Abstract
Objective
To systematically evaluate the clinical effect of Xiaoke Decoction in the treatment of type 2 diabetes.
Methods
Chinese databases such as CNKI, Wanfang, Weipu Chinese Biomedical Journal Database, and Chinese Medical Biological Literature Database, PubMed, Cochrane Library, Embase, and Web of Science were searched for English language literature from their inception until November 2019. A Meta-analysis was performed using RevMan 5.3 and Stata 12.0.
Results
Thirty-eight studies were included in this study, with a total of 3757 patients. It was found that adding Xiaoke Decoction could improve total efficiency. The Xiaoke Decoction groups surpassed the western medicine groups regarding improvement in total efficiency (OR = 3.49; 95% CI: 2.78–4.39, P < 0.00001). Adding Xiaoke Decoction could lower the fasting plasma glucose (FPG) level. The Xiaoke Decoction groups surpassed the western medicine groups regarding reduction in FPG levels (MD = −1.14; 95% CI: −1.36 to 0.92, P < 0.00001). Adding Xiaoke Decoction could lower the 2 h postprandial blood glucose (2hPG) level. The Xiaoke Decoction groups surpassed the western medicine groups regarding reduction in 2hPG (MD = −1.40; 95% CI: −1.61 to 1.19, P < 0.00001). Adding Xiaoke Decoction could lower glycated hemoglobin (HbA1c). The Xiaoke Decoction groups surpassed the western medicine groups regarding reduction in HbA1c (MD = −0.77; 95% CI: −0.95 to 0.58, P < 0.00001). It was found that adding Xiaoke Decoction could lower the traditional Chinese medicine (TCM) syndrome score. The TCM syndrome scores among patients in the Xiaoke Decoction group were lower than those among patients in the control group after treatment (MD = −4.90; 95% CI: −7.22 to 2.57, P < 0.0001). At the same time, we conducted a subgroup and sensitivity analysis of age and intervention duration on the heterogeneity of total efficiency, FPG, 2hPG, HbAlc, and TCM syndrome score outcome indicators. For detecting publication bias, an egger test was conducted.
Conclusion
Compared with western medicine alone, Xiaoke Decoction has more advantages for the treatment of type 2 diabetes with respect to total efficiency, FPG, 2hPG, HbAlc, and TCM syndrome score.
Keywords: Meta-analysis, type II diabetes, Xiaoke Decoction
1. Introduction
Diabetes is a metabolic endocrine disease characterized by high blood glucose concentration. Type 2 diabetes accounts for more than 90% of all diabetes patients and has a very high incidence worldwide. It is characterized by either absolute or relative insufficient insulin secretion (impaired insulin secretion) or decreased sensitivity of the target organs or tissues to insulin (insulin resistance) (Chinese Medical Association Diabetes Branch, 2017). It is often accompanied by a variety of chronic complications, thereby causing severe damage to multiple organ systems in the body (Zhang & Jiang, 2012). In 2017, the World Diabetes Federation reported that there were approximately 451 million diabetes patients worldwide and is expected to soar to 693 million in 2045. In recent years, the number of diabetes patients in China has increased dramatically, and diabetes has become the third most common disease after cardiovascular diseases and tumors. At present, type 2 diabetes is mostly managed using western medicine. Treatment methods are mostly oral hypoglycemic drugs or insulin injections. Western medicine alone has obvious hypoglycemic effects. However, long-term use is likely to cause liver and kidney damage, and the effect of improving certain complications is not obvious. Traditional Chinese medicine (TCM) has been used for thousands of years in China and plays an important role in medical care. Since ancient times, several Chinese herbs and herbal formulas have been widely used to treat diabetes (Gong, Ji, & Xu, 2019). TCM has its unique advantages in the treatment process. It is characterized by wide sources, convenient material collection, simple production, easy storage, low price, and small side effects. Thus, it has become widely used in the treatment of diabetes.
In TCM, diabetes belongs to the category of “Xiaoke” and has the appellation, eliminate sensation of spleen, eliminate medium, and so on. The treatment principle is to clear heat, moisten dryness, nourish yin, and produce fluid. The Xiaoke Decoction comes from the “Danxi’s Experimental Therapy” (Danxi Xinfa in Chinese) of Dan xi Zhu, which was composed of Coptidis Rhizoma, Trichosanthis Radix, Lotus Rhizoma, Rehmanniae Radix, Zingiberis Recens Rhizoma, Mel, human milk (or cow's milk) among others. Moreover, Xiaoke Decoction and its derivative prescriptions showed their beneficial efficacy in treating type 2 diabetes. Only by eliminating thirst can effectively reduce oxidative stress response, improve islet function, and enhance insulin sensitivity in patients. The efficacy of the prescription has been widely recognized (Jin & Jin, 2019). We comprehensively searched domestic and foreign literatures for randomized clinical control trials on the treatment of type 2 diabetes using Xiaoke Decoction, and assessed the treatment of type 2 diabetes by means of Meta-analysis. This study aims to comprehensively evaluate the effectiveness and safety of Xiaoke Decoction for the treatment of type 2 diabetes.
2. Materials and methods
2.1. Inclusion and exclusion criteria
The included literatures met the following criteria: (1) Type of study: Randomized control trial of Xiaoke Decoction for the treatment of type 2 diabetes, regardless of the method of allocation and concealment used; (2) No limit on the sample size: All the selected candidates met the diagnostic criteria listed in the Guidelines for the Prevention and Treatment of Type 2 Diabetes in China (2017 Edition), (Chinese Diabetes Society, 2018); (3) Interventions: patients in the experimental group were given Xiaoke Decoction plus or minus, or combined with hypoglycemic drugs or insulin. Patients in the control group were treated with hypoglycemic drugs or insulin; and (4) Outcome indicators: At least one or more times of the total effective rate (Ministry of Health, 2002), fasting plasma glucose (FPG), 2h postprandial blood glucose level (2h-PBG), glycated hemoglobin (HbA1c), and TCM syndrome score (Diabetes Branch of Chinese Medical Association, 2017).
Documents with the following characteristics were excluded: (1) Non-compliance with the diagnostic criteria; (2) The use of other efficacy evaluation indicators; (3) The original data were unpublished literature or conference articles, animal experiments, reviews, and so on; (4) Original literature was a non-clinical randomized control experiment; And (5) the original literature trial design was not rigorous with no control group.
2.2. Literature search
We searched academic Chinese databases such as CNKI, Wanfang, Chinese Biomedical Journal Database (CMJD), Chinese Medical and Biological Literature Database (CBM), and those in foreign languages such as PubMed, Cochrane Library, Embase, and Web of Science. The retrieval time for each database was set from the time of inception to November 2019. The Chinese search terms used were “Xiaoke Decoction”, “type 2 diabetes”, “clinical observation”, “random”, and so on. The English search terms used were “Xiaoke Decoction”, “type 2 diabetes mellitus”, “clinical observation”, and “random”. We searched for relevant literature that may have met the criteria.
2.3. Literature screening and quality evaluation
The downloaded documents were screened and evaluated by the two researchers in accordance to the established inclusion and exclusion criteria. The titles and abstracts of all documents were further read to eliminate duplicates and to exclude those that clearly did not meet the inclusion criteria. When the preliminary determination that the text may meet the inclusion criteria was made, we read the full text of the literature and selected articles that met the inclusion criteria. When the opinions of the two researchers were not unified, discussions and consultations were conducted or a third researcher could have been invited to jointly resolve the problem.
2.4. Statistical methods
Count data are presented as odds ratios (ORs), and measurement data as the weighted average value (MD) or standardized mean difference (SMD) and its 95% confidence interval (CI). Heterogeneity among the included studies was analyzed using the χ2 test. In the test of heterogeneity, P > 0.10 and I2 < 50% indicated that there was no statistical heterogeneity among the studies and that a fixed-effects model was used for analysis. Otherwise, a random-effects model was used. An inverted funnel plot was used to assess publication bias based on the main blood glucose indicators and TCM syndrome scores. Meta-analysis was performed using RevMan 5.3 and Stata 12.0. Items with P < 0.05 were considered statistically significant.
3. Results
3.1. Literature search results and basic information of included studies
A total of 193 articles were retrieved in the preliminary search. Duplicate articles that did not meet the inclusion criteria were excluded. Finally, 38 articles were included. A total of 3750 patients, including 1875 patients in the experimental group and 1875 patients in the control group, were identified. The literature screening process was shown in Fig. 1. The basic information of the included studies was shown in Table 1.
Fig. 1.
Flow chart of selection process.
Table 1.
Basic information included in literatures.
| Author/Publishing Year | Test group (n) | Control group (n) | Test group treatment | Control group treatment | Course/week | Average age mean (SD) | Outcome indicator |
|---|---|---|---|---|---|---|---|
| Wang Ping (2016) | 50 | 50 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 12 | 48(7.29) | abcd |
| Dai Yuancheng (2013) | 60 | 60 | Xiaoke Decoction + Regraine | Regraine | 8 | 55(1.2) | abc |
| Xie Junyan (2018) | 30 | 30 | Self-made Wuwei Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 4 | 54(1.79) | abc |
| Wen Wu (2018) | 20 | 20 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 8 | 46.2(1.52) | abcd |
| Yang Ling (2014) | 44 | 44 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | – | 48(12.58) | abc |
| Zhou Lai le (2014) | 40 | 40 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | – | 45.5(6.3) | bce |
| Zhang Guoping (2015) | 30 | 30 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 12 | 49.6(7.07) | abcd |
| Shi Ying (2000) | 20 | 20 | Xiaoke Decoction + Glibenclamide + Metformin Tablets | Glibenclamide + Metformin Tablets | – | 53.5(1.52) | abc |
| Zhang Guige (2006) | 20 | 20 | Xiaoke Decoction + Glibenclamide + Metformin Tablets | Glibenclamide + Metformin Tablets | – | 53.5(1.52) | abc |
| Duan Yutong (2012) | 36 | 36 | Xiaoke decoction + Xiaoke Pills + Metformin Tablets | Xiaokepills + Metformin Tablets | – | 55.5(0.5) | abc |
| Li Yu (2014) | 39 | 39 | Xiaoke decoction + Metformin Tablets | Metformin Tablets | – | 42.26(3.84) | bcd |
| Feng Yulian (2016) | 40 | 40 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 8 | 65.8(1.55) | abcd |
| (Eri et al., 2018) | 60 | 60 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 12 | 56.6(8.26) | abc |
| Du Xueyuan (2018) | 50 | 50 | Xiaoke Decoction + Gliclazide Tablets | Gliclazide Tablets | 4 | 50.7(10.93) | abc |
| Zhu Xiaohong (2014) | 39 | 39 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 12 | 48.3(7.03) | a |
| Xie Shujun (2016) | 48 | 48 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 8 | 50.2(7.35) | abcd |
| Wang Haixia (2018) | 45 | 45 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 8 | 45.2(2.24) | abc |
| Zhang Haitao (2017) | 40 | 40 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 8 | 55(9.01) | abcd |
| Li Xiuxia (2010) | 82 | 82 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 8 | 58.76(10.37) | abcd |
| Chen Qi (2013) | 43 | 43 | Self made Xiaoke Decoction + Sitagliptin | Sitagliptin | 12 | 49.2(2.22) | bcd |
| Shan Liangliang (2017) | 62 | 63 | Wuwei Xiaoke Decoction | 1/20 Original medicine + Rice | 4 | 54.1(11.33) | abcd |
| Sun & Chen, 2019 | 42 | 41 | Wuwei Xiaoke decoction + Metformin Tablets | Metformin Tablets | 12 | 46.8(5.22) | abcde |
| Han Junling (2019) | 45 | 45 | Wuwei Xiaoke decoction + Metformin Tablets | Metformin Tablets | 4 | 55.8(8.6) | abcd |
| Zheng Zhenxiong (2014) | 98 | 98 | Matsuba Xiaoke decoction + Damicon + Gehuazhi | Damicon + Gehuazhi | 12 | 56.5(1.5) | abcd |
| Zhang Tao (2017) | 82 | 82 | Huangqi Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 12 | 57.2(8.87) | abcd |
| Lai Changqin (2013) | 60 | 60 | Qijing Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 8 | 50.9(6) | abce |
| Cheng Hongwei (2017) | 40 | 40 | Qidi Xiaoke decoction + Eugenol 25 | Eugenol 25 | 12 | 60.5(6.78) | abcd |
| Xu Yinglie (2015) | 72 | 72 | Jiangtang Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 4 | 53.5(15.4) | abcde |
| Xia Zhengqin (2017) | 146 | 146 | Modified Xiaoke Decoction + Intensive insulin treatment | Intensive insulin treatment | 2 | 53.3(13.15) | bce |
| Liu Yaning (2016) | 50 | 50 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 4 | 52.3(3.4) | bcde |
| Zhu Tingting (2019) | 50 | 50 | Huangqi Xiaoke Decoction + Insulin | Insulin | 8 | 53.5(4.28) | bcd |
| Feng Xiaonan (2017) | 60 | 60 | Huangqi Xiaoke Decoction + Insulin | Insulin | 12 | 48.7(10.1) | bcd |
| Cui Can (2017) | 40 | 40 | Huangqi Xiaoke Decoction + Insulin | Insulin | 8 | 54.4(4.66) | bcd |
| Ge Zhihua (2019) | 44 | 44 | Huangqi Xiaoke Decoction + Insulin | Insulin | 8 | – | abcd |
| Zeng Jibin (2014) | 30 | 30 | Huangqi Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 12 | 54.7(9.63) | abcd |
| Liu Shanghua (2019) | 32 | 32 | Huangqi Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 12 | 62.4(5.2) | a |
| Yan Fengzuo (2015) | 50 | 50 | Tongluo Xiaoke decoctiong + Insulin | Insulin | – | – | abcd |
| Zhang Zhaoxia (2015) (Zhang & Gong, 2015) | 36 | 36 | Xiaoke Decoction + Metformin Tablets | Metformin Tablets | 8 | 64.8(5.5) | abcd |
Note: a: total efficiency; b: FPG; c: 2 h-PBG; d: HbA1c; e: TCM syndrome point.
3.2. Results of evaluation of literature quality
Of the 38 selected papers, 33 mentioned random methods. The remaining five were grouped according to treatment plan, and 38 did not mention allocation and blinding. One mentioned double-blinding, whereas the remaining 37 did not mention double-blinding. The 38 articles were complete with outcome data and selection reports. The bias risk assessments included in the study were shown in Fig. 2, Fig. 3.
Fig. 2.
Overall evaluation results of biased risk assessment included in literature.
Fig. 3.

Biased risk assessment results for each included literature.
3.3. Results of evaluation of included studies
3.3.1. Comparison of total efficiency
The 30 tentative (including 2810 patients) results were compared regarding the total therapeutic efficiency of Xiaoke Decoction combined with western medicine and western medicine only. The number of participants among the trials ranged between 20 and 98. It was found that adding Xiaoke Decoction could improve total efficiency (Fig. 4). The Xiaoke Decoction groups surpassed the western medicine groups in terms of improvement in total efficiency. The OR of the comparison between the Xiaoke Decoction groups and the control groups was 3.49 (95% CI: 2.78–4.39, P < 0.00001).
Fig. 4.
Meta-analysis forest map of efficacy on total efficiency between Xiaoke Decoction groups and control groups.
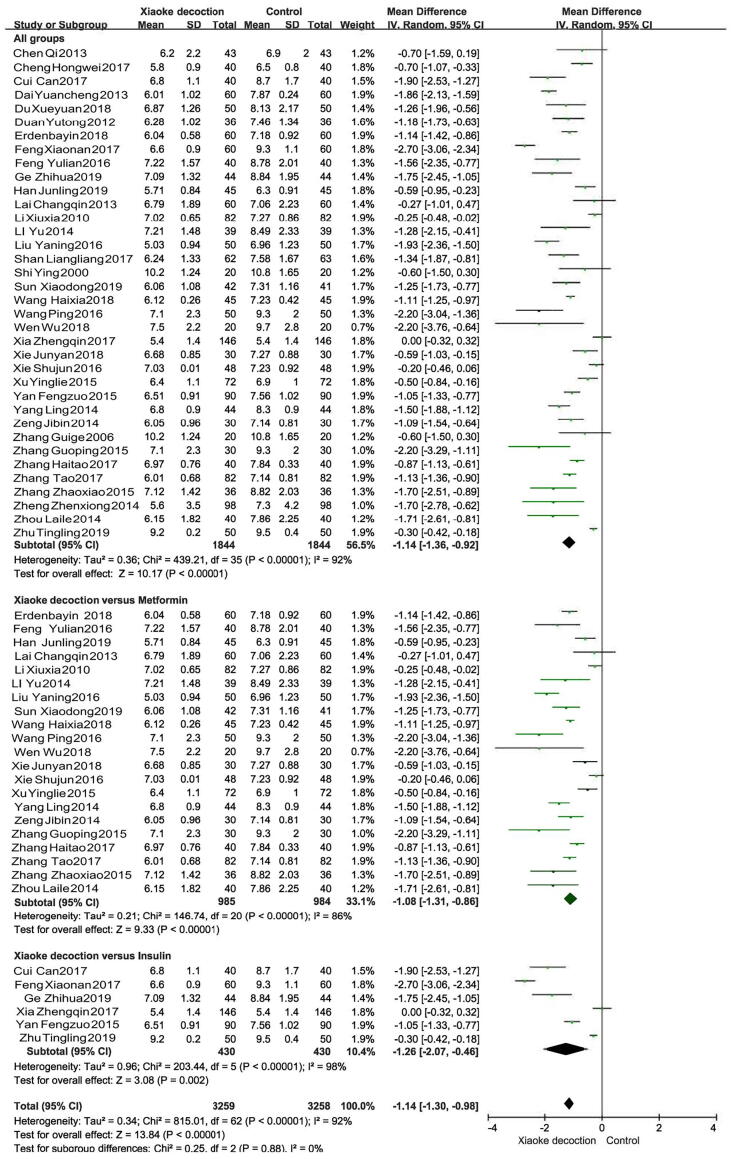
3.3.2. Comparison of FPG
The 36 tentative (including 3688 patients) results compared the therapeutic FPG of Xiaoke Decoction combined with western medicine to that of western medicine only. The number of participants among the trials ranged between 20 and 146. It was found that adding Xiaoke Decoction could lower the FPG (Fig. 5). There was statistical heterogeneity among the studies. The Xiaoke Decoction groups surpassed the western medicine groups in terms of reduction in FPG. The MD between the Xiaoke Decoction groups and control groups was −1.14 (95% CI: −1.36 to −0.92, P < 0.00001).
Fig. 5.
Meta-analysis forest map of FPG in Xiaoke Decoction groups and control groups of patients.
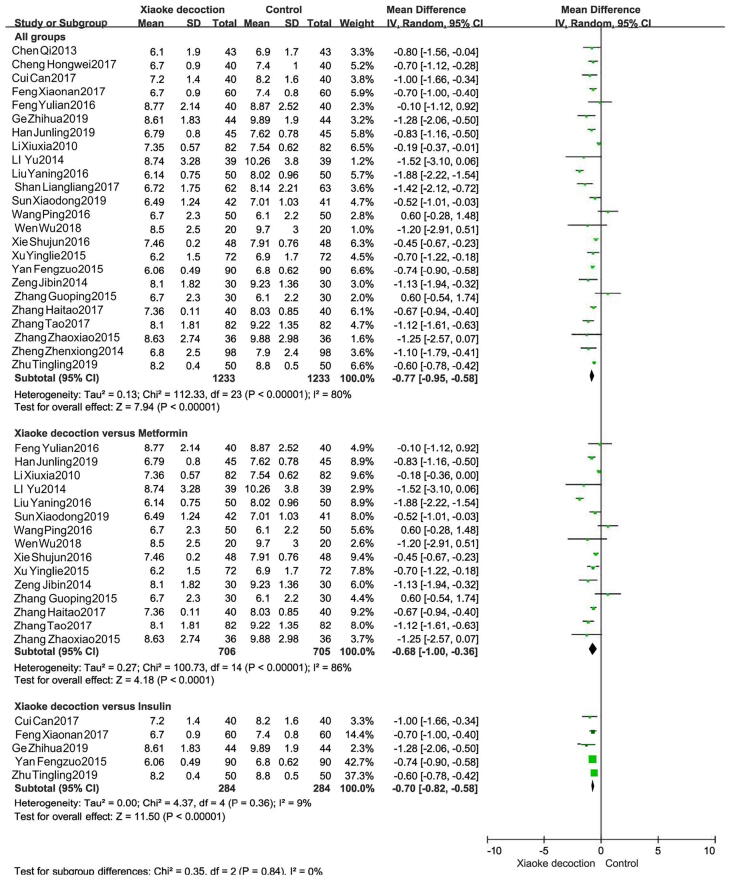
3.3.3. Comparison of 2hPG
The 36 tentative (including 3688 patients) results compared the therapeutic 2hPG of Xiaoke Decoction combined with western medicine to that of western medicine only. The number of participants in the trials ranged between 20 and 146. We found that adding Xiaoke Decoction could lower the 2hPG (Fig. 6). The Xiaoke Decoction groups surpassed the western medicine groups in terms of reduction in 2hPG. The MD between the Xiaoke Decoction groups and control groups was −1.40 (95% CI: −1.61 to −1.19, P < 0.00001).
Fig. 6.
Meta-analysis forest map of 2hPG in Xiaoke Decoction groups and control groups of patients.
3.3.4. Comparison of HbA1c
The 24 tentative (including 2466 patients) results compared the therapeutic HbA1c of Xiaoke Decoction combined with western medicine to that of western medicine only. The number of participants in the trials ranged between 20 and 98. We found that adding Xiaoke Decoction could lower the HbA1c (Fig. 7). The Xiaoke Decoction groups surpassed the western medicine groups in terms of reduction in HbA1c. The MD between the Xiaoke Decoction groups and control groups was −0.77 (95% CI: −0.95 to −0.58, P < 0.00001).
Fig. 7.
Meta-analysis forest map of HbAlc in Xiaoke Decoction groups and control groups of patients.
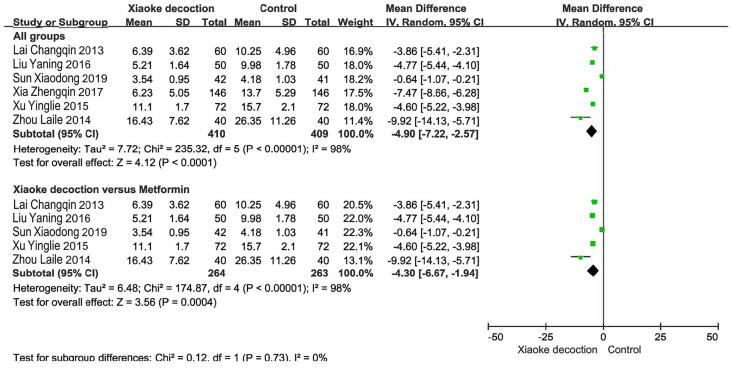
3.3.5. Comparison of TCM syndrome score
The six tentative (including 819 patients) results compared the therapeutic TCM syndrome score of Xiaoke Decoction combined with western medicine to that of western medicine only. The number of participants in the trials ranged between 40 and 146. We found that adding Xiaoke Decoction could lower the TCM syndrome score (Fig. 8). The TCM syndrome score of patients in the Xiaoke Decoction group was obviously lower than that of the control group after treatment. The MD between the Xiaoke Decoction groups and control groups was −4.90 (95% CI: −7.22 to −2.57, P < 0.0001).
Fig. 8.
Meta-analysis forest map of TCM syndrome points in Xiaoke Decoction groups and control groups of patients.
3.4. Analysis of combination of Xiaoke Decoction with metformin and insulin
As Xiaoke Decoction was used in combination with a variety of western medicines, it was necessary to examine the effect of Xiaoke Decoction according to the categories of western medicine. Primarily, 10 western drugs or combinations were included: insulin, metformin tablets, Eugenol 25, Damicon + Gehuazhi, 1/20 original medicine + rice, sitagliptin, gliclazide tablets, Xiaoke Pills + metformin tablets, glibenclamide + metformin tablets, and regraine. Among them, metformin and insulin were the most commonly used. Therefore, the former two medicines were investigated separately in the present study.
Twenty-three studies based on metformin showed that the combined use of Xiaoke Decoction could significantly improve the treatment of diabetes. Twenty of these studies showed that Xiaoke Decoction was effective in improving total efficiency (OR = 3.20, 95% CI: 2.42–4.24, P < 0.00001).
Twenty-one of these studies showed that Xiaoke Decoction was effective in lowering FPG and 2hPG levels (FPG: MD = −1.08, 95% CI: −1.31 to −0.86, P < 0.00001; 2hPG: MD = −1.57, 95% CI: −1.93 to −1.21, P < 0.00001). Fifteen of these studies showed that Xiaoke Decoction was effective in lowering HbA1c levels (MD = −0.68, 95% CI: −1.00 to −0.36, P < 0.0001). Five studies reported that Xiaoke Decoction was effective in reducing the TCM syndrome score (MD = −4.30, 95% CI: −6.67 to −1.94, P = 0.0004). Six studies that assessed the combined use of insulin and Xiaoke Decoction consistently showed that Xiaoke Decoction could effectively reduce FPG levels (MD = −1.26, 95% CI: −2.07 to −0.46, P = 0.002) and 2hPG (MD = −1.55, 95% CI: −2.29 to −0.81, P < 0.00001). Two studies showed that Xiaoke Decoction was effective in improving total efficiency (OR = 4.90, 95% CI: 2.21–10.91, P < 0.0001). Finally, five studies showed that Xiaoke Decoction was effective in lowering HbA1c levels (MD = −0.70, 95% CI: −0.82 to −0.58, P < 0.00001).
3.5. Subgroup analysis
Subgroup analysis according to intervention duration found that in terms of total efficiency, the total efficiency (OR: 4.069) of intervention duration in 9–12 weeks was higher than that in 4–8 weeks. The intervention duration lasted 4–8 weeks; 2hPG (SMD: −1.597; 95% CI: −2.087 to −1.107) and HbA1c (SMD: −0.775; 95% CI: −1.017 to −0.532). The effect was better than 9–12 weeks. Moreover, the effect of FPG was relatively stable after taking Xiaoke Decoction. Subgroup analysis of the <50 age group and ≥50 age group showed that, within age <50, total efficiency (OR: 5.412), FPG (SMD: −1.328; 95% CI: −1.851 to −0.804) and 2hPG (SMD: −0.927; 95% CI: −1.076 to −0.779) had better therapeutic effects than age ≥50. In terms of HbA1c (SMD: −0.693; 95% CI: −0.797 to −0.589), age ≥50 was more effective than age <50 (Table 2).
Table 2.
Relationship between Xiaoke Decoction and western medicine based on subgroup analysis.
| Variables | Xiaoke decoction group (n)/Control group (n) |
Pooled SMD | OR | 95% CI | Z-value | P- value | I-squared/% |
|---|---|---|---|---|---|---|---|
| Intervention duration (weeks) | |||||||
| 4–8 | 732/733 | − | 3.346 | 2.478–4.518 | 7.88 | 0.000 | 0.0 |
| 9–12 | 503/502 | − | 4.069 | 2.722–6.083 | 6.84 | 0.000 | 0.0 |
| FPG | |||||||
| 4–8 | 874/875 | −1.048 | − | −1.366 to 0.729 | 6.44 | 0.000 | 89.7 |
| 9–12 | 535/534 | −1.158 | − | −1.563 to 0.753 | 5.60 | 0.000 | 89.2 |
| 2hPG | |||||||
| 4–8 | 874/875 | −1.597 | − | −2.087 to 1.107 | 6.39 | 0.000 | 95.2 |
| 9–12 | 535/534 | −0.775 | − | −1.017 to 0.532 | 6.26 | 0.000 | 72.1 |
| HbA1c | |||||||
| 4–8 | 609/608 | −0.758 | − | −1.041 to 0.475 | 5.25 | 0.000 | 82.3 |
| 9–12 | 475/474 | −0.428 | − | −0.682 to 0.175 | 3.31 | 0.001 | 72.5 |
| Age | |||||||
| <50 | 270/269 | − | 5.412 | 3.004–9.749 | 5.62 | 0.000 | 0.0 |
| ≥50 | 1003/1004 | − | 3.185 | 2.441–4.155 | 8.54 | 0.000 | 0.0 |
| FPG | |||||||
| <50 | 413/412 | −1.328 | − | −1.851 to 0.804 | 4.97 | 0.000 | 91.2 |
| ≥50 | 1257/1258 | −0.884 | − | −1.135 to 0.634 | 6.92 | 0.000 | 88.7 |
| 2hPG | |||||||
| <50 | 413/412 | −0.927 | − | −1.076 to 0.779 | 12.26 | 0.000 | 90.6 |
| ≥50 | 1257/1258 | −0.736 | − | −0.820 to 0.652 | 17.17 | 0.000 | 94.0 |
| HbA1c | |||||||
| <50 | 284/283 | −0.314 | − | −0.481–0.146 | 3.68 | 0.000 | 72.3 |
| ≥50 | 775/776 | −0.693 | − | −0.797 to 0.589 | 13.10 | 0.000 | 81.1 |
3.6. Source analysis of heterogeneity
The Meta-analysis results of FPG, 2hPG, HbA1c, and TCM syndrome score showed heterogeneity among studies included in the indicators. By eliminating the studies one by one and analyzing the remaining studies, the heterogeneity was still large and showed that the results before and after treatment have not changed significantly. According to the subgroup analysis based on the treatment time, the heterogeneity was still large and showed that the results before and after treatment have not changed, thereby suggesting low sensitivity and high stability. The sensitivity analysis results were shown in Fig. 9.
Fig. 9.
Sensitivity analysis.
3.7. Publication bias
The results of the Meta-analysis including more than 10 articles were evaluated for the risk of publication bias, total efficiency, FPG, 2hPG. The funnel chart showed that the left and right sides were not completely symmetrical with a skewed distribution. At the same time, the egger’s test was performed. Results showed that the total efficiency (t = 7.20, p = 0.00), FPG (t = −3.78, p = 0.001), 2hPG (t = −4.49, p = 0.00) further proves the existence of publication bias, which may be related to the quality of the included literature, the small sample size, or the unpublished negative results. Observe the HbA1c funnel chart and perform egger's test at the same time. HbA1c (t = −0.36, p = 0.725) dots were concentrated on both sides, showing a roughly symmetrical distribution and suggesting that the publication bias of the included literature may be small (Fig. 10).
Fig. 10.
Funnel plot of Meta-analysis.
4. Discussion
The results of 38 articles included in this study show that, based on conventional western medicine treatment, the clinical efficacy of including Xiaoke Decoction in the treatment of type 2 diabetes yielded results which were significantly better than that of the conventional western medicine group. Compared with the conventional western medicine group, we found that there were significant differences in total efficiency, FPG, 2hPG, HbA1c, and TCM syndrome score. Particularly, when we studied metformin or insulin combined with Xiaoke Decoction, the declines in FPG, 2hPG, HbA1c were more obvious. Because of the high heterogeneity among the studies, a subgroup analysis was performed. The results showed that the Xiaoke Decoction group can effectively reduce FPG, 2hPG, and HbA1c in different intervention times, but the treatment effect was obvious during the intervention time (4–8 weeks). The effect stabilized at 9–12 weeks. The results of age showed that: Age <50 has a significant effect, possibly due to the increasing age of patients, the reduction in basic functions and overall level of the body to a certain extent, especially the sensitivity of the patients to drugs had decreased. The prevalence of type 2 diabetes has been high in China. In the past 30 years, the prevalence of adult diabetes in China has seen a significant increase. Studies showed that the prevalence of adult diabetes in China in 2013 was 10.4% (Chinese Diabetes Society, 2018).
Diabetes belongs to the category of “Xiaoke” in TCM and has a history of thousands of years. TCM believes that the loss of yin, body fluids, and internal heat is the main pathogenesis. Among the 38 documents included in this study, 19 had a clear TCM syndrome type. All of which were qi and yin deficiency, and yin deficiency and internal heat syndrome. Therefore, doctors of the past dynasties believed that the treatment of diabetes should be based on clearing the lungs and moisturizing dryness, nourishing yin and promoting fluid, and nourishing the liver and kidneys. Xiaoke Decoction was first seen in Dan xi Zhu's “Dan Xi Xin Fa” in the Yuan Dynasty. The main medicines were Coptidis Rhizoma, Trichosanthis Radix, Lotus Rhizoma, Rehmanniae Radix, Zingiberis Recens Rhizoma, Mel among others. Trichosanthis Radix can promote body fluid production to quench thirst, clear away heat, and moisturize dryness. It also acts as the main medicine. The bitter cold of Coptidis Rhizoma can relieve heart fire. Lotus Rhizome and Rehmanniae Radix can nourish yin and moisturize dryness. All medicines were compatible and used together to nourish yin, moisturize dryness, clear heat, and promote fluid. The purpose is to treat diabetes with the basic functions of nourishing yin and clearing heat. Sun Fenghui et al. (Sun, Wang, & Qiu, 2018) believed that both TCM, TCM prescriptions, and proprietary Chinese medicines were effective in treating type 2 diabetes, and that TCM treatment can also be advantageous in treating the complications of diabetes (Qu, Yang, & Ning, 2018). Therefore, there is a need to develop a combination of TCM and western medicine treatment. Combined Chinese and western medical treatment aim to improve patients quality of life, reduce clinical symptoms of patients, and delay the development of type 2 diabetes.
In summary, compared with western medicine alone, Xiaoke Decoction has more advantages for the treatment of type 2 diabetes with respect to total efficiency, FPG, 2hPG, HbAlc, and TCM syndrome score. However there are still some gaps in knowledge that need to be clarified. Future potential clinical studies should address the following issues: (a) Inconsistencies or lack of standards regarding patients' oral dose and TCM Xiaoke Decoction active ingredient. The dosage of TCM is very important to achieve the ideal therapeutic effect. Changes often affect the curative effect, pharmacological action, and side effects of TCM. Therefore, standardizing dosage and active ingredient content is the basis to ensure clinical efficacy; (b) In recent years, more studies have shown that type 2 diabetes and obesity were interrelated and influenced each other pathologically (Saadeldeen, Niu, & Wang, 2020). In future studies, the influence of diabetes and obesity should be included in the diagnostic indicators; (c) All the included trials were conducted in China, which means that there was a high risk of bias. The sample size of the included literature was small and the quality of the literature was generally low. Therefore, it is necessary to carry out more high-quality and high-level clinical research; (d) At present, there is a lack of clinical trials on the treatment of type 2 diabetes with Xiaoke Decoction alone as compared with western medicine, thereby making it impossible to reveal whether its curative effect was therapeutic or beneficial. Therefore, clinical trials of Xiaoke Decoction alone should be urgently conducted. If there are studies that can make such comparisons, then people can expect Xiaoke Decoction as an independent treatment.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No. 81760776), the Natural Science Foundation of Inner Mongolia Autonomous Region (No. 2018ZD13).
Contributor Information
Cunxia Ren, Email: rcxss@163.com.
Minhui Li, Email: prof_liminhui@yeah.net.
References
- Chen Q., Zheng P.Z., Lin R.K., Zhou Y.L. Clinical observation of sitagliptin combined with self-designed Xiaoke decoction in the treatment of 43 cases of initial type 2 diabetes. Zhejiang Journal of Traditional Chinese Medicine. 2013;48(2):120. [Google Scholar]
- Cheng H.W. Clinical study on Qidi Xiaoke decoction in the treatment of type 2 diabetes. Modern Journal of Integrated Traditional Chinese and Western Medicine. 2017;26(26):2887–2890. [Google Scholar]
- Chinese Diabetes Society. Chinese guidelines for the prevention and treatment of type 2 diabetes (2017 Edition). (2018). Chinese Journal of Practical Internal Medicine. 38(4), 292-344.
- Cui C. Clinical study of Huangqi Xiaoke decoction combined with insulin in the treatment of type Ⅱ diabetes. Asia-Pacific Traditional Medicine. 2017;13(24):152–153. [Google Scholar]
- Dai Y.C. Clinical observation on self-prepared Xiaoke decoction combined with western medicine syndrome differentiation to treat type 2 diabetes. Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease. 2013;21(10):42–43. [Google Scholar]
- Du X.Y. Clinical observation on 100 cases of diabetes treated with modified Xiaoke decoction. China Reflexolocy. 2018;27(12):179–180. [Google Scholar]
- Duan Y.T., Chen Y.L. Xiaoke decoction in the treatment of 36 cases of type Ⅱ diabetes. Shanxi Journal of Traditional Chinese Medicine. 2012;11:60–61. [Google Scholar]
- Eri D.B.Y., Shen G.J., Lu M.J. Efficacy observation of Xiaoke decoction combined with metformin in the treatment of type 2 diabetes. Diabetes World. 2018;15(6):81–82. [Google Scholar]
- Feng X.N., Chu H. Clinical study of insulin with root of remembranous milk vetch to patients with newly diagnosed type 2 diabetes. Chinese Archives of Traditional Chinese Medicine. 2017;35(03):735–737. [Google Scholar]
- Feng Y.L., Yu X. Clinical observation of Xiaoke decoction combined with metformin in the new diagnosis of type 2 diabetes. Clinical Research and Practice. 2016;1:22. [Google Scholar]
- Gong X., Ji M., Xu J., Zhang C., Li M. Hypoglycemic effects of bioactive ingredients from medicine food homology and medicinal health food species used in China. Critical Reviews in Food Science and Nutrition. 2019;60(14):2303–2326. doi: 10.1080/10408398.2019.1634517. [DOI] [PubMed] [Google Scholar]
- Ge Z.H. Clinical analysis of astragalus antithirst prescription combined with insulin in treatment of type 2 diabetes mellitus. Smart Healthcare. 2019;5(09):82–83. [Google Scholar]
- Han J.L. Clinical observation of Wuwei Xiaoke decoction combined with metformin in the treatment of type 2 diabetes. China's Naturopathy. 2019;27(13):37–38. [Google Scholar]
- Jin H.Y., Jin J.G. Clinical efficacy of Jianpi Ziyin Xiaoke decoction in patients with type 2 diabetes mellitus of qi-yin deficiency syndrome and its effects on insulin sensitivity and β cell function. Chinese Journal of Information on Traditional Chinese Medicine. 2019;26(07):35–39. [Google Scholar]
- Lai C.Q. Observation on the curative effect of Qijing Xiaoke decoction on 60 cases of type 2 diabetes. Journal of Fujian University of Traditional Chinese Medicine. 2016;23(03):52–53. [Google Scholar]
- Li X.X. Observation on the curative effect of Xiaoke decoction Jia jian on 82 cases of type 2 diabetes. Guide of China Medicine. 2010;8(5):60–61. [Google Scholar]
- Li Y. Application of Xiaoke decoction in the treatment of type 2 diabetes. The Chinese and Foreign Health Abstract. 2014;23:47–48. [Google Scholar]
- Liu S.H. Effect of Huang qi Xiaoke decoction on patients with type 2 diabetes of qi-yin deficiency type. Renowned Doctor. 2019;2019(01):237. [Google Scholar]
- Liu, Y.N. 2016. Effect of modified Xiaoke decoction combined with metformin on clinical indicators of patients with type 2 diabetes of qi-deficiency and blood-stasis pattern. World Chinese Medicine. 11(11), 2271-2273+2277.
- Ministry of Health. Guiding Principles for Clinical Research of New Chinese Medicines. Beijing: China Medical Science and Technology Press. 237, 362-364.
- Qu C., Yang Y.F., Ning S.Y., et al. Meta-analysis on Xuefu Zhuyu Decoction for treatment of diabetic retinopathy. Journal of Liaoning University of Traditional Chinese Medicine. 2018;20(09):184–188. [Google Scholar]
- Saadeldeen F.S.A., Niu Y., Wang H., Zhou L., Meng L., Chen S., et al. Natural products: Regulating glucose metabolism and improving insulin resistance. Food Science and Human Wellness. 2020;9(3):214–228. [Google Scholar]
- Shan L.L., Deng X.M., Guo C.M., et al. Clinical observation of Wuwei Xiaoke decoction in treatment of type 2 diabetes with qi and yin deficiency. Chinese Journal of Experimental Traditional Medical Formulae. 2017;23(24):170–174. [Google Scholar]
- Shi Y., Su L. Xiaoke decoction in the treatment of 20 cases of type 2 diabetes. Shandong Journal of Traditional Chinese Medicine. 2001;6:345–346. [Google Scholar]
- Sun, F. H., Wang, Q. H., Qiu, Z. L., et al. (2018). Research progress of mechanisms of traditional Chinese medicine in treatment of insulin resistance of type 2 diabetes mellitus. Medical Recapitulate. 24(20), 4068-4072+4077. 10.3969/j.issn.1006-2084.2018.20.021.
- Sun X.D., Chen T. Efficacy of Wuwei Xiaoke decoction in the treatment of type 2 diabetes with qi and yin deficiency. Practical Clinical Journal of Integrated Traditional Chinese and Western Medicine. 2019;19:20–22. [Google Scholar]
- Wang H.X., Feng X.Y. Application and feasibility study of Xiaoke decoction in the treatment of type 2 diabetes. Diabetes New World. 2018;21(05):33–34. [Google Scholar]
- Wang P. Clinical observation on 100 cases of type 2 diabetes treated by self-made Xiaoke decoction. Family Medicine. Medical Treatment and Selection. 2016;7:138–139. [Google Scholar]
- Wen W. Observation of curative effect of traditional Chinese medicine Xiaoke decoction combined with western medicine on type 2 diabetes. Chinese Community Doctor. 2018;34(22):88–90. [Google Scholar]
- Xia Z.Q., Dai L. Observation of clinical efficacy of Jiawei Xiaoke decoction in the treatment of first-onset type 2 diabetes. Diabetes New World. 2017;20(11):93–94. [Google Scholar]
- Xie J.Y., Wang Z.G., Deng X.M. Clinical observation on 30 cases of type 2 diabetes treated by addition and subtraction of Wuwei Xiaoke decoction. Hunan Traditional Chinese Medicine. 2018;34(1):60–61. [Google Scholar]
- Xie, S. J. (2016). Efficacy of Xiaoke decoction in the treatment of patients with type 2 diabetes. Cardiovascular Disease Journal of Integrated Traditional Chinese and Western Medicine. 4(16), 169-169.
- Xu Y.L., Huang Y.S. Clinical observation on Jiangtang Xiaoke decoction in the treatment of type 2 diabetes. Shanxi Journal of Traditional Chinese Medicine. 2015;36(12):1608–1609. [Google Scholar]
- Yan, Z. F. (2015). Observation of clinical effects of TongLuo Xiaoke decoctionon treating diabetes. Journal of Clinical Rational Drug Use. 8(28), 48-49+52.
- Yang L. Observation of curative effect of traditional Chinese medicine Xiaoke decoction combined with western medicine on type 2 diabetes. Clinical Journal of Chinese Medicine. 2014;19:114–115. [Google Scholar]
- Zeng J.B., Pan Y., Huang Y.L., et al. Effect of Huangqi Xiaoke decoction on traditional Chinese medical symptoms of type 2 diabetes mellitus patients with deficiency of both qi and yin. Journal of New Chinese Medicine. 2014;46(04):146–148. [Google Scholar]
- Zhang, G. G. (2006). Xiaoke decoction in the treatment of 20 cases of type 2 diabetes. Journal of Henan University of Chinese Medicine. 21(4), 42-42.
- Zhang G.P. Xiaoke decoction for 60 cases of type 2 diabetes. Traditional Chinese Medicinal Research. 2015;2:25–26. [Google Scholar]
- Zhang, H. T. (2017). Clinical observation on 40 cases of type 2 diabetes treated by Xiaoke decoction. China Pharmaceuticals. A02, 93-93.
- Zhang T. Changes of glucose and lipid metabolism of patients with type 2 diabetes with syndrome of deficiency of qi-yin after Huangqi xiaoke decoction treatment (syndrome of deficiency of qi-yin) after Huangqi xiaoke decoction. Journal of Baotou Medical College. 2017;33(02):92–93. [Google Scholar]
- Zhang T.T., Jiang J.G. Active ingredients of traditional Chinese medicine in the treatment of diabetes and diabetic complications. Expert Opinion on Investigational Drugs. 2012;21(11):1625–1642. doi: 10.1517/13543784.2012.713937. [DOI] [PubMed] [Google Scholar]
- Zhang Z.X., Gong H.R. Clinical value of traditional Chinese medicine Xiaoke decoction combined with western medicine in the treatment of type 2 diabetes. Diabetes New World. 2015;2015(06):62–63. [Google Scholar]
- Zheng Z.X., Zheng Y.Y., Lin C.G., Yao X. Clinical observation of pine diabetes decoction on the treatment of type 2 diabetes. Guide of China Medicine. 2014;12(32):44–45. [Google Scholar]
- Zhou L.L. Clinical study of Xiaoke decoction in the treatment of type Ⅱ diabetes of yin deficiency and heat. Special Health. 2014;6:81–82. [Google Scholar]
- Zhu, T. T. (2019). Clinical summary analysis of Huangqi Xiaoke decoction combined with insulin in the treatment of newly diagnosed type Ⅱ diabetes. Healthful Friend. 2019, (13).
- Zhu X.H. Observation on the curative effect of Xiaoke decoction in the treatment of first-onset type 2 diabetes. Clinical Journal of Chinese Medicine. 2014;6(23):43–44. [Google Scholar]