Abstract
BACKGROUND
There is mounting empirical evidence of the detrimental effects of the coronavirus disease 2019 (COVID-19) outbreak on mental health. Previous research has underscored the effects of similar destabilizing situations such as war, natural disasters or other pandemics on acute stress levels which have been shown to exacerbate current and future psychopathological symptoms.
AIM
To explore the role of acute stress responses (intrusive, avoidance and hyperarousal) as mediators in the association between fear of COVID-19 and emotional dysfunction-related problems: Depression, agoraphobia, panic, obsessive-compulsive, generalized anxiety, social anxiety and health anxiety symptoms.
METHODS
A sample of 439 participants from a university community in Spain (age: mean ± SD: 36.64 ± 13.37; 73.1% females) completed several measures assessing their fear of COVID-19, acute stress responses and emotional dysfunction syndromes through an online survey. Data collection was carried out from the start of home confinement in Spain until May 4, 2020, coinciding with initial de-escalation measures. Processing of the dataset included descriptive and frequency analyses, Mann-Whitney U Test of intergroup comparisons and path analysis for direct and indirect effects. This is an observational, descriptive-correlational and cross-sectional study.
RESULTS
The prevalence of clinical symptoms in our sample, reported since the beginning of the pandemic, reached 31.44%. The female group presented higher scores although the effect size was small. Overall, the participants who exceeded the clinical cut-off points in emotional problems showed higher levels of fear of COVID-19 and of cognitive, motor and psychophysiological responses of acute stress, unlike the group with normative scores. In addition, the results show significant mediated effects of hyperarousal stress among fear of COVID-19 and emotional dysfunction psychopathology. However, the clinical syndromes most related to the consequences of the pandemic (e.g., social contact avoidance or frequent hand washing), such as agoraphobia and obsessive-compulsive symptoms, were in fact predicted directly by fear of COVID-19 and/or the acute stress response associated with the pandemic and had a greater predictive power.
CONCLUSION
The present study illustrates a clearer picture of the role of acute stress on several forms of psychopathology during the COVID-19 crisis and home confinement.
Keywords: Fear of COVID-19, Acute stress, Emotional dysfunction, Psychophysiological activation, Mediated effects
Core Tip: This study provides the prevalence of emotional dysfunction which reached 30% during the confinement stage in Spain. Our results point to higher levels of fear of coronavirus disease 2019 (COVID-19) and acute stress in participants with purely clinical symptoms compared with the normative group. We found clinically relevant associations between emotional dysfunction, fear of COVID-19 and acute stress. The mediated role of a psychophysiological activation response to explain indirect effects from fear of COVID-19 on various clinical syndromes is emphasized. These results support the need to include a therapeutic component of acute stress management in prevention and psychological intervention strategies in the face of exceptional events of a traumatic nature.
INTRODUCTION
Initial psychological impact of coronavirus disease 2019
The coronavirus disease 2019 (COVID-19) pandemic has had an enormously consequential impact not just on financial and health systems worldwide, but also in day-to-day life. In many countries, a strict home confinement was implemented initially which resulted in a dramatic shift in a society’s freedom of movement and general lifestyle affecting the population’s mental health. Issues ranging from sleep quality to mood and anxiety disorders have been widely and closely scrutinized[1-3]. The incidence of depressive, anxiety-related, and acute stress moderate/severe symptoms in general population has been estimated around 16%, 28% and 8%, respectively[4-6], especially because of social isolation[7]. Prevalence of other psychopathological symptoms (e.g., health anxiety) may have been dramatically increased and exacerbated by the outbreak of an infectious disease such as COVID-19[8]. In fact, preliminary evidence points toward the detrimental effects of COVID-19-related to quarantine on mental health as it has shown links to depression, stress, panic attacks, phobic symptoms, low mood and post-traumatic stress symptoms[9]. Considering that the symptoms of acute, as well as chronic stress [and in its most severe manifestation, posttraumatic stress disorder, (PTSD)[10]] have been associated with an array of destabilizing situations, such as war[11], financial crises[12] and natural disasters[13], and also with the psychopathology associated with trauma[14,15]. Exploring the effects of stress and its consequences during the COVID-19 outbreak seems important both theoretically and clinically.
Fear, stress reactions and psychopathology
Prior research has highlighted the important role of psychological reactions such as infection-related fear, anxiety and uncertainty in the face of epidemics and pandemics, underscoring the high prevalence of mental health symptoms in these circumstances[16]. In the current environment, studies have already been published on stress-related symptoms, the onset of which have been contingent with the coronavirus outbreak in patients[17] and in medical staff and the general population[18-20]. Acute stress could not only explain psychopathological manifestations, but its association with fear is also directly linked to anxious and mood disorders[10]. Fear has shown to be sensitized by acute traumatic stress[21], where stressful life events can lead to maladaptive, fear-related behaviors, facilitating the development of anxiety-related disorders[22,23]. Acute stress has been found to modulate the effects of fear on learning paradigms in humans, increasing the resistance to extinction in the case of cue-dependent fear[24]. The influence among fear and stress is reciprocal, such that stress responses are found to be more severe in the concurrent experience of fear[25]. In the context of the COVID-19 pandemic, this relation may yield greater psychopathological manifestations in at-risk patients as well as in the general population.
Mediated effects from stress
Experiencing fear in critical conditions such as pandemics, natural disasters and financial crises has shown to lead to symptoms of acute stress which in some cases may persist and lead to forms of chronic stress[13] and other psychological problems like depression or anxiety[26]. Stress is a common symptom in several manifestations of psychopathology in the short and long-term[27] as well as an important antecedent toward the development of many different emotional dysfunction problems[28].
Several specific stress symptoms are described within the literature such as avoidance behaviors, hyperarousal or intrusive thoughts. Also, differentiated long-term effects from different types of symptoms are commonly found. For instance, intrusive recall is often described as a predictor of chronic stress[29]. Thus, it is normal to expect that these types of symptoms are related to several forms of stress (such as trauma and stress-related disorders). In contrast, the manifestation of hyperarousal would be a predictor of other stress responses such as avoidance and reexperiencing, thereby highlighting its distinctive nature in the expression of severe posttraumatic distress[30]. Moreover, it is also described as a strong predictor of psychological impact severity[31]. General acute stress, on its part, would be a determinant of future emotional recovery[32]. To our knowledge, there is very little evidence on the distinct effects of different stress responses on the psychopathology linked to COVID-19. As such, exploring early stress responses, especially hyperarousal, may be highly relevant toward prevention plans during stressful life events such as a health crisis derived from a pandemic.
Present study
The main purpose of this study is to clarify the mediated role of acute stress reactions (i.e. intrusive reexperiencing, motor and cognitive avoidance strategies and psychophysiological activation) to explain the association between fear of COVID-19 and emotional dysfunction (i.e. depression, agoraphobia, panic, obsessive-compulsive, generalized anxiety, social anxiety and health anxiety symptoms). As secondary objectives, to examine the clinical prevalence and sex differences of emotional dysfunction and acute stress reported since the beginning of the pandemic and during confinement. Additionally, to compare levels of COVID-19 fear and acute stress among groups of participants with normative vs clinical scores on the different psychopathological syndromes and examine the associations between the study variables.
Based on the literature described above, we expected to find prevalence rates of emotional dysfunction and acute stress in the 10%-30% range, especially among the female group. We also expected to identify higher levels of fear of COVID-19 and acute stress in participants with scores above the cutoff point in the different clinical syndromes; and a positive, significant and clinically relevant raw association between all variables under study. Lastly, we expected that fear of COVID-19 and all seven assessed syndromes would be mainly indirectly linked via hyperarousal stress, such that higher fear of COVID-19 would be related to higher hyperarousal, which in turn would be associated with higher reports of psychological symptoms.
MATERIALS AND METHODS
Participants and procedure
The present study is part of the project PSICO-RECURSOS COVID-19, developed and implemented by the Centre of Applied Psychology from the Health Psychology Department at Miguel Hernández University in Elche (Alicante, Spain). This initiative arose with the goal of determining the psychological impact brought on by COVID-19 in the general population and underscores the influence of personal psychological resources such as resilience, coping strategies, socioemotional competencies and healthy habits. This is a descriptive-correlational, observational, cross-sectional study. Data collection was carried out employing self-reports which were completed through the application Detecta-Web, constructed with LimeSurvey software. Participation throughout the whole study process was completely voluntary. Anonymity and confidentiality of the data were also ensured by emphasizing its use exclusively for academic and/or research purposes. Approval for this study was granted by the Ethics Committee of Miguel Hernández University (reference: DPS.JPR.01.20).
Thus, an initial sample of 660 participants from a university community were recruited until the 4th of May, the end of full confinement and beginning of de-escalation measures. Only participants who endorsed active acceptance to participate voluntarily and consented to use of the data and those that completed measures about fear of COVID-19, psychopathology and stress were included in the final analysis. Thereby, the final sample was composed of 439 participants (age: mean ± SD: 36.64 ± 13.37) where an overrepresentation of females was observed (73.1%; n = 321). As for employment situation of the participants, 34.9% (n = 153) were university students studying for state exams or civil servants; 52.2% (n = 229) were active workers, including full-time and part-time workers, freelance workers and scholarship holders; and 12.8% (n = 56) were unemployed, affected by temporary layoffs, currently on sick leave or retired, among others.
Measures
For all measures, composite scores were created by averaging items. Higher scores indicated higher levels of the constructs.
Fear of COVID-19 scale[33]: This scale assesses fear of COVID-19 through 7 items answered on a 5-point, Likert-type scale, reflecting agreement with each statement (1: Totally agree; 5: Totally disagree). The total score ranges from 7 to 35, with higher values indicating a greater fear of COVID-19.
Impact of event scale-revised[34]: This instrument allows for assessment of the three core symptoms of acute stress contemplated by the Diagnostic and Statistical Manual of Mental Disorders (DSM)[10], regardless of its version: (1) Intrusive reexperiencing symptoms; (2) Motor and cognitive avoidance strategies; and (3) Level of psychophysiological activation. The impact of event scale-revised has 22 items and is answered on a 5-point Likert-type scale, reflecting the degree to which the symptoms are experienced (0: Absent or very mild; 4: Very severe). For this study, the content and verbal tenses of instructions and items were adapted to contextualize the stressful event to the COVID-19 health crisis and subsequent mandatory confinement measures.
Anxiety and depression disorders symptoms scale, ESTAD[35]: This instrument was designed to assess internalizing psychopathology according to the DSM-5[10]. Specifically, it allows for evaluation of agoraphobia, panic, generalized anxiety, social anxiety, obsessive-compulsive, health anxiety and depressive symptoms. The ESTAD consists of 36 items and is answered on a 5-point Likert-type scale (0: Never or almost never, 4: Always or almost always). The instructions were slightly modified to limit the questionnaire’s scope to the beginning of the health crisis brought on by COVID-19 and mandatory home confinement measures.
Statistical analyses
Prior to processing the dataset, the reliability of the psychological assessment measures was tested (Cronbach’s alpha; criteria value α > 0.70). Accordingly, descriptive (mean ± SD) and frequency (%) analyses were carried out to examine the clinical prevalence of emotional dysfunction problems, acute stress and fear of COVID-19 from the cutoff points reported in the respective validation studies. Then, a double intergroup comparison was made: (1) Sex differences for all study variables; and (2) Differences in fear of COVID-19 and acute stress associated to pandemic variables, according to the grouping of participants scoring above/below the cutoff point (normative vs clinical) for each psychological syndrome (alpha level: P < 0.001). For this purpose, the non-parametric Mann-Whitney U Test was used after ascertaining non-normality and heterogeneity of variances in all hypothesized comparisons (results of these previous analyses are available upon request). The effect size was calculated using Hedges’ g (criteria values g: Approximately 0.20 small, approximately 0.50 medium, approximately 0.80 large). Then, the raw association between all the variables under study was analyzed using Pearson's correlation (magnitude criteria values r: Approximately 0.10 small, approximately 0.30 medium, approximately 0.50 large). This analysis block was performed using the IBM® SPSS® Statistics 27 software.
To explore the mediating role of acute stress between fear of COVID-19 and internalized psychopathology, a fully saturated path model was conducted using Mplus 8.4 software. Within the model, fear of COVID-19 was introduced as a predictor variable; acute stress in the form of avoidance, intrusive and hyperarousal reaction as a mediated variable; and psychopathological syndromes (agoraphobia, panic, generalized anxiety, social anxiety, obsessive-compulsive, health anxiety, and depressive symptoms) as output variables. Age and sex were entered as covariates in the model because of the differences observed among Spanish research[36] and even in this study. Missing data were handled using full information maximum likelihood[37]. Moreover, we examined the total, direct and indirect effects using bias-corrected bootstrapped estimates[38] based on 10000 bootstrapped samples which provides a powerful test of mediation[39] and is also robust to small departures from normality[40]. Statistical significance was determined by 99% bias-corrected bootstrapped confidence intervals not containing zero due to the sample size.
RESULTS
Descriptive data and sex differences
The prevalence of clinical symptoms reported since the beginning of the pandemic was 31.44% for agoraphobia, 13.44% for obsessive-compulsive, 11.62% for health anxiety, 11.39% for panic and social anxiety, 11.16% for depression and 8.43% for generalized anxiety in the whole sample. Likewise, the psychological impact of the health crisis in terms of acute stress was 21.18% severe, 6.83% moderate, 17.54% mild and 54.44% normative. The fear of COVID-19 scale does not have Spanish cutoff points to determinate its clinical prevalence among this sample. In addition, analysis of sex differences reported slightly higher scores in the female group although the effect size was small (Table 1).
Table 1.
Descriptive data and sex differences
| Study variables | α |
Total sample, n = 439
|
Females, n = 321
|
Males, n = 118
|
Mann-Whitney U test
|
|||||
|
Mdn
|
Rng
|
Mdn
|
Rng
|
Mdn
|
Rng
|
U
|
P
value
|
g
|
||
| Fear of COVID-19 | 0.84 | 15 | 26 | 15 | 26 | 13 | 23 | 26026 | < 0.001 | 0.37 |
| Avoidance stress | 0.83 | 8 | 28 | 9 | 27 | 6 | 23 | 15317 | < 0.001 | 0.42 |
| Intrusive stress | 0.83 | 7 | 27 | 7 | 27 | 6 | 23 | 16208 | 0.001 | 0.38 |
| Hyperarousal stress | 0.84 | 6 | 27 | 7 | 25 | 5 | 27 | 16771 | 0.003 | 0.30 |
| Depression | 0.86 | 2 | 20 | 3 | 20 | 2 | 17 | 15536 | 0.004 | 0.27 |
| Agoraphobia | 0.83 | 3 | 19 | 3 | 19 | 2 | 15 | 16309 | 0.024 | 0.22 |
| Obsessive-Compulsive | 0.69 | 4 | 17 | 4 | 17 | 4 | 15 | 18604 | 0.775 | 0.01 |
| Panic | 0.88 | 1 | 19 | 1 | 19 | 0 | 16 | 16480 | 0.027 | 0.28 |
| Health anxiety | 0.87 | 3 | 20 | 3 | 18 | 3 | 20 | 17374 | 0.180 | 0.15 |
| Generalized anxiety | 0.91 | 5 | 20 | 6 | 20 | 3 | 20 | 13322 | < 0.001 | 0.50 |
| Social anxiety | 0.84 | 3 | 20 | 4 | 19 | 2 | 20 | 15102 | 0.001 | 0.33 |
COVID-19: Coronavirus disease 2019; Mdn: Median; Rng: Range; U: Mann-Whitney U test; Hedge’s g effect size: Approximately 0.20 small, approximately 0.50 medium, approximately 0.80 large.
Comparisons between clinical vs normative groups
Table 2 presents comparisons in fear of COVID-19 and acute stress that were made according to the grouping of participants with normative vs clinical scores for each psychological syndrome. Fear of COVID-19 was clinically higher among participants who exceeded the cutoff point for health anxiety, panic, agoraphobia, and obsessive-compulsive syndromes (P < 0.001; g from 0.84 to 1.17); while no differences were identified as reported in depression, generalized anxiety and social anxiety (P > 0.001). Motor and cognitive avoidance strategies were mostly found among clinical groups of generalized anxiety and social anxiety (P < 0.001; g from 0.80 to 0.87). In this respect, no differences were identified in avoidance stress according to obsessive-compulsive and health anxiety indicators (P > 0.001). All clinical groups of emotional dysfunction problems presented high intrusive re-experiencing levels associated with the pandemic (P < 0.001), especially pronounced in panic, health anxiety and generalized anxiety syndromes (g from 1.04 to 1.45). However, it was in the level of psychophysiological activation where the most statistically (P < 0.001) and clinically (g > 0.80) relevant intergroup differences were invariably found. In this regard, the differences between the normative and clinical groups of depression, panic and generalized anxiety presented a particularly large effect size (g from 1.57 to 1.70). In the remaining intergroup comparisons analyzed, a moderate effect size was observed (g approximately 0.50).
Table 2.
Mann-Whitney U Test according to the grouping of participants above/below the cutoff point in emotional dysfunction, n = 439
| Emotional dysfunction | n |
Fear of COVID-19
|
Acute stress associated to COVID-19 pandemic
|
|||||||||||||||||||
|
Avoidance stress
|
Intrusive stress
|
Hyperarousal stress
|
||||||||||||||||||||
|
Mdn
|
Rng
|
U
|
P
value
|
g
|
Mdn
|
Rng
|
U
|
P
value
|
g
|
Mdn
|
Rng
|
U
|
P
value
|
g
|
Mdn
|
Rng
|
U
|
P
value
|
g
|
|||
| Depression | ≤ 8 | 390 | 15 | 26 | 9080 | 0.515 | 0.15 | 7 | 28 | 6045 | < 0.001 | 0.69 | 6 | 26 | 5140 | < 0.001 | 0.91 | 5 | 22 | 2821 | < 0.001 | 1.60 |
| ≥ 9 | 49 | 15 | 26 | 11 | 27 | 12 | 26 | 14 | 27 | |||||||||||||
| Agoraphobia | ≤ 4 | 301 | 14 | 25 | 11712 | < 0.001 | 0.86 | 7 | 28 | 15261 | < 0.001 | 0.53 | 6 | 26 | 11894 | < 0.001 | 0.80 | 5 | 22 | 12931 | < 0.001 | 0.83 |
| ≥ 5 | 138 | 17.5 | 26 | 10 | 27 | 10 | 27 | 10 | 27 | |||||||||||||
| Obsessive-Compulsive | ≤ 8 | 380 | 14 | 26 | 6931 | < 0.001 | 0.84 | 8 | 28 | 9584 | 0.060 | 0.32 | 6 | 26 | 7616 | < 0.001 | 0.66 | 6 | 22 | 6707 | < 0.001 | 0.86 |
| ≥ 9 | 59 | 19 | 26 | 9 | 27 | 12 | 27 | 10 | 27 | |||||||||||||
| Panic | ≤ 5 | 389 | 14 | 25 | 5844 | < 0.001 | 0.90 | 7 | 28 | 5779 | < 0.001 | 0.79 | 6 | 26 | 4269 | < 0.001 | 1.16 | 5 | 22 | 3147 | < 0.001 | 1.57 |
| ≥ 6 | 50 | 19.5 | 26 | 11.5 | 26 | 12 | 25 | 14 | 25 | |||||||||||||
| Health anxiety | ≤ 8 | 388 | 14 | 22 | 4551 | < 0.001 | 1.17 | 8 | 28 | 8011 | 0.022 | 0.33 | 7 | 27 | 5591 | < 0.001 | 1.04 | 6 | 25 | 5013 | < 0.001 | 1.07 |
| ≥ 9 | 51 | 21 | 26 | 10 | 27 | 13 | 24 | 12 | 27 | |||||||||||||
| Generalized anxiety | ≤ 14 | 402 | 15 | 26 | 6009 | 0.046 | 0.49 | 8 | 28 | 3915 | < 0.001 | 0.87 | 6 | 26 | 2676 | < 0.001 | 1.45 | 6 | 22 | 2033 | < 0.001 | 1.70 |
| ≥ 15 | 37 | 16 | 26 | 13 | 23 | 14 | 23 | 16 | 23 | |||||||||||||
| Social anxiety | ≤ 9 | 388 | 15 | 26 | 7438 | 0.003 | 0.47 | 8 | 27 | 6277 | < 0.001 | 0.80 | 6 | 26 | 5276 | < 0.001 | 0.91 | 6 | 22 | 5242 | < 0.001 | 0.96 |
| ≥ 10 | 51 | 16 | 26 | 12 | 28 | 12 | 26 | 11 | 27 | |||||||||||||
COVID-19: Coronavirus disease 2019; ≤/≥: Normative/clinical cutoff points of ESTAD; Mdn: Median; Rng: Range; U: Mann-Whitney U test; Hedge’s g effect size: Approximately 0.20 small, approximately 0.50 medium, approximately 0.80 large.
Association between study variables
Bivariate correlations and general descriptive statistics for each measure are presented in Table 3. Fear of COVID-19 showed positive and significant associations (P < 0.001) with the three forms of acute stress manifestation, especially large with intrusive re-experiencing (r = 0.55). It also presented positive and significant correlations with the totality of psychopathological syndromes (P < 0.001). As expected, fear of COVID-19 was more strongly associated with health anxiety symptoms than others (r = 0.56). Also, a medium magnitude of association was observed between this construct and agoraphobia, obsessive-compulsive, panic, and generalized anxiety symptoms (r from 0.36 to 0.41); while it was weakly linked to depression and social anxiety (r = 0.18 and 0.24, respectively). In turn, the correlation between acute stress and clinical syndromes associated to the pandemic was also positive and significant (P < 0.001). Avoidant strategies did not show strong relation magnitudes with emotional dysfunction problems, but moderate ones with panic, agoraphobia, depression, and generalized anxiety (r from 0.30 to 0.45). Intrusive and hyperarousal stress showed large associations with generalized anxiety and panic (r from 0.52 to 0.68). Depression and psychophysiological activation were also strongly associated (r = 0.63). The correlation of the sociodemographic data with the variables under study was very small (r < 0.28).
Table 3.
Bivariate correlations and descriptive statistics among all study variables
|
No.
|
|
1
|
2
|
3
|
4
|
5
|
6
|
7
|
8
|
9
|
10
|
11
|
| 1 | Fear of COVID-19 | 1 | ||||||||||
| 2 | Avoidance stress | 0.39c | 1 | |||||||||
| 3 | Intrusive stress | 0.55c | 0.60c | 1 | ||||||||
| 4 | Hyperarousal stress | 0.45c | 0.60c | 0.80c | 1 | |||||||
| 5 | General anxiety | 0.36c | 0.45c | 0.59c | 0.68c | 1 | ||||||
| 6 | Depression | 0.18c | 0.36c | 0.45c | 0.63c | 0.71c | 1 | |||||
| 7 | Agoraphobia | 0.41c | 0.30c | 0.41c | 0.40c | 0.52c | 0.42c | 1 | ||||
| 8 | Social Anxiety | 0.24c | 0.27c | 0.38c | 0.40c | 0.59c | 0.55c | 0.56c | 1 | |||
| 9 | Panic | 0.39c | 0.37c | 0.52c | 0.61c | 0.69c | 0.63c | 0.60c | 0.54c | 1 | ||
| 10 | Obsessive-Compulsive | 0.40c | 0.20c | 0.32c | 0.33c | 0.43c | 0.31c | 0.56c | 0.43c | 0.46c | 1 | |
| 11 | Health anxiety | 0.56c | 0.27c | 0.44c | 0.45c | 0.54c | 0.36c | 0.49c | 0.42c | 0.52c | 0.56c | 1 |
| 12 | Sex | 0.15b | 0.18c | 0.17c | 0.14b | 0.22c | 0.12a | 0.10a | 0.15b | 0.12a | -0.00 | 0.07 |
| 13 | Age | 0.08 | -0.20c | -0.07 | -0.24c | -0.28c | -0.27c | -0.10a | -0.24c | -0.12a | -0.08 | -0.04 |
P < 0.05.
P < 0.01.
P < 0.001.
Sex was coded 0 = male, 1 = female. COVID-19: Coronavirus disease 2019.
Mediation model results
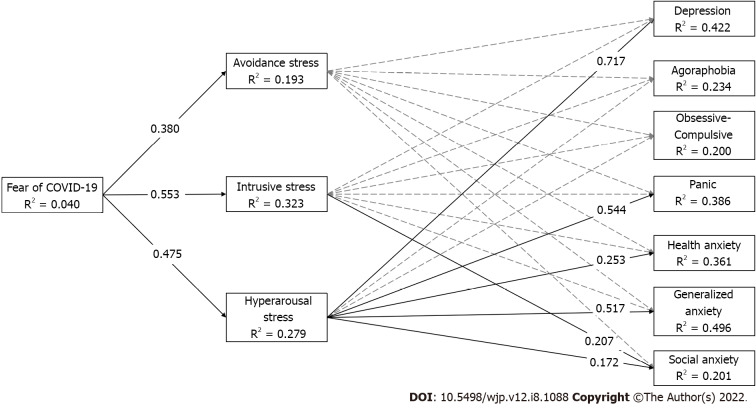
Total, direct and indirect effects are summarized in Figure 1 and Table 4. Significant direct effects (99%CI) from fear of COVID-19 to all three types of acute stress reactions (intrusive, hyperarousal and avoidance stress) were observed. Moreover, a significant direct effect from intrusive re-experiencing symptoms on social anxiety was found. Hyperarousal stress significantly predicted depression, panic, health anxiety, generalized anxiety and social anxiety symptoms. Among mediation effects, depression and generalized anxiety symptoms were significant and fully mediated via hyperarousal stress such that the higher fear of COVID-19 was related to higher levels of psychophysiological activation which in turn was related to higher levels of depression (β = 0.340, 99%CI: 0.236, 0.460) and generalized anxiety symptoms (β = 0.245, 99%CI: 0.162, 0.343). Similarly, significant partial mediated effects from fear of COVID-19 to panic and health anxiety symptoms were observed such that more fear of COVID-19 led to higher levels of hyperarousal which in turn led to more endorsement of panic (β = 0.258, 99%CI: 0.155, 0.382) and health anxiety symptoms (β = 0.120, 99%CI: 0.025, 0.229). It is important to note that significant positive direct effects between fear of COVID-19 and some types of emotional dysfunction (i.e. agoraphobia, OCD, panic, and health anxiety) were still observed even when accounting for the effects of all variables.
Figure 1.
Estimated path mediation model. Significant associations are indicated by the solid line for emphasis and were determined by a 99% bias-corrected standardized bootstrapped confidence interval (based on 10000 bootstrapped samples) that does not contain zero. Effects from covariates (age and sex) are omitted for parsimony but results are available upon request. COVID-19: Coronavirus disease 2019.
Table 4.
Summary of total, indirect, and direct effects of mediation models
|
Predictor variable: Fear of COVID-19
|
Depression
|
Agoraphobia
|
Obsessive-Compulsive
|
Panic
|
Health anxiety
|
Generalized anxiety
|
Social anxiety
|
| Total | 0.197 (0.074, 0.316) | 0.423 (0.296, 0.535) | 0.423 (0.295, 0.536) | 0.402 (0.252, 0.533) | 0.569 (0.463, 0.663) | 0.376 (0.261, 0.487) | 0.253 (0.115, -0.379) |
| Total indirect | 0.293 (0.190, 0.402) | 0.143 (0.006, 0.232) | 0.083 (0.006, 0.166) | 0.253 (0.166, 0.346) | 0.111 (0.035, 0.203) | 0.310 (0.211, 0.414) | 0.183 (0.100, 0.276) |
| Avoidance stress | -0.007 (-0.058, 0.041) | 0.006 (-0.067, 0.080) | -0.024 (-0.091, 0.042) | -0.012 (-0.068, 0.045) | -0.031 (-0.088, 0.020) | -0.002 (-0.050, 0.043) | -0.013 (-0.077, 0.053) |
| Intrusive stress | -0.041 (-0.145, 0.064) | 0.070 (-0.066, 0.208) | 0.034 (-0.080, 0.147) | 0.007 (-0.118, 0.134) | 0.023 (-0.092, 0.148) | 0.067 (-0.024, 0.167) | 0.114 (-0.013, 0.241) |
| Hyperarousal stress | 0.340 (0.236, 0.460) | 0.067 (-0.047, 0.197) | 0.073 (-0.028, 0.188) | 0.258 (0.155, 0.382) | 0.120 (0.025, 0.229) | 0.245 (0.162, 0.343) | 0.082 (-0.013, 0.189) |
| Direct | -0.096 (-0.224, 0.026) | 0.281 (0.135, 0.411) | 0.340 (0.196, 0.475) | 0.148 (0.009, 0.289) | 0.458 (0.340, 0.568) | 0.066 (-0.056, 0.193) | 0.069 (-0.076, 0.206) |
β (99%CI): Significant associations were determined by a 99% bias-corrected standardized bootstrapped confidence interval (based on 10000 bootstrapped samples) that does not contain zero. COVID-19: Coronavirus disease 2019.
DISCUSSION
The first objective of this study was to examine the clinical prevalence of emotional dysfunction problems and acute stress reported since the beginning of the pandemic and during the home confinement stage in Spain, in addition to analyzing sex differences. In line with our hypotheses, a prevalence ranging between 8.34% and 31.44% was found for clinical syndromes. In addition, 45.56% of the sample exceeded the cutoff score of acute stress, 21.18% at severe levels. The female group presented higher scores in all study variables although the effect size was small. In obsessive-compulsive and health anxiety symptoms, mostly associated with pandemic, sex differences were practically non-existent; however, the effect of this sociodemographic variable was controlled for in subsequent analyses. Previous studies in Spanish samples found similar prevalence in the assessment of anxious-depressive states and of specific fears during the same stage of the pandemic, also with a higher affectation in the female group[36], although obtaining lower scores for acute stress levels (i.e. approximately 15%)[7,41]; findings which are in the same vein as international studies[9]. In this regard, the selection of assessment instruments, diagnostic cut-off points, data collection methods, and idiosyncratic characteristics of samples, were highly heterogeneous among different studies focused on the psychological impact of COVID-19. This points to the need for standardized diagnostic assessment protocols that would allow for accurate and reliable comparisons between different groups and specific contexts (e.g., cross-cultural studies).
The following objective was to compare levels of fear of COVID-19 and acute stress responses among normative vs clinical groups on the different psychopathological syndromes and analyze the association between all variables in the study. Then, we expected to identify higher levels of these constructs in participants with scores above the clinical cutoff point and a positive, significant and clinically relevant raw association between the variables. In comparison terms, clinical groups reported higher levels of fear of COVID-19 and acute stress reactions than the normative group. In addition, the raw association between variables was positive, significant and of a medium-to-large magnitude in almost all cases. In this regard, previous studies identified a significant exacerbation of symptoms in patients with specific psychopathological conditions, mostly associated with fear of COVID-19, worries and psychosocial stress generated by the pandemic[42], especially in health anxiety syndrome[8]. This finding highlights the need to provide special attention to psychologically vulnerable groups.
The last and main purpose of this study was to examine the (in)direct association between fear of COVID-19 and emotional dysfunction via intrusive, avoidance and hyperarousal acute stress reactions. In terms of predictive capability, and in line with the hypotheses, significant direct effects of fear of COVID-19 were found on motor and cognitive avoidance strategies, level of psychophysiological activation and especially intrusive re-experiencing symptoms. In this context, studies have already been published on stress-related symptoms, the onset of which have been contingent with the coronavirus outbreak in patients, medical staff and the general population[17-20]. To re-iterate a previous point, the influence among fear and stress is reciprocal, such that stress responses are found to be more severe in the concurrent experience of fear[25]. In addition, this construct presented direct effects on agoraphobia, obsessive-compulsive, panic and health anxiety symptoms but not on depression, generalized anxiety and social anxiety. Acute stress associated to the pandemic showed, on the other hand, direct effects of intrusive re-experiencing on social anxiety while the level of psychophysiological activation had a strong influence on depression, panic and generalized anxiety and to a lesser extent on health anxiety and social anxiety. Avoidant acute stress did not present any direct effects. In this respect, different authors point to fear of illness, self-isolation/confinement and decreased quality of life having dramatically increased the level of stress-related disorders in the population. These symptoms and early warning signs may become episodic or chronic psychopathological problems[13,16,26-28,43].
The analysis of indirect effects of fear of COVID-19 on the different psychopathological syndromes showed a marked tendency of hyperactive stress to mediate this relation in line with previous longitudinal data[31]. Specifically, relevant indirect effects were found on health anxiety, generalized anxiety and, especially, on depression and panic symptoms. This indicates that they were not predicted simply by the level of fear of COVID-19, but that a third variable was needed to observe a significant relationship like other studies where early stress response determined the subsequent psychological impact more than simple direct exposure[44]. This may point toward these symptoms being more reactive to the emergency posed by COVID-19 and, thereby, require special attention. Avoidant and intrusive acute stress, on the other hand, did not demonstrate a mediating role between fear of COVID-19 and psychopathological profiles assessed. In addition, none of the manifestations of acute stress had a direct or mediated influence on agoraphobia and obsessive-compulsive symptoms; in other words, these clinical syndromes, most related to the consequences of the pandemic (e.g., social contact avoidance or frequent hand washing), were directly related to fear of COVID-19 with a greater predictive power. In this regard, Sandín's study identified intolerance to uncertainty and overexposure to the media as the main risk factors associated with fear of COVID-19[6]. On the one hand, the transdiagnostic nature of intolerance to uncertainty is purported to influence the etiopathogenesis of emotional disorders, especially anxiety disorders[45]. On the other hand, the informative overexposure to the coronavirus through different media would have a direct negative effect on the levels of anxiety, worry and insomnia[46,47]. These findings should be considered as preventive measures.
In summation, the psychophysiological activation of stress would be a strong point to consider in developing specific protocols for screening, clinical assessment and early intervention of the psychological impact of the COVID-19 outbreak as a cost-effective way of dealing with trauma-consequences[30,31,48]. Also, interventions that may help to lower distress during the subsequent phases in overcoming COVID-19 may be of greater relevance given the evidenced association with other psychopathological syndromes[49-52] and/or other dimensional categories, such as specific fears and other distress syndromes such as PTSD[53]. Thus, a transdiagnostic approach intervention based on reducing the manifestation and dysfunctionality of initial psychological impact produced by fear of COVID-19 and acute stress reactions could be decisive in preventing future comorbidities and/or serious mental health problems. These results may be of interest and serve as a basis for future research related to other exceptional situations of a traumatic nature such as the current war in Ukraine.
Limitations and future lines of research
Whereas we believe that this study contributes to the evidence of psychopathological symptoms being linked to COVID-19, some limitations should be considered. Due to the cross-sectional study design, it is not possible to infer causal relations between the variables. In this sense, it is considered relevant to longitudinally test whether the persistence of high levels of acute stress, especially in its hyperarousal manifestation, predicts a worse prognosis of the reported psychopathology. It would also be appropriate to consider the use of different representative samples, in terms of age (e.g., adolescents) and other groupings (e.g., clinical populations), individual-vulnerability factors related to disasters[26] and other idiosyncratic characteristics (e.g., personality traits, especially neuroticism[54]). Also, it is important to note that this study was conducted during the COVID-19 pandemic, thereby specific factors of the confinement situation (e.g., remote work, uncertainty and lack of control associated with the alarm state, among others) could be affecting our findings. It is also important to underscore that given the adaptation of measures to the COVID-19 situation, our findings revolve around reactive and specific symptoms to the current environment. Therefore, we cannot extrapolate the results to other, more general settings. In any case, these findings are much in line with previous studies.
CONCLUSION
Fear of COVID-19 is indirectly related to several psychopathological syndromes (generalized anxiety, depression, health anxiety and panic) via specific hyperarousal acute stress. Thereby, higher levels of psychophysiological activation led to explain the indirect effect of fear of COVID-19 during the global “crisis” on the emotional dysfunction observed. The present study extends the literature on the relevant role of acute stress in better understanding the origin, development and exacerbation of different symptoms of psychopathology in a similar social-health context. It also responds to the call made to provide and expand the evidence on the early psychological impact of these events and their related factors contributing to the construction of an empirical basis for the design of preventive and intervention strategies during the "de-escalation" process and other future stages of this global crisis.
ARTICLE HIGHLIGHTS
Research background
The coronavirus disease 2019 (COVID-19) pandemic and initial home confinement stage have had an indisputable psychological impact on society. Previous studies show that similar destabilizing events of a traumatic nature have resulted in the origin and exacerbation of current and future psychopathological symptoms in which fear plays a key role. In this sense, scientific literature underlines the importance of early reduction of the initial acute stress response to that fear since its continuity over time could be the prelude to more severe clinical conditions (e.g., post-traumatic stress disorder).
Research motivation
This study sought to elucidate a threefold question: (1) Does fear of COVID-19 produce emotional dysfunction problems? (2) Does the level of acute stress play a mediating role between fear of COVID-19 and psychopathological symptoms? and (3) If affirmative, do the 3 core symptoms of acute stress (i.e. intrusive re-experiencing, motor and cognitive avoidance strategies and psychophysiological activation) equally modulate this relation? Knowing the answer to these questions would allow us to identify the pandemic risk factors that contribute to the manifestation and chronicity of associated psychopathology.
Research objectives
The main purpose of this study is to explore the role of acute stress responses (intrusive, avoidance and hyperarousal) as mediators in the association between fear of COVID-19 and emotional dysfunction problems: Depression, agoraphobia, panic, obsessive-compulsive, generalized anxiety, social anxiety and health anxiety symptoms. As secondary objectives: (1) To examine the clinical prevalence and sex differences; (2) To compare levels of COVID-19 fear and acute stress among groups of participants with normative vs clinical scores on the psychopathological syndromes; and (3) To examine the associations between the study variables.
Research methods
This is an observational, descriptive-correlational and cross-sectional study. Data collection was conducted through an online survey since the beginning of the pandemic and during the home confinement stage in Spain. It was disseminated among the members of the university community (n = 439; age: mean ± SD = 36.64 ± 13.37; 73.1% females). Processing of the dataset included descriptive and frequency analyses, Mann-Whitney U Test of intergroup comparisons and path analysis using the double software: IBM® SPSS® Statistics 27 and Mplus 8.4.
Research results
The main findings indicate that the hyperarousal stress assume mediator role among fear of COVID-19 and emotional dysfunction. However, the clinical syndromes most related to the consequences of the pandemic (i.e. agoraphobia and obsessive-compulsive symptoms) were predicted directly by fear of COVID-19 and/or the acute stress response associated with the pandemic. In addition, the prevalence of clinical symptoms reached 31.44%. The female group presented higher scores although the effect size was small. Overall, the participants who exceeded the clinical cut-off points in emotional problems showed higher levels of fear of COVID-19 and acute stress.
Research conclusions
Our findings highlight the mediator role of hyperarousal response to explain indirect effects from the fear of COVID-19 on the origin, development and exacerbation of psychopathological syndromes. These results provide an empirical basis for reducing the psychological impact of the pandemic through selection of more targeted intervention techniques and application in future similar social and health conditions.
Research perspectives
We consider it relevant to longitudinally test whether the persistence of high levels of acute stress, especially in its hyperarousal manifestation, predicts a worse prognosis of the reported psychopathology. It would also be appropriate to consider the use of different representative samples and even analyze whether this psychological component of fear and acute stress influences the manifestation, course and prognosis of COVID-19 disease as previous studies in the field of Health Psychology have shown (for instance, in cancer patients).
ACKNOWLEDGEMENTS
We acknowledge the special collaboration and support of Vicerrectorado de Inclusión, Sostenibilidad y Deportes of Universidad Miguel Hernández, especially to Raul Reina-Vaillo, for making this study possible. PSICO-RECURSOS COVID-19 study group is composed of (in alphabetical order): Raquel Falcó, Universidad Miguel Hernández; Agustín E Martínez-González, Universidad de Alicante; Juan C Marzo, Universidad Miguel Hernández; Ornela Mateu, Universidad Miguel Hernández; Beatriz Moreno-Amador, Universidad Miguel Hernández; David Pineda, Universidad Miguel Hernández; Jose A Piqueras, Universidad Miguel Hernández; Maria Rivera-Riquelme, Universidad Miguel Hernández; Tíscar Rodríguez-Jiménez, Universidad de Zaragoza; Victoria Soto-Sanz, Universidad Miguel Hernández; Verónica Vidal-Arenas, Universitat Jaume I.
Footnotes
Institutional review board statement: The study was reviewed and approved by Oficina de Investigación Responsable of Órgano Evaluador de Proyectos of Universidad Miguel Hernández, No. DPS.JPR.02.17.
Informed consent statement: All study participants and their legal guardian provided informed written consent prior to study enrollment.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
STROBE statement: The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: March 20, 2022
First decision: May 30, 2022
Article in press: July 16, 2022
Specialty type: Psychiatry
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El Sayed S, Egypt; Wang DJ, China S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
Contributor Information
Raquel Falcó, Department of Health Psychology and Center for Applied Psychology, Universidad Miguel Hernández, Elche 03202, Alicante, Spain.
Verónica Vidal-Arenas, Department of Basic and Clinical Psychology and Psychobiology, Universitat Jaume I, Castelló de la Plana 12071, Castellón, Spain. vvidal@uji.es.
Jordi Ortet-Walker, Department of Basic and Clinical Psychology and Psychobiology, Universitat Jaume I, Castelló de la Plana 12071, Castellón, Spain.
Juan C Marzo, Department of Health Psychology and Center for Applied Psychology, Universidad Miguel Hernández, Elche 03202, Alicante, Spain.
José A Piqueras, Department of Health Psychology and Center for Applied Psychology, Universidad Miguel Hernández, Elche 03202, Alicante, Spain.
PSICO-RECURSOS COVID-19 Study Group, Department of Health Psychology and Center for Applied Psychology, Universidad Miguel Hernández, Elche 03202, Alicante, Spain.
Data sharing statement
The dataset and outputs are available upon request.
References
- 1.Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, Worthman CM, Yardley L, Cowan K, Cope C, Hotopf M, Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li J, Zhang YY, Cong XY, Ren SR, Tu XM, Wu JF. 5-min mindfulness audio induction alleviates psychological distress and sleep disorders in patients with COVID-19. World J Clin Cases. 2022;10:576–584. doi: 10.12998/wjcc.v10.i2.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sandín B, Valiente RM, García-Escalera J, Chorot P. Impacto psicológico de la pandemia de COVID-19: Efectos negativos y positivos en población española asociados al periodo de confinamiento nacional. Revista Psicopa Psicol Clín. 2020;25:1–22. [Google Scholar]
- 7.Dos Santos ERR, Silva de Paula JL, Tardieux FM, Costa-E-Silva VN, Lal A, Leite AFB. Association between COVID-19 and anxiety during social isolation: A systematic review. World J Clin Cases. 2021;9:7433–7444. doi: 10.12998/wjcc.v9.i25.7433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asmundson GJG, Taylor S. Coronaphobia: Fear and the 2019-nCoV outbreak. J Anxiety Disord. 2020;70:102196. doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Psychiatric Association. DSM-5. Diagnostic and statistical manual of mental disorders, 5th ed. Arlington (VA), 2013. [Google Scholar]
- 11.Morina N, Stam K, Pollet TV, Priebe S. Prevalence of depression and posttraumatic stress disorder in adult civilian survivors of war who stay in war-afflicted regions. A systematic review and meta-analysis of epidemiological studies. J Affect Disord. 2018;239:328–338. doi: 10.1016/j.jad.2018.07.027. [DOI] [PubMed] [Google Scholar]
- 12.Mucci N, Giorgi G, Roncaioli M, Fiz Perez J, Arcangeli G. The correlation between stress and economic crisis: a systematic review. Neuropsychiatr Dis Treat. 2016;12:983–993. doi: 10.2147/NDT.S98525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beaglehole B, Mulder RT, Frampton CM, Boden JM, Newton-Howes G, Bell CJ. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychiatry. 2018;213:716–722. doi: 10.1192/bjp.2018.210. [DOI] [PubMed] [Google Scholar]
- 14.Bryant RA, Harvey AG. Relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry. 1998;155:625–629. doi: 10.1176/ajp.155.5.625. [DOI] [PubMed] [Google Scholar]
- 15.Ma ZR, Ma WH, Idris S, Pan QW, Baloch Z. COVID-19 impact on high school student's education and mental health: A cohort survey in China. World J Psychiatry. 2021;11:232–241. doi: 10.5498/wjp.v11.i6.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. United Kingdom: Cambridge Scholars Publishing, 2019. [Google Scholar]
- 17.Bo HX, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, Wu X, Xiang YT. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. 2021;51:1052–1053. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cai CZ, Lin YL, Hu ZJ, Wong LP. Psychological and mental health impacts of COVID-19 pandemic on healthcare workers in China: A review. World J Psychiatry. 2021;11:337–346. doi: 10.5498/wjp.v11.i7.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, Bi J, Zhan G, Xu X, Wang L, Zhou Q, Zhou C, Pan Y, Liu S, Zhang H, Yang J, Zhu B, Hu Y, Hashimoto K, Jia Y, Wang H, Wang R, Liu C, Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020;88:916–919. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou ZQ, Yuan T, Tao XB, Huang L, Zhan YX, Gui LL, Li M, Liu H, Li XD. Cross-sectional study of traumatic stress disorder in frontline nurses 6 mo after the outbreak of the COVID-19 in Wuhan. World J Psychiatry. 2022;12:338–347. doi: 10.5498/wjp.v12.i2.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perusini JN, Meyer EM, Long VA, Rau V, Nocera N, Avershal J, Maksymetz J, Spigelman I, Fanselow MS. Induction and Expression of Fear Sensitization Caused by Acute Traumatic Stress. Neuropsychopharmacology. 2016;41:45–57. doi: 10.1038/npp.2015.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. 2000;61 Suppl 7:22–32. [PubMed] [Google Scholar]
- 23.Rosen JB, Schulkin J. From normal fear to pathological anxiety. Psychol Rev. 1998;105:325–350. doi: 10.1037/0033-295x.105.2.325. [DOI] [PubMed] [Google Scholar]
- 24.Simon-Kutscher K, Wanke N, Hiller C, Schwabe L. Fear Without Context: Acute Stress Modulates the Balance of Cue-Dependent and Contextual Fear Learning. Psychol Sci. 2019;30:1123–1135. doi: 10.1177/0956797619852027. [DOI] [PubMed] [Google Scholar]
- 25.Johnson LR. Editorial: How Fear and Stress Shape the Mind. Front Behav Neurosci. 2016;10:24. doi: 10.3389/fnbeh.2016.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonanno GA, Brewin CR, Kaniasty K, Greca AM. Weighing the Costs of Disaster: Consequences, Risks, and Resilience in Individuals, Families, and Communities. Psychol Sci Public Interest. 2010;11:1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- 27.O'Donnell ML, Bryant RA, Creamer M, Carty J. Mental health following traumatic injury: toward a health system model of early psychological intervention. Clin Psychol Rev. 2008;28:387–406. doi: 10.1016/j.cpr.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Slavich GM. Psychopathology and stress. In: Miller HL. The SAGE encyclopedia of theory in psychology. Thousand Oaks: Sage, 2016: 762-764. [Google Scholar]
- 29.Baum A. Stress, intrusive imagery, and chronic distress. Health Psychol. 1990;9:653–675. doi: 10.1037//0278-6133.9.6.653. [DOI] [PubMed] [Google Scholar]
- 30.Marshall GN, Schell TL, Glynn SM, Shetty V. The role of hyperarousal in the manifestation of posttraumatic psychological distress following injury. J Abnorm Psychol. 2006;115:624–628. doi: 10.1037/0021-843X.115.3.624. [DOI] [PubMed] [Google Scholar]
- 31.Schell TL, Marshall GN, Jaycox LH. All symptoms are not created equal: the prominent role of hyperarousal in the natural course of posttraumatic psychological distress. J Abnorm Psychol. 2004;113:189–197. doi: 10.1037/0021-843X.113.2.189. [DOI] [PubMed] [Google Scholar]
- 32.O'Donnell ML, Elliott P, Lau W, Creamer M. PTSD symptom trajectories: from early to chronic response. Behav Res Ther. 2007;45:601–606. doi: 10.1016/j.brat.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 33.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict. 2022;20:1537–1545. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Báguena MJ, Villarroya E, Beleña A, Díaz A, Roldán C, Reig R. Psychometric properties of the Spanish version of the Impact of Event Scale-Revised (IES-R) Análisis y Modificación de Conducta. 2001;27:581–604. [Google Scholar]
- 35.Sandín B, Valiente RM, Pineda D, García-Escalera J, Chorot P. Escala de Síntomas de los Trastornos de Ansiedad y Depresión (ESTAD): Datos preliminares sobre su estructura factorial y sus propiedades psicométricas. Revista de Psicopatología y Psicología Clínica. 2018;23:163–177. [Google Scholar]
- 36.Odriozola-González P, Planchuelo-Gómez A, Irurtia MJ, de Luis-García R. Psychological symptoms of the outbreak of the COVID-19 confinement in Spain. J Health Psychol. 2022;27:825–835. doi: 10.1177/1359105320967086. [DOI] [PubMed] [Google Scholar]
- 37.Muthén LK, Muthén BO. Mplus user’s guide. 8th ed. Los Ángeles (CA), 2017. [Google Scholar]
- 38.Efron B, Tibshirani R. An introduction to the bootstrap. CRC Monographs on Statistics and Applied Probability 1993; In press. [Google Scholar]
- 39.Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychol Sci. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Erceg-Hurn DM, Mirosevich VM. Modern robust statistical methods: an easy way to maximize the accuracy and power of your research. Am Psychol. 2008;63:591–601. doi: 10.1037/0003-066X.63.7.591. [DOI] [PubMed] [Google Scholar]
- 41.Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36:e00054020. doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- 42.Quittkat HL, Düsing R, Holtmann FJ, Buhlmann U, Svaldi J, Vocks S. Perceived Impact of Covid-19 Across Different Mental Disorders: A Study on Disorder-Specific Symptoms, Psychosocial Stress and Behavior. Front Psychol. 2020;11:586246. doi: 10.3389/fpsyg.2020.586246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kotova OV, Medvedev VE, Akarachkova ES, Belyaev AA. [COVID-19 and stress-related disorders] Zh Nevrol Psikhiatr Im S S Korsakova. 2021;121:122–128. doi: 10.17116/jnevro2021121052122. [DOI] [PubMed] [Google Scholar]
- 44.Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. JAMA. 2002;288:1235–1244. doi: 10.1001/jama.288.10.1235. [DOI] [PubMed] [Google Scholar]
- 45.Sandín B, Chorot P, Valiente RM. Transdiagnóstico: Nueva frontera en psicología clínica. Revista de Psicopatología y Psicología Clínica. 2012;17:185–203. [Google Scholar]
- 46.Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15:e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083. doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Collaborating Centre for Mental Health (UK) Post-Traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care. Leicester (UK): Gaskell; 2005. [PubMed] [Google Scholar]
- 49.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 50.Hirschfeld RM. The Comorbidity of Major Depression and Anxiety Disorders: Recognition and Management in Primary Care. Prim Care Companion J Clin Psychiatry. 2001;3:244–254. doi: 10.4088/pcc.v03n0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hopwood CJ, Bagby RM, Gralnick T, Ro E, Ruggero C, Mullins-Sweatt S, Kotov R, Bach B, Cicero DC, Krueger RF, Patrick CJ, Chmielewski M, DeYoung CG, Docherty AR, Eaton NR, Forbush KT, Ivanova MY, Latzman RD, Pincus AL, Samuel DB, Waugh MH, Wright AGC, Zimmermann J. Integrating psychotherapy with the hierarchical taxonomy of psychopathology (HiTOP) J Psychother Integr . 2020;30:477–497. [Google Scholar]
- 52.Soto-Sanz V, Castellví P, Piqueras JA, Rodríguez-Marín J, Rodríguez-Jiménez T, Miranda-Mendizábal A, Parés-Badell O, Almenara J, Alonso I, Blasco MJ, Cebrià A, Gabilondo A, Gili M, Lagares C, Roca M, Alonso J. Internalizing and externalizing symptoms and suicidal behaviour in young people: a systematic review and meta-analysis of longitudinal studies. Acta Psychiatr Scand. 2019;140:5–19. doi: 10.1111/acps.13036. [DOI] [PubMed] [Google Scholar]
- 53.Ruggero CJ, Kotov R, Hopwood CJ, First M, Clark LA, Skodol AE, Mullins-Sweatt SN, Patrick CJ, Bach B, Cicero DC, Docherty A, Simms LJ, Bagby RM, Krueger RF, Callahan JL, Chmielewski M, Conway CC, De Clercq B, Dornbach-Bender A, Eaton NR, Forbes MK, Forbush KT, Haltigan JD, Miller JD, Morey LC, Patalay P, Regier DA, Reininghaus U, Shackman AJ, Waszczuk MA, Watson D, Wright AGC, Zimmermann J. Integrating the Hierarchical Taxonomy of Psychopathology (HiTOP) into clinical practice. J Consult Clin Psychol. 2019;87:1069–1084. doi: 10.1037/ccp0000452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kroencke L, Geukes K, Utesch T, Kuper N, Back MD. Neuroticism and emotional risk during the COVID-19 pandemic. J Res Pers. 2020;89:104038. doi: 10.1016/j.jrp.2020.104038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset and outputs are available upon request.