560–569. doi: 10.1002/ana.22277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thambisetty M, An Y, Nalls M, Sojkova J, Swaminathan S, Zhou Y, et al. Effect of complement CR1 on brain amyloid burden during aging and its modification by APOE genotype. Biol Psychiatry. 2013;73:422–428. doi: 10.1016/j.biopsych.2012.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Swaminathan S, Shen L, Risacher SL, Yoder KK, West JD, Kim S, et al. Amyloid pathway-based candidate gene analysis of [(11)C]PiB-PET in the Alzheimer’s disease neuroimaging initiative (ADNI) cohort. Brain Imaging Behav. 2012;6:1–15. doi: 10.1007/s11682-011-9136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shulman JM, Chen K, Keenan BT, Chibnik LB, Fleisher A, Thiyyagura P, et al. Genetic susceptibility for Alzheimer disease neuritic plaque pathology. JAMA Neurol. 2013;70:1150–1157. doi: 10.1001/jamaneurol.2013.2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hohman TJ, Koran ME, Thornton-Wells T. Epistatic genetic effects among Alzheimer’s candidate genes. PLoS ONE. 2013;8:e80839. doi: 10.1371/journal.pone.0080839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lehmann M, Ghosh PM, Madison C, Karydas A, Coppola G, O’Neil JP, et al. Greater medial temporal hypometabolism and lower cortical amyloid burden in ApoE4-positive AD patients. J Neurol Neurosurg Psychiatry. 2014;85:266–273. doi: 10.1136/jnnp-2013-305858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ramanan VK, Risacher SL, Nho K, Kim S, Swaminathan S, Shen L, et al. APOE and BCHE as modulators of cerebral amyloid deposition: a florbetapir PET genome-wide association study. Mol Psychiatry. 2014;19:351–357. doi: 10.1038/mp.2013.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Scelsi MA, Khan RR, Lorenzi M, Christopher L, Greicius MD, Schott JM, et al. Genetic study of multimodal imaging Alzheimer’s disease progression score implicates novel loci. Brain. 2018;141:2167–2180. doi: 10.1093/brain/awy141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Li J, Chen F, Zhang Q, Meng X, Yao X, Risacher SL, et al. Genome-wide network-assisted association and enrichment study of amyloid imaging phenotype in Alzheimer’s disease. Curr Alzheimer Res. 2019;16:1163–1174. doi: 10.2174/1567205016666191121142558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kim HR, Jung SH, Kim J, Jang H, Kang SH, Hwangbo S, et al. Identifying novel genetic variants for brain amyloid deposition: a genome-wide association study in the Korean population. Alzheimers Res Ther. 2021;13(1):117. doi: 10.1186/s13195-021-00854-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liu H, Lutz M, Luo S, Alzheimer’s Disease Neuroimaging Initiative. Association between polygenic risk score and the progression from mild cognitive impairment to Alzheimer’s disease. J Alzheimers Dis. 2021;84(3):1323–35 [DOI] [PMC free article] [PubMed]
- 83.Smith R, Puschmann A, Schöll M, Ohlsson T, Van Swieten J, Honer M, et al. 18F-AV-1451 tau PET imaging correlates strongly with tau neuropathology in MAPT mutation carriers. Brain. 2016;139:2372–9. doi: 10.1093/brain/aww163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mattsson N, Ossenkoppele R, Smith R, Strandberg O, Ohlsson T, Jögi J, et al. Greater tau load and reduced cortical thickness in APOE ε4-negative Alzheimer’s disease: a cohort study. Alzheimer’s Res Ther. 2018;10:77. doi: 10.1186/s13195-018-0403-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shen XN, Miao D, Li JQ, Tan CC, Cao XP, Tan L, et al. MAPT rs242557 variant is associated with hippocampus tau uptake on 18 F-AV-1451 PET in non-demented elders. Aging (Albany NY) 2019;11:874–884. doi: 10.18632/aging.101783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Therriault J, Benedet AL, Pascoal TA, Mathotaarachchi S, Chamoun M, Savard M, et al. Association of apolipoprotein E ε4 with medial temporal tau independent of amyloid-β. JAMA Neurol. 2020;77:470–479. doi: 10.1001/jamaneurol.2019.4421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Franzmeier N, Rubinski A, Neitzel J, Ewers M, Morris J, Raichle M, et al. The BIN1 rs744373 SNP is associated with increased tau-PET levels and impaired memory. Nat Commun. 2019;10(1):1766. doi: 10.1038/s41467-019-09564-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yan S, Zheng C, Paranjpe MD, Li J, Benzinger TLS, Lu J, et al. Association of sex and APOE ε4 with brain tau deposition and atrophy in older adults with Alzheimer’s disease. Theranostics. 2020;10:10563–10572. doi: 10.7150/thno.48522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Neitzel J, Franzmeier N, Rubinski A, Binette AP, Poirier J, Villeneuve S, et al. ApoE4 associated with higher tau accumulation independent of amyloid burden. Alzheimer’s Dement. 2020;16:e046206. doi: 10.1002/alz.046206. [DOI] [Google Scholar]
- 90.Franzmeier N, Ossenkoppele R, Brendel M, Rubinski A, Smith R, Kumar A, et al. The BIN1 rs744373 Alzheimer’s disease risk SNP is associated with faster Aβ-associated tau accumulation and cognitive decline. Alzheimer’s Dement. 2022;18(1):103–115. doi: 10.1002/alz.12371. [DOI] [PubMed] [Google Scholar]
- 91.Neitzel J, Franzmeier N, Rubinski A, Dichgans M, Brendel M, Weiner M, et al. KL-VS heterozygosity is associated with lower amyloid-dependent tau accumulation and memory impairment in Alzheimer’s disease. Nat Commun. 2021;12(1):3825. doi: 10.1038/s41467-021-23755-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sun Y, Wang M, Zhao Y, Hu K, Liu Y, Liu B. A Pathway-specific polygenic risk score is associated with tau pathology and cognitive decline. J Alzheimer’s Dis. 2022;85:1745–1754. doi: 10.3233/JAD-215163. [DOI] [PubMed] [Google Scholar]
- 93.Lunetta KL, Erlich PM, Cuenco KT, Adrienne Cupples L, Green RC, Farrer LA, et al. Heritability of magnetic resonance imaging (MRI) traits in Alzheimer disease cases and their siblings in the MIRAGE study. Alzheimer Dis Assoc Disord. 2007;21:85–91. doi: 10.1097/WAD.0b013e3180653bf7. [DOI] [PubMed] [Google Scholar]
- 94.Potkin SG, Guffanti G, Lakatos A, Turner JA, Kruggel F, Fallon JH, et al. Hippocampal atrophy as a quantitative trait in a genome-wide association study identifying novel susceptibility genes for Alzheimer’s disease. PLoS ONE. 2009;4:e6501. doi: 10.1371/journal.pone.0006501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wolk DA, Dickerson BC. Apolipoprotein E (APOE) genotype has dissociable effects on memory and attentional-executive network function in Alzheimer’s disease. Proc Natl Acad Sci U S A. 2010;107:10256–10261. doi: 10.1073/pnas.1001412107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Biffi A, Anderson CD, Desikan RS, Sabuncu M, Cortellini L, Schmansky N, et al. Genetic Variation and neuroimaging measures in Alzheimer disease. Arch Neurol. 2010;67(6):677–685. doi: 10.1001/archneurol.2010.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Meda SA, Koran MEI, Pryweller JR, Vega JN, Thornton-Wells TA. Genetic interactions associated with 12-month atrophy in hippocampus and entorhinal cortex in Alzheimer’s disease neuroimaging initiative. Neurobiol Aging. 2013;34:1518.e9–1518.e18. doi: 10.1016/j.neurobiolaging.2012.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jahanshad N, Rajagopalan P, Hua X, Hibar DP, Nir TM, Toga AW, et al. Genome-wide scan of healthy human connectome discovers SPON1 gene variant influencing dementia severity. Proc Natl Acad Sci U S A. 2013;110:4768–4773. doi: 10.1073/pnas.1216206110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Morgen K, Ramirez A, Froelich L, Tost H, Plichta MM, Koelsch H, et al. Genetic interaction of PICALM and APOE is associated with brain atrophy and cognitive impairment in Alzheimer’s disease. Alzheimers Dement. 2014;10:S269–S276. doi: 10.1016/j.jalz.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 100.Hohman TJ, Koran MEI, Thornton-Wells TA. Genetic variation modifies risk for neurodegeneration based on biomarker status. Front Aging Neurosci. 2014;6:183. doi: 10.3389/fnagi.2014.00183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chauhan G, Adams HHH, Bis JC, Weinstein G, Yu L, Töglhofer AM, et al. Association of Alzheimer’s disease GWAS loci with MRI markers of brain aging. Neurobiol Aging. 2015;36:1765.e7–1765.e16. doi: 10.1016/j.neurobiolaging.2014.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Desikan RS, Fan CC, Wang Y, Schork AJ, Cabral HJ, Cupples LA, et al. Genetic assessment of age-associated Alzheimer disease risk: development and validation of a polygenic hazard score. PLoS Med. 2017;14:e1002258. doi: 10.1371/journal.pmed.1002258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yang X, Li J, Liu B, Li Y, Jiang T. Impact of PICALM and CLU on hippocampal degeneration. Hum Brain Mapp. 2016;37:2419–2430. doi: 10.1002/hbm.23183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ramirez LM, Goukasian N, Porat S, Hwang KS, Eastman JA, Hurtz S, et al. Common variants in ABCA7 and MS4A6A are associated with cortical and hippocampal atrophy. Neurobiol Aging. 2016;39:82–89. doi: 10.1016/j.neurobiolaging.2015.10.037. [DOI] [PubMed] [Google Scholar]
- 105.Habes M, Toledo JB, Resnick SM, Doshi J, Van Der Auwera S, Erus G, et al. Relationship between APOE genotype and structural MRI measures throughout adulthood in the study of health in pomerania population-based cohort. Am J Neuroradiol. 2016;37:1636–1642. doi: 10.3174/ajnr.A4805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Foley SF, Tansey KE, Caseras X, Lancaster T, Bracht T, Parker G, et al. Multimodal brain imaging reveals structural differences in Alzheimer’s disease polygenic risk carriers: a study in healthy young adults. Biol Psychiatry. 2017;81:154–161. doi: 10.1016/j.biopsych.2016.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Harrison TM, Mahmood Z, Lau EP, Karacozoff AM, Burggren AC, Small GW, et al. An Alzheimer’s disease genetic risk score predicts longitudinal thinning of hippocampal complex subregions in healthy older adults. eNeuro. 2016;3:795–804. doi: 10.1523/ENEURO.0098-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wang ZX, Wan Y, Tan L, Liu J, Wang HF, Sun FR, et al. Genetic association of HLA gene variants with MRI brain structure in Alzheimer’s disease. Mol Neurobiol. 2017;54(5):3195–3204. doi: 10.1007/s12035-016-9889-z. [DOI] [PubMed] [Google Scholar]
- 109.Wang ZX, Wang HF, Tan L, Sun FR, Tan MS, Tan CC, et al. HLA-A2 alleles mediate Alzheimer’s disease by altering hippocampal volume. Mol Neurobiol. 2017;54:2469–2476. doi: 10.1007/s12035-016-9832-3. [DOI] [PubMed] [Google Scholar]
- 110.Xiao E, Chen Q, Goldman AL, Tan HY, Healy K, Zoltick B, et al. Late-onset Alzheimer’s disease polygenic risk profile score predicts hippocampal function. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2:673–679. doi: 10.1016/j.bpsc.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 111.Axelrud LK, Santoro ML, Pine DS, Talarico F, Gadelha A, Manfro GG, et al. Polygenic risk score for Alzheimer’s disease: implications for memory performance and hippocampal volumes in early life. Am J Psychiatry. 2018;175:555–563. doi: 10.1176/appi.ajp.2017.17050529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li J, Zhang X, Li A, Liu S, Qin W, Yu C, et al. Polygenic risk for Alzheimer’s disease influences precuneal volume in two independent general populations. Neurobiol Aging. 2018;64:116–122. doi: 10.1016/j.neurobiolaging.2017.12.022. [DOI] [PubMed] [Google Scholar]
- 113.Lancaster TM, Hill MJ, Sims R, Williams J. Microglia: Mediated immunity partly contributes to the genetic association between Alzheimer’s disease and hippocampal volume. Brain Behav Immun. 2019;79:267–273. doi: 10.1016/j.bbi.2019.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lyall DM, Cox SR, Lyall LM, Celis-Morales C, Cullen B, Mackay DF, et al. Association between APOE e4 and white matter hyperintensity volume, but not total brain volume or white matter integrity. Brain Imaging Behav. 2020;14:1468–1476. doi: 10.1007/s11682-019-00069-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Cong S, Yao X, Huang Z, Risacher SL, Nho K, Saykin AJ, et al. Volumetric GWAS of medial temporal lobe structures identifies an ERC1 locus using ADNI high-resolution T2-weighted MRI data. Neurobiol Aging. 2020;95:81–93. doi: 10.1016/j.neurobiolaging.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.De Marco M, Manca R, Kirby J, Hautbergue GM, Blackburn DJ, Wharton SB, et al. The association between polygenic hazard and markers of Alzheimer’s disease following stratification for APOE genotype. Curr Alzheimer Res. 2020;17(7):667–679. doi: 10.2174/1567205017666201006161800. [DOI] [PubMed] [Google Scholar]
- 117.van der Meer D, Rokicki J, Kaufmann T, Córdova-Palomera A, Moberget T, Alnæs D, et al. Brain scans from 21,297 individuals reveal the genetic architecture of hippocampal subfield volumes. Mol Psychiatry. 2020;25(11):3053–3065. doi: 10.1038/s41380-018-0262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Foo H, Thalamuthu A, Jiang J, Koch F, Mather KA, Wen W, et al. Associations between Alzheimer’s disease polygenic risk scores and hippocampal subfield volumes in 17,161 UK Biobank participants. Neurobiol Aging. 2021;98:108–115. doi: 10.1016/j.neurobiolaging.2020.11.002. [DOI] [PubMed] [Google Scholar]
- 119.Tank R, Ward J, Flegal KE, Smith DJ, Bailey MES, Cavanagh J, et al. Association between polygenic risk for Alzheimer’s disease, brain structure and cognitive abilities in UK Biobank. Neuropsychopharmacology. 2022;47:564–569. doi: 10.1038/s41386-021-01190-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Corneveaux JJ, Liang WS, Reiman EM, Webster JA, Myers AJ, Zismann VL, et al. Evidence for an association between KIBRA and late-onset Alzheimer’s disease. Neurobiol Aging. 2010;31:901–909. doi: 10.1016/j.neurobiolaging.2008.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Miller JE, Shivakumar MK, Lee Y, Han S, Horgousluoglu E, Risacher SL, et al. Rare variants in the splicing regulatory elements of EXOC3L4 are associated with brain glucose metabolism in Alzheimer’s disease. BMC Med Genom. 2018;11:76. doi: 10.1186/s12920-018-0390-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kong L-L, Miao D, Tan L, Liu S-L, Li J-Q, Cao X-P, et al. Genome-wide association study identifies RBFOX1 locus influencing brain glucose metabolism. Ann Transl Med. 2018;6:436. doi: 10.21037/atm.2018.07.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Seo J, Byun MS, Yi D, Lee JH, Jeon SY, Shin SA, et al. Genetic associations of in vivo pathology influence Alzheimer’s disease susceptibility. Alzheimer’s Res Ther. 2020;12:156. doi: 10.1186/s13195-020-00722-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wang RZ, Yang YX, Li HQ, Shen XN, Chen SD, Dong Q, et al. Genome-wide association study of brain Alzheimer’s disease-related metabolic decline as measured by [18F] FDG-PET imaging. J Alzheimers Dis. 2020;77:401–409. doi: 10.3233/JAD-200415. [DOI] [PubMed] [Google Scholar]
- 125.Bookheimer SY, Strojwas MH, Cohen MS, Saunders AM, Pericak-Vance MA, Mazziotta JC, et al. Patterns of brain activation in people at risk for Alzheimer’s disease. N Engl J Med. 2000;343(7):450–6. [DOI] [PMC free article] [PubMed]
- 126.Erk S, Meyer-Lindenberg A, von Boberfeld CO, Esslinger C, Schnell K, Kirsch P, et al. Hippocampal function in healthy carriers of the CLU Alzheimer’s disease risk variant. J Neurosci. 2011;31:18180–18184. doi: 10.1523/JNEUROSCI.4960-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lancaster TM, Baird A, Wolf C, Jackson MC, Johnston SJ, Donev R, et al. Neural hyperactivation in carriers of the Alzheimer’s risk variant on the clusterin gene. Eur Neuropsychopharmacol. 2011;21:880–884. doi: 10.1016/j.euroneuro.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 128.Green AE, Gray JR, DeYoung CG, Mhyre TR, Padilla R, DiBattista AM, et al. A combined effect of two Alzheimer’s risk genes on medial temporal activity during executive attention in young adults. Neuropsychologia. 2014;56:1–8. doi: 10.1016/j.neuropsychologia.2013.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Guerini FR, Agliardi C, Sironi M, Arosio B, Calabrese E, Zanzottera M, et al. Possible association between SNAP-25 single nucleotide polymorphisms and alterations of categorical fluency and functional MRI parameters in Alzheimer’s disease. J Alzheimer’s Dis. 2014;42:1015–1028. doi: 10.3233/JAD-140057. [DOI] [PubMed] [Google Scholar]
- 130.Liu X, Bai F, Yue C, Shi Y, Yu H, Luo B, et al. The association between TOMM40 gene polymorphism and spontaneous brain activity in amnestic mild cognitive impairment. J Neurol. 2014;261:1499–1507. doi: 10.1007/s00415-014-7368-x. [DOI] [PubMed] [Google Scholar]
- 131.Lancaster TM, Brindley LM, Tansey KE, Sims RC, Mantripragada K, Owen MJ, et al. Alzheimer’s disease risk variant in CLU is associated with neural inefficiency in healthy individuals. Alzheimer’s Dement. 2015;11:1144–1152. doi: 10.1016/j.jalz.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 132.Zhang X, Yu JT, Li J, Wang C, Tan L, Liu B, et al. Bridging integrator 1 (BIN1) genotype effects on working memory, hippocampal volume, and functional connectivity in young healthy individuals. Neuropsychopharmacology. 2015;40:1794–1803. doi: 10.1038/npp.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sun DM, Chen HF, Zuo QL, Su F, Bai F, Liu CF. Effect of PICALM rs3851179 polymorphism on the default mode network function in mild cognitive impairment. Behav Brain Res. 2017;331:225–232. doi: 10.1016/j.bbr.2017.05.043. [DOI] [PubMed] [Google Scholar]
- 134.Su F, Shu H, Ye Q, Xie C, Yuan B, Zhang Z, et al. Integration of multilocus genetic risk into the default mode network longitudinal trajectory during the Alzheimer’s disease process. J Alzheimer’s Dis. 2017;56:491–507. doi: 10.3233/JAD-160787. [DOI] [PubMed] [Google Scholar]
- 135.Korthauer LE, Zhan L, Ajilore O, Leow A, Driscoll I. Disrupted topology of the resting state structural connectome in middle-aged APOE ε4 carriers. Neuroimage. 2018;178:295–305. doi: 10.1016/j.neuroimage.2018.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Franzmeier N, Ren J, Damm A, Monté-Rubio G, Boada M, Ruiz A, et al. The BDNFVal66Met SNP modulates the association between beta-amyloid and hippocampal disconnection in Alzheimer’s disease. Mol Psychiatry. 2021;26:614–628. doi: 10.1038/s41380-019-0404-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chandler HL, Wise RG, Murphy K, Tansey KE, Linden DEJ, Lancaster TM. Polygenic impact of common genetic risk loci for Alzheimer’s disease on cerebral blood flow in young individuals. Sci Rep. 2019;9:467. doi: 10.1038/s41598-018-36820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Axelrud LK, Sato JR, Santoro ML, Talarico F, Pine DS, Rohde LA, et al. Genetic risk for Alzheimer’s disease and functional brain connectivity in children and adolescents. Neurobiol Aging. 2019;82:10–17. doi: 10.1016/j.neurobiolaging.2019.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chandler HL, Hodgetts CJ, Caseras X, Murphy K, Lancaster TM. Polygenic risk for Alzheimer’s disease shapes hippocampal scene-selectivity. Neuropsychopharmacology. 2020;45:1171–1178. doi: 10.1038/s41386-019-0595-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Smith CD, Chebrolu H, Andersen AH, Powell DA, Lovell MA, Xiong S, et al. White matter diffusion alterations in normal women at risk of Alzheimer’s disease. Neurobiol Aging. 2010;31:1122–1131. doi: 10.1016/j.neurobiolaging.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Nierenberg J, Pomara N, Hoptman MJ, Sidtis JJ, Ardekani BA, Lim KO. Abnormal white matter integrity in healthy apolipoprotein E epsilon4 carriers. NeuroReport. 2005;16(12):1369–1372. doi: 10.1097/01.wnr.0000174058.49521.16. [DOI] [PubMed] [Google Scholar]
- 142.Warstadt NM, Dennis EL, Jahanshad N, Kohannim O, Nir TM, Mcmahon KL, et al. Serum cholesterol and variant in cholesterol-related gene CETP predict white matter microstructure and for the Alzheimer’s disease neuroimaging initiative (ADNI) Neurobiol Aging. 2014;35:2504–2513. doi: 10.1016/j.neurobiolaging.2014.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Liang Y, Li H, Lv C, Shu N, Chen K, Li X, et al. Sex moderates the effects of the Sorl1 gene rs2070045 polymorphism on cognitive impairment and disruption of the cingulum integrity in healthy elderly. Neuropsychopharmacology. 2015;40:1519–1527. doi: 10.1038/npp.2015.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cavedo E, Lista S, Rojkova K, Chiesa PA, Houot M, Brueggen K, et al. Disrupted white matter structural networks in healthy older adult APOE ε4 carriers: an international multicenter DTI study. Neuroscience. 2017;357:119–133. doi: 10.1016/j.neuroscience.2017.05.048. [DOI] [PubMed] [Google Scholar]
- 145.Rutten-Jacobs LCA, Tozer DJ, Duering M, Malik R, Dichgans M, Markus HS, et al. Genetic study of white matter integrity in UK Biobank (N = 8448) and the overlap with stroke, depression, and dementia. Stroke. 2018;49:1340–1347. doi: 10.1161/STROKEAHA.118.020811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gu X, Chu T, Liu L, Han X. Genetic influences on white matter and metabolism abnormal change in Alzheimer’s disease: Meta-analysis for neuroimaging research on presenilin 1 mutation. Clin Neurol Neurosurg. 2019;177:47–53. doi: 10.1016/j.clineuro.2018.12.016. [DOI] [PubMed] [Google Scholar]
- 147.Yan J, Raja V, Huang Z, Amico E, Nho K, Fang S. Brain-wide structural connectivity alterations under the control of Alzheimer risk genes. Int J Comput Biol Drug Des. 2020;13:58–70. doi: 10.1504/IJCBDD.2020.105098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Horgusluoglu-Moloch E, Xiao G, Wang M, Wang Q, Zhou X, Nho K, et al. Systems modeling of white matter microstructural abnormalities in Alzheimer’s disease. NeuroImage Clin. 2020;26:102203. doi: 10.1016/j.nicl.2020.102203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yan Q, Nho K, Del-Aguila JL, Wang X, Risacher SL, Fan KH, et al. Genome-wide association study of brain amyloid deposition as measured by Pittsburgh compound-B (PiB)-PET imaging. Mol Psychiatry. 2021;26:309–321. doi: 10.1038/s41380-018-0246-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Initi ADN, Ramanan VK, Risacher SL, Nho K, Kim S, Swaminathan S, et al. APOE and BCHE as modulators of cerebral amyloid deposition: a florbetapir PET genome-wide association study. Mol Psychiatry. 2014;19:351–357. doi: 10.1038/mp.2013.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Tan CH, Bonham LW, Fan CC, Mormino EC, Sugrue LP, Broce IJ, et al. Polygenic hazard score, amyloid deposition and Alzheimer’s neurodegeneration. Brain. 2019;142:460–470. doi: 10.1093/brain/awy327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ramanan VK, Wang XK, Przybelski SA, Pillai SKR, Kosel ML, Batzler AK, et al. Genome-wide association study of tau-PET: association of variant near NTNG2 with resistance to tau deposition. Alzheimer’s Dement. 2020;16:e044321. [Google Scholar]
- 153.Risacher SL, Kim S, Shen L, Nho K, Foroud T, Green RC, et al. The role of apolipoprotein E (APOE) genotype in early mild cognitive impairment (E-MCI) Front Aging Neurosci. 2013;5:11. doi: 10.3389/fnagi.2013.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.De Velasco OJ, Vallejo EE, Estrada K, Taméz Peña JG. Disease neuroimaging initiative TA. Benchmarking machine learning models for late-onset Alzheimer’s disease prediction from genomic data. BMC Bioinf. 2019;20:709. doi: 10.1186/s12859-019-3158-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Gray KR, Aljabar P, Heckemann RA, Hammers A, Rueckert D. Random forest-based similarity measures for multi-modal classification of Alzheimer’s disease. Neuroimage. 2013;65:167–175. doi: 10.1016/j.neuroimage.2012.09.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kohannim O, Hua X, Hibar DP, Lee S, Chou YY, Toga AW, et al. Boosting power for clinical trials using classifiers based on multiple biomarkers. Neurobiol Aging. 2010;31:1429–1442. doi: 10.1016/j.neurobiolaging.2010.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Dukart J, Sambataro F, Bertolino A. Accurate prediction of conversion to Alzheimer’s disease using imaging, genetic, and neuropsychological biomarkers. J Alzheimer’s Dis. 2015;49:1143–1159. doi: 10.3233/JAD-150570. [DOI] [PubMed] [Google Scholar]
- 158.Bi XA, Cai R, Wang Y, Liu Y. Effective diagnosis of Alzheimer’s disease via multimodal fusion analysis framework. Front Genet. 2019;10:976. doi: 10.3389/fgene.2019.00976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Varol E, Sotiras A, Davatzikos C. HYDRA: Revealing heterogeneity of imaging and genetic patterns through a multiple max-margin discriminative analysis framework. Neuroimage. 2017;145:346–364. doi: 10.1016/j.neuroimage.2016.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Liu Y, Li Z, Ge Q, Lin N, Xiong M. Deep feature selection and causal analysis of Alzheimer’s disease. Front Neurosci. 2019;13:1198. doi: 10.3389/fnins.2019.01198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Spasov S, Passamonti L, Duggento A, Liò P, Toschi N. A parameter-efficient deep learning approach to predict conversion from mild cognitive impairment to Alzheimer’s disease. Neuroimage. 2019;189:276–287. doi: 10.1016/j.neuroimage.2019.01.031. [DOI] [PubMed] [Google Scholar]
- 162.Zhou T, Thung KH, Zhu X, Shen D. Feature learning and fusion of multimodality neuroimaging and genetic data for multi-status dementia diagnosis. Mach Learn Med Imaging. 2017;10541:132–140. doi: 10.1007/978-3-319-67389-9_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Shigemizu D, Akiyama S, Higaki S, Sugimoto T, Sakurai T, Boroevich KA, et al. Prognosis prediction model for conversion from mild cognitive impairment to Alzheimer’s disease created by integrative analysis of multi-omics data. Alzheimer’s Res Ther. 2020;12(1):145. doi: 10.1186/s13195-020-00716-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zhang Z, Huang H, Shen D. Integrative analysis of multi-dimensional imaging genomics data for Alzheimer’s disease prediction. Front Aging Neurosci. 2014;6:260. doi: 10.3389/fnagi.2014.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.An L, Adeli E, Liu M, Zhang J, Lee SW, Shen D. A Hierarchical feature and sample selection framework and its application for Alzheimer’s disease diagnosis. Sci Rep. 2017;7:45269. doi: 10.1038/srep45269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Leonenko G, Shoai M, Bellou E, Sims R, Williams J, Hardy J, et al. Genetic risk for Alzheimer disease is distinct from genetic risk for amyloid deposition. Ann Neurol. 2019;86:427–435. doi: 10.1002/ana.25530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gupta Y, Kim JI, Kim BC, Kwon GR. Classification and graphical analysis of Alzheimer’s disease and its prodromal stage using multimodal features from structural, diffusion, and functional neuroimaging data and the APOE genotype. Front Aging Neurosci. 2020;12:238. doi: 10.3389/fnagi.2020.00238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Saeed U, Mirza SS, MacIntosh BJ, Herrmann N, Keith J, Ramirez J, et al. APOE-ε4 associates with hippocampal volume, learning, and memory across the spectrum of Alzheimer’s disease and dementia with Lewy bodies. Alzheimer’s Dement. 2018;14:1137–1147. doi: 10.1016/j.jalz.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 169.Zhang C, Kong M, Wei H, Zhang H, Ma G, Ba M. The effect of ApoE ε 4 on clinical and structural MRI markers in prodromal Alzheimer’s disease. Quant Imaging Med Surg. 2020;10:464–474. doi: 10.21037/qims.2020.01.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Weigand AJ, Thomas KR, Bangen KJ, Eglit GML, Delano-Wood L, Gilbert PE, et al. APOE interacts with tau PET to influence memory independently of amyloid PET in older adults without dementia. Alzheimer’s Dement. 2021;17:61–69. doi: 10.1002/alz.12173. [DOI] [PubMed] [Google Scholar]
- 171.Carter CS, Bearden CE, Bullmore ET, Geschwind DH, Glahn DC, Gur RE, et al. Enhancing the informativeness and replicability of imaging genomics studies. Biol Psychiatry. 2017;82:157–164. doi: 10.1016/j.biopsych.2016.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Sepulcre J, Grothe MJ, d’Oleire Uquillas F, Ortiz-Terán L, Diez I, Yang HS, et al. Neurogenetic contributions to amyloid beta and tau spreading in the human cortex. Nat Med. 2018;24:1910–1918. doi: 10.1038/s41591-018-0206-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kelley DR, Snoek J, Rinn JL. Basset: learning the regulatory code of the accessible genome with deep convolutional neural networks. Genome Res. 2016;26:990–999. doi: 10.1101/gr.200535.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhou J, Troyanskaya OG. Predicting effects of noncoding variants with deep learning-based sequence model. Nat Methods. 2015;12:931–934. doi: 10.1038/nmeth.3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Alipanahi B, Delong A, Weirauch MT, Frey BJ. Predicting the sequence specificities of DNA- and RNA-binding proteins by deep learning. Nat Biotechnol. 2015;33:831–838. doi: 10.1038/nbt.3300. [DOI] [PubMed] [Google Scholar]
- 176.Li L, Yang Y, Zhang Q, Wang J, Jiang J. Use of deep-learning genomics to discriminate healthy individuals from those with Alzheimer’s disease or mild cognitive impairment. Behav Neurol. 2021;2021:3359103. doi: 10.1155/2021/3359103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Bai B, Vanderwall D, Li Y, Wang X, Poudel S, Wang H, et al. Proteomic landscape of Alzheimer’s disease: novel insights into pathogenesis and biomarker discovery. Mol Neurodegener. 2021;16(1):55. doi: 10.1186/s13024-021-00474-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Garcés P, Vicente R, Wibral M, Pineda-Pardo J, López ME, Aurtenetxe S, et al. Brain-wide slowing of spontaneous alpha rhythms in mild cognitive impairment. Front Aging Neurosci. 2013;5:100. doi: 10.3389/fnagi.2013.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Fernández A, Hornero R, Mayo A, Poza J, Gil-Gregorio P, Ortiz T. MEG spectral profile in Alzheimer’s disease and mild cognitive impairment. Clin Neurophysiol. 2006;117:306–314. doi: 10.1016/j.clinph.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 180.López-Sanz D, Bruña R, Garcés P, Martín-Buro MC, Walter S, Delgado ML, et al. Functional connectivity disruption in subjective cognitive decline and mild cognitive impairment: a common pattern of alterations. Front Aging Neurosci. 2017;9:109. doi: 10.3389/fnagi.2017.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Babiloni C, Benussi L, Binetti G, Bosco P, Busonero G, Cesaretti S, et al. Genotype (cystatin C) and EEG phenotype in Alzheimer disease and mild cognitive impairment: a multicentric study. Neuroimage. 2006;29:948–964. doi: 10.1016/j.neuroimage.2005.08.030. [DOI] [PubMed] [Google Scholar]
- 182.Ponomareva NV, Andreeva TV, Protasova MS, Shagam LI, Malina DD, Goltsov AY, et al. Quantitative EEG during normal aging: association with the Alzheimer’s disease genetic risk variant in PICALM gene. Neurobiol Aging. 2017;51:177.e1–177.e8. doi: 10.1016/j.neurobiolaging.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 183.Ponomareva N, Andreeva T, Protasova M, Konovalov R, Krotenkova M, Malina D, et al. Genetic association between Alzheimer’s disease risk variant of the PICALM gene and EEG functional connectivity in non-demented adults. Front Neurosci. 2020;14:324. doi: 10.3389/fnins.2020.00324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.De PVG, Gómez C, Poza J, Maturana-Candelas A, Martins S, Gomes I, et al. Relationship between the presence of the ApoE ε4 allele and EEG complexity along the Alzheimer’s disease continuum. Sensors (Basel) 2020;20:3849. doi: 10.3390/s20143849. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy for literature.
Data Availability Statement
Not applicable.